Early Recognition of Sepsis The Nurses Role Definitions
- Slides: 14
Early Recognition of Sepsis The Nurse’s Role
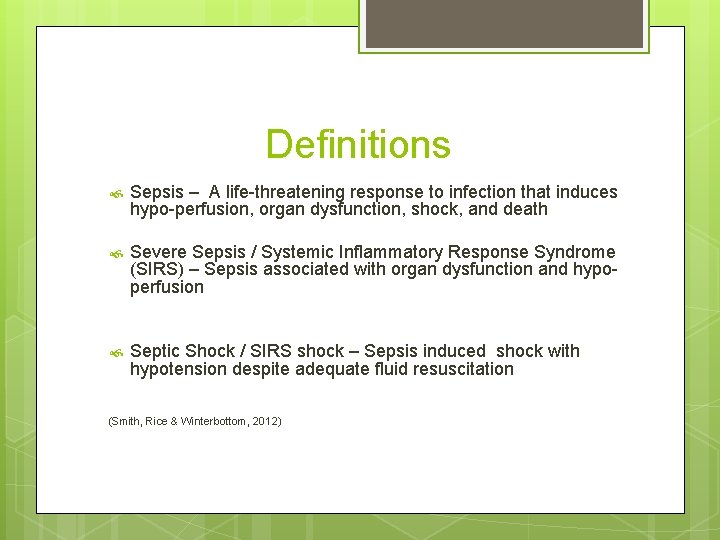
Definitions Sepsis – A life-threatening response to infection that induces hypo-perfusion, organ dysfunction, shock, and death Severe Sepsis / Systemic Inflammatory Response Syndrome (SIRS) – Sepsis associated with organ dysfunction and hypoperfusion Septic Shock / SIRS shock – Sepsis induced shock with hypotension despite adequate fluid resuscitation (Smith, Rice & Winterbottom, 2012)
Statistics Sepsis is the primary cause of death from infection Sepsis has a mortality rate ranging from 30% to 50% Sepsis costs the United States 16. 7 Billion dollars annually Sepsis is not often recognized early as a medical emergency (Buck, 2013)
Early Recognition Like other life threatening conditions, early recognition and time-effective management of sepsis is crucial for patient outcomes The Surviving Sepsis Campaign Guidelines Committee suggested that the greatest improvement in outcomes can be made through education and process changes (Surviving Sepsis Campaign, 2013)
Urgency Every minute counts when treating sepsis For every hour that sepsis goes untreated, the risk of death increases by 7. 6 % Prioritize, Obtain assistance from another nurse and call the physician
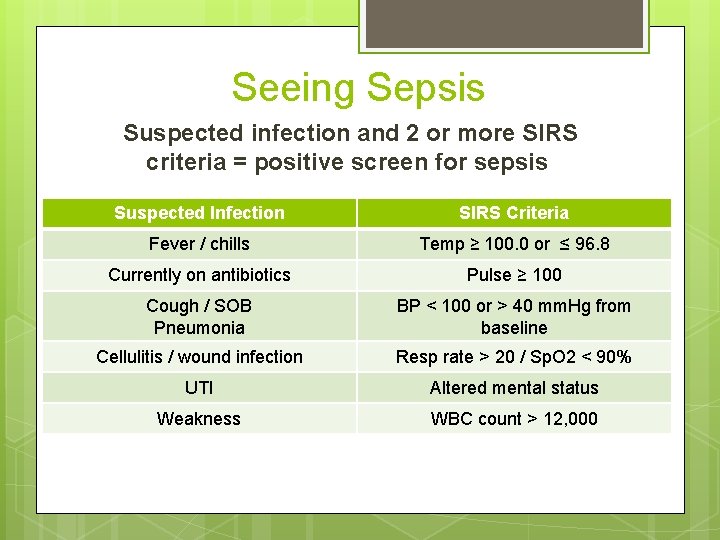
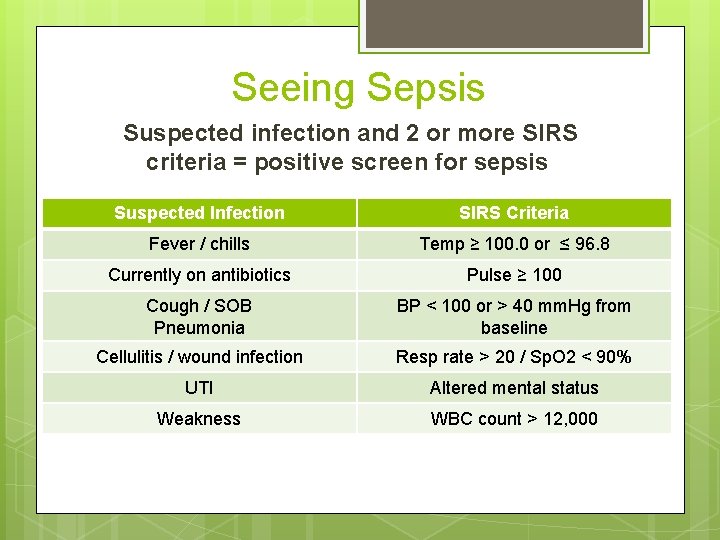
Seeing Sepsis Suspected infection and 2 or more SIRS criteria = positive screen for sepsis Suspected Infection SIRS Criteria Fever / chills Temp ≥ 100. 0 or ≤ 96. 8 Currently on antibiotics Pulse ≥ 100 Cough / SOB Pneumonia BP < 100 or > 40 mm. Hg from baseline Cellulitis / wound infection Resp rate > 20 / Sp. O 2 < 90% UTI Altered mental status Weakness WBC count > 12, 000
Time is Critical Once sepsis is suspected or a patient has screened positive, time is of the essence The provider must be contacted promptly in order to make appropriate decisions based on patient / family wishes and goals In general, hospital transfer is preferred if keeping within the patient’s advanced directives, wishes, and goals of treatment
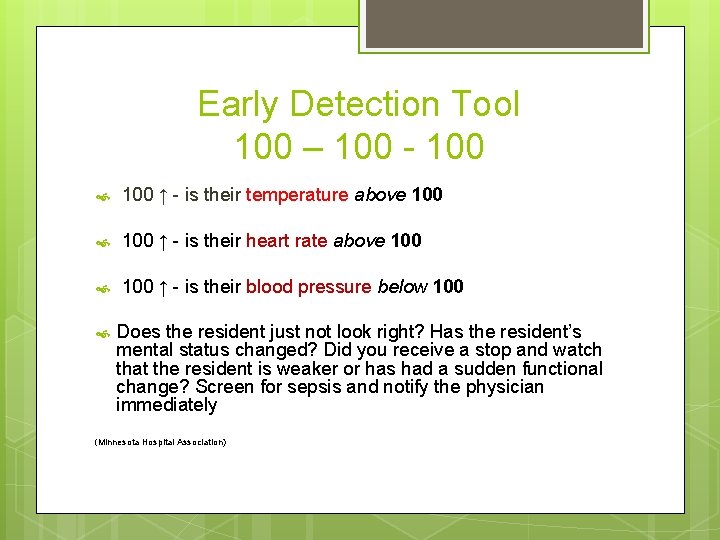
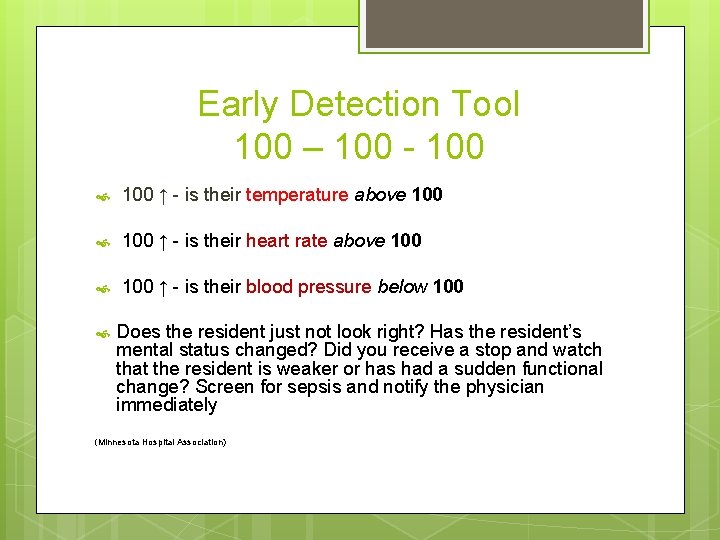
Early Detection Tool 100 – 100 - 100 ↑ - is their temperature above 100 ↑ - is their heart rate above 100 ↑ - is their blood pressure below 100 Does the resident just not look right? Has the resident’s mental status changed? Did you receive a stop and watch that the resident is weaker or has had a sudden functional change? Screen for sepsis and notify the physician immediately (Minnesota Hospital Association)
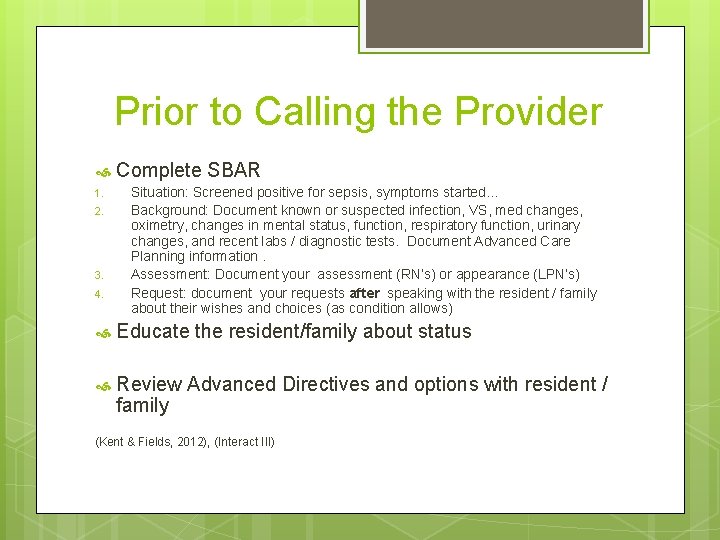
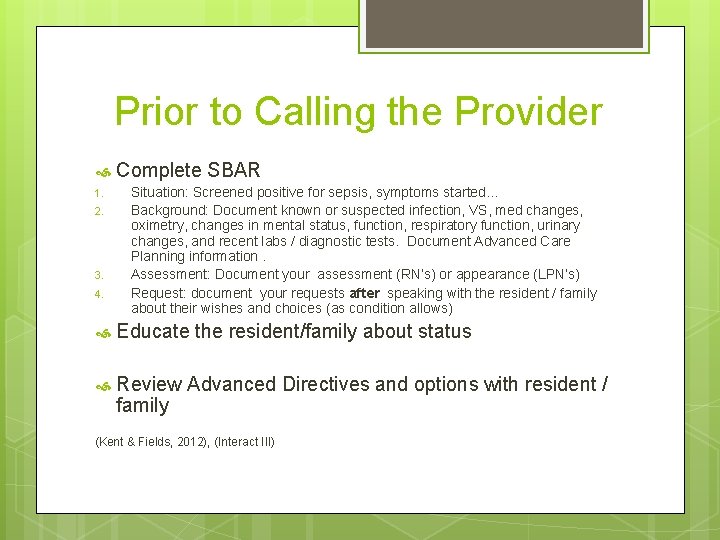
Prior to Calling the Provider 1. 2. 3. 4. Complete SBAR Situation: Screened positive for sepsis, symptoms started… Background: Document known or suspected infection, VS, med changes, oximetry, changes in mental status, function, respiratory function, urinary changes, and recent labs / diagnostic tests. Document Advanced Care Planning information. Assessment: Document your assessment (RN’s) or appearance (LPN’s) Request: document your requests after speaking with the resident / family about their wishes and choices (as condition allows) Educate the resident/family about status Review Advanced Directives and options with resident / family (Kent & Fields, 2012), (Interact III)
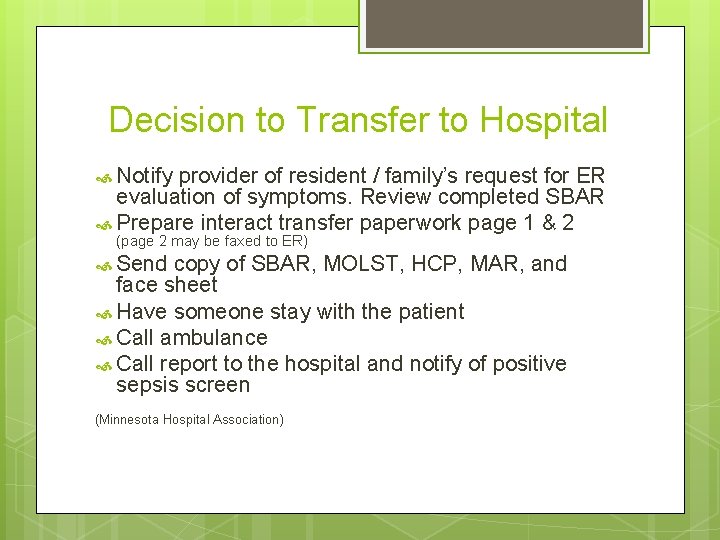
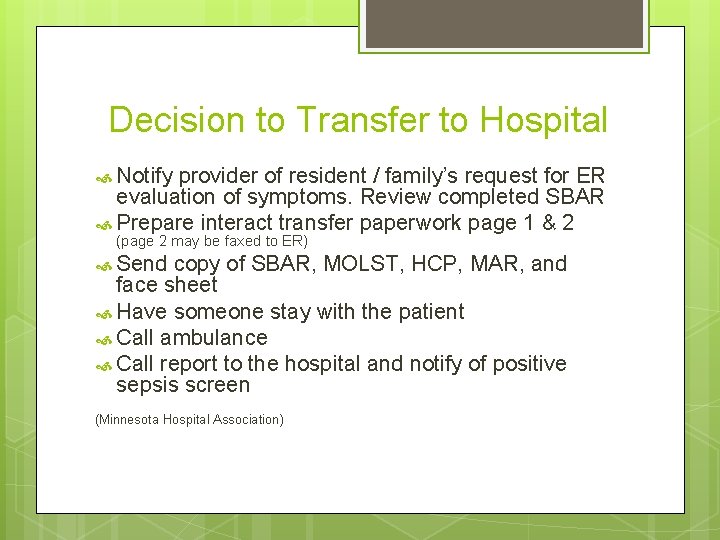
Decision to Transfer to Hospital Notify provider of resident / family’s request for ER evaluation of symptoms. Review completed SBAR Prepare interact transfer paperwork page 1 & 2 (page 2 may be faxed to ER) Send copy of SBAR, MOLST, HCP, MAR, and face sheet Have someone stay with the patient Call ambulance Call report to the hospital and notify of positive sepsis screen (Minnesota Hospital Association)
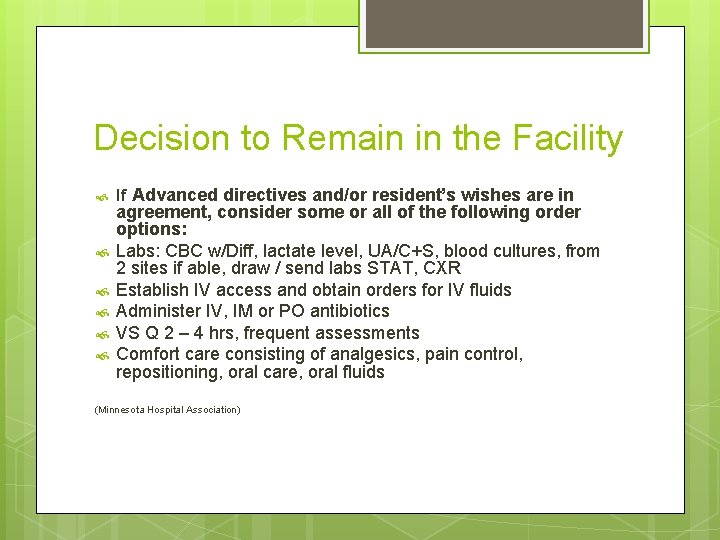
Decision to Remain in the Facility If Advanced directives and/or resident’s wishes are in agreement, consider some or all of the following order options: Labs: CBC w/Diff, lactate level, UA/C+S, blood cultures, from 2 sites if able, draw / send labs STAT, CXR Establish IV access and obtain orders for IV fluids Administer IV, IM or PO antibiotics VS Q 2 – 4 hrs, frequent assessments Comfort care consisting of analgesics, pain control, repositioning, oral care, oral fluids (Minnesota Hospital Association)
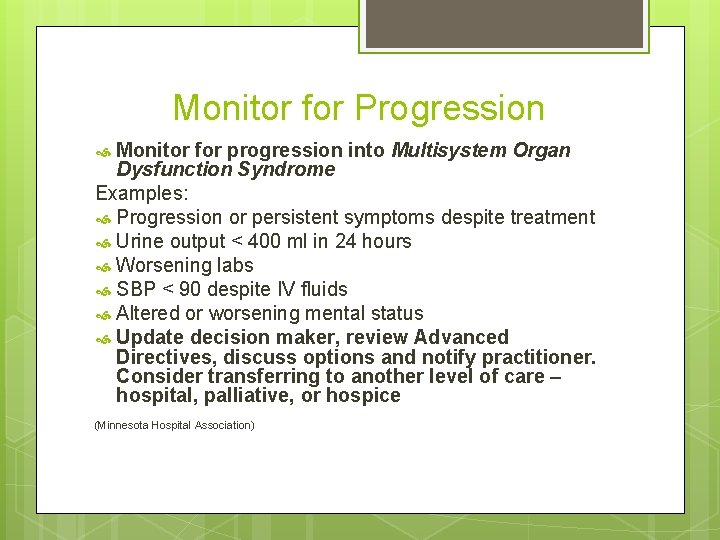
Monitor for Progression Monitor for progression into Multisystem Organ Dysfunction Syndrome Examples: Progression or persistent symptoms despite treatment Urine output < 400 ml in 24 hours Worsening labs SBP < 90 despite IV fluids Altered or worsening mental status Update decision maker, review Advanced Directives, discuss options and notify practitioner. Consider transferring to another level of care – hospital, palliative, or hospice (Minnesota Hospital Association)
Early Recognition is Key The use of the 100 – 100 early detection tool will assist nurses with early recognition of sepsis Whether the patient’s wishes are to be treated in the nursing home or the hospital, early identification and treatment consisting of antibiotics, IV fluids, laboratory studies, and frequent re-assessment by nurses is crucial for patient outcomes.
References Minnesota Hospital Association Seeing Sepsis Interact III Fields, W. , Kent, N. (2012). Early recognition of sepsis in the emergency department: An evidence-based project. Journal of Emergency Medicine, 38, 139 – 144. Buck, K. , (2014). Developing an early sepsis alert program. Journal of Nursing Care Quality, 29, 124 – 132. Winterbottom, F. (2012). Nurses’ critical role in identifying sepsis and implementing early goal-directed therapy. The Journal of Continuing Education in Nursing, 43, 247 – 248. Castren, M. , Kurland, L. , Svensson, A. & Wallgren, U. (2014). Identification of adult septic patients in the prehospital setting: a comparison of two screening tools and clinical judgement. Journal of Emergency Medicine, 21, 260 - 265
 Q sofa
Q sofa Role of chn nurse
Role of chn nurse Therapeutic milieu
Therapeutic milieu Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Role taking krappmann
Role taking krappmann Statuses and their related roles determine the structure
Statuses and their related roles determine the structure C# azure worker role example
C# azure worker role example Sepsis triangle
Sepsis triangle Surviving sepsis definition
Surviving sepsis definition Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Sepsis
Sepsis Sepsis bundle
Sepsis bundle Bjarni geir viðarsson
Bjarni geir viðarsson Sepsis
Sepsis Stages of sepsis
Stages of sepsis