End of Life Care Education MODULE 1 Case

- Slides: 11
End of Life Care Education MODULE 1 Case Scenario 3 End of Life Care Webinar
Case Scenario 3 (Part 1 of 5) 68 year old male, metastatic lung cancer with bilateral pulmonary nodules, chest wall involvement and liver metastasis. Has already completed chemo radiotherapy. No further disease modifying treatment planned/relevant. Reports right sided pleuritic chest pain 8/10 somatic nociceptive, with resting dyspnea and cough Sp. O 2 91% on room air, HR 122/min, ECOG 4, Pallor present Chest bilaterally decreased air entry with no adventitious sounds Routine bloods: Hb 8. 9 gm% TLC Normal, Metabolic workup unremarkable, CXR bilateral lung nodules, no clinical evidence of pleural effusion or lower respiratory tract infection
Case Scenario 3 (Part 2 of 5) Prognosticated survival days to shorter weeks (based on ECOG, PPS) Goals of care were discussed with the wife and 2 sons – Futility of invasive medical interventions discussed. Patient was aware of diagnosis and prognosis. No collusion existed in the family Family decided to continue his medical care in the ward. Agreed for “allowing natural death” and explicitly expressed “NO” for any life prolonging interventions Oral Morphine 10 mg Q 4 H was started for pain along with other supportive care measures. One of patient’s son who is a medical practitioner expressed concerns about using Morphine in presence of dyspnea – These concerns were clarified and addressed.
Discussion points Prognostication Discussion and decision making on goals of care Transition to palliative approach/avoiding ICU admission Good symptom control approach Using Morphine/Strong analgesics for pain control Using Morphine for dyspnea (Benefits/Justification/Evidence)
Case Scenario 3 (Part 3 of 5) Pain and dyspnea were poorly controlled with oral and parenteral Morphine. Patient was very restless, agitated and hallucinations Family members were distressed and upset. Family meeting was conducted and refractory nature of symptoms and need to initiate sedation to control these symptoms were discussed Family agreed with the plan, informed consent was taken, intent and plan of management was documented. Patient was initiated on continuous infusion of Morphine and Midazolam the dose was constantly titrated –symptom response and treatment toxicity were frequently assessed/reassessed
Discussion points End of Life Symptoms Terminal Delirium Palliative Sedation (When/Where/How) End points of Palliative Sedation
Case Scenario 3 (Part 4 of 5) Patient’s pain and symptoms were well controlled. Patient remained drowsy with intermittent awakening and minimal verbal response Moist respirations were managed with Glycopyrrolate. Over next 1 day changing in breathing pattern was noted. Patient was shifted to a single room for privacy. Patient and family had belonged to Buddhist faith, and as per family's request Buddhist monks were allowed to be present during patient’s final moments along with the family. Patient died peacefully in the ward in the presence of family Family provided input about religious customs involved in immediate after death care and these suggestions were incorporated.
Discussion points Perimortem period care (Silver Hour) Addressing non-physical needs in end of life care Minimum infrastructural requirements for good end of life care After death care
Case Scenario 3 (Part 5 of 5) Patient was promptly attended by the treating physician, death was verified and certification for cause of death was provided. All arrangements were made for timely and dignified transport of dead person from the hospital Bereavement phone call was made 1 week after patient’s death and 3 weeks later a bereavement home visit was done by doctor and nurses team. Few pending/unanswered questions were answered during bereavement home visit. Social worker was involved for further ongoing bereavement support Death was discussed in the multi-disciplinary team meeting and the care process was reviewed Family had a normal grieving process, are back to their lives in few months
Discussion points Verification and certification of death (Correct steps/guidelines) Bereavement support High risk bereavement/Prolonged grief Review of care process

THANK YOU This education program is a joint initiative of Indian Society of Critical Care Medicine and Indian Association of Palliative Care. 2014 © All rights reserved
 End to end accounting life cycle tasks
End to end accounting life cycle tasks End-to-end procurement life cycle
End-to-end procurement life cycle Best case worst case average case
Best case worst case average case Chapter 55 end of life care
Chapter 55 end of life care North west end of life care model
North west end of life care model End of life care in south tyneside
End of life care in south tyneside End of life care in icu
End of life care in icu Primary secondary tertiary care definition
Primary secondary tertiary care definition C device module module 1
C device module module 1 Cardiac output
Cardiac output End-diastolic volume vs end-systolic volume
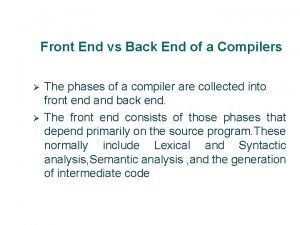
End-diastolic volume vs end-systolic volume Front end of compiler
Front end of compiler