Concepts of Continuous Renal Replacement Therapy in Adult

- Slides: 30
Concepts of Continuous Renal Replacement Therapy in Adult critical care at LTHT Including: Anticoagulation Prescribing Protocol
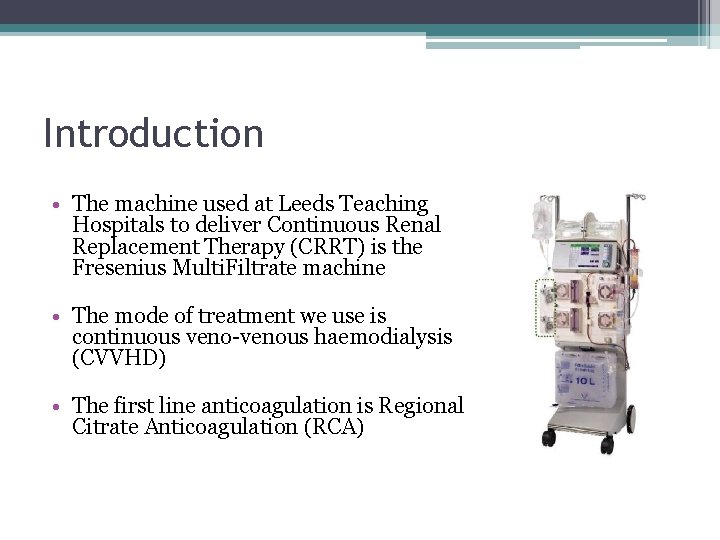
Introduction • The machine used at Leeds Teaching Hospitals to deliver Continuous Renal Replacement Therapy (CRRT) is the Fresenius Multi. Filtrate machine • The mode of treatment we use is continuous veno-venous haemodialysis (CVVHD) • The first line anticoagulation is Regional Citrate Anticoagulation (RCA)
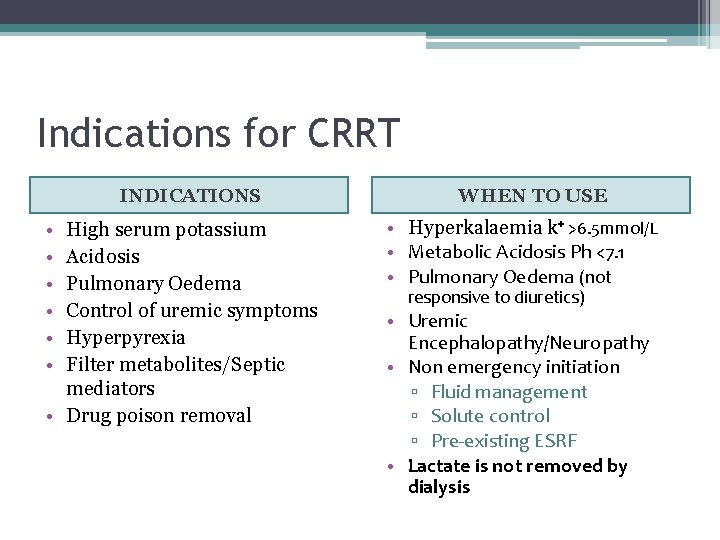
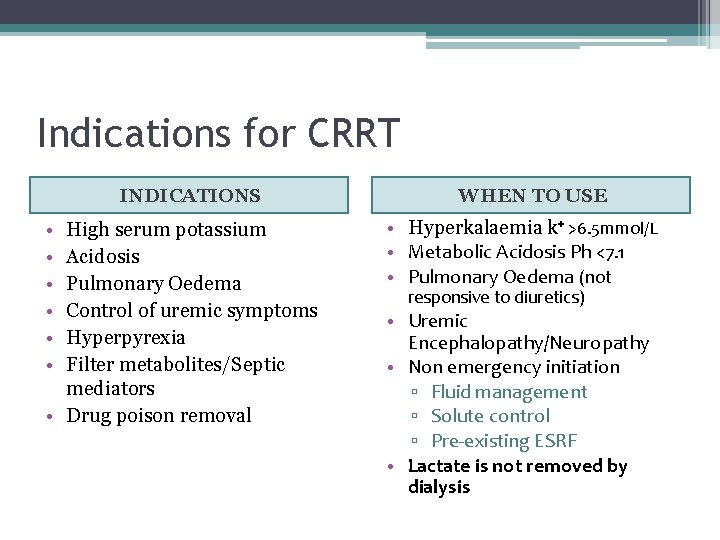
Indications for CRRT INDICATIONS • • • High serum potassium Acidosis Pulmonary Oedema Control of uremic symptoms Hyperpyrexia Filter metabolites/Septic mediators • Drug poison removal WHEN TO USE • Hyperkalaemia k⁺ >6. 5 mmol/L • Metabolic Acidosis Ph <7. 1 • Pulmonary Oedema (not responsive to diuretics) • Uremic Encephalopathy/Neuropathy • Non emergency initiation ▫ Fluid management ▫ Solute control ▫ Pre-existing ESRF • Lactate is not removed by dialysis
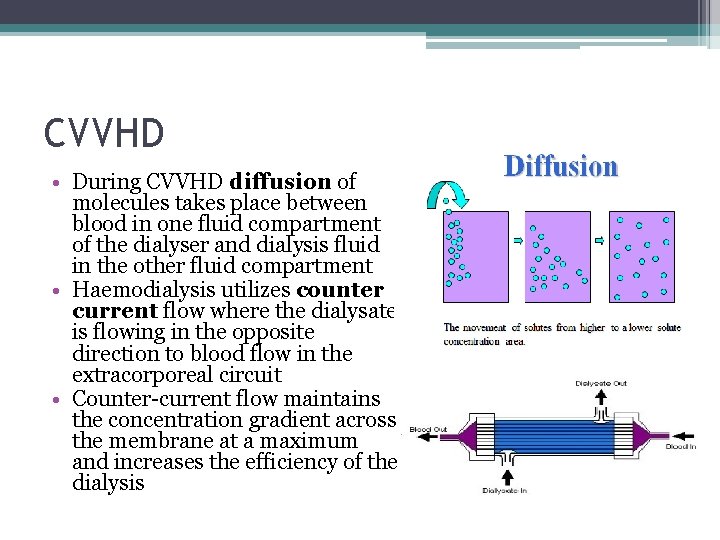
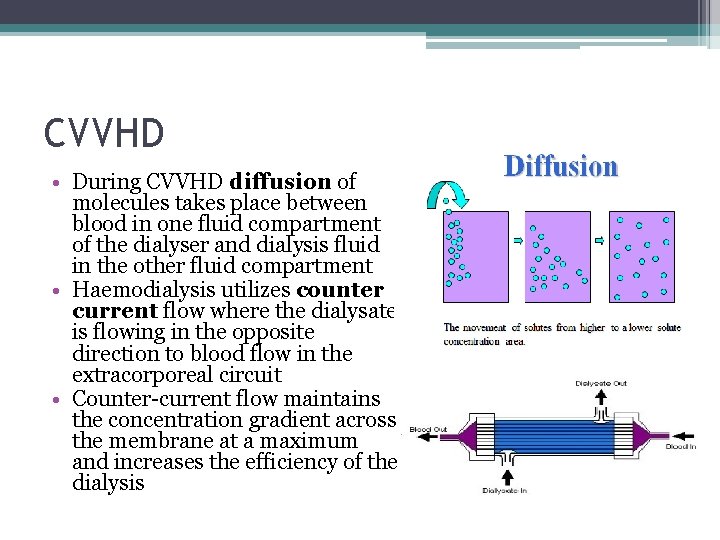
CVVHD • During CVVHD diffusion of molecules takes place between blood in one fluid compartment of the dialyser and dialysis fluid in the other fluid compartment • Haemodialysis utilizes counter current flow where the dialysate is flowing in the opposite direction to blood flow in the extracorporeal circuit • Counter-current flow maintains the concentration gradient across the membrane at a maximum and increases the efficiency of the dialysis
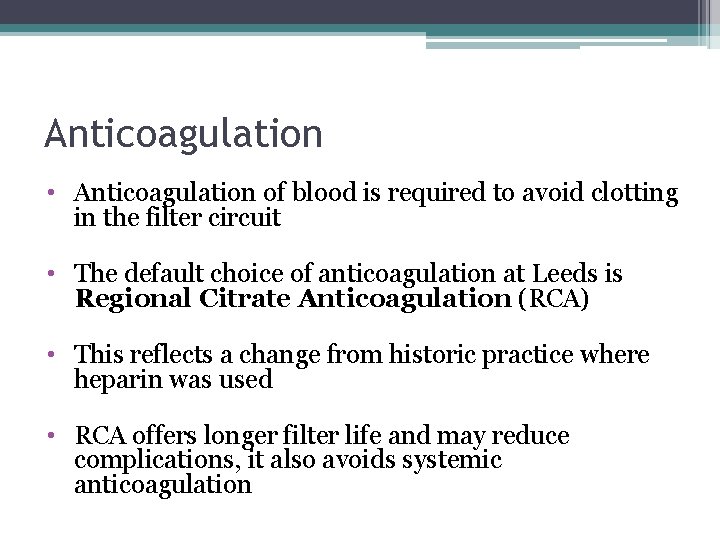
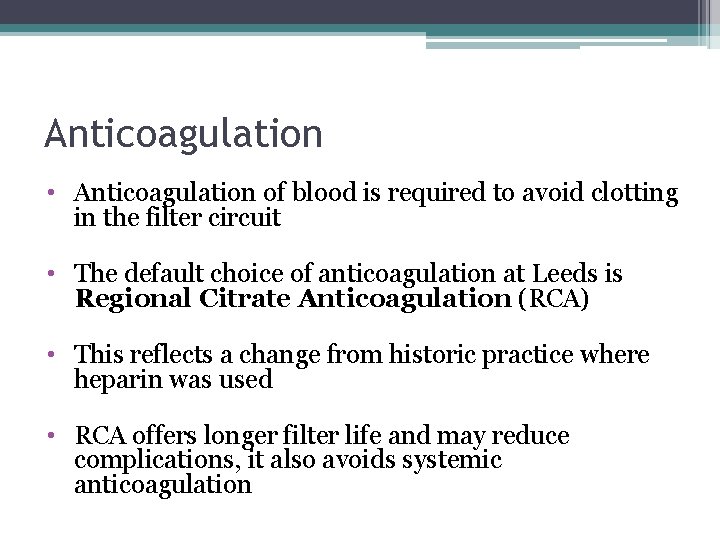
Anticoagulation • Anticoagulation of blood is required to avoid clotting in the filter circuit • The default choice of anticoagulation at Leeds is Regional Citrate Anticoagulation (RCA) • This reflects a change from historic practice where heparin was used • RCA offers longer filter life and may reduce complications, it also avoids systemic anticoagulation
Alternative anticoagulation options • Unfractionated heparin • None if INR >2. 5 and platelets <80 • Prostacycline used rarely
Regional Citrate Anticoagulation • • Negatively charged ion Binds with ionised calcium Forms a single negatively charged chelate complex Concentration of free ionised calcium in blood is reduced in the circuit • Ionised calcium is essential to the coagulation cascade – reducing it reduces clotting • Some of the citrate-calcium complex is removed by the filter and rest passes into patient where it is metabolised by the liver
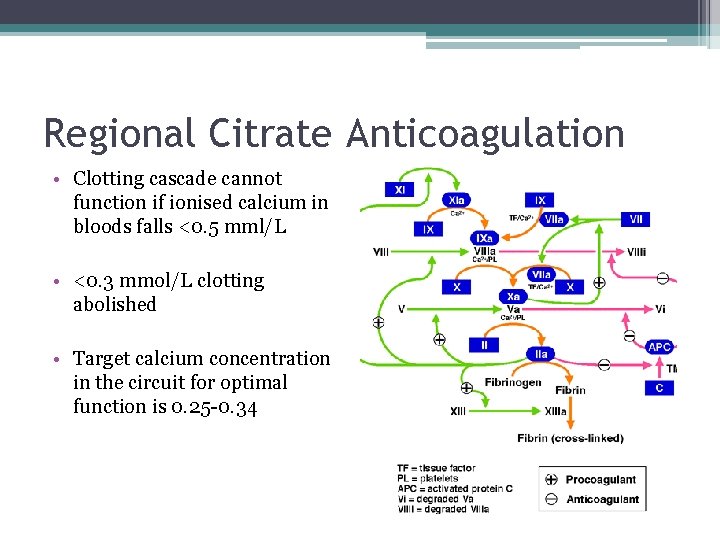
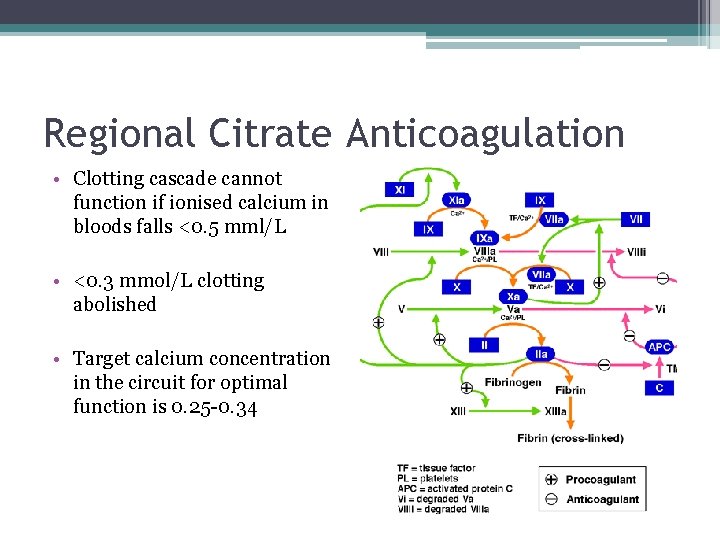
Regional Citrate Anticoagulation • Clotting cascade cannot function if ionised calcium in bloods falls <0. 5 mml/L • <0. 3 mmol/L clotting abolished • Target calcium concentration in the circuit for optimal function is 0. 25 -0. 34
Fresenius Multifiltrate • This is the machine used in Leeds • It can be used with RCA or heparin • Ci-Ca is the system for RCA • Multibic with heparin (separate protocol)
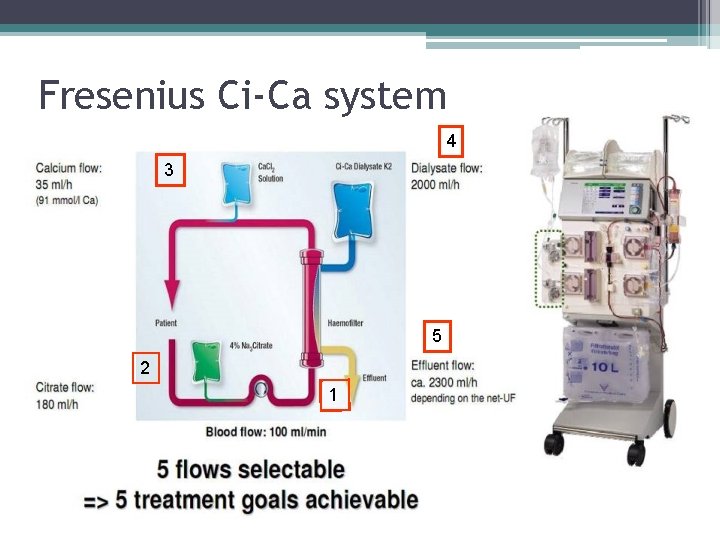
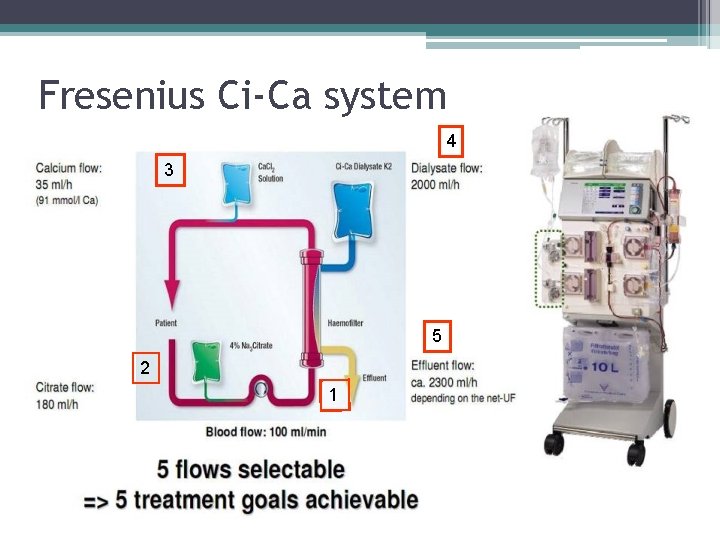
Fresenius Ci-Ca system 4 3 5 2 1
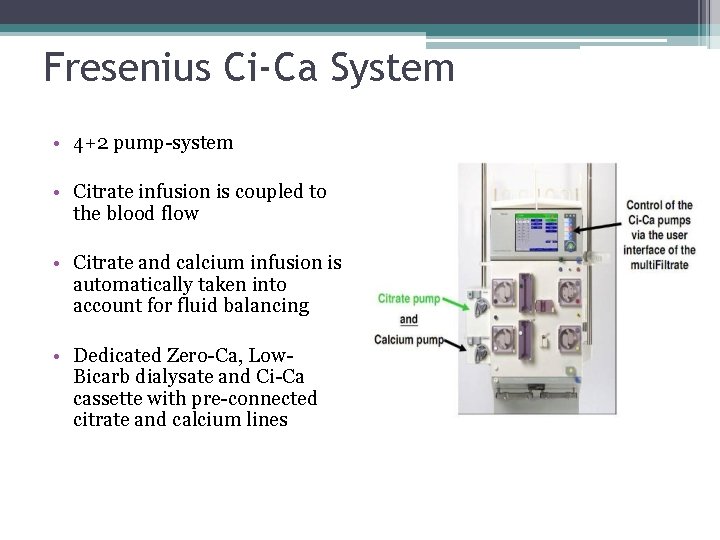
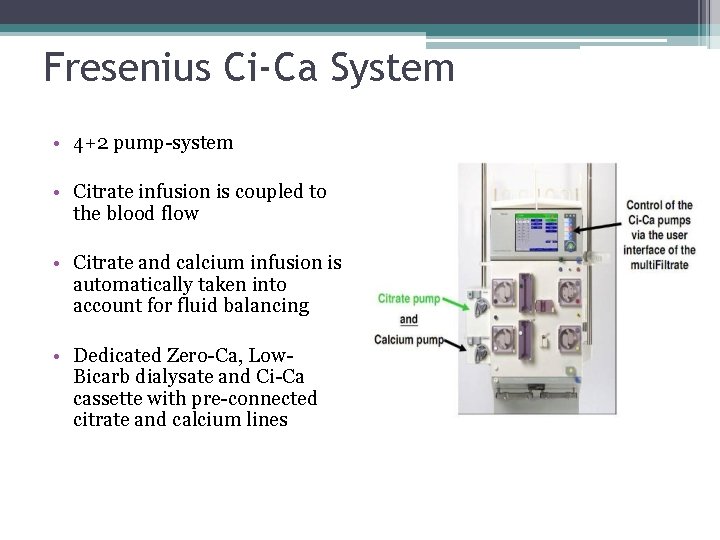
Fresenius Ci-Ca System • 4+2 pump-system • Citrate infusion is coupled to the blood flow • Citrate and calcium infusion is automatically taken into account for fluid balancing • Dedicated Zero-Ca, Low. Bicarb dialysate and Ci-Ca cassette with pre-connected citrate and calcium lines
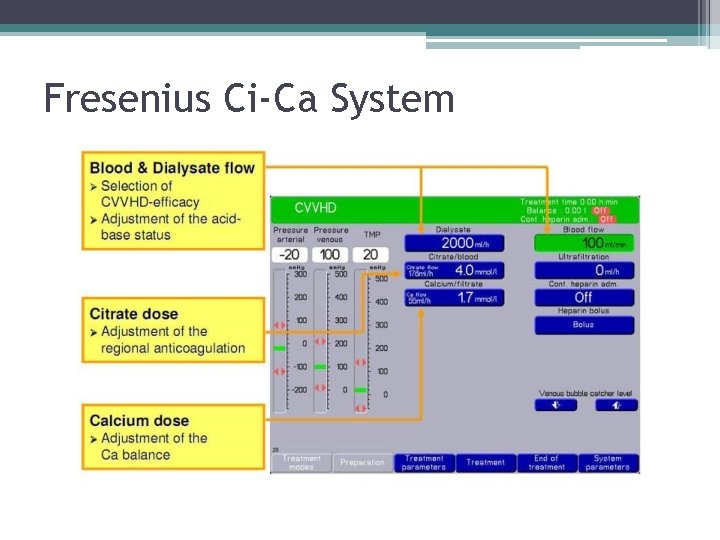
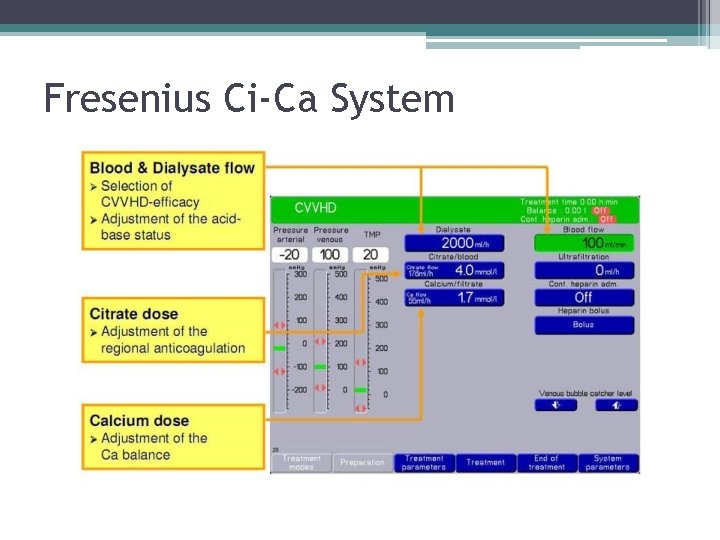
Fresenius Ci-Ca System
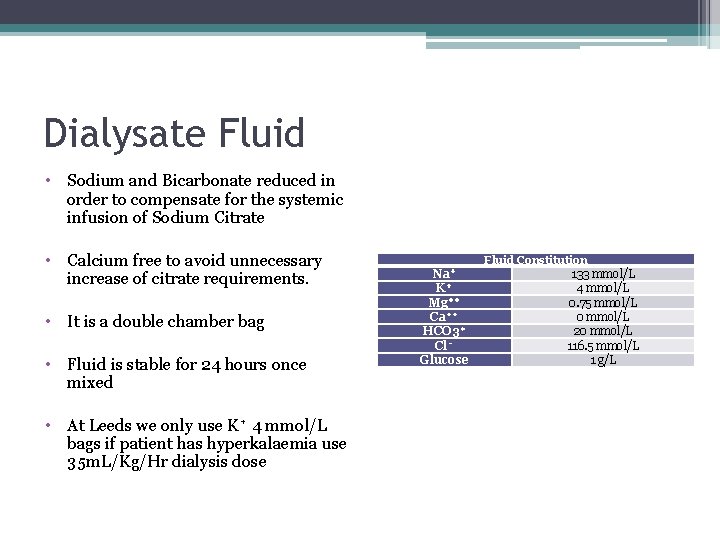
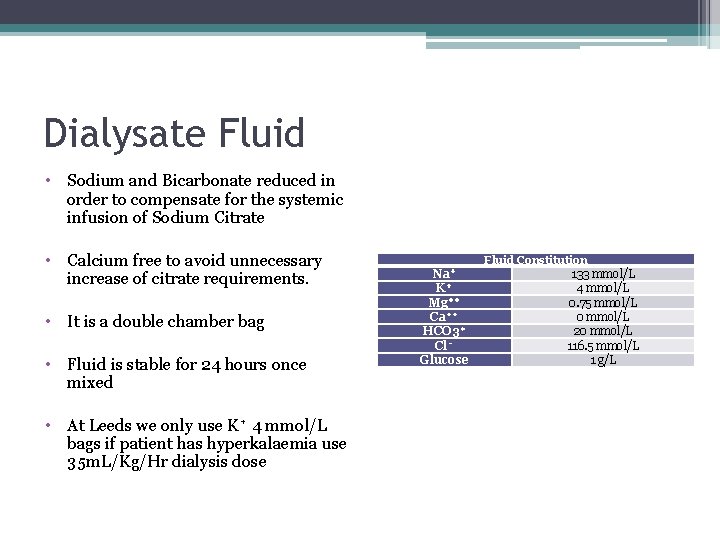
Dialysate Fluid • Sodium and Bicarbonate reduced in order to compensate for the systemic infusion of Sodium Citrate • Calcium free to avoid unnecessary increase of citrate requirements. • It is a double chamber bag • Fluid is stable for 24 hours once mixed • At Leeds we only use K⁺ 4 mmol/L bags if patient has hyperkalaemia use 35 m. L/Kg/Hr dialysis dose Fluid Constitution Na⁺ K⁺ Mg⁺⁺ Ca⁺⁺ HCO 3⁺ Cl⁻ Glucose 133 mmol/L 4 mmol/L 0. 75 mmol/L 0 mmol/L 20 mmol/L 116. 5 mmol/L 1 g/L
Core safety concepts • Protocol must be followed • Prescription must be written before patient connected to system and then daily • RCA interferes with normal calcium homeostasis maintain a safe serum ionised calcium level
Core safety concepts • Safety check via T: I ratio – this is the total: ionised calcium ratio and is a marker of citrate accumulation • RCA interferes with acid-base balance - be aware that the blood flow and dialysate flow need to be balanced (1: 20 ratio) to prevent iatrogenic acidosis or alkalosis • Liver patients may not tolerate RCA – separate guidance
Limits • Maximum treatment duration is 120 hours per filter • Washback, recirculation and disconnection circuit can be reconnected up to four hours • Recirculation with blood – circuit can be reconnected up to 30 mins
Dose choice • Dialysis dose can be chosen as 25 ml/kg/hr or 35 ml/kg/hr – weight based guidance charts in protocol • 25 is the default choice • 35 should be chosen in patients with: ▫ ▫ Severe hyperkalaemia (>7 mmol/l) Severe acidosis (p. H <7. 0) Ethylene glycol poisoning Inadequate treatment on 25 ml/kg/hr
Calcium Management • Refer to the protocol for guidance in calcium management • Around 60% of patients in critical care need to be pre-treated with calcium • Be mindful that in all patients the systemic ionised calcium will drop in the first 24 -48 hours, this is not a citrate accumulation unless the T: I ratio is > 2. 5 • Calcium management is the single most important factor of citrate anticoagulation
Fluid management • CRRT is a powerful tool for correcting fluid balance • Prescription should state a range of removal rates and a target fluid balance • Start the removal rate based upon current input and target balance and adjust in response to changes over the course of the day
Fluid management example • Hourly input total 50 ml (propofol/alfentanil/feed) ▫ 50 x 24=1200 • Anuric, no drains/loose stools etc • Target balance –ve 1000 ml/24 hours • Set initial removal at 100 ml/hr (approximated) ▫ 1200+1000=2200 ▫ 2200/24=92 • After 12 hours patient given 500 ml blood ▫ Balance, before blood, at 12 hours is -600 ml [(50 x 12)-(100 x 12)] ▫ After blood is -100 ml with 12 hours left, input still 50 ml/hr ▫ Aim remains -1000 ml • Set removal at 125 ml/hr ▫ -100 + (50 x 12) = +500 ▫ 500+1000=1500; 1500/12=125
Acid-Base Management • Citrate is metabolised in the liver • The by-product of citrate metabolism is bicarbonate • One molecule of citrate produces 3 molecules of bicarbonate • You require a prescription at a 20: 1 (dialysate flow: blood flow) ratio to maintain homeostasis • Any derangement in acid-base must be assessed to ascertain if it is a due to patient pathology or due to the RCA itself
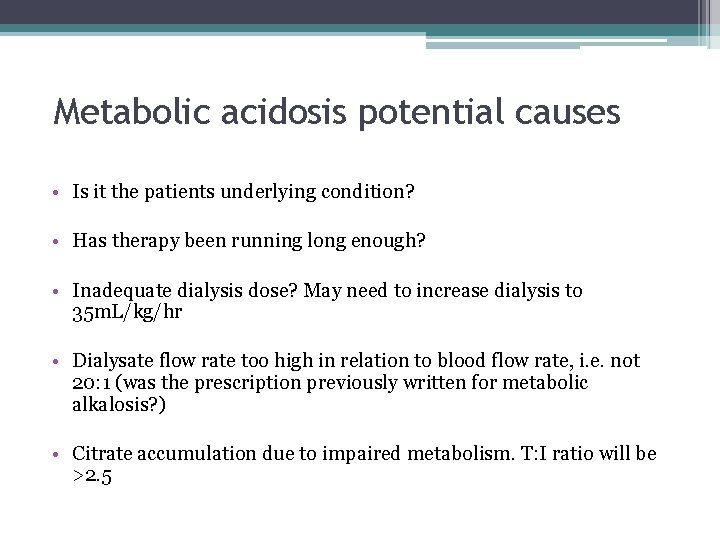
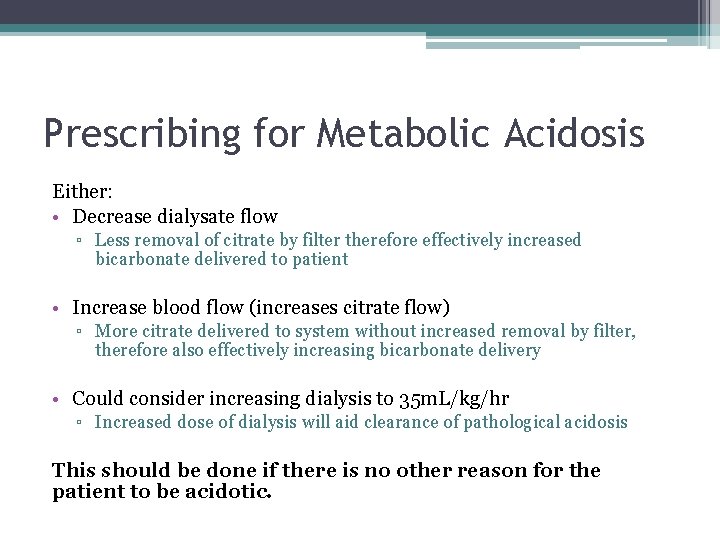
Metabolic acidosis potential causes • Is it the patients underlying condition? • Has therapy been running long enough? • Inadequate dialysis dose? May need to increase dialysis to 35 m. L/kg/hr • Dialysate flow rate too high in relation to blood flow rate, i. e. not 20: 1 (was the prescription previously written for metabolic alkalosis? ) • Citrate accumulation due to impaired metabolism. T: I ratio will be >2. 5
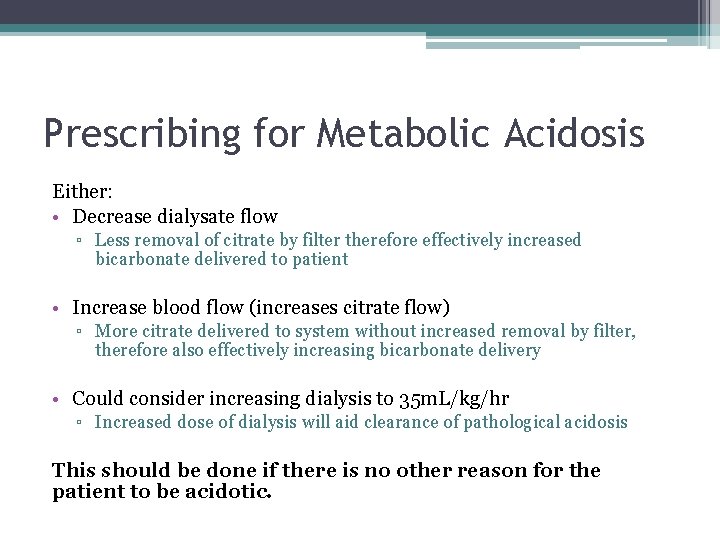
Prescribing for Metabolic Acidosis Either: • Decrease dialysate flow ▫ Less removal of citrate by filter therefore effectively increased bicarbonate delivered to patient • Increase blood flow (increases citrate flow) ▫ More citrate delivered to system without increased removal by filter, therefore also effectively increasing bicarbonate delivery • Could consider increasing dialysis to 35 m. L/kg/hr ▫ Increased dose of dialysis will aid clearance of pathological acidosis This should be done if there is no other reason for the patient to be acidotic.
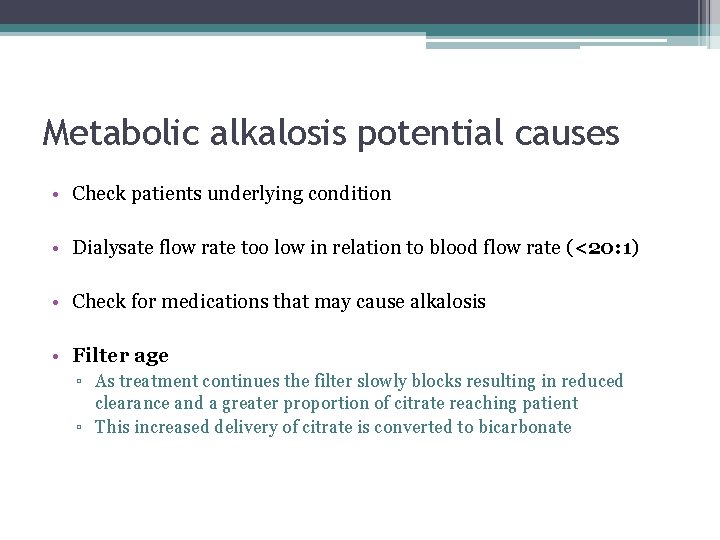
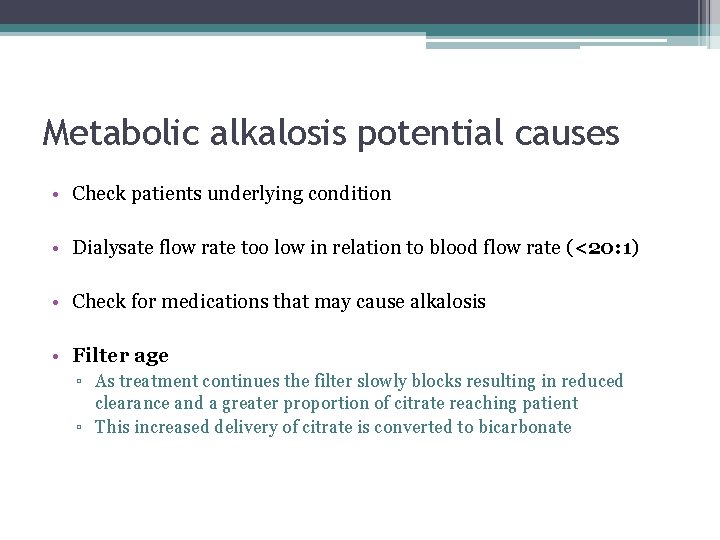
Metabolic alkalosis potential causes • Check patients underlying condition • Dialysate flow rate too low in relation to blood flow rate (<20: 1) • Check for medications that may cause alkalosis • Filter age ▫ As treatment continues the filter slowly blocks resulting in reduced clearance and a greater proportion of citrate reaching patient ▫ This increased delivery of citrate is converted to bicarbonate
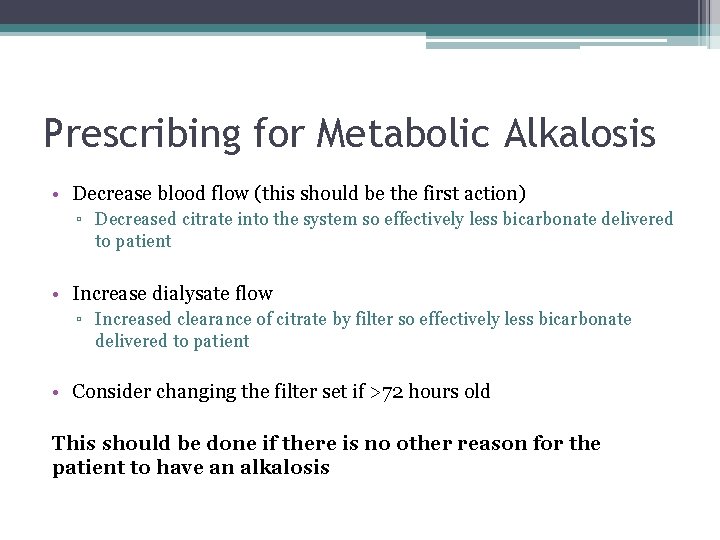
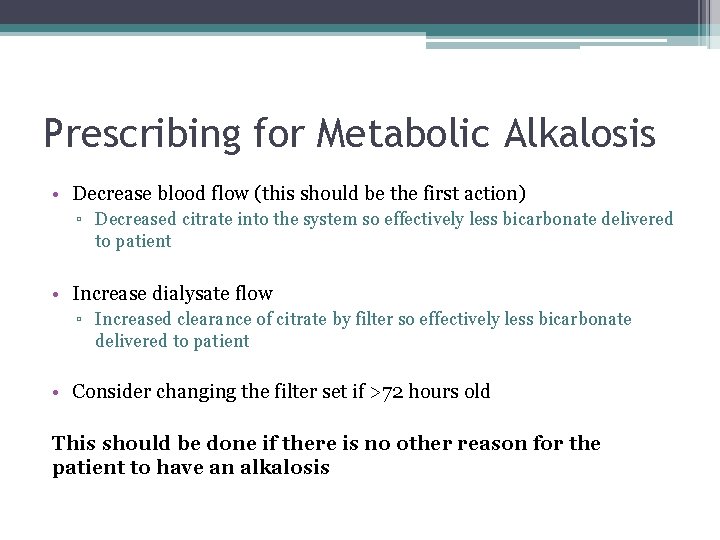
Prescribing for Metabolic Alkalosis • Decrease blood flow (this should be the first action) ▫ Decreased citrate into the system so effectively less bicarbonate delivered to patient • Increase dialysate flow ▫ Increased clearance of citrate by filter so effectively less bicarbonate delivered to patient • Consider changing the filter set if >72 hours old This should be done if there is no other reason for the patient to have an alkalosis
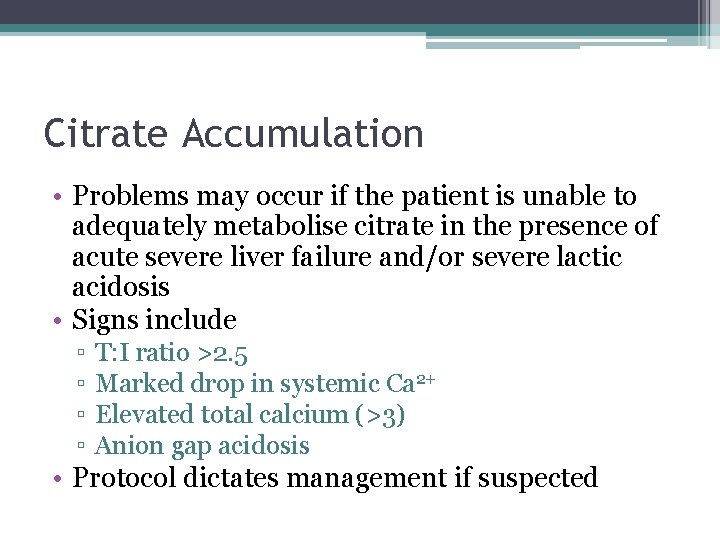
Citrate Accumulation • Problems may occur if the patient is unable to adequately metabolise citrate in the presence of acute severe liver failure and/or severe lactic acidosis • Signs include ▫ ▫ T: I ratio >2. 5 Marked drop in systemic Ca 2+ Elevated total calcium (>3) Anion gap acidosis • Protocol dictates management if suspected

Liver Patients • Altered protocol if lactate >8 and total to ionised (TI) calcium ratio >2 ▫ Always pretreat with calcium ▫ Increased initial calcium flow rates • At increased risk of citrate accumulation. Vigilance required
Summary • Main indications for CRRT are hyperkalaemia, acidosis or fluid overload • Anticoagulation is usually with citrate which works by binding to ionised calcium which prevents activation of the clotting cascade • You must monitor and control patients and filters Ca 2+ levels • Fluid balance targets must be adhered to • Be aware that the system can both cause and correct an acid-base imbalance • T: I ratio is an essential safety check – risk of citrate accumulation
Points of contact • Charlotte Trumper – Clinical Nurse Specialist • James Beck – ICM Consultant • Andy Lewington – Renal Consultant
 Res extra commercium
Res extra commercium Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Rrt aeiou
Rrt aeiou Vasa recta vs peritubular capillaries
Vasa recta vs peritubular capillaries Combustion equation
Combustion equation Occupational therapy hip replacement interventions
Occupational therapy hip replacement interventions 18004149025
18004149025 Electrolyte replacement therapy
Electrolyte replacement therapy Future past progressive
Future past progressive Past simple future
Past simple future Psychoanalytic vs humanistic
Psychoanalytic vs humanistic Bioness integrated therapy system price
Bioness integrated therapy system price Humanistic therapies aim to boost
Humanistic therapies aim to boost Feminist therapy key concepts
Feminist therapy key concepts Milton erickson
Milton erickson Aorta zone
Aorta zone Anna neary
Anna neary Pathophysiology of kidney stones
Pathophysiology of kidney stones Peritubular capillaries
Peritubular capillaries Epitheleal
Epitheleal Universidad del zulia facultad de medicina
Universidad del zulia facultad de medicina Renal cell carcinoma
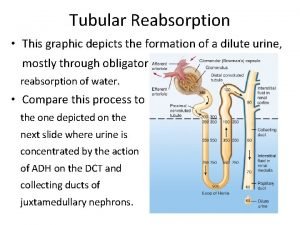
Renal cell carcinoma Where is water reabsorbed in the nephron
Where is water reabsorbed in the nephron Lamivudine renal dose
Lamivudine renal dose Vasa recta vs peritubular capillaries
Vasa recta vs peritubular capillaries Earthy look in chronic renal failure
Earthy look in chronic renal failure Palpación monomanual
Palpación monomanual Secondary hyperparathyroidism of renal origin
Secondary hyperparathyroidism of renal origin Creatinine clearance formula
Creatinine clearance formula Clearance equation renal
Clearance equation renal Renal
Renal