EARLY AND LATE COMPLICATIONS OF PROSTATE LOW DOSE





- Slides: 28
EARLY AND LATE COMPLICATIONS OF PROSTATE LOW DOSE BRACHYTHERAPY A. DZNELADZE, MD, Ph. D G. BOTCHORISHVILI, MD, PROF. A. BOCHORISHVILI, MD
Prostate Brachytherapy accounts more than one century. First attempt to treat prostate cancer with radiation was done in 1901 in Paris, France.
Different techniques and different radioactive materials had been used to treat prostate cancer

Results were controversial until 80 th, when ultrasound developed and industry offered transrectal approach and commercially available I 125 and P 103 seeds.
One of the first patients treated by modern Prostate Brachytherapy – Low Dose Radiation
LDR - the method we use to treat patients with prostate cancer since 2010
Awareness among patients and even among urologists was and is still poor
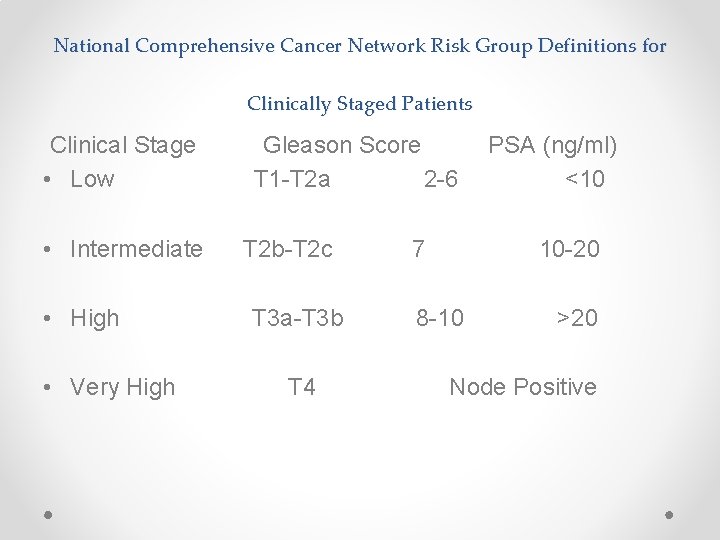
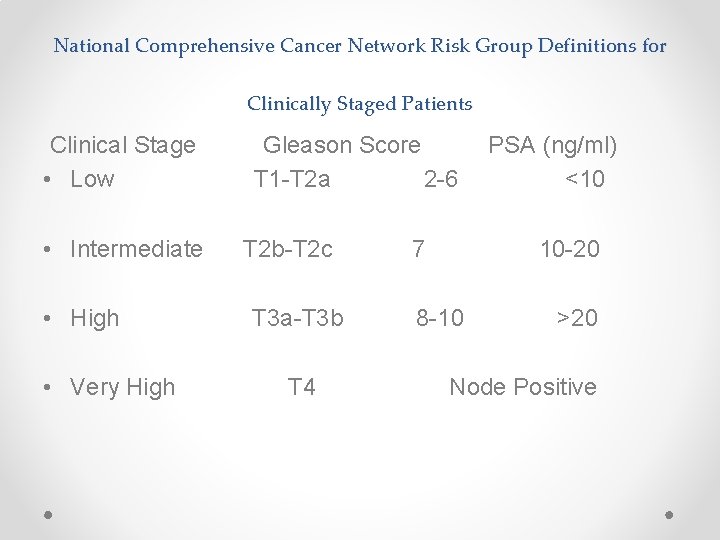
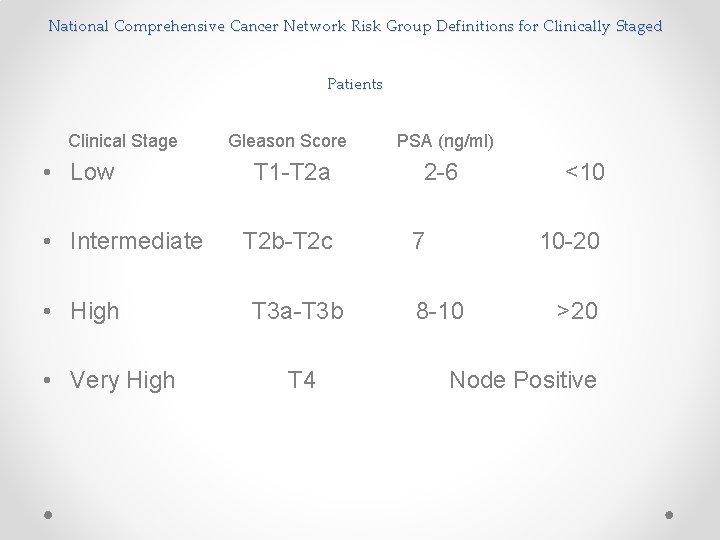
National Comprehensive Cancer Network Risk Group Definitions for Clinically Staged Patients Clinical Stage • Low • Intermediate • High • Very High Gleason Score T 1 -T 2 a 2 -6 T 2 b-T 2 c T 3 a-T 3 b T 4 7 PSA (ng/ml) <10 10 -20 8 -10 >20 Node Positive
Different kinds of techniques are proposed to plan and insert radioactive materials into the prostate • Pre-treatment planning with previously loaded needles. • Real-Time planning with sophisticated software to plan and insert seeds. • Peripheral planning & inserting the seeds using Mick Applicator.

Peripheral planning & inserting the seeds using Mick Applicator
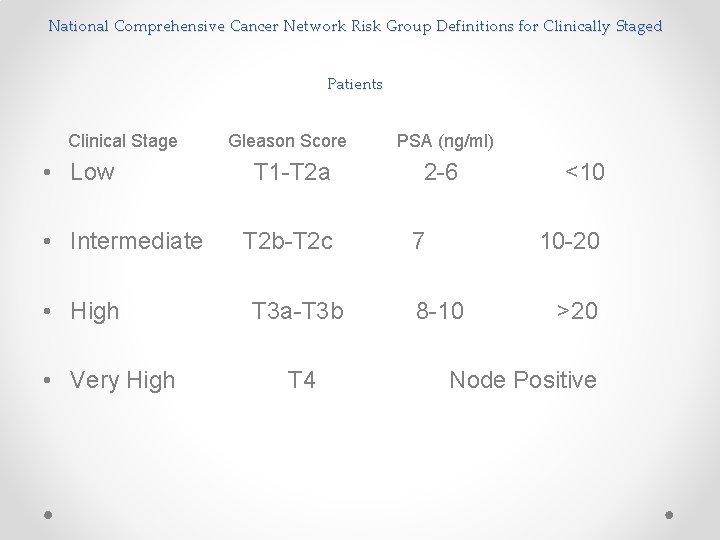
National Comprehensive Cancer Network Risk Group Definitions for Clinically Staged Patients Clinical Stage • Low • Intermediate • High • Very High Gleason Score PSA (ng/ml) T 1 -T 2 a 2 -6 T 2 b-T 2 c T 3 a-T 3 b T 4 7 <10 10 -20 8 -10 >20 Node Positive
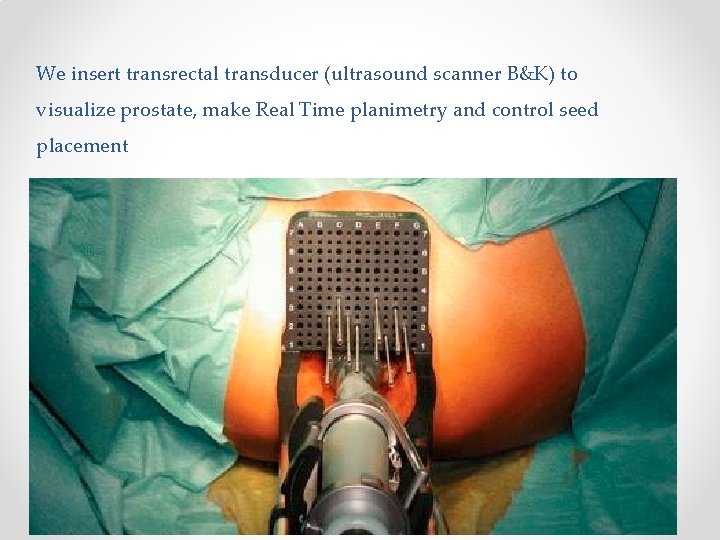
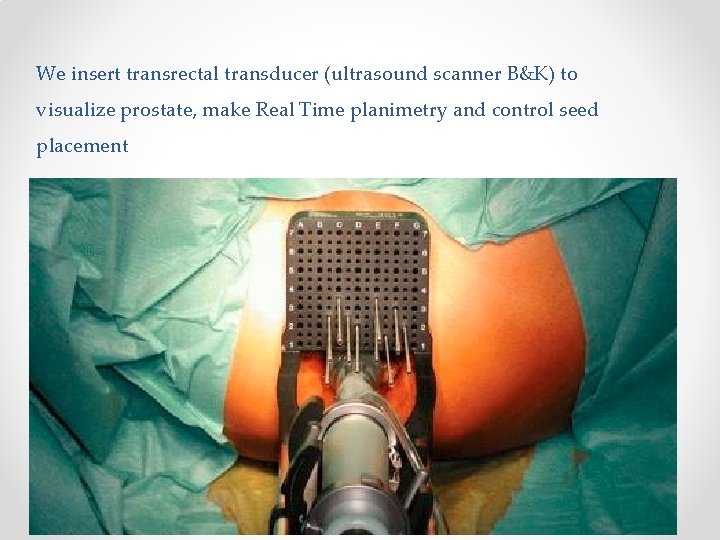
We insert transrectal transducer (ultrasound scanner B&K) to visualize prostate, make Real Time planimetry and control seed placement
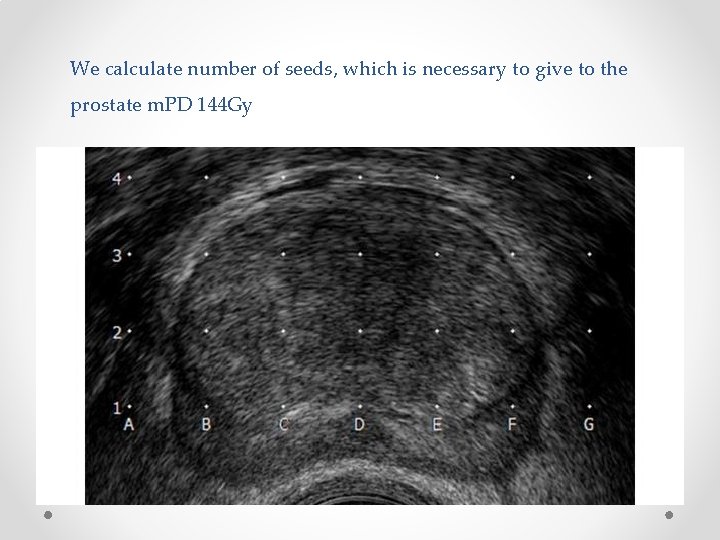
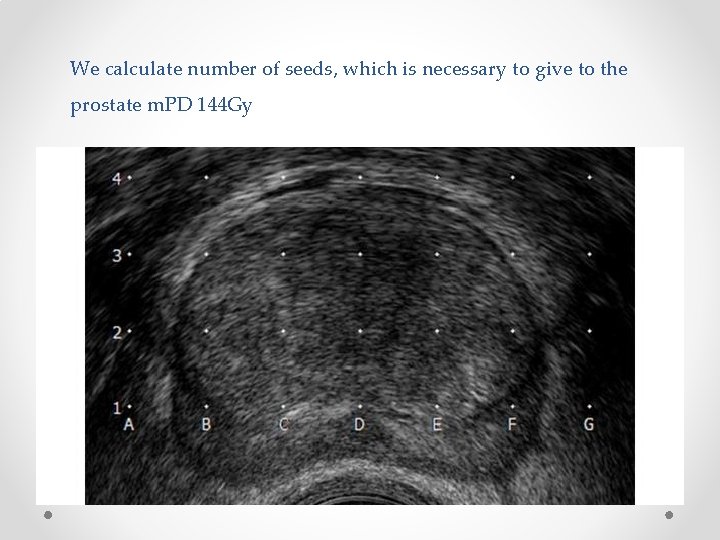
We calculate number of seeds, which is necessary to give to the prostate m. PD 144 Gy
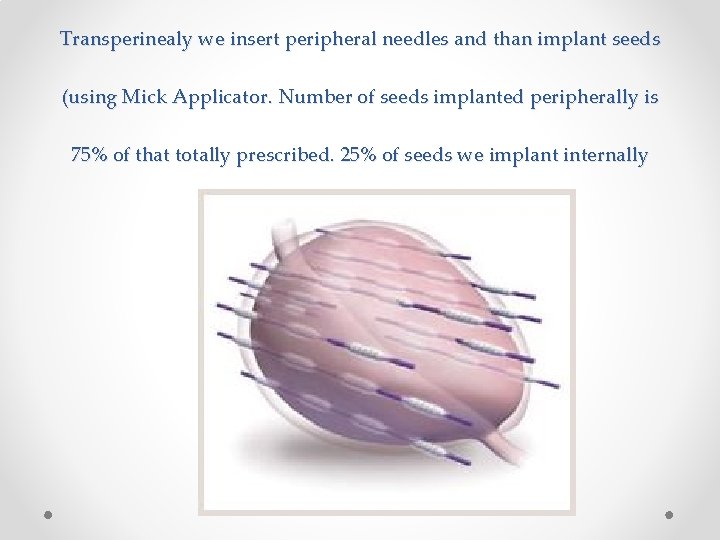
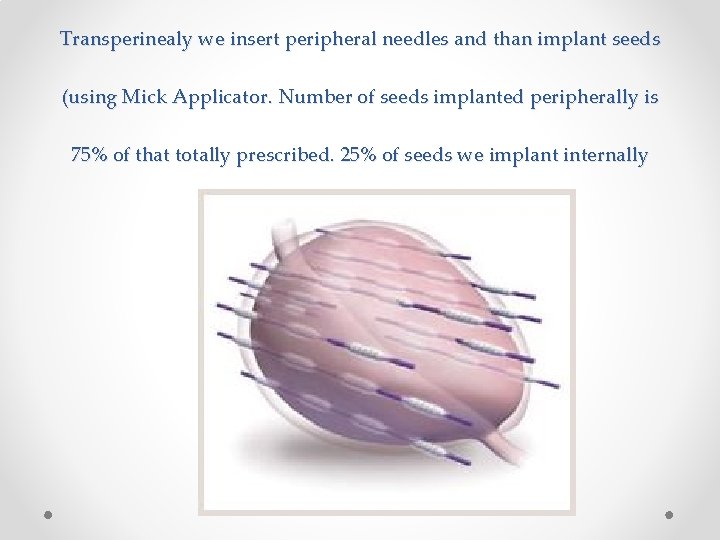
Transperinealy we insert peripheral needles and than implant seeds (using Mick Applicator. Number of seeds implanted peripherally is 75% of that totally prescribed. 25% of seeds we implant internally
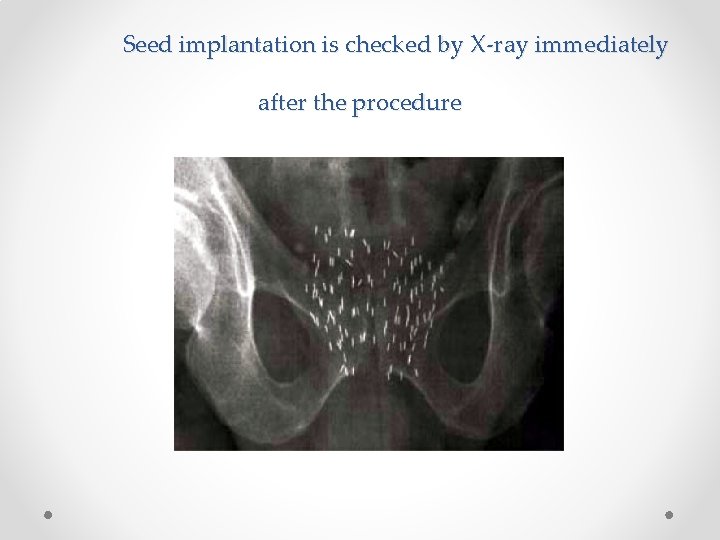
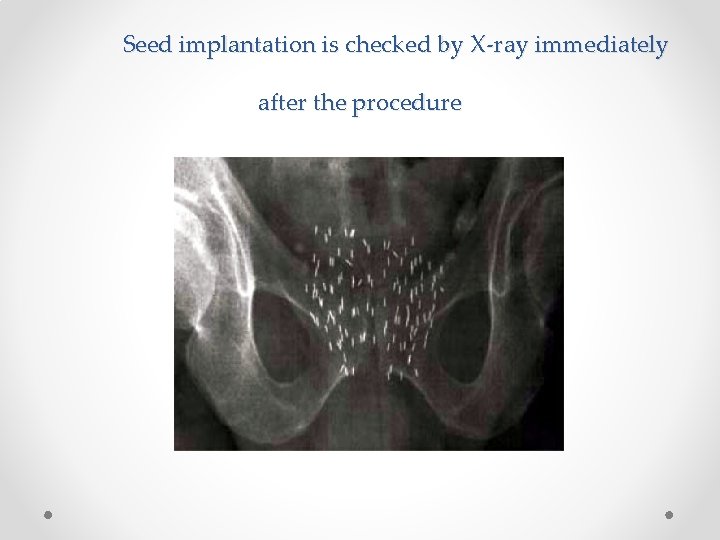
Seed implantation is checked by X-ray immediately after the procedure

From 2010 -2017 years 51 Patients
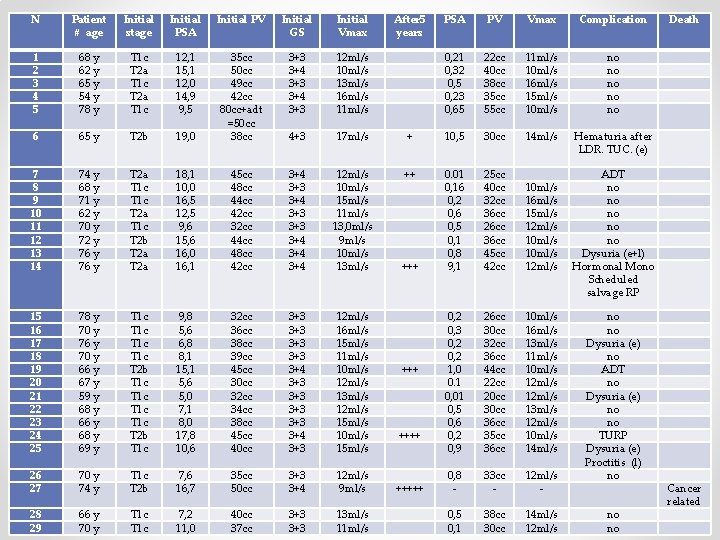
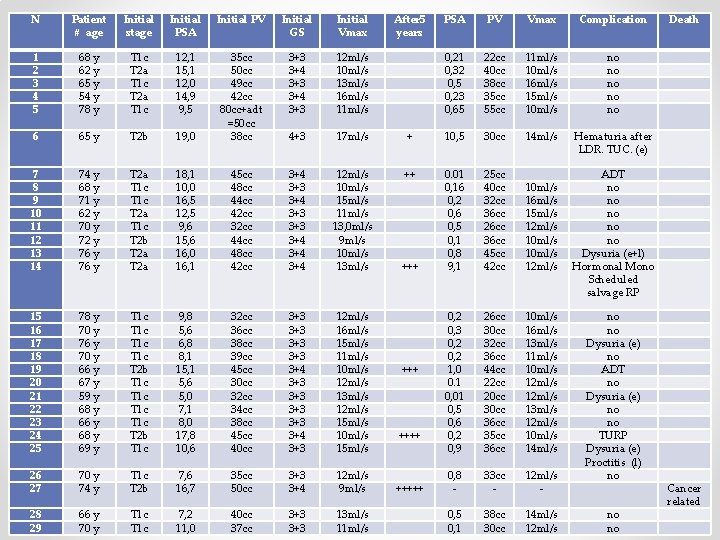
N Patient # age Initial stage Initial PSA Initial PV Initial GS Initial Vmax After 5 years PSA PV Vmax Complication Death 1 2 3 4 5 68 y 62 y 65 y 54 y 78 y T 1 c T 2 a T 1 c 12, 1 15, 1 12, 0 14, 9 9, 5 3+3 3+4 3+3 12 ml/s 10 ml/s 13 ml/s 16 ml/s 11 ml/s 0, 21 0, 32 0, 5 0, 23 0, 65 22 cc 40 cc 38 cc 35 cc 55 cc 11 ml/s 10 ml/s 16 ml/s 15 ml/s 10 ml/s no no no 6 65 y T 2 b 19, 0 35 cc 50 cc 49 cc 42 cc 80 cc+adt =50 cc 38 cc 4+3 17 ml/s + 10, 5 30 cc 14 ml/s Hematuria after LDR. TUC. (e) 7 8 9 10 11 12 13 14 74 y 68 y 71 y 62 y 70 y 72 y 76 y T 2 a T 1 c T 2 b T 2 a 18, 1 10, 0 16, 5 12, 5 9, 6 15, 6 16, 0 16, 1 45 cc 48 cc 44 cc 42 cc 32 cc 44 cc 48 cc 42 cc 3+4 3+3 3+3 3+4 3+4 12 ml/s 10 ml/s 15 ml/s 11 ml/s 13, 0 ml/s 9 ml/s 10 ml/s 13 ml/s ++ +++ 0. 01 0, 16 0, 2 0, 6 0, 5 0, 1 0, 8 9, 1 25 cc 40 cc 32 cc 36 cc 26 cc 36 cc 45 cc 42 cc 10 ml/s 16 ml/s 15 ml/s 12 ml/s 10 ml/s 12 ml/s ADT no no no Dysuria (e+l) Hormonal Mono Scheduled salvage RP 15 16 17 18 19 20 21 22 23 24 25 78 y 70 y 76 y 70 y 66 y 67 y 59 y 68 y 66 y 68 y 69 y T 1 c T 1 c T 2 b T 1 c 9, 8 5, 6 6, 8 8, 1 15, 1 5, 6 5, 0 7, 1 8, 0 17, 8 10, 6 32 cc 36 cc 38 cc 39 cc 45 cc 30 cc 32 cc 34 cc 38 cc 45 cc 40 cc 3+3 3+3 3+4 3+3 12 ml/s 16 ml/s 15 ml/s 11 ml/s 10 ml/s 12 ml/s 13 ml/s 12 ml/s 15 ml/s 10 ml/s 15 ml/s ++++ 0, 2 0, 3 0, 2 1, 0 0. 1 0, 01 0, 5 0, 6 0, 2 0, 9 26 cc 30 cc 32 cc 36 cc 44 cc 22 cc 20 cc 36 cc 35 cc 36 cc 10 ml/s 16 ml/s 13 ml/s 11 ml/s 10 ml/s 12 ml/s 13 ml/s 12 ml/s 10 ml/s 14 ml/s 26 27 70 y 74 y T 1 c T 2 b 7, 6 16, 7 35 cc 50 cc 3+3 3+4 12 ml/s 9 ml/s +++++ 0, 8 - 33 cc - 12 ml/s - no no Dysuria (e) no ADT no Dysuria (e) no no TURP Dysuria (e) Proctitis (l) no 28 29 66 y 70 y T 1 c 7, 2 11, 0 40 cc 37 cc 3+3 13 ml/s 11 ml/s 0, 5 0, 1 38 cc 30 cc 14 ml/s 12 ml/s no no Cancer related
29 Patients • Average – 68 • Highest PSA - 18. 1 ng/ml
Histological • 18 patients Gs 6 3+3 (Grade 1) • 10 patients Gs 7 3+4 (Grade 2) • 1 patients Gs 7 4+3 (Grade 3)
• Prostate volume 30 -50 cc • Urodynamics Vmax lowest 9, 1 ml/s

During 5 years • PSA control every 3 month • TRUS every 6 month
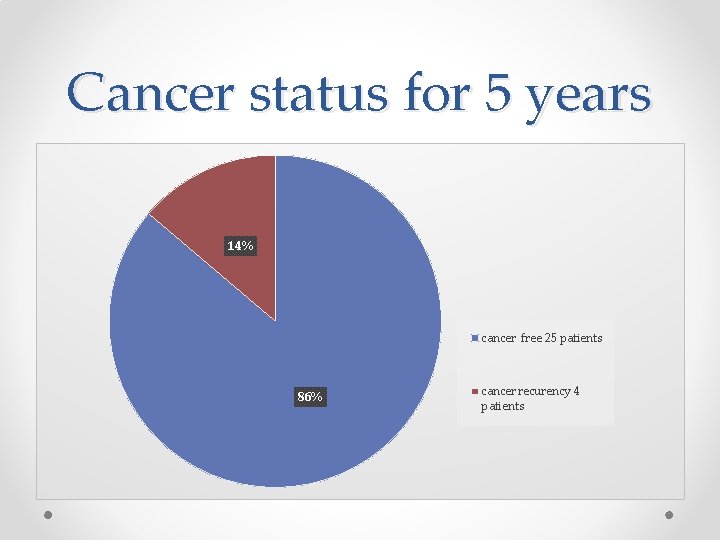
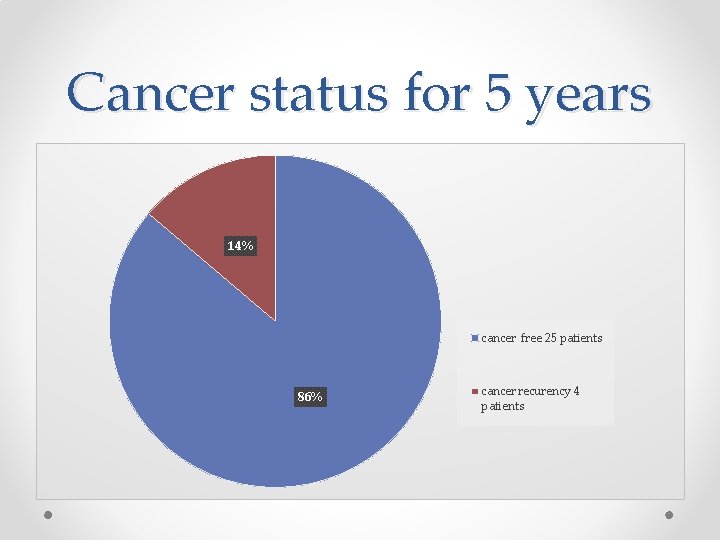
Cancer status for 5 years 14% cancer free 25 patients 86% cancer recurency 4 patients
4 patients cancer recurancy • 3 patient – ADT • 1 Patient died due to cancer progression • 1 patient is waiting for salvage prostatectomy
Early Complications • Two cases of Urine Retention: 1 case retention 1 case with hematuria
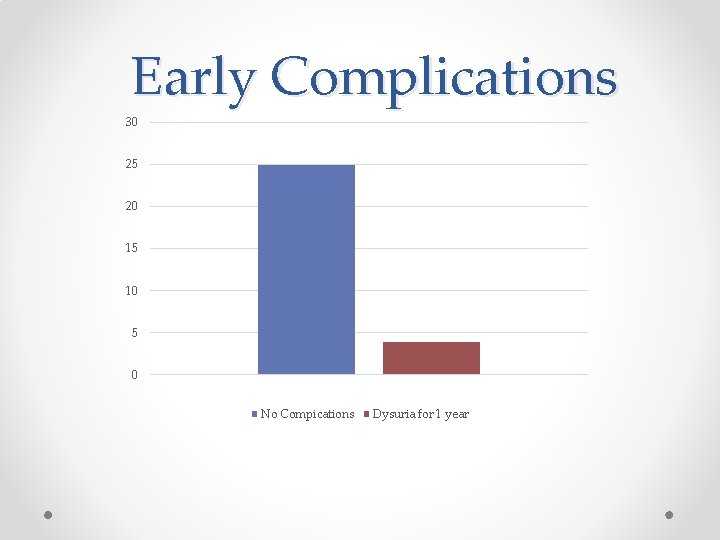
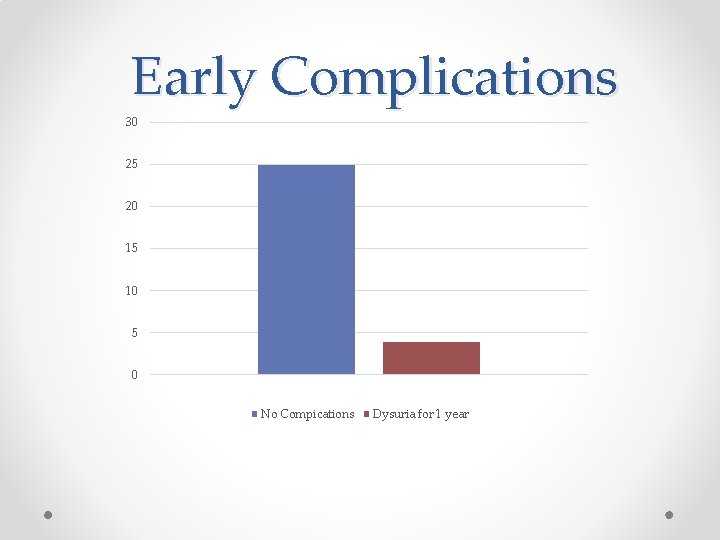
Early Complications 30 25 20 15 10 5 0 No Compications Dysuria for 1 year
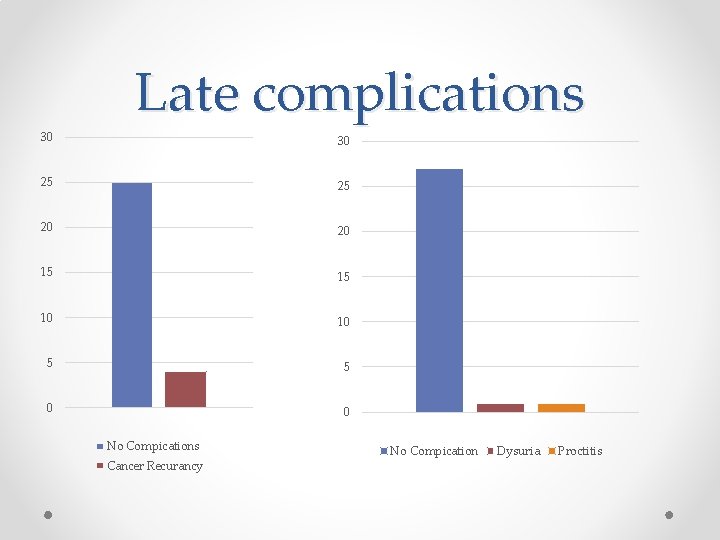
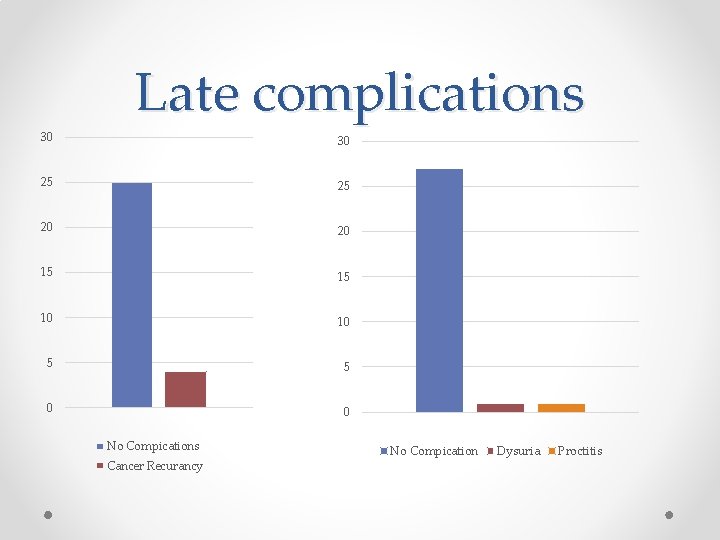
Late complications 30 30 25 25 20 20 15 15 10 10 5 5 0 0 No Compications Cancer Recurancy No Compication Dysuria Proctitis

Conclusion Prostate Low Dose Radiation is well accepted method of treatment of prostate cancer in Low and sometime Intermediate Risk patients. This method is recommended by guidelines of Urology and Radiation Oncology associations. We know, that modern approach to manage low risk patients is also active survilance. Though, many patients diagnosed with prostate cancer are anxious and demand to be treated. Prostate Low Dose Brachytherapy is good option to offer to those patients. This is effective method of treatment with comparably less complications. Number of early and late complications, we observed are limited to urine retention, bleeding and inflammation associated with radiation. Any inflammation lasts until radiation expires. Urine retention and bleeding must be treated surgically. Although surgeon must aware, that intervention after radiation should be minimal. We had no case if urine incontinence after implantation. We know, that this is rare complication and in most of the cases it happens after TURP.
Thank you for your attention.
 Early and late complications of blood transfusion
Early and late complications of blood transfusion Blood transfusion complications
Blood transfusion complications Complications of iv infusion
Complications of iv infusion Perkins timetable of fracture healing
Perkins timetable of fracture healing Softwood anatomy
Softwood anatomy V
V Dental follicle
Dental follicle Dobutamine low dose
Dobutamine low dose Standard screening tomohd
Standard screening tomohd Walgreen uti test
Walgreen uti test Low dominance and low sociability
Low dominance and low sociability Arti kale
Arti kale Salvador late or early theme
Salvador late or early theme Early vs late wood
Early vs late wood Dynamic binding
Dynamic binding Late latent syphilis
Late latent syphilis Welcome to english
Welcome to english Salvador late or early answer key
Salvador late or early answer key Salvador late or early theme
Salvador late or early theme Early cpr and early defibrillation can: *
Early cpr and early defibrillation can: * Middle = low + (high - low) / 2
Middle = low + (high - low) / 2 Low accuracy low precision
Low accuracy low precision Low voltage hazards
Low voltage hazards Function of the ductus deferens
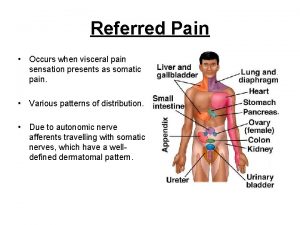
Function of the ductus deferens Prostate referred pain
Prostate referred pain Prostate
Prostate Normal weight of prostate
Normal weight of prostate Prostate
Prostate Viscerosomatic levels
Viscerosomatic levels