Consent in light of the Montgomery ruling Roger


![• Tasmin v Barts Health NHS Trust [2015] EWHC 3135 • CP following • Tasmin v Barts Health NHS Trust [2015] EWHC 3135 • CP following](https://slidetodoc.com/presentation_image_h2/64819eaa3543e98f628ae460ac96a3cc/image-21.jpg)
![• Mrs A v East Kent Hospitals University NHS Foundation Trust [2015] EWHC • Mrs A v East Kent Hospitals University NHS Foundation Trust [2015] EWHC](https://slidetodoc.com/presentation_image_h2/64819eaa3543e98f628ae460ac96a3cc/image-22.jpg)
![• Reid, E [2015] 'Montgomery v Lanarkshire Health Board and the Rights of • Reid, E [2015] 'Montgomery v Lanarkshire Health Board and the Rights of](https://slidetodoc.com/presentation_image_h2/64819eaa3543e98f628ae460ac96a3cc/image-23.jpg)
- Slides: 24
Consent in light of the Montgomery ruling Roger Smyth Department of Psychological Medicine Royal Infirmary of Edinburgh
The role of consent
• • Clinical function: • establish collaborative relationship with the patient • inform the patient of the nature, purpose and risks of the procedure Legal function: • removes the legal barriers which exist to protect persons from interference with their personal autonomy and physical integrity - i. e. the criminal offences of battery and assault; the civil offence of trespass to the person; or civil tort (alleging negligence) - subject to “de minimis non curat lex” - “Every human being of adult years and sound mind has a right to determine what shall be done with his own body; and a surgeon who performs an operation without the patient’s consent commits an assault”. Schloendorff v Society of New York Hospital 105 NE 92 (NY, 1914) - "In general it is a criminal and tortious assault to perform physically invasive medical treatment, however minimal the invasion might be, without the patient's consent”. Butler-Sloss, LJ, Re MB [1997] 2 FLR 426
Valid consent

• To be valid consent must be: • voluntary • informed • given by a competent adult or ‘mature minor’
Limitations of consent
• Limited scope • only pertains to those treatments to which the consent was specifically given - • • (unless the additional action or treatment can be justified under the doctrine of necessity) acting beyond the consent risks action for assault and battery as if no consent had existed Williamson v East London and City Health Authority (1988) 41 BMLR 85 No obligation to treat • “it creates no obligation to treat. It is merely a key which unlocks a door. " Lord Donaldson MR, Re R [1992] Fam 11 - legal analogies: “key” or “flak-jacket”
Capacity to consent & refuse
• • Test for competence in relation to consent was definitively set out in the case of Re C (adult: refusal of medical treatment) [1994] 1 All ER 819 • court had to determine whether a prisoner with paranoid schizophrenia, whose leg had become infected with gangrene, was competent to refuse consent to the proposed amputation of his leg • established three steps, or criteria, in the form of a 'test' of competence that future courts have interpreted, and continue to follow: - 1) does the individual have the ability to comprehend, and retain, the information s/he is given about the treatment (its nature, purposes, and consequences)? - 2) does s/he have the ability to believe that information? and - 3) does s/he have the ability to weigh the information in the balance, so as to arrive at a choice? Test now established in statute • Mental Capacity Act 2005, s. 3(1) • Adults with Incapacity (Scotland) Act 2000, s. 1(6) • Mental Capacity Act (Northern Ireland) 2016, s. 4
• Rationale for choice • choices need be neither reasonable nor rational - • • “If the doctor … advises the patient to submit to the operation, the patient is entitled to reject that advice for reasons which are rational or irrational or for no reason”. Lord Templeman, Sidaway [1985] 1 AC 871 Presumption of capacity • common law principle now affirmed by statute • legal burden of proving that the patient is incompetent rests on those seeking to override the patient's wishes • presumed to be retained in relation to a decision even if clearly absent in other areas Undue influence • in certain instances the law recognizes that a person's free will may be so influenced by another that agreements made by that person should be set aside - e. g. Re T (adult: refusal of medical treatment) [1992] 4 All ER 649
‘Prudent doctor’ to ‘prudent patient’
• Negligence • the defendant owed a duty of care to that patient • the defendant was in breach of that duty • that the breach of the duty of care caused the damage complained of by the plaintiff
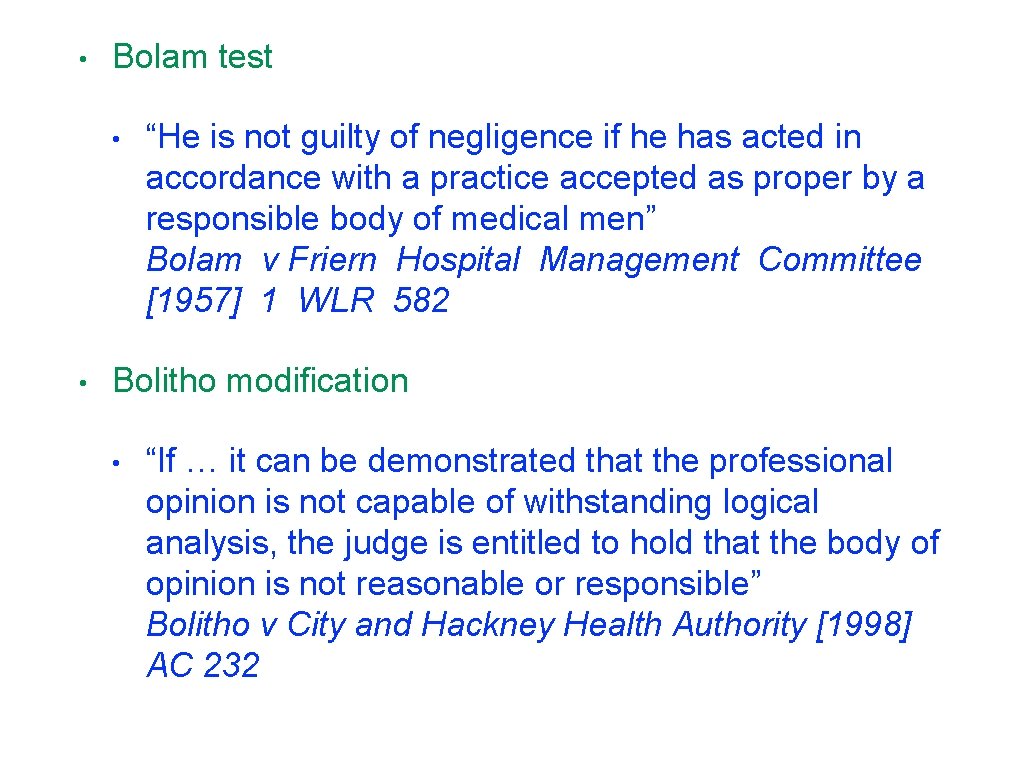
• Bolam test • • “He is not guilty of negligence if he has acted in accordance with a practice accepted as proper by a responsible body of medical men” Bolam v Friern Hospital Management Committee [1957] 1 WLR 582 Bolitho modification • “If … it can be demonstrated that the professional opinion is not capable of withstanding logical analysis, the judge is entitled to hold that the body of opinion is not reasonable or responsible” Bolitho v City and Hackney Health Authority [1998] AC 232
• Sidaway case • • “consent does not require an elaborate explanation of remote side effects”; “when questioned specifically by a patient about risks, it is the doctor’s duty to answer truthfully and as fully as the questioner requires” Sidaway v Board of Governors of the Bethlem Royal Hospital and the Maudsley Hospital [1985] AC 87 Sidaway dissent (Lord Scarman) if the patient: • • - suffers damage as a result of an undisclosed risk - which would have been disclosed by a doctor exercising reasonable care to respect her patient’s right to decide whether to incur the risk - the patient would have avoided the injury if the risk had been disclosed then the patient will in principle have a cause of action based on negligence
• Pearce case • • “if there is a significant risk which would affect the judgment of a reasonable patient, then in the normal course it is the responsibility of a doctor to inform the patient of that significant risk, if the information is needed so that the patient can determine for him or herself as to what course he or she should adopt” Pearce v United Bristol Healthcare NHS Trust [1999] ECC 167 Rogers case (Australia) • “a risk is material if, in the circumstances of the particular case, a reasonable person in the patient's position, if warned of the risk, would be likely to attach significance to it or if the medical practitioner is or should reasonably be aware that the particular patient, if warned of the risk, would be likely to attach significance to it” Rogers v Whitaker (1992) 175 CLR 479

• Montgomery case (1) • Shoulder dystocia during vaginal delivery • Subsequent cerebral palsy in infant • Initial case alleged: • - failure to obtain/act on CTG - failure to warn of risks Case failed at original trial - “In order for a duty to explain the risks to arise, Mrs Montgomery would have had to have ‘raised questions of specific risks’ ”
• ‘Good Medical Practice’ GMC 2013 • • “Work in partnership with patients. Listen to, and respond to, their concerns and preference s. Give patients the information they want or need in a way they can understand. Respect patients’ right to reach decisions with you about their treatment and care” ‘Consent: patients and doctors making decisions together’ GMC 2008 • “The doctor explains the options to the patient, setting out the potential benefits, risks, burdens and side effects of each option, including the option to have no treatment. The doctor may recommend a particular option which they believe to be best for the patient, but they must not put pressure on the patient to accept their advice. The patient weighs up the potential benefits, risks and burdens of the various options as well as any nonclinical issues that are relevant to them. The patient decides whether to accept any of the options and, if so, which one”
• • Montgomery case (2) • Case succeeded at Supreme Court Montgomery V Lanarkshire Health Board [2015] 2 WLR 768 • Damages of £ 5. 25 M Established new test: • An adult person of sound mind is entitled to decide which, if any, of the available forms of treatment to undergo, and his/her consent must be obtained before treatment interfering with his/her bodily integrity is undertaken
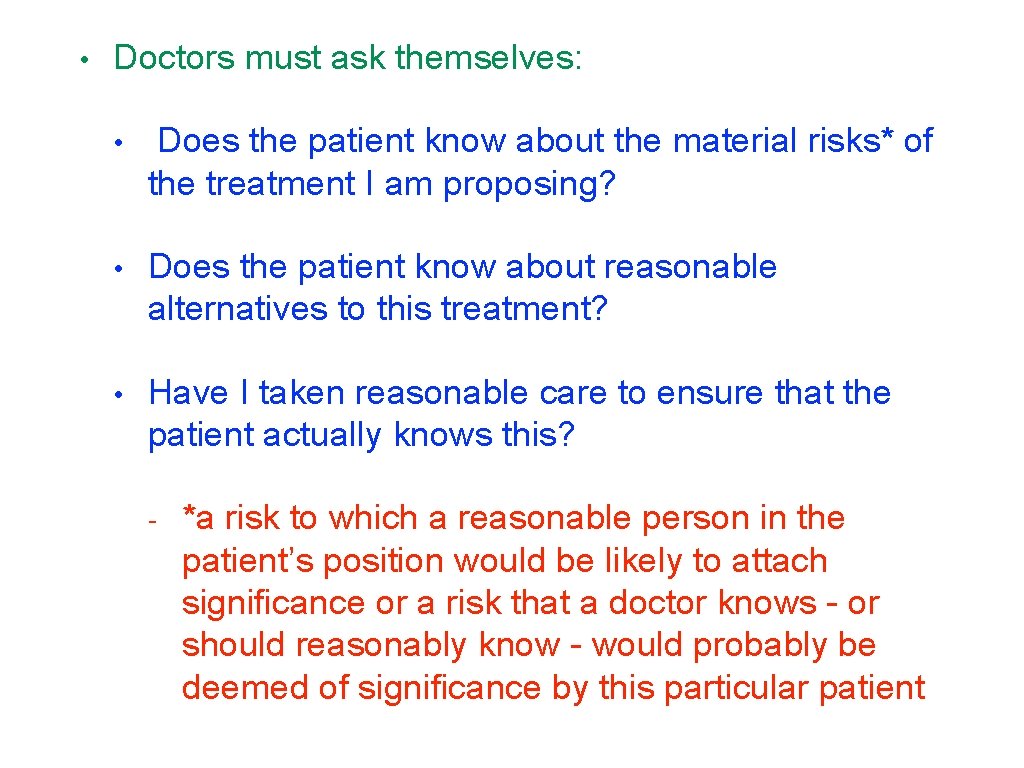
• Doctors must ask themselves: • Does the patient know about the material risks* of the treatment I am proposing? • Does the patient know about reasonable alternatives to this treatment? • Have I taken reasonable care to ensure that the patient actually knows this? - *a risk to which a reasonable person in the patient’s position would be likely to attach significance or a risk that a doctor knows - or should reasonably know - would probably be deemed of significance by this particular patient
Cases since Montgomery
![Tasmin v Barts Health NHS Trust 2015 EWHC 3135 CP following • Tasmin v Barts Health NHS Trust [2015] EWHC 3135 • CP following](https://slidetodoc.com/presentation_image_h2/64819eaa3543e98f628ae460ac96a3cc/image-21.jpg)
• Tasmin v Barts Health NHS Trust [2015] EWHC 3135 • CP following intrapartum hypoxia • “a risk of 1: 1, 000 is an immaterial risk for the purposes of paragraph 87 of Montgomery. The Supreme Court eschewed characterising the risk in percentage terms, but it was doing so in the context of defining the borderline between materiality and immateriality. Here, I am quite satisfied that the relevant risk was so low that it was below that borderline. I am not to be understood as saying exactly where threshold should be defined”
![Mrs A v East Kent Hospitals University NHS Foundation Trust 2015 EWHC • Mrs A v East Kent Hospitals University NHS Foundation Trust [2015] EWHC](https://slidetodoc.com/presentation_image_h2/64819eaa3543e98f628ae460ac96a3cc/image-22.jpg)
• Mrs A v East Kent Hospitals University NHS Foundation Trust [2015] EWHC 1038 (QB) • birth of a child with chromosomal abnormality • claimant argued that she would have had a termination if warned of risk • “in my judgment the decision in Montgomery affirms the importance of patient autonomy, and the proper practice set out in the GMC Guidance and the proper approach set out in Pearce and Wyatt. It is not authority for the proposition that medical practitioners need to warn about risks which are theoretical and not material”
![Reid E 2015 Montgomery v Lanarkshire Health Board and the Rights of • Reid, E [2015] 'Montgomery v Lanarkshire Health Board and the Rights of](https://slidetodoc.com/presentation_image_h2/64819eaa3543e98f628ae460ac96a3cc/image-23.jpg)
• Reid, E [2015] 'Montgomery v Lanarkshire Health Board and the Rights of the Reasonable Patient’ Edinburgh Law Review 19(3) 360 • “for the time being, however, all medical staff advising patients need to be aware that there is no simple rule on a specific level of risk that triggers the requirement to disclose … • … in judging which information to disclose and which to withhold they must make comprehensive efforts to ascertain the patient’s perspective on what they want of their treatment – and, of course, to document that they have done so”