Delirium Nancy Weintraub MD FACP Professor of Medicine
Delirium Nancy Weintraub, MD, FACP Professor of Medicine, UCLA Director, UCLA Geriatric Medicine Fellowship Director, VA Special Advanced Fellowship in Geriatrics at GLA VA
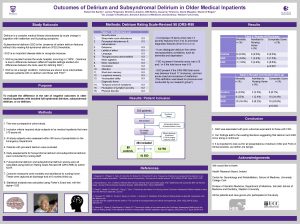
Definition Acute alteration of consciousness Inattention Can look like dementia Reversible More common in patients with dementia Lack of brain reserve during stress
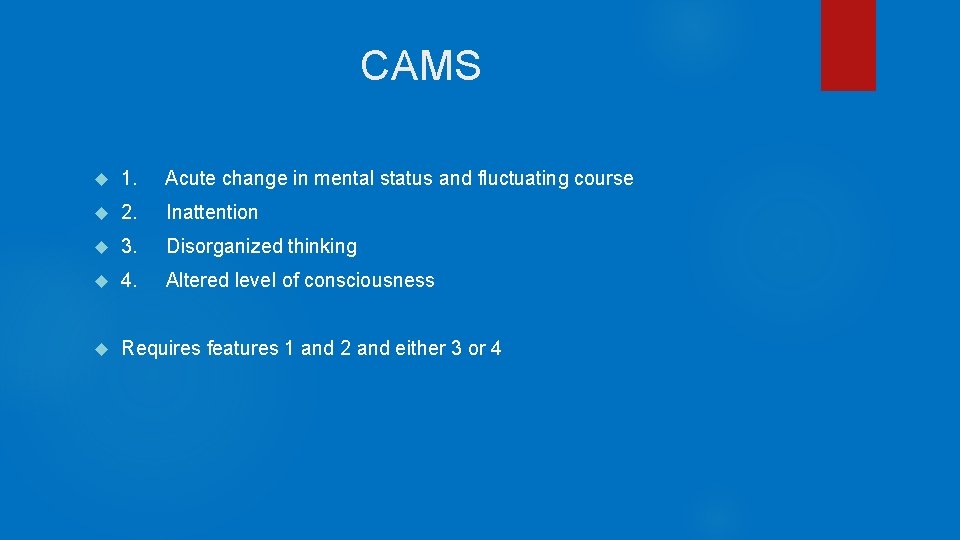
CAMS 1. Acute change in mental status and fluctuating course 2. Inattention 3. Disorganized thinking 4. Altered level of consciousness Requires features 1 and 2 and either 3 or 4
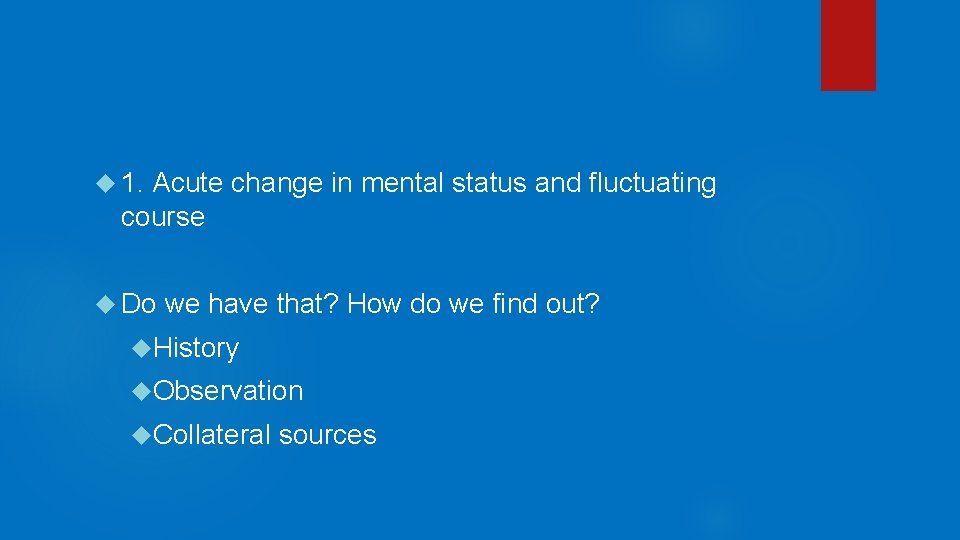
1. Acute change in mental status and fluctuating course Do we have that? How do we find out? History Observation Collateral sources
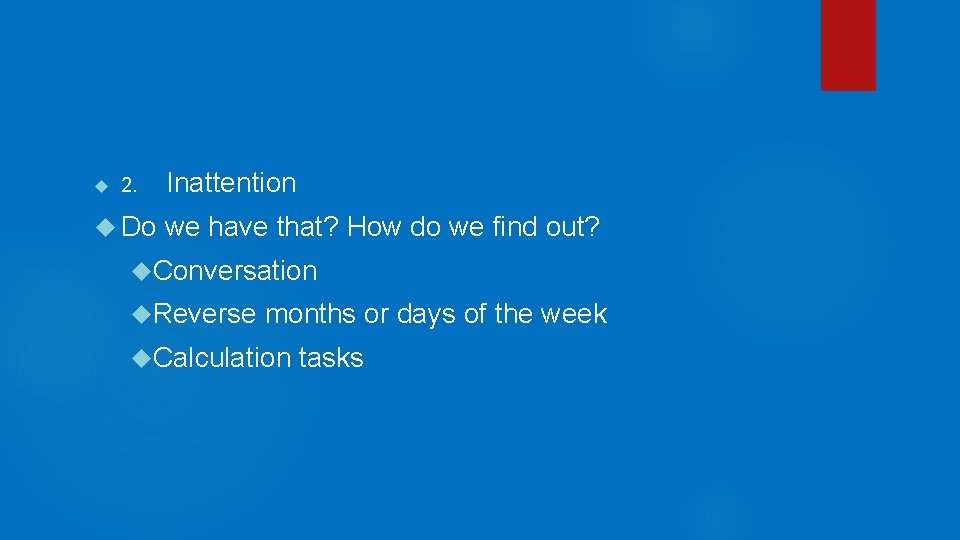
2. Do Inattention we have that? How do we find out? Conversation Reverse months or days of the week Calculation tasks
3. Disorganized thinking Conversation Reasoning questions
Altered level of consciousness Somnolence Agitation
Consequences of Delirium Persistent or early cognitive decline Prolonged hospitalization Increased risk of death Increased risk of institutionalization
Some Causes Medications added (especially anticholinergics or sedatives) or subtracted Metabolic derangements Infections Sensory deprivation Restraints Anesthesia Pain Lack of Sleep
Preventive Strategies Mobility Light in daytime, quiet and dark at night Avoid known anticholinergic drugs Frequent orientation Avoid restraints, catheters, tubes, etc. Friends and family present
Dealing with Delirium Attempt to remove all potentially causative agents/environmental factors, e. g. Remove restraints Remove as many tubes as possible Remove potentially contributing medications Treat pain Resume necessary medications inadvertently left out Treat infections Light in day, quiet and dark at night Enlist family and friends Get patient out of bed
Dealing with Delirium Last resort: low dose antipsychotics Only if safety is at risk Never in hypoactive delirium
Delirium may not clear until patient returns to familiar environment
- Slides: 13