Degenerative scoliosis Considerations and indications for surgical treatment

- Slides: 34
Degenerative scoliosis Considerations and indications for surgical treatment Presenter’s name Arial 24 pt Meeting Arial 24 pt Presenter’s title Arial 20 pt City, Month, Year Arial 20 pt
Learning outcomes • Outline the treatment principles and options in relation to adult or degenerative spinal deformity • Recognize associated comorbidities and their influence on the outcome of surgery • Outline the principles in relation to restoration and maintenance of spinal balance • Perform assessment in relation to restoration and maintenance of spinal balance
Outline • Etiology • Relevant history • Significant examination findings • Indications for and interpretation of relevant investigations • Indications for surgery and surgical principles • Achieving spinal balance • Relevant complications
Etiology • Idiopathic scoliosis progressing into adulthood • Superimposed degeneration, usually worse in the concavity, leads to progression of deformity (typically over 50 years of age) • Usually, patients who have not had scoliosis as an adolescent develop a lumbar or thoracolumbar deformity due to symmetrical degeneration in later life
Natural history • Progression influenced by: • Magnitude of deformity • Spinal balance • Bone quality • Comorbidities • General fitness and muscle tone
Clinically (1/3) • Patient is usually over 60 years old • Presents with symptoms related to: • Degenerative disease (discs and/or facet joints) • Canal stenosis • Foraminal compromise • Spinal imbalance and muscle fatigue
Clinically (2/3) • Associated comorbidities • Hip, knee, and sacroiliac joint degeneration • Cardiac disease (BP, IHD, arrhythmias, anticoagulant use) • Respiratory disease • Diabetes • Smoking • Osteoporosis
Clinically (3/3) • Examination • Assess spinal balance and gait • Sagittal imbalance and loss of lumbar lordosis a common finding in patients presenting for surgical treatment • Neurological examination is often normal in the absence of nerve root compression (similar to lumbar canal stenosis patients) • Important to assess general medical condition of patient
Diagnosis • Identify origin of pain to determine most appropriate treatment
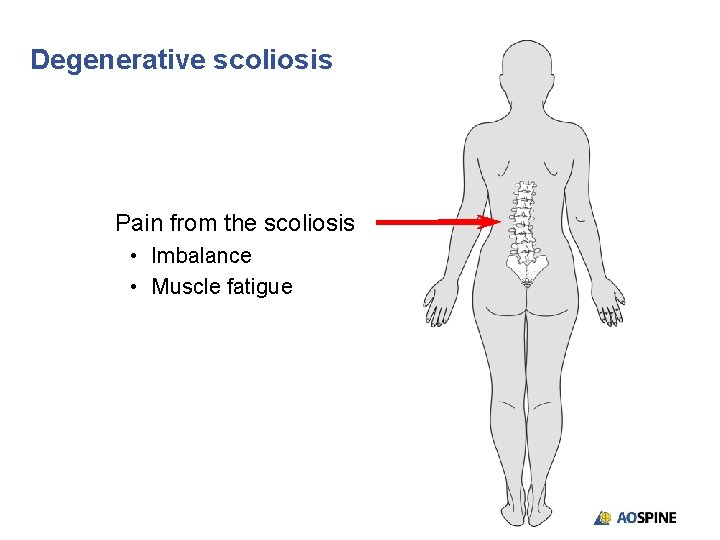
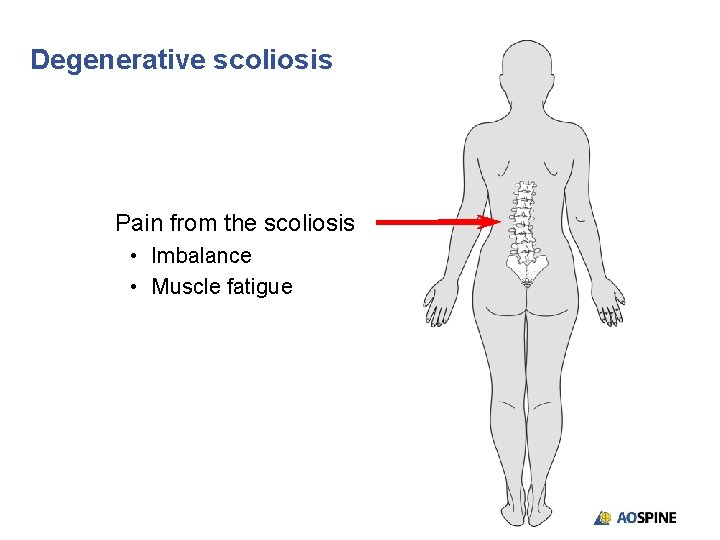
Degenerative scoliosis Pain from the scoliosis • Imbalance • Muscle fatigue
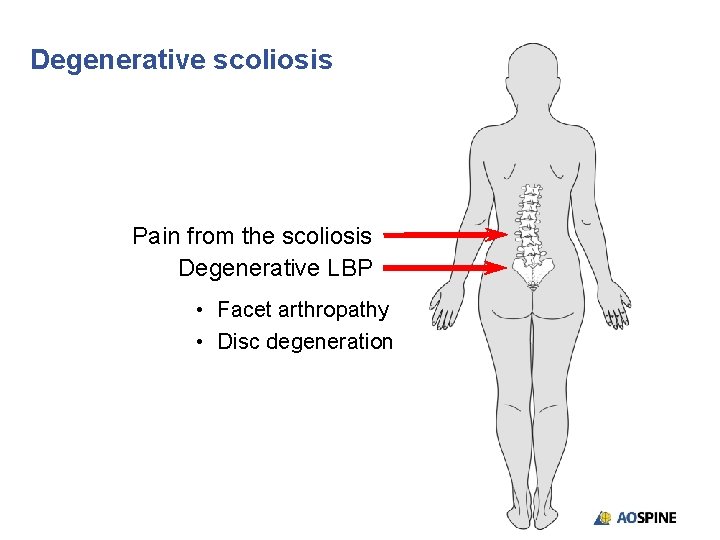
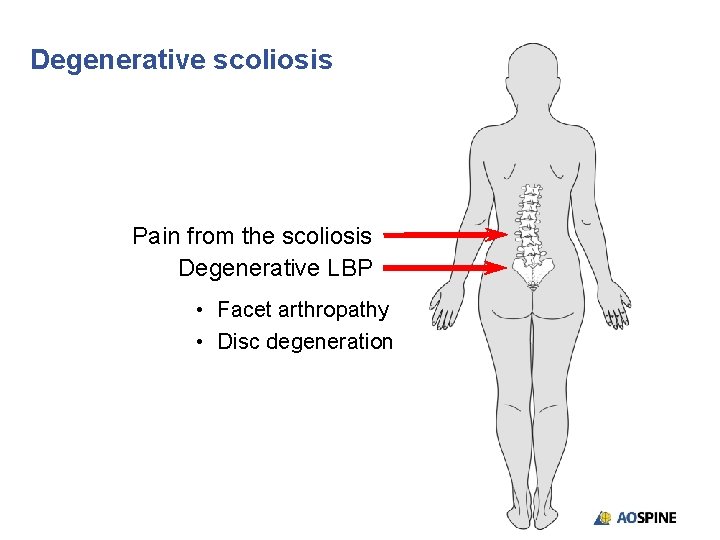
Degenerative scoliosis Pain from the scoliosis Degenerative LBP • Facet arthropathy • Disc degeneration
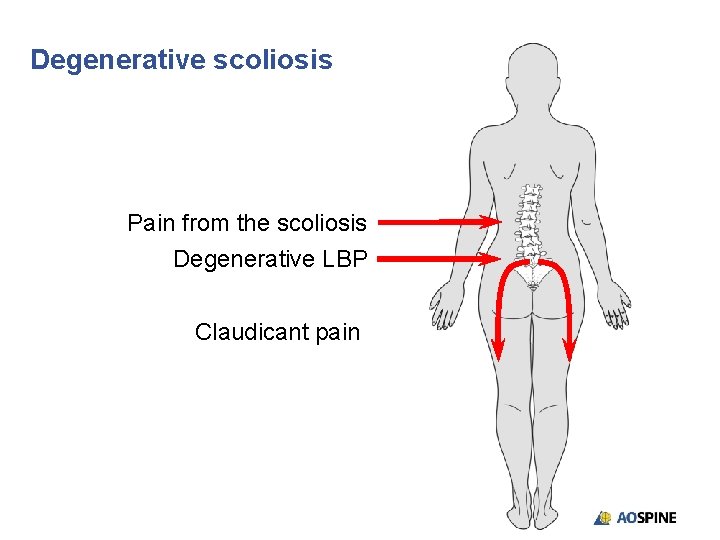
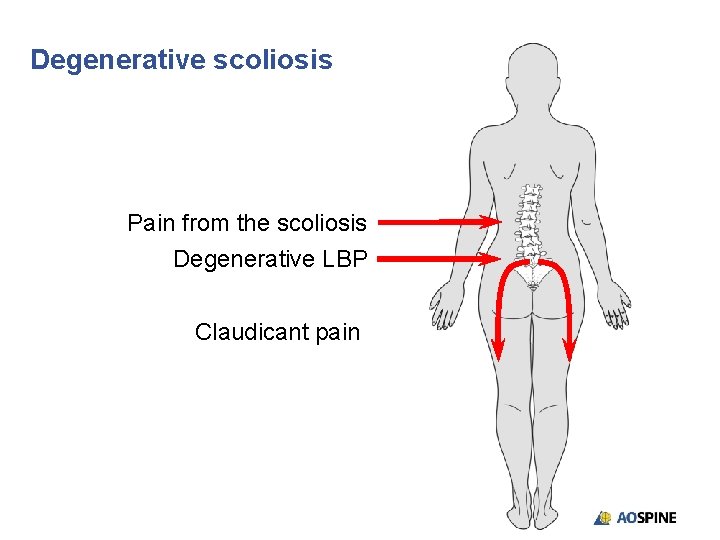
Degenerative scoliosis Pain from the scoliosis Degenerative LBP Claudicant pain
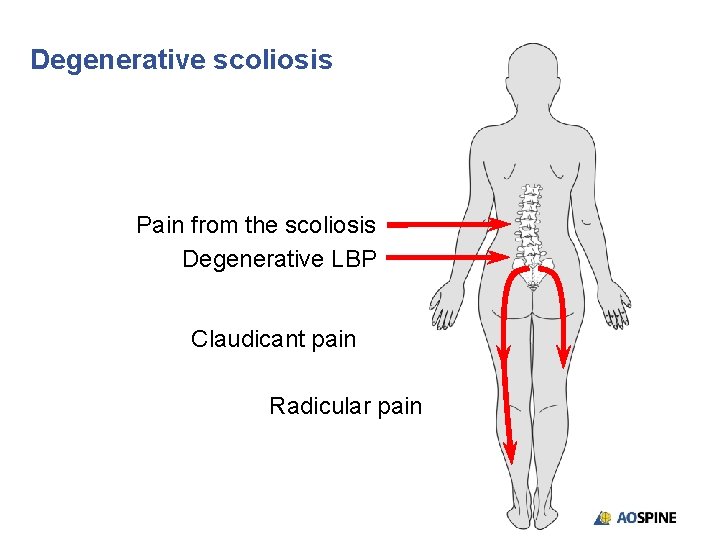
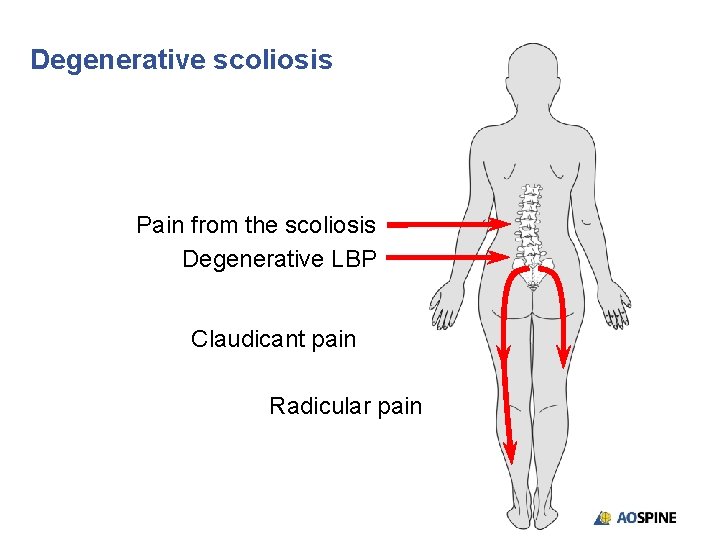
Degenerative scoliosis Pain from the scoliosis Degenerative LBP Claudicant pain Radicular pain
Diagnosis • Imaging should include: • Long, standing AP and lateral x-rays • MRI or CT myelography (if unable to have MRI) • Bending or traction x-rays may be indicated to assess flexibility of deformity
Red flags • Abnormal neurological findings (radicular or myelopathic) • Symptoms of neoplastic disease (nocturnal pain, constitutional upset, weight loss, etc) • Presence of a pathological fracture
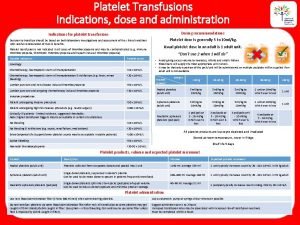
Treatment (1/4) • Physical therapy and core stabilization • Hydrotherapy and regular swimming often useful in patients with this condition • Epidural or foraminal injections may provide relief of claudicant or radicular symptoms
Treatment (2/4) • Surgical intervention is usually major in this patient group • Localized foraminal or canal decompression may be tried for localized symptoms of neural compromise, but often develop recurrent symptoms and may aggravate back pain or lead to accelerated curve progression • Important for the patient to have appropriate expectations regarding the outcome of any surgery, which usually involves extensive fusion, often to the pelvis
Treatment (3/4) • Evaluate the risks and benefits of surgery in relation to: • Nature of the symptoms • Patient’s expectations • Chance of success • Risk of significant complications
Treatment (4/4) • Surgical principles • Achieve and maintain spinal balance • May need osteotomy to achieve this and important to consider pelvic parameters
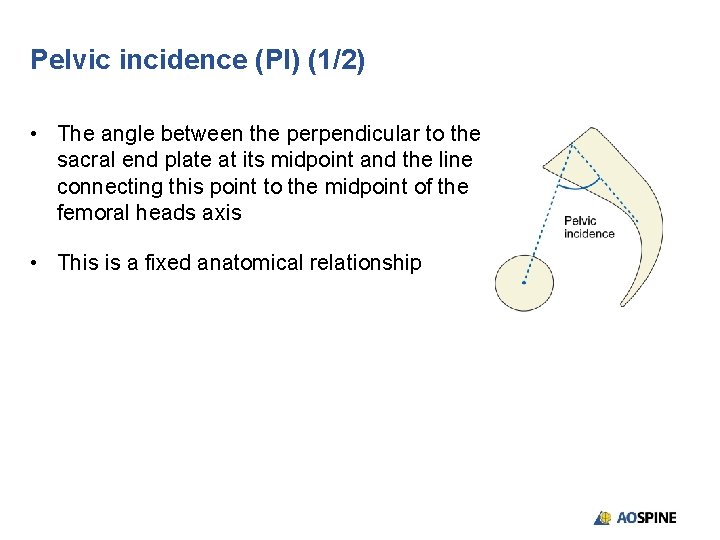
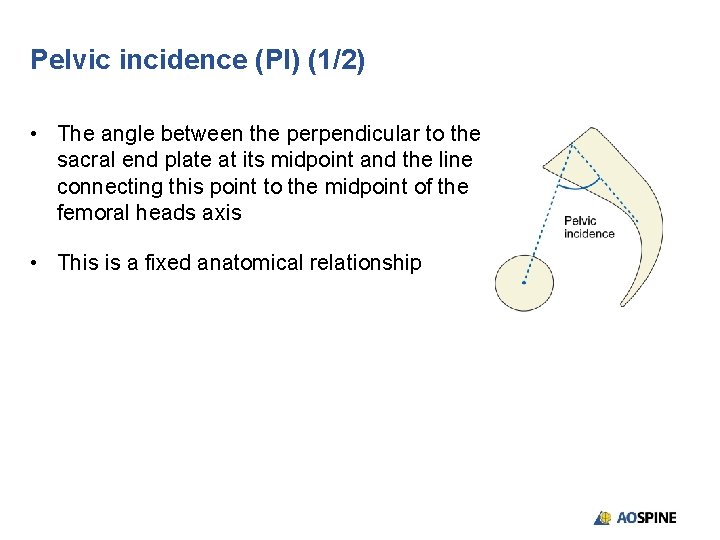
Pelvic incidence (PI) (1/2) • The angle between the perpendicular to the sacral end plate at its midpoint and the line connecting this point to the midpoint of the femoral heads axis • This is a fixed anatomical relationship
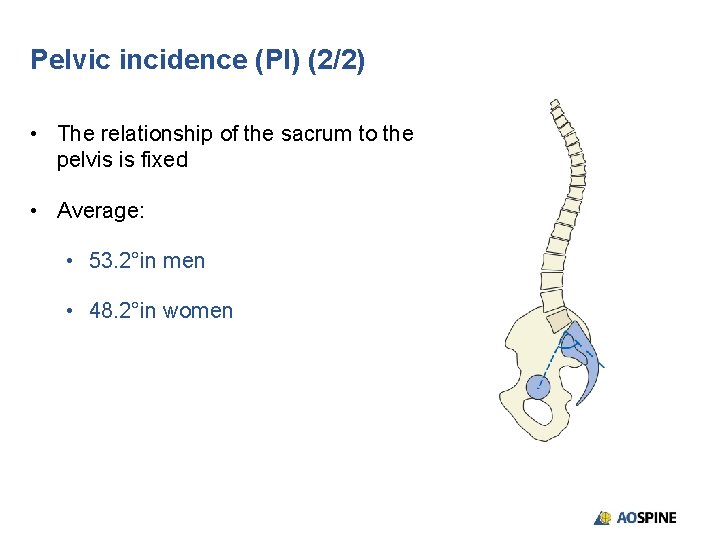
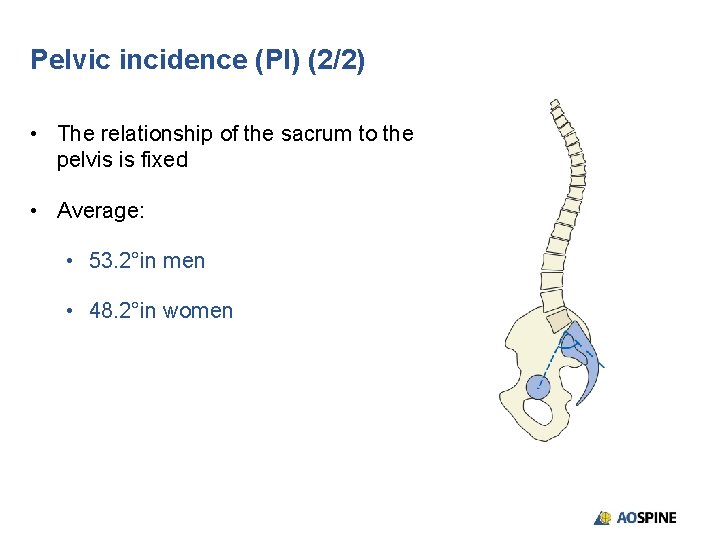
Pelvic incidence (PI) (2/2) • The relationship of the sacrum to the pelvis is fixed • Average: • 53. 2°in men • 48. 2°in women
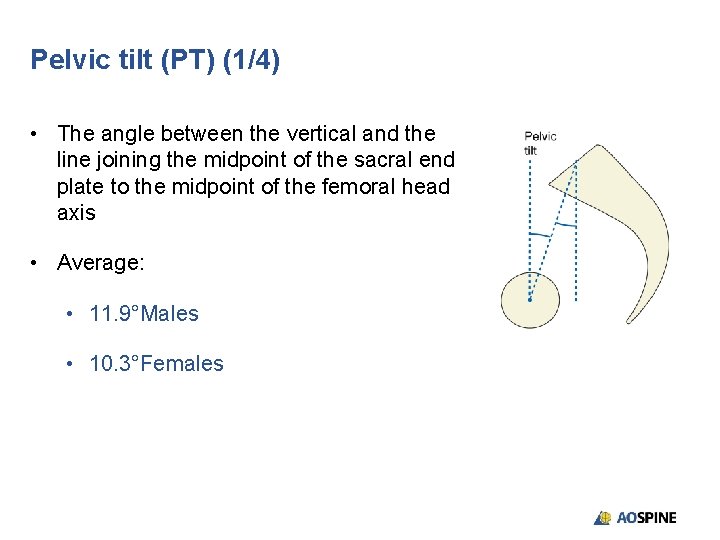
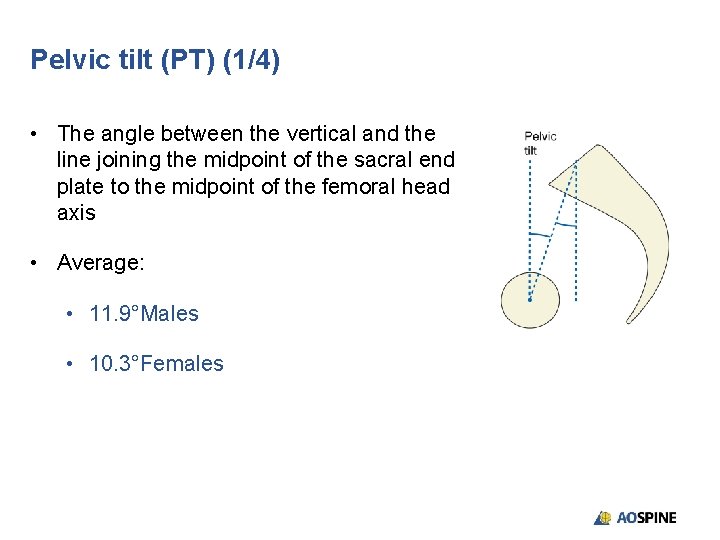
Pelvic tilt (PT) (1/4) • The angle between the vertical and the line joining the midpoint of the sacral end plate to the midpoint of the femoral head axis • Average: • 11. 9°Males • 10. 3°Females
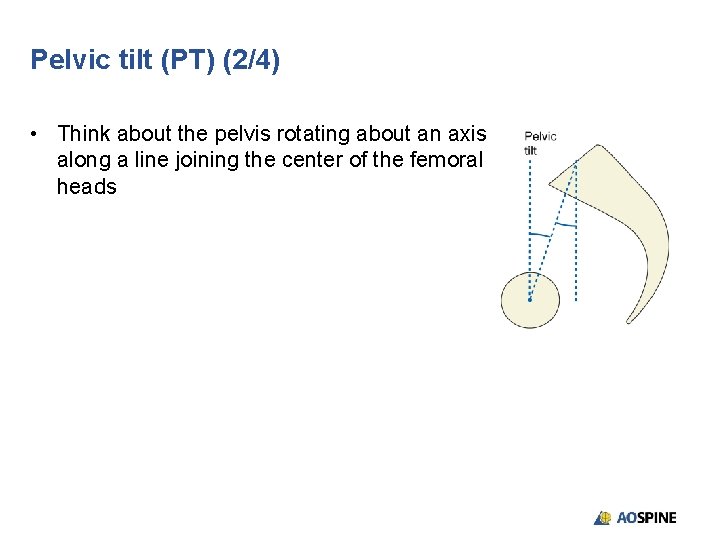
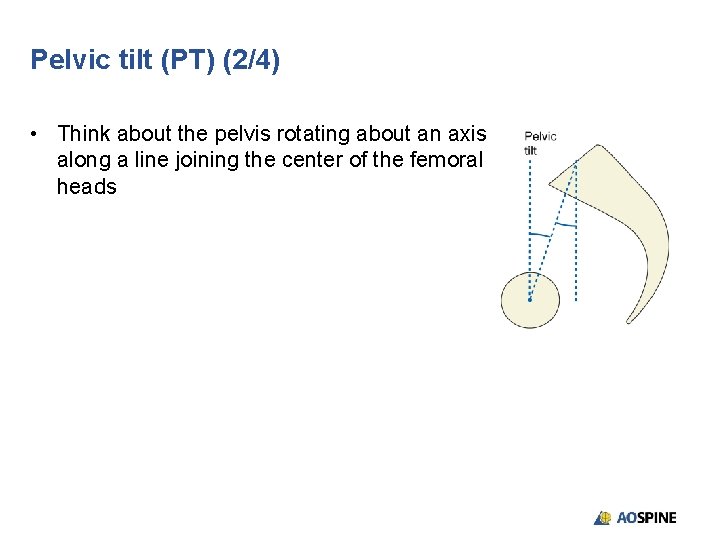
Pelvic tilt (PT) (2/4) • Think about the pelvis rotating about an axis along a line joining the center of the femoral heads
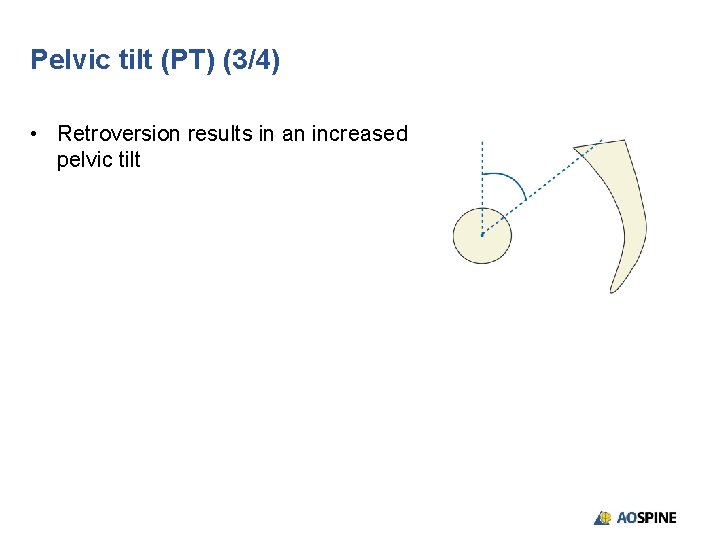
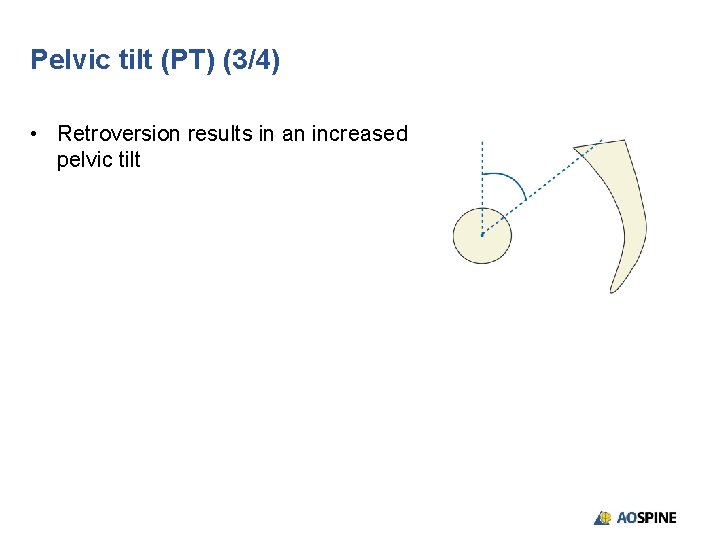
Pelvic tilt (PT) (3/4) • Retroversion results in an increased pelvic tilt
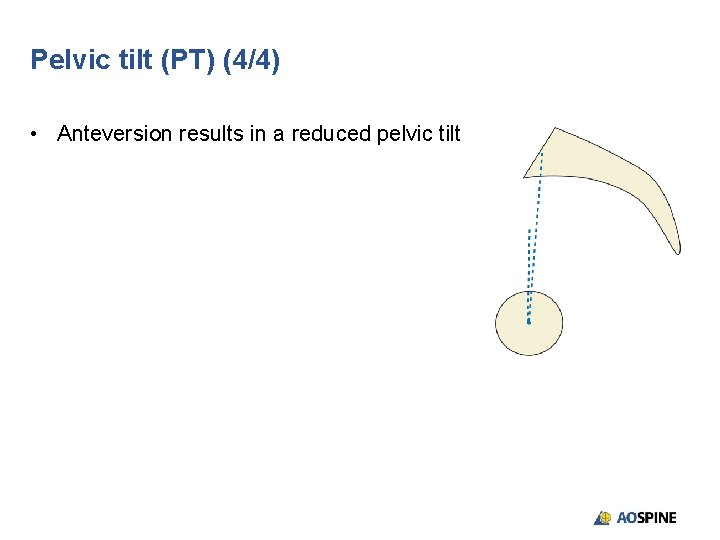
Pelvic tilt (PT) (4/4) • Anteversion results in a reduced pelvic tilt
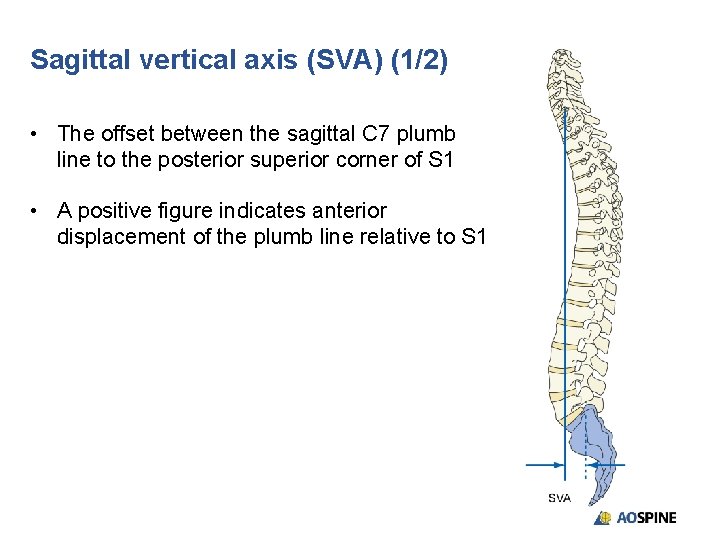
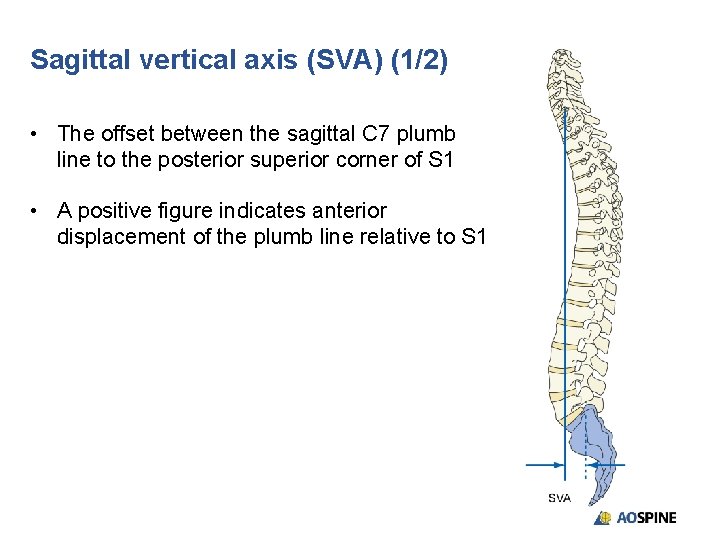
Sagittal vertical axis (SVA) (1/2) • The offset between the sagittal C 7 plumb line to the posterior superior corner of S 1 • A positive figure indicates anterior displacement of the plumb line relative to S 1
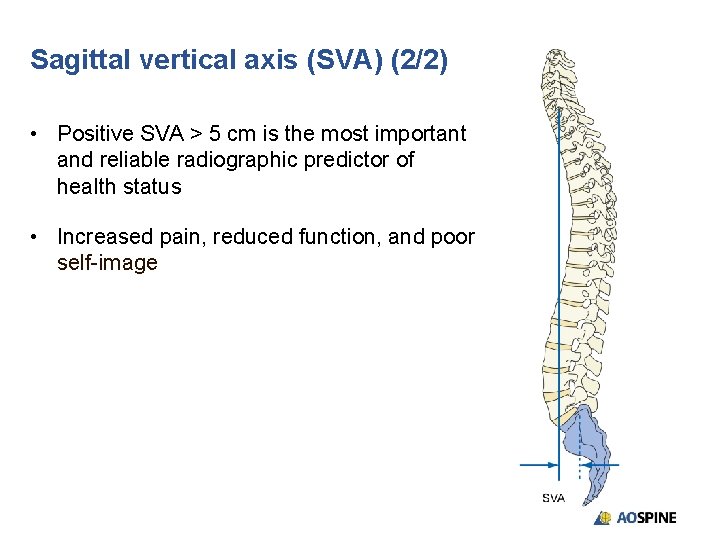
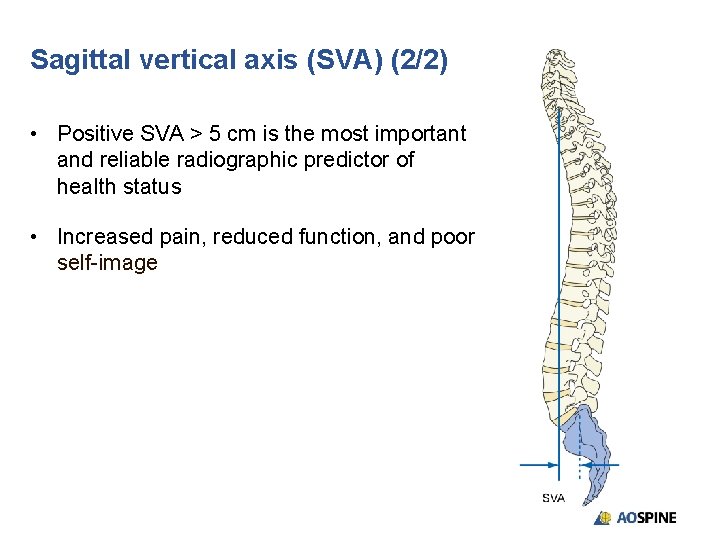
Sagittal vertical axis (SVA) (2/2) • Positive SVA > 5 cm is the most important and reliable radiographic predictor of health status • Increased pain, reduced function, and poor self-image
Treatment (1/2) • Surgical principles • Preoperative planning is essential to ensure surgical goals are understood and achievable • If normal disc and facets L 5–S 1 in younger patient, then avoid fusion to pelvis in first instance
Treatment (2/2) • Surgical principles • Degeneration of L 5–S 1 or oblique take-off of L 5 from pelvis requires fusion to pelvis • Fusion to pelvis requires A/P approach at L 5–S 1, and also generally at L 4/5 and above where accessible • Pelvic fixation may also be indicated • Important not to stop instrumentation at apex of kyphosis or scoliosis
Prognosis • For appropriately selected patients, clinical success and improved levels of activity and function are achieved in 80– 85% of patients • Good medical management is needed to minimize risks due to comorbidities
Potential complications • Cardiac or pulmonary complications: • Myocardial infarction, cardiovascular accident, pulmonary embolism • Persistent imbalance • Junctional breakdown • Degeneration, loss of fixation, or fracture • Nonunion and implant failure • Infection • Neurological complications • Persistent pain
Take-home messages • Degenerative scoliosis is not uncommon • Surgical intervention should be considered as a last resort in elderly patients, particularly those with significant comorbidities, due to associated risks • For well-selected patients with appropriate expectations, the outcome is generally good • Achieve and maintain spinal balance • Surgical planning is essential • Good medical management is needed to manage comorbidities

References 1. Aebi M. The adult scoliosis. Eur Spine J. 2005; 14(10): 925 -948. 2. Shapiro GS, Taira G Boachie-Adjei. Results of surgical treatment of adult idiopathic scoliosis with low back pain and spinal stenosis: a study of long-term clinical and radiographic outcomes. Spine. 2003; 28(4): 358 -363. 3. Ali RM, Boachie-Adjei O, Rowlins BA. Functional and radiographic outcomes after surgery for adult scoliosis using third-generation instrumentation techniques. Spine. 2003; 28(11): 1169 -1170. 4. Bradford DS, Tay BK, Hu SS. Adult scoliosis: surgical indications, operative management, complications, and outcomes. Spine. 1999; 24(24): 2617 -2629. 5. Ascani E, Bartolozzi P, Logroscino CA, et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine. 1986; 11(8): 784 -789. 6. Nachemson A. Adult scoliosis and back pain. Spine. 1979; 4(6): 513 -517.
Excellence in Spine
 Degenerative myelopathy wayne
Degenerative myelopathy wayne Fascetaria
Fascetaria Vaginal pessary
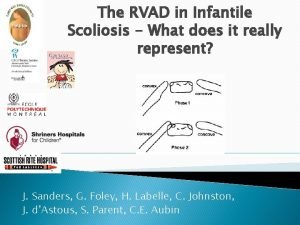
Vaginal pessary Rvad angle
Rvad angle Scoliosis chiropractor seminole county
Scoliosis chiropractor seminole county Risser score scoliosis
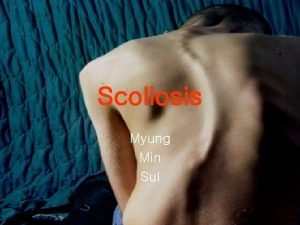
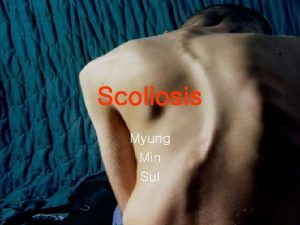
Risser score scoliosis Scoliosis
Scoliosis Scoliosis research society
Scoliosis research society Wheelchair backrest for scoliosis
Wheelchair backrest for scoliosis Mri scoliosis protocol
Mri scoliosis protocol Thoracogenic scoliosis of thoracolumbar region
Thoracogenic scoliosis of thoracolumbar region Disorder of synovium and tendon
Disorder of synovium and tendon Infantile scoliosis casting
Infantile scoliosis casting Costodesis
Costodesis Early onset scoliosis classification
Early onset scoliosis classification Rib hump scoliosis
Rib hump scoliosis Coronal balance
Coronal balance Dr abdullah sayegh
Dr abdullah sayegh Factors affecting traction
Factors affecting traction Derotation cast
Derotation cast Turnbuckle cast scoliosis
Turnbuckle cast scoliosis Writing strategies and ethical considerations
Writing strategies and ethical considerations Ethical consideration in experimental research sample
Ethical consideration in experimental research sample Pricing considerations and approaches
Pricing considerations and approaches What are the general considerations in machine design?
What are the general considerations in machine design? Tax considerations for setting up a new business
Tax considerations for setting up a new business Software architecture of atm machine
Software architecture of atm machine Three considerations of societal marketing concept
Three considerations of societal marketing concept Mechanical considerations of transmission line
Mechanical considerations of transmission line Database design considerations
Database design considerations Contrasting acquisition
Contrasting acquisition Cloud delivery models
Cloud delivery models Pre analytical considerations in phlebotomy
Pre analytical considerations in phlebotomy Bioreactor considerations for animal cell culture
Bioreactor considerations for animal cell culture Collaboration design considerations
Collaboration design considerations