Sepsis Early Recognition and Management Therese Hughes Ph

- Slides: 22
Sepsis Early Recognition and Management Therese Hughes, Ph. D, MPA, RN 1
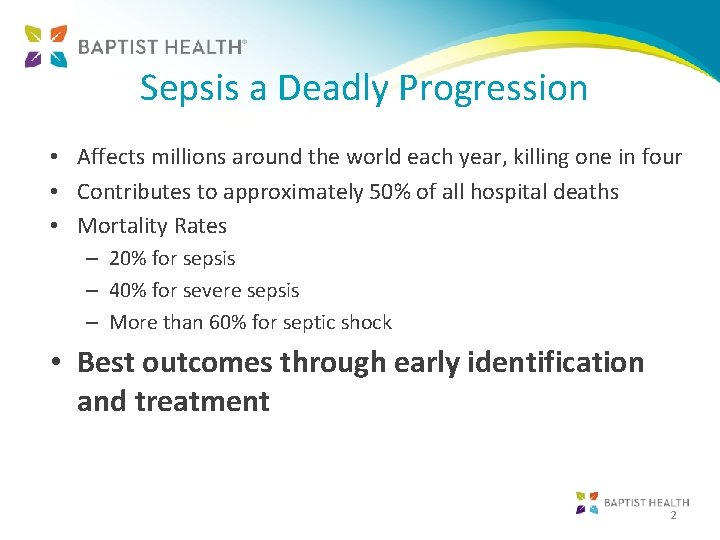
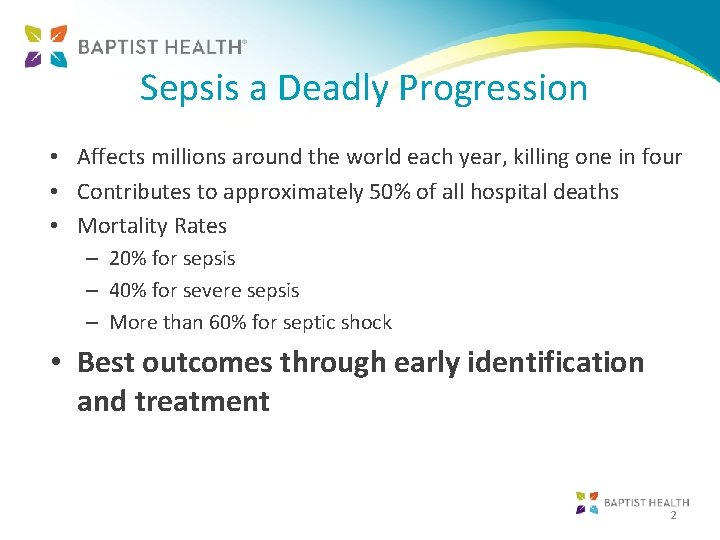
Sepsis a Deadly Progression • Affects millions around the world each year, killing one in four • Contributes to approximately 50% of all hospital deaths • Mortality Rates – 20% for sepsis – 40% for severe sepsis – More than 60% for septic shock • Best outcomes through early identification and treatment 2
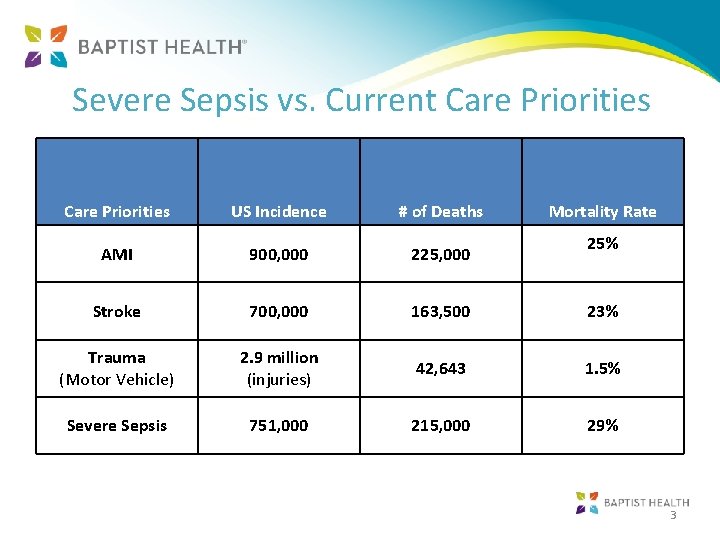
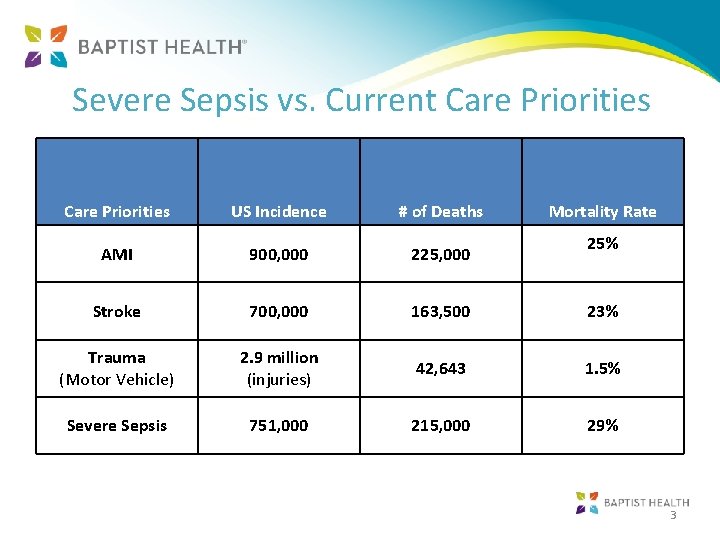
Severe Sepsis vs. Current Care Priorities US Incidence # of Deaths Mortality Rate AMI 900, 000 225, 000 Stroke 700, 000 163, 500 23% Trauma (Motor Vehicle) 2. 9 million (injuries) 42, 643 1. 5% Severe Sepsis 751, 000 215, 000 29% 25% 3
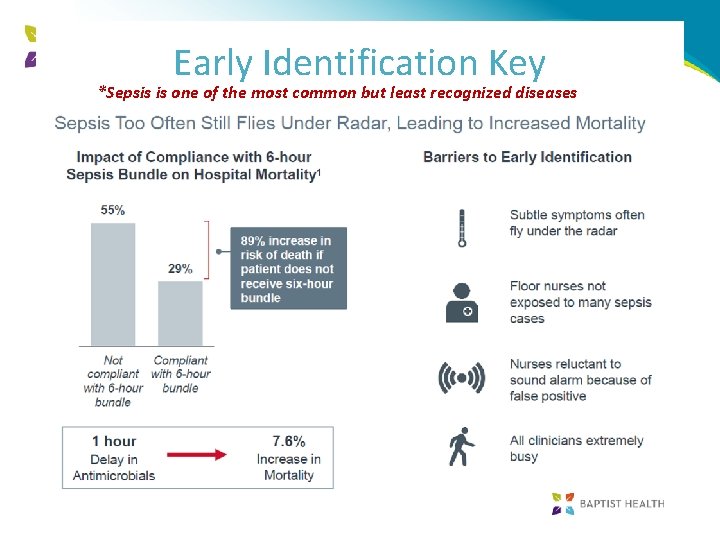
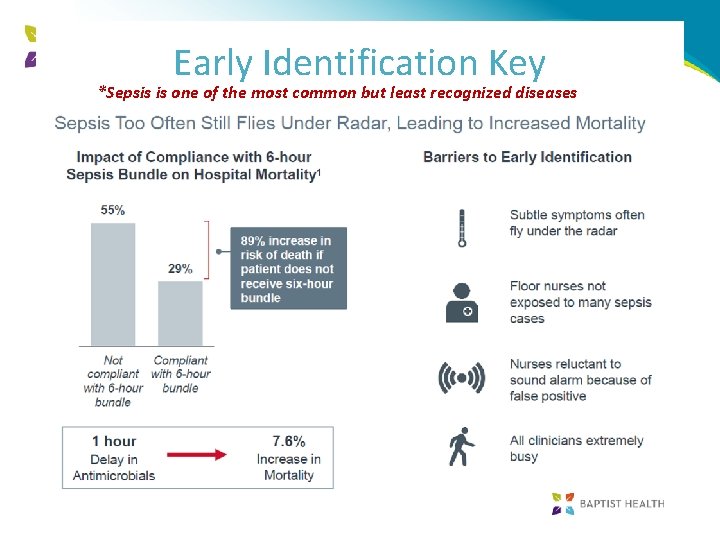
Early Identification Key *Sepsis is one of the most common but least recognized diseases
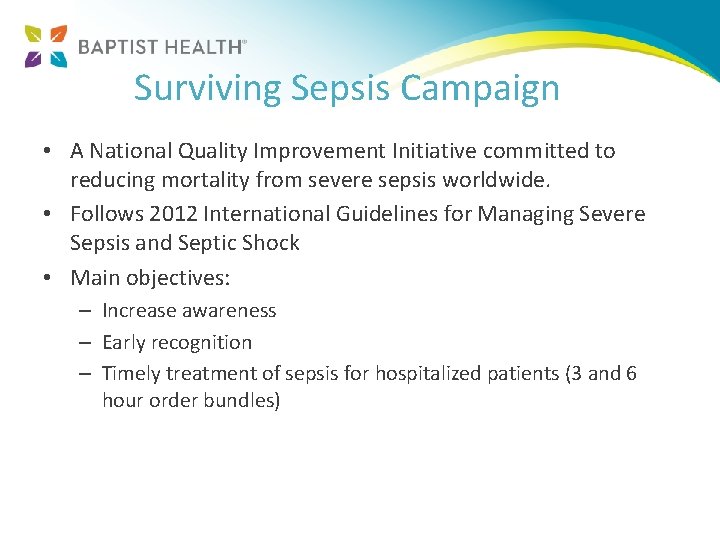
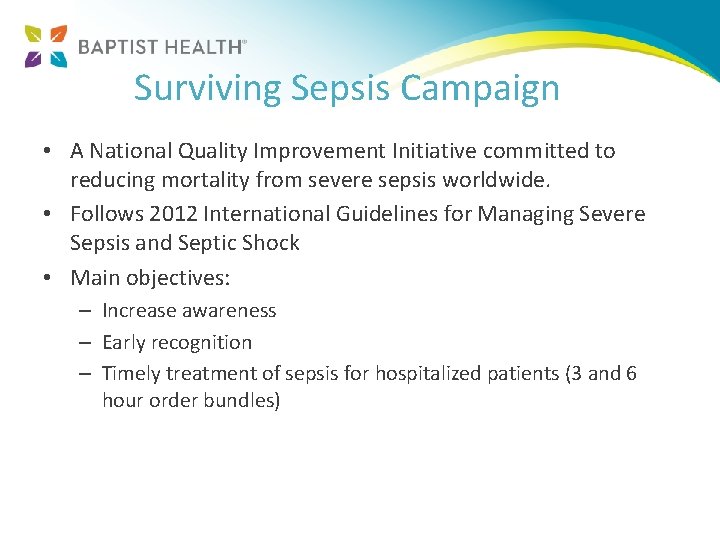
Surviving Sepsis Campaign • A National Quality Improvement Initiative committed to reducing mortality from severe sepsis worldwide. • Follows 2012 International Guidelines for Managing Severe Sepsis and Septic Shock • Main objectives: – Increase awareness – Early recognition – Timely treatment of sepsis for hospitalized patients (3 and 6 hour order bundles)
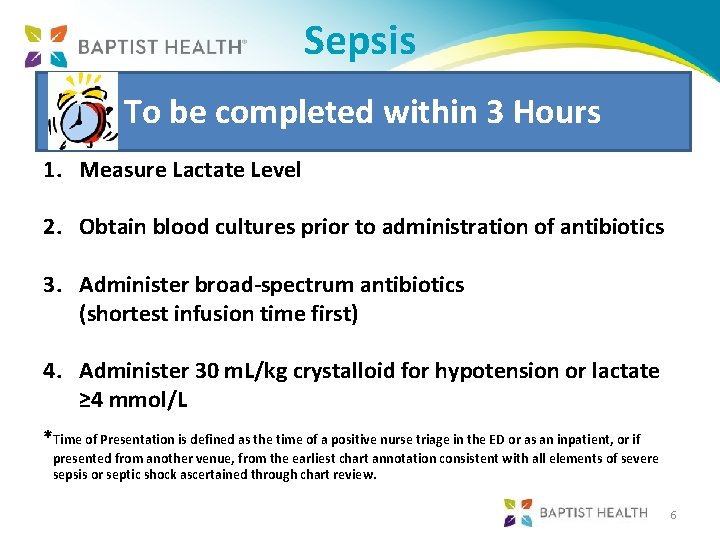
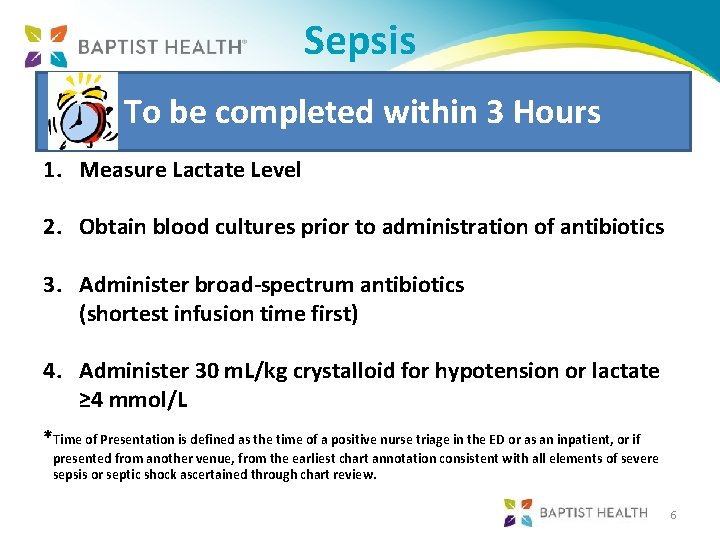
Sepsis To be completed within 3 Hours 1. Measure Lactate Level 2. Obtain blood cultures prior to administration of antibiotics 3. Administer broad-spectrum antibiotics (shortest infusion time first) 4. Administer 30 m. L/kg crystalloid for hypotension or lactate ≥ 4 mmol/L *Time of Presentation is defined as the time of a positive nurse triage in the ED or as an inpatient, or if presented from another venue, from the earliest chart annotation consistent with all elements of severe sepsis or septic shock ascertained through chart review. 6

Sepsis To be completed within 6 Hours 5. Apply vasopressors (for hypotension that does not respond to initial fluid bolus) to maintain a SBP >90 or MAP >65 mm. Hg 6. In the event of persistent arterial hypotension despite volume resuscitation, or initial lactate ≥ 4 mmol/L (Septic Shock) you must complete a “Septic Shock Focused Exam” within 6 hours of septic shock diagnosis: fluid bolus must be completed prior to assessment; Refer to Septic Shock Focused Exam. Form must be printed from Optio 7. Re-measure lactate acid if initial lactate was elevated > 2 (within 6 hrs) *Time of Presentation is defined as the time of a positive nurse triage in the ED or as an inpatient, or if presented from another venue, from the earliest chart annotation consistent with all elements of severe sepsis or septic shock ascertained through chart review. 7
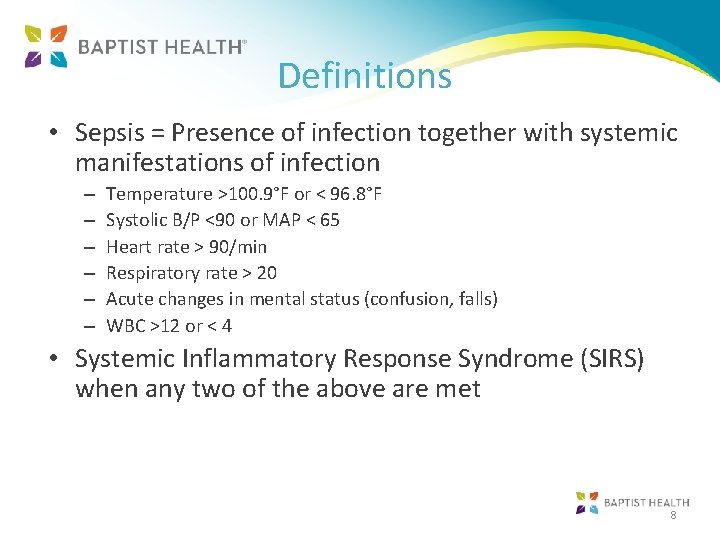
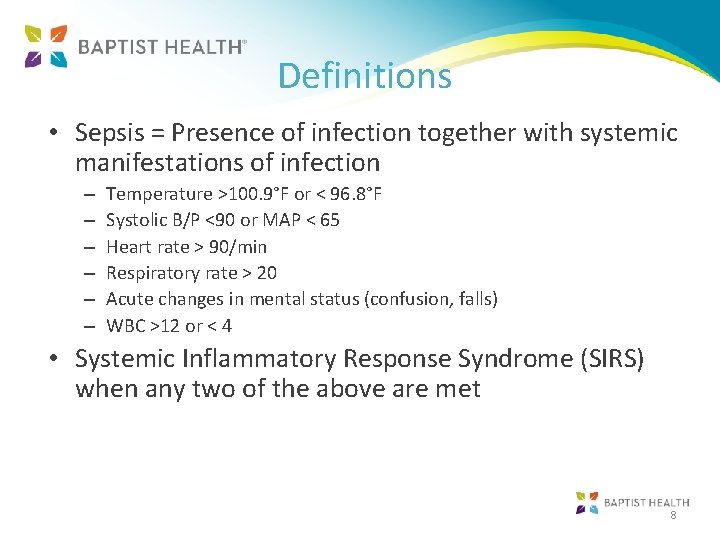
Definitions • Sepsis = Presence of infection together with systemic manifestations of infection – – – Temperature >100. 9°F or < 96. 8°F Systolic B/P <90 or MAP < 65 Heart rate > 90/min Respiratory rate > 20 Acute changes in mental status (confusion, falls) WBC >12 or < 4 • Systemic Inflammatory Response Syndrome (SIRS) when any two of the above are met 8
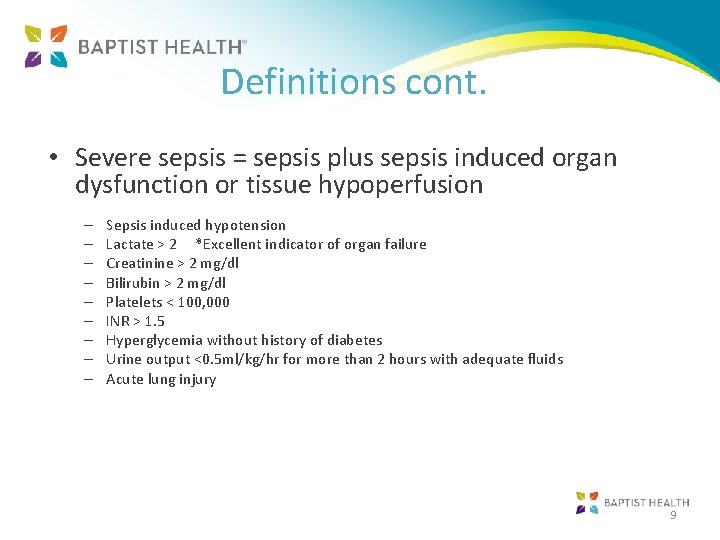
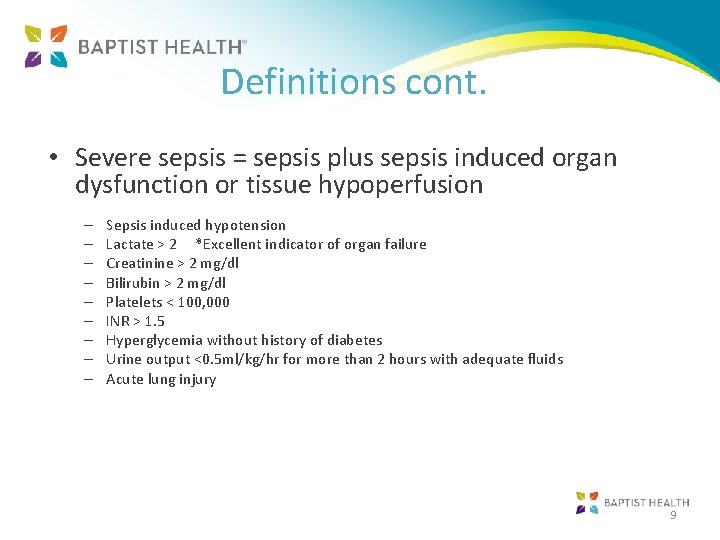
Definitions cont. • Severe sepsis = sepsis plus sepsis induced organ dysfunction or tissue hypoperfusion – – – – – Sepsis induced hypotension Lactate > 2 *Excellent indicator of organ failure Creatinine > 2 mg/dl Bilirubin > 2 mg/dl Platelets < 100, 000 INR > 1. 5 Hyperglycemia without history of diabetes Urine output <0. 5 ml/kg/hr for more than 2 hours with adequate fluids Acute lung injury 9
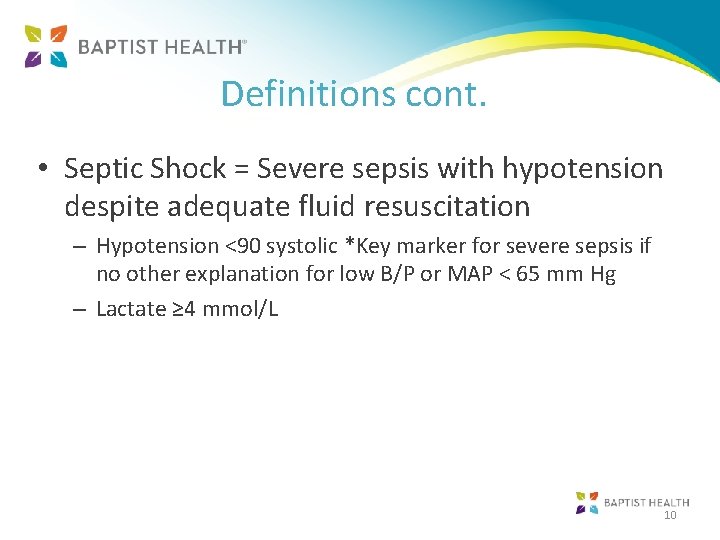
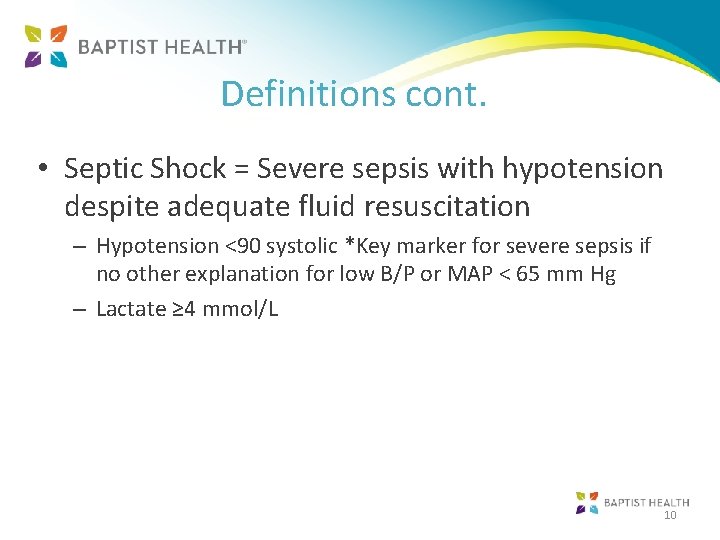
Definitions cont. • Septic Shock = Severe sepsis with hypotension despite adequate fluid resuscitation – Hypotension <90 systolic *Key marker for severe sepsis if no other explanation for low B/P or MAP < 65 mm Hg – Lactate ≥ 4 mmol/L 10
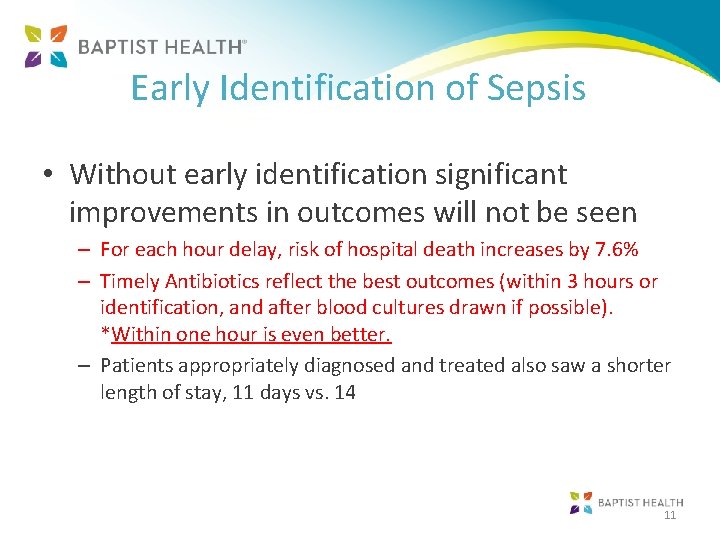
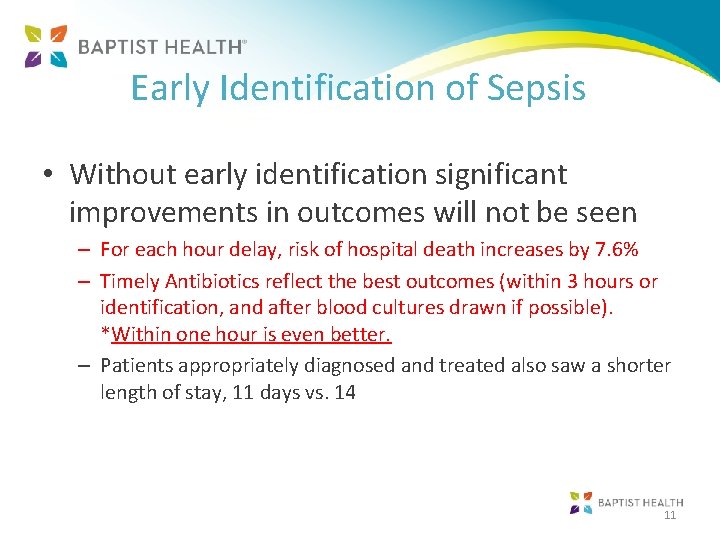
Early Identification of Sepsis • Without early identification significant improvements in outcomes will not be seen – For each hour delay, risk of hospital death increases by 7. 6% – Timely Antibiotics reflect the best outcomes (within 3 hours or identification, and after blood cultures drawn if possible). *Within one hour is even better. – Patients appropriately diagnosed and treated also saw a shorter length of stay, 11 days vs. 14 11
Tools For Early Identification and Treatment • Nurse Sepsis Screening Tool – All ED patient screened in triage – Inpatients screened for sepsis at the beginning of each shift (Every 12 hours unless previously positive) 12
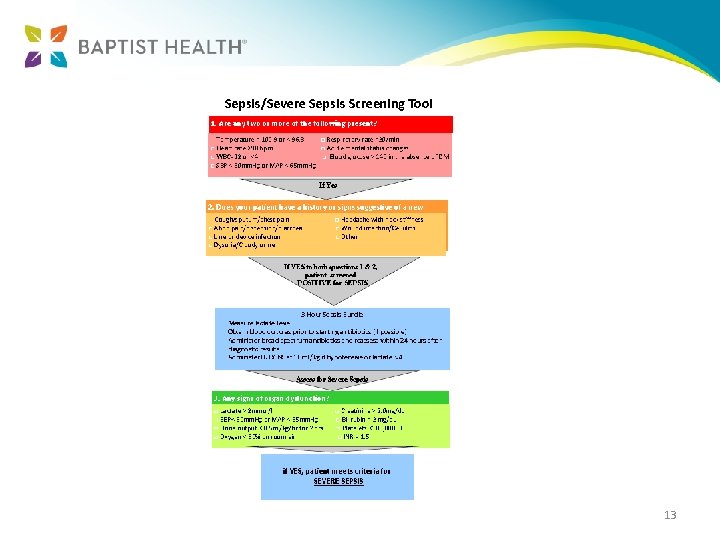
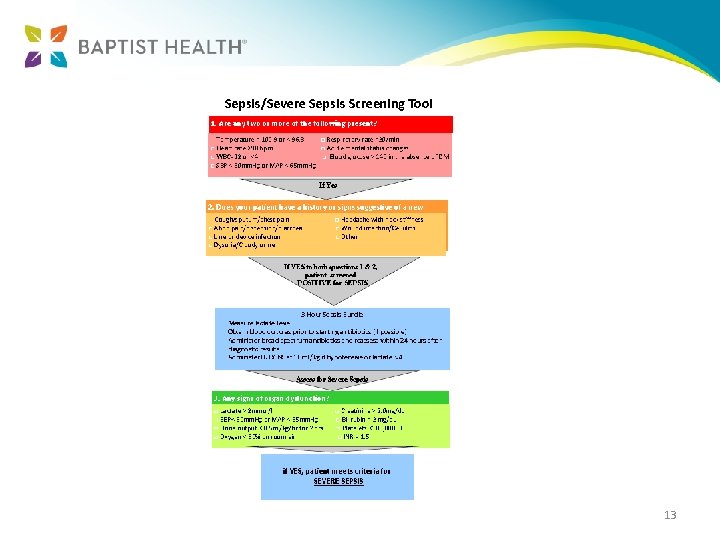
13
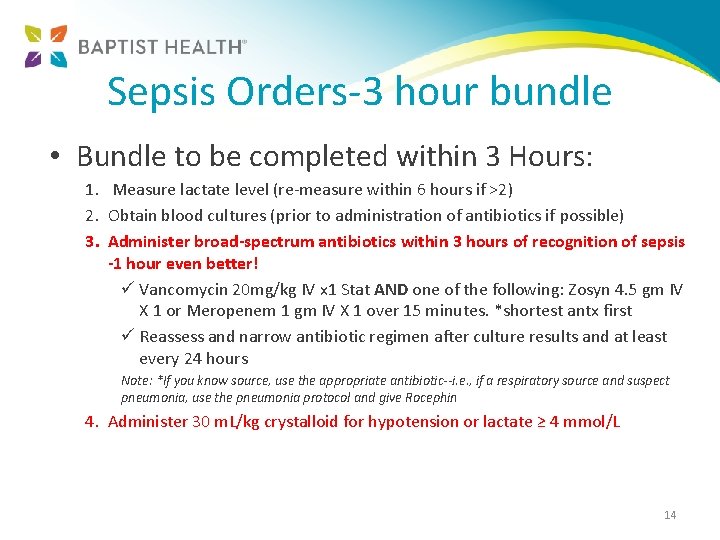
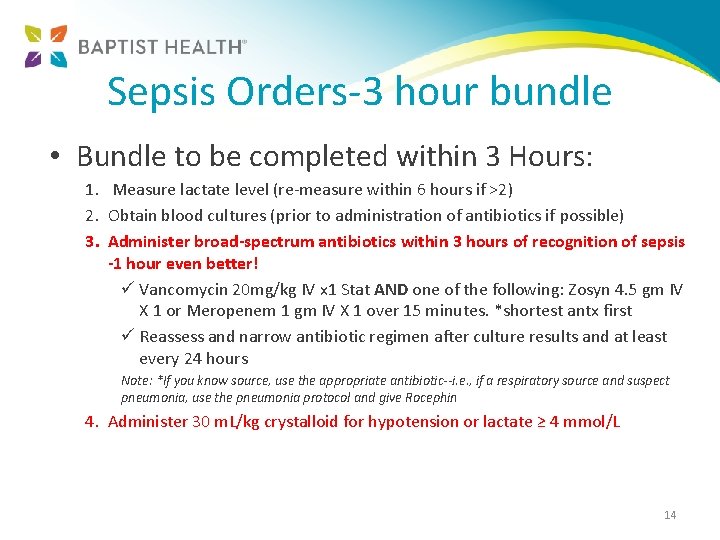
Sepsis Orders-3 hour bundle • Bundle to be completed within 3 Hours: 1. Measure lactate level (re-measure within 6 hours if >2) 2. Obtain blood cultures (prior to administration of antibiotics if possible) 3. Administer broad-spectrum antibiotics within 3 hours of recognition of sepsis -1 hour even better! ü Vancomycin 20 mg/kg IV x 1 Stat AND one of the following: Zosyn 4. 5 gm IV X 1 or Meropenem 1 gm IV X 1 over 15 minutes. *shortest antx first ü Reassess and narrow antibiotic regimen after culture results and at least every 24 hours Note: *If you know source, use the appropriate antibiotic--i. e. , if a respiratory source and suspect pneumonia, use the pneumonia protocol and give Rocephin 4. Administer 30 m. L/kg crystalloid for hypotension or lactate ≥ 4 mmol/L 14
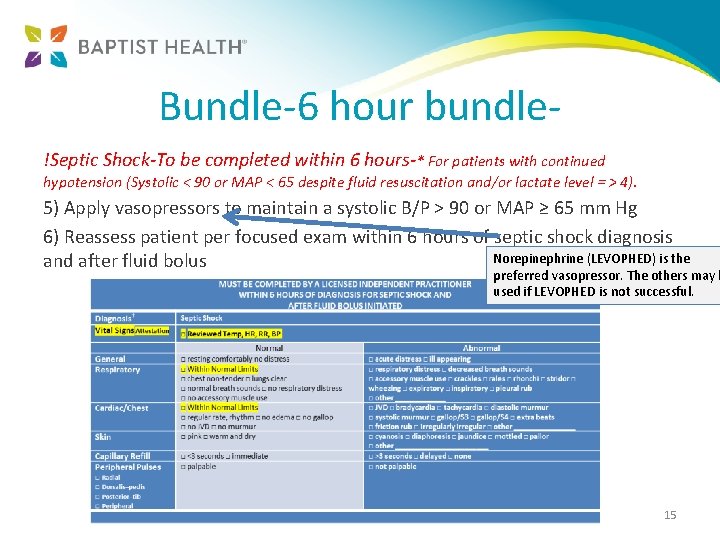
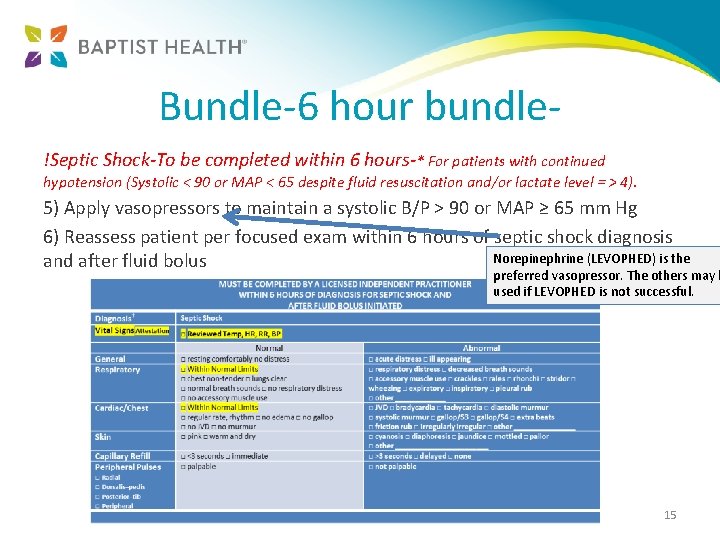
Bundle-6 hour bundle!Septic Shock-To be completed within 6 hours-* For patients with continued hypotension (Systolic < 90 or MAP < 65 despite fluid resuscitation and/or lactate level = > 4). 5) Apply vasopressors to maintain a systolic B/P > 90 or MAP ≥ 65 mm Hg 6) Reassess patient per focused exam within 6 hours of septic shock diagnosis Norepinephrine (LEVOPHED) is the and after fluid bolus preferred vasopressor. The others may b used if LEVOPHED is not successful. 15
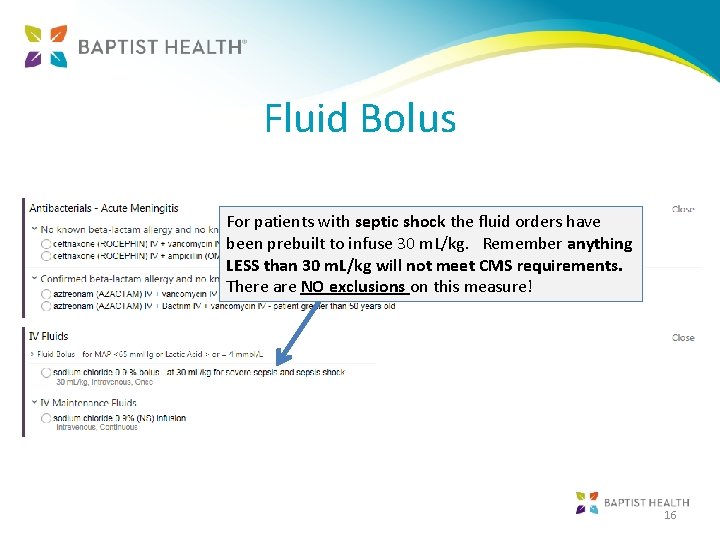
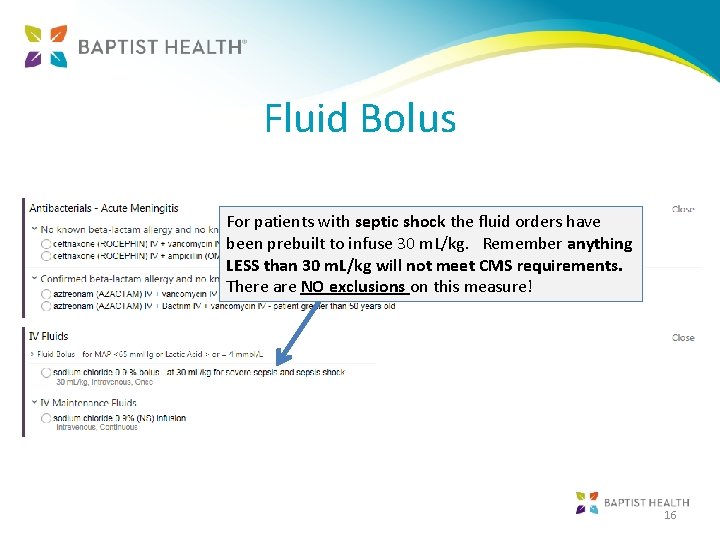
Fluid Bolus For patients with septic shock the fluid orders have been prebuilt to infuse 30 m. L/kg. Remember anything LESS than 30 m. L/kg will not meet CMS requirements. There are NO exclusions on this measure! 16
Diagnostics • • • Blood Cultures Urinalysis and Culture Respiratory culture with gram stain Portable Chest X-Ray-rule out infiltrates Wound Cultures if indicated 17
Case Study • 75 year old female living at home presented to the ED complaining of cramping abdominal pain, diarrhea and weakness X 4 days. Seen by physician at 2: 10 pm • Stated she had fallen at home a couple of times, which was new for her • Denied any blood in her stools. Denied any recent use of antibiotics. • No fever, chills or tachycardia. • Systolic B/P 66 -70 • WBC 6. 4, HGB 13. 6, Creatinine 2. 9 • History of Hypertension, Colitis and Hiatal Hernia • Treatment initiated for IV fluids, occult blood, stool PCR for C-Diff and CT of the Abdomen. 18
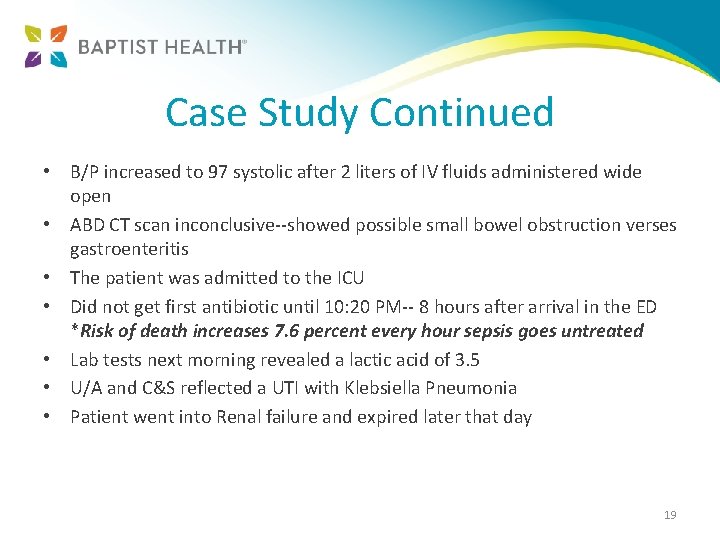
Case Study Continued • B/P increased to 97 systolic after 2 liters of IV fluids administered wide open • ABD CT scan inconclusive--showed possible small bowel obstruction verses gastroenteritis • The patient was admitted to the ICU • Did not get first antibiotic until 10: 20 PM-- 8 hours after arrival in the ED *Risk of death increases 7. 6 percent every hour sepsis goes untreated • Lab tests next morning revealed a lactic acid of 3. 5 • U/A and C&S reflected a UTI with Klebsiella Pneumonia • Patient went into Renal failure and expired later that day 19
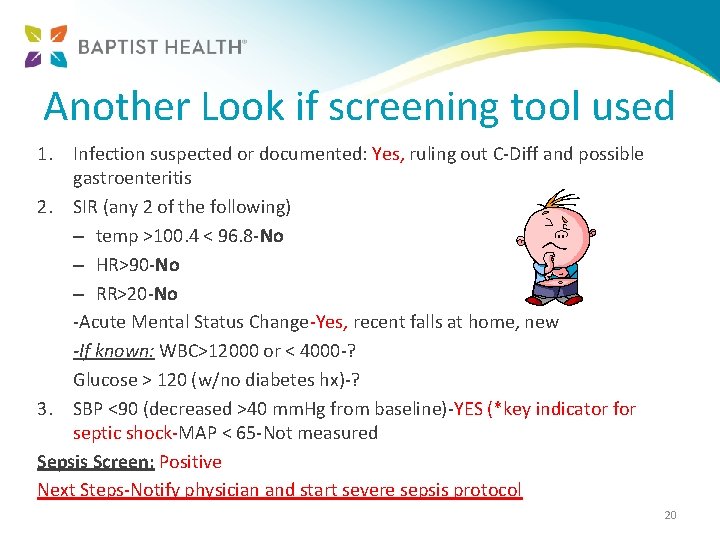
Another Look if screening tool used 1. Infection suspected or documented: Yes, ruling out C-Diff and possible gastroenteritis 2. SIR (any 2 of the following) – temp >100. 4 < 96. 8 -No – HR>90 -No – RR>20 -No -Acute Mental Status Change-Yes, recent falls at home, new -If known: WBC>12000 or < 4000 -? Glucose > 120 (w/no diabetes hx)-? 3. SBP <90 (decreased >40 mm. Hg from baseline)-YES (*key indicator for septic shock-MAP < 65 -Not measured Sepsis Screen: Positive Next Steps-Notify physician and start severe sepsis protocol 20
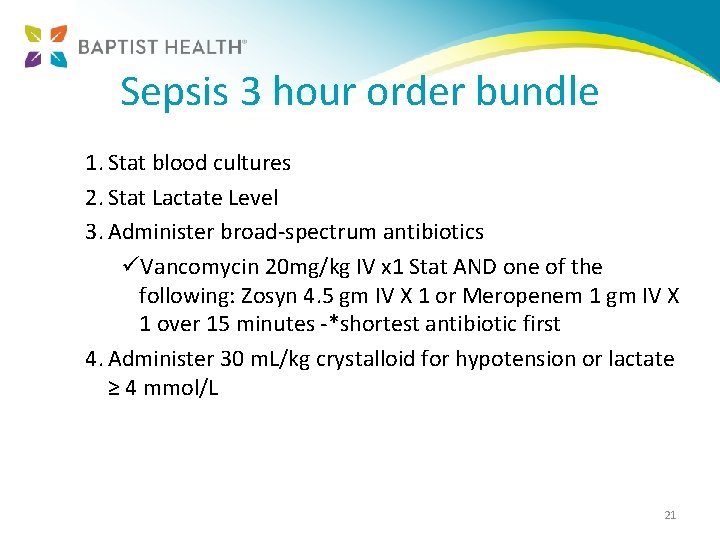
Sepsis 3 hour order bundle 1. Stat blood cultures 2. Stat Lactate Level 3. Administer broad-spectrum antibiotics üVancomycin 20 mg/kg IV x 1 Stat AND one of the following: Zosyn 4. 5 gm IV X 1 or Meropenem 1 gm IV X 1 over 15 minutes -*shortest antibiotic first 4. Administer 30 m. L/kg crystalloid for hypotension or lactate ≥ 4 mmol/L 21
Thank you! Questions? 22
 Sepsis 2 vs sepsis 3
Sepsis 2 vs sepsis 3 Therese hughes
Therese hughes Mark hughes jill hughes
Mark hughes jill hughes Sepsis dietary management
Sepsis dietary management Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * St michael water
St michael water St therese tattoo
St therese tattoo St therese of lisieux facts
St therese of lisieux facts Nina roque
Nina roque Therese stenberg
Therese stenberg Rauquin
Rauquin Therese stamper karlsen
Therese stamper karlsen Thérèse desqueyroux chapitre 13 analyse
Thérèse desqueyroux chapitre 13 analyse Rster
Rster Incipit thérèse raquin
Incipit thérèse raquin Therese duane md
Therese duane md Erlend lilleberg
Erlend lilleberg O oscar ma petite therese
O oscar ma petite therese Therese kemp
Therese kemp St therese of lisieux
St therese of lisieux Therese lindström tiedemann
Therese lindström tiedemann Therese sild
Therese sild Therese raquin naturalism
Therese raquin naturalism