Clinical decision support systems in child and adolescent

- Slides: 40
Clinical decision support systems in child and adolescent psychiatry: a systematic review Bilal Hamdar
Contents. 01. 02. 03. Introduction Methods Results 04. 05. Validation of reviewed CDSS Discussion 06. Conclusions
01. Introduction Psychiatric disorders are among the most prevalent and impairing conditions in childhood and adolescence. However, frontline health providers (e. g. GPs, child protection workers, public health nurses, paediatricians) are not adequately trained to address these ubiquitous problems. This results in great social and economic costs.
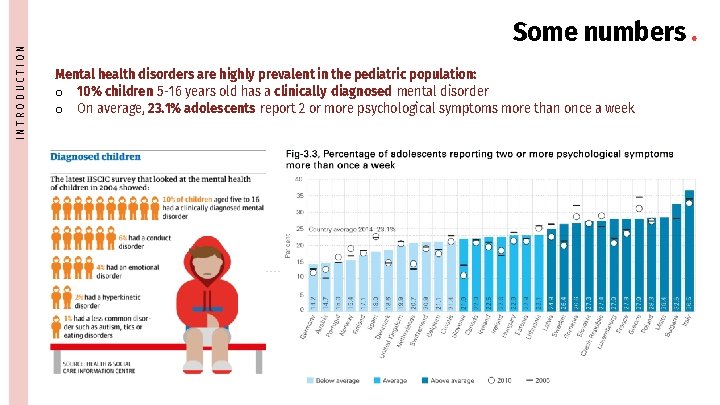
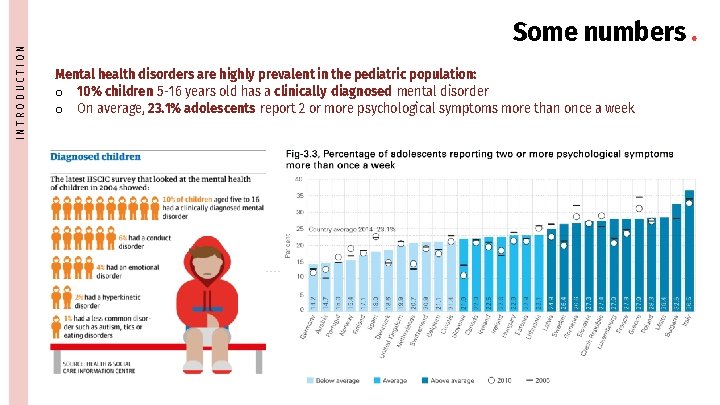
INTRODUCTION Some numbers. Mental health disorders are highly prevalent in the pediatric population: o 10% children 5 -16 years old has a clinically diagnosed mental disorder o On average, 23. 1% adolescents report 2 or more psychological symptoms more than once a week
INTRODUCTION Lack of a real support system. • Still less than 1/3 of all mental health disorders cases in the EU receive actual treatment • Number of suitably trained specialists providers (i. e. child and adolescent psychiatrists and psychologists) per 100, 000 pediatric population is very low max 26 in Finland – min 4 in Albania • In most countries, training programs for pediatricians, GPs, nurses and other allied professionals – that are most likely the first to encounter these youth – contain LITTLE or NO TRAINING on child and adolescent mental health • Significant gap with a complete lack of EARLY DETECTION/DIAGNOSIS and INTERVENTION/THERAPY which might mitigate the long-term consequences of such conditions.
INTRODUCTION Great social & economic impact. Disability Decreased Qo. L Decreased productivity Healthcare costs Decreased productivity
INTRODUCTION
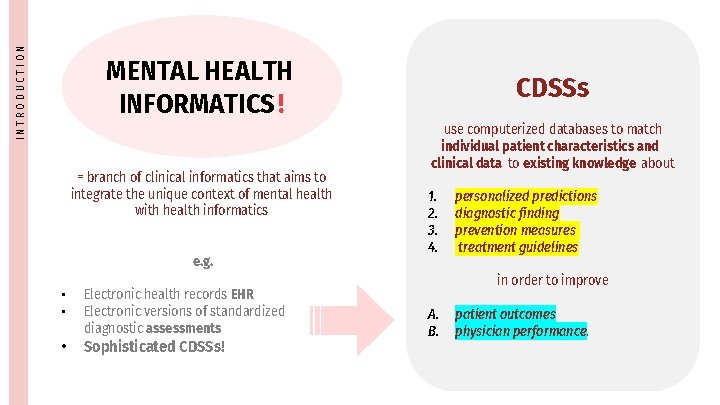
INTRODUCTION MENTAL HEALTH INFORMATICS! = branch of clinical informatics that aims to integrate the unique context of mental health with health informatics e. g. • • Electronic health records EHR Electronic versions of standardized diagnostic assessments • Sophisticated CDSSs!
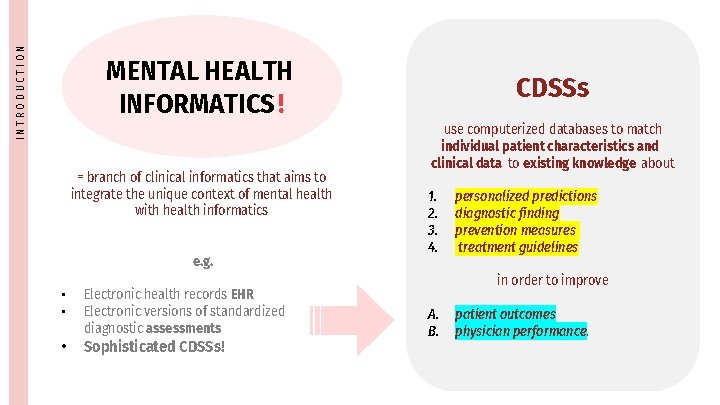
INTRODUCTION MENTAL HEALTH INFORMATICS! = branch of clinical informatics that aims to integrate the unique context of mental health with health informatics e. g. • • Electronic health records EHR Electronic versions of standardized diagnostic assessments • Sophisticated CDSSs! CDSSs use computerized databases to match individual patient characteristics and clinical data to existing knowledge about 1. 2. 3. 4. personalized predictions diagnostic finding prevention measures treatment guidelines in order to improve A. B. patient outcomes physician performance.
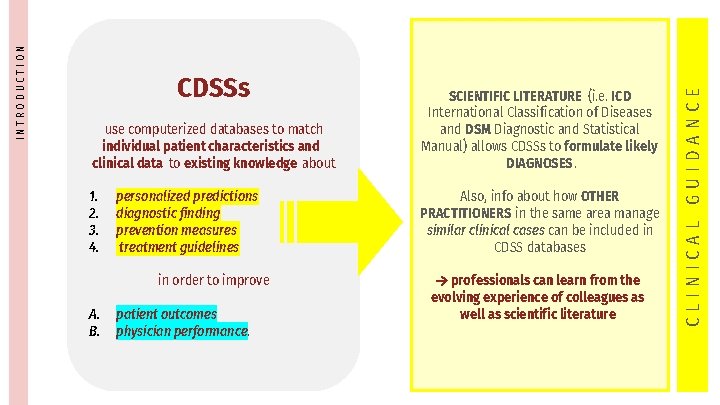
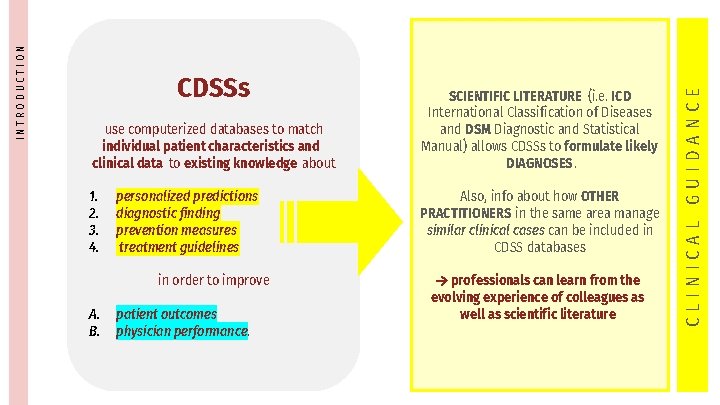
use computerized databases to match individual patient characteristics and clinical data to existing knowledge about SCIENTIFIC LITERATURE (i. e. ICD International Classification of Diseases and DSM Diagnostic and Statistical Manual) allows CDSSs to formulate likely DIAGNOSES. 1. 2. 3. 4. Also, info about how OTHER PRACTITIONERS in the same area manage similar clinical cases can be included in CDSS databases personalized predictions diagnostic finding prevention measures treatment guidelines in order to improve A. B. patient outcomes physician performance. professionals can learn from the evolving experience of colleagues as well as scientific literature CLINICAL GUIDANCE INTRODUCTION CDSSs
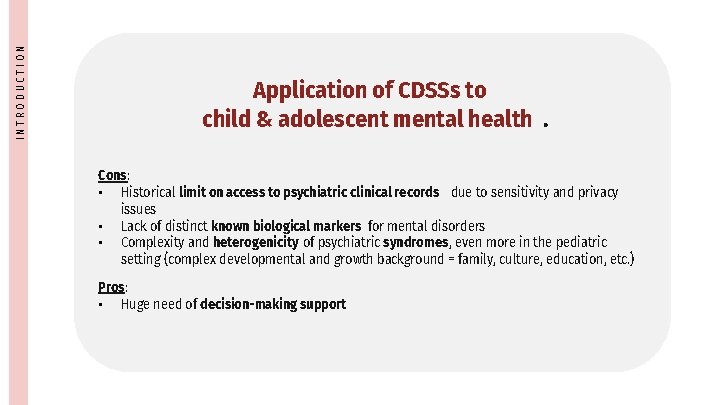
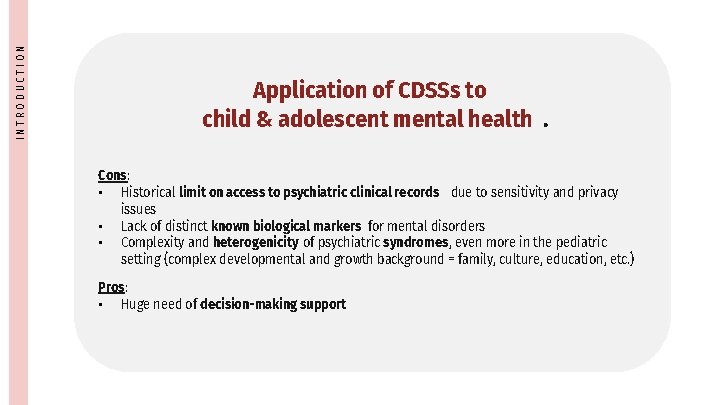
INTRODUCTION Application of CDSSs to child & adolescent mental health. Cons: • Historical limit on access to psychiatric clinical records due to sensitivity and privacy issues • Lack of distinct known biological markers for mental disorders • Complexity and heterogenicity of psychiatric syndromes, even more in the pediatric setting (complex developmental and growth background = family, culture, education, etc. ) Pros: • Huge need of decision-making support
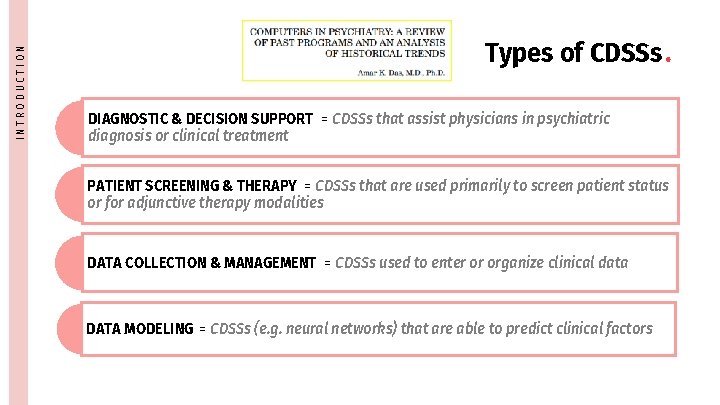
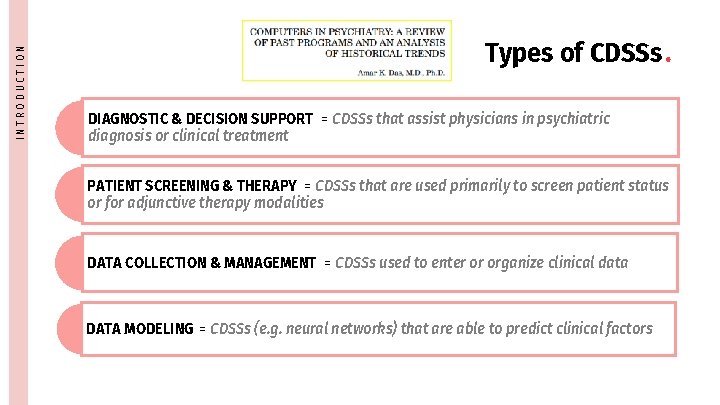
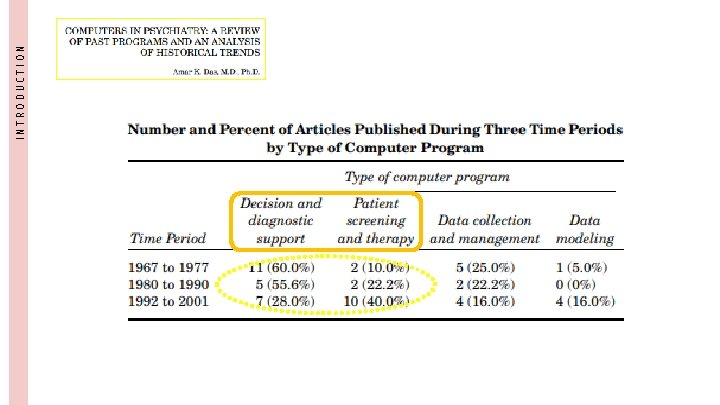
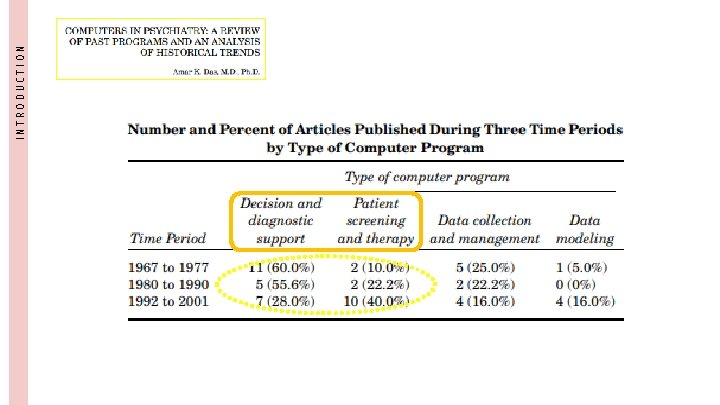
INTRODUCTION Types of CDSSs. DIAGNOSTIC & DECISION SUPPORT = CDSSs that assist physicians in psychiatric diagnosis or clinical treatment PATIENT SCREENING & THERAPY = CDSSs that are used primarily to screen patient status or for adjunctive therapy modalities DATA COLLECTION & MANAGEMENT = CDSSs used to enter or organize clinical data DATA MODELING = CDSSs (e. g. neural networks) that are able to predict clinical factors
INTRODUCTION
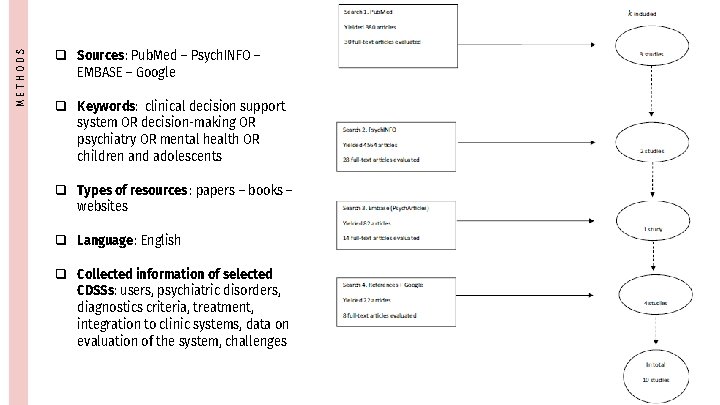
02. Methods The paper offers a systematic review of currently available CDSS for child and adolescent mental health disorders, included their strengths and weaknesses. Applying strict elegibility and inclusion criteria, 10 studies were selected out of 5048.
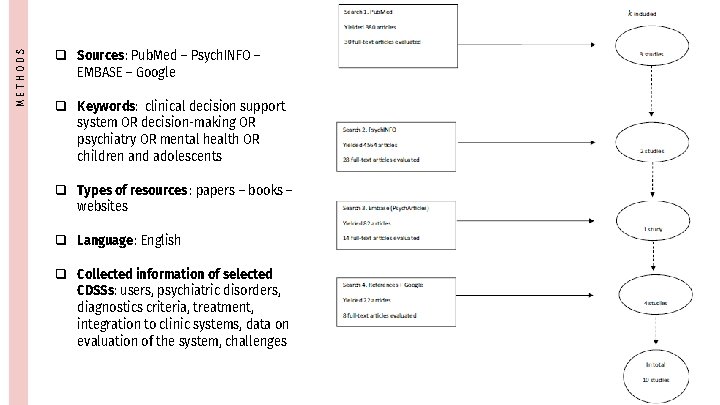
METHODS q Sources: Pub. Med – Psych. INFO – EMBASE – Google q Keywords: clinical decision support system OR decision-making OR psychiatry OR mental health OR children and adolescents q Types of resources : papers – books – websites q Language: English q Collected information of selected CDSSs: users, psychiatric disorders, diagnostics criteria, treatment, integration to clinic systems, data on evaluation of the system, challenges
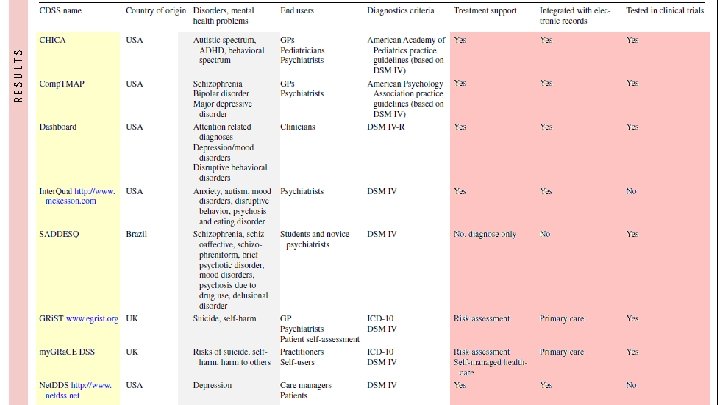
03. Results Altogether, 8 original CDSSs were designed to support clinicians when dealing with specific pediatric mental or behavioural disorders, e. g. depression, schizophrenia, suicide, other. The reviewed papers included 1968 patients.
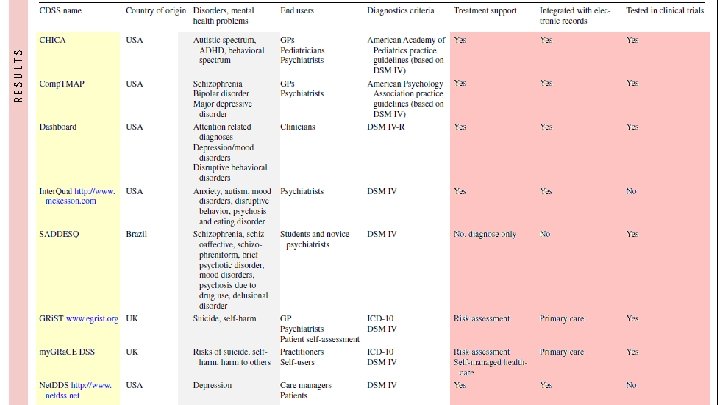
RESULTS
04. Evaluation & validation of the reviewed CDSS Some positive results were reported for almost all CDSSs.
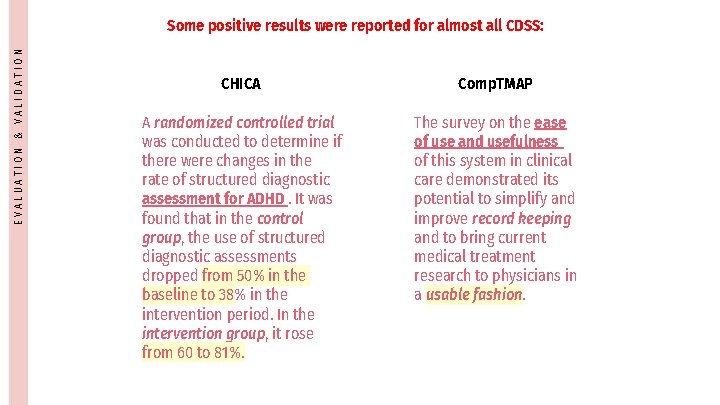
EVALUATION & VALIDATION Some positive results were reported for almost all CDSS: CHICA Comp. TMAP A randomized controlled trial was conducted to determine if there were changes in the rate of structured diagnostic assessment for ADHD. It was found that in the control group, the use of structured diagnostic assessments dropped from 50% in the baseline to 38% in the intervention period. In the intervention group, it rose from 60 to 81%. The survey on the ease of use and usefulness of this system in clinical care demonstrated its potential to simplify and improve record keeping and to bring current medical treatment research to physicians in a usable fashion.
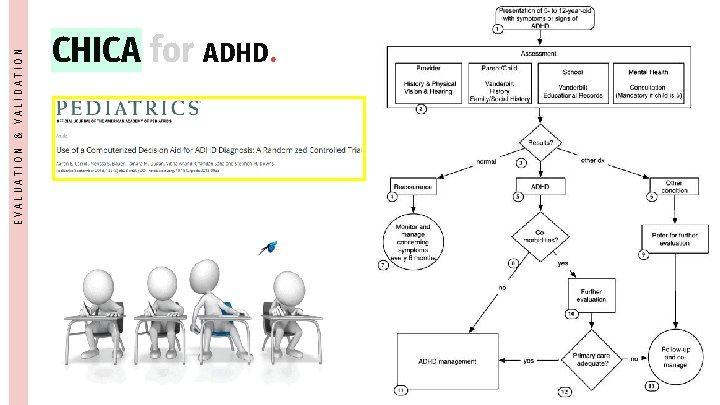
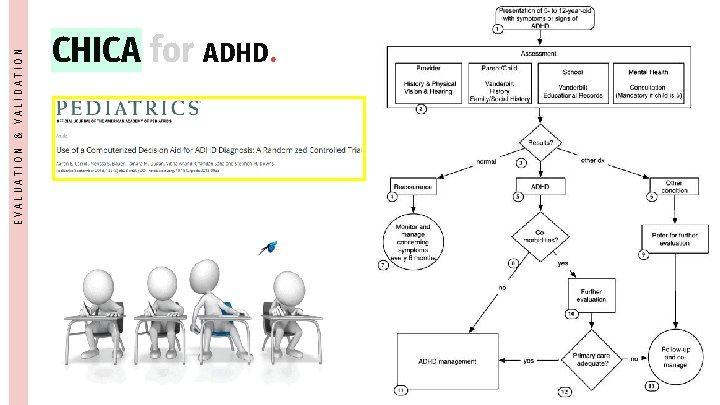
EVALUATION & VALIDATION CHICA for ADHD.
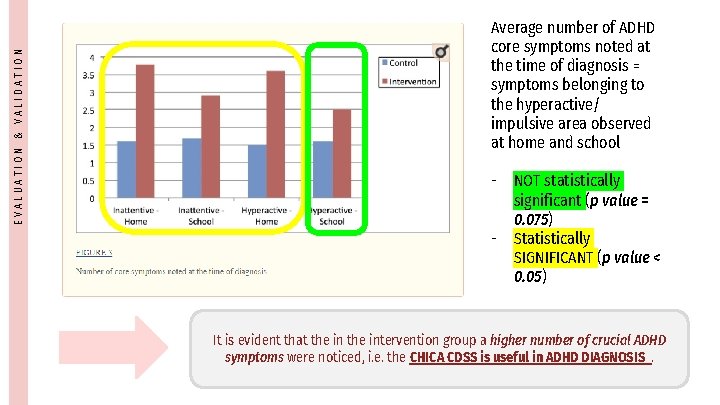
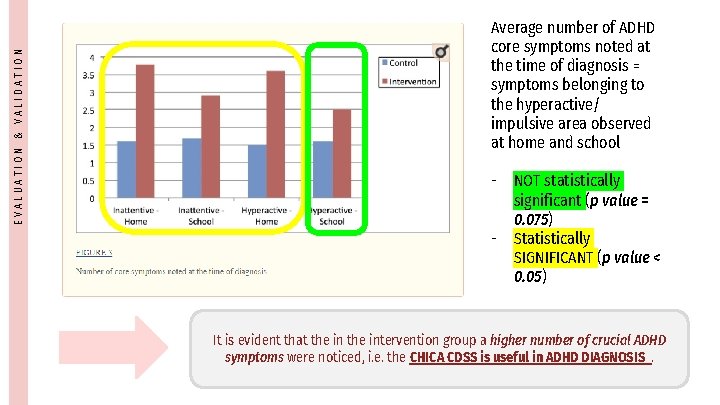
EVALUATION & VALIDATION Average number of ADHD core symptoms noted at the time of diagnosis = symptoms belonging to the hyperactive/ impulsive area observed at home and school - NOT statistically significant (p value = 0. 075) - Statistically SIGNIFICANT (p value < 0. 05) It is evident that the intervention group a higher number of crucial ADHD symptoms were noticed, i. e. the CHICA CDSS is useful in ADHD DIAGNOSIS.
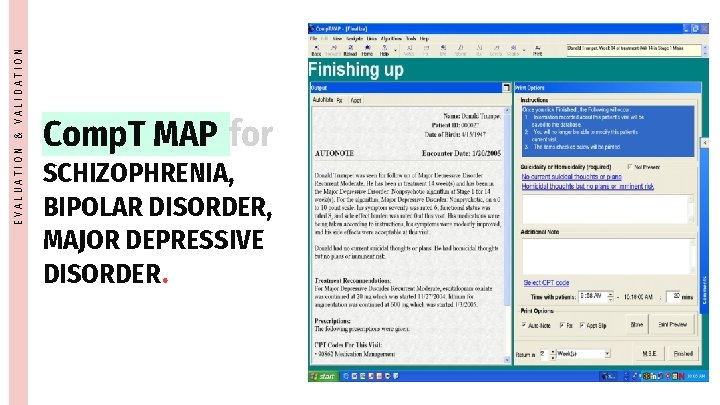
EVALUATION & VALIDATION Comp. T MAP for SCHIZOPHRENIA, BIPOLAR DISORDER, MAJOR DEPRESSIVE DISORDER.
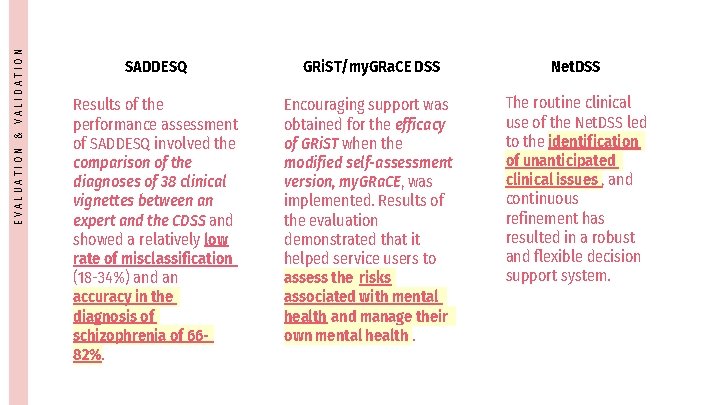
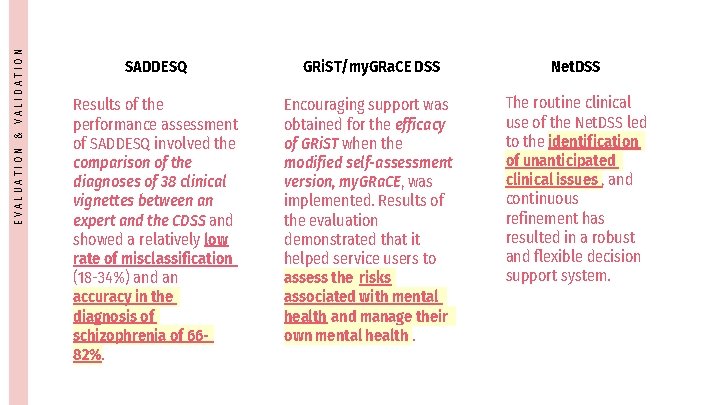
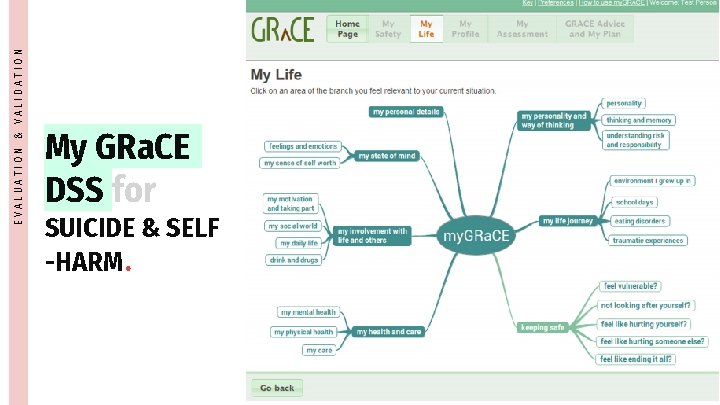
EVALUATION & VALIDATION SADDESQ GRi. ST/my. GRa. CE DSS Net. DSS Results of the performance assessment of SADDESQ involved the comparison of the diagnoses of 38 clinical vignettes between an expert and the CDSS and showed a relatively low rate of misclassification (18 -34%) and an accuracy in the diagnosis of schizophrenia of 6682%. Encouraging support was obtained for the efficacy of GRi. ST when the modified self-assessment version, my. GRa. CE, was implemented. Results of the evaluation demonstrated that it helped service users to assess the risks associated with mental health and manage their own mental health. The routine clinical use of the Net. DSS led to the identification of unanticipated clinical issues , and continuous refinement has resulted in a robust and flexible decision support system.
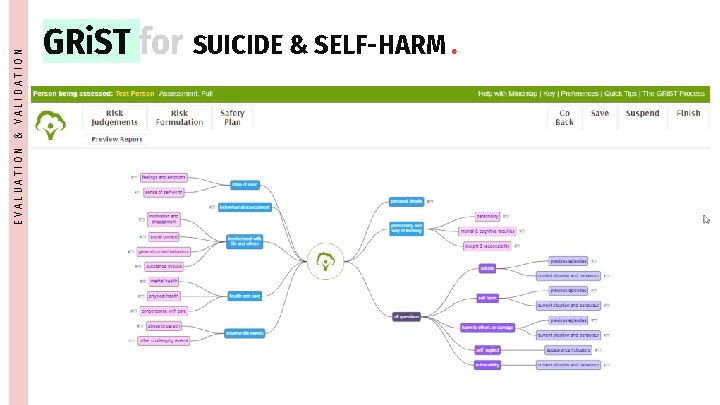
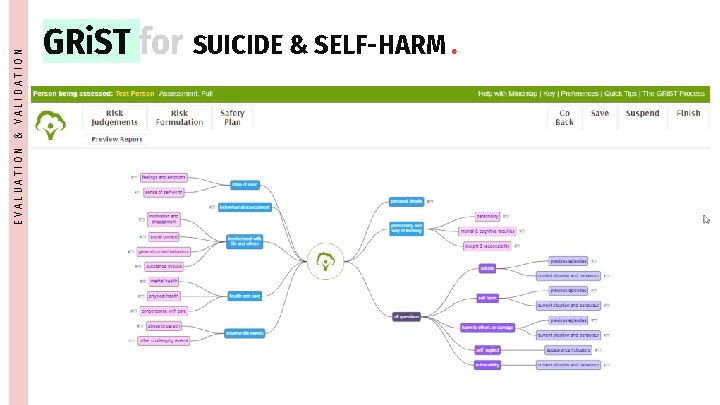
EVALUATION & VALIDATION GRi. ST for SUICIDE & SELF-HARM.
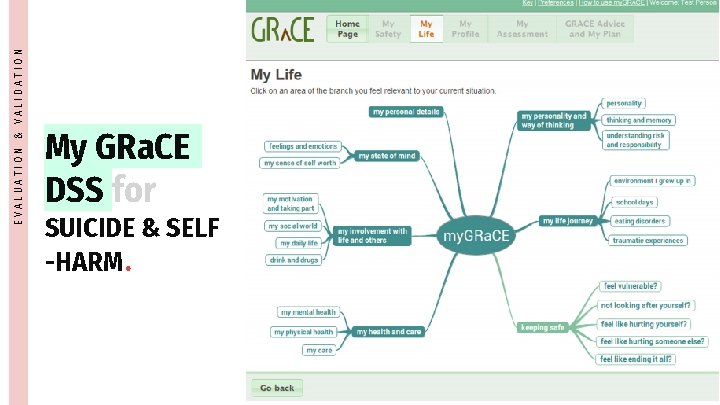
EVALUATION & VALIDATION My GRa. CE DSS for SUICIDE & SELF -HARM.
05. Discussion Despite the several upsides of using the reviewed CDSSs, there appears to be a need for the development and implementation of new and readily available CDSSs for child neuropsychiatric disorder, that could overcome the five current limitations of the existing CDSSs.
DISCUSSION Which are the PROS of implementing CDSSs in healthcare settings ?
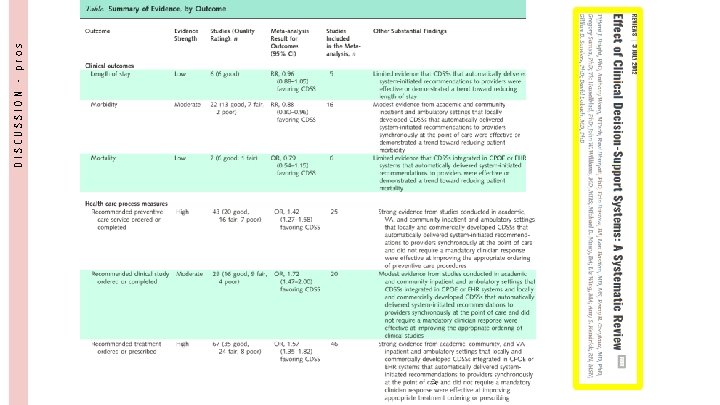
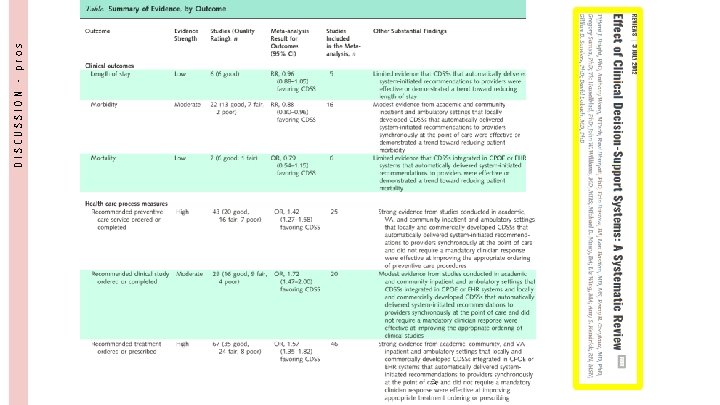
DISCUSSION - pros
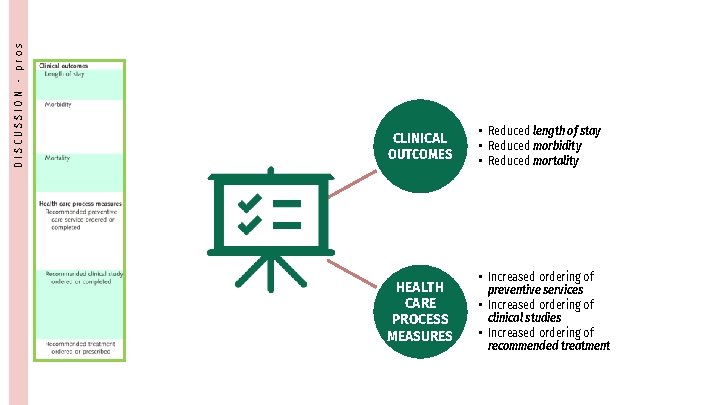
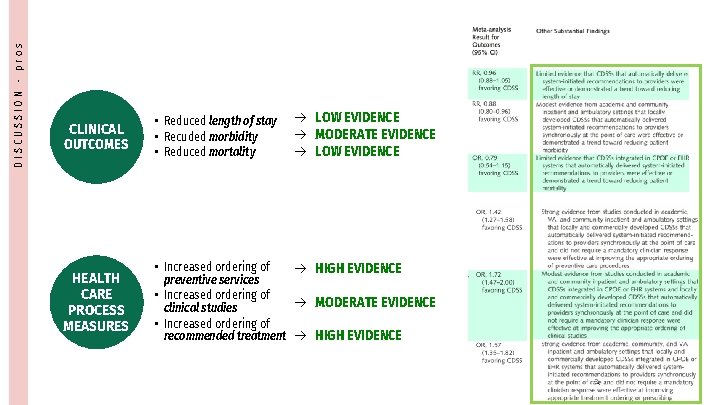
DISCUSSION - pros CLINICAL OUTCOMES HEALTH CARE PROCESS MEASURES • Reduced length of stay • Reduced morbidity • Reduced mortality • Increased ordering of preventive services • Increased ordering of clinical studies • Increased ordering of recommended treatment
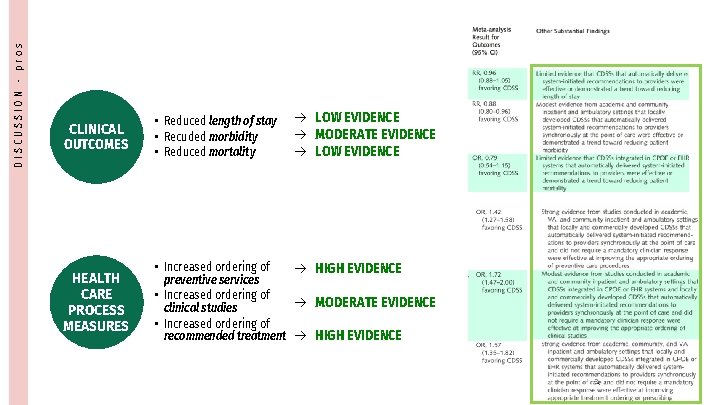
DISCUSSION - pros CLINICAL OUTCOMES HEALTH CARE PROCESS MEASURES • Reduced length of stay • Recuded morbidity • Reduced mortality LOW EVIDENCE MODERATE EVIDENCE LOW EVIDENCE • Increased ordering of HIGH EVIDENCE preventive services • Increased ordering of MODERATE EVIDENCE clinical studies • Increased ordering of recommended treatment HIGH EVIDENCE
DISCUSSION Which are the CONS of implementing CDSSs in healthcare settings ?
DISCUSSION - cons A. Physician noncompliance with the practice standards
DISCUSSION - cons A. Physician noncompliance with the practice standards B. Lack of CDSS broad integration into their respective practice
DISCUSSION - cons C. Lack of predictive models for diagnosis and appropriate therapeutic interventions A. Physician noncompliance with the practice standards B. Lack of CDSS broad integration into their respective practice
DISCUSSION - cons C. Lack of predictive models for diagnosis and appropriate therapeutic interventions A. Physician noncompliance with the practice standards B. Lack of CDSS broad integration into their respective practice D. Some CDSSs produce too many FALSE POSITIVES alerts. This leads to ALERT FATIGUE , i. g. a physician exposed to an excessive number of FP alerts becomes desensitized to ALL alerts
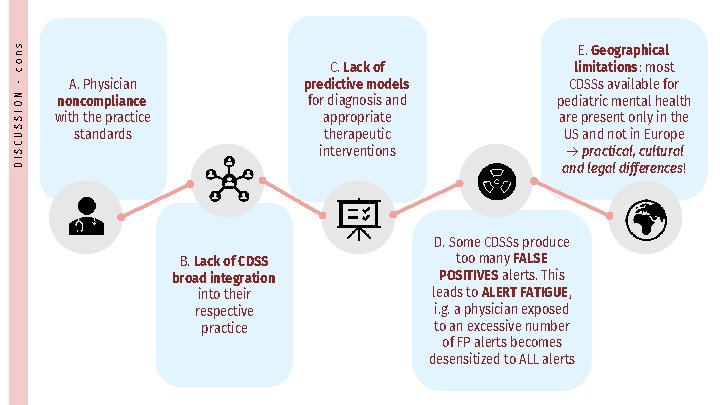
DISCUSSION - cons C. Lack of predictive models for diagnosis and appropriate therapeutic interventions A. Physician noncompliance with the practice standards B. Lack of CDSS broad integration into their respective practice E. Geographical limitations : most CDSSs available for pediatric mental health are present only in the US and not in Europe practical, cultural and legal differences! D. Some CDSSs produce too many FALSE POSITIVES alerts. This leads to ALERT FATIGUE , i. g. a physician exposed to an excessive number of FP alerts becomes desensitized to ALL alerts
06. Conclusions There is a potential for a clinical decision support system which integrates heterogeneous data sources, subject-specific computer models and highly visual data representations to improve mental health of children and adolescents.
CONCLUSIONS Pressing need for more studies of good quality, testing for diagnostic accuracy and long-term findings of CDSS implementation CDSS for child neuropsychiatric disorders should promote evidencebased, best practices , while enabling consideration variation in practices cross nationally It is necessary to implement a broader range of clinical disorders and target frontline practice environments where expertise in child and adolescent psychiatry is very limited and decision support is most needed.
References. Buckingham C, Adams A, Vail L, Kumar A, Ahmed A, Whelan A, Karasouli E (2015) Integrating service user and practitioner expertise within a webbased system for collaborative mental-health risk and safety management. Patient Educ Couns 98: 1189– 1196. Bright T et al (2012) Effect of clinical decision-support systems. A systematic review. Ann Intern Med 1: 29– 48 Koposov, R. , Fossum, S. , Frodl, T. et al. Clinical decision support systems in child and adolescent psychiatry: a systematic review. Eur Child Adolesc Psychiatry 26, 1309– 1317 (2017). Das A (2002) Computers in psychiatry: a review of past programs and an analysis of historical trends. Psychiatr Q 73(4): 351– 365 Carroll A, Bauer N, Dugan T et al (2013) Use of a computerized decision aid for ADHD diagnosis: a randomized controlled trial. Pediatrics 132: 23– 29 37. World Health Organization & Wonca (2008) Integrating mental health into primary care: a global perspective. World Health Organization, Geneva.

Thanks for your attention! b. hamdar@campus. unimib. it