Renal Failure Renal replacement therapy ChihKang Chiang MD


- Slides: 61
Renal Failure: Renal replacement therapy Chih-Kang Chiang MD. Ph. D 姜至剛教授 20180409 16: 30~17: 20 國防醫學院 2教室
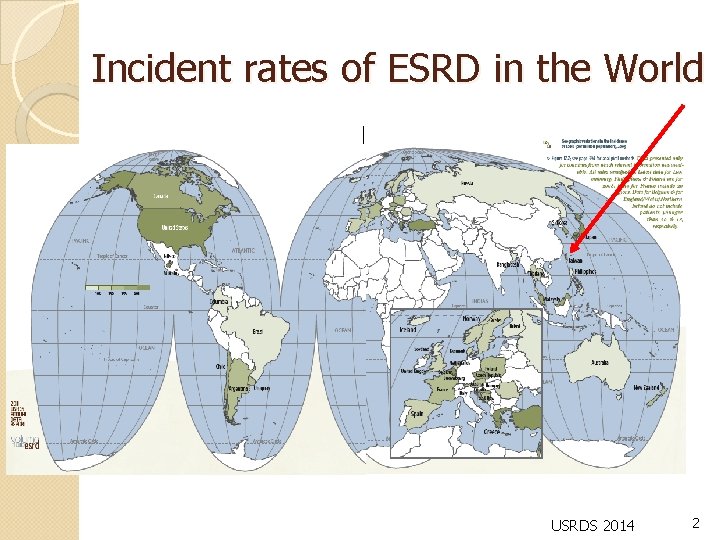
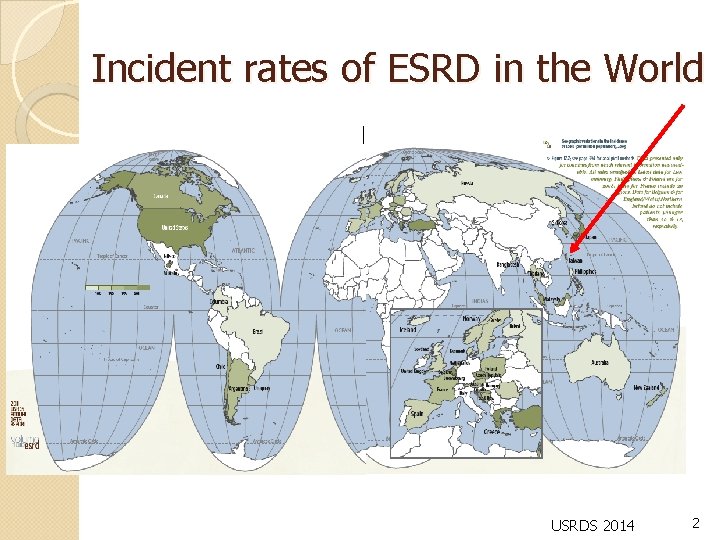
Incident rates of ESRD in the World USRDS 2014 2
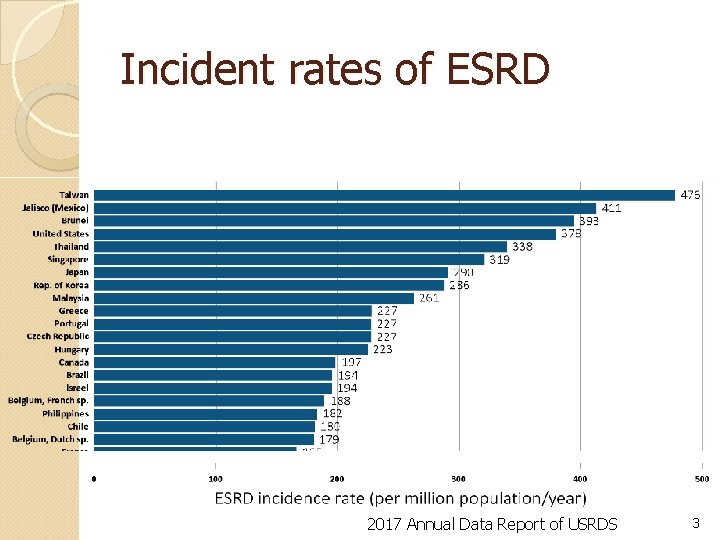
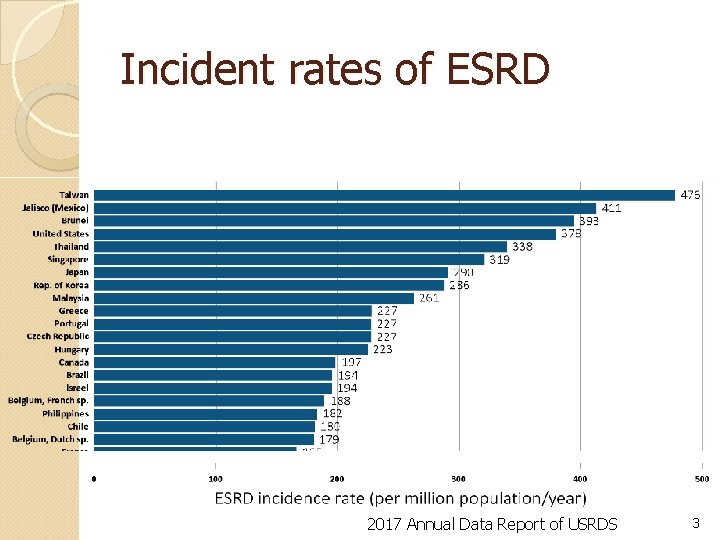
Incident rates of ESRD 2017 Annual Data Report of USRDS 3
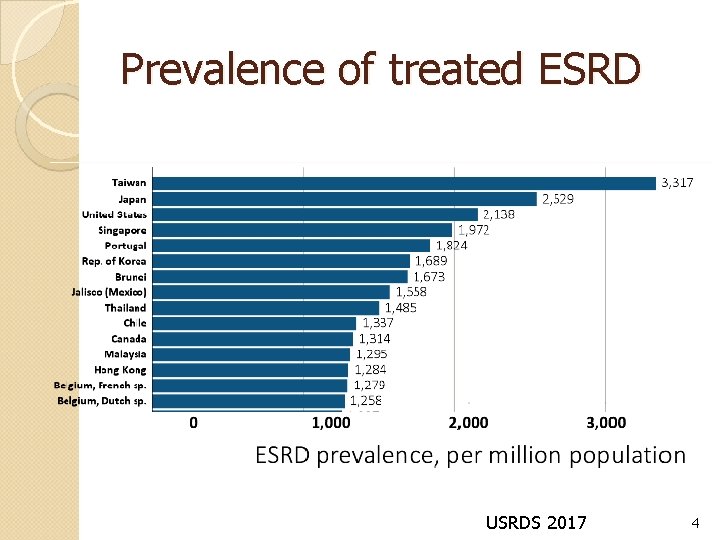
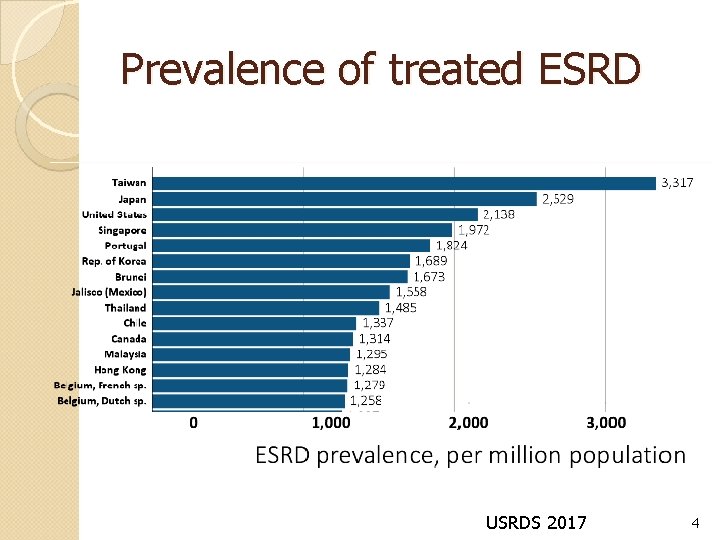
Prevalence of treated ESRD USRDS 2017 4
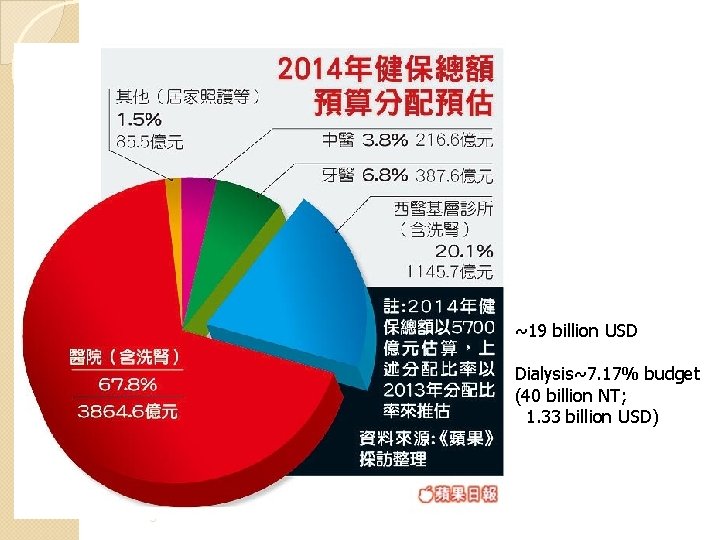
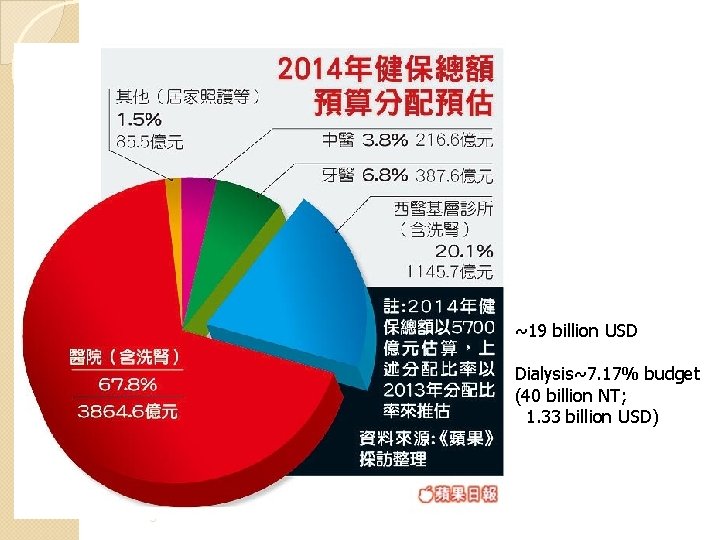
~19 billion USD Dialysis~7. 17% budget (40 billion NT; 1. 33 billion USD) 5
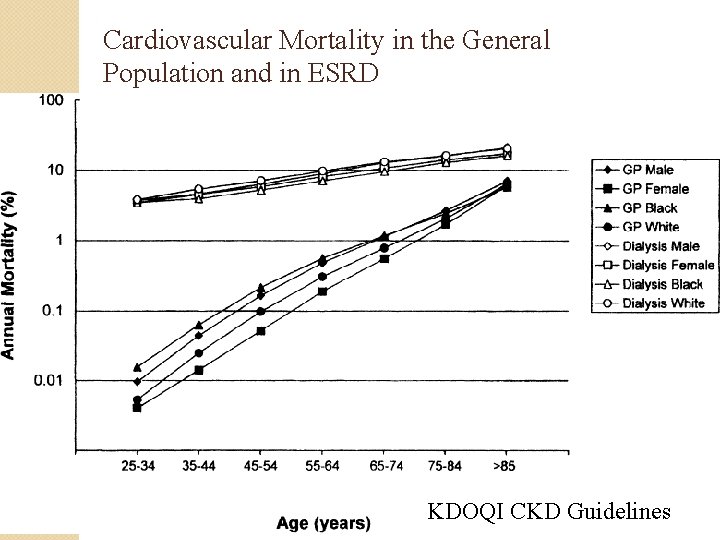
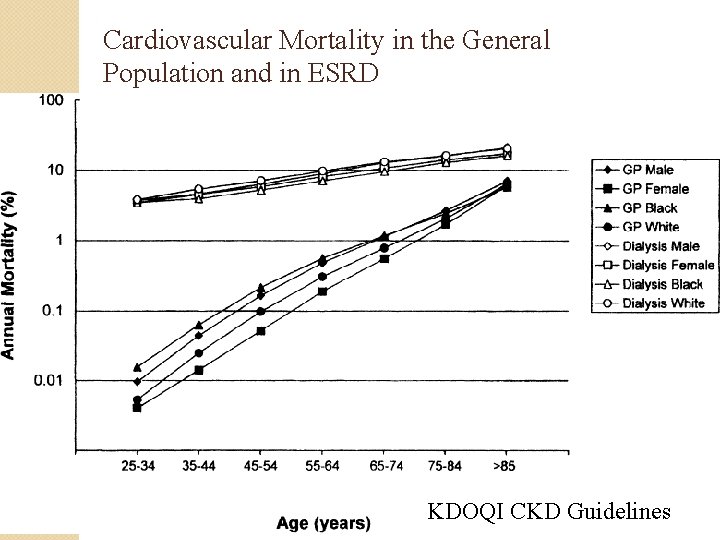
Cardiovascular Mortality in the General Population and in ESRD KDOQI CKD Guidelines
Indications for Renal Replacement Therapy Hyperkalemia Metabolic acidosis Fluid overload (recurrent CHF admissions) Uremic pericarditis (rub) Other non specific uremic symptoms: anorexia and nausea, impaired nutritional status, increased sleepiness, and decreased energy level, attentiveness, and cognitive tasking, …
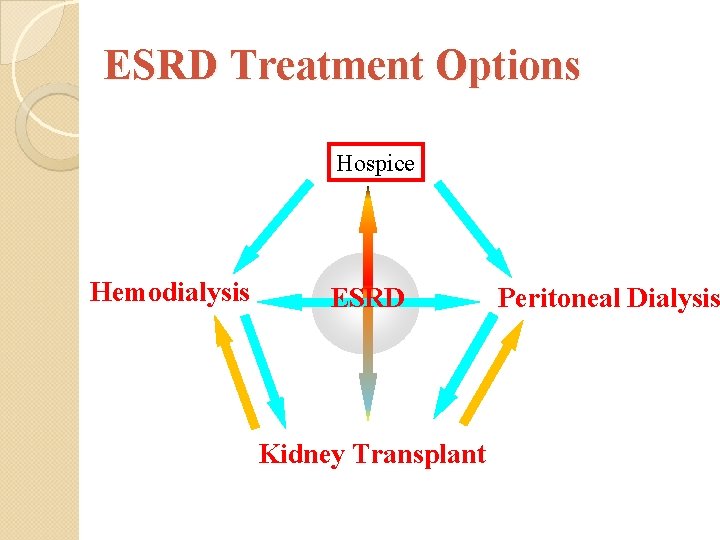
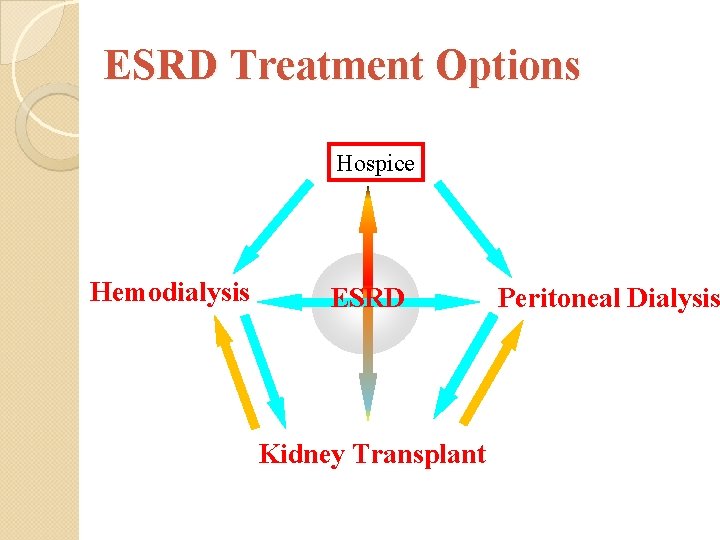
ESRD Treatment Options Hospice Hemodialysis ESRD Kidney Transplant Peritoneal Dialysis
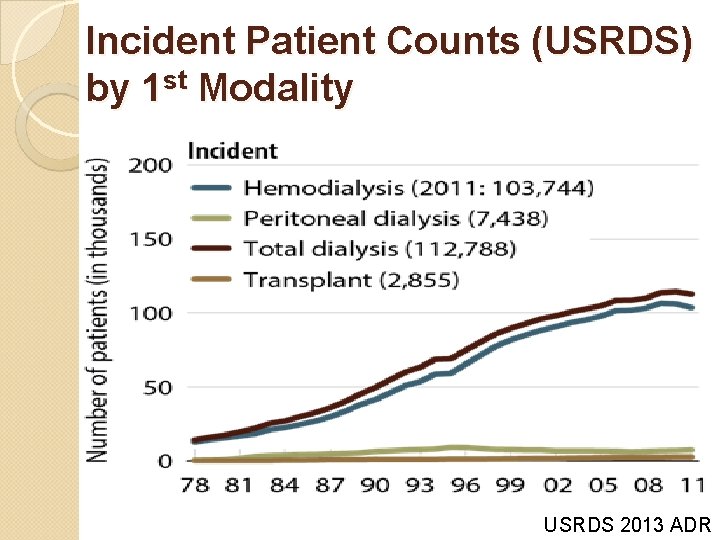
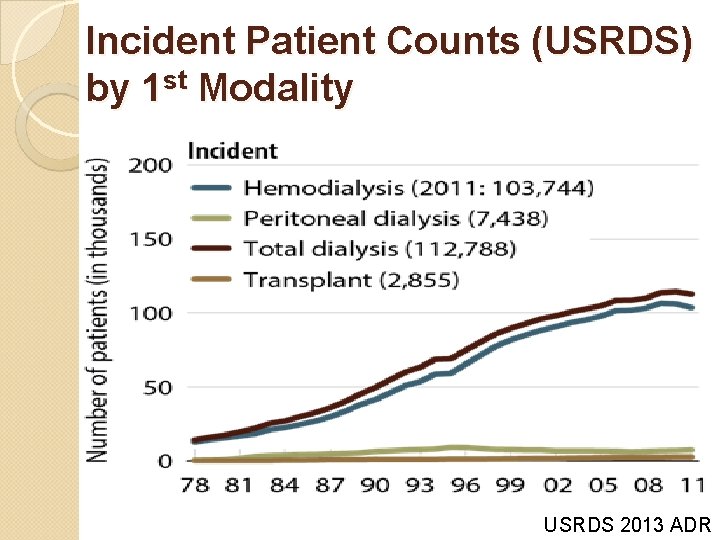
Incident Patient Counts (USRDS) by 1 st Modality USRDS 2013 ADR
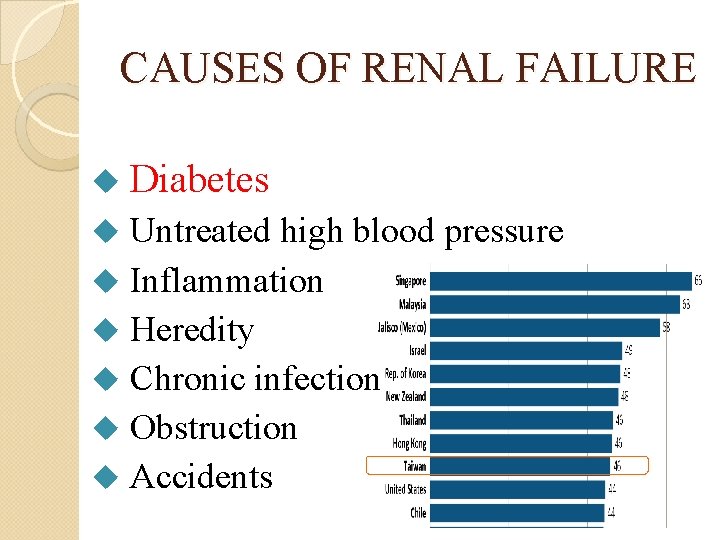
CAUSES OF RENAL FAILURE u Diabetes Untreated high blood pressure u Inflammation u Heredity u Chronic infection u Obstruction u Accidents u
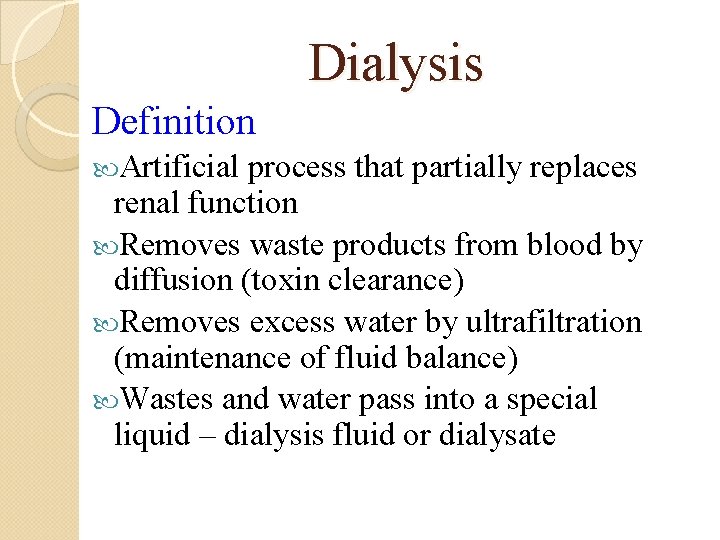
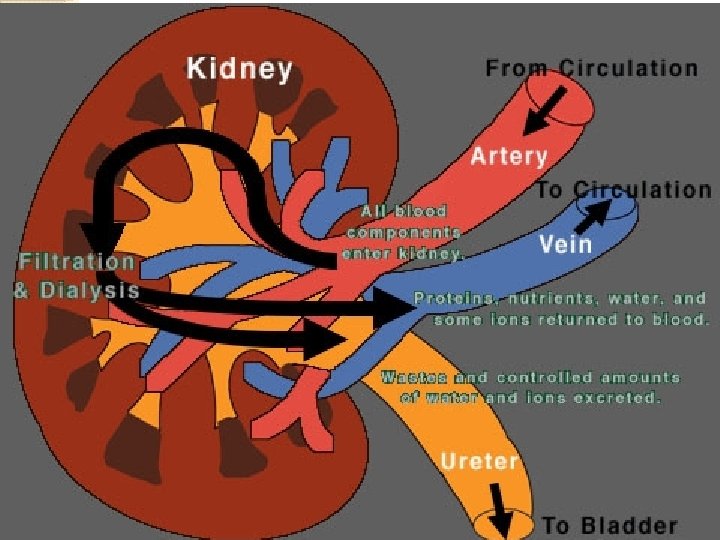
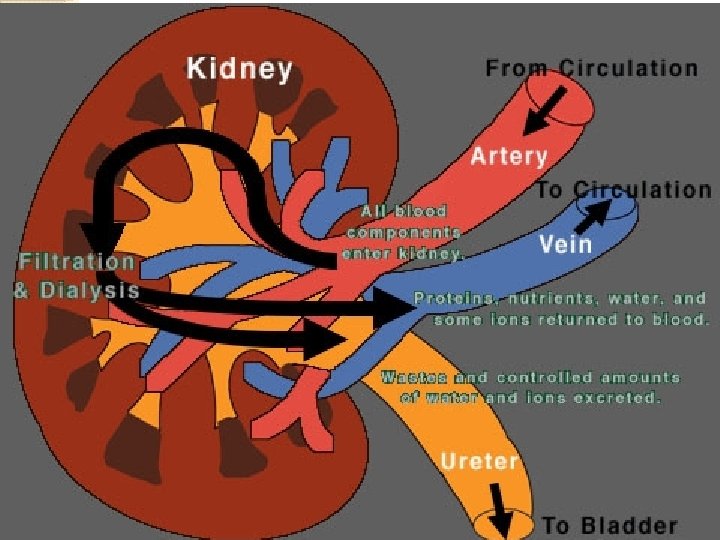
Dialysis Definition Artificial process that partially replaces renal function Removes waste products from blood by diffusion (toxin clearance) Removes excess water by ultrafiltration (maintenance of fluid balance) Wastes and water pass into a special liquid – dialysis fluid or dialysate
Types Haemodialysis (HD) Peritoneal Dialysis (PD) They work on similar principles: Movement of solute or water across a semipermeable membrane (dialysis membrane)
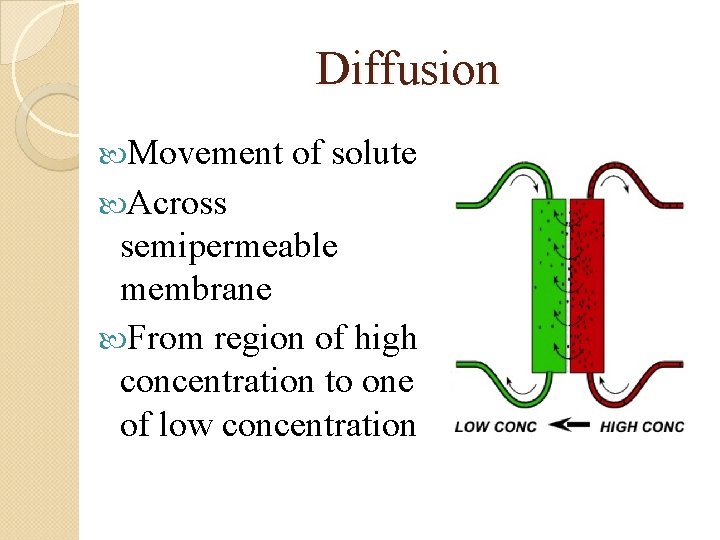
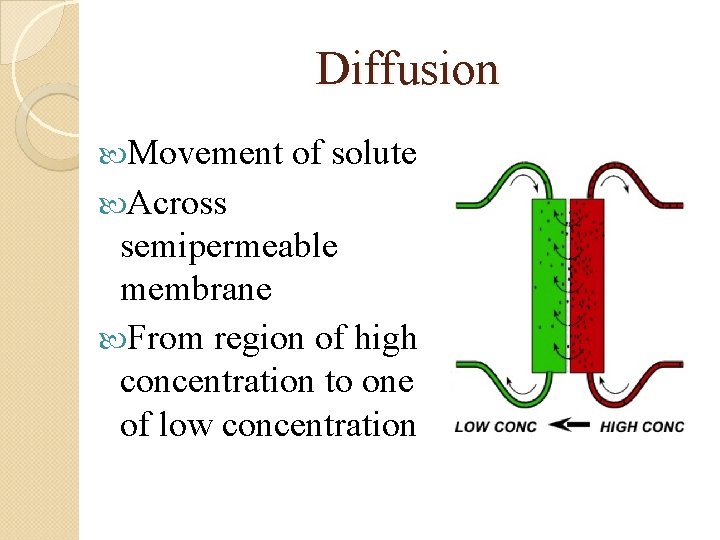
Diffusion Movement of solute Across semipermeable membrane From region of high concentration to one of low concentration
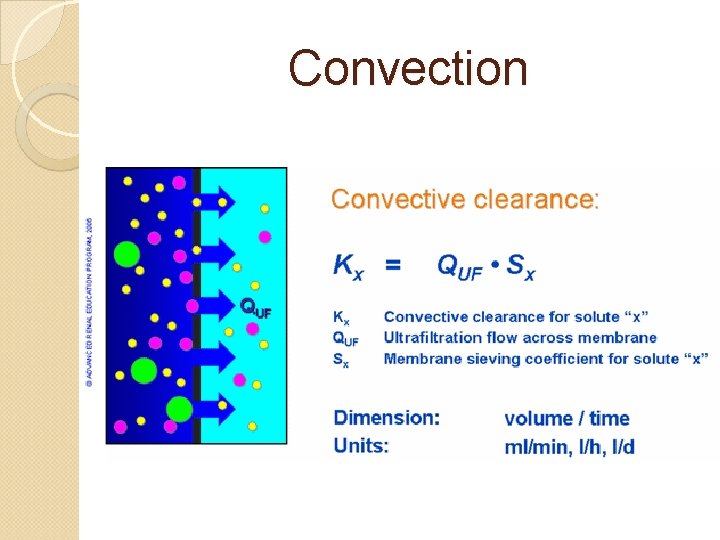
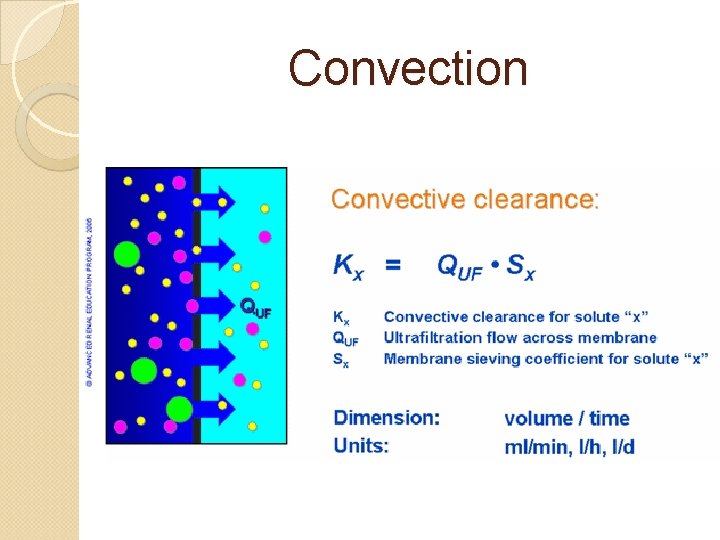
Convection
Selection for HD/PD Clinical condition Lifestyle Patient competence/hygiene (PD high risk of infection) Affordability / Availability
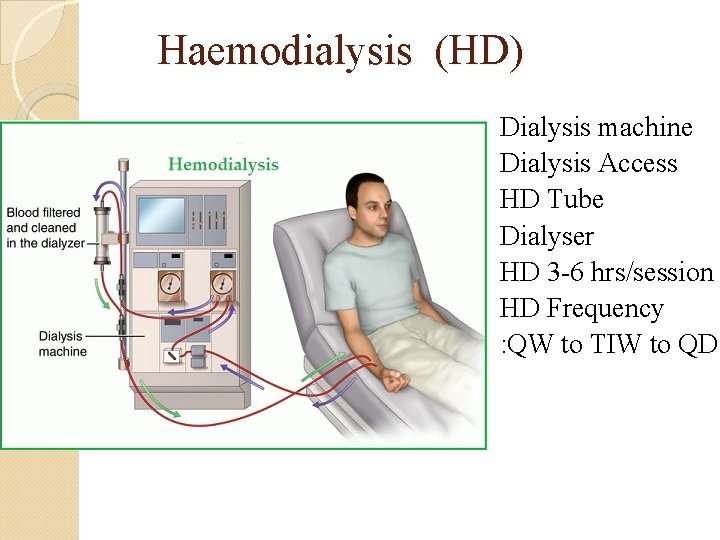
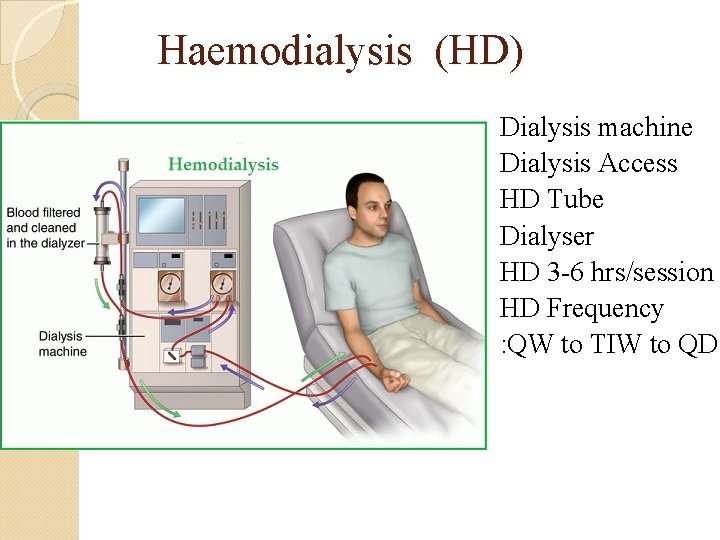
Haemodialysis (HD) Dialysis machine Dialysis Access HD Tube Dialyser HD 3 -6 hrs/session HD Frequency : QW to TIW to QD
Requirements for HD Good access to patients circulation Good cardiovascular status (dramatic changes in BP may occur)
Performing HD HD may be carried out: In a HD Unit At a Minimal Care / Self-Care Centre At Home
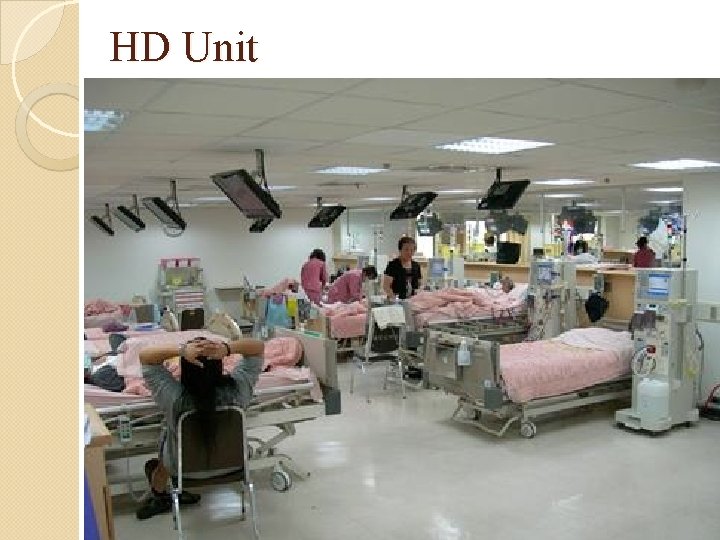
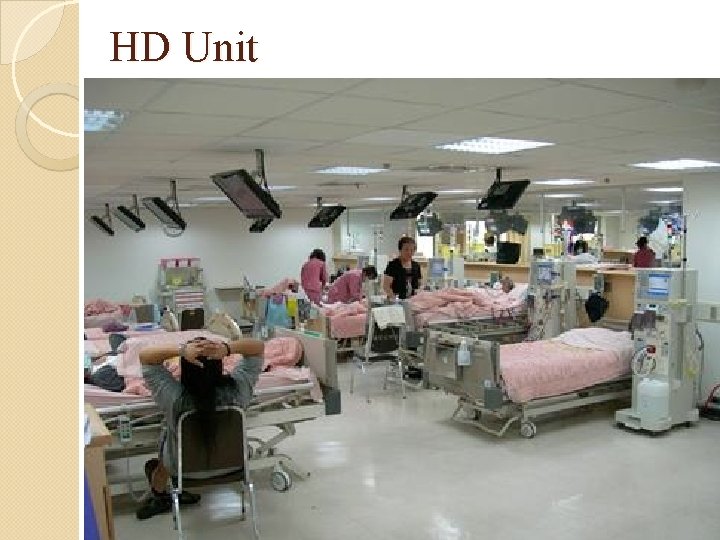
HD Unit Specially designed Renal Unit within a hospital Patients must travel to the Unit 3 x a week Patients are unable to move around while on dialysis; may chat, read, watch TV or eat Nursing staff prepare equipment, insert the needles and supervise the sessions
Minimal / Self-Care Dialysis Patients take a more active role Patients prepare the dialysis machine, insert the needles, adjust pump speeds and machine settings and chart their progress under the supervision of dialysis staff Patients must travel to the unit 3 x / week Patients need to be on a fixed schedule
Home Haemodialysis Use of machines set up at home Machines have many safety devices inbuilt Thorough patient training Requires the help of a partner at home every time Suitability is assessed by the haemodialysis team Ideal for patients who value their independence and need to fit in their treatment around a busy schedule
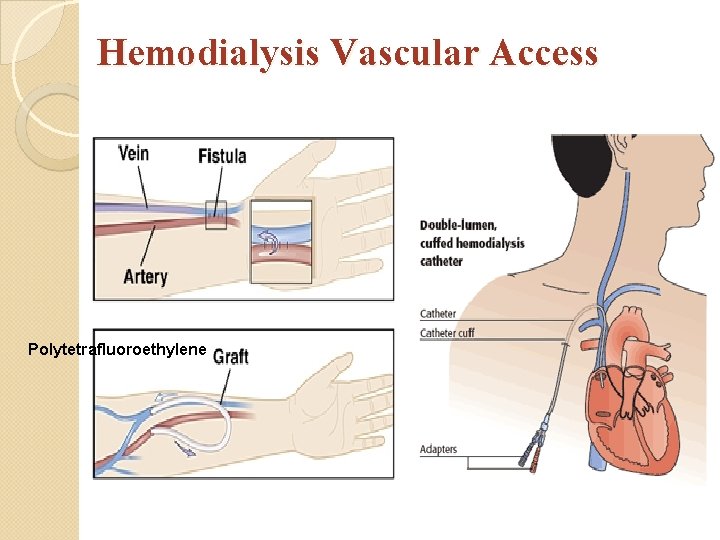
HD Access 2 types of access for HD: ◦ Must provide good flow ◦ Reliable access A fistula: arterio-venous (AV) Vascular Access Catheter
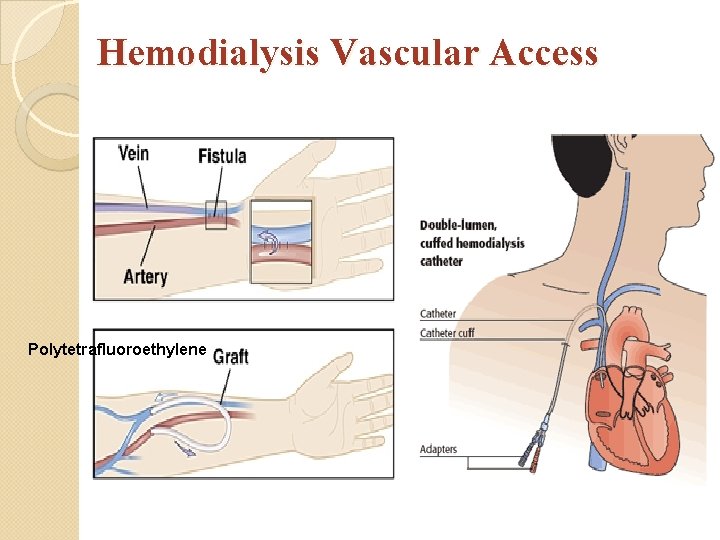
Hemodialysis Vascular Access Polytetrafluoroethylene
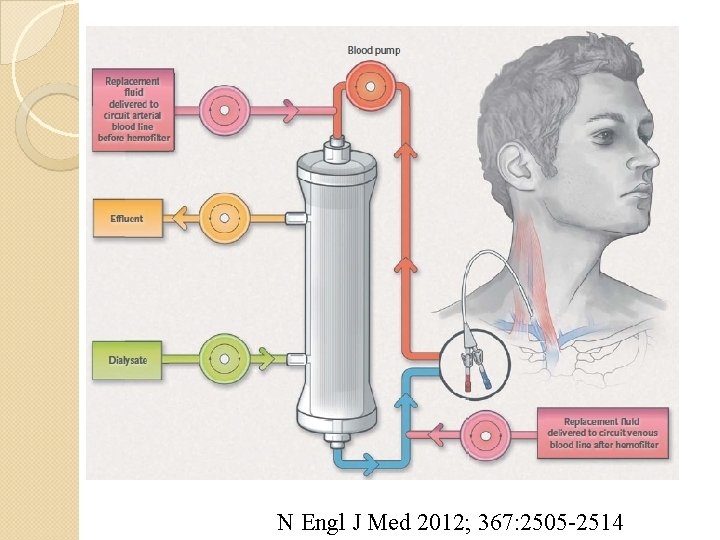
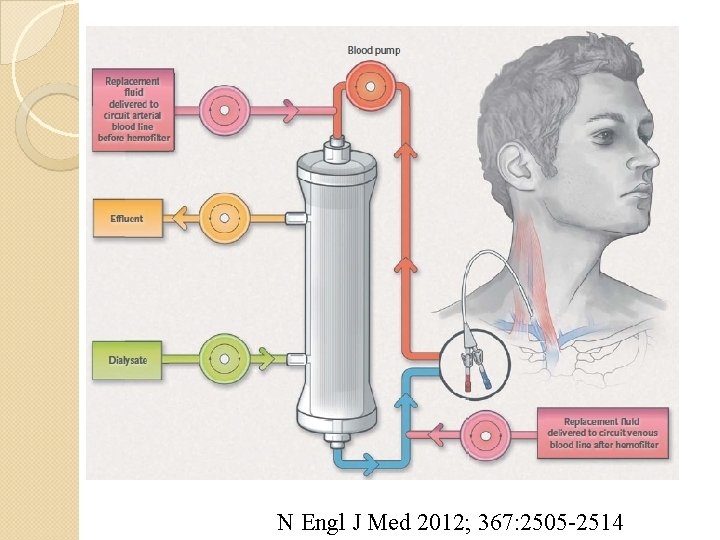
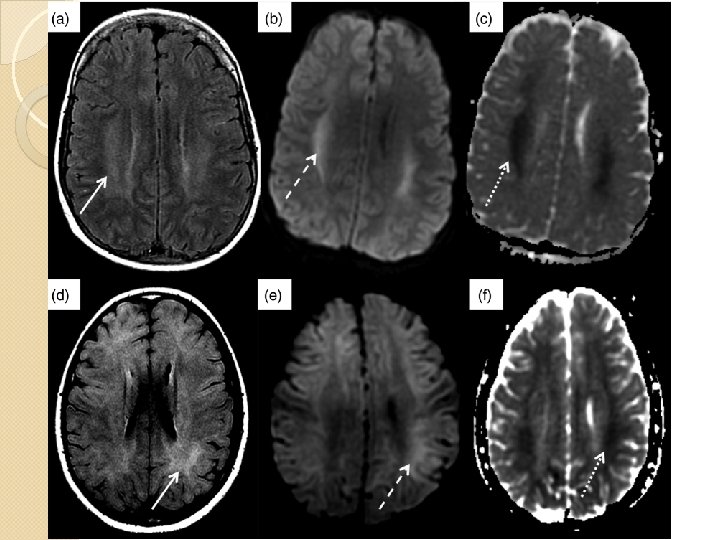
N Engl J Med 2012; 367: 2505 -2514
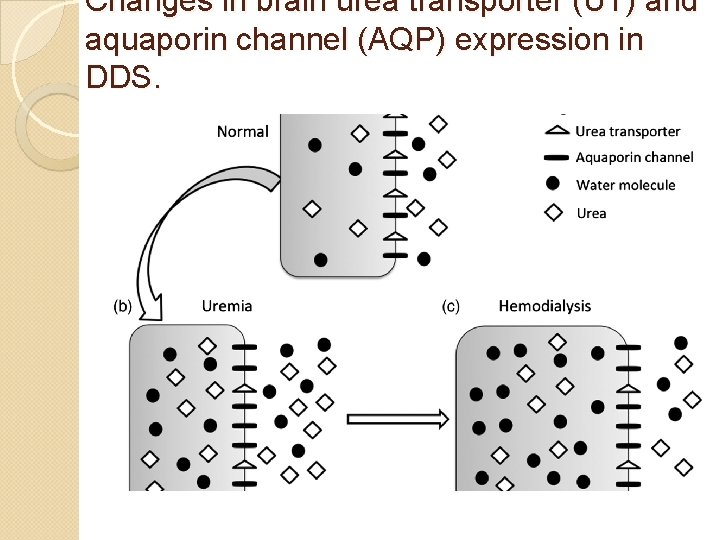
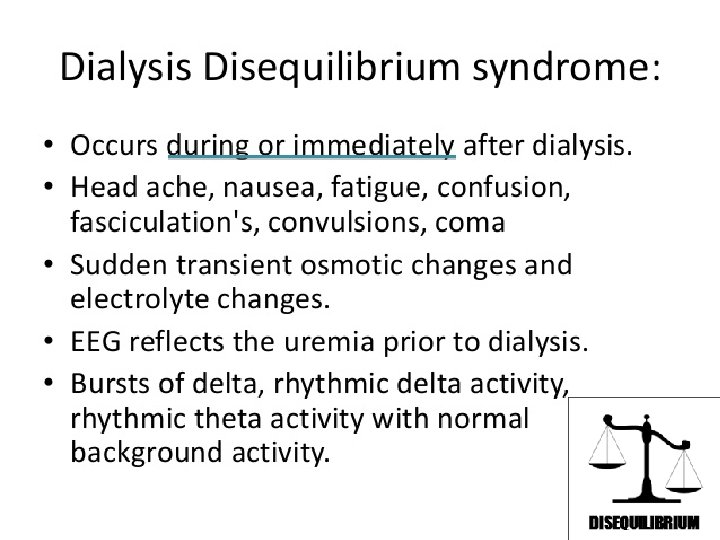
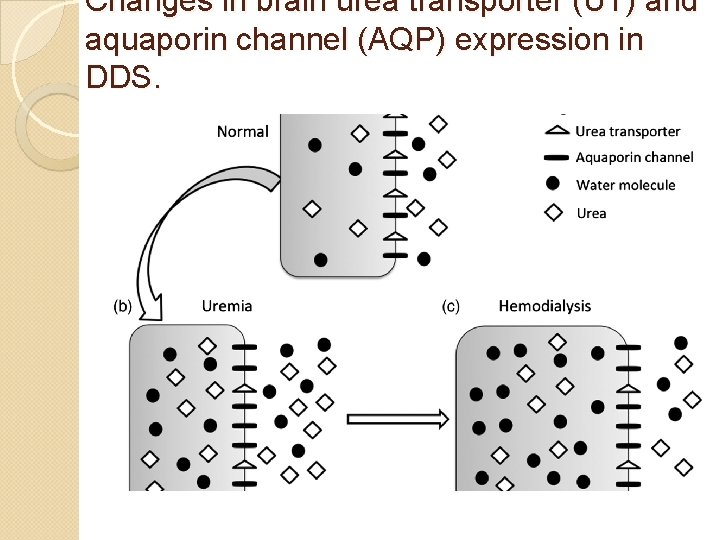
Changes in brain urea transporter (UT) and aquaporin channel (AQP) expression in DDS.
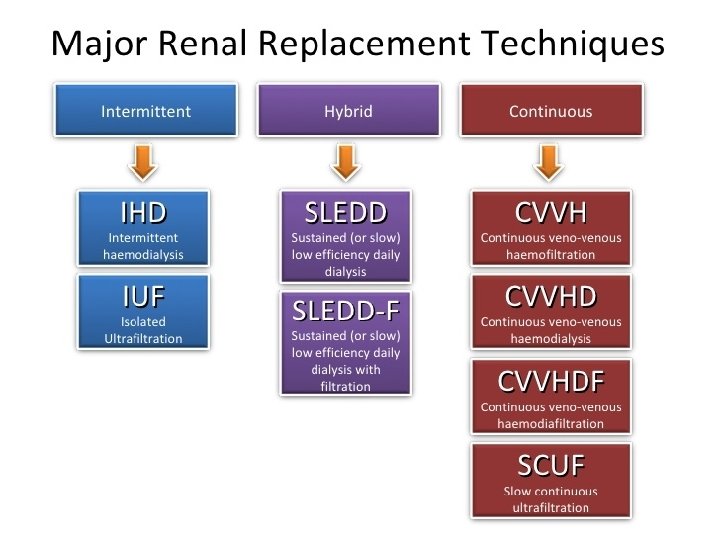
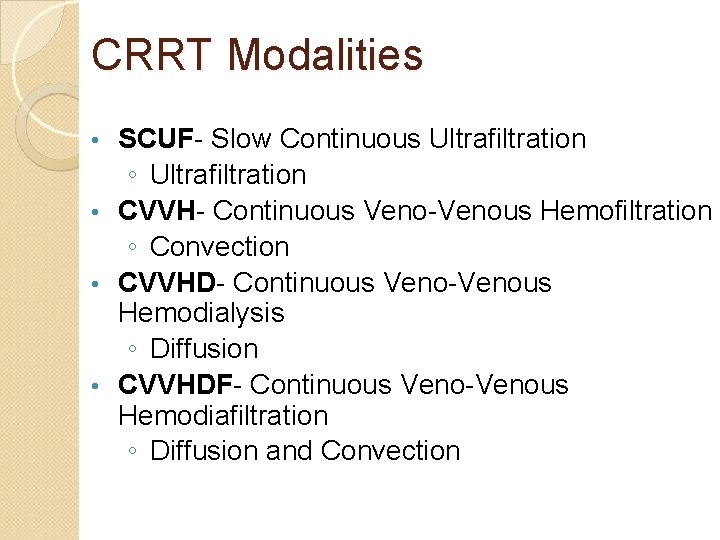
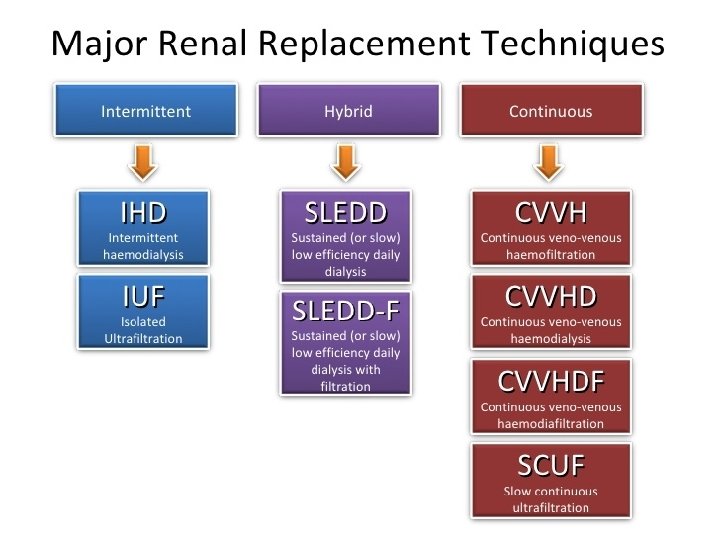
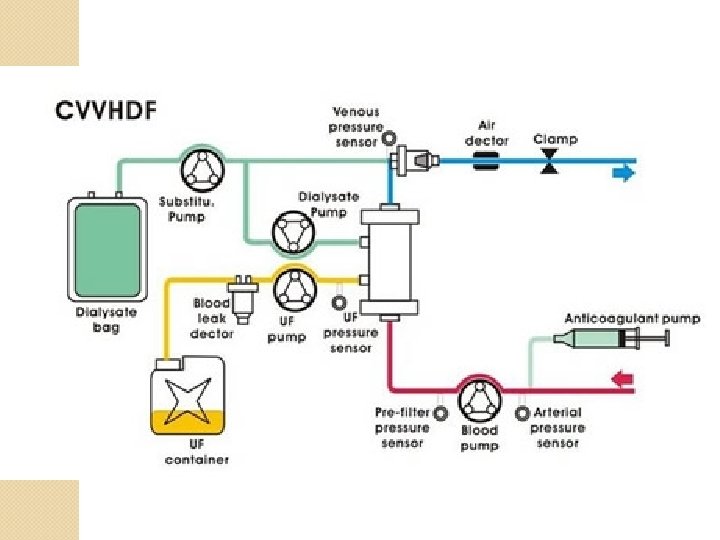
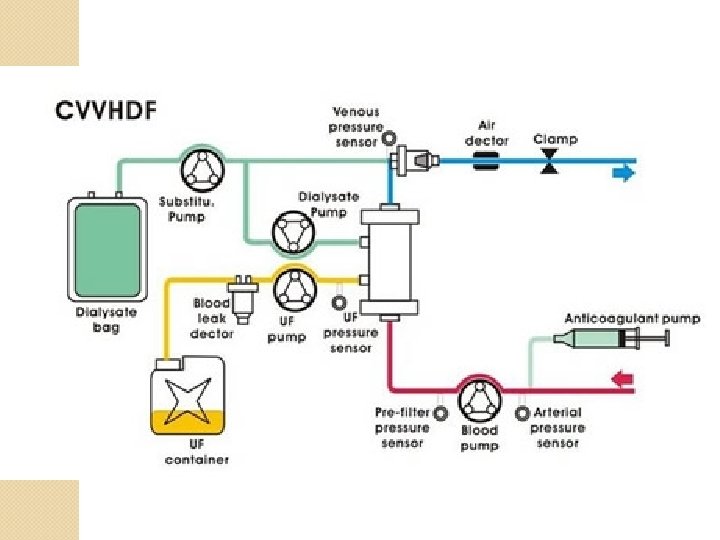
CRRT Modalities SCUF- Slow Continuous Ultrafiltration ◦ Ultrafiltration • CVVH- Continuous Veno-Venous Hemofiltration ◦ Convection • CVVHD- Continuous Veno-Venous Hemodialysis ◦ Diffusion • CVVHDF- Continuous Veno-Venous Hemodiafiltration ◦ Diffusion and Convection •
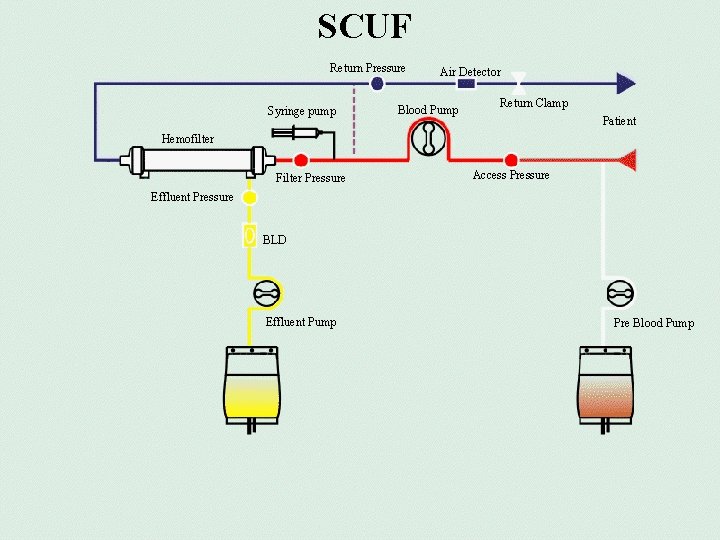
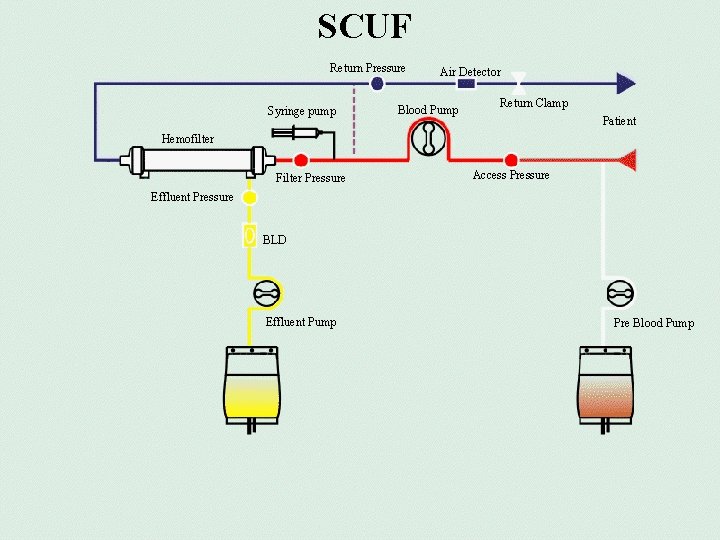
SCUF Return Pressure Syringe pump Air Detector Blood Pump Return Clamp Patient Hemofilter Filter Pressure Access Pressure Effluent Pressure BLD Effluent Pump Pre Blood Pump
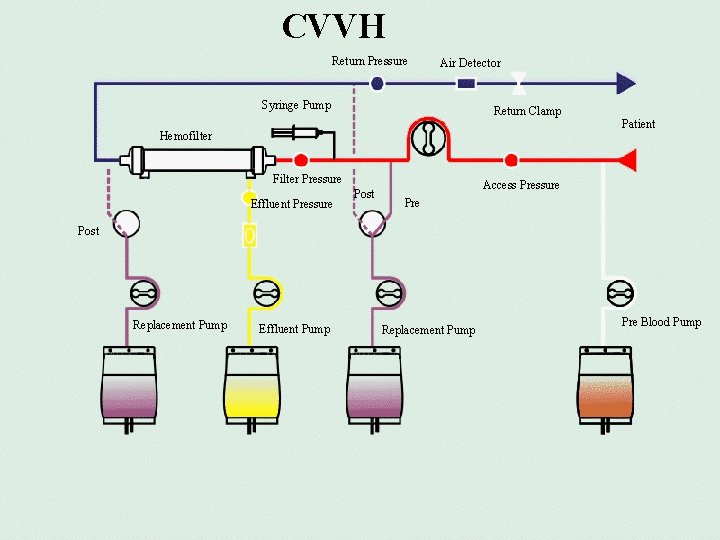
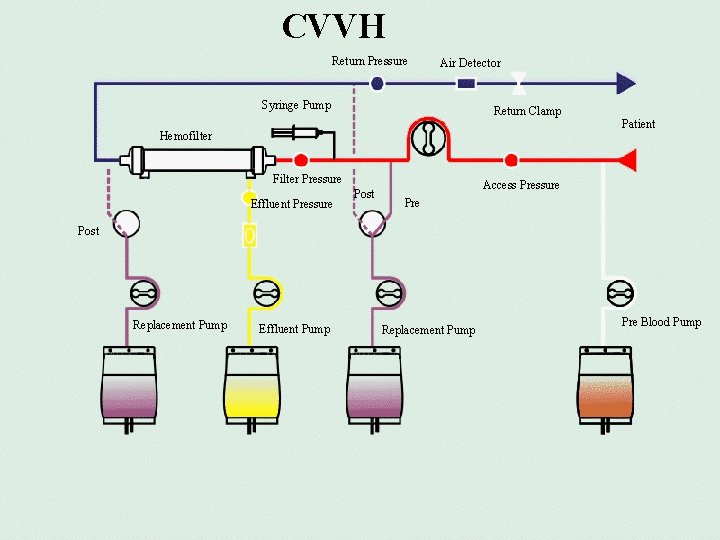
CVVH Return Pressure Air Detector Syringe Pump Return Clamp Hemofilter Filter Pressure Effluent Pressure Post Patient Access Pressure Post Replacement Pump Effluent Pump Replacement Pump 306100135 Pre Blood Pump
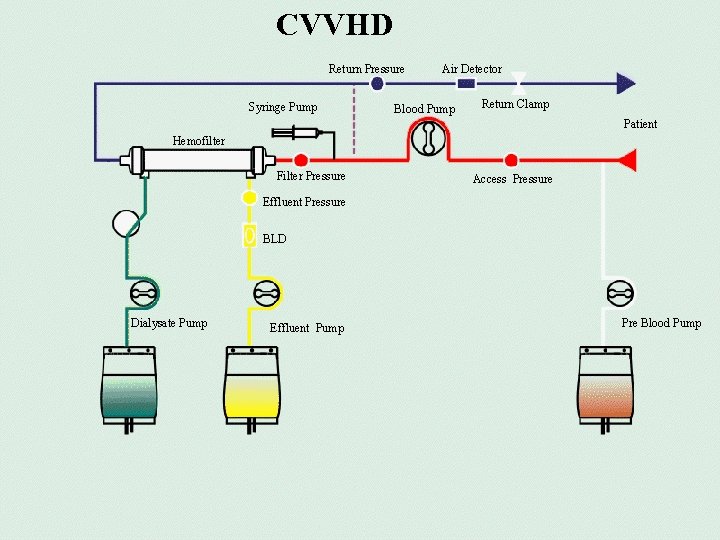
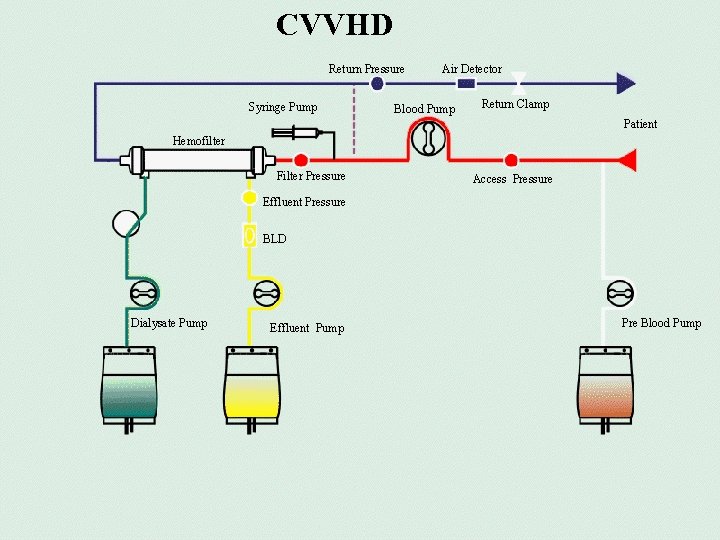
CVVHD Return Pressure Syringe Pump Air Detector Blood Pump Return Clamp Patient Hemofilter Filter Pressure Access Pressure Effluent Pressure BLD Dialysate Pump Pre Blood Pump Effluent Pump 306100135
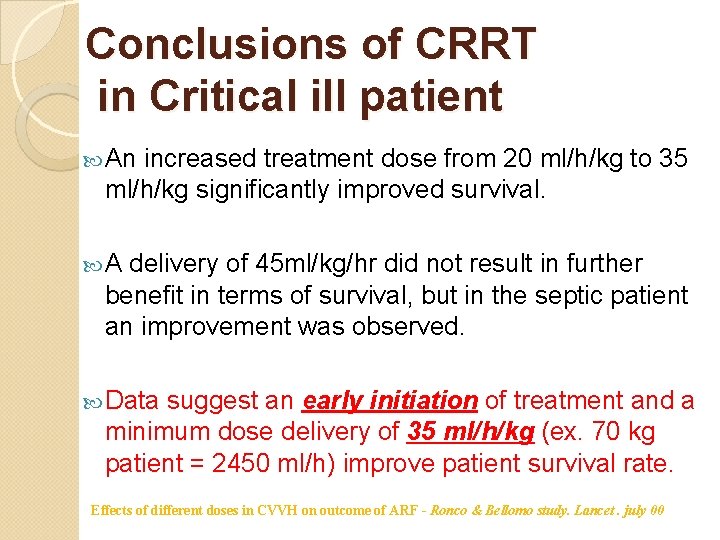
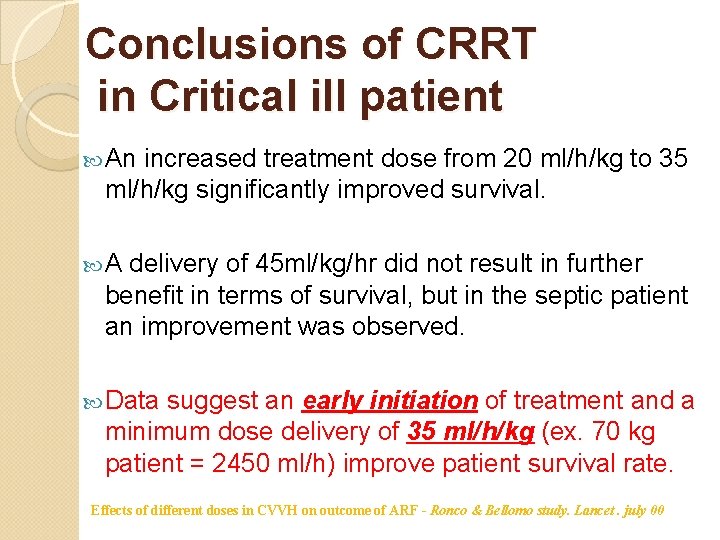
Conclusions of CRRT in Critical ill patient An increased treatment dose from 20 ml/h/kg to 35 ml/h/kg significantly improved survival. A delivery of 45 ml/kg/hr did not result in further benefit in terms of survival, but in the septic patient an improvement was observed. Data suggest an early initiation of treatment and a minimum dose delivery of 35 ml/h/kg (ex. 70 kg patient = 2450 ml/h) improve patient survival rate. Effects of different doses in CVVH on outcome of ARF - Ronco & Bellomo study. Lancet. july 00
Effects of HD on Lifestyle Flexibility: ◦ Difficult to fit in with school, work esp if unit is far from home. Home HD offers more flexibility Travel: ◦ Necessity to book in advance with HD unit of places of travel Responsibility & Independence: ◦ Home HD allows the greatest degree of independence
Effects of HD on Lifestyle Sexual Activity: ◦ Anxiety of living with renal failure affects relationship with partner Sport & Exercise: Body Image: ◦ Can exercise and participate in most sports ◦ Esp with fistula; patient can be very self conscious about it
Problems with HD Rapid changes in BP ◦ fainting, vomiting, cramps, chest pain, irritability, fatigue, temporary loss of vision Fluid overload ◦ esp in between sessions Fluid restrictions ◦ more stringent with HD than PD Hyperkalaemia ◦ esp in between sessions

Problems with HD Loss of independence Problems with access ◦ poor quality, blockage etc. Infection (vascular access catheters) Pain with needles Bleeding ◦ from the fistula during or after dialysis Infections ◦ during sessions; exit site infections; blood-borne viruses e. g. Hepatitis, HIV
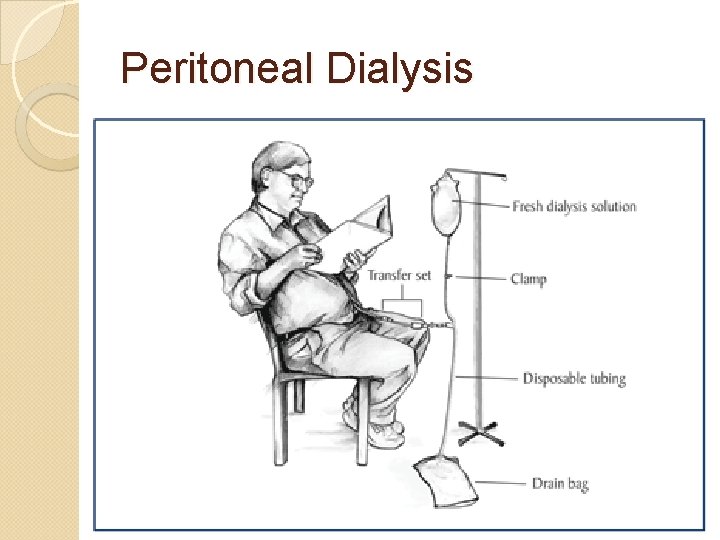
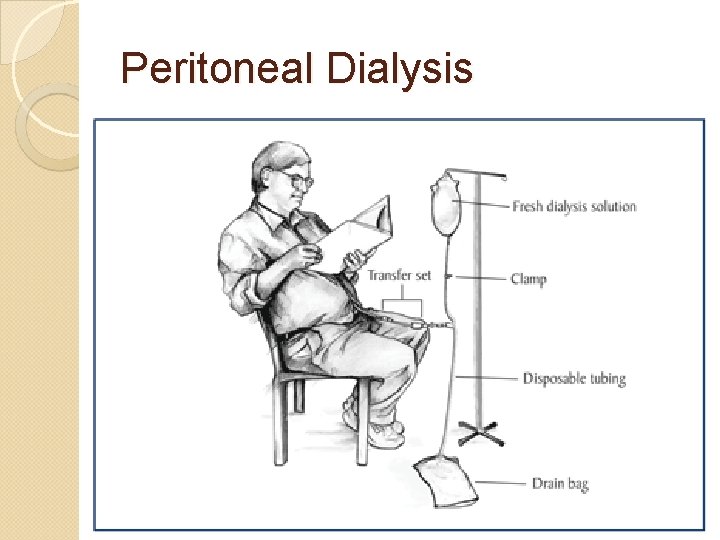
Peritoneal Dialysis
Peritoneal Dialysis (PD) Uses natural membrane (peritoneum) for dialysis Access is by PD catheter, a soft plastic tube Catheter and dialysis fluid may be hidden under clothing Suitability ◦ Excludes patients with prior peritoneal scarring e. g. peritonitis, laparotomy ◦ Excludes patients unable to care for self
Addendum to Principles (PD) Fluid across the membrane faster than solutes; therefore longer dwell times are needed for solute transfer Protein loss in PD fluid is significant ~ 89 g/day Protein loss ↑s during peritonitis PD patients require adequate daily protein averaging 1. 2 – 1. 5 g/kg/day Other substances lost in the dialysate ◦ Amino acids, water soluble vitamins, some medications and hormones Calcium and dextrose are absorbed from the dialysate fluid into the circulation
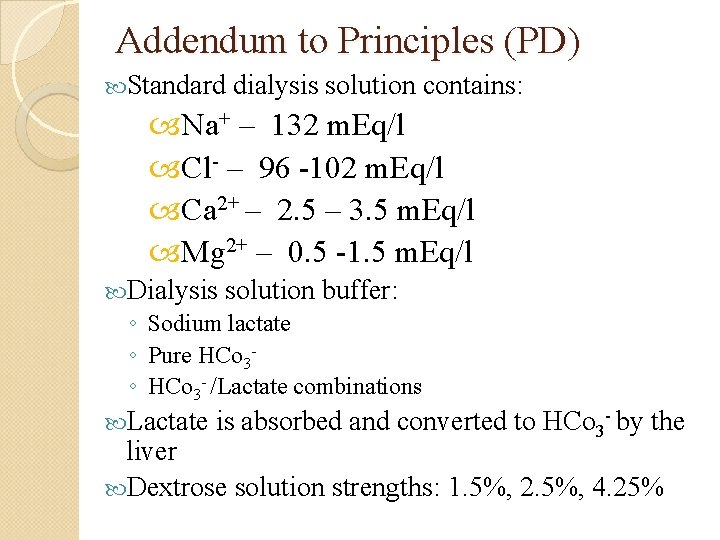
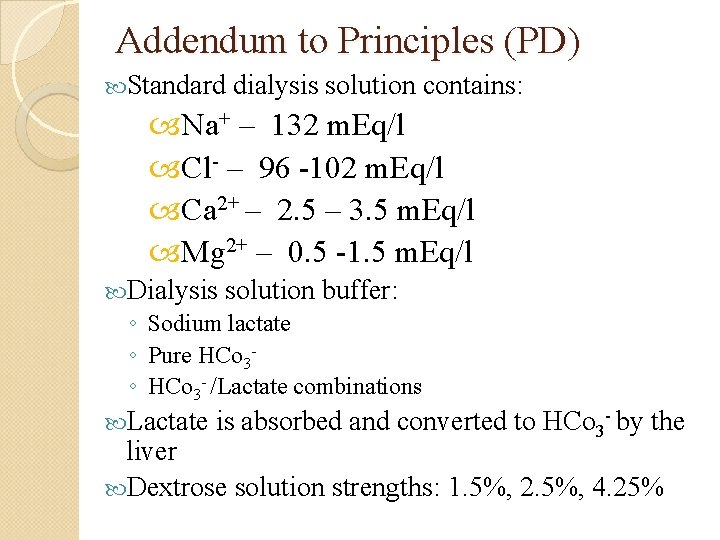
Addendum to Principles (PD) Standard dialysis solution contains: Na+ – 132 m. Eq/l Cl- – 96 -102 m. Eq/l Ca 2+ – 2. 5 – 3. 5 m. Eq/l Mg 2+ – 0. 5 -1. 5 m. Eq/l Dialysis solution buffer: ◦ Sodium lactate ◦ Pure HCo 3◦ HCo 3 - /Lactate combinations Lactate is absorbed and converted to HCo 3 - by the liver Dextrose solution strengths: 1. 5%, 2. 5%, 4. 25%
Types Continuous Ambulatory Peritoneal Dialysis (CAPD) Automated peritoneal Dialysis (APD)
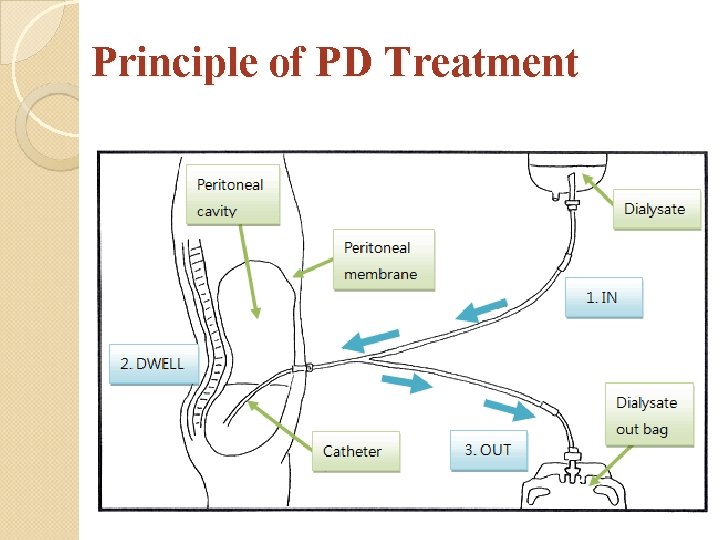
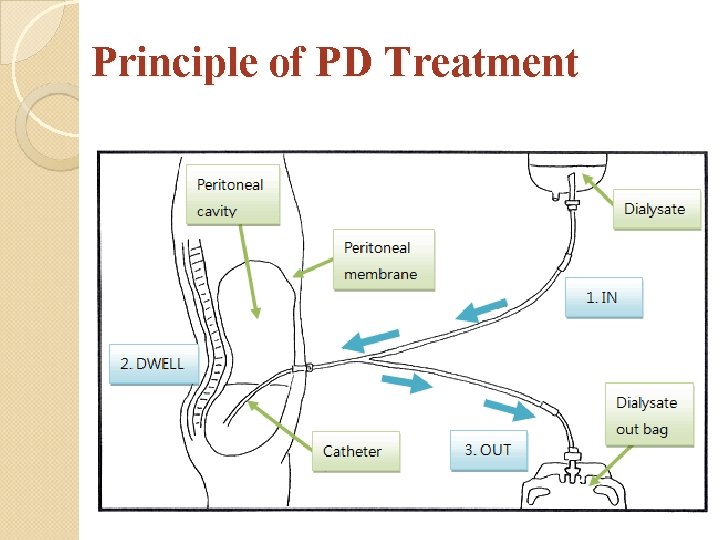
Principle of PD Treatment
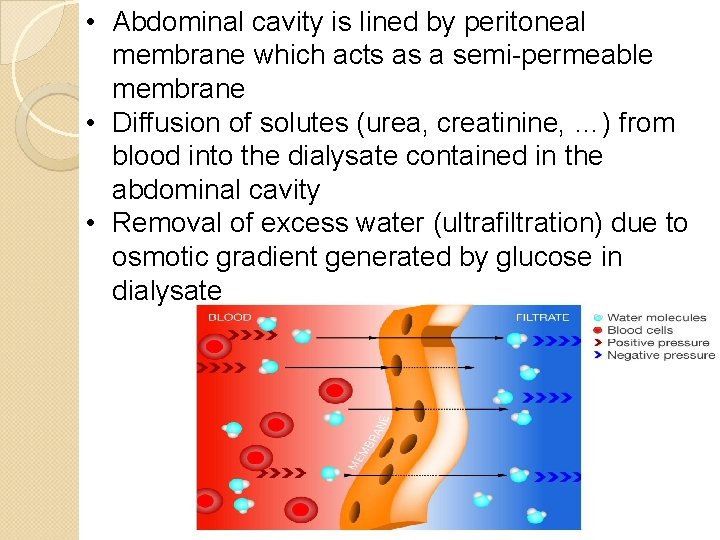
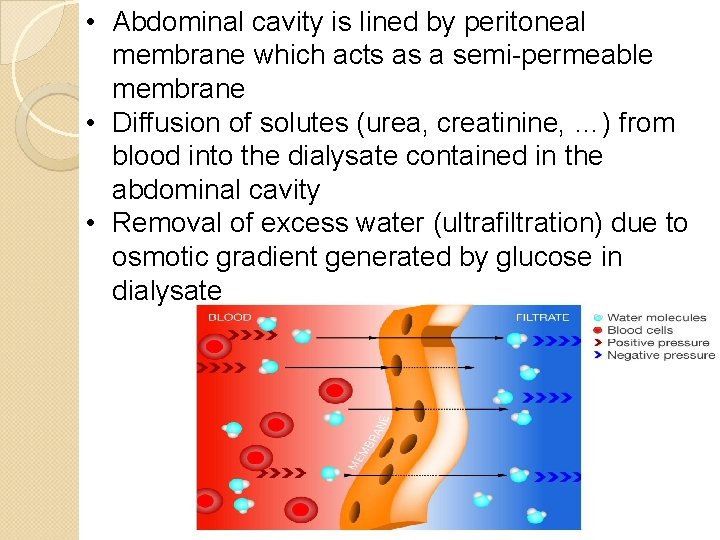
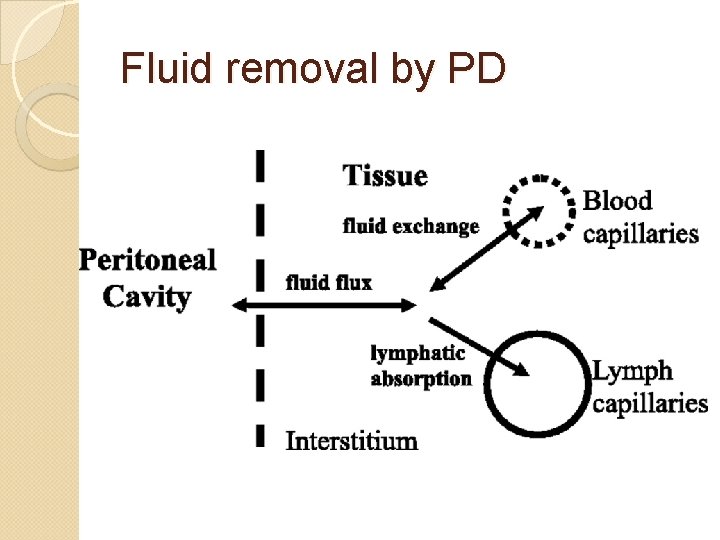
• Abdominal cavity is lined by peritoneal membrane which acts as a semi-permeable membrane • Diffusion of solutes (urea, creatinine, …) from blood into the dialysate contained in the abdominal cavity • Removal of excess water (ultrafiltration) due to osmotic gradient generated by glucose in dialysate
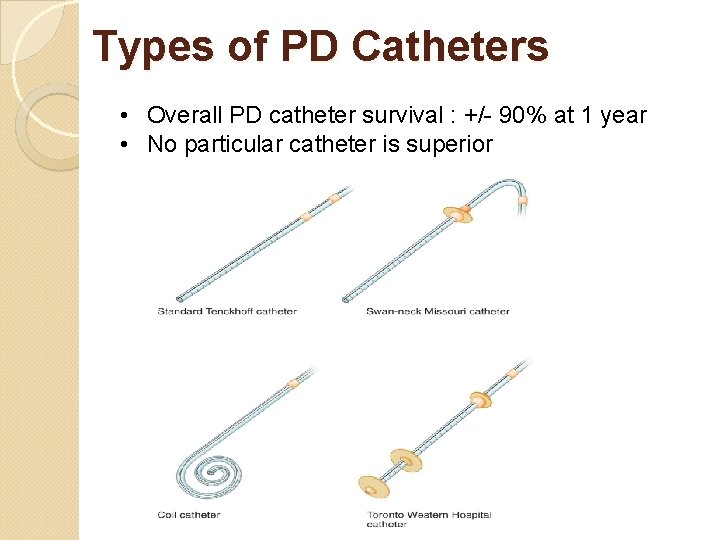
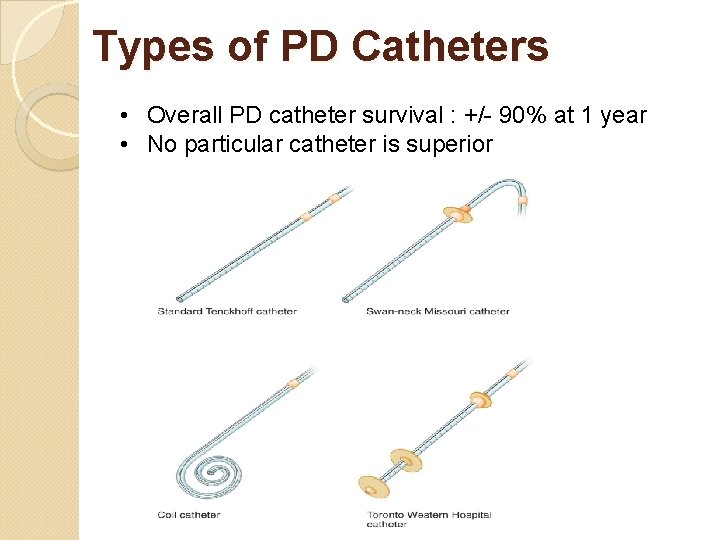
Types of PD Catheters • Overall PD catheter survival : +/- 90% at 1 year • No particular catheter is superior
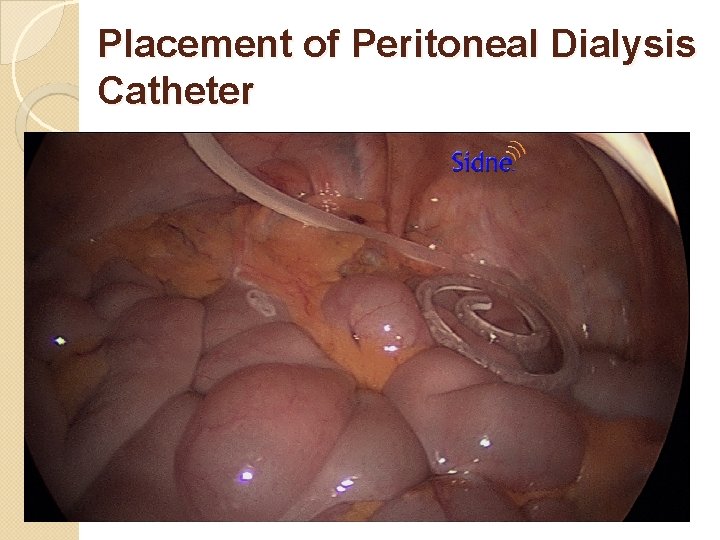
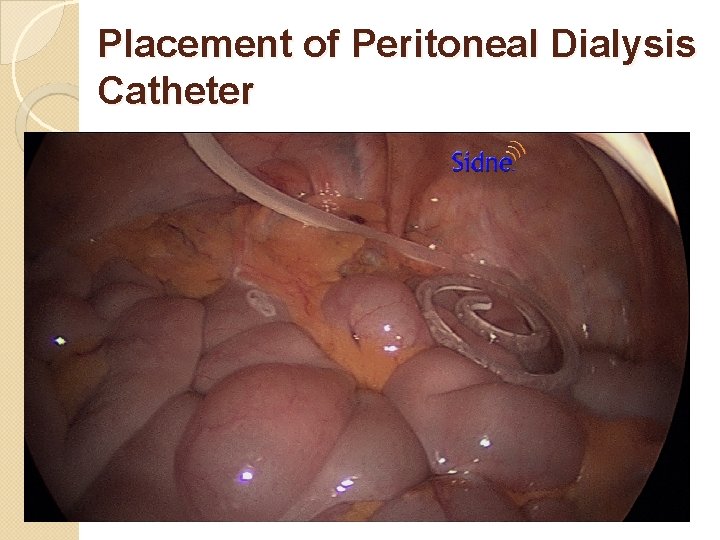
Placement of Peritoneal Dialysis Catheter
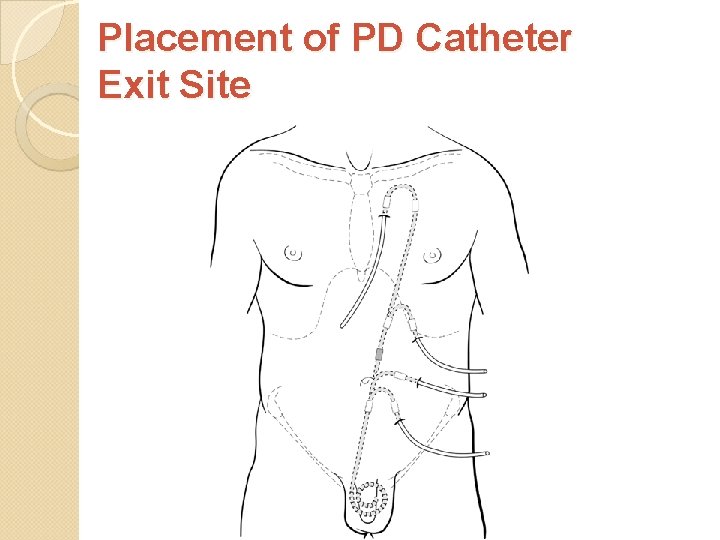
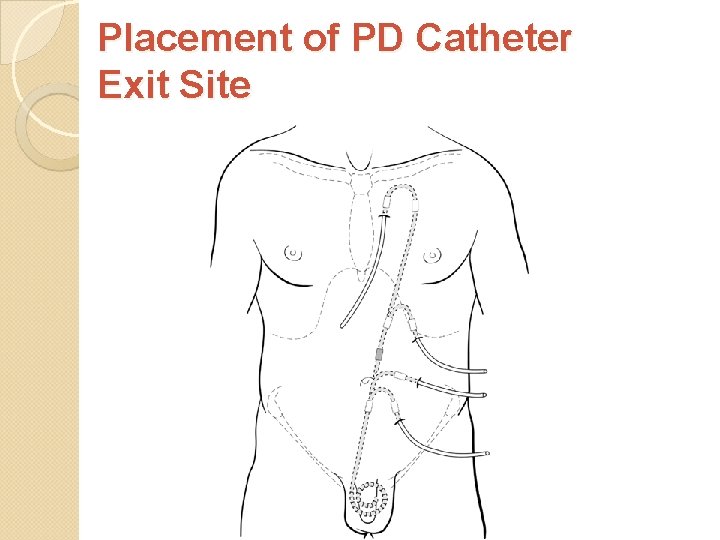
Placement of PD Catheter Exit Site
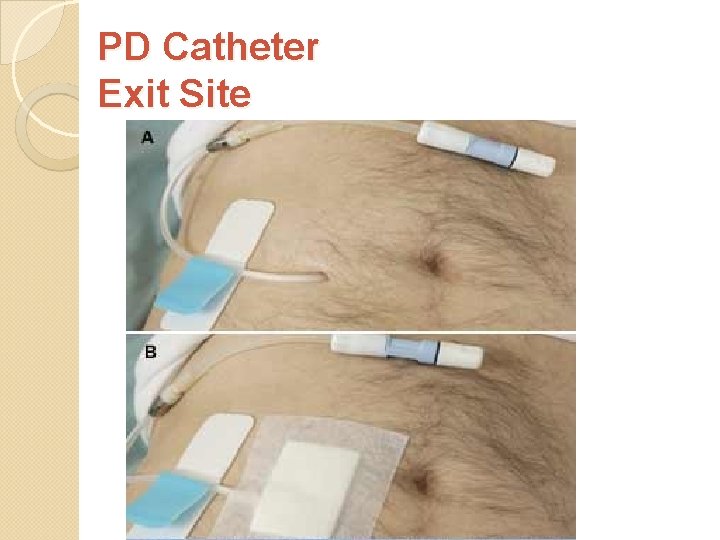
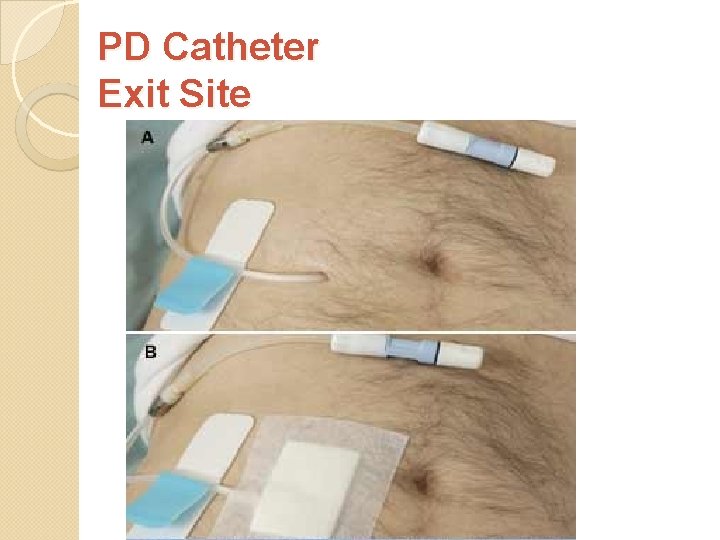
PD Catheter Exit Site
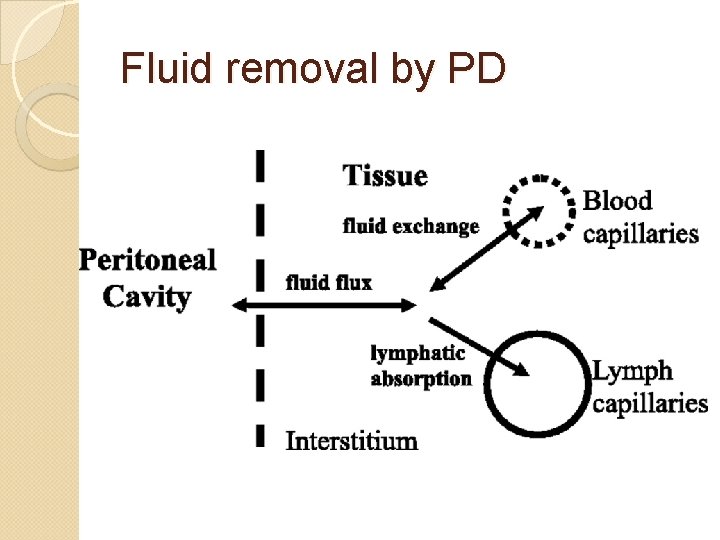
Fluid removal by PD
CAPD Dialysis takes place 24 hrs a day, 7 days a week • Patient is not attached to a machine for treatment • Exchanges are usually carried out by patient after training by a CAPD nurse • Most patients need 3 -5 exchanges a day i. e. • • 4 -6 hour intervals (Dwell time) 30 mins per exchange May use 2 -3 litres of fluid in abdomen • No needles are used • Less dietary and fluid restriction •
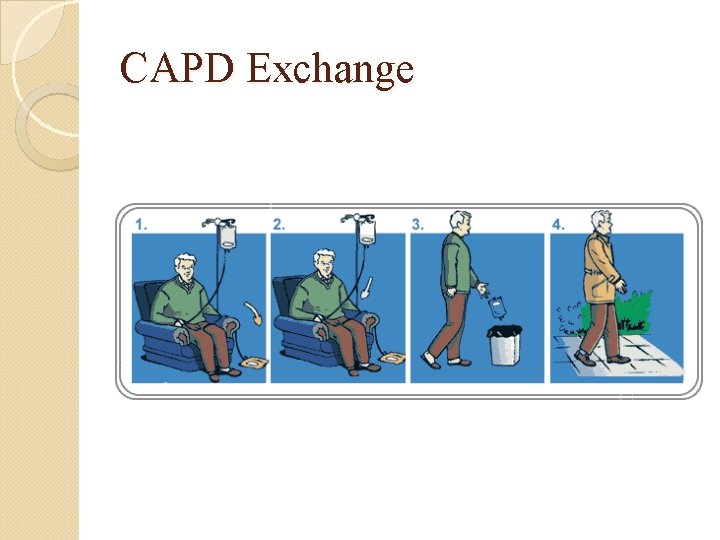
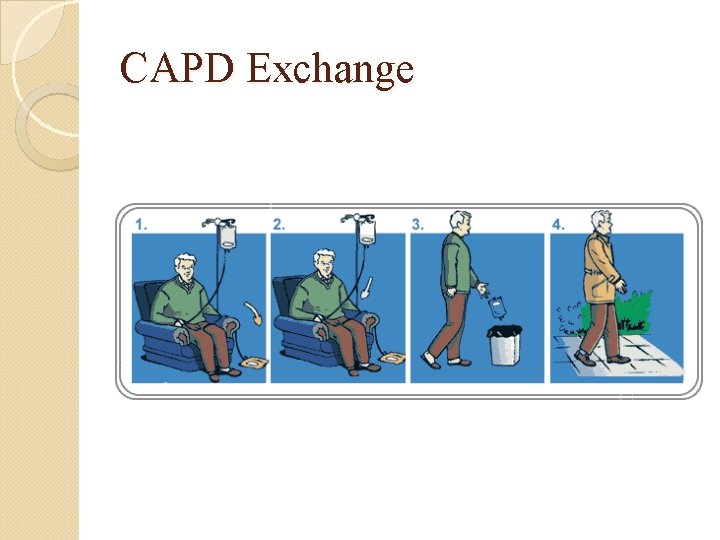
CAPD Exchange
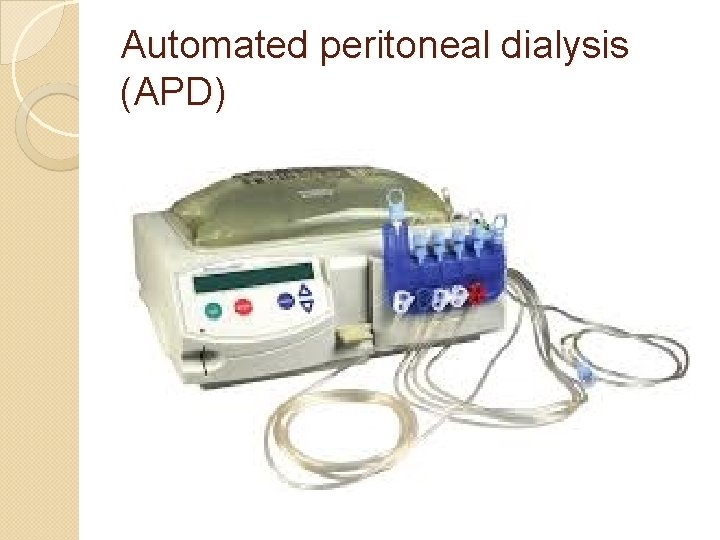
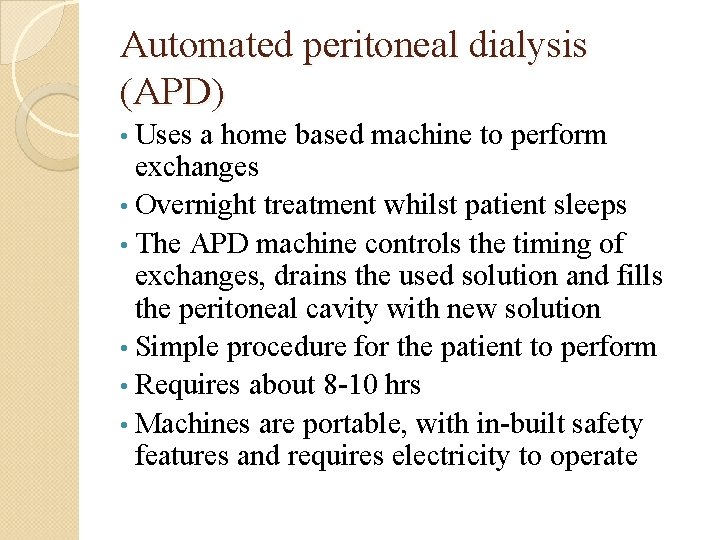
Automated peritoneal dialysis (APD)
Automated peritoneal dialysis (APD) • Uses a home based machine to perform exchanges • Overnight treatment whilst patient sleeps • The APD machine controls the timing of exchanges, drains the used solution and fills the peritoneal cavity with new solution • Simple procedure for the patient to perform • Requires about 8 -10 hrs • Machines are portable, with in-built safety features and requires electricity to operate
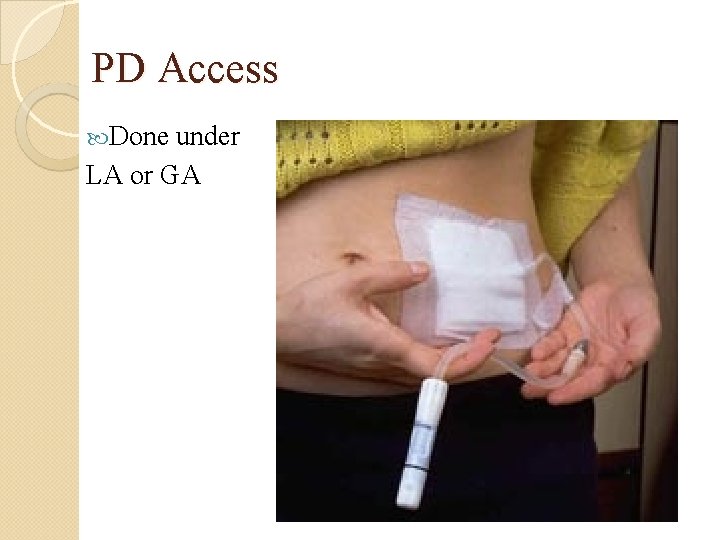
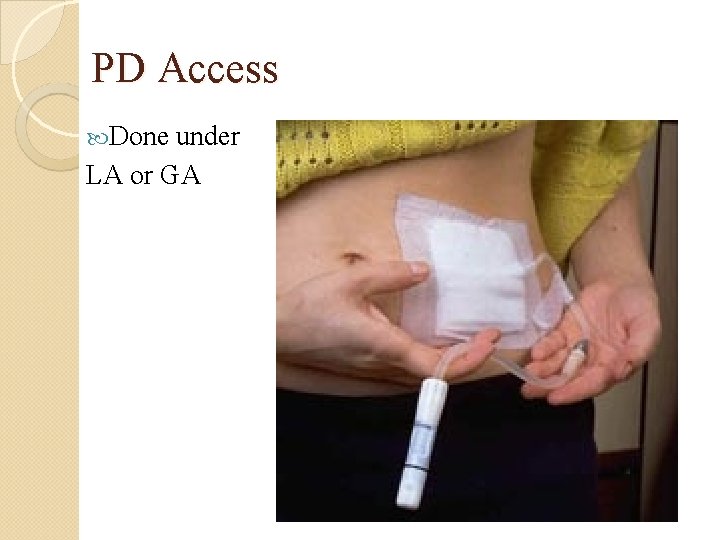
PD Access Done under LA or GA
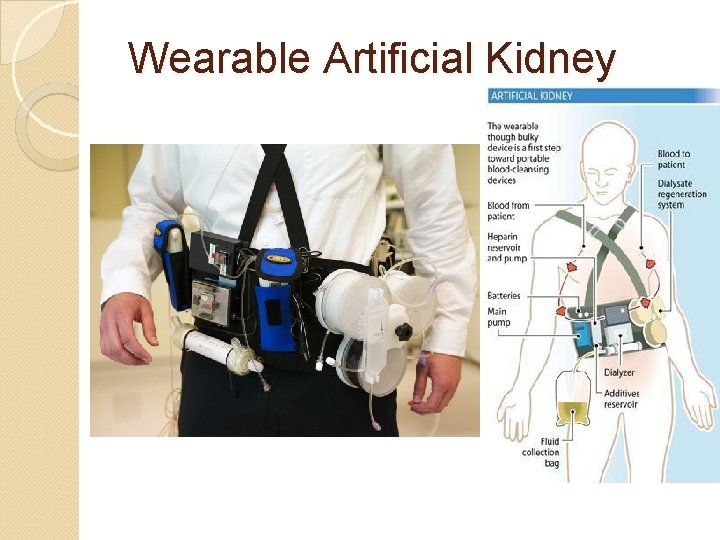
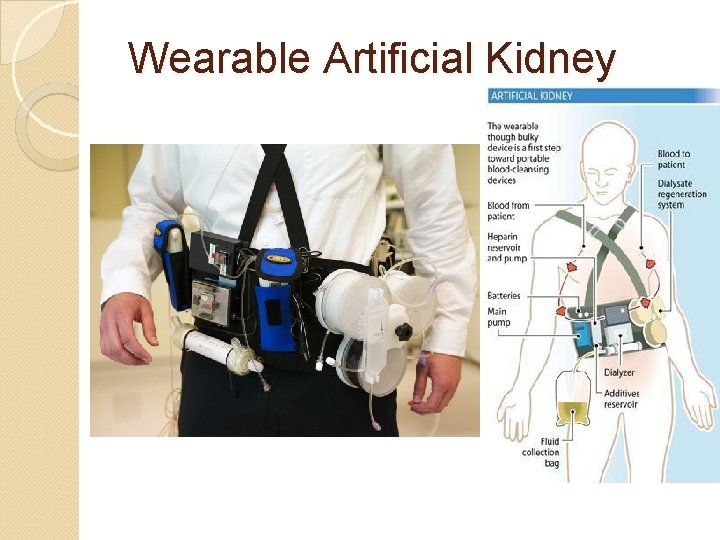
Wearable Artificial Kidney
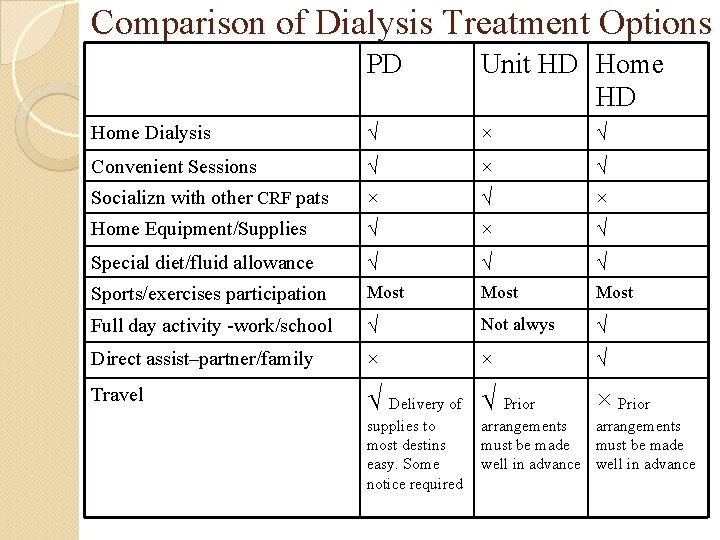
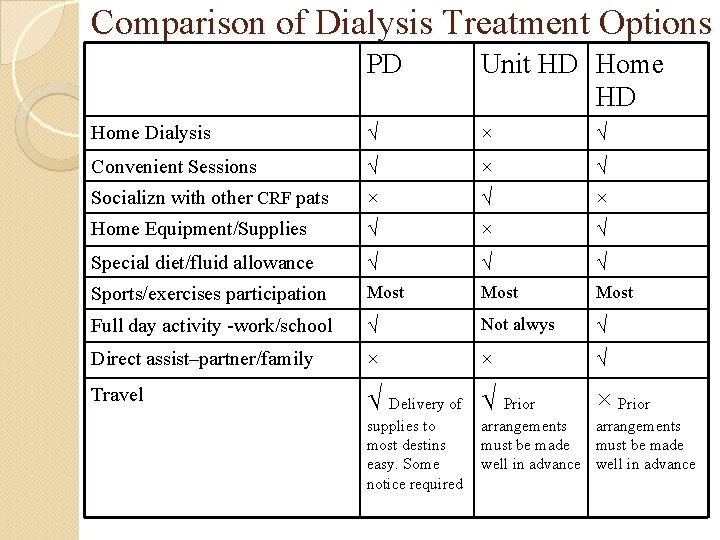
Comparison of Dialysis Treatment Options PD Unit HD Home Dialysis √ × √ Convenient Sessions √ × √ Socializn with other CRF pats × √ × Home Equipment/Supplies √ × √ Special diet/fluid allowance √ √ √ Sports/exercises participation Most Full day activity -work/school √ Not alwys √ Direct assist–partner/family × × √ Travel √ Delivery of √ Prior supplies to most destins easy. Some notice required × Prior arrangements must be made well in advance
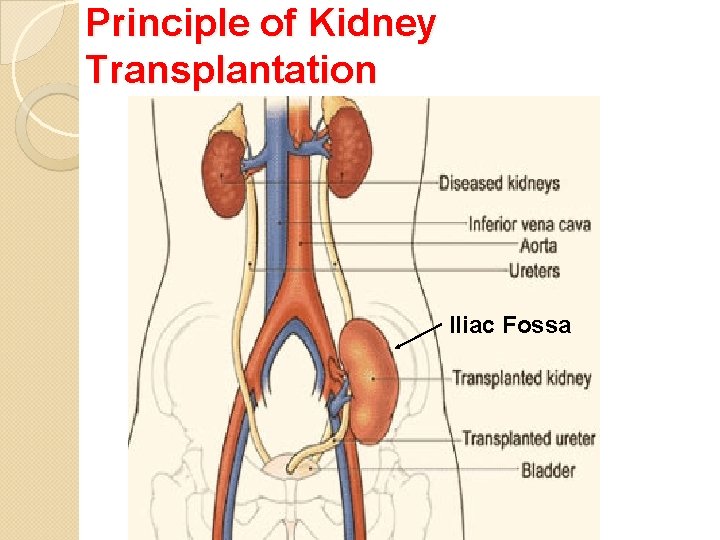
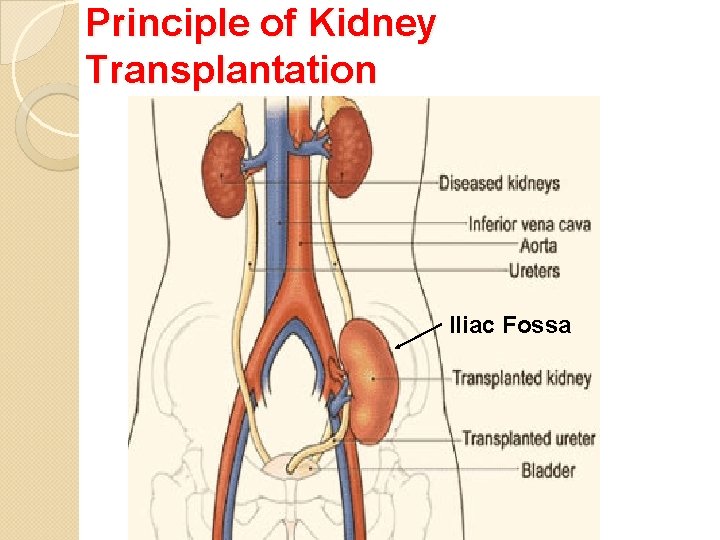
Principle of Kidney Transplantation Iliac Fossa

Thanks !! ckchiang@ntu. edu. tw
 Res extra commercium
Res extra commercium Ira pré renal renal e pós renal
Ira pré renal renal e pós renal Aeiou rrt
Aeiou rrt Single replacement vs double replacement
Single replacement vs double replacement Ductile vs brittle fracture
Ductile vs brittle fracture Failure to capture vs failure to sense ecg
Failure to capture vs failure to sense ecg Failure to sense vs failure to capture
Failure to sense vs failure to capture Renal failure
Renal failure Earthy look in chronic renal failure
Earthy look in chronic renal failure Treatments for acute renal failure
Treatments for acute renal failure Azotemia
Azotemia Cortical and juxtamedullary nephrons difference
Cortical and juxtamedullary nephrons difference Electrolyte replacement therapy
Electrolyte replacement therapy Occupational therapy hip replacement interventions
Occupational therapy hip replacement interventions 866-841-7659
866-841-7659 Chiang
Chiang Security response center
Security response center Implantes dentales precio chiang mai
Implantes dentales precio chiang mai Chiang
Chiang Lbo analysis
Lbo analysis Patrick chiang
Patrick chiang Mae lai village
Mae lai village Chiang kai shek
Chiang kai shek Holiday garden hotel & resort chiang mai
Holiday garden hotel & resort chiang mai Chiang kai-shek
Chiang kai-shek Iatul
Iatul Chiang kai shek
Chiang kai shek Ano ang nasyonalismo sa silangang asya
Ano ang nasyonalismo sa silangang asya Betty chiang
Betty chiang Chiang kai shek
Chiang kai shek Humanistic therapy aims to
Humanistic therapy aims to Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness integrated therapy system occupational therapy
Bioness integrated therapy system occupational therapy Welcome us bank
Welcome us bank Cappagh hospital admissions
Cappagh hospital admissions Replacement analysis in engineering economics
Replacement analysis in engineering economics Arc: a self-tuning, low overhead replacement cache
Arc: a self-tuning, low overhead replacement cache Total ionic equation example
Total ionic equation example Bayonet fuse replacement
Bayonet fuse replacement Replacement analysis in engineering economics
Replacement analysis in engineering economics Saxophone cork replacement
Saxophone cork replacement Abl flex 90
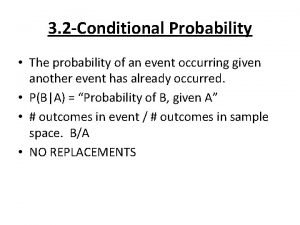
Abl flex 90 Probability of b given a
Probability of b given a Endnr
Endnr Banner document management system
Banner document management system Cache replacement championship
Cache replacement championship Replacement chart in hrm
Replacement chart in hrm Dot
Dot Human resource management chapter 5
Human resource management chapter 5 Aging algorithm page replacement
Aging algorithm page replacement Double replacement
Double replacement Greensmart 2 remote replacement
Greensmart 2 remote replacement Talcum powder vs cornstarch
Talcum powder vs cornstarch Bicarb replacement formula
Bicarb replacement formula Buffer management systems
Buffer management systems Belady's anomaly example
Belady's anomaly example Predicting single replacement reactions
Predicting single replacement reactions Ma x va = mb x vb
Ma x va = mb x vb Second chance page replacement algorithm
Second chance page replacement algorithm Adaptive replacement cache
Adaptive replacement cache Single replacement example
Single replacement example Meal replacement programs
Meal replacement programs