Cummings Ch 2324 Maxillofacial Trauma Reconstruction of Facial
- Slides: 30
Cummings Ch 23/24 Maxillofacial Trauma Reconstruction of Facial Defects Julianna Pesce October 29, 2014
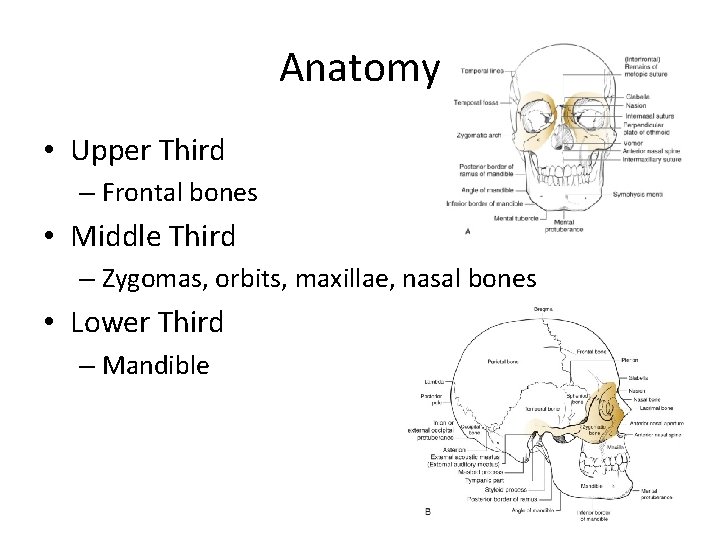
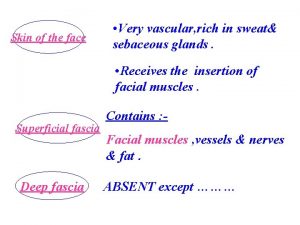
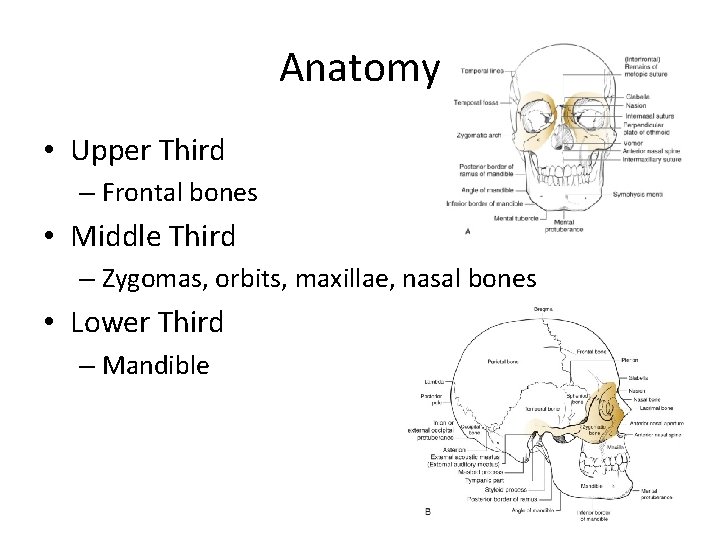
Anatomy • Upper Third – Frontal bones • Middle Third – Zygomas, orbits, maxillae, nasal bones • Lower Third – Mandible
Evaluation and Diagnosis • ABCs – Airway – High rate of c-spine fractures if facial trauma • PE – scalp, forehead – Orbits/vision, zygomas, nasal bones, septum, maxillae – Teeth, mandible, occlusion – Sensation, facial nerve function • CT is workhorse
Frontal Sinus • Anterior/posterior table, comminution, thickness • Sakas and colleagues: the more central and the more severe the fracture, more likely csf leakage
Frontal Sinus Repair • Is exploration necessary? Is obliteration necessary? • Anterior wall for cosmesis • Posterior wall to protect anterior cranial fossa • If nasofrontal ducts involved may lead to infection • Obliteration via cranialization if posterior wall severely comminuted
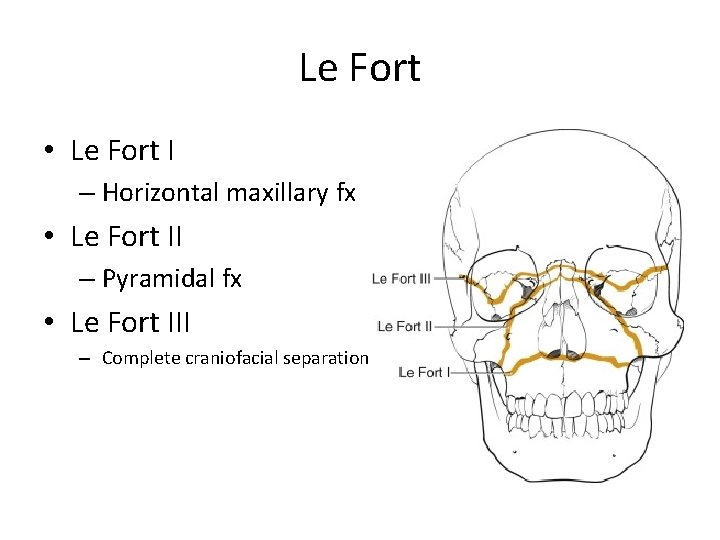
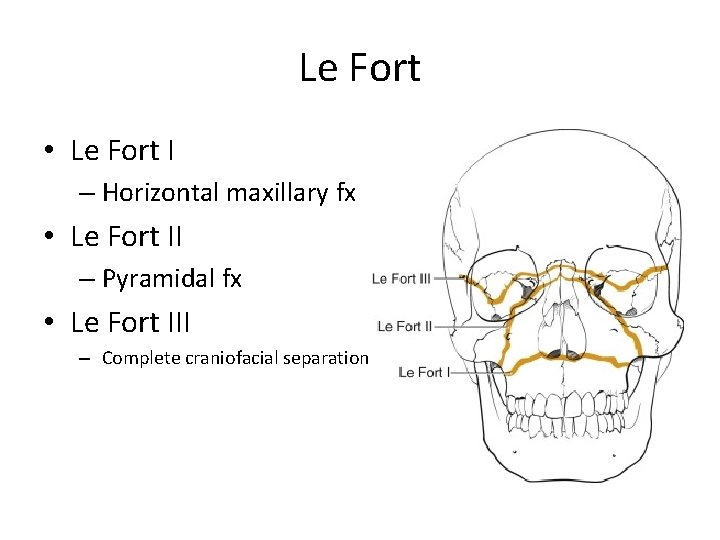
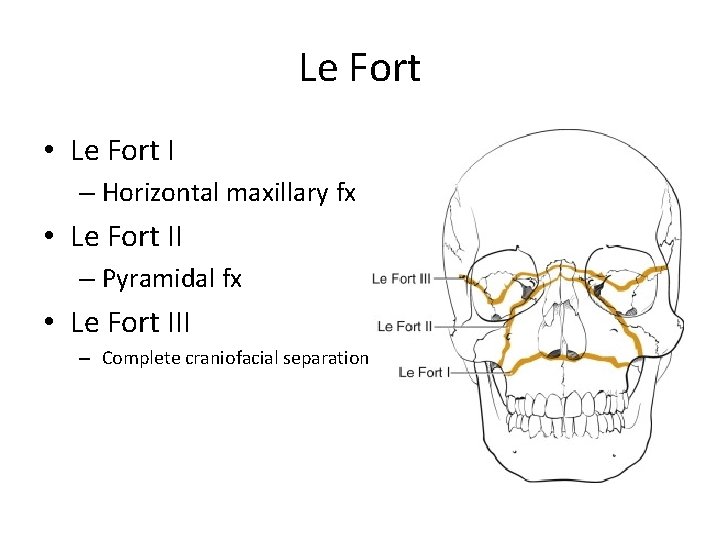
Le Fort • Le Fort I – Horizontal maxillary fx • Le Fort II – Pyramidal fx • Le Fort III – Complete craniofacial separation
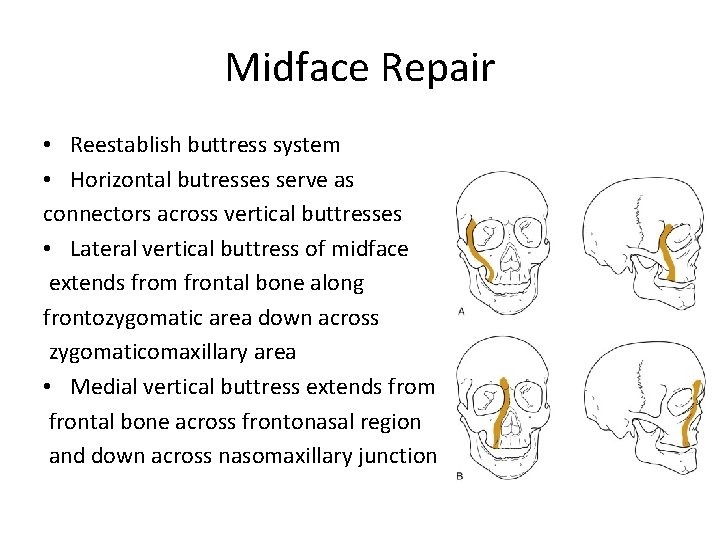
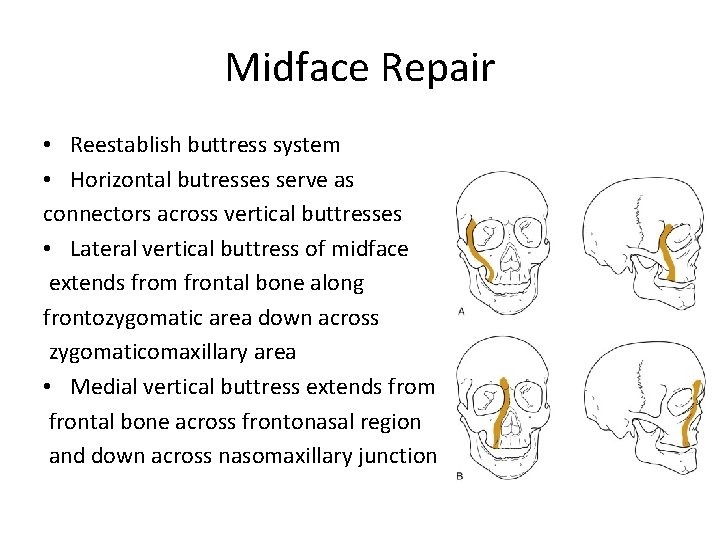
Midface Repair • Reestablish buttress system • Horizontal butresses serve as connectors across vertical buttresses • Lateral vertical buttress of midface extends from frontal bone along frontozygomatic area down across zygomaticomaxillary area • Medial vertical buttress extends from frontal bone across frontonasal region and down across nasomaxillary junction
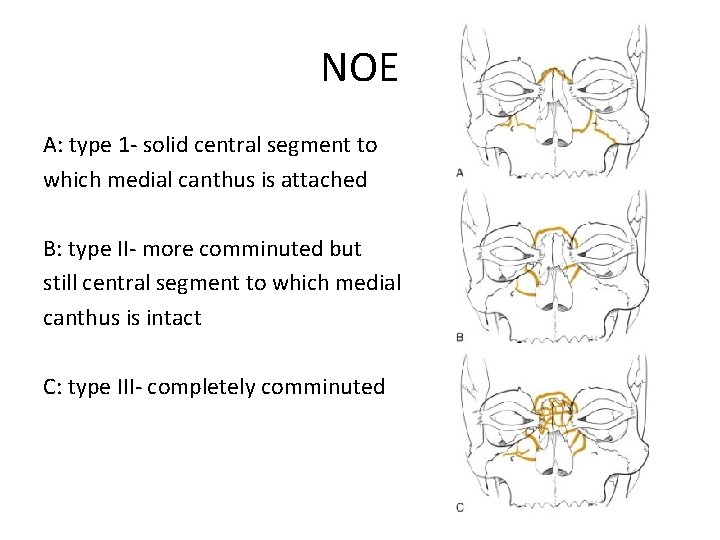
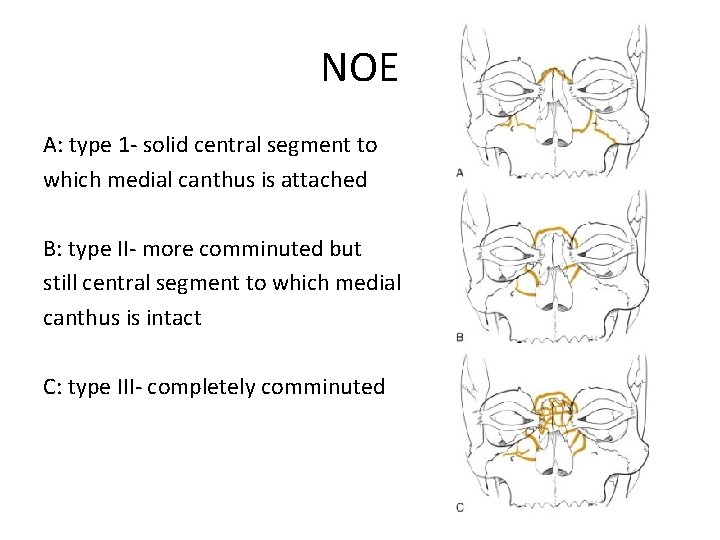
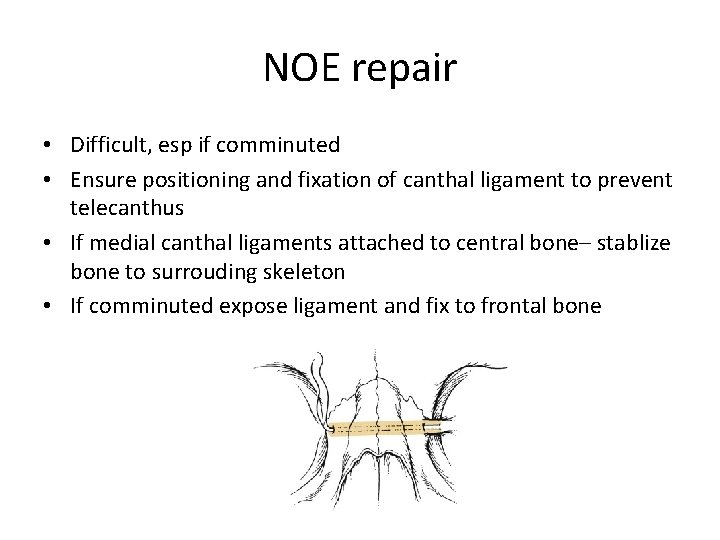
NOE A: type 1 - solid central segment to which medial canthus is attached B: type II- more comminuted but still central segment to which medial canthus is intact C: type III- completely comminuted
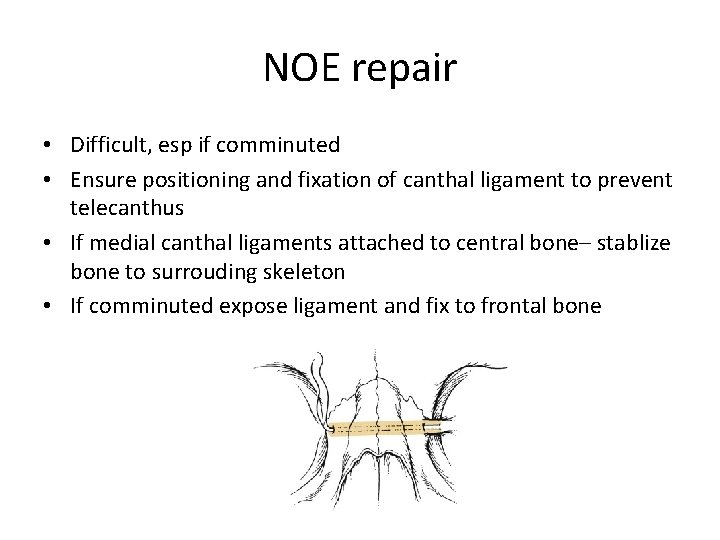
NOE repair • Difficult, esp if comminuted • Ensure positioning and fixation of canthal ligament to prevent telecanthus • If medial canthal ligaments attached to central bone– stablize bone to surrouding skeleton • If comminuted expose ligament and fix to frontal bone
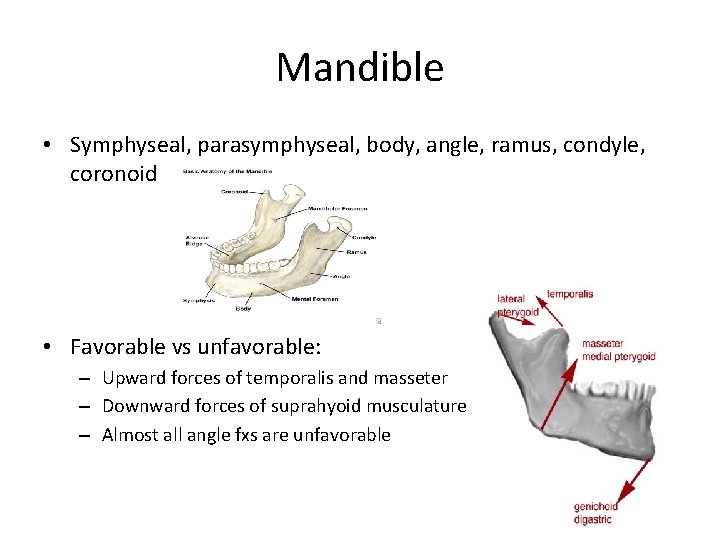
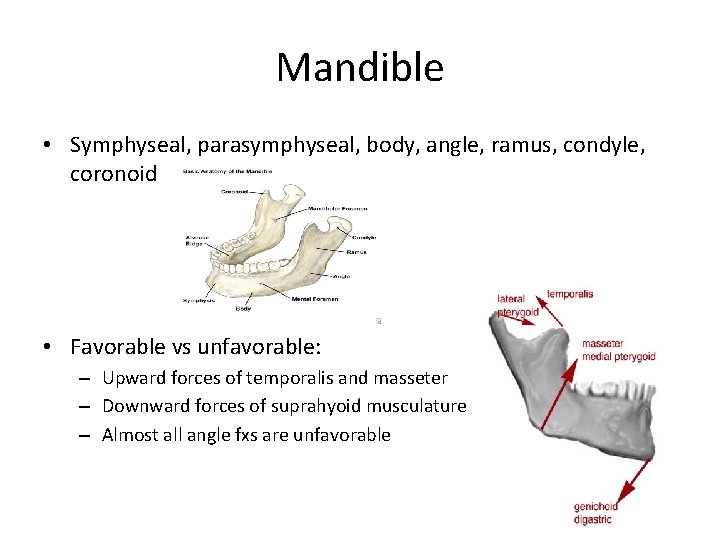
Mandible • Symphyseal, parasymphyseal, body, angle, ramus, condyle, coronoid • Favorable vs unfavorable: – Upward forces of temporalis and masseter – Downward forces of suprahyoid musculature – Almost all angle fxs are unfavorable
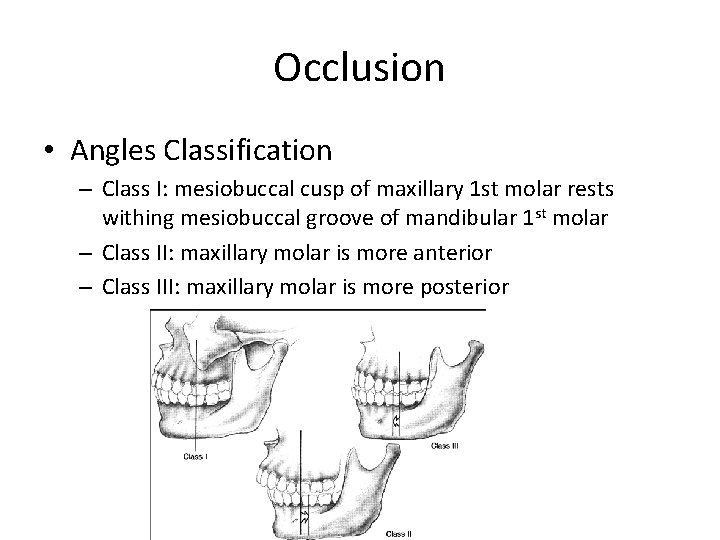
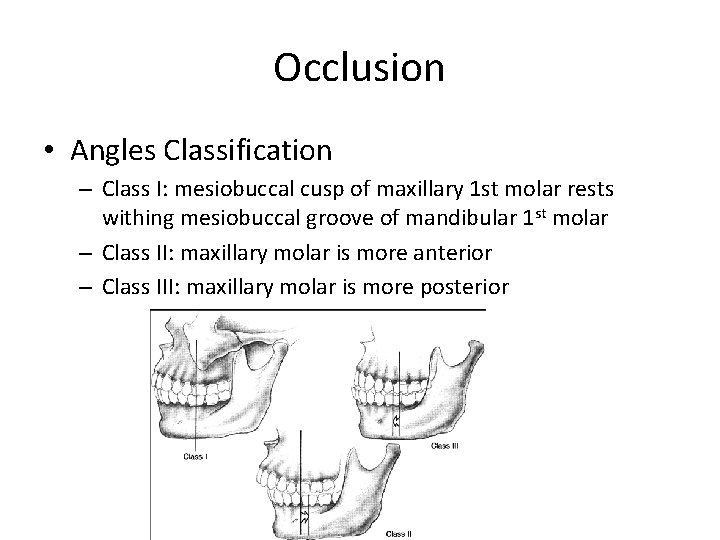
Occlusion • Angles Classification – Class I: mesiobuccal cusp of maxillary 1 st molar rests withing mesiobuccal groove of mandibular 1 st molar – Class II: maxillary molar is more anterior – Class III: maxillary molar is more posterior
Mandible Repair • Occlusion! • Plating if displaced, comminuted, unfavorable • Subcondylar fxs are controversial – MMF – Open reduction if condylar displacement into middle fossa, inability to obtain reduction, lateral extacapsular displacement of condyle, invasion by foreign body • Teeth in fracture line: pull if infected
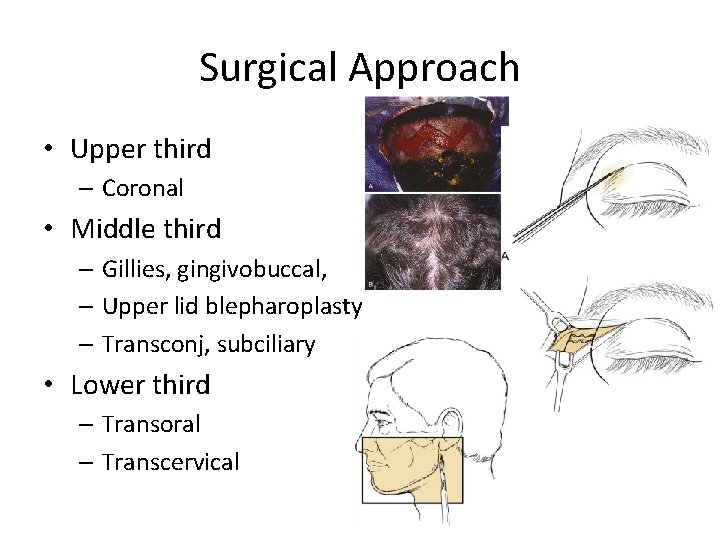
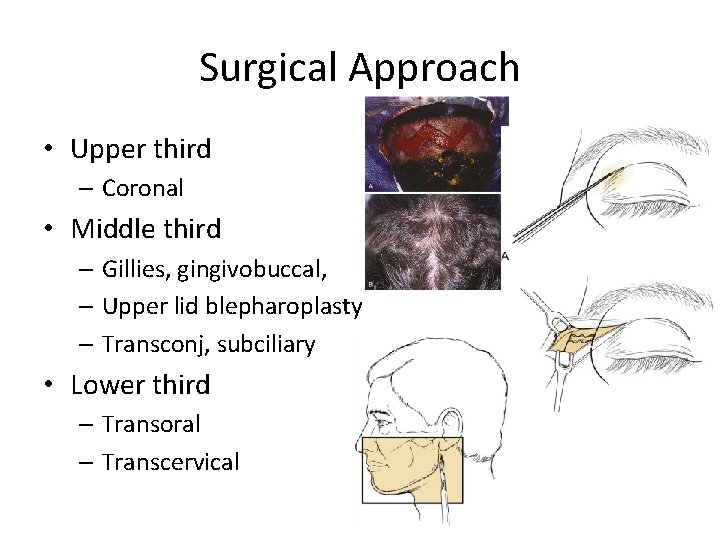
Surgical Approach • Upper third – Coronal • Middle third – Gillies, gingivobuccal, – Upper lid blepharoplasty – Transconj, subciliary • Lower third – Transoral – Transcervical
COCLIA • Review the Le. Fort Fracture levels • When would you obliterate a frontal sinus fracture and what would you use? • What are indications for opening a condyle fracture? • Discuss subciliary vs transconjunctival approach to orbital fractures. �
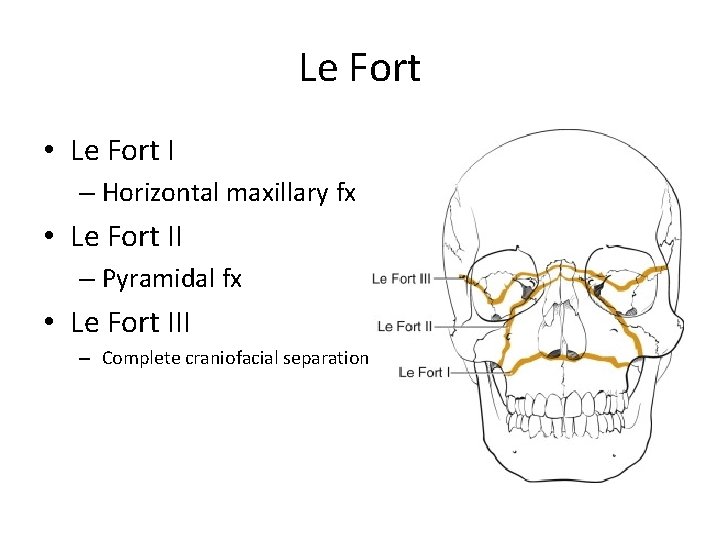
Le Fort • Le Fort I – Horizontal maxillary fx • Le Fort II – Pyramidal fx • Le Fort III – Complete craniofacial separation
• Frontal sinus fractures and obliteration are controversial • Posterior table displaced more than one table width • Very comminuted fractures • Persistant csf leak • Obliteration with fat, bone, pericranial fat
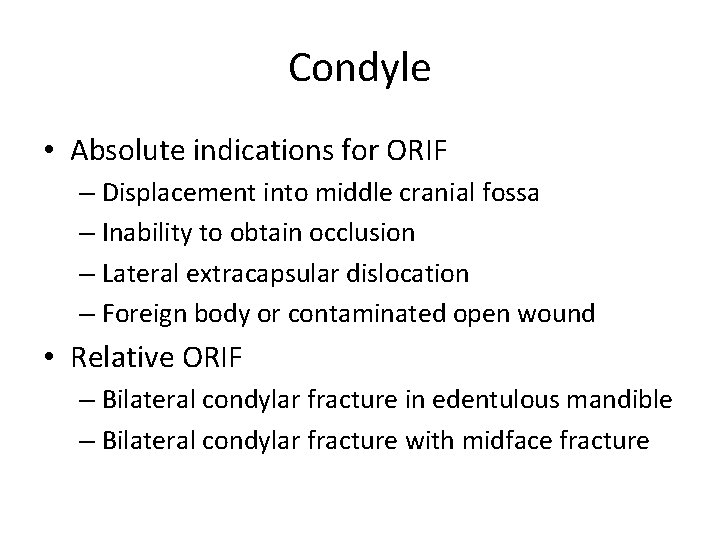
Condyle • Absolute indications for ORIF – Displacement into middle cranial fossa – Inability to obtain occlusion – Lateral extracapsular dislocation – Foreign body or contaminated open wound • Relative ORIF – Bilateral condylar fracture in edentulous mandible – Bilateral condylar fracture with midface fracture
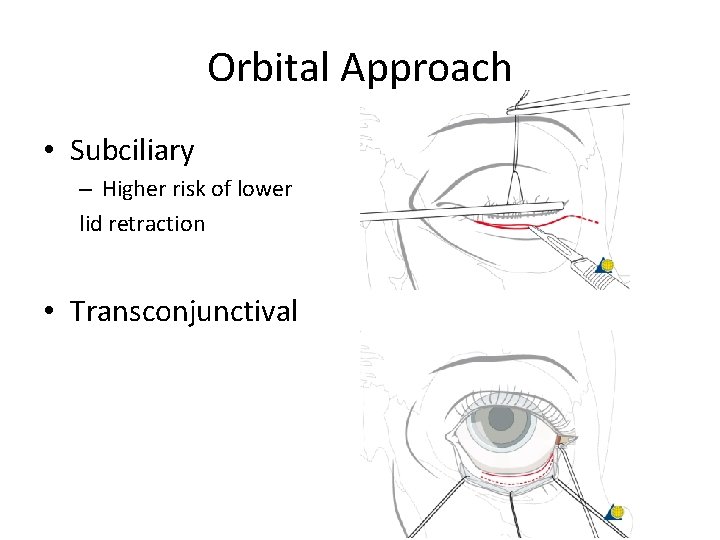
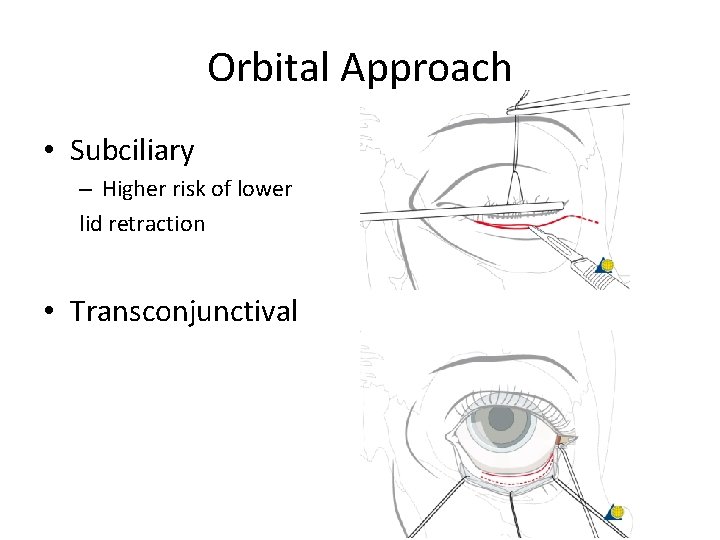
Orbital Approach • Subciliary – Higher risk of lower lid retraction • Transconjunctival
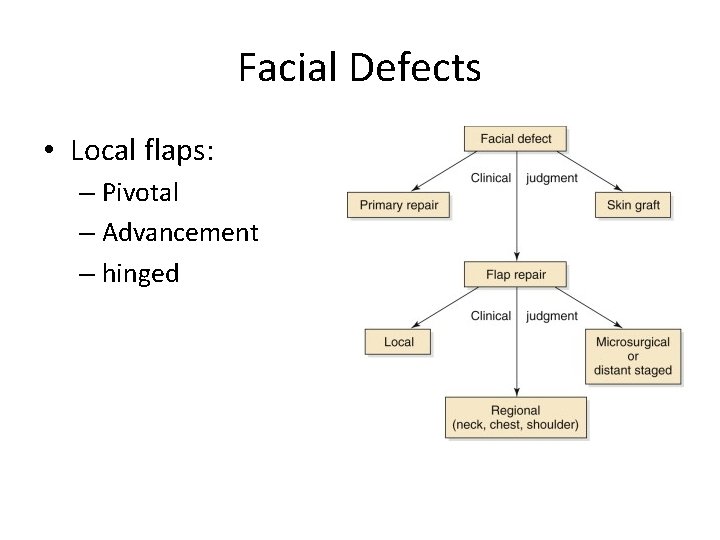
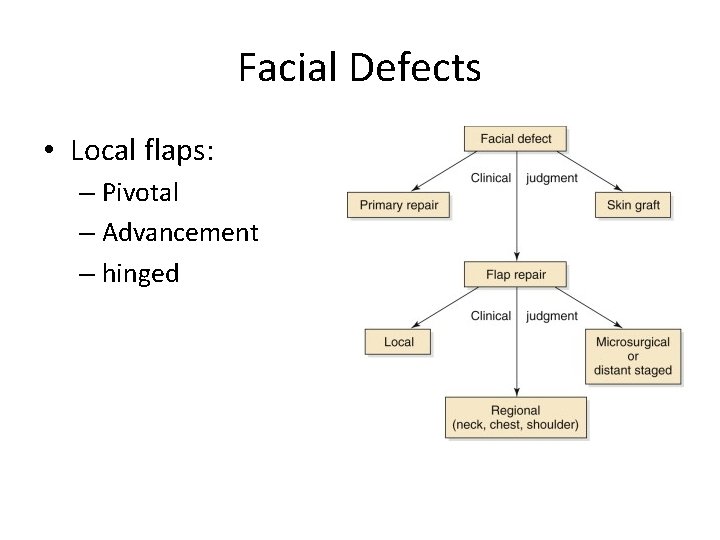
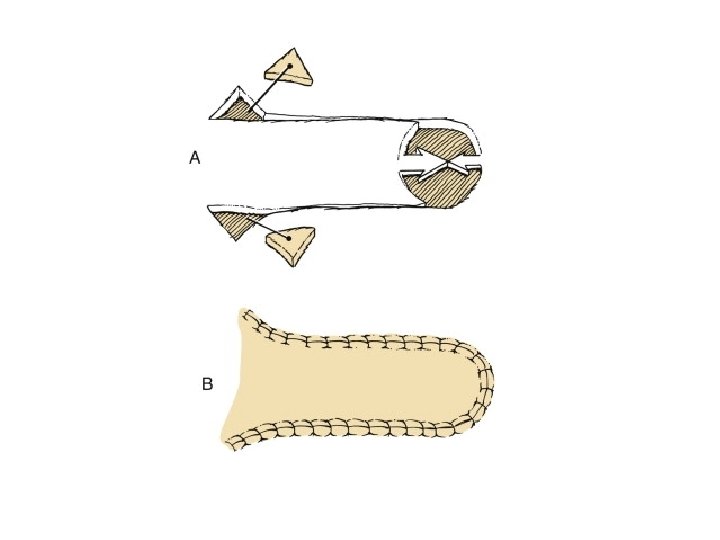
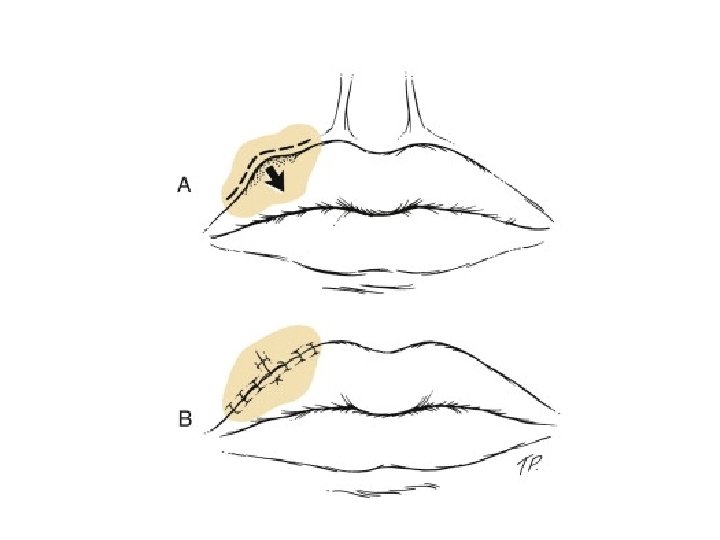
Facial Defects • Local flaps: – Pivotal – Advancement – hinged
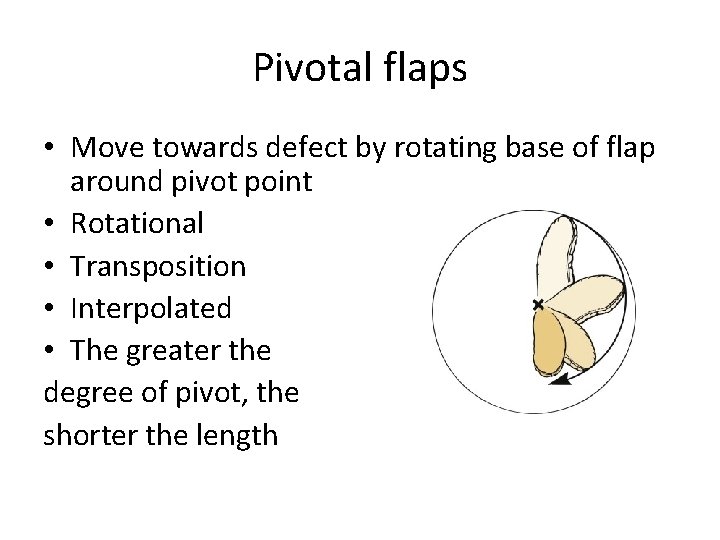
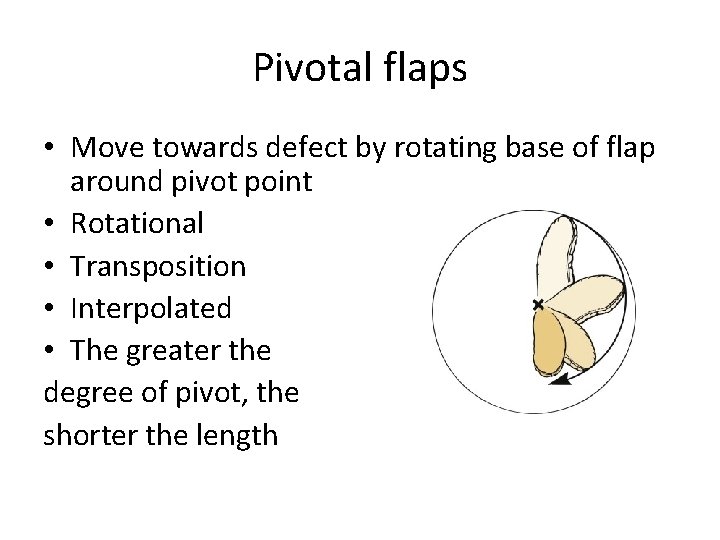
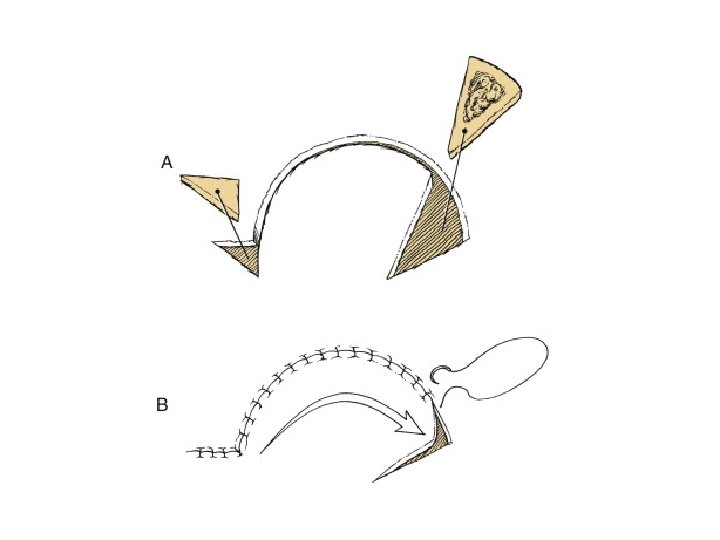
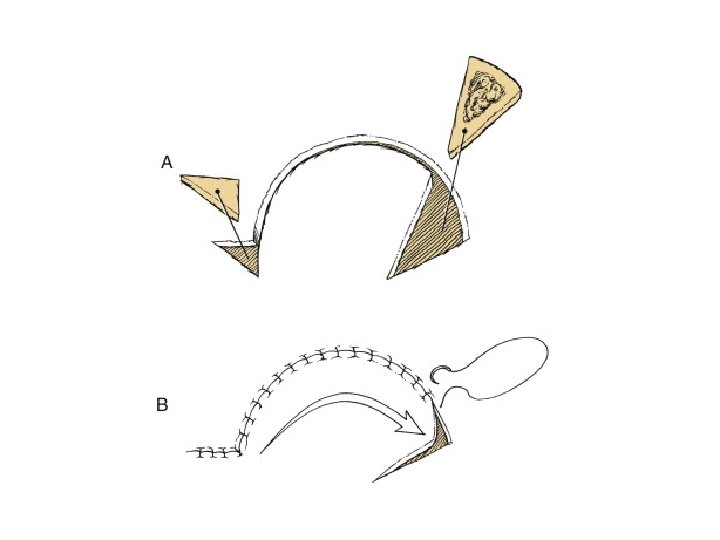
Pivotal flaps • Move towards defect by rotating base of flap around pivot point • Rotational • Transposition • Interpolated • The greater the degree of pivot, the shorter the length
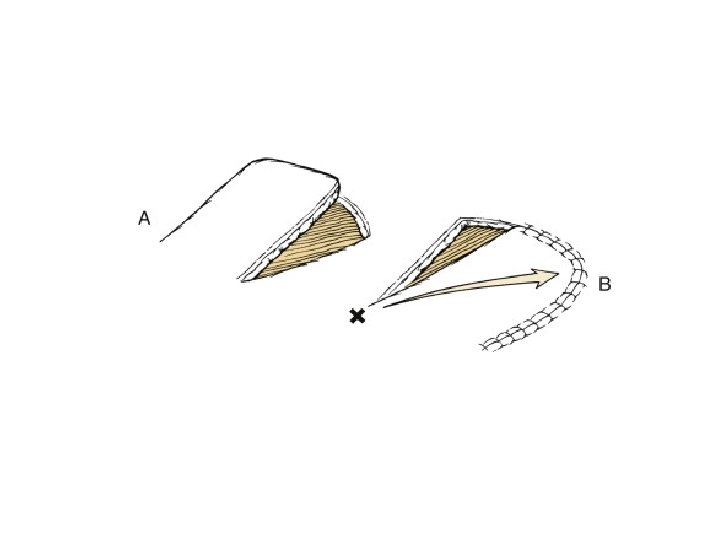
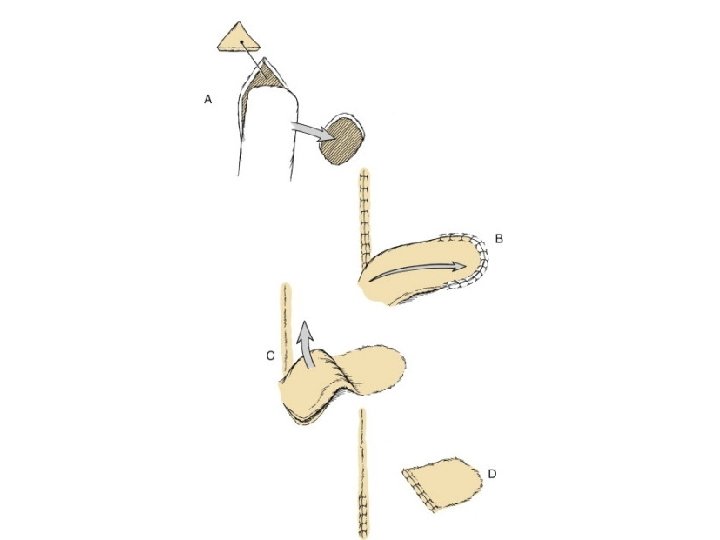
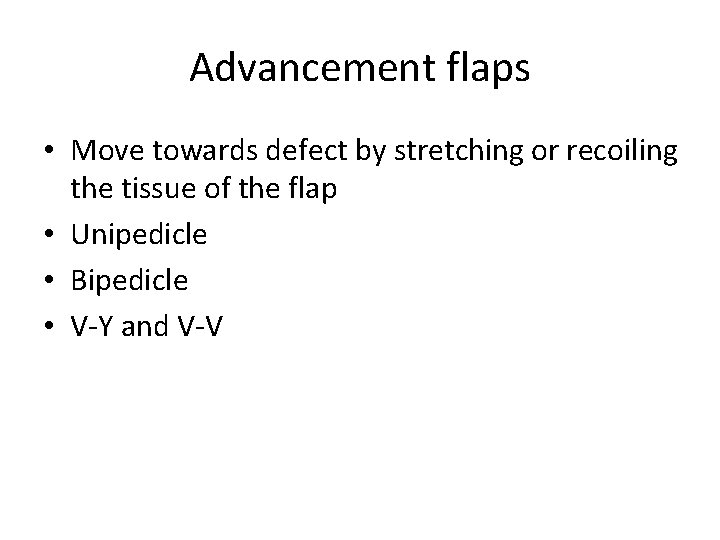
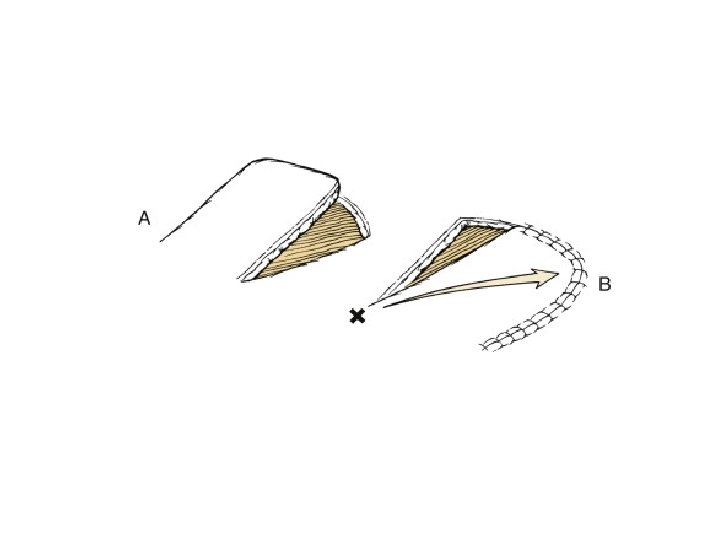
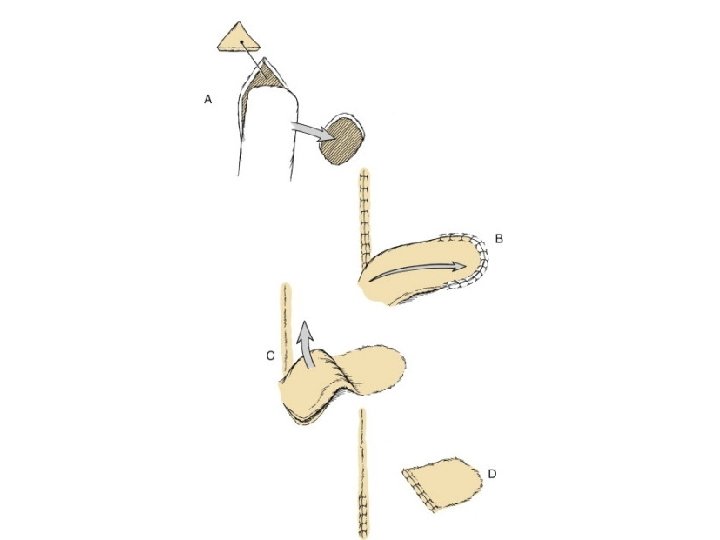
Advancement flaps • Move towards defect by stretching or recoiling the tissue of the flap • Unipedicle • Bipedicle • V-Y and V-V
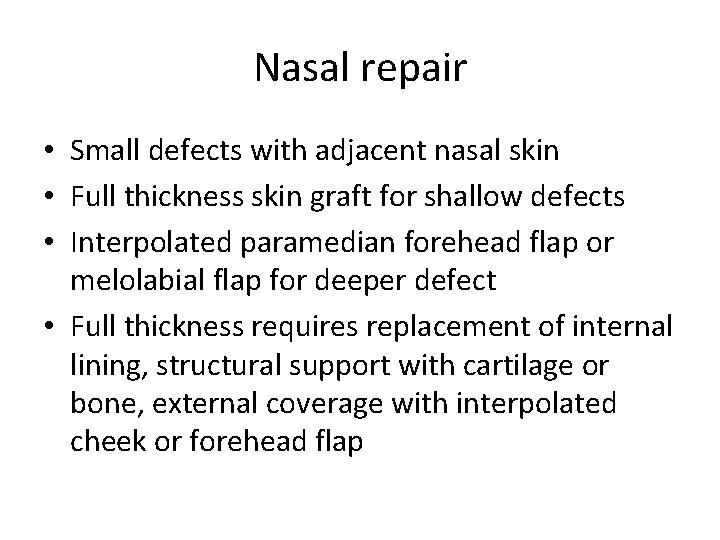
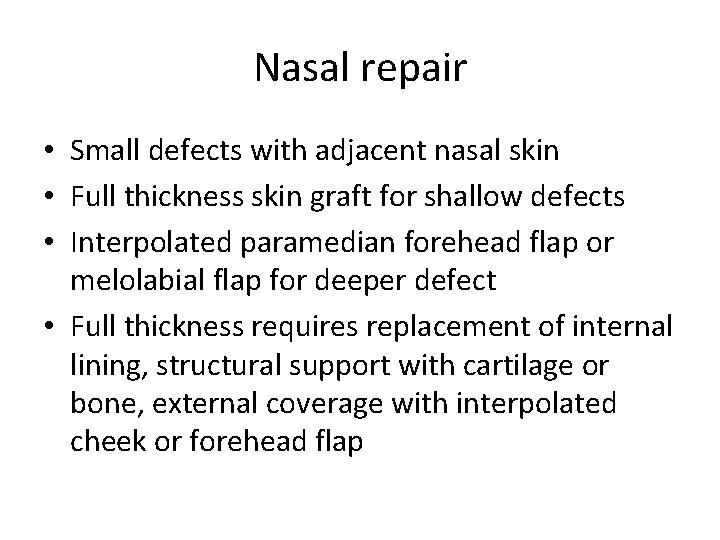
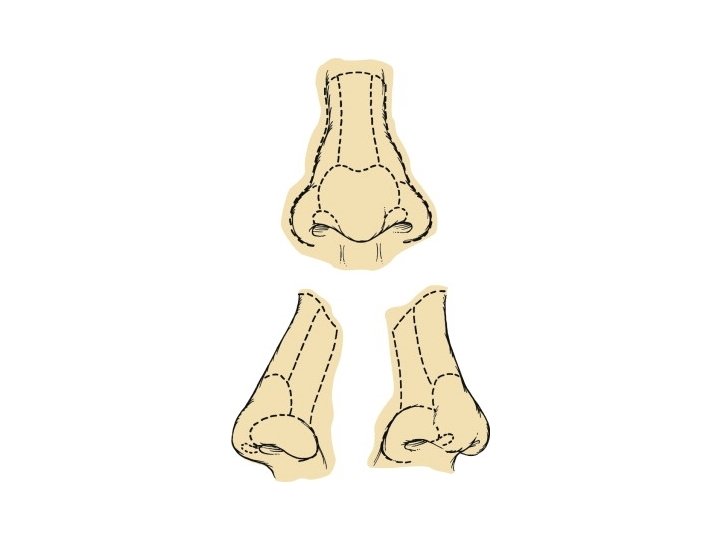
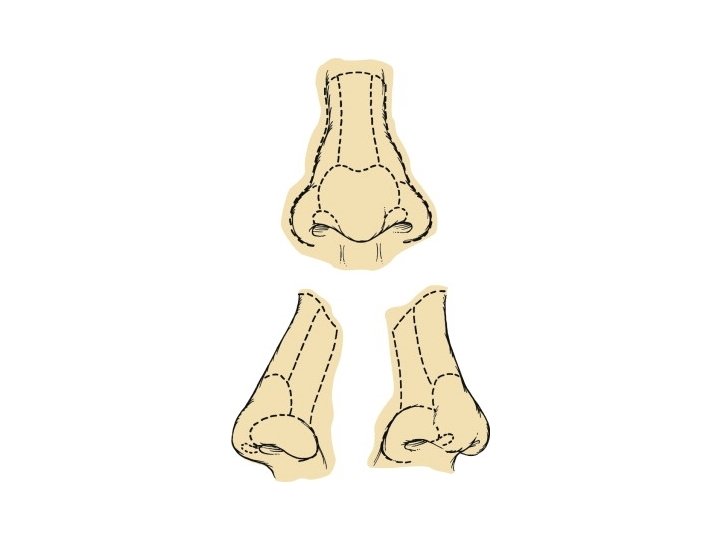
Nasal repair • Small defects with adjacent nasal skin • Full thickness skin graft for shallow defects • Interpolated paramedian forehead flap or melolabial flap for deeper defect • Full thickness requires replacement of internal lining, structural support with cartilage or bone, external coverage with interpolated cheek or forehead flap
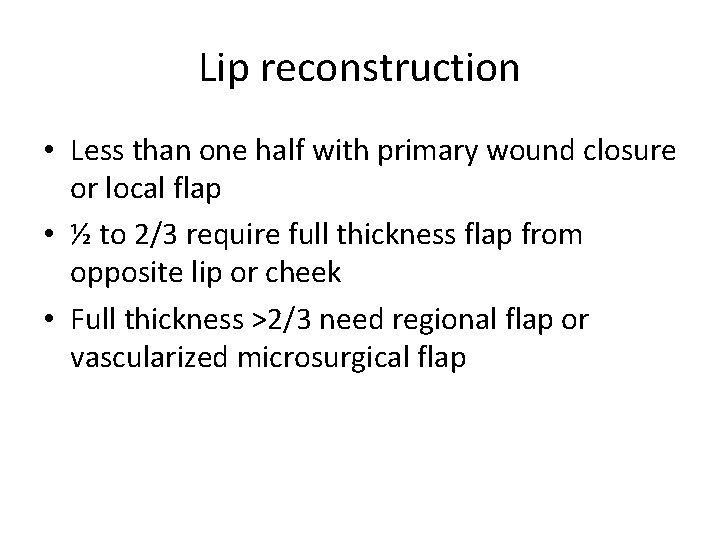
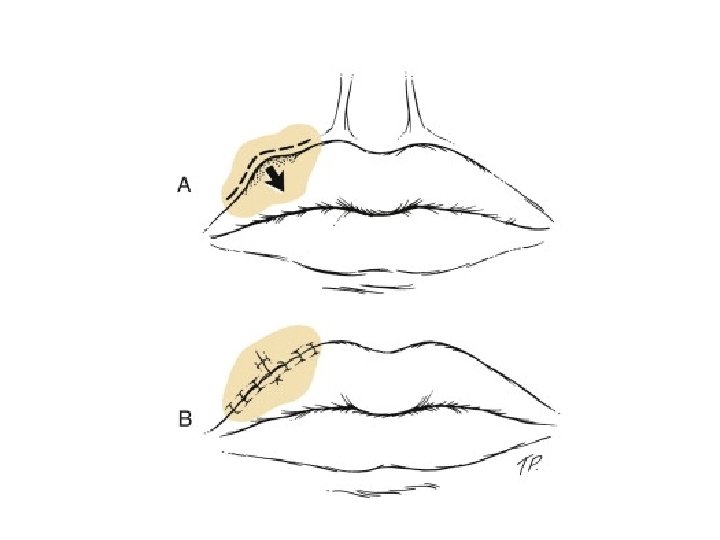
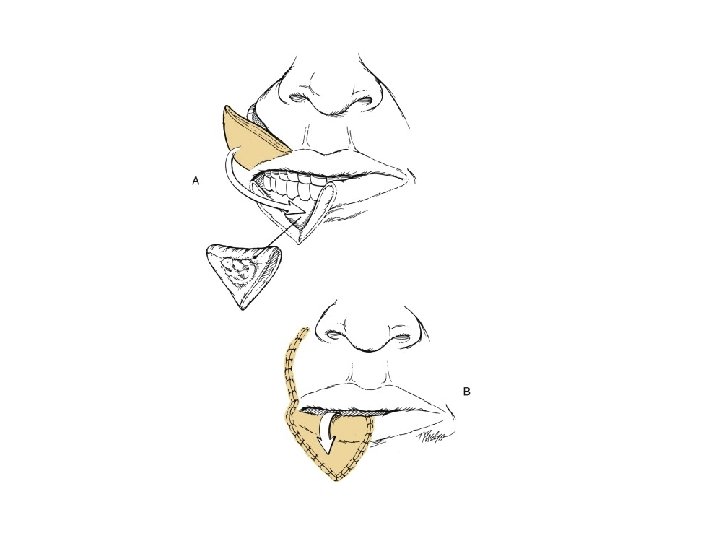
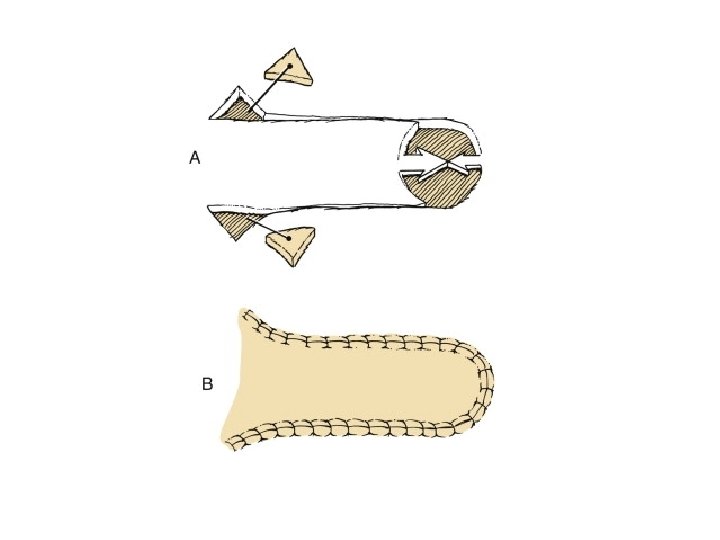
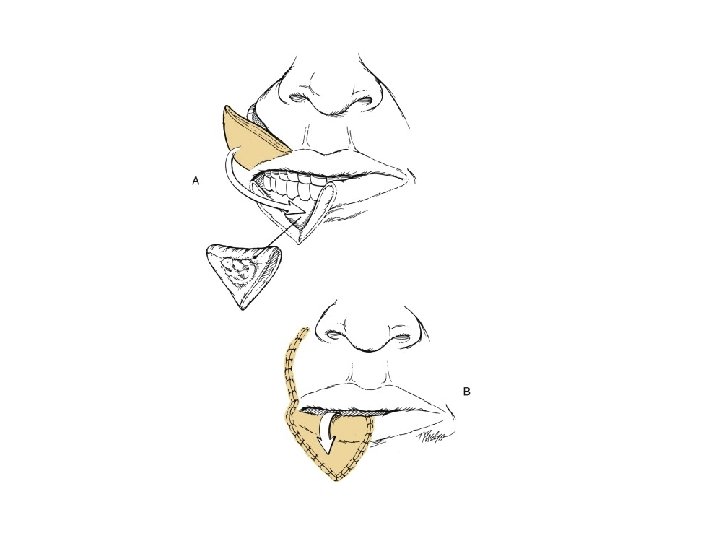
Lip reconstruction • Less than one half with primary wound closure or local flap • ½ to 2/3 require full thickness flap from opposite lip or cheek • Full thickness >2/3 need regional flap or vascularized microsurgical flap
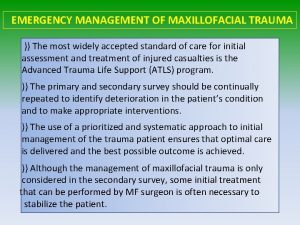
 Emergency management of maxillofacial trauma
Emergency management of maxillofacial trauma Facial trauma
Facial trauma Facial trauma
Facial trauma Inophthalmos
Inophthalmos Facial trauma
Facial trauma Facial vein and facial artery
Facial vein and facial artery Odontogenic inflammation
Odontogenic inflammation Chapter 26 oral and maxillofacial surgery
Chapter 26 oral and maxillofacial surgery Maxillofacial
Maxillofacial Shape of bone
Shape of bone Ch 56 oral and maxillofacial surgery
Ch 56 oral and maxillofacial surgery American academy of oral and maxillofacial radiology
American academy of oral and maxillofacial radiology Chapter 56 oral and maxillofacial surgery
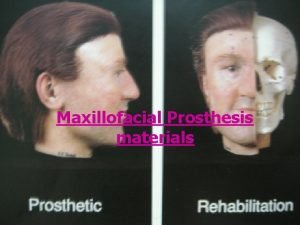
Chapter 56 oral and maxillofacial surgery Materials used in maxillofacial prosthesis
Materials used in maxillofacial prosthesis Maxillofacial
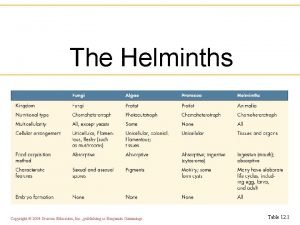
Maxillofacial 2004 pearson education inc. publishing as benjamin cummings
2004 pearson education inc. publishing as benjamin cummings Benjamin cummings
Benjamin cummings Modernist poetry
Modernist poetry Clint cummings
Clint cummings Cummings love is thicker than forget
Cummings love is thicker than forget Maddie cummings
Maddie cummings Pearson education publishing as benjamin cummings
Pearson education publishing as benjamin cummings Benjamin cummings
Benjamin cummings Benjamin cummings
Benjamin cummings Quickserve.cummins.com
Quickserve.cummins.com Pearson education, inc
Pearson education, inc Ee cummings somewhere i have never travelled
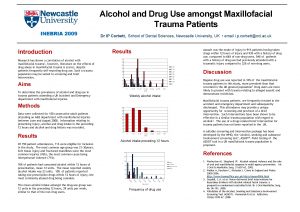
Ee cummings somewhere i have never travelled Cummings et al
Cummings et al Holly cummings
Holly cummings Cummings
Cummings Alma cummings dance marathon
Alma cummings dance marathon