Cummings Chapters 63 64 Acute and Chronic Laryngitis


- Slides: 41
Cummings Chapters 63 & 64 Acute and Chronic Laryngitis Laryngeal and Tracheal Manifestations of Systemic Disease Travis Shiba 12/6/13
Acute and Chronic Laryngitis n Key Points #1 cause of acute laryngitis = viral n #1 cause of chronic laryngitis = reflux n Candidal laryngitis can occur in non immuno compromised n Even in setting of likely neoplasm, still consider infection n
Laryngitis n Inflammation of the larynx n Can impair swallowing, phonating and breathing
Acute Laryngitis Phonotrauma n Viral Laryngitis n Acute Bacterial Laryngitis n Acute Fungal Laryngitis n
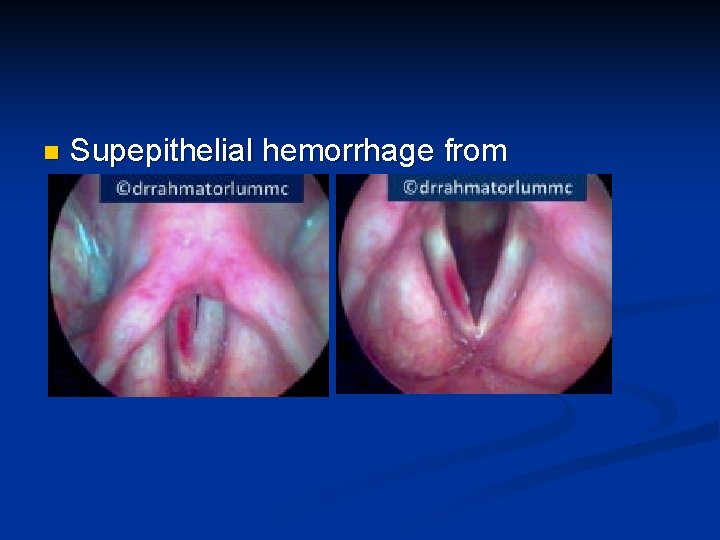
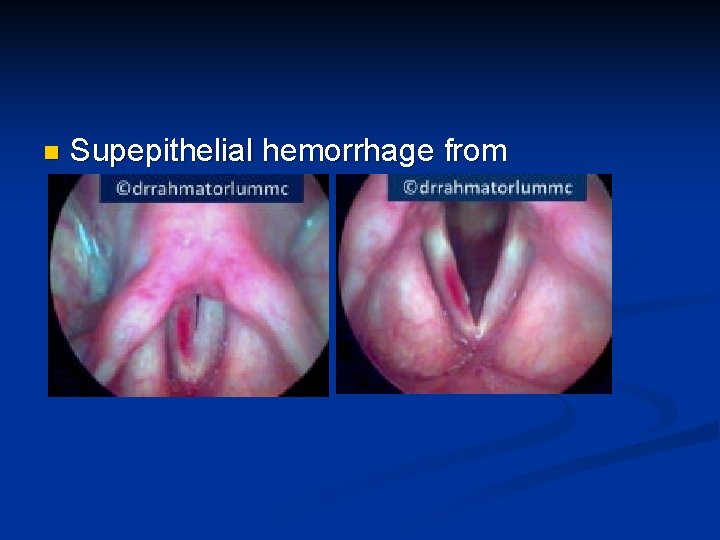
n Supepithelial hemorrhage from phonotrauma
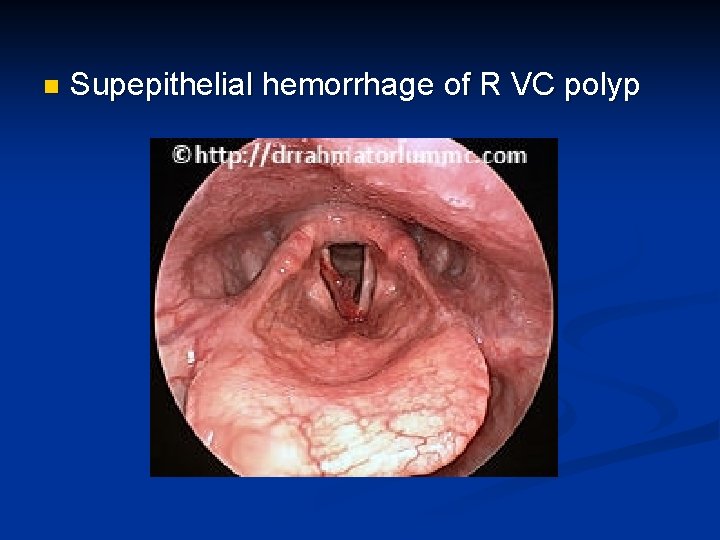
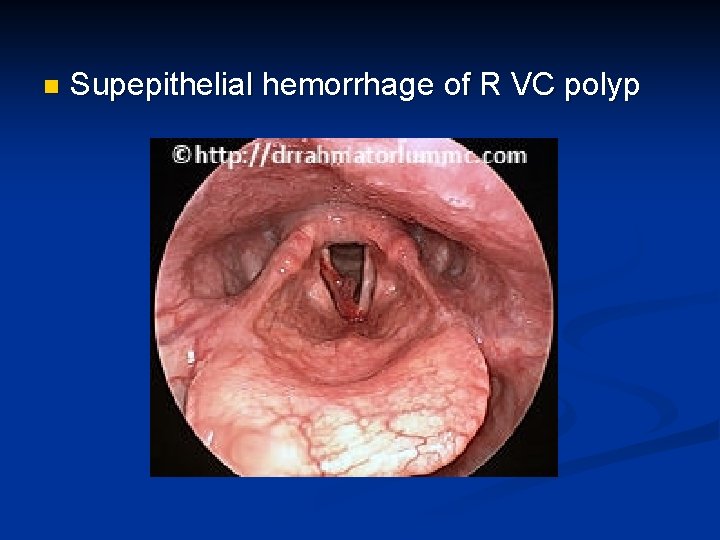
n Supepithelial hemorrhage of R VC polyp
Acute Laryngitis Phonotrauma n Viral Laryngitis n Acute Bacterial Laryngitis n Acute Fungal Laryngitis n
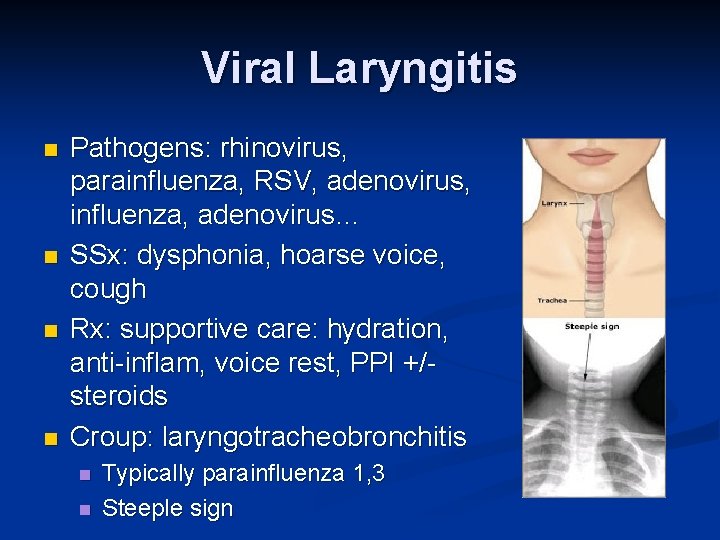
Viral Laryngitis n n Pathogens: rhinovirus, parainfluenza, RSV, adenovirus, influenza, adenovirus… SSx: dysphonia, hoarse voice, cough Rx: supportive care: hydration, anti-inflam, voice rest, PPI +/steroids Croup: laryngotracheobronchitis n n Typically parainfluenza 1, 3 Steeple sign
Acute Laryngitis Phonotrauma n Viral Laryngitis n Acute Bacterial Laryngitis n Acute Fungal Laryngitis n
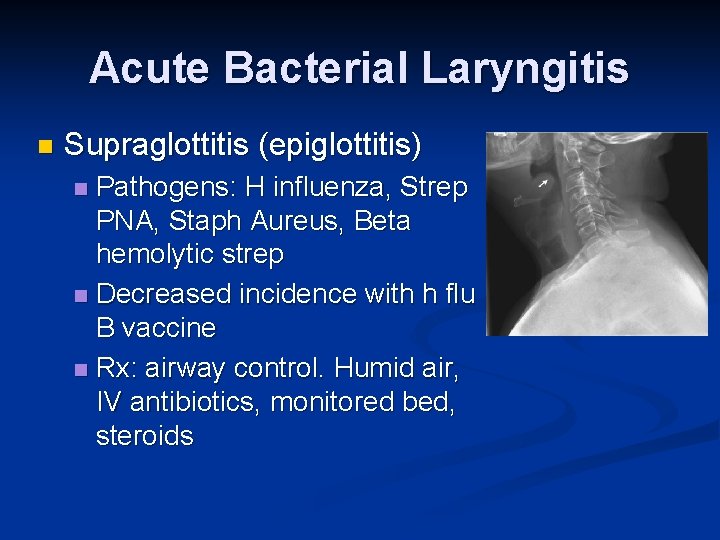
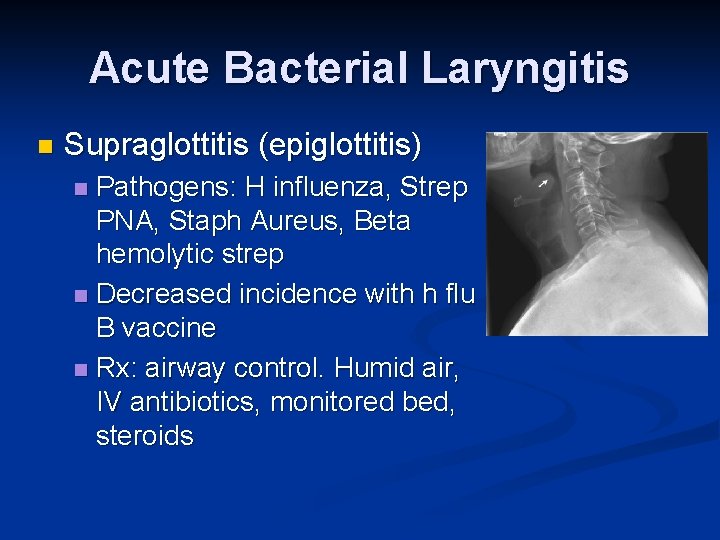
Acute Bacterial Laryngitis n Supraglottitis (epiglottitis) Pathogens: H influenza, Strep PNA, Staph Aureus, Beta hemolytic strep n Decreased incidence with h flu B vaccine n Rx: airway control. Humid air, IV antibiotics, monitored bed, steroids n
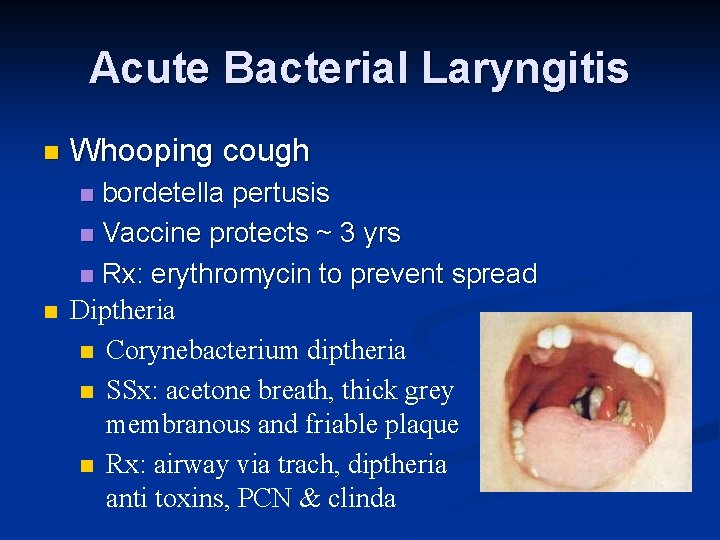
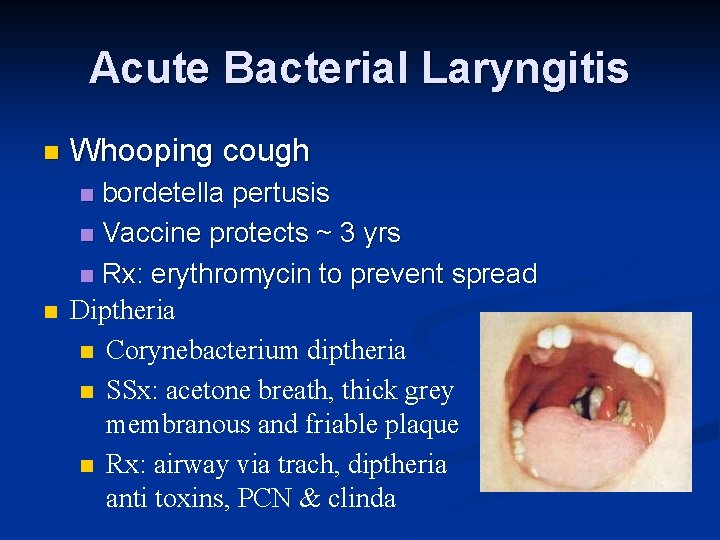
Acute Bacterial Laryngitis n Whooping cough bordetella pertusis n Vaccine protects ~ 3 yrs n Rx: erythromycin to prevent spread Diptheria n Corynebacterium diptheria n SSx: acetone breath, thick grey membranous and friable plaque n Rx: airway via trach, diptheria anti toxins, PCN & clinda n n
Acute Laryngitis Phonotrauma n Viral Laryngitis n Acute Bacterial Laryngitis n Acute Fungal Laryngitis n
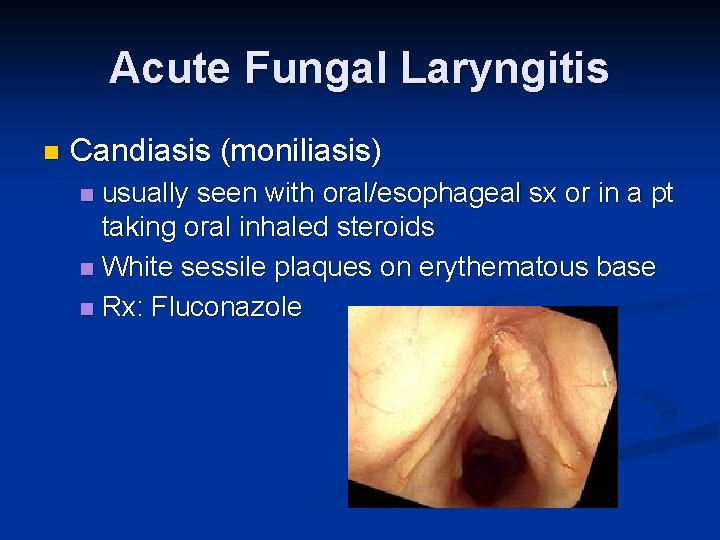
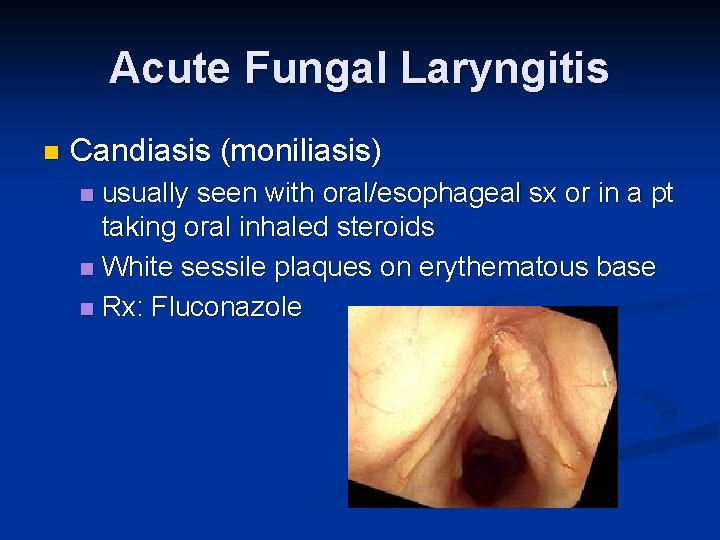
Acute Fungal Laryngitis n Candiasis (moniliasis) usually seen with oral/esophageal sx or in a pt taking oral inhaled steroids n White sessile plaques on erythematous base n Rx: Fluconazole n
Chronic Laryngitis Bacterial n Fungal n Mycobacterial n Non infectious n
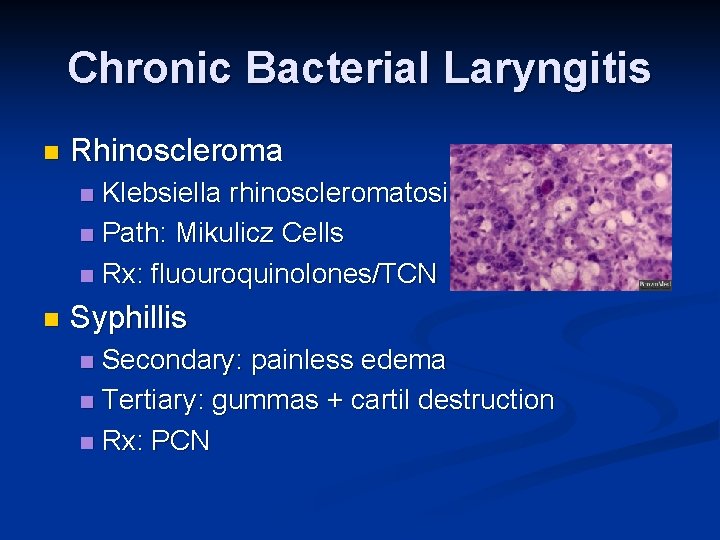
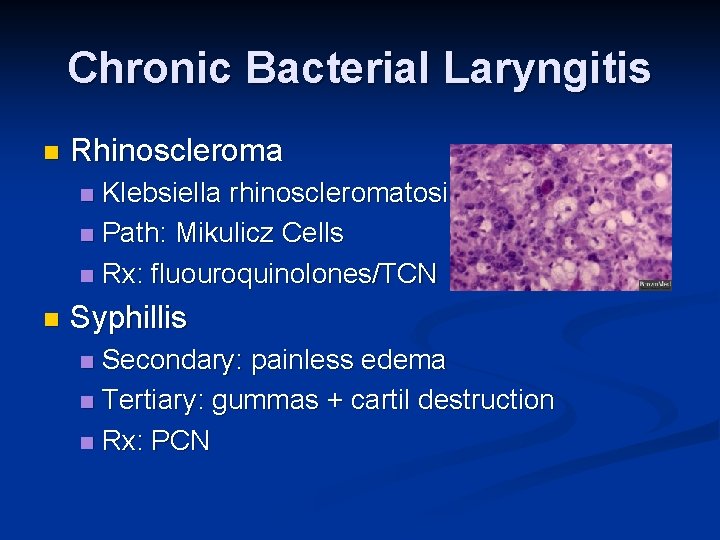
Chronic Bacterial Laryngitis n Rhinoscleroma Klebsiella rhinoscleromatosis n Path: Mikulicz Cells n Rx: fluouroquinolones/TCN n n Syphillis Secondary: painless edema n Tertiary: gummas + cartil destruction n Rx: PCN n
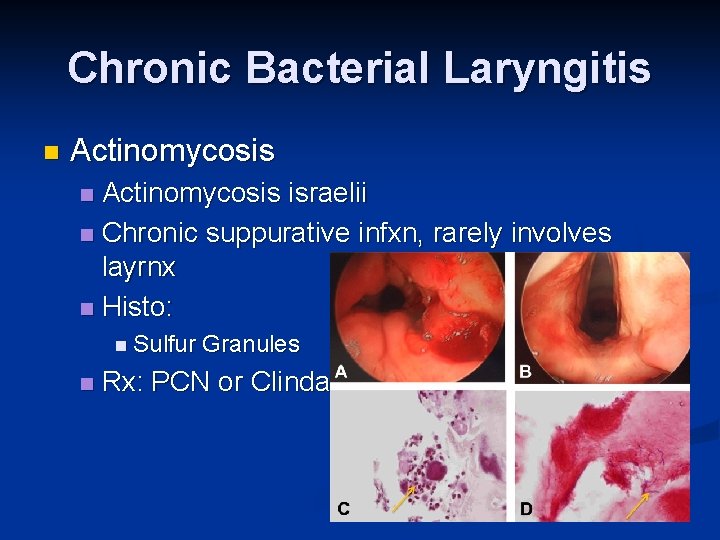
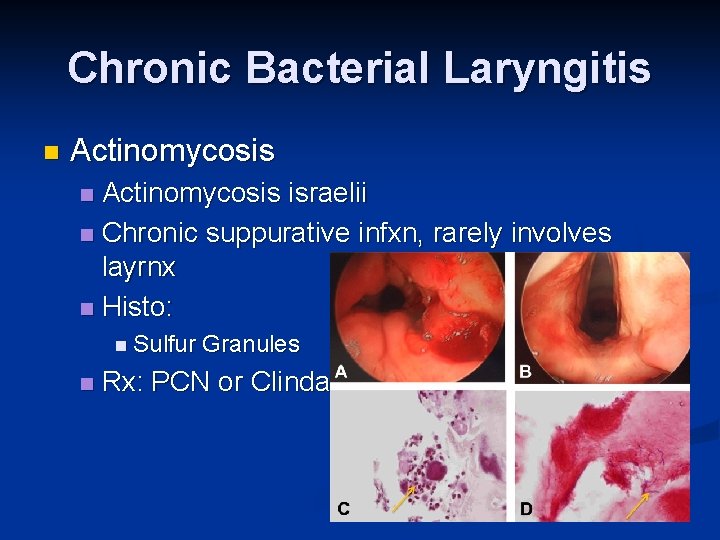
Chronic Bacterial Laryngitis n Actinomycosis israelii n Chronic suppurative infxn, rarely involves layrnx n Histo: n n Sulfur n Granules Rx: PCN or Clinda
Chronic Laryngitis Bacterial n Fungal n Histoplasmosis n Blastomycosis n Cryptococcus n Coccidiomycosis n Mycobacterial n Non infectious n
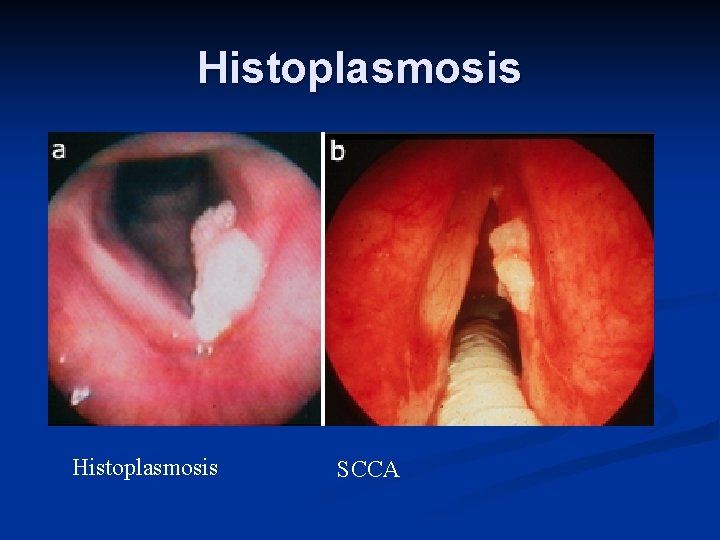
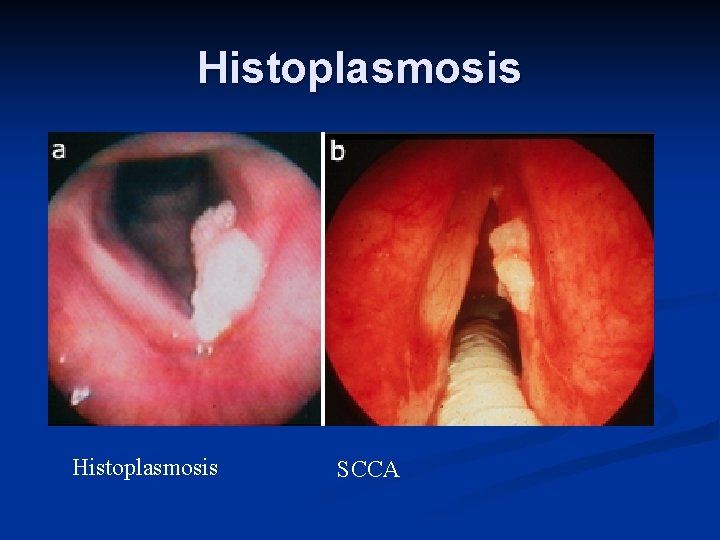
Histoplasmosis SCCA
Histoplasmosis n Histoplasma capsulatum Mississippi River Valley n Acute/Chronic, Pulmonary/systemic n Laryngeal Lesions: anterior larynx and epiglottis n Bx: poorly defined granulomas, multinucleated giant cells and pseudoepitheliomatous hyperplasia n Grows on Sabouraouds agar n Tx: Ampho/Azoles n
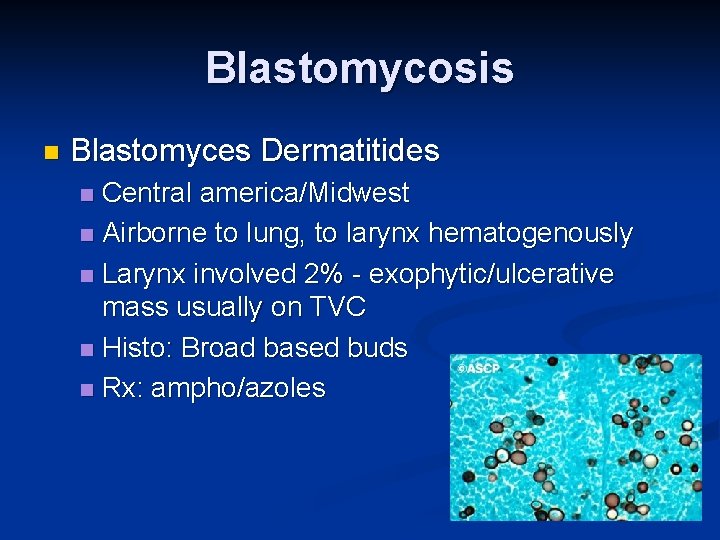
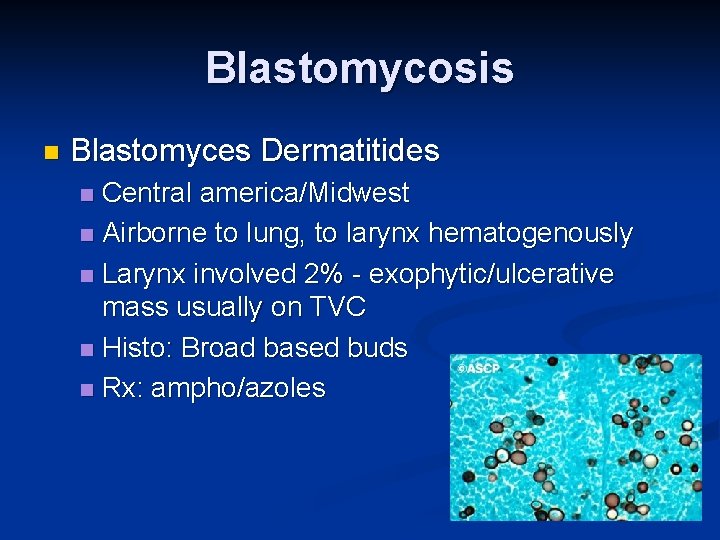
Blastomycosis n Blastomyces Dermatitides Central america/Midwest n Airborne to lung, to larynx hematogenously n Larynx involved 2% - exophytic/ulcerative mass usually on TVC n Histo: Broad based buds n Rx: ampho/azoles n
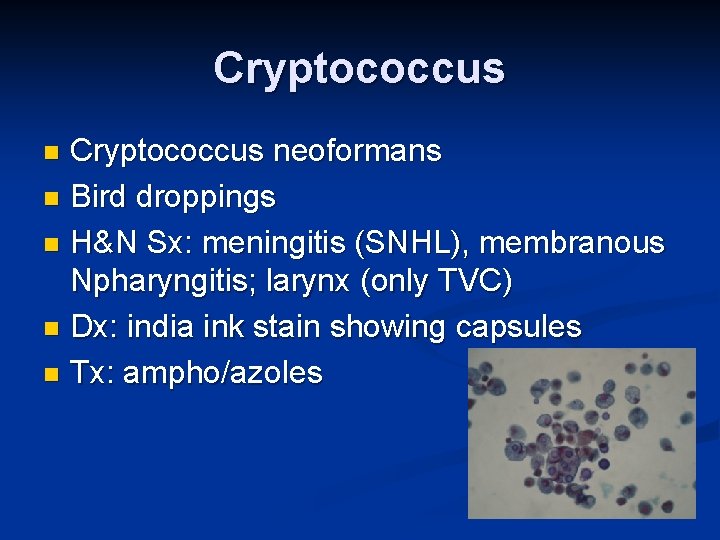
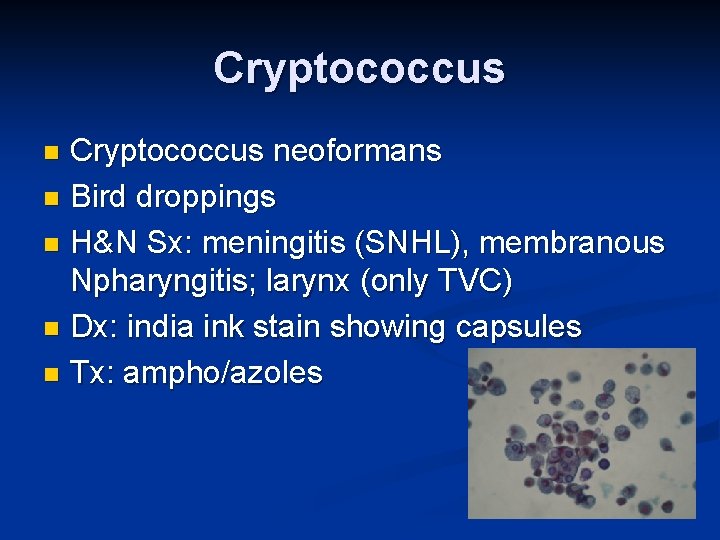
Cryptococcus neoformans n Bird droppings n H&N Sx: meningitis (SNHL), membranous Npharyngitis; larynx (only TVC) n Dx: india ink stain showing capsules n Tx: ampho/azoles n
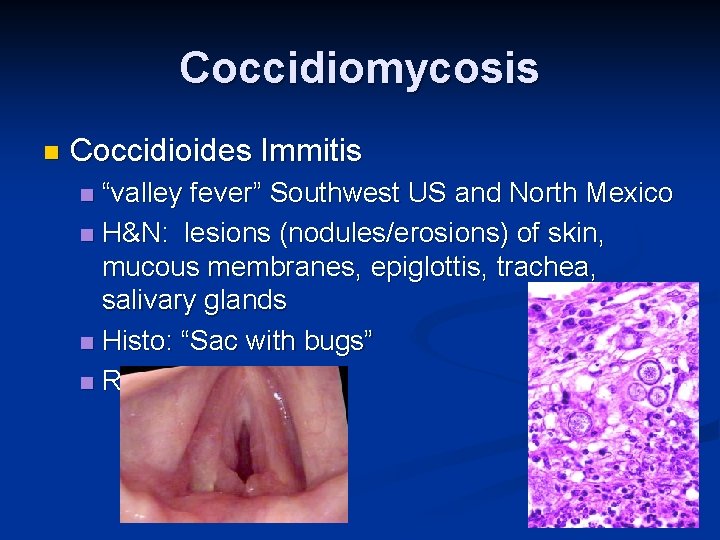
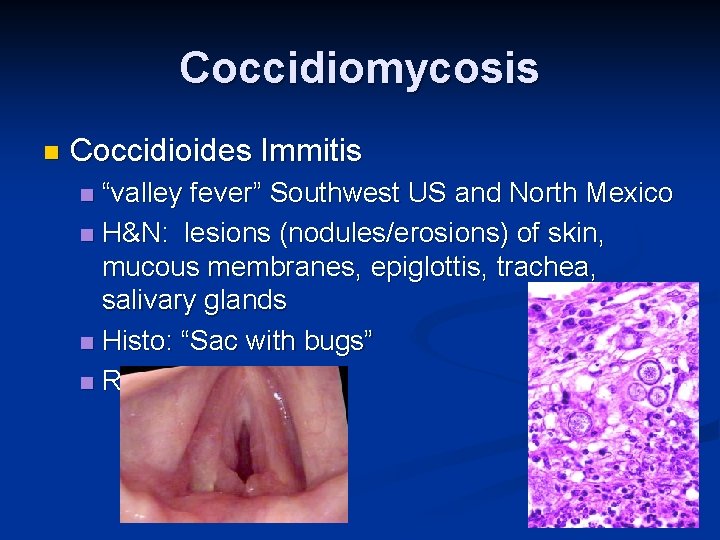
Coccidiomycosis n Coccidioides Immitis “valley fever” Southwest US and North Mexico n H&N: lesions (nodules/erosions) of skin, mucous membranes, epiglottis, trachea, salivary glands n Histo: “Sac with bugs” n Rx: ampho/azole n
Chronic Laryngitis Bacterial n Fungal n Mycobacterial n Non infectious n
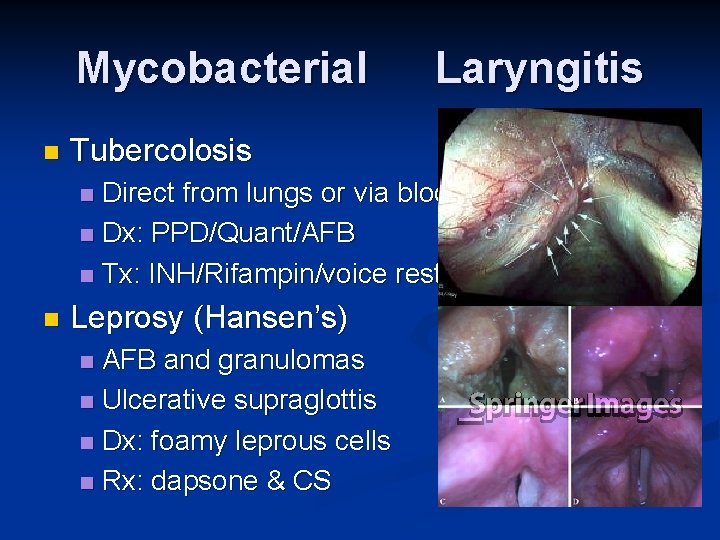
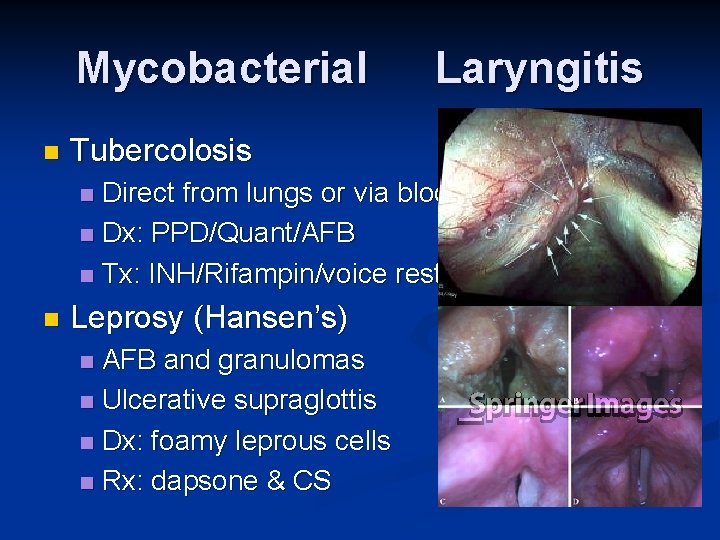
Mycobacterial n Laryngitis Tubercolosis Direct from lungs or via blood n Dx: PPD/Quant/AFB n Tx: INH/Rifampin/voice rest n n Leprosy (Hansen’s) AFB and granulomas n Ulcerative supraglottis n Dx: foamy leprous cells n Rx: dapsone & CS n
Chronic Laryngitis Bacterial n Fungal n Mycobacterial n Non infectious n
Non Infectious Laryngitis Smoking n Pollution n Vocal Abuse n Rhinosinusitis n Laryngopharyngeal Reflux n
LPR Etiologies: acid/bile/pepsin n RF: obsity, Et. OH, hiatial hernia, preg, scleroderma, feeding tube n SSx: Hoarse (am>pm), globus, dysphagia n Dx: trial of PPI/NP scope n Barium swallow n 24 hour dual p. H probe n esophagoscopy n

LPR n Rx: n Behavioral: smoking cessation, elevate HOB, avoid late meals, overeating, avoid tight close/loose weight n Decrease caffiene, Et. OH, mints, chocolate, n Avoid ASA, nitrates, CCB n Medications n PPI (usually 2 x dose for LPR versus GERD) n H 2 blockers n Surgery n Fundoplication

Laryngeal and Tracheal Manifestations of Systemic Disease n Key Points Symptoms: hoarseness, cough, stridor, airway compromise n Mimic laryngeal carcinoma n
n n n Wegener’s Granulomatosis Relapsing Polychondritis Sarcoidosis Rheumatoid Arthritis Pemphigus/pemphigoid Amyloidosis
Wegener’s Granulomatosis Idiopathic necrotizing granulomatous vasculitis n Types: n Limited (no renal) n Systemic (pulm and renal) n Laryngeal SSx: subglottic mass, dyspnea, biphasic stridor n Rx: Steroids + cyclophosphamide then MTX/Azathiaprine n
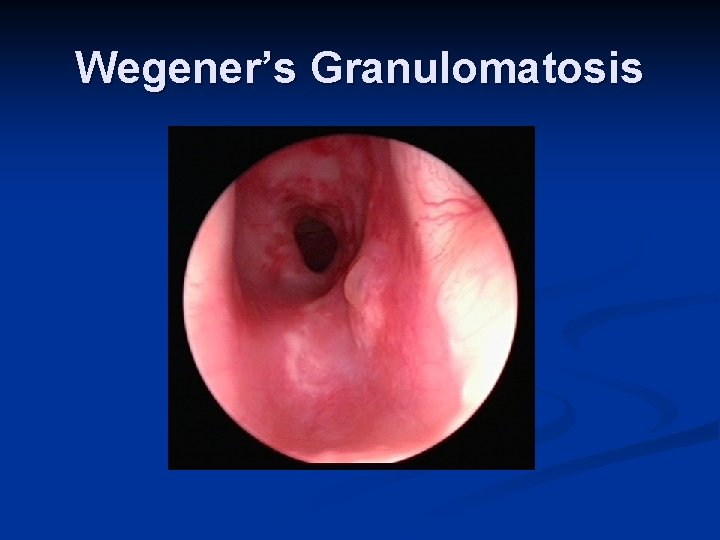
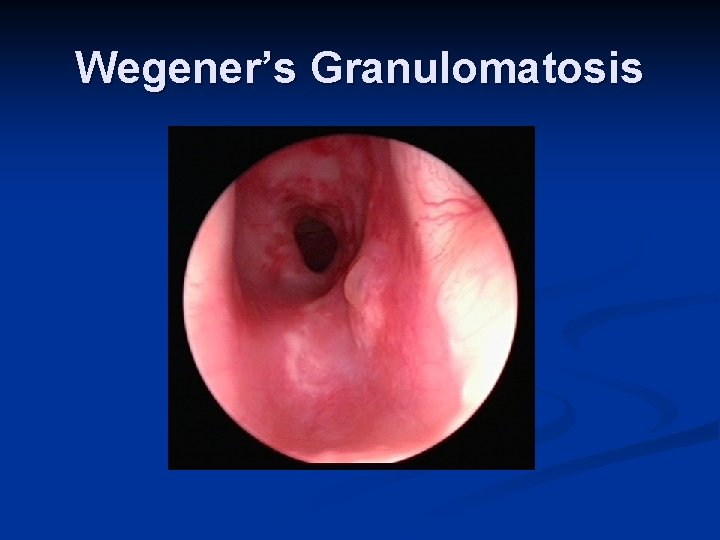
Wegener’s Granulomatosis
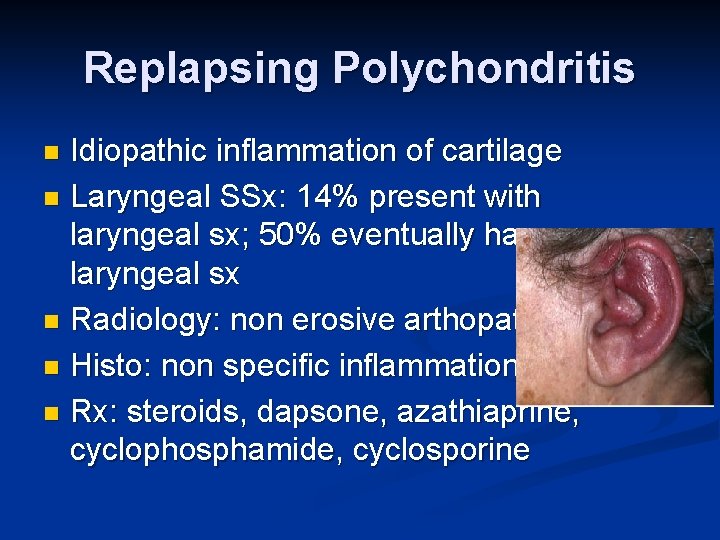
Replapsing Polychondritis Idiopathic inflammation of cartilage n Laryngeal SSx: 14% present with laryngeal sx; 50% eventually have laryngeal sx n Radiology: non erosive arthopathy n Histo: non specific inflammation n Rx: steroids, dapsone, azathiaprine, cyclophosphamide, cyclosporine n
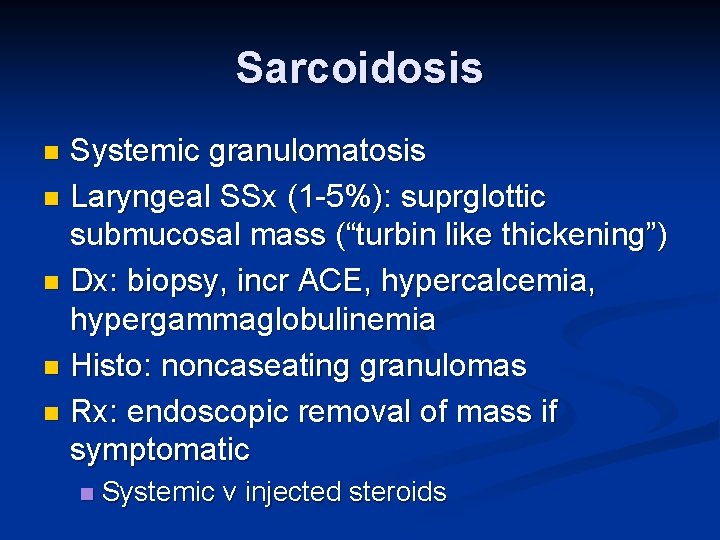
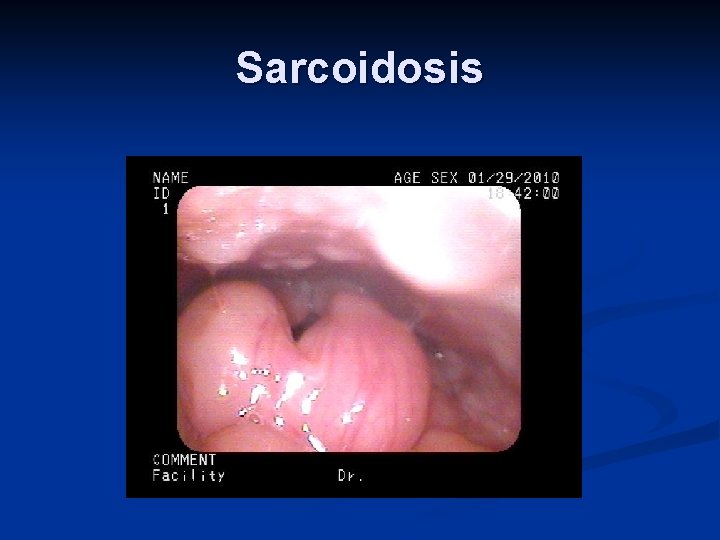
Sarcoidosis Systemic granulomatosis n Laryngeal SSx (1 -5%): suprglottic submucosal mass (“turbin like thickening”) n Dx: biopsy, incr ACE, hypercalcemia, hypergammaglobulinemia n Histo: noncaseating granulomas n Rx: endoscopic removal of mass if symptomatic n n Systemic v injected steroids
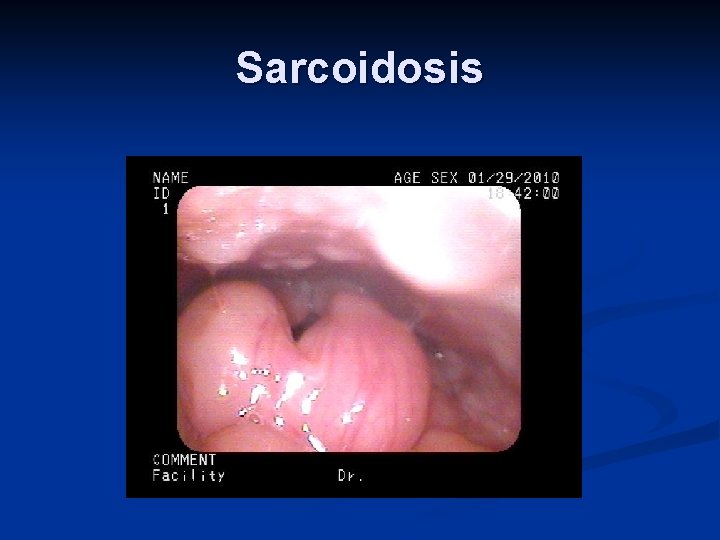
Sarcoidosis
Rheumatoid Arthritis Autoimmune n 25% Laryngeal involvement n Acute: tender/erythematous larynx n Chronic: cricoarytenoid ankylosis, submucosal nodules n Increased RF, ESR; decreased C’ n Rx: steroids and antireflux n
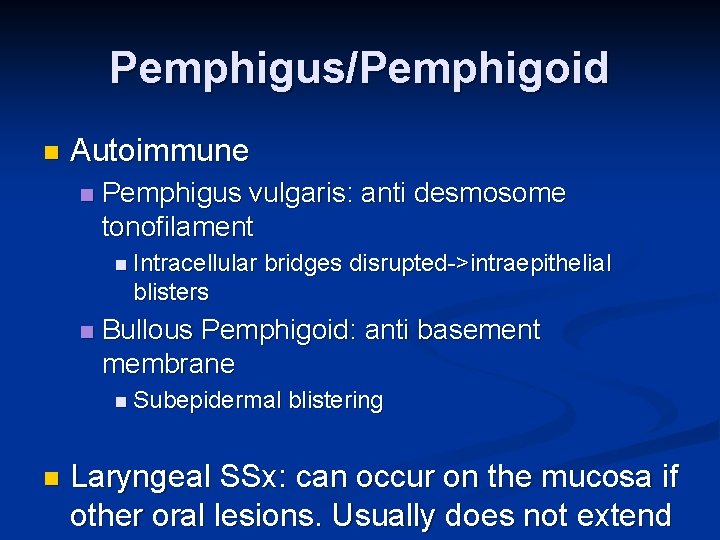
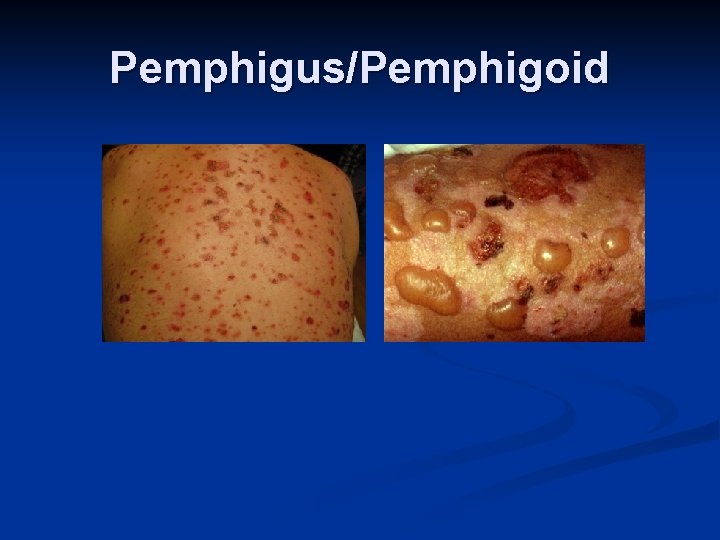
Pemphigus/Pemphigoid n Autoimmune n Pemphigus vulgaris: anti desmosome tonofilament n Intracellular bridges disrupted->intraepithelial blisters n Bullous Pemphigoid: anti basement membrane n Subepidermal n blistering Laryngeal SSx: can occur on the mucosa if other oral lesions. Usually does not extend
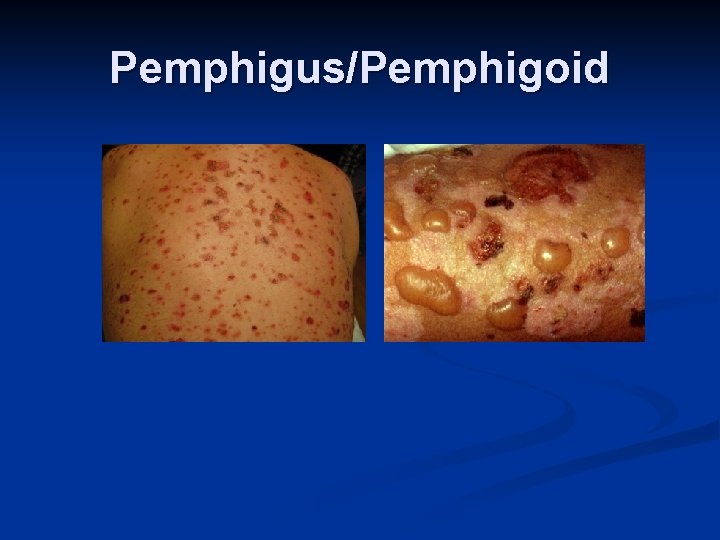
Pemphigus/Pemphigoid
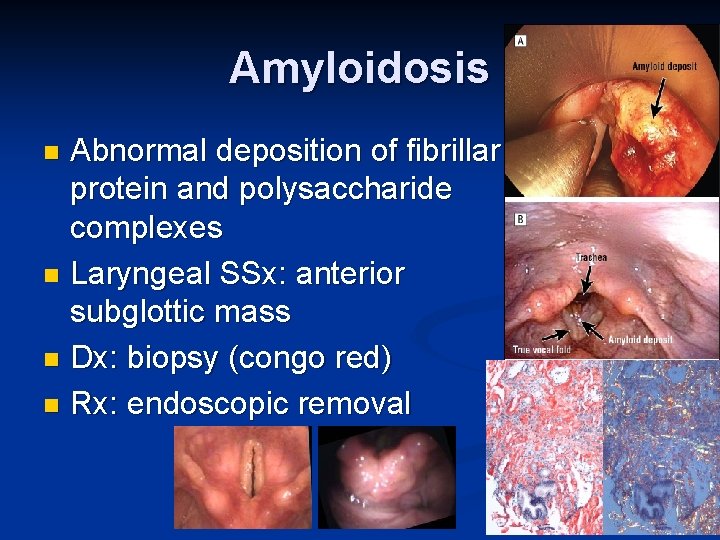
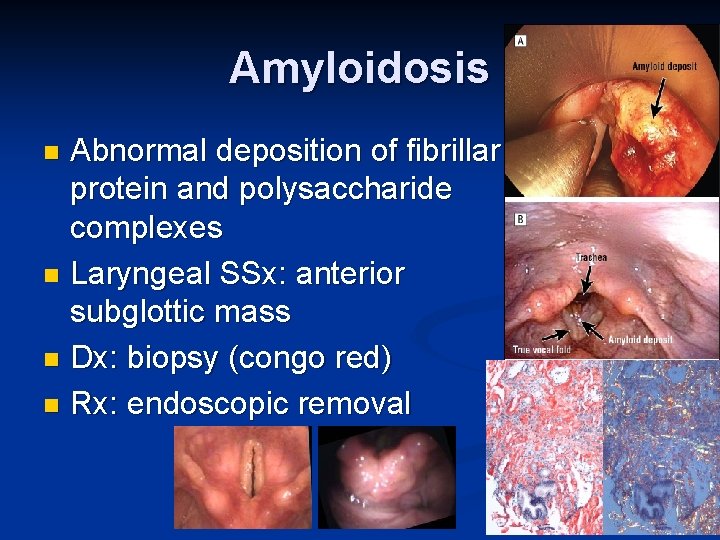
Amyloidosis Abnormal deposition of fibrillar protein and polysaccharide complexes n Laryngeal SSx: anterior subglottic mass n Dx: biopsy (congo red) n Rx: endoscopic removal n