Current Management of Anal Fistulas in Crohns Disease




- Slides: 22
Current Management of Anal Fistulas in Crohn’s Disease Rita YK Chang Joint Hospital Surgical Grand Round 23 th April 2016
Background • 20 -50% Crohn’s disease (CD) have perianal fistula • More distal luminal CD are at higher risk – 90% proctitis have fistula • Low remission and high recurrence • More complications – Stricture, stenosis, abscess
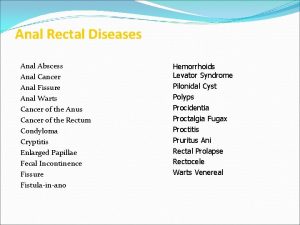
Classification • Park’s classification • High vs. low • Simple vs. complex – Complex: • • Secondary branches Involving >= 1/3 of the sphincter circuit Anterior fistulas in women Faecal incontinence, strictures

Investigations • Colonoscopy – Concomitant active proctocolitis – Malignancy • Examination under anaesthesia (EUA): – Accuracy of 90% – Allow concomitant surgery
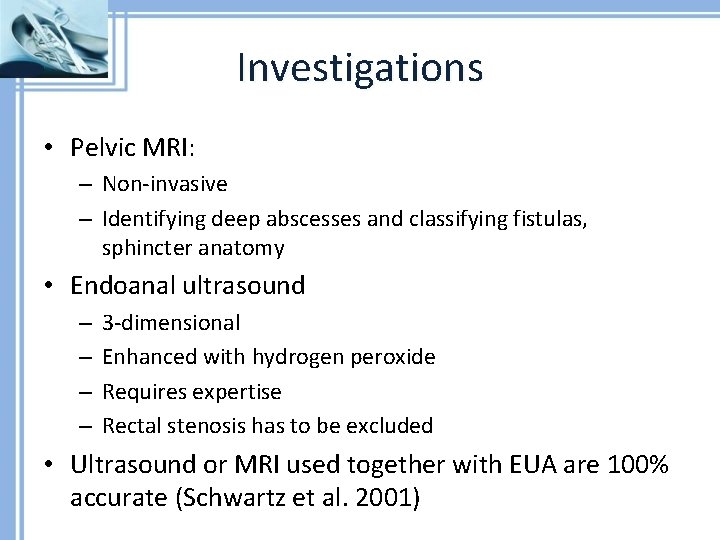
Investigations • Pelvic MRI: – Non-invasive – Identifying deep abscesses and classifying fistulas, sphincter anatomy • Endoanal ultrasound – – 3 -dimensional Enhanced with hydrogen peroxide Requires expertise Rectal stenosis has to be excluded • Ultrasound or MRI used together with EUA are 100% accurate (Schwartz et al. 2001)
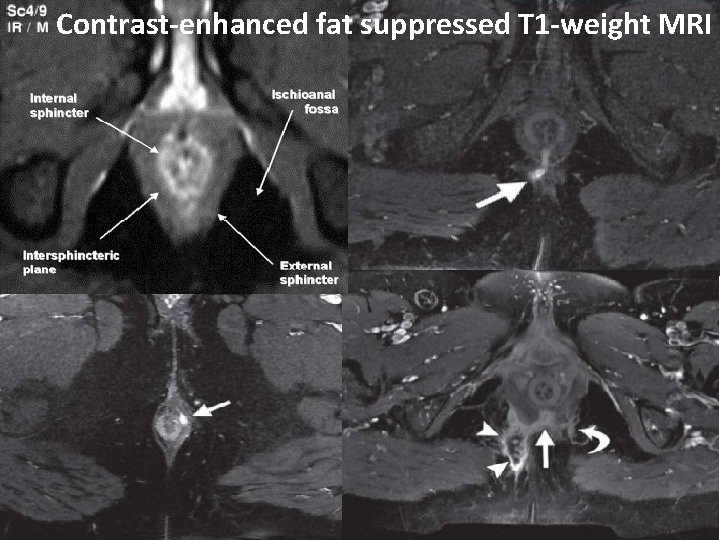
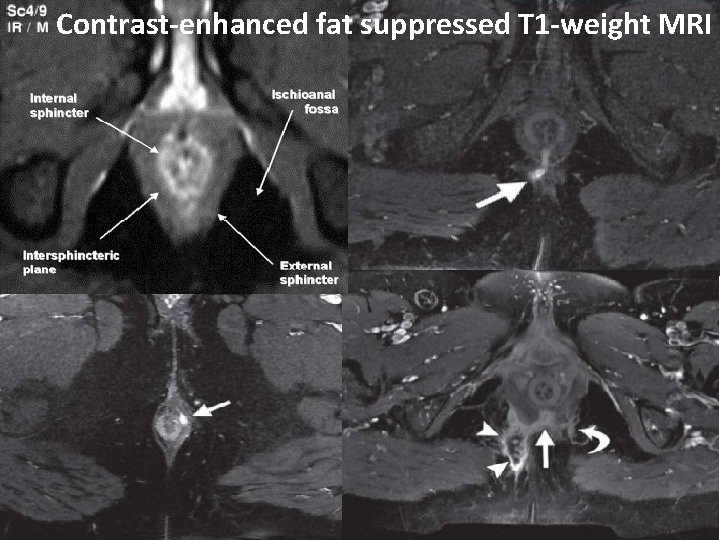
Contrast-enhanced fat suppressed T 1 -weight MRI

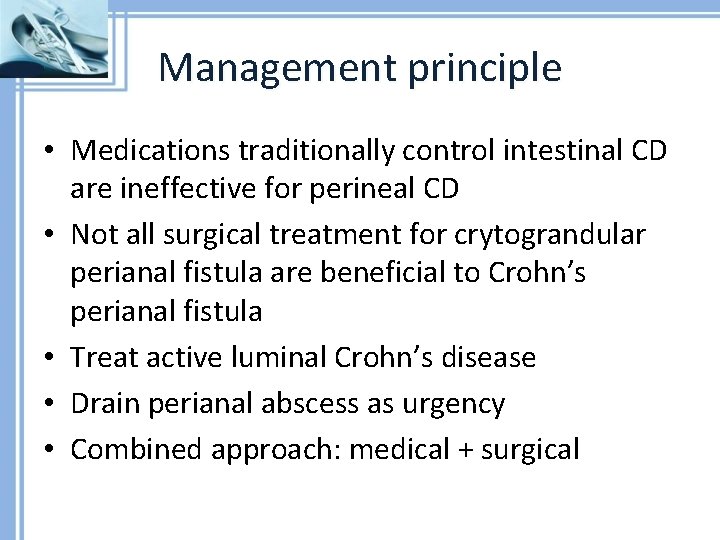
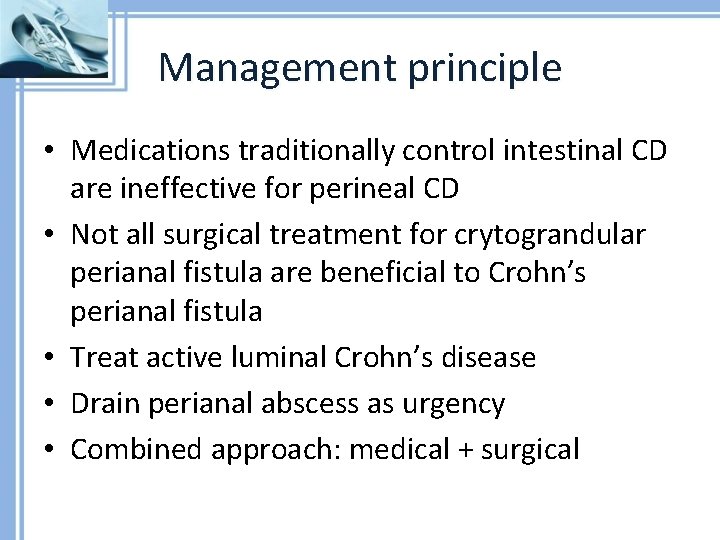
Management principle • Medications traditionally control intestinal CD are ineffective for perineal CD • Not all surgical treatment for crytograndular perianal fistula are beneficial to Crohn’s perianal fistula • Treat active luminal Crohn’s disease • Drain perianal abscess as urgency • Combined approach: medical + surgical
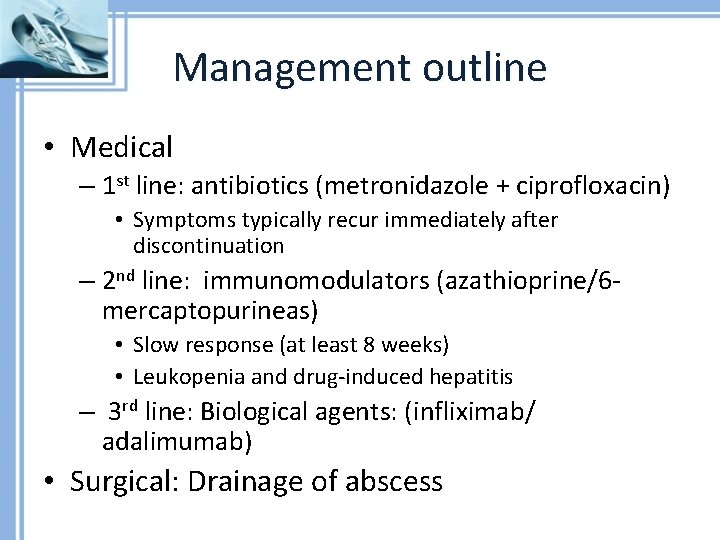
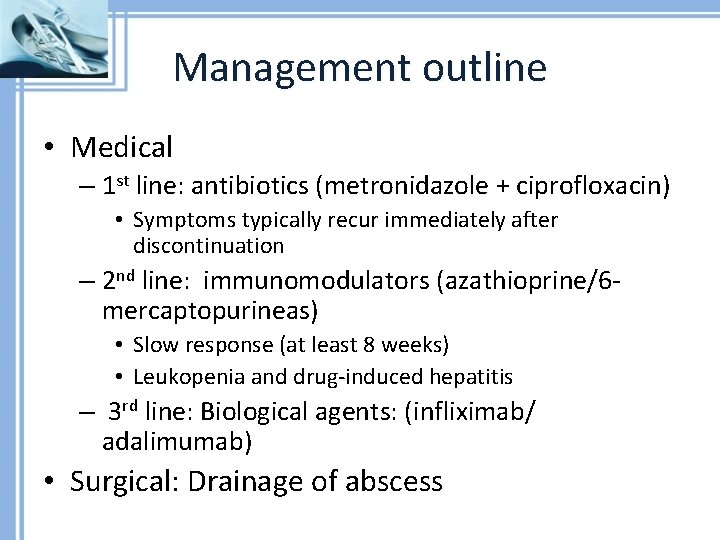
Management outline • Medical – 1 st line: antibiotics (metronidazole + ciprofloxacin) • Symptoms typically recur immediately after discontinuation – 2 nd line: immunomodulators (azathioprine/6 mercaptopurineas) • Slow response (at least 8 weeks) • Leukopenia and drug-induced hepatitis – 3 rd line: Biological agents: (infliximab/ adalimumab) • Surgical: Drainage of abscess
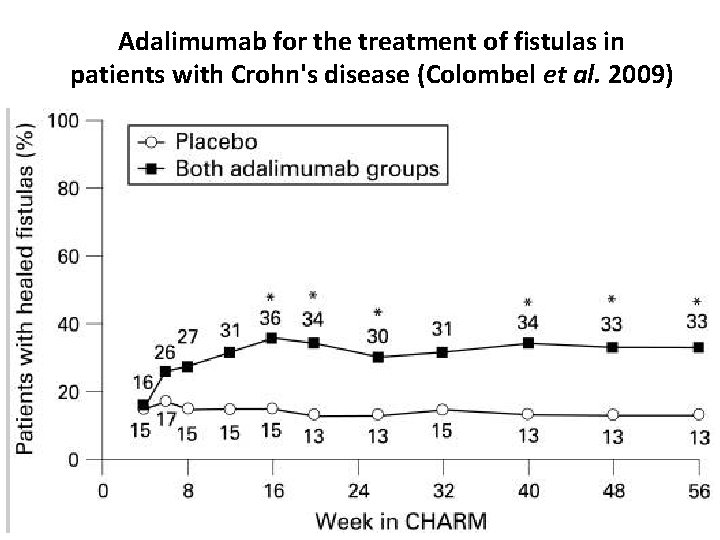
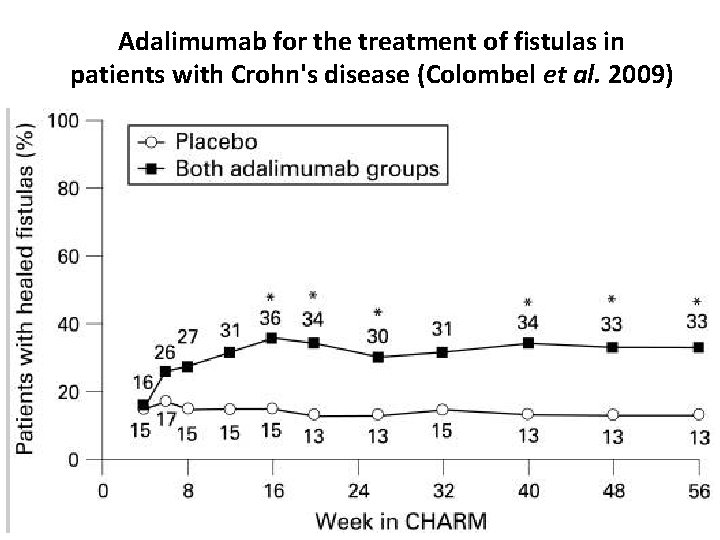
Adalimumab for the treatment of fistulas in patients with Crohn's disease (Colombel et al. 2009)
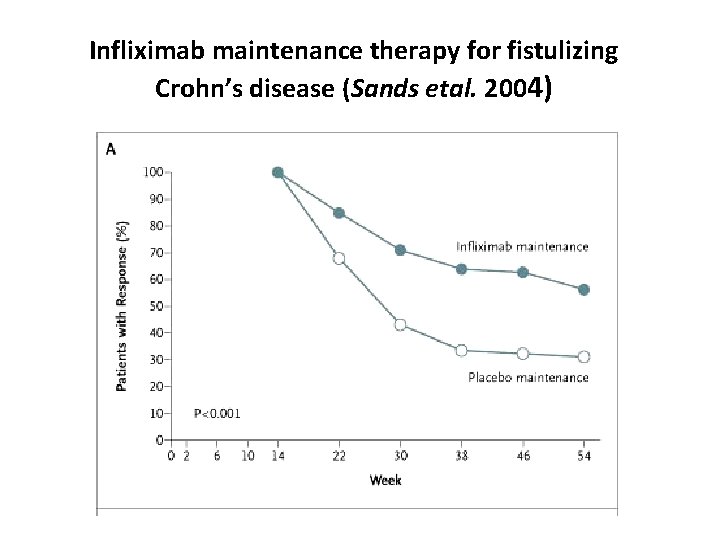
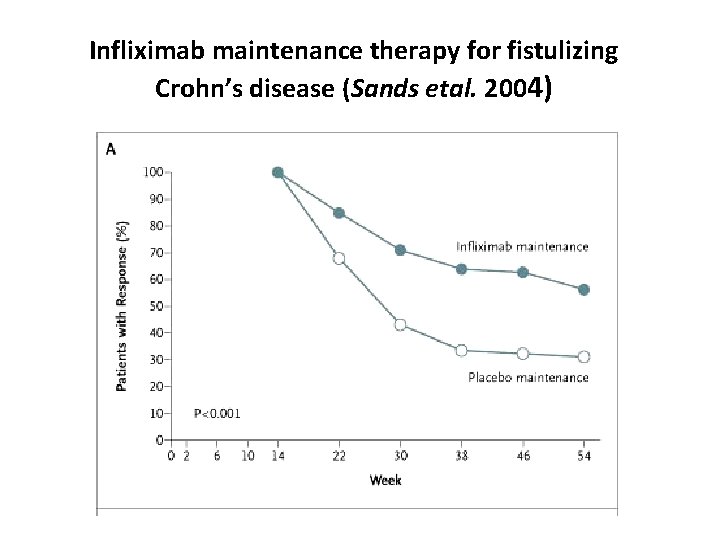
Infliximab maintenance therapy for fistulizing Crohn’s disease (Sands etal. 2004)
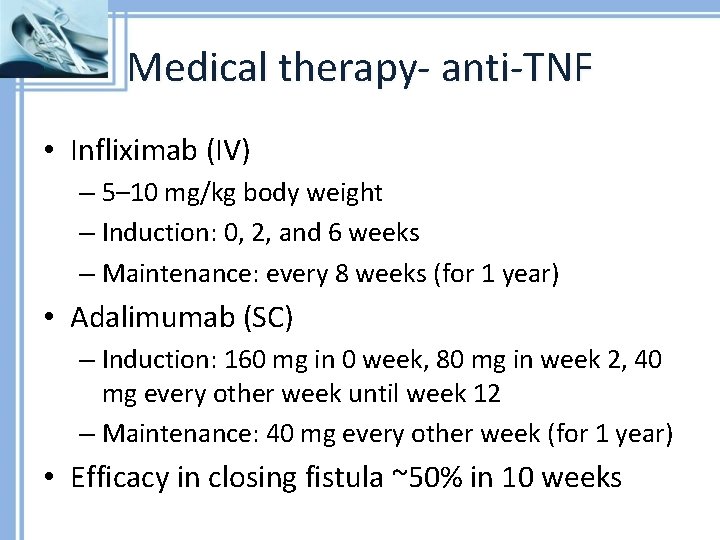
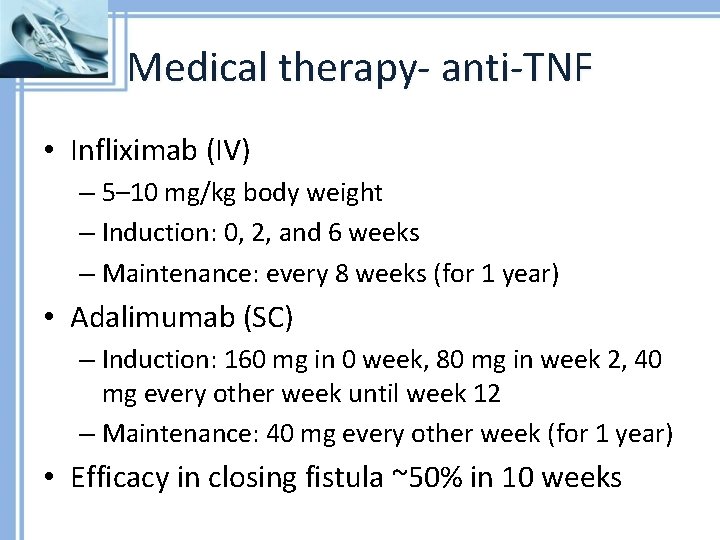
Medical therapy- anti-TNF • Infliximab (IV) – 5– 10 mg/kg body weight – Induction: 0, 2, and 6 weeks – Maintenance: every 8 weeks (for 1 year) • Adalimumab (SC) – Induction: 160 mg in 0 week, 80 mg in week 2, 40 mg every other week until week 12 – Maintenance: 40 mg every other week (for 1 year) • Efficacy in closing fistula ~50% in 10 weeks
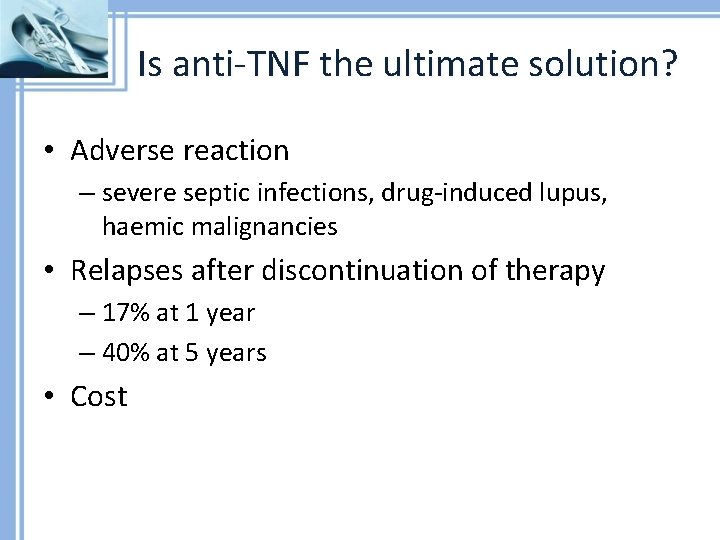
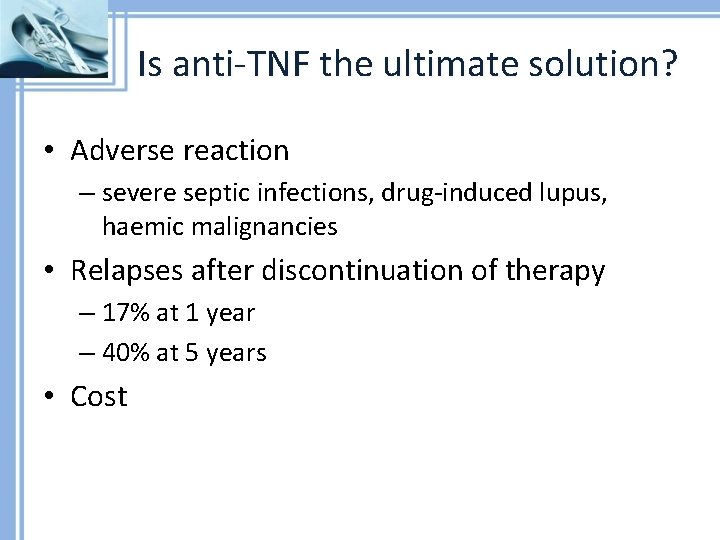
Is anti-TNF the ultimate solution? • Adverse reaction – severe septic infections, drug-induced lupus, haemic malignancies • Relapses after discontinuation of therapy – 17% at 1 year – 40% at 5 years • Cost
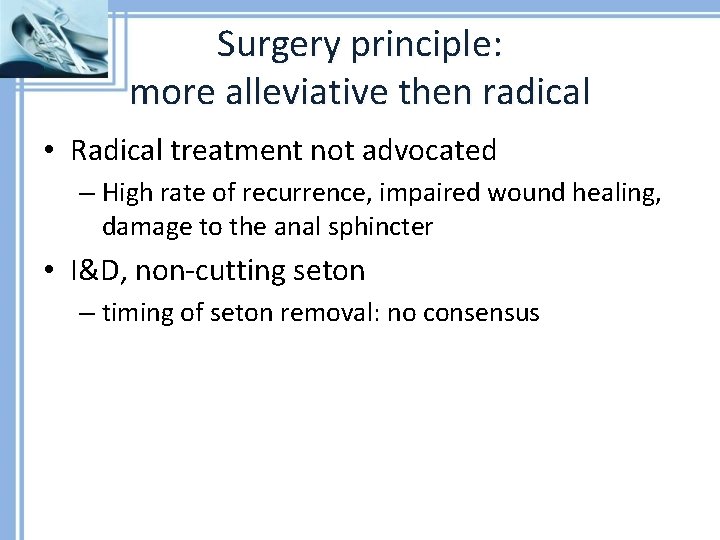
Surgery principle: more alleviative then radical • Radical treatment not advocated – High rate of recurrence, impaired wound healing, damage to the anal sphincter • I&D, non-cutting seton – timing of seton removal: no consensus
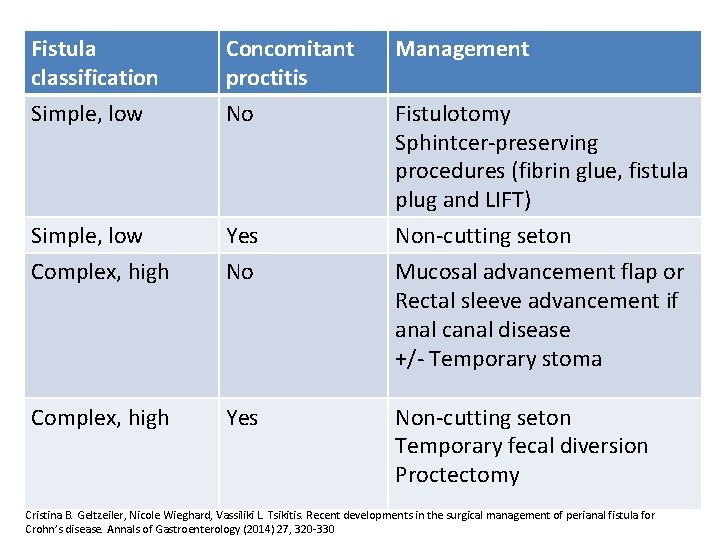
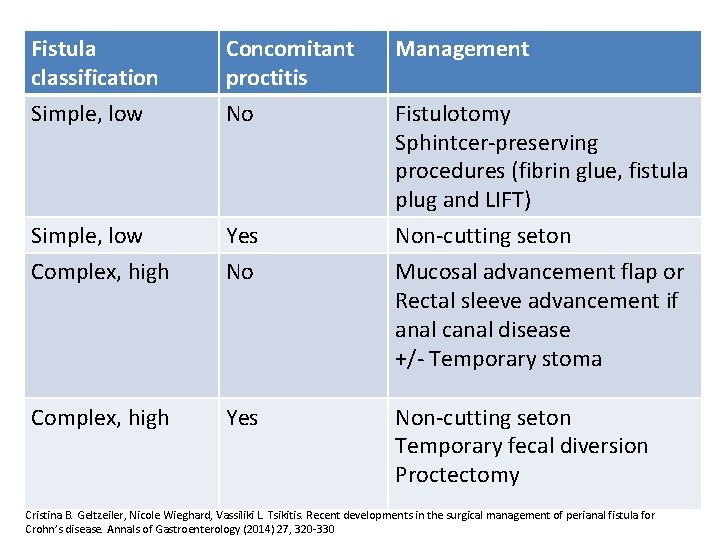
Fistula classification Simple, low Concomitant proctitis No Management Simple, low Complex, high Yes No Non-cutting seton Mucosal advancement flap or Rectal sleeve advancement if anal canal disease +/- Temporary stoma Complex, high Yes Non-cutting seton Temporary fecal diversion Proctectomy Fistulotomy Sphintcer-preserving procedures (fibrin glue, fistula plug and LIFT) Cristina B. Geltzeiler, Nicole Wieghard, Vassiliki L. Tsikitis. Recent developments in the surgical management of perianal fistula for Crohn’s disease. Annals of Gastroenterology (2014) 27, 320 -330

Anorectal advancement flap Rakinic J, Poola VP. Curr Probl Surg. 2014. 51 (3): 98 -137
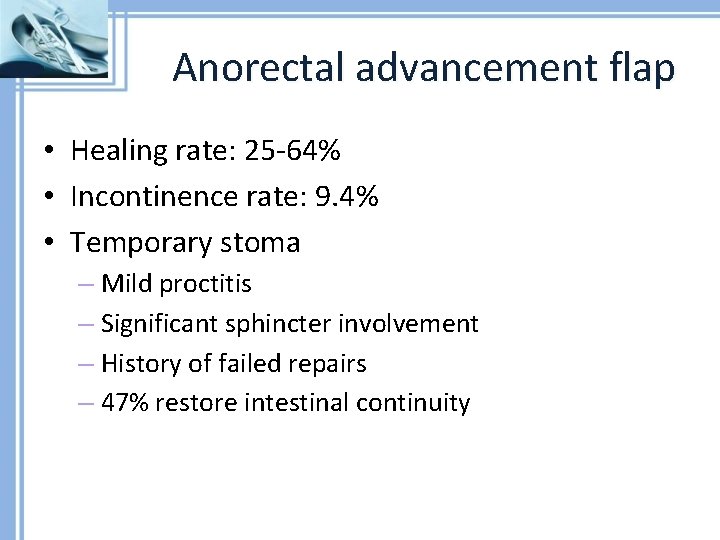
Anorectal advancement flap • Healing rate: 25 -64% • Incontinence rate: 9. 4% • Temporary stoma – Mild proctitis – Significant sphincter involvement – History of failed repairs – 47% restore intestinal continuity
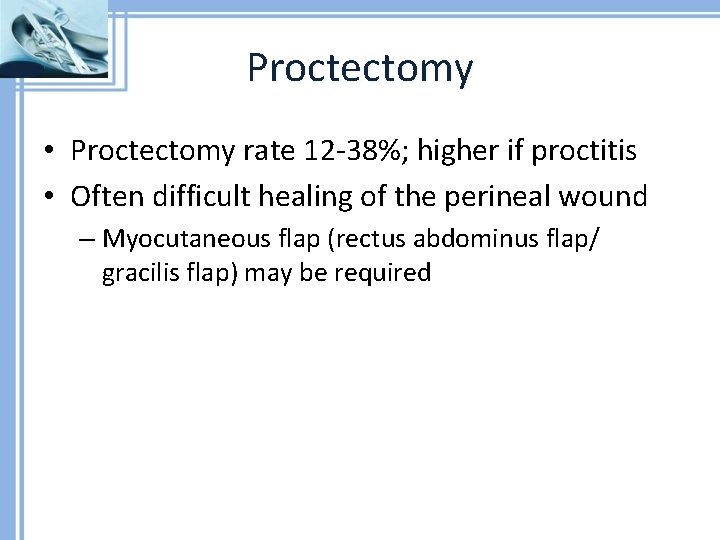
Proctectomy • Proctectomy rate 12 -38%; higher if proctitis • Often difficult healing of the perineal wound – Myocutaneous flap (rectus abdominus flap/ gracilis flap) may be required
New treatment • Local anti-TNF injection • Stem cell in fibrin glue • Video-assisted fistula treatment
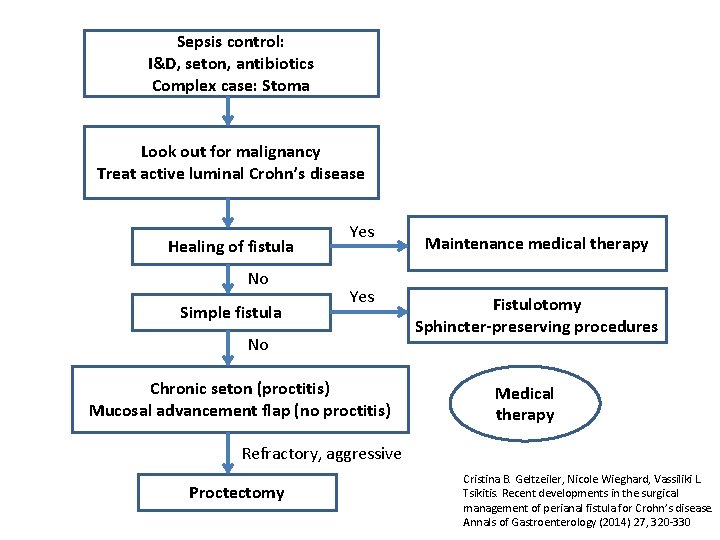
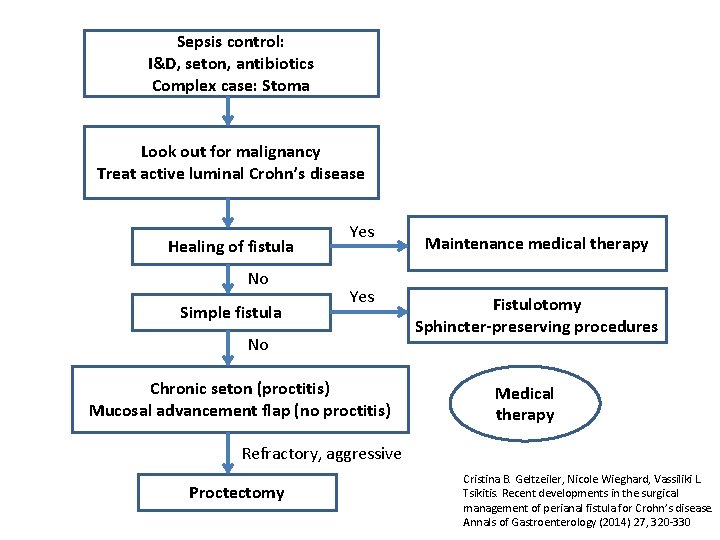
Sepsis control: I&D, seton, antibiotics Complex case: Stoma Look out for malignancy Treat active luminal Crohn’s disease Healing of fistula No Simple fistula Yes No Chronic seton (proctitis) Mucosal advancement flap (no proctitis) Maintenance medical therapy Fistulotomy Sphincter-preserving procedures Medical therapy Refractory, aggressive Proctectomy Cristina B. Geltzeiler, Nicole Wieghard, Vassiliki L. Tsikitis. Recent developments in the surgical management of perianal fistula for Crohn’s disease. Annals of Gastroenterology (2014) 27, 320 -330

References: • • • Cristina B. Geltzeiler, Nicole Wieghard, Vassiliki L. Tsikitis. Recent developments in the surgical management of perianal fistula for Crohn’s disease. Annals of Gastroenterology (2014) 27, 320 -330 Elsa Limura, Pasquale Giordano. Modern management of anal fistula. World J Gastroenterol 2015 January 7; 21(1): 12 -20 Meniero P. Tech Coloproctol 2009 13: 347 Rojanasakul A. LIFT procedure: a simplified technique for fistula-in-ano. Tech. Coloproctol. 2009 Sep; 13(3): 237 -40. Yamaguchi T, Kagawa R, Takahashi H, Takeda R, Sakata S, Nishizaki D. Diagnostic implications of MR imaging for mucinous adenocarcinoma arising from fistula in ano. Tech Coloproctol. 2009 Sep; 13(3): 251 -3. doi: 10. 1007/s 10151 -009 -0509 -z. Epub 2009 Jul 17. Rakinic J, Poola VP. Hemorrhoids and fistulas: new solutions to old problems. Curr Probl Surg. 2014. 51 (3): 98 -137 G. A. Santoro, C. Ratto. Accuracy and Reliability of Endoanal Ultrasonography in the Evaluation of Perianal Abscesses and Fistula-in-ano. P. 141 -182 Z Abdool, A H Sultan, R Thakar. Ultrasound imaging of the anal sphincter complex: a review. Br J Radiol. 2012 Jul; 85(1015): 865– 875 Michael R. Torkzad and Urban Karlbom. MRI for assessment of anal fistula. Insights Imaging. 2010 May; 1(2): 62– 71
 Crohn's disease classification
Crohn's disease classification Fosa isquirectal
Fosa isquirectal Clasificacion saint james fistulas
Clasificacion saint james fistulas Fistula
Fistula Crohns disese
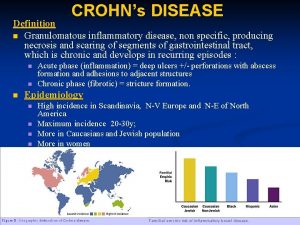
Crohns disese What is crohns didease
What is crohns didease Communicable disease and non communicable disease
Communicable disease and non communicable disease A balanced delta connected load having an impedance 20-j15
A balanced delta connected load having an impedance 20-j15 Difference between phase voltage and line voltage
Difference between phase voltage and line voltage Drift current and diffusion current
Drift current and diffusion current Line current and phase current
Line current and phase current Drift current and diffusion current
Drift current and diffusion current Ceramic composition resistors
Ceramic composition resistors At cut off the jfet channel is
At cut off the jfet channel is Balanced y-y connection
Balanced y-y connection Holding current and latching current
Holding current and latching current Drift current density unit
Drift current density unit All of the heat produced by sma weld stays in the weld.
All of the heat produced by sma weld stays in the weld. Touch current vs leakage current
Touch current vs leakage current Mesh current method with current source
Mesh current method with current source To'g'ri ichak kasalliklari
To'g'ri ichak kasalliklari Automatic bladder vs autonomic bladder
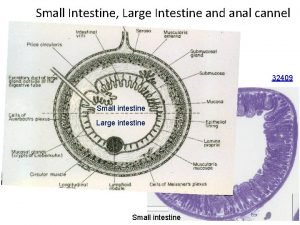
Automatic bladder vs autonomic bladder Crypts of lieberkuhn
Crypts of lieberkuhn