Duty of Candour Southern Health NHS Foundation Trust

















- Slides: 71
Duty of Candour - Southern Health NHS Foundation Trust Carlton Sadler, Senior Associate 6 February 2015

Duty of Candour - Southern Health NHS Foundation Trust • • Contractual Duty and Sanctions Statutory Duty – thresholds Delivering candour Professional Duties CQC Inspection Candour case studies
The size of the problem • Estimated that one in ten patients admitted to hospitals in developed countries will be unintentionally the victim of an error. • Around 50% of these events could have been avoided, if lessons from previous incidents had been learned. Carruthers & Philip (2006) Safety First – a report for patients, clinicians and healthcare managers.
Candour “To err is human, to cover up is unforgivable, to fail to learn is inexcusable” – Sir Liam Donaldson
Candour • “I’d far rather be treated by a doctor who at some stage in their career has made a mistake, owned up to it, learnt from the mistake and become a better doctor as a result of that” – Peter Walsh Av. MA • “if I was going to be choosing -- if the only information I had was reporting systems for my choice of hospital, I would choose the one with the highest possible reporting rate” – Prof Charles Vincent
“What is required now is a real change in culture, a refocusing and recommitment of all who work in the NHS – from top to bottom of the system - on putting the patient first” - Robert Francis QC
Candour (and more) • Openness: enabling concerns to be raised and disclosed freely without fear, and for questions to be answered; • Transparency: allowing true information about performance and outcomes to be shared with staff, patients and the public; • Candour: ensuring that patients harmed by a healthcare service are informed of the fact and that an appropriate remedy is offered, whether or not a complaint has been made or a question asked about it.
Candour (and more) • • • Openness • Complaints - Facilitating / quarterly publishing • Raising concerns and Whistle blowing • ‘Gagging’ clauses Duties of candour • professional • contractual • statutory Transparency • ‘duty of co-operation’ • Inquest disclosure • Offence – false or misleading information

Candour – the duties
Candour – the contractual duty • SC 35 – since 1 April 2013 (and change to NHS Constitution) • “Reportable Patient Safety Incident” – moderate or severe harm or death • “occurs or is suspected”
Candour – the contractual duty • “Reportable Patient Safety Incident” – a Patient Safety Incident which involves moderate harm or severe harm • “Patient Safety Incident” - any unintended or unexpected incident that occurs in respect of a Service User, during and as a result of the provision of the Services, that could have led, or did lead to, harm to that Service User • Moderate: Any patient safety incident that resulted in a moderate increase in treatment and which caused significant but not permanent harm, to one or more persons receiving NHS-funded care. Severe: Any patient safety incident that appears to have resulted in permanent harm to one or more persons receiving NHS-funded care. •
Candour – the contractual duty • Notify “as soon as practicable, but in any event within 10 Operational Days” • Verbal/ in person “including, where possible the clinician responsible for the episode of care” • Provide all facts the provider knows about • Appropriate Apology • Offer of written notification • “a step by step explanation of events and circumstances which resulted in the incident and any other pertinent information … updated as the investigation proceeds” • Copy of the investigation report (35. 1. 6)
Candour – the contractual duty • Provider failure to comply – Co-ordinating Commissioner: • Notifies CQC Requires formal written apology and explanation to the Relevant person • Provider to “publish details of that failure prominently” on its website • • Can implement contractual consequences – deductions • “Recovery of the cost of the episode of care, or £ 10, 000 if the cost of the episode of care is unknown or indeterminate” - SC 35. 3 and 4
Candour – the statutory duty A statutory obligation should be imposed to observe a duty of candour: • On healthcare providers who believe or suspect that treatment or care provided by it to a patient has caused death or serious injury to a patient to inform that patient or other duly authorised person as soon as is practicable of that fact and thereafter to provide such information and explanation as the patient reasonably may request; • On registered medical practitioners and registered nurses … • The provision of information in compliance with this requirement should not of itself be evidence or an admission of any civil or criminal liability, but non -compliance with the statutory duty should entitle the patient to a remedy. - MSI r 181
Candour – the statutory duty

Candour – the statutory duty

Candour – the statutory duty • • • Regulatory requirement – s 81 Care Act 2014 Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 – regulation 20 Threshold – ? ? • ‘health service bodies’ • other providers Direct prosecution – Level 4 fine Providers Directors etc “consent/ connivance/ neglect”
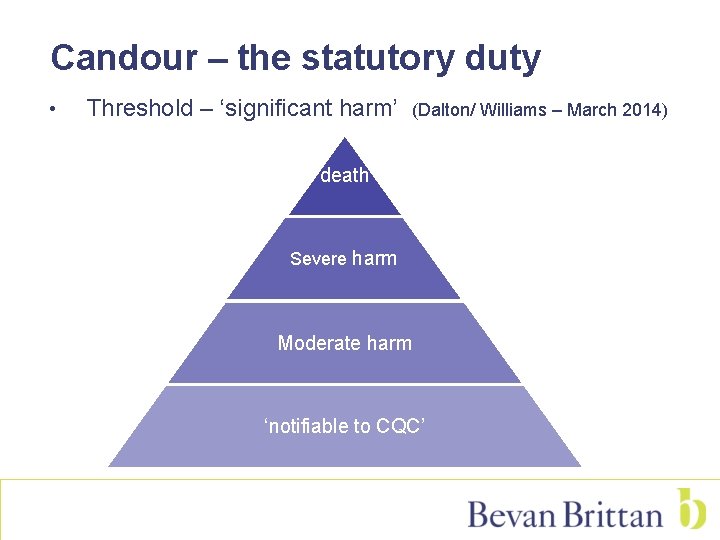
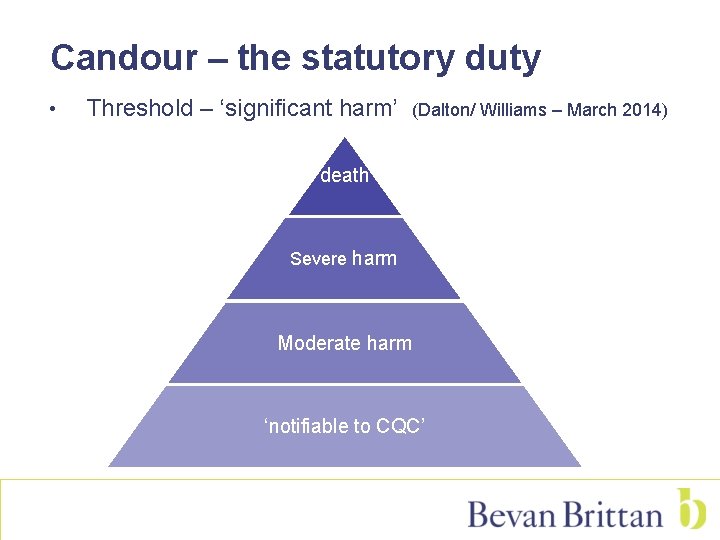
Candour – the statutory duty • Threshold – ‘significant harm’ (Dalton/ Williams – March 2014) death Severe harm Moderate harm ‘notifiable to CQC’
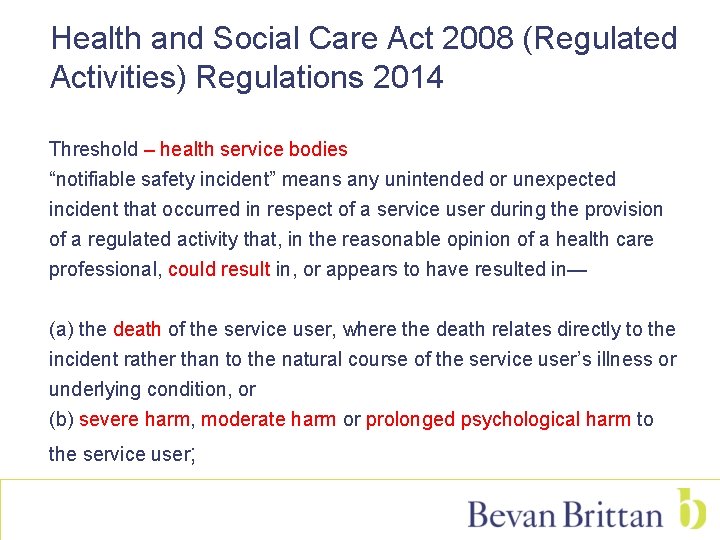
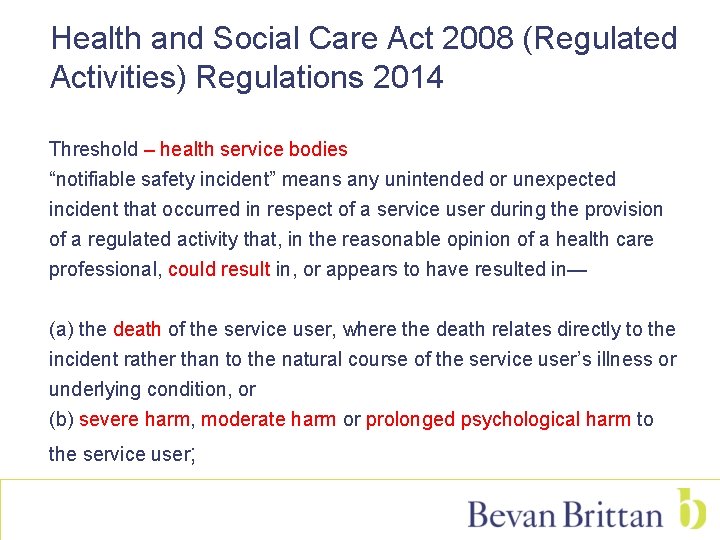
Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 Threshold – health service bodies “notifiable safety incident” means any unintended or unexpected incident that occurred in respect of a service user during the provision of a regulated activity that, in the reasonable opinion of a health care professional, could result in, or appears to have resulted in— (a) the death of the service user, where the death relates directly to the incident rather than to the natural course of the service user’s illness or underlying condition, or (b) severe harm, moderate harm or prolonged psychological harm to the service user;

Notifiable Safety Incident - thresholds • “severe harm” means a permanent lessening of bodily, sensory, motor, physiologic or intellectual functions, including removal of the wrong limb or organ or brain damage, that is related directly to the incident and not related to the natural course of the service user’s illness or underlying condition. • “moderate harm” means— (a) harm that requires a moderate increase in treatment, and (b) significant, but not permanent, harm; • “moderate increase in treatment” means an unplanned return to surgery, an unplanned re-admission, a prolonged episode of care, extra time in hospital or as an outpatient, cancelling of treatment, or transfer to another treatment area (such as intensive care);
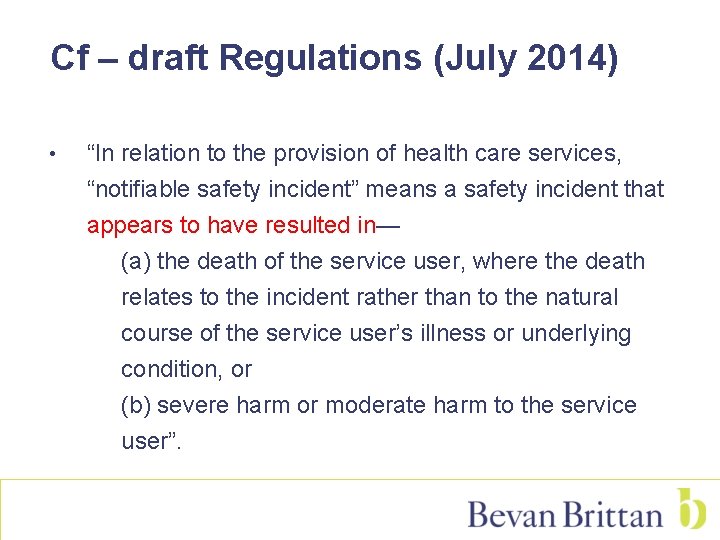
Cf – draft Regulations (July 2014) • “In relation to the provision of health care services, “notifiable safety incident” means a safety incident that appears to have resulted in— (a) the death of the service user, where the death relates to the incident rather than to the natural course of the service user’s illness or underlying condition, or (b) severe harm or moderate harm to the service user”.
Delivering candour
Candour – a history lesson? • “Guidance and policies should be reviewed to ensure that they will lead to compliance with Being Open, the guidance published by the National Patient Safety Agency” – MSI r 180
Candour – a history lesson? • Being Open – NPSA (2005 – reissued in 2009) • It is Step 5: Involve and communicate with patients and the public (in Seven steps to patient safety) • Benefits for the organisation include: - reinforces a culture of openness; - potentially reduces the costs of litigation; - improves the patient experience and satisfaction with the organisation; - greater opportunity to learn when things go wrong

Candour – practicalities • Mechanisms of Being open • Apology – meaningful, not delayed for investigation • Professional support - to ensure a robust and consistent approach to incident investigation, healthcare organisations are advised to use the NRLS’s Incident Decision Tree
Candour - practicalities • Mechanisms of Being open (cont’d) • Risk management - Root Cause Analysis, Significant Event Audit (SEA) or similar should be used to uncover the underlying causes of the incident. - every organisation’s Being open policy should be integrated into local incident reporting and risk management policies and processes • Clinical (Quality) governance - Being open involves a system of accountability through the chief executive to the board to ensure implementation and review of effectiveness. - Continuous learning programmes and audits should be developed that allow healthcare organisations to learn from the patient’s experience of Being open
Candour – practicalities Being open actions Boards • Identifying executive and non-executive leads responsible for ensuring that the Being open principles and policy are embedded in the organisation. • Ensuring that a Being open policy is in place and fully implemented throughout the organisation – the policy must be fully integrated with other policies, especially clinical governance, risk management and concerns and complaints policies • Gaining assurance that a training programme is in place to raise awareness amongst all staff of the Being open framework
The statutory duty 20. —(1) A health service body must act in an open and transparent way with relevant persons in relation to care and treatment provided to service users in carrying on a regulated activity.
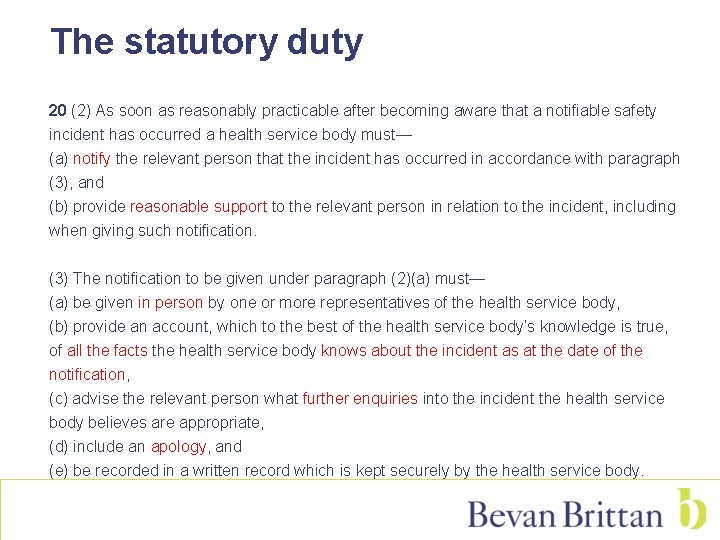
The statutory duty 20 (2) As soon as reasonably practicable after becoming aware that a notifiable safety incident has occurred a health service body must— (a) notify the relevant person that the incident has occurred in accordance with paragraph (3), and (b) provide reasonable support to the relevant person in relation to the incident, including when giving such notification. (3) The notification to be given under paragraph (2)(a) must— (a) be given in person by one or more representatives of the health service body, (b) provide an account, which to the best of the health service body’s knowledge is true, of all the facts the health service body knows about the incident as at the date of the notification, (c) advise the relevant person what further enquiries into the incident the health service body believes are appropriate, (d) include an apology, and (e) be recorded in a written record which is kept securely by the health service body.
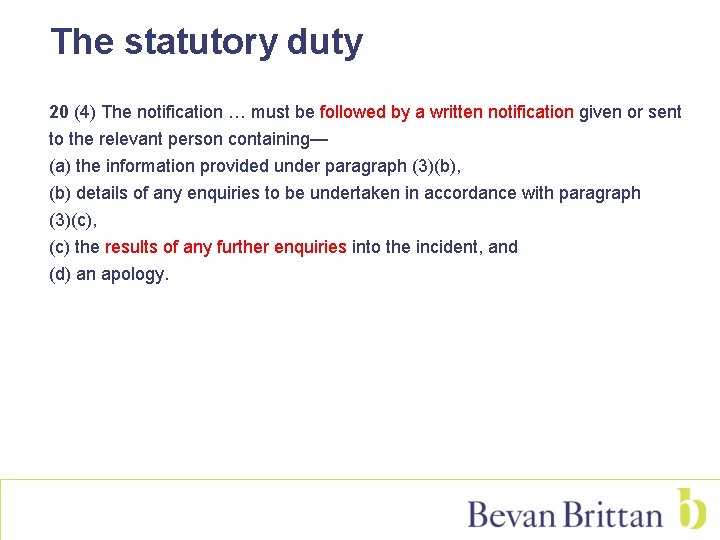
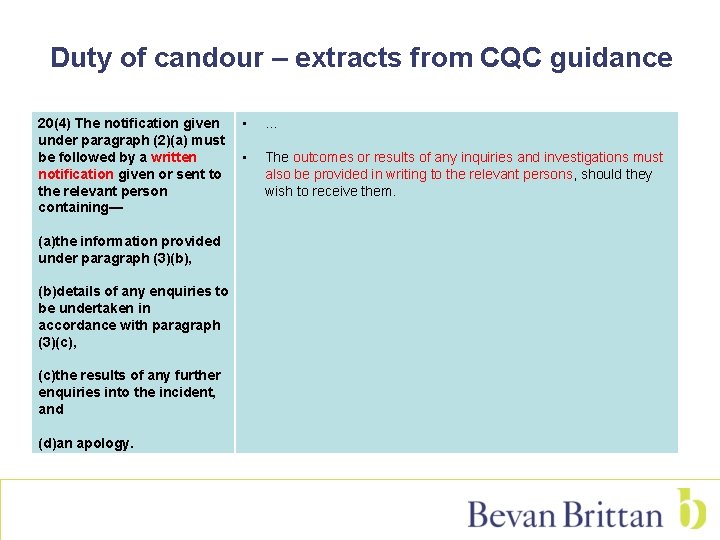
The statutory duty 20 (4) The notification … must be followed by a written notification given or sent to the relevant person containing— (a) the information provided under paragraph (3)(b), (b) details of any enquiries to be undertaken in accordance with paragraph (3)(c), (c) the results of any further enquiries into the incident, and (d) an apology.
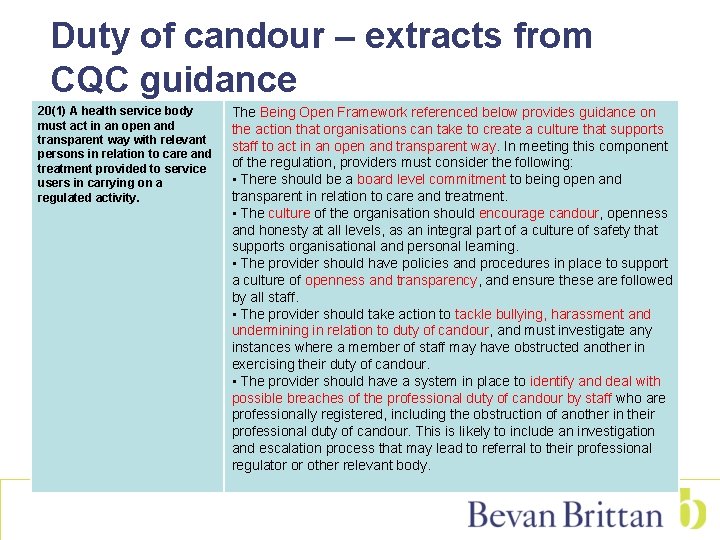
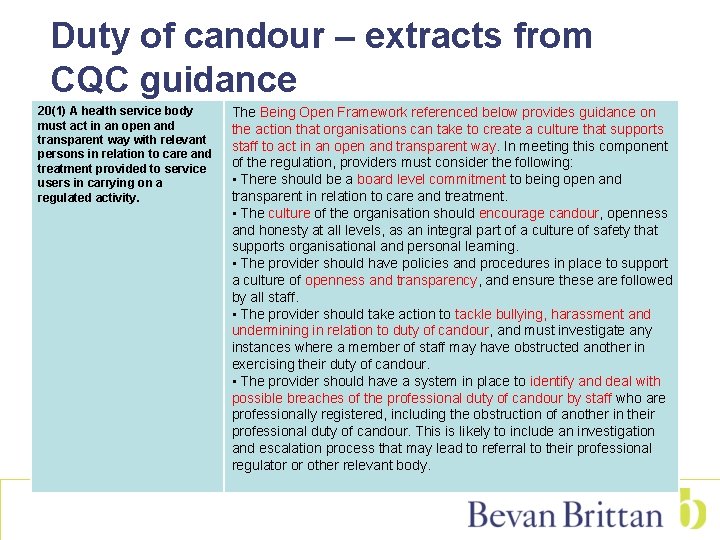
Duty of candour – extracts from CQC guidance 20(1) A health service body must act in an open and transparent way with relevant persons in relation to care and treatment provided to service users in carrying on a regulated activity. The Being Open Framework referenced below provides guidance on the action that organisations can take to create a culture that supports staff to act in an open and transparent way. In meeting this component of the regulation, providers must consider the following: • There should be a board level commitment to being open and transparent in relation to care and treatment. • The culture of the organisation should encourage candour, openness and honesty at all levels, as an integral part of a culture of safety that supports organisational and personal learning. • The provider should have policies and procedures in place to support a culture of openness and transparency, and ensure these are followed by all staff. • The provider should take action to tackle bullying, harassment and undermining in relation to duty of candour, and must investigate any instances where a member of staff may have obstructed another in exercising their duty of candour. • The provider should have a system in place to identify and deal with possible breaches of the professional duty of candour by staff who are professionally registered, including the obstruction of another in their professional duty of candour. This is likely to include an investigation and escalation process that may lead to referral to their professional regulator or other relevant body.
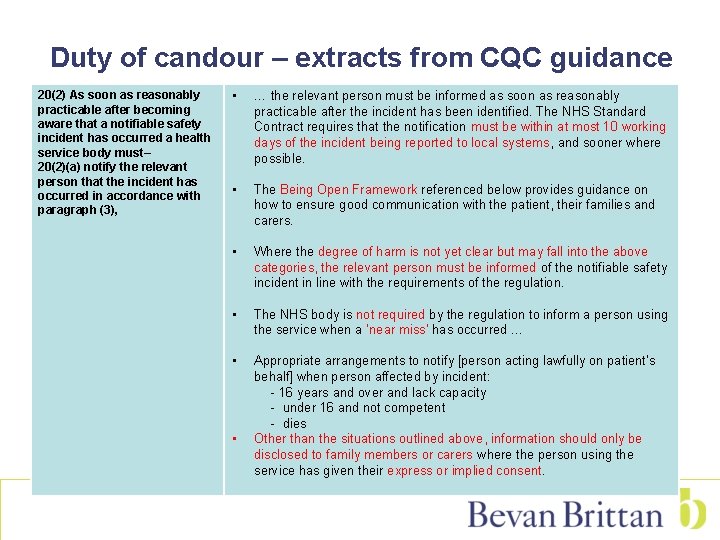
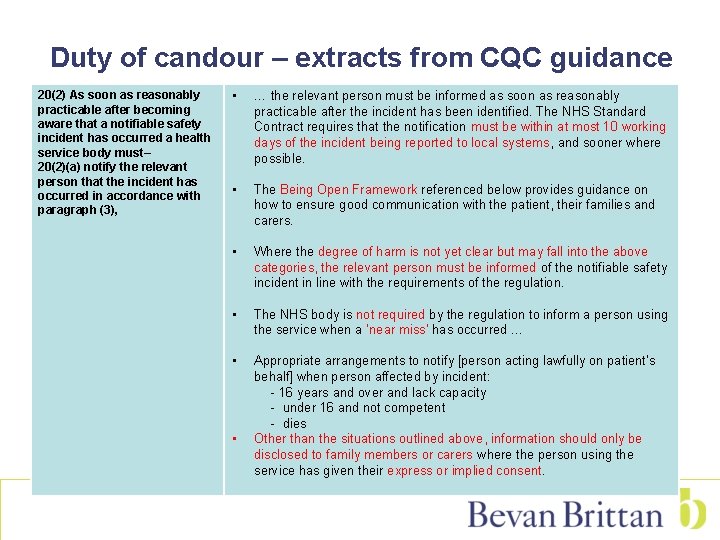
Duty of candour – extracts from CQC guidance 20(2) As soon as reasonably practicable after becoming aware that a notifiable safety incident has occurred a health service body must– 20(2)(a) notify the relevant person that the incident has occurred in accordance with paragraph (3), • … the relevant person must be informed as soon as reasonably practicable after the incident has been identified. The NHS Standard Contract requires that the notification must be within at most 10 working days of the incident being reported to local systems, and sooner where possible. • The Being Open Framework referenced below provides guidance on how to ensure good communication with the patient, their families and carers. • Where the degree of harm is not yet clear but may fall into the above categories, the relevant person must be informed of the notifiable safety incident in line with the requirements of the regulation. • The NHS body is not required by the regulation to inform a person using the service when a ‘near miss’ has occurred … • Appropriate arrangements to notify [person acting lawfully on patient’s behalf] when person affected by incident: - 16 years and over and lack capacity - under 16 and not competent - dies • Other than the situations outlined above, information should only be disclosed to family members or carers where the person using the service has given their express or implied consent.
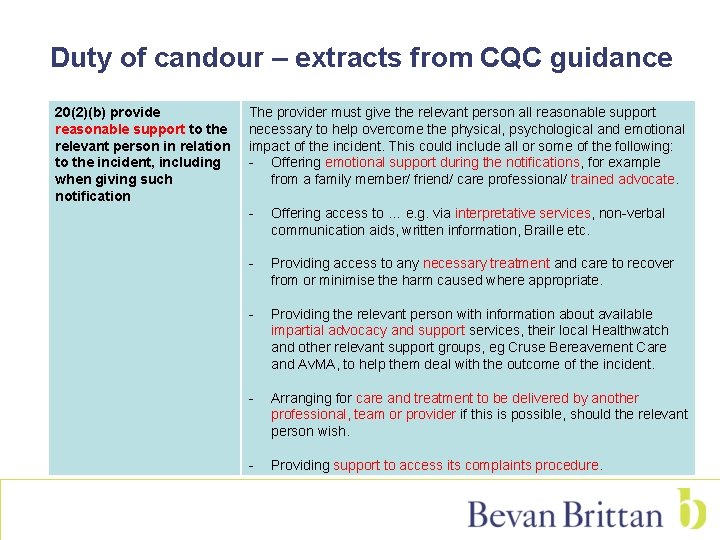
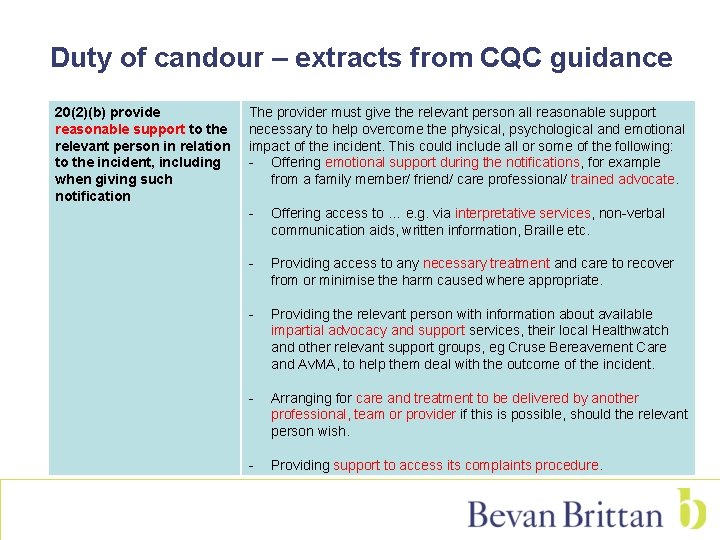
Duty of candour – extracts from CQC guidance 20(2)(b) provide reasonable support to the relevant person in relation to the incident, including when giving such notification The provider must give the relevant person all reasonable support necessary to help overcome the physical, psychological and emotional impact of the incident. This could include all or some of the following: - Offering emotional support during the notifications, for example from a family member/ friend/ care professional/ trained advocate. - Offering access to … e. g. via interpretative services, non-verbal communication aids, written information, Braille etc. - Providing access to any necessary treatment and care to recover from or minimise the harm caused where appropriate. - Providing the relevant person with information about available impartial advocacy and support services, their local Healthwatch and other relevant support groups, eg Cruse Bereavement Care and Av. MA, to help them deal with the outcome of the incident. - Arranging for care and treatment to be delivered by another professional, team or provider if this is possible, should the relevant person wish. - Providing support to access its complaints procedure.
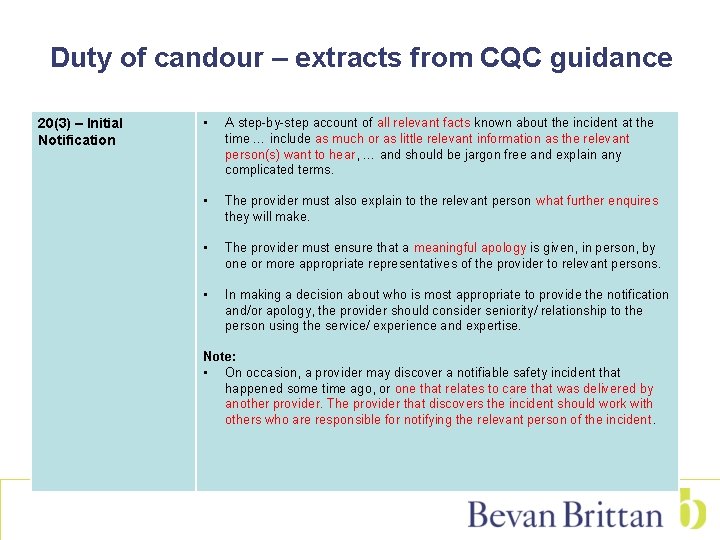
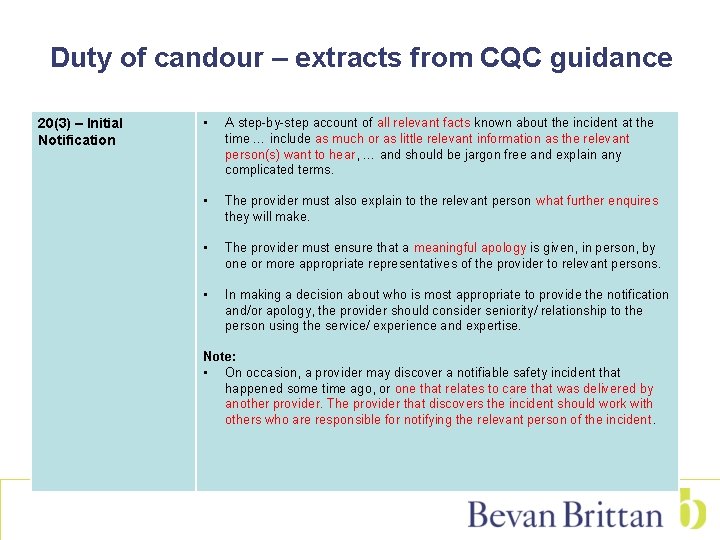
Duty of candour – extracts from CQC guidance 20(3) – Initial Notification • A step-by-step account of all relevant facts known about the incident at the time … include as much or as little relevant information as the relevant person(s) want to hear, … and should be jargon free and explain any complicated terms. • The provider must also explain to the relevant person what further enquires they will make. • The provider must ensure that a meaningful apology is given, in person, by one or more appropriate representatives of the provider to relevant persons. • In making a decision about who is most appropriate to provide the notification and/or apology, the provider should consider seniority/ relationship to the person using the service/ experience and expertise. Note: • On occasion, a provider may discover a notifiable safety incident that happened some time ago, or one that relates to care that was delivered by another provider. The provider that discovers the incident should work with others who are responsible for notifying the relevant person of the incident.
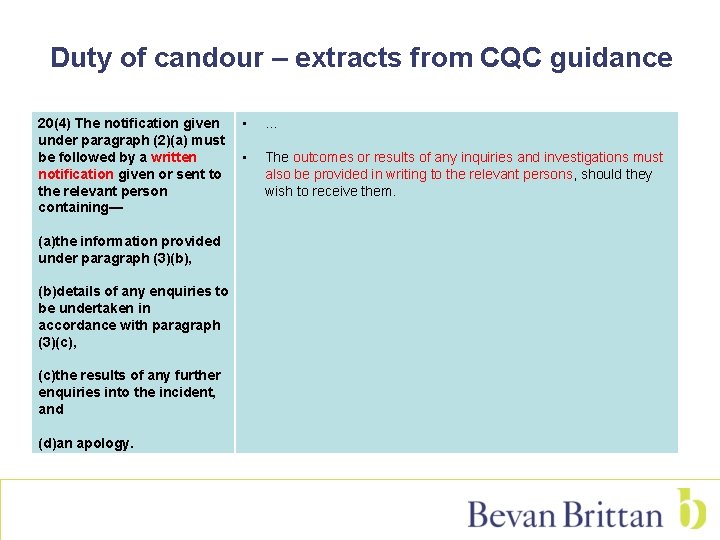
Duty of candour – extracts from CQC guidance 20(4) The notification given under paragraph (2)(a) must be followed by a written notification given or sent to the relevant person containing— (a)the information provided under paragraph (3)(b), (b)details of any enquiries to be undertaken in accordance with paragraph (3)(c), (c)the results of any further enquiries into the incident, and (d)an apology. • . . . • The outcomes or results of any inquiries and investigations must also be provided in writing to the relevant persons, should they wish to receive them.
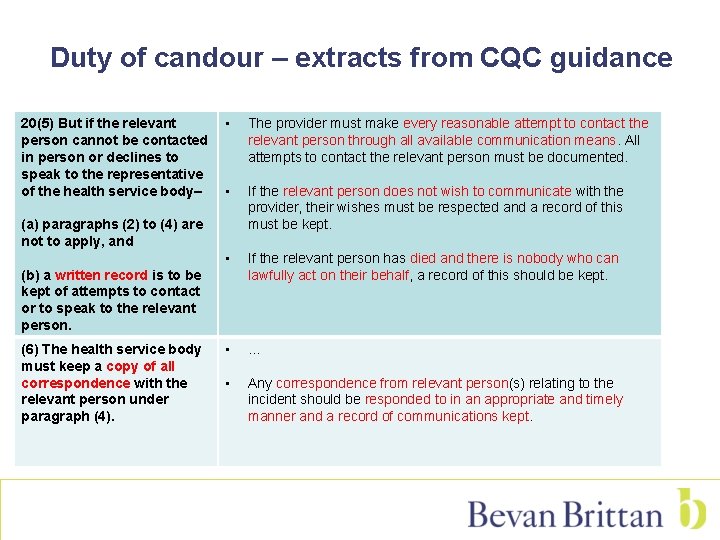
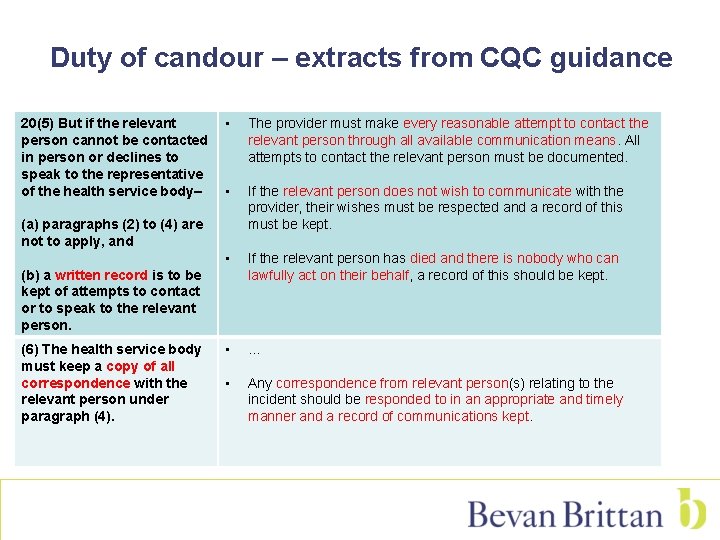
Duty of candour – extracts from CQC guidance 20(5) But if the relevant person cannot be contacted in person or declines to speak to the representative of the health service body– • The provider must make every reasonable attempt to contact the relevant person through all available communication means. All attempts to contact the relevant person must be documented. • If the relevant person does not wish to communicate with the provider, their wishes must be respected and a record of this must be kept. • If the relevant person has died and there is nobody who can lawfully act on their behalf, a record of this should be kept. • … • Any correspondence from relevant person(s) relating to the incident should be responded to in an appropriate and timely manner and a record of communications kept. (a) paragraphs (2) to (4) are not to apply, and (b) a written record is to be kept of attempts to contact or to speak to the relevant person. (6) The health service body must keep a copy of all correspondence with the relevant person under paragraph (4).
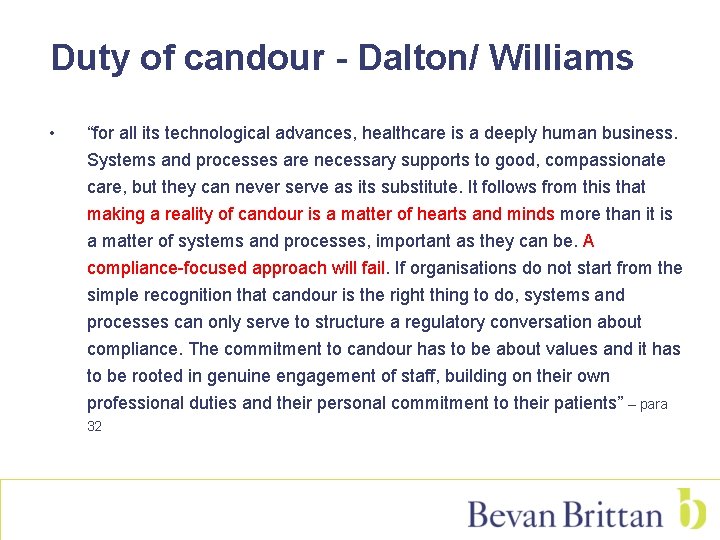
Duty of candour - Dalton/ Williams • “for all its technological advances, healthcare is a deeply human business. Systems and processes are necessary supports to good, compassionate care, but they can never serve as its substitute. It follows from this that making a reality of candour is a matter of hearts and minds more than it is a matter of systems and processes, important as they can be. A compliance-focused approach will fail. If organisations do not start from the simple recognition that candour is the right thing to do, systems and processes can only serve to structure a regulatory conversation about compliance. The commitment to candour has to be about values and it has to be rooted in genuine engagement of staff, building on their own professional duties and their personal commitment to their patients” – para 32
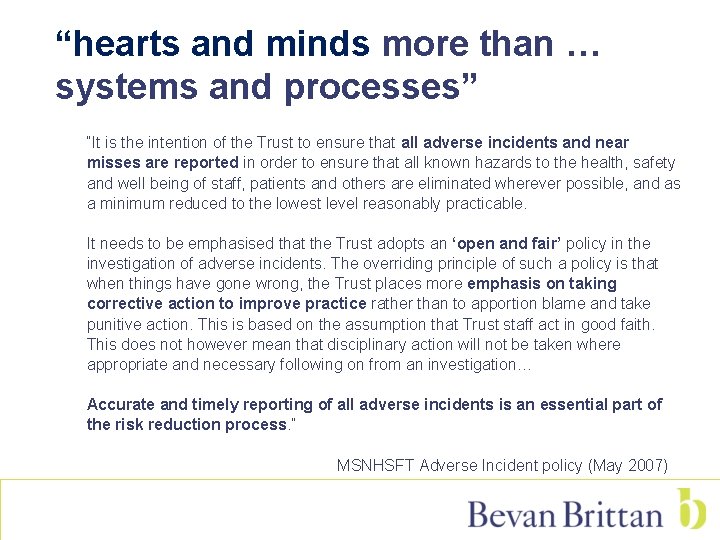
“hearts and minds more than … systems and processes” “It is the intention of the Trust to ensure that all adverse incidents and near misses are reported in order to ensure that all known hazards to the health, safety and well being of staff, patients and others are eliminated wherever possible, and as a minimum reduced to the lowest level reasonably practicable. It needs to be emphasised that the Trust adopts an ‘open and fair’ policy in the investigation of adverse incidents. The overriding principle of such a policy is that when things have gone wrong, the Trust places more emphasis on taking corrective action to improve practice rather than to apportion blame and take punitive action. This is based on the assumption that Trust staff act in good faith. This does not however mean that disciplinary action will not be taken where appropriate and necessary following on from an investigation… Accurate and timely reporting of all adverse incidents is an essential part of the risk reduction process. ” MSNHSFT Adverse Incident policy (May 2007)

Duty of candour - Dalton/ Williams • The importance of consent • “where practitioners are isolated, they are likely to need support to ensure that they are candid” • CQC – “looking for patterns in organisational behaviour rather than one-off breaches (though stark cases will of course merit particular scrutiny). ” - para 10

Dalton/ Williams – Australian Open Disclosure Framework
Professional Duties
Candour – professional duties • “The professional regulators will develop new guidance to make it clear professionals’ responsibility to report ‘near misses’ for errors that could have led to death or serious injury, as well as actual harm, … and will review their professional codes of conduct to bring them into line with this guidance. ” – Hard Truths vol 2 p 157
Candour – professional duties Be open and candid with all service users about all aspects of care and treatment, including when any mistakes or harm have taken place To achieve this, you must: 14. 1 act immediately to put right the situation if someone has suffered actual harm for any reason or an incident has happened which had the potential for harm 14. 2 explain fully and promptly what has happened, including the likely effects, and apologise to the person affected and, where appropriate, their advocate, family or carers, and 14. 3 document all these events formally and take further action (escalate) if appropriate so they can be dealt with quickly. - para 14 NMC Code (Jan 2015) “You must be open and honest with patients if things go wrong. If a patient under your care has suffered harm or distress, you should: a. put matters right (if that is possible) b. offer an apology c. explain fully and promptly what has happened and the likely short-term and long-term effects” – para 55 Good Medical Practice
• Openness and honesty when things go wrong: the professional duty of candour A draft for consultation – NMC/GMC – 4 November 2014 http: //www. gmc-uk. org/Openness_and_honesty___Draft_guidance. pdf_58423740. pdf
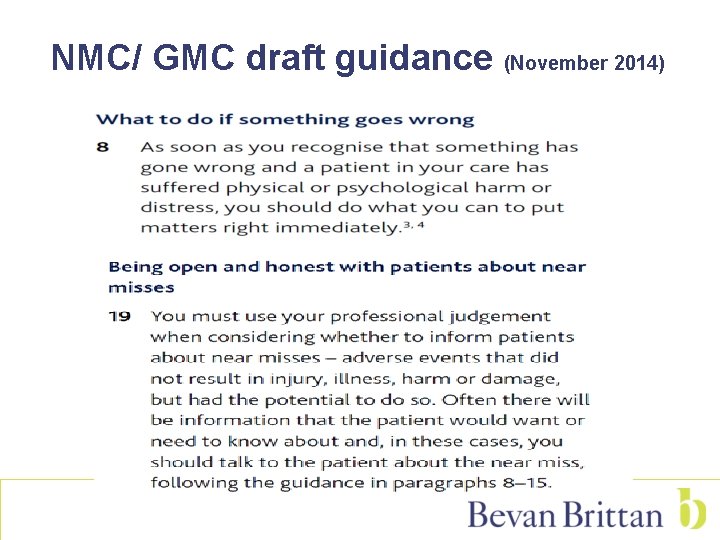
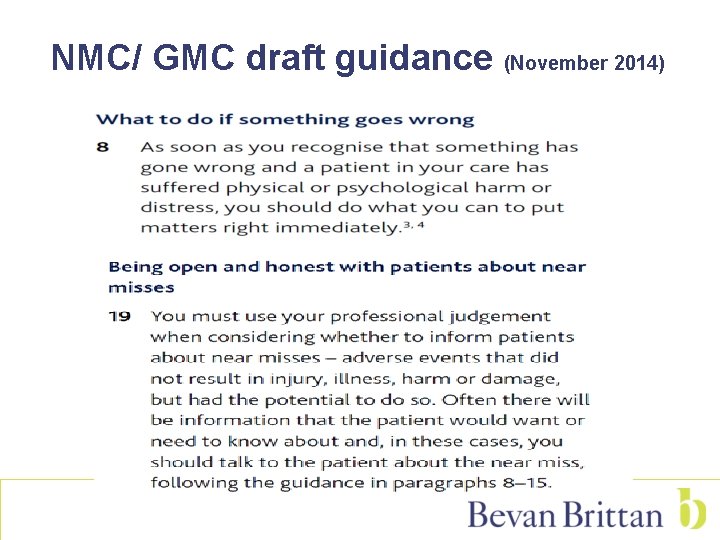
NMC/ GMC draft guidance (November 2014)
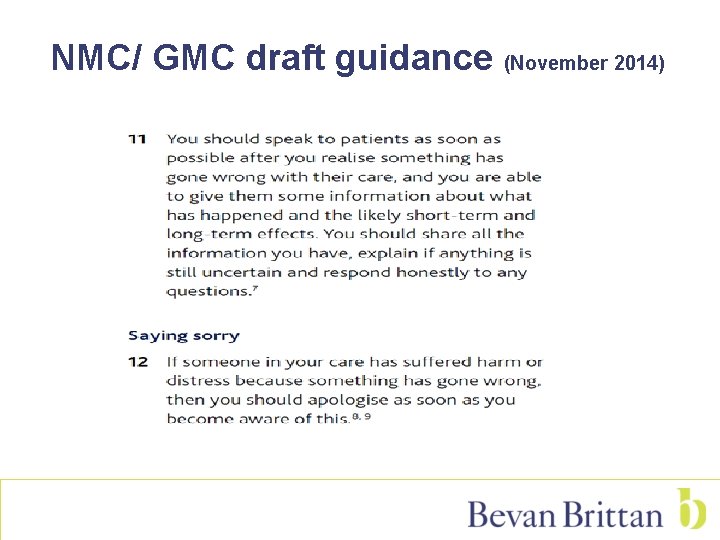
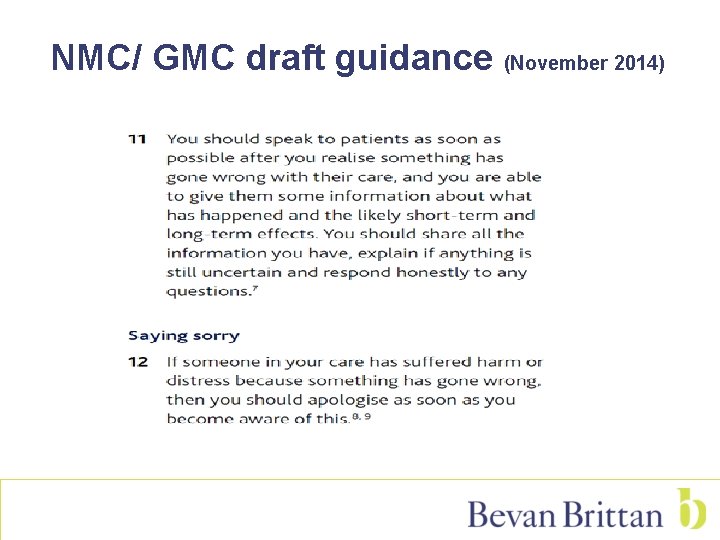
NMC/ GMC draft guidance (November 2014)
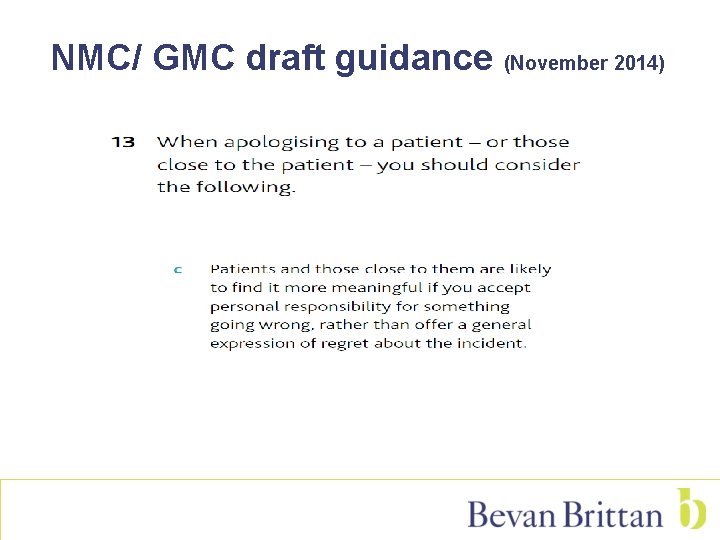
NMC/ GMC draft guidance (November 2014)
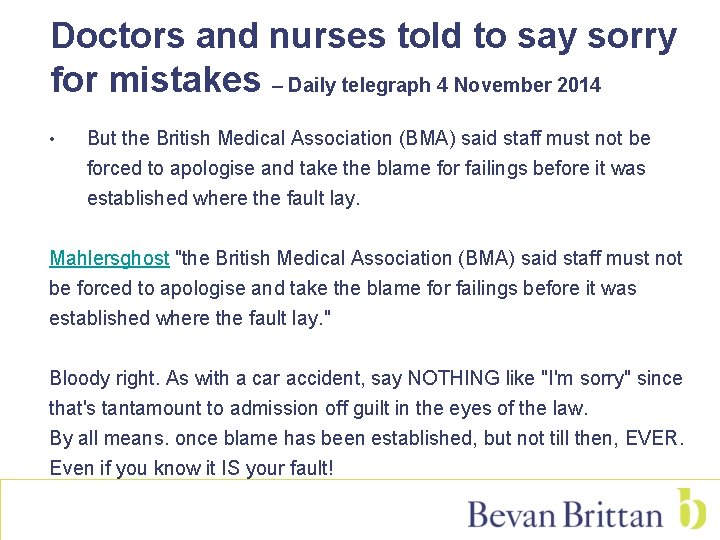
Doctors and nurses told to say sorry for mistakes – Daily telegraph 4 November 2014 • But the British Medical Association (BMA) said staff must not be forced to apologise and take the blame for failings before it was established where the fault lay. Mahlersghost "the British Medical Association (BMA) said staff must not be forced to apologise and take the blame for failings before it was established where the fault lay. " Bloody right. As with a car accident, say NOTHING like "I'm sorry" since that's tantamount to admission off guilt in the eyes of the law. By all means. once blame has been established, but not till then, EVER. Even if you know it IS your fault!
“The way you change the culture of the organisation is by having conversations that don’t result in action plans. We talk about it! … What I want the organisation to know is we’ve talked about it. Changing culture – it is about signs, symbols and iconography and it’s about lots of things. You change the culture by talking”. (Chief executive, case study respondent) – Nuffield Trust
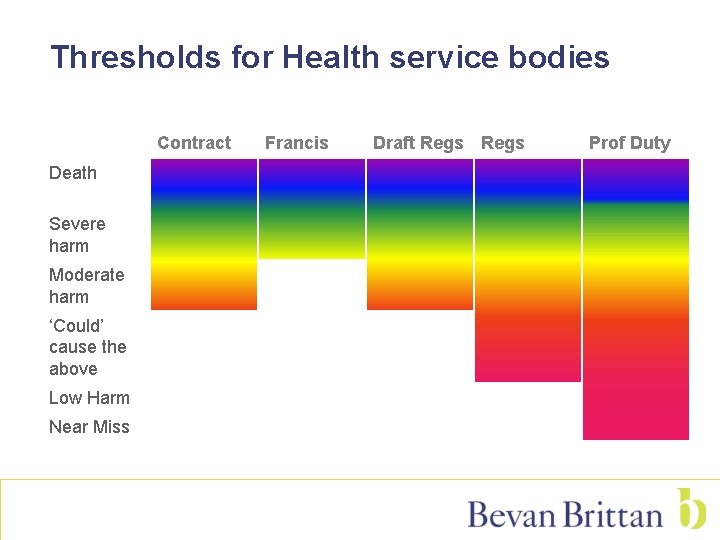
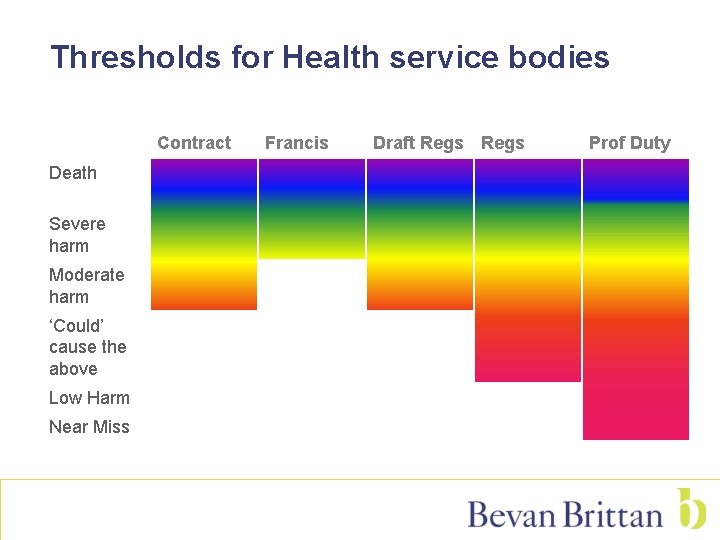
Thresholds for Health service bodies Contract Death Severe harm Moderate harm ‘Could’ cause the above Low Harm Near Miss Francis Draft Regs Prof Duty
CQC Inspection
Duty of candour – CQC guidance • We expect to mainly use the new regulations on candour to confirm or encourage good practice through the ratings we give, rather than to enforce them directly. • • • Criminal sanctions have a role to play – but by themselves they are unlikely to be the strongest driver for promoting a culture of openness in providers. We will … develop the processes that our inspectors will use to inspect and enforce the duty of candour … and ensure that our approach is proportionate, for example taking account of the degree of harm and the extent to which a breach was an act of omission as opposed to commission. We will not shy away from using the full weight of our powers, but we anticipate that this will be in cases where we have evidence of deliberate withholding or manipulation of information.

Scrutiny of candour • CQC intelligent monitoring system reviews: - staff surveys and whistleblowing to CQC - “Moderate” and “Serious” incidents reported to NRLS - incidents not reported as “Moderate” or “Serious”
Scrutiny of candour (CQC November 2014) • During our inspections we will sample the records of a number of notifiable safety incidents and determine whether: - The notification was given by a representative of the provider. - The relevant person received (to the best of the provider’s knowledge) a true account of the incident to date. - The provider explained what further enquiries were being made. - The provider included an apology (defined as an expression of sorrow or regret in respect of the incident). - The action taken was recorded in writing and kept securely.
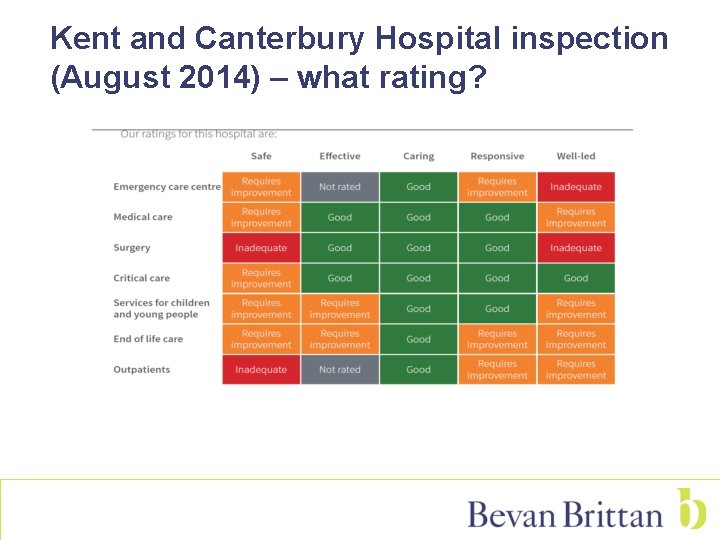
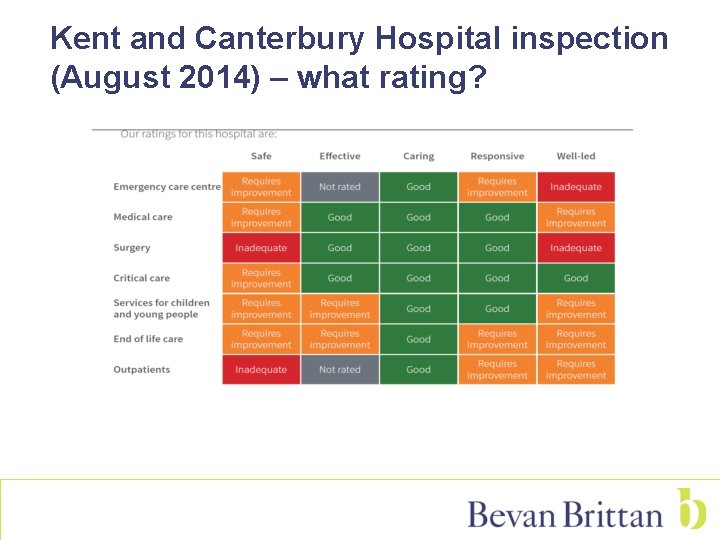
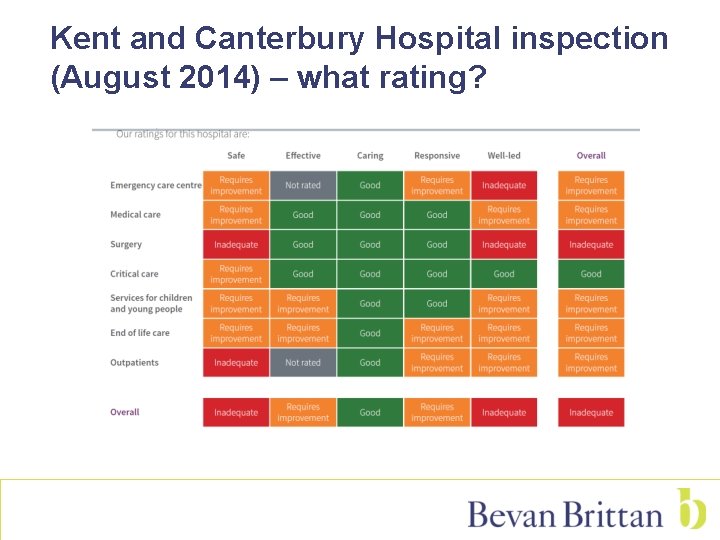
Kent and Canterbury Hospital inspection (August 2014) – what rating?
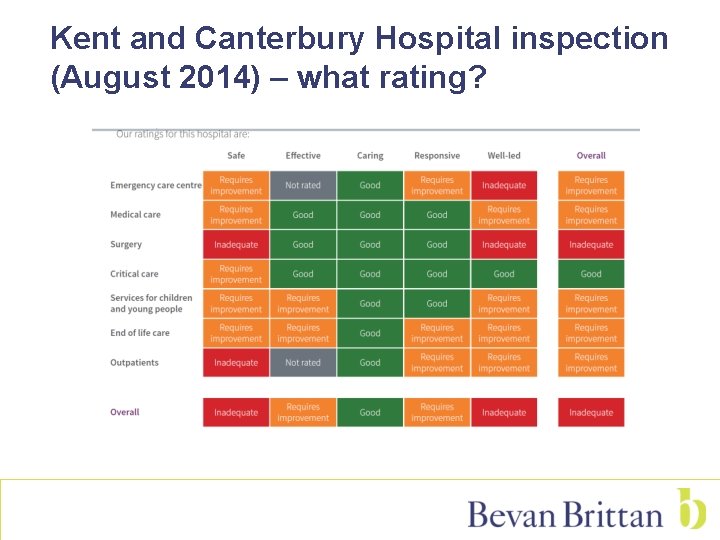
Kent and Canterbury Hospital inspection (August 2014) – what rating?
The Legal Implications of Apologies • An apology is not a legal admission of liability • Negligence - a determination for the court Admissions of fact may influence the question of liability at common law NHSLA’s position • • • “The NHS LA is not an insurer and we will never withhold cover for a claim because an apology or explanation has been given” - Saying Sorry leaflet http: //www. nhsla. com/Claims/Documents/Saying%20 Sorry%20%20 Leaflet. pdf

Concluding thoughts • • • Classification of incidents ? ‘candour’ field in Datix Policies – integrate Training/ candour champions? EVIDENCE candour Culture of organisation should encourage candour Tackle bullying or harassment undermining the duty of candour System in place to deal with breaches of a professional duty of candour by staff Sign up to Safety
• • 3 year plan Reduce avoidable harm by 50% Save 6, 000 lives If eligible, members will have the potential to access a one off payment to support implementation of their SIP plans. ie up to 10% of current contribution, paid in 2015/16.
Candour case studies

Is the duty of candour triggered? • where there has been a failure to implement a discharge care plan in time for discharge (due to an error)? • where a patient in hospital subject to delayed discharge contracts C. diff? • By a resuscitation events? • In relation to harm done to deceased patients (eg grazes to a deceased patient's body in the mortuary)?
Is the duty of candour triggered? • where a detention is unlawful based on a technicality (ie where there has been an administrative error on a form) but the individual would have been detained in any event? • where there has been inadvertent disclosure of information to the nearest relative, where the patient has expressly refused permission for information to be shared? • Cancellation of a patient’s hip-replacement surgery for two weeks due to decontamination issues in theatre? • Patient assaults healthcare assistant with a knife resulting in staff member suffering severe injury and patient prosecuted for GBH. A SIRI report is produced by the Trust.
Duty of candour – case study 1 • Julie is a 65 year old who suffers from dementia. She is currently detained under s. 2 MHA on Wood Ward. Other than this, Julie is fit and well. Julie has been assessed as a high risk of falls and she is meant to be receiving 1: 1 care. However, due to a bout of influenza, Wood Ward is short staffed and instead, Julie is receiving 15 minute observations. • Julie is found on the floor next to her bed by an HCA undertaking observations. Nursing staff attend and request a medical review. The junior doctor assesses Julie and determines that she has no obvious injuries and requests neurological observations for the next 2 hours. • Unfortunately, no neurological observations are undertaken. 3 days later Julie presents with increased confusion and dizzy spells. She has lost the use of her right arm. Investigations are undertaken and a CT scan shows that Julie has suffered a bleed on the brain consistent with a stroke. Sadly, it is too late for Julie to receive surgical treatment to reverse the symptoms of the stroke. • Due to her dementia, Julie lacks capacity to make decisions about her care and treatment. She has 2 daughters who visit her most days.
Duty of candour – case study 2 Bob suffers from treatment resistant schizophrenia. He lives in the community with his mother and is under a CTO. Bob is prescribed clozapine, an antipsychotic, which is delivered to Bob on a weekly basis by his CPN. Bob takes clozapine in a liquid format and the pharmacy dispense it in individual daily doses. When Jess, Bob's CPN visits, Bob appears to have deteriorated. His mother informs Jess that Bob stopped taking his clozapine 4 days ago. Jess speaks with the pharmacist over the telephone who explains that Bob's clozapine will need to be re-titrated from a much lower dose. Instead of returning the medication and re-issuing it in individual bottles, Jess and the pharmacist agree that the pharmacist will provide a re-titration chart, setting out the dosage that Bob needs to receive each day for the next 7 days. Jess arranges for a registered nurse to visit Bob each day to draw up the right dosage of his clozapine from his pre-existing supply.

Duty of candour – case study 2 (cont’d) Jess is not able to visit Bob for 3 days, but she goes to see him on day 4 of his re-titration. She reviews his medication chart and considers the re-titration chart. Jess realises that the nurses that have visited Bob over the past couple of days have miscalculated the dosage and that Bob has actually received a minor overdose. Jess undertakes a thorough physical examination and determines that Bob does not appear to be suffering from any side effects. As part of receiving clozapine, Bob is required to have routine blood tests, so Jess draws some blood to determine the levels of clozapine in his system. Given that Bob is not displaying any adverse side effects, Jess is reluctant to inform him of the overdose unless and until the blood test results show that he has a dangerous level in his system. One of Bob's presenting complaints of his schizophrenia is paranoia and Jess is very worried that if she advises him of the mistake, he will refuse to accept treatment at all.

Duty of candour – case study 3 Darren is referred to mental health services and offered an outpatient appointment for 1 September. Darren does not attend the appointment but subsequently contacts the Trust requesting a further appointment, which is arranged for 11 September. However, Darren commits suicide on 9 September.
Duty of candour – case study 4 Warren is referred to mental health services and offered an outpatient appointment for 1 September. Warren's appointment on 1 September is subsequently cancelled by the Trust, due to a shortage of staff, and rearranged for 11 September. However, Warren commits suicide on 9 September.

Duty of candour – case study 5 A Community Intervention Crisis Team operates flexible appointments when they plan to see patients at home during a particular 'window' within the day. However, the Crisis Team member gets held up dealing with Tina so that, when they arrive at Stephanie's house just outside of the allotted time, Stephanie is no longer there and cannot be contacted. Is the duty of candour triggered?

Any Questions? Contact: Carlton. sadler@bevanbrittan. com t: 0870 194 1633


Our promises to clients • To understand you • To provide solutions that contribute to your success • To give you fair pricing and clarity on costs • To give you the right team • To communicate clearly • To care about our relationship with you
 What is duty of candour
What is duty of candour Duty of candour
Duty of candour What is duty of candour
What is duty of candour Process governance
Process governance Tasmin v barts health nhs trust
Tasmin v barts health nhs trust Duty of trust and confidence cipd
Duty of trust and confidence cipd Portsmouth trust values
Portsmouth trust values Uhcw library
Uhcw library Simon sheppard nhs birmingham
Simon sheppard nhs birmingham Portsmouth hospitals nhs trust jobs
Portsmouth hospitals nhs trust jobs Airedale nhs trust v bland
Airedale nhs trust v bland Northern trust charitable trust
Northern trust charitable trust Keshav sita memorial foundation trust
Keshav sita memorial foundation trust Shallow pad foundation
Shallow pad foundation Composition of urine slideshare
Composition of urine slideshare Recovery college lincoln
Recovery college lincoln Southern connecticut state university criminal justice
Southern connecticut state university criminal justice Dr ysr aarogyasri health care trust
Dr ysr aarogyasri health care trust Acec life health trust
Acec life health trust Helene fuld health trust
Helene fuld health trust Electbenefits.com/nhs
Electbenefits.com/nhs Teachers health trust allegiance
Teachers health trust allegiance National general 888-781-0585 nc
National general 888-781-0585 nc Public health foundation enterprises inc
Public health foundation enterprises inc Kentucky physicians health foundation
Kentucky physicians health foundation Kansas health foundation
Kansas health foundation Far 117 table c
Far 117 table c Countervailing duty
Countervailing duty Duty to accommodate definition
Duty to accommodate definition The duty of writers
The duty of writers Duty of care certificate
Duty of care certificate Swingline 800
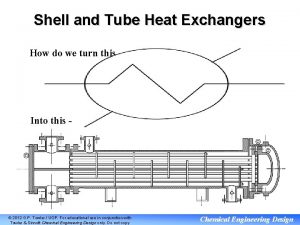
Swingline 800 Heat exchanger duty
Heat exchanger duty Responsibility in relationships
Responsibility in relationships Duty and responsibility
Duty and responsibility Peter oliphant
Peter oliphant Philmont treks 2020 itinerary guide
Philmont treks 2020 itinerary guide Off duty misconduct
Off duty misconduct Duty to god activities
Duty to god activities Stamp duty(amendment) proclamation no. 612/2008
Stamp duty(amendment) proclamation no. 612/2008 Kind of an ode to duty
Kind of an ode to duty Introduction to hand tools
Introduction to hand tools Icegate e payment
Icegate e payment Afternoon duty
Afternoon duty Basic front office operations
Basic front office operations What is the duty of commissioner
What is the duty of commissioner Assessment in customs
Assessment in customs Types of custom duty
Types of custom duty Responsibility vs duty
Responsibility vs duty Heavy duty truck axle repair
Heavy duty truck axle repair Philmont itineraries
Philmont itineraries Philmont duty roster
Philmont duty roster Custom basic
Custom basic What duty was mary warren performing in the court
What duty was mary warren performing in the court Types of custom duty
Types of custom duty Square of chalk makes temporary marks on fabric
Square of chalk makes temporary marks on fabric Yania v. bigan
Yania v. bigan Oors nycdoe
Oors nycdoe New innovations duty hours
New innovations duty hours Malik is the gatekeeper of heaven
Malik is the gatekeeper of heaven Irregularities in the performance of duty
Irregularities in the performance of duty Yurtdışına çıkmadan duty free
Yurtdışına çıkmadan duty free On my honor scout
On my honor scout Radial flow pumps
Radial flow pumps Senior scout motto
Senior scout motto Weekend duty
Weekend duty Heartfit for duty
Heartfit for duty Air brake chamber cutaway
Air brake chamber cutaway Training for election duty
Training for election duty Care certificate 10
Care certificate 10 Tac duty manager
Tac duty manager On my honor i will do my duty
On my honor i will do my duty