End of Life Care Education MODULE 1 Module



- Slides: 23
End of Life Care Education MODULE 1 Module 2 End of Life Care Symptom Management
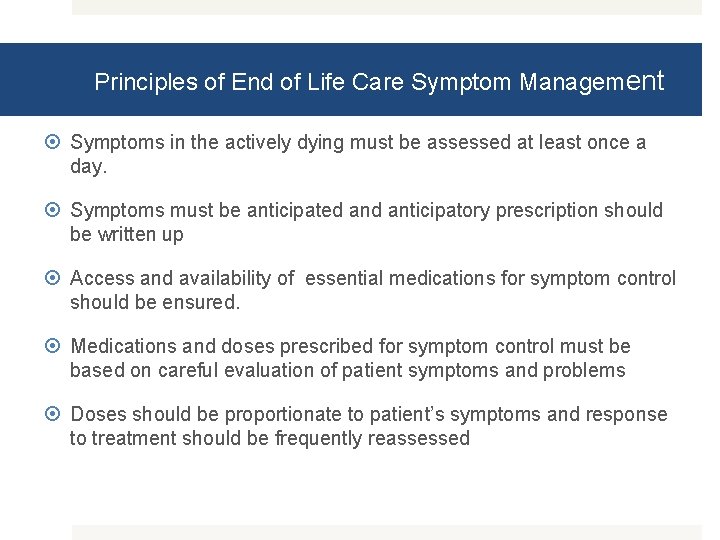
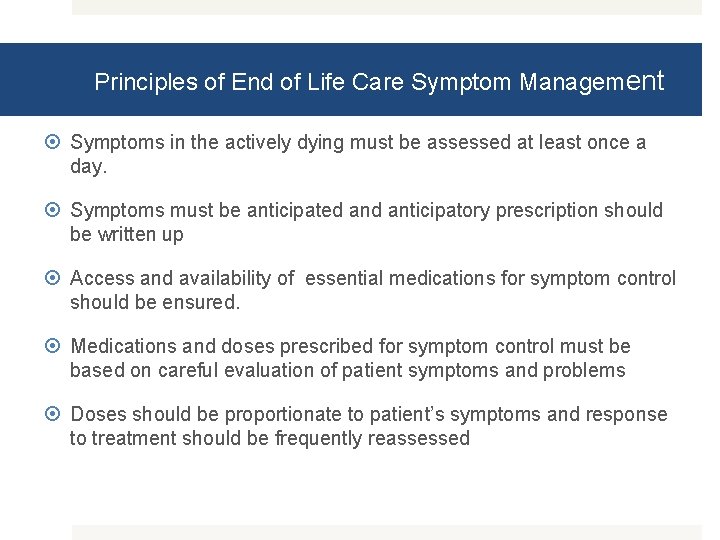
Principles of End of Life Care Symptom Management Symptoms in the actively dying must be assessed at least once a day. Symptoms must be anticipated anticipatory prescription should be written up Access and availability of essential medications for symptom control should be ensured. Medications and doses prescribed for symptom control must be based on careful evaluation of patient symptoms and problems Doses should be proportionate to patient’s symptoms and response to treatment should be frequently reassessed
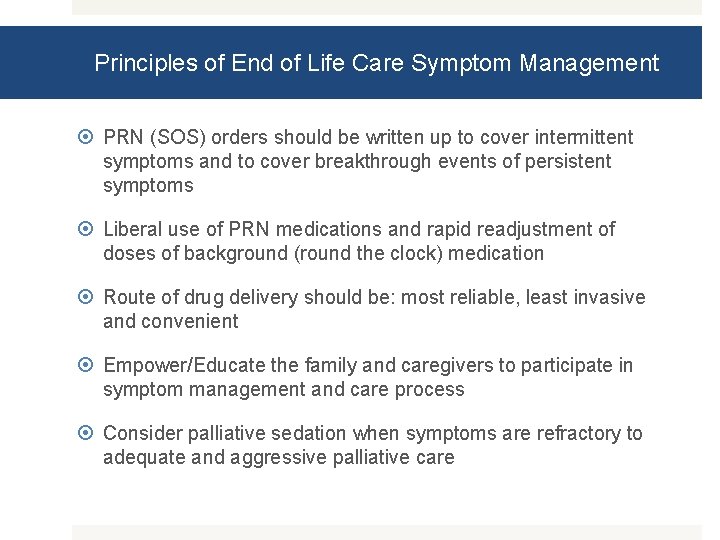
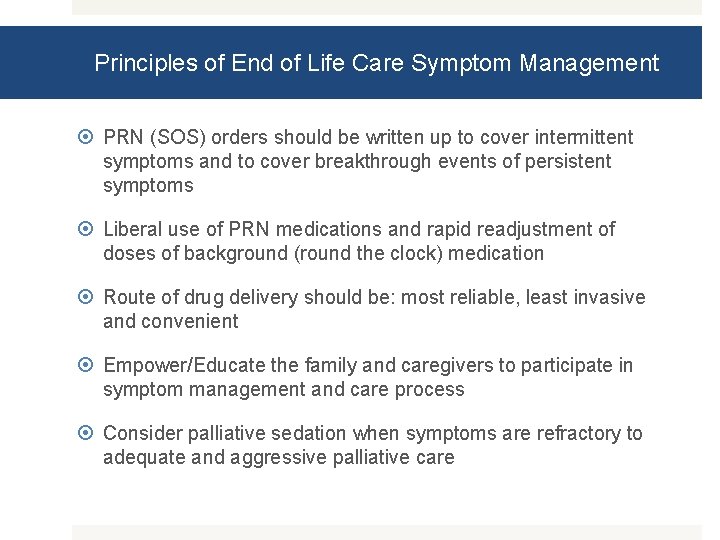
Principles of End of Life Care Symptom Management PRN (SOS) orders should be written up to cover intermittent symptoms and to cover breakthrough events of persistent symptoms Liberal use of PRN medications and rapid readjustment of doses of background (round the clock) medication Route of drug delivery should be: most reliable, least invasive and convenient Empower/Educate the family and caregivers to participate in symptom management and care process Consider palliative sedation when symptoms are refractory to adequate and aggressive palliative care

Six step EOLC Approach Steps Description STEP 1 Identify “When to initiate” “Whom to initiate” STEP 2 Assessment of physical symptoms and distress Assessment of non physical issues Assessment of communication needs STEP 3 Plan Site of care Review existing care protocol/medication chart and stop all unnecessary interventions/medications/investigations Anticipatory prescription writing Communication, Consensus, Consent
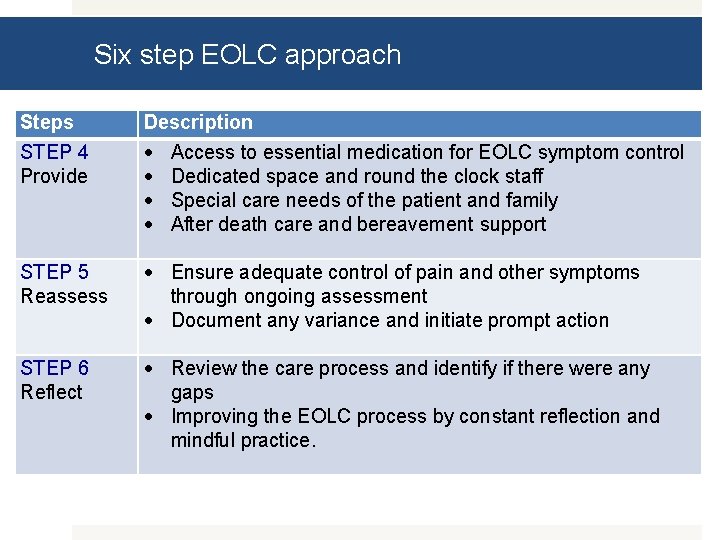
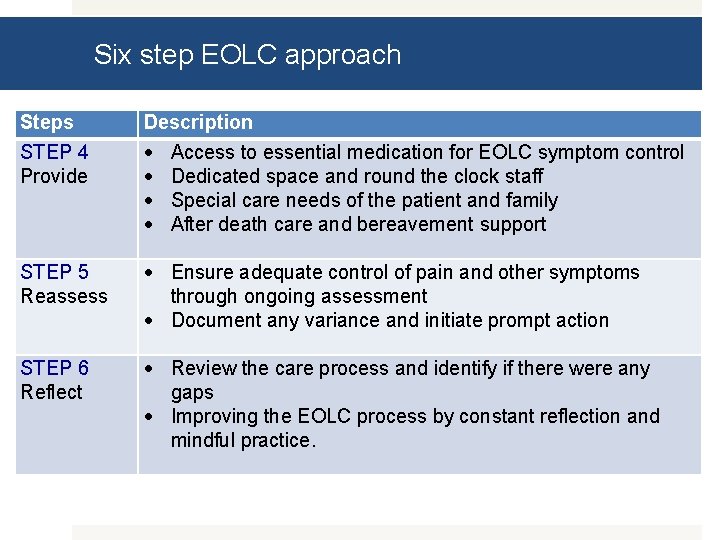
Six step EOLC approach Steps STEP 4 Provide Description Access to essential medication for EOLC symptom control Dedicated space and round the clock staff Special care needs of the patient and family After death care and bereavement support STEP 5 Reassess Ensure adequate control of pain and other symptoms through ongoing assessment Document any variance and initiate prompt action STEP 6 Reflect Review the care process and identify if there were any gaps Improving the EOLC process by constant reflection and mindful practice.
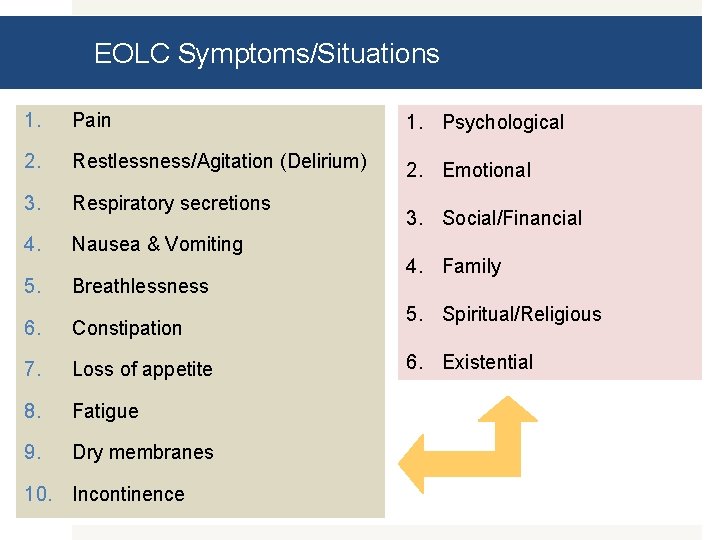
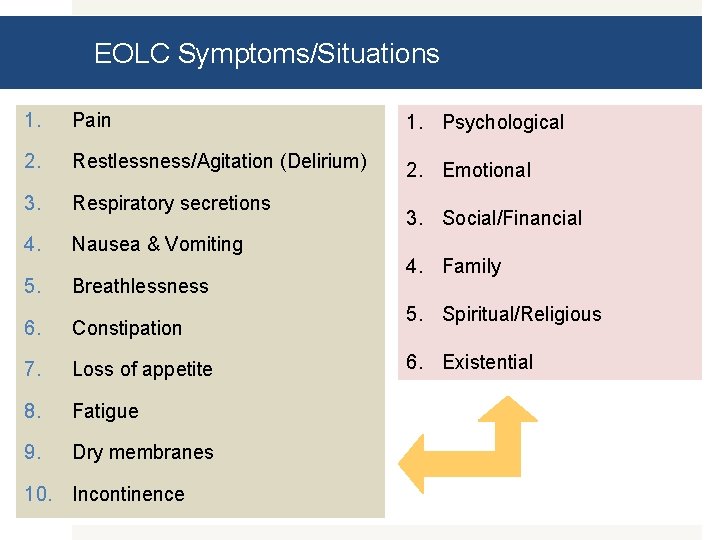
EOLC Symptoms/Situations 1. Pain 1. Psychological 2. Restlessness/Agitation (Delirium) 2. Emotional 3. Respiratory secretions 4. Nausea & Vomiting 5. Breathlessness 6. Constipation 7. Loss of appetite 8. Fatigue 9. Dry membranes 10. Incontinence 3. Social/Financial 4. Family 5. Spiritual/Religious 6. Existential
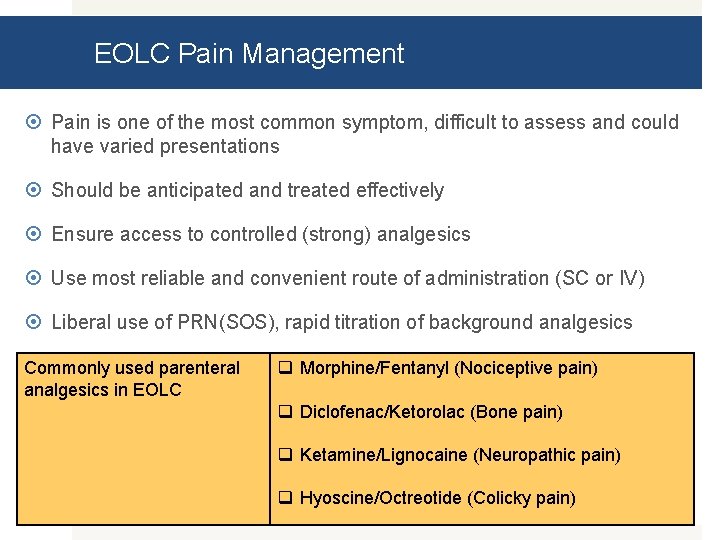
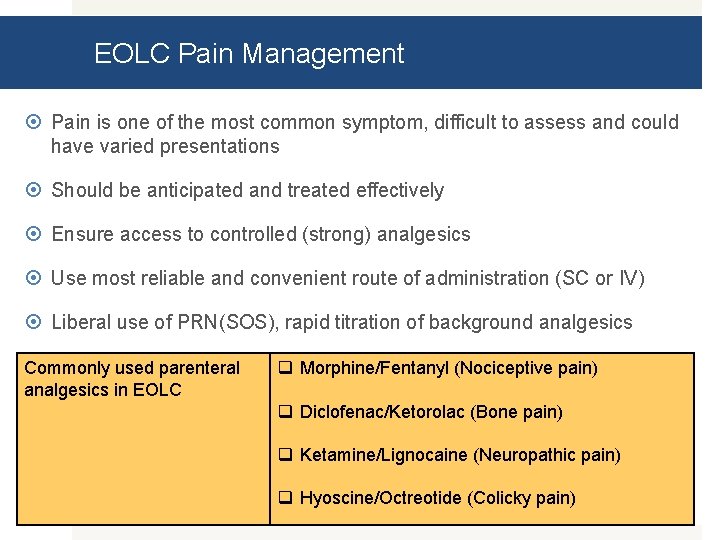
EOLC Pain Management Pain is one of the most common symptom, difficult to assess and could have varied presentations Should be anticipated and treated effectively Ensure access to controlled (strong) analgesics Use most reliable and convenient route of administration (SC or IV) Liberal use of PRN(SOS), rapid titration of background analgesics Commonly used parenteral analgesics in EOLC q Morphine/Fentanyl (Nociceptive pain) q Diclofenac/Ketorolac (Bone pain) q Ketamine/Lignocaine (Neuropathic pain) q Hyoscine/Octreotide (Colicky pain)
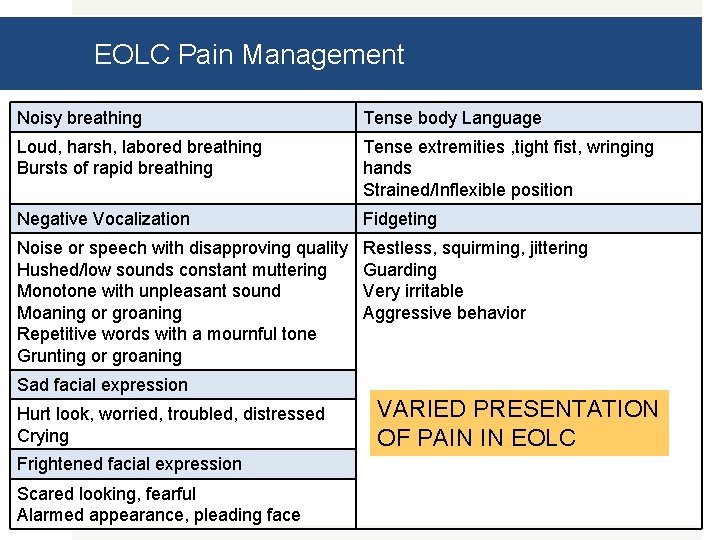
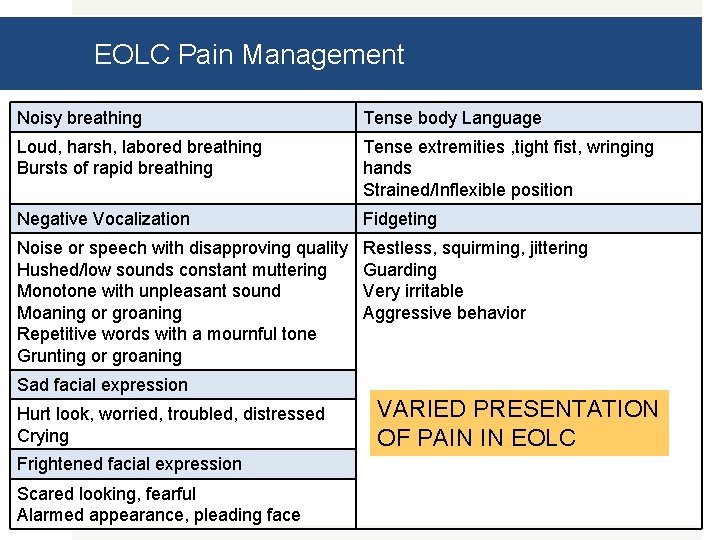
EOLC Pain Management Noisy breathing Tense body Language Loud, harsh, labored breathing Bursts of rapid breathing Tense extremities , tight fist, wringing hands Strained/Inflexible position Negative Vocalization Fidgeting Noise or speech with disapproving quality Hushed/low sounds constant muttering Monotone with unpleasant sound Moaning or groaning Repetitive words with a mournful tone Grunting or groaning Restless, squirming, jittering Guarding Very irritable Aggressive behavior Sad facial expression Hurt look, worried, troubled, distressed Crying Frightened facial expression Scared looking, fearful Alarmed appearance, pleading face VARIED PRESENTATION OF PAIN IN EOLC
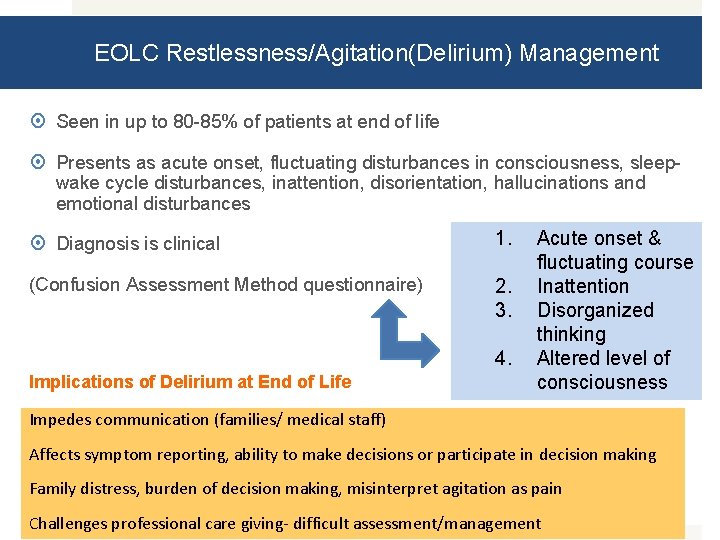
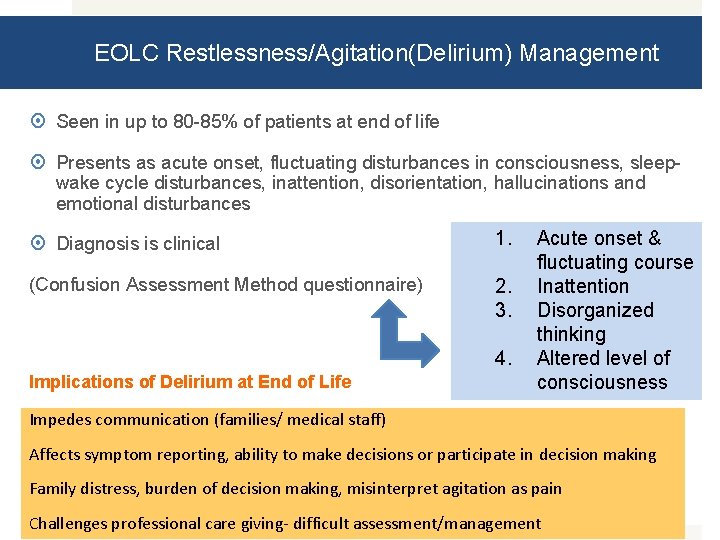
EOLC Restlessness/Agitation(Delirium) Management Seen in up to 80 -85% of patients at end of life Presents as acute onset, fluctuating disturbances in consciousness, sleepwake cycle disturbances, inattention, disorientation, hallucinations and emotional disturbances Diagnosis is clinical 1. (Confusion Assessment Method questionnaire) 2. 3. 4. Implications of Delirium at End of Life Acute onset & fluctuating course Inattention Disorganized thinking Altered level of consciousness Impedes communication (families/ medical staff) Affects symptom reporting, ability to make decisions or participate in decision making Family distress, burden of decision making, misinterpret agitation as pain Challenges professional care giving- difficult assessment/management
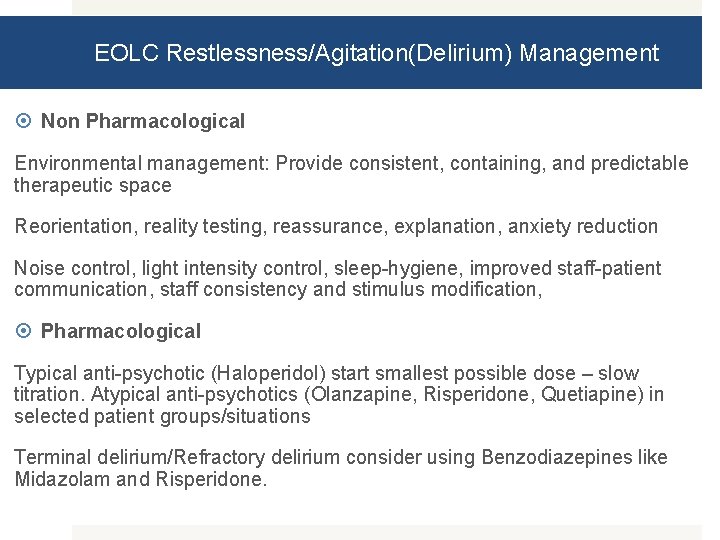
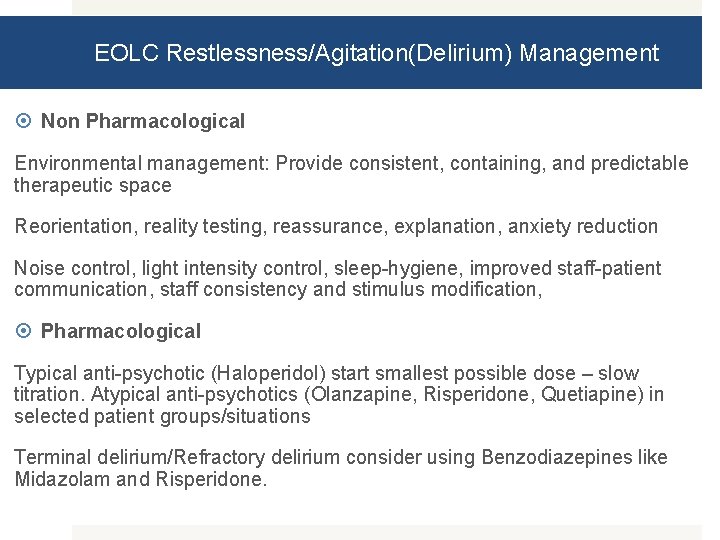
EOLC Restlessness/Agitation(Delirium) Management Non Pharmacological Environmental management: Provide consistent, containing, and predictable therapeutic space Reorientation, reality testing, reassurance, explanation, anxiety reduction Noise control, light intensity control, sleep-hygiene, improved staff-patient communication, staff consistency and stimulus modification, Pharmacological Typical anti-psychotic (Haloperidol) start smallest possible dose – slow titration. Atypical anti-psychotics (Olanzapine, Risperidone, Quetiapine) in selected patient groups/situations Terminal delirium/Refractory delirium consider using Benzodiazepines like Midazolam and Risperidone.
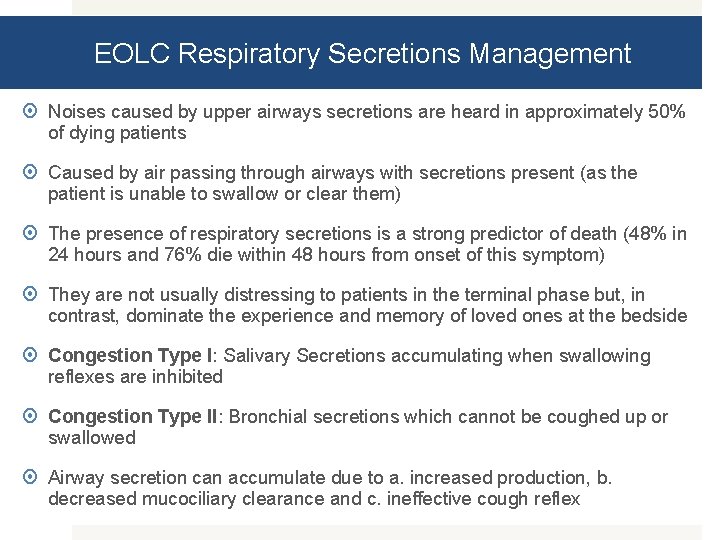
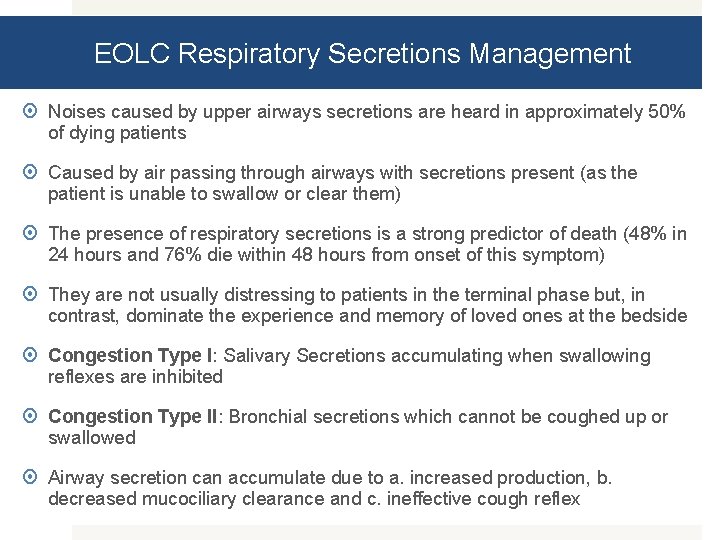
EOLC Respiratory Secretions Management Noises caused by upper airways secretions are heard in approximately 50% of dying patients Caused by air passing through airways with secretions present (as the patient is unable to swallow or clear them) The presence of respiratory secretions is a strong predictor of death (48% in 24 hours and 76% die within 48 hours from onset of this symptom) They are not usually distressing to patients in the terminal phase but, in contrast, dominate the experience and memory of loved ones at the bedside Congestion Type I: Salivary Secretions accumulating when swallowing reflexes are inhibited Congestion Type II: Bronchial secretions which cannot be coughed up or swallowed Airway secretion can accumulate due to a. increased production, b. decreased mucociliary clearance and c. ineffective cough reflex
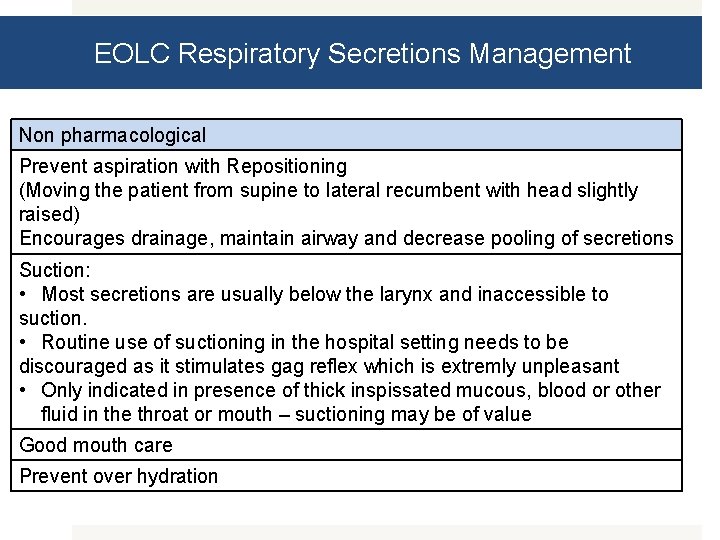
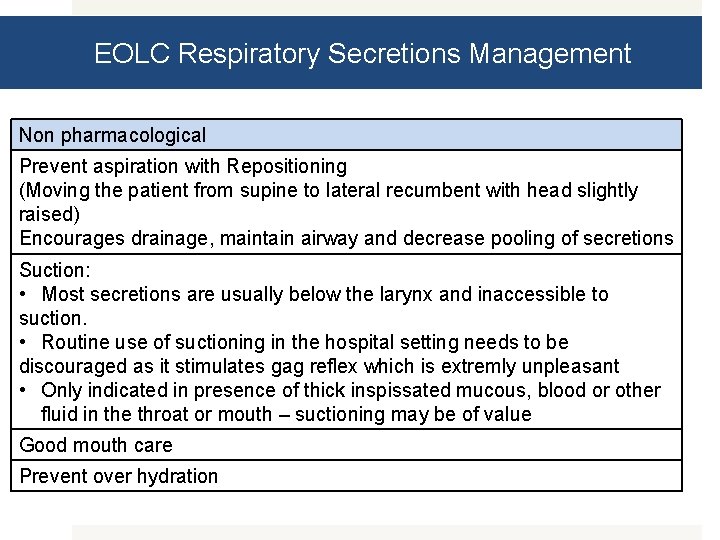
EOLC Respiratory Secretions Management Non pharmacological Prevent aspiration with Repositioning (Moving the patient from supine to lateral recumbent with head slightly raised) Encourages drainage, maintain airway and decrease pooling of secretions Suction: • Most secretions are usually below the larynx and inaccessible to suction. • Routine use of suctioning in the hospital setting needs to be discouraged as it stimulates gag reflex which is extremly unpleasant • Only indicated in presence of thick inspissated mucous, blood or other fluid in the throat or mouth – suctioning may be of value Good mouth care Prevent over hydration

EOLC Respiratory Secretions Management Pharmacological Atropine 0. 4 to 0. 8 mg S. C. q 4 h and q 1 h p. r. n Scopolamine (hyoscine hydro bromide) 0. 3 to 0. 6 mg S. C. q 4 to 6 h regularly and/or p. r. n Scopolamine transdermal patch 1. 5 mg q 72 h; slow onset thus not indicated in terminal phase unless augmented with subcutaneous route for 8 to 12 hours. Glycopyrrolate 0. 1 to 0. 2 mg S. C. q 6 to 8 h regularly and/or p. r. n. does not cross the blood brain barrier thus should be considered in non-obtunded patients.
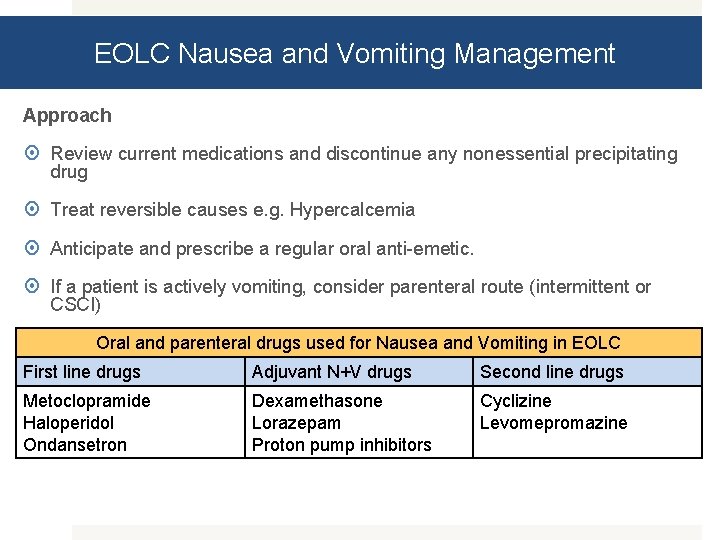
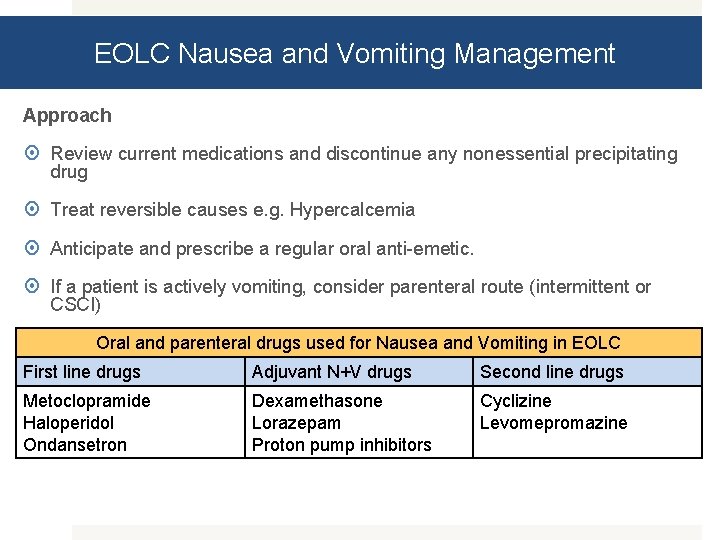
EOLC Nausea and Vomiting Management Approach Review current medications and discontinue any nonessential precipitating drug Treat reversible causes e. g. Hypercalcemia Anticipate and prescribe a regular oral anti-emetic. If a patient is actively vomiting, consider parenteral route (intermittent or CSCI) Oral and parenteral drugs used for Nausea and Vomiting in EOLC First line drugs Adjuvant N+V drugs Second line drugs Metoclopramide Haloperidol Ondansetron Dexamethasone Lorazepam Proton pump inhibitors Cyclizine Levomepromazine
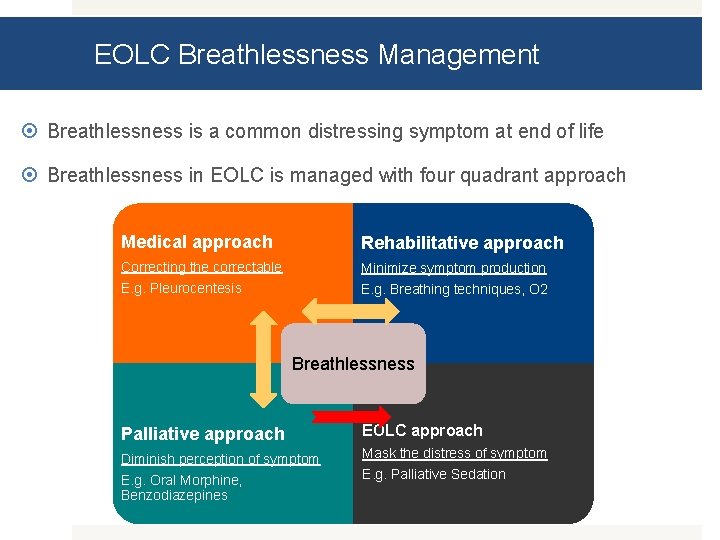
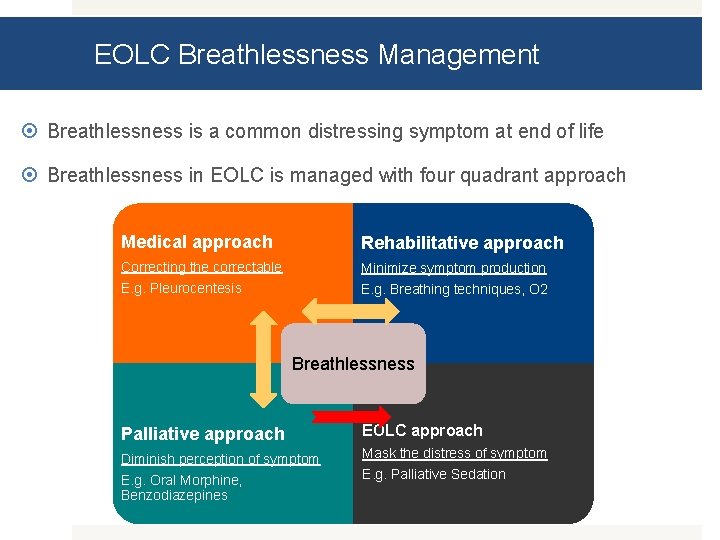
EOLC Breathlessness Management Breathlessness is a common distressing symptom at end of life Breathlessness in EOLC is managed with four quadrant approach Medical approach Rehabilitative approach Correcting the correctable E. g. Pleurocentesis Minimize symptom production E. g. Breathing techniques, O 2 Breathlessness Palliative approach EOLC approach Diminish perception of symptom Mask the distress of symptom E. g. Palliative Sedation E. g. Oral Morphine, Benzodiazepines
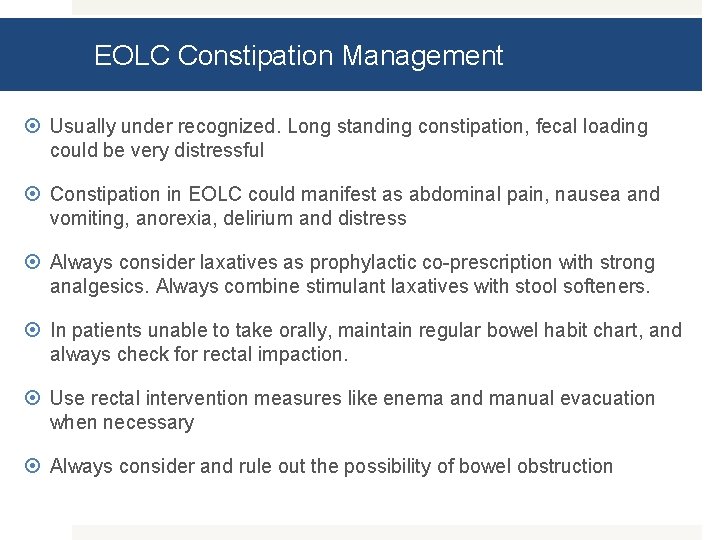
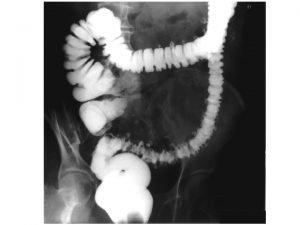
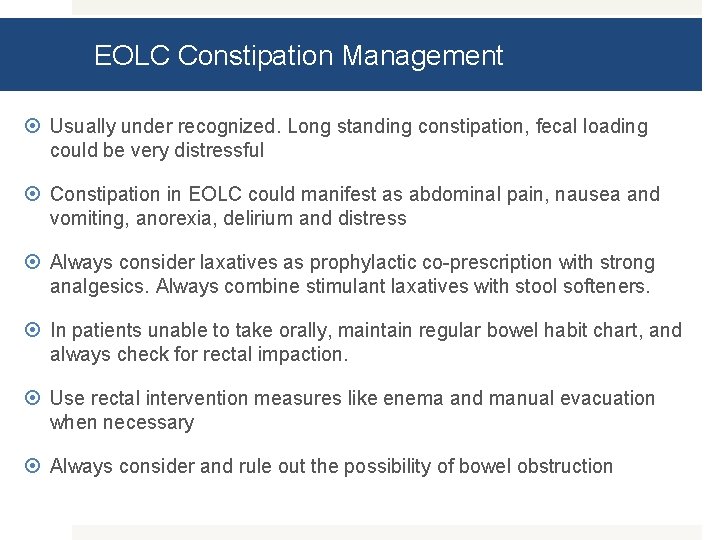
EOLC Constipation Management Usually under recognized. Long standing constipation, fecal loading could be very distressful Constipation in EOLC could manifest as abdominal pain, nausea and vomiting, anorexia, delirium and distress Always consider laxatives as prophylactic co-prescription with strong analgesics. Always combine stimulant laxatives with stool softeners. In patients unable to take orally, maintain regular bowel habit chart, and always check for rectal impaction. Use rectal intervention measures like enema and manual evacuation when necessary Always consider and rule out the possibility of bowel obstruction
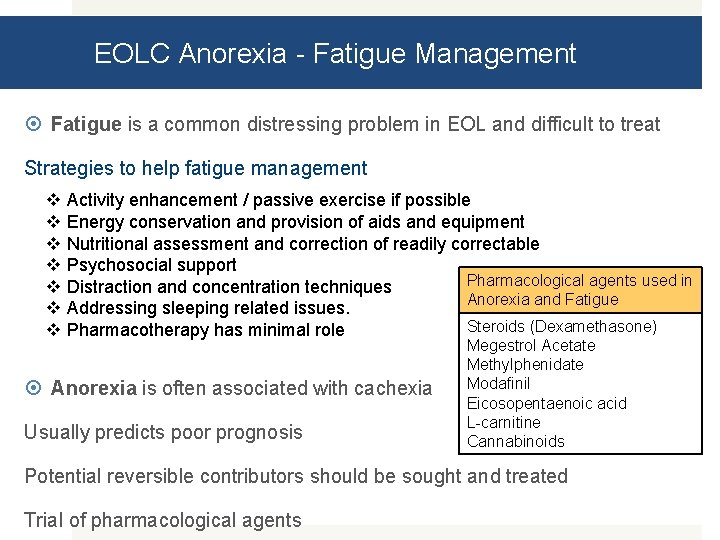
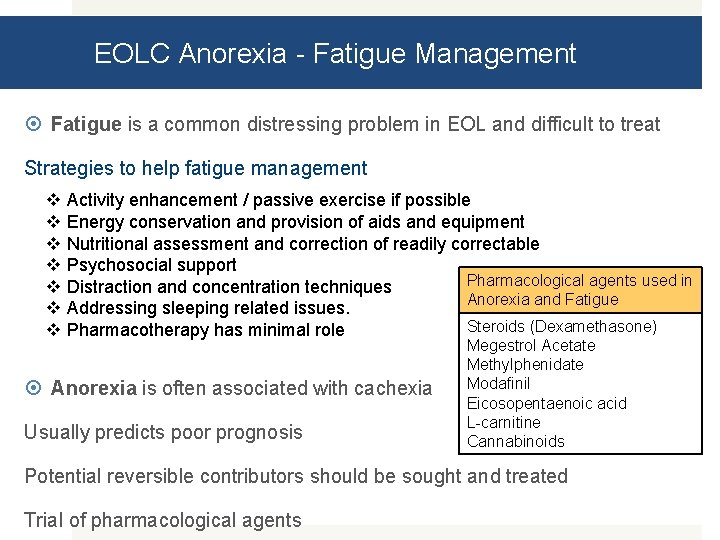
EOLC Anorexia - Fatigue Management Fatigue is a common distressing problem in EOL and difficult to treat Strategies to help fatigue management v v v v Activity enhancement / passive exercise if possible Energy conservation and provision of aids and equipment Nutritional assessment and correction of readily correctable Psychosocial support Pharmacological agents used in Distraction and concentration techniques Anorexia and Fatigue Addressing sleeping related issues. Steroids (Dexamethasone) Pharmacotherapy has minimal role Anorexia is often associated with cachexia Usually predicts poor prognosis Megestrol Acetate Methylphenidate Modafinil Eicosopentaenoic acid L-carnitine Cannabinoids Potential reversible contributors should be sought and treated Trial of pharmacological agents
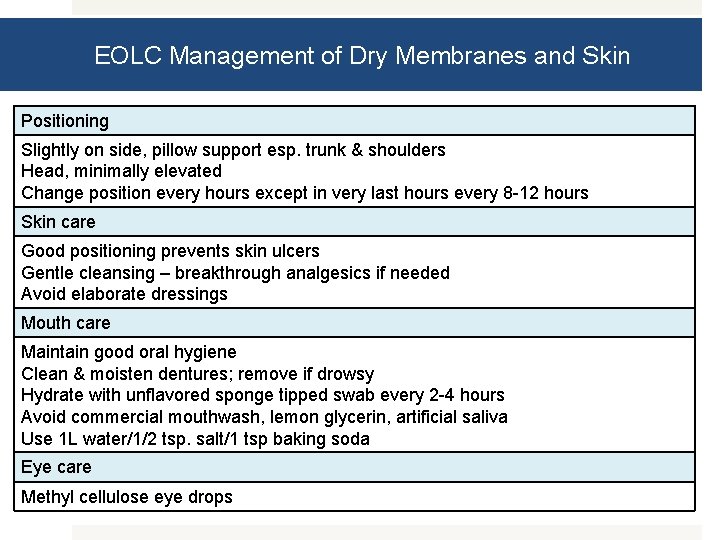
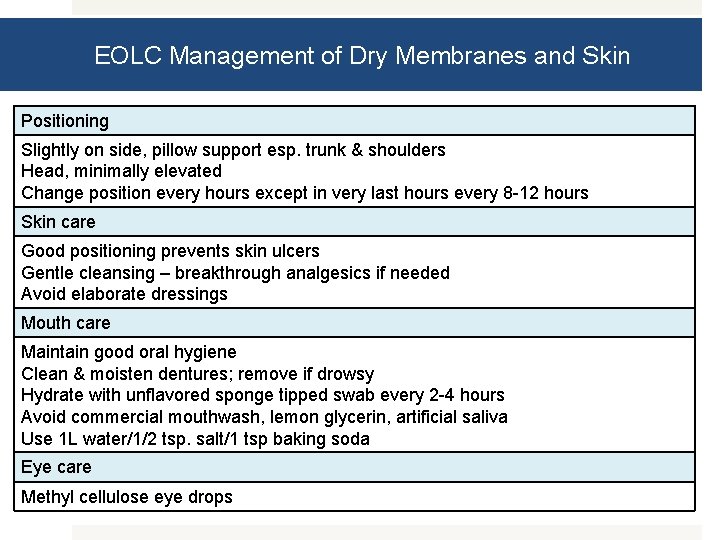
EOLC Management of Dry Membranes and Skin Positioning Slightly on side, pillow support esp. trunk & shoulders Head, minimally elevated Change position every hours except in very last hours every 8 -12 hours Skin care Good positioning prevents skin ulcers Gentle cleansing – breakthrough analgesics if needed Avoid elaborate dressings Mouth care Maintain good oral hygiene Clean & moisten dentures; remove if drowsy Hydrate with unflavored sponge tipped swab every 2 -4 hours Avoid commercial mouthwash, lemon glycerin, artificial saliva Use 1 L water/1/2 tsp. salt/1 tsp baking soda Eye care Methyl cellulose eye drops
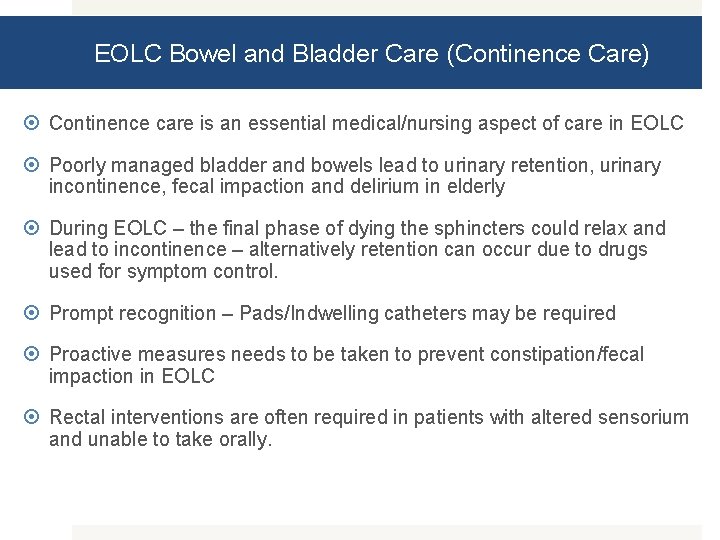
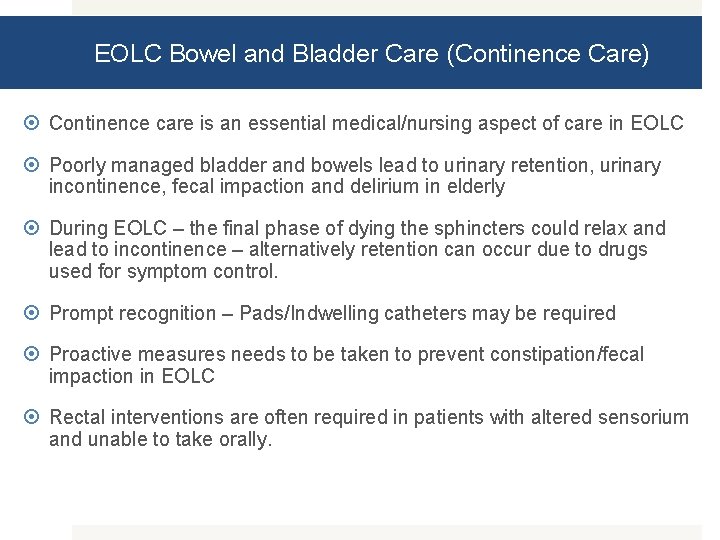
EOLC Bowel and Bladder Care (Continence Care) Continence care is an essential medical/nursing aspect of care in EOLC Poorly managed bladder and bowels lead to urinary retention, urinary incontinence, fecal impaction and delirium in elderly During EOLC – the final phase of dying the sphincters could relax and lead to incontinence – alternatively retention can occur due to drugs used for symptom control. Prompt recognition – Pads/Indwelling catheters may be required Proactive measures needs to be taken to prevent constipation/fecal impaction in EOLC Rectal interventions are often required in patients with altered sensorium and unable to take orally.
EOLC Special Issues Clinically assisted (artificial) hydration and (artificial) will not be of benefit and decisions about their use should be individualized and made in patient’s best interest Symptoms of thirst / dry mouth are often due to mouth breathing or medication / oxygen therapy and good mouth care, frequent wetting of mouth will alleviate symptoms of thirst. If clinically assisted artificial hydration or nutritional support is in place, review rate/ volume / route according to individual need such that complications related to overt hydration and parenteral nutrition at EOLC is avoided. IV antibiotics at EOL should be rationalized and judiciously prescribed as it may not confer any additional benefit during EOLC
EOLC Palliative Sedation Palliative sedation is defined as medication-induced sedation that is administered, without intending to cause death, utilizing a non opioid drug to control intolerable symptoms that are refractory to conventional treatment in patients with advanced and incurable disease whose death is imminent (death expected in hours or days) Common conditions where Palliative Sedation is considered is intractable pain, intractable dyspnea and intractable delirium When to consider palliative sedation? v v v Symptoms are refractory to pharmacological and non-pharmacological options Death is imminent in days or weeks Additional treatments are unlikely to bring relief Aggressive palliative treatment has failed to control symptoms Goal is relief of distress of symptom Not enough time to try a potential non- sedative approach – impending death
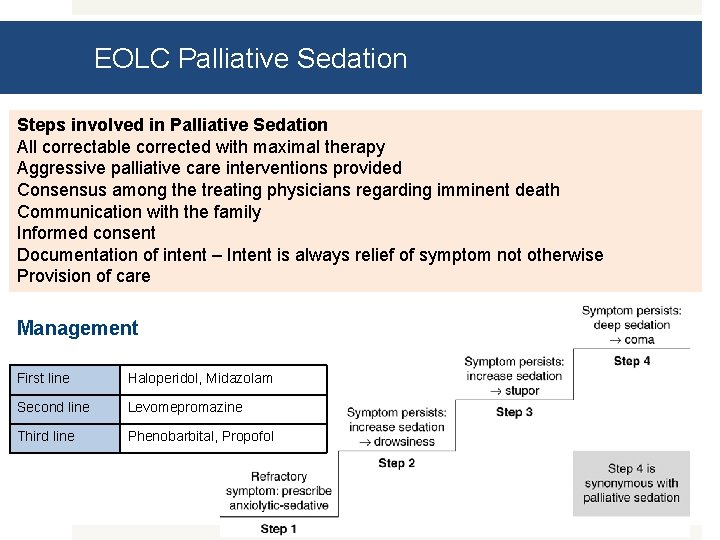
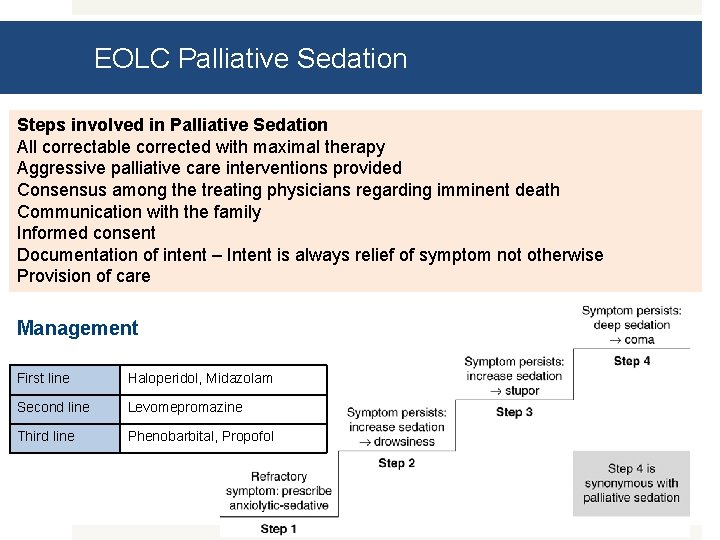
EOLC Palliative Sedation Steps involved in Palliative Sedation All correctable corrected with maximal therapy Aggressive palliative care interventions provided Consensus among the treating physicians regarding imminent death Communication with the family Informed consent Documentation of intent – Intent is always relief of symptom not otherwise Provision of care Management First line Haloperidol, Midazolam Second line Levomepromazine Third line Phenobarbital, Propofol

THANK YOU This education program is a joint initiative of Indian Society of Critical Care Medicine and Indian Association of Palliative Care. 2014 © All rights reserved
 End to end accounting life cycle tasks
End to end accounting life cycle tasks Multiple procurement cycles
Multiple procurement cycles Chapter 55 end of life care
Chapter 55 end of life care North west end of life care model
North west end of life care model End of life care in south tyneside
End of life care in south tyneside End of life care in icu
End of life care in icu Primary secondary tertiary care nursing
Primary secondary tertiary care nursing What decreases stroke volume
What decreases stroke volume Stroke volume
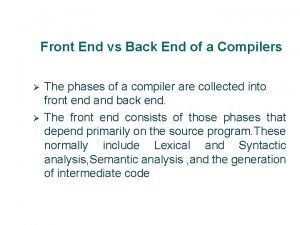
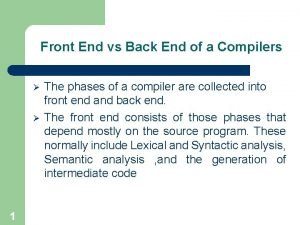
Stroke volume Front end of compiler
Front end of compiler Compiler front end vs back end
Compiler front end vs back end Kolondivertikulose definition
Kolondivertikulose definition Yichao zhou
Yichao zhou End to end argument
End to end argument End to end delay
End to end delay End to end delay
End to end delay End to end
End to end End-to-end construction of nlp knowledge graph
End-to-end construction of nlp knowledge graph C device module module 1
C device module module 1 Cornelia m ruland
Cornelia m ruland Microsoft identity manager end of life
Microsoft identity manager end of life Cisco prime collaboration deployment 12
Cisco prime collaboration deployment 12 Life cycle of a small to medium star
Life cycle of a small to medium star Microsoft identity manager tutorial
Microsoft identity manager tutorial