Civil Air Patrol U S Air Force Auxiliary

- Slides: 28

Civil Air Patrol U. S. Air Force Auxiliary Health Services Medical Planners Course 1 hour 2019 Lt Col Thomas Janisko, CAP Chief, Health Services National Headquarters Lt Col Stephen Leighton, CAP Deputy Senior Program Director National CAP Health Services
Outline • HSO Position Description and operational reporting chain; • HSO medical planner mission; • Completion of ICS 206 for FEMA/CAP ES missions; • Activity Health Assessments.
Health Services – Position Description TRUSTED ADVISOR to the Unit Commander, Activity Director, Incident Commander, Team Leader, and Safety Officer on all matters that involve the health of the force. NOT A DECISION MAKER, but a skilled and trained presenter of multiple courses of action that meet the requirements of maintaining the health of the force. Unit Commanders, Activity Directors, Incident Commanders, and Team Leaders assume risk. Health Services Officers and Safety Officers identify risks and advise decision makers on mitigation efforts.
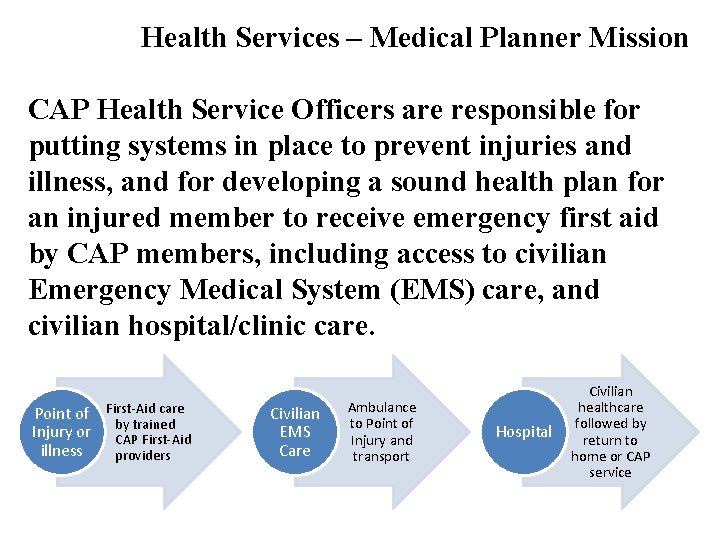
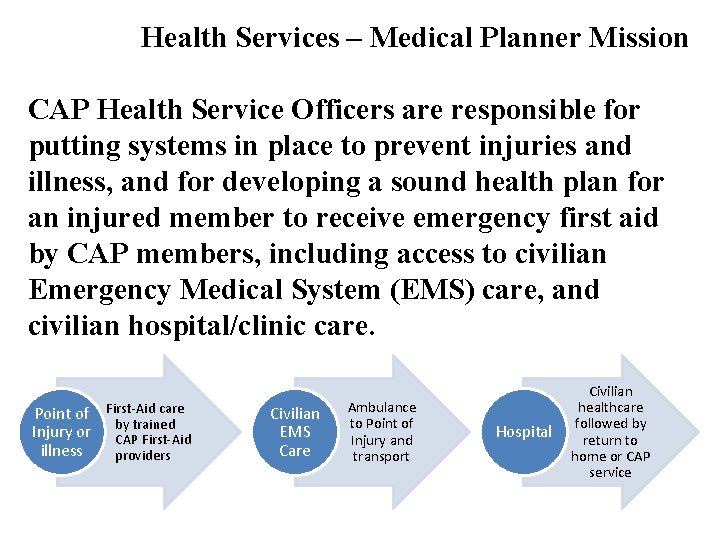
Health Services – Medical Planner Mission CAP Health Service Officers are responsible for putting systems in place to prevent injuries and illness, and for developing a sound health plan for an injured member to receive emergency first aid by CAP members, including access to civilian Emergency Medical System (EMS) care, and civilian hospital/clinic care. Point of First-Aid care by trained Injury or CAP First-Aid illness providers Civilian EMS Care Ambulance to Point of Injury and transport Hospital Civilian healthcare followed by return to home or CAP service
Health Services – Operational Reporting Chain • Depending on your situation, your operational reporting chain may be different. • Proactively identifying how your operational reporting chain works is important to reduce confusion and improve communications. • As a general rule, for confidential health discussions, it is important to speak directly with the Commander, Incident Commander, or Activity Director.
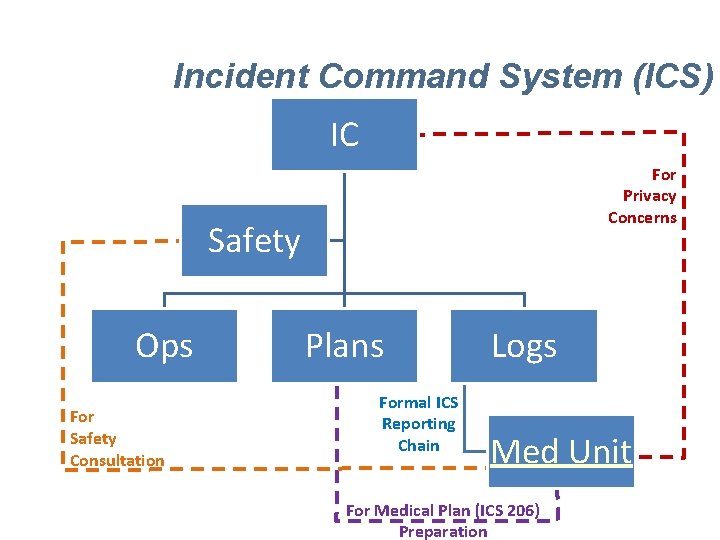
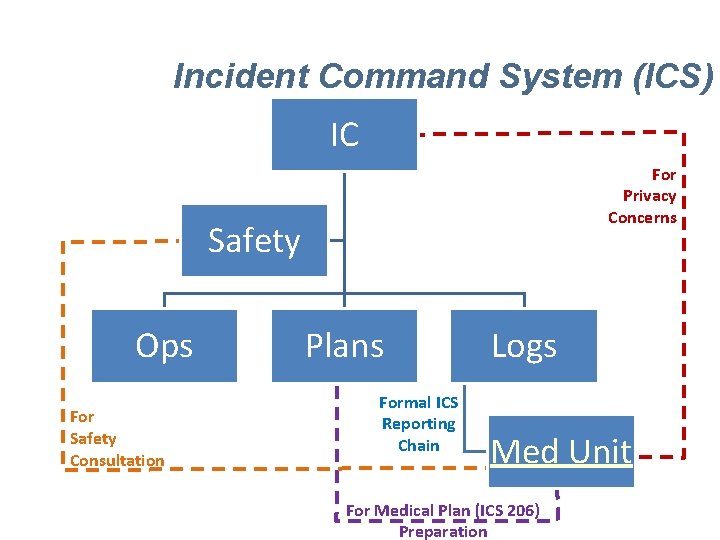
Incident Command System (ICS) IC For Privacy Concerns Safety Ops For Safety Consultation Plans Formal ICS Reporting Chain Logs Med Unit For Medical Plan (ICS 206) Preparation
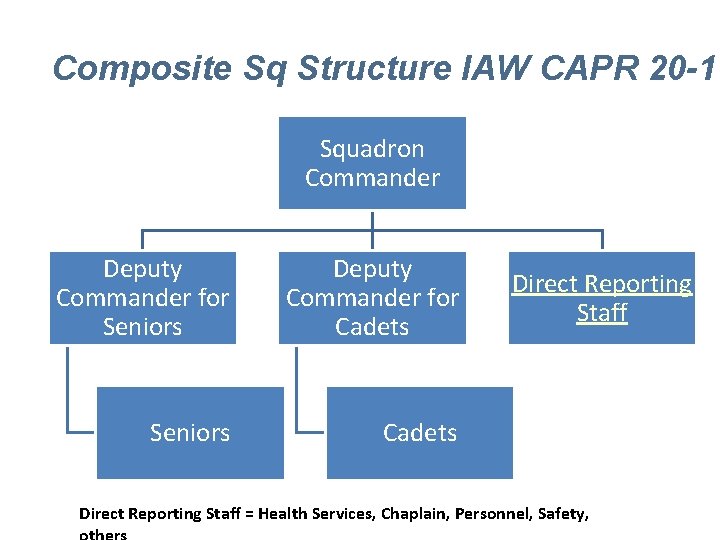
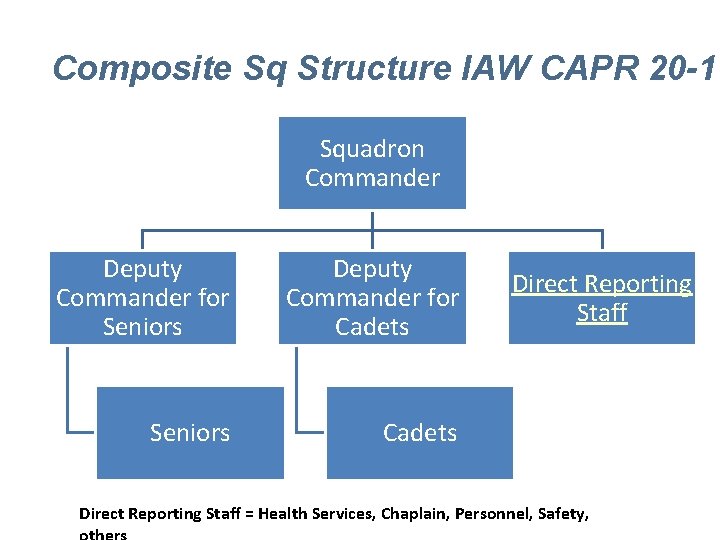
Composite Sq Structure IAW CAPR 20 -1 Squadron Commander Deputy Commander for Seniors Deputy Commander for Cadets Seniors Cadets Direct Reporting Staff = Health Services, Chaplain, Personnel, Safety,
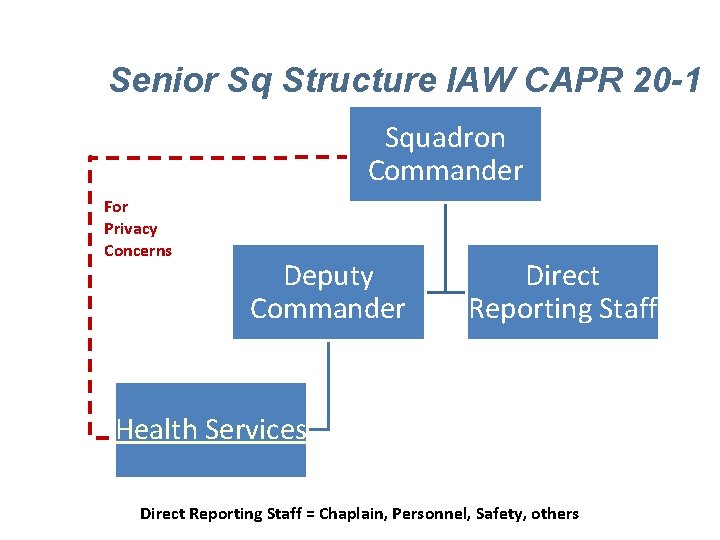
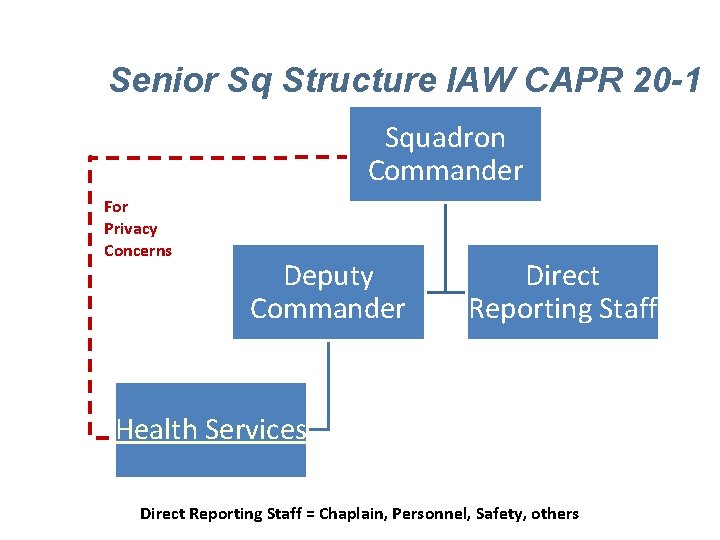
Senior Sq Structure IAW CAPR 20 -1 Squadron Commander For Privacy Concerns Deputy Commander Direct Reporting Staff Health Services Direct Reporting Staff = Chaplain, Personnel, Safety, others
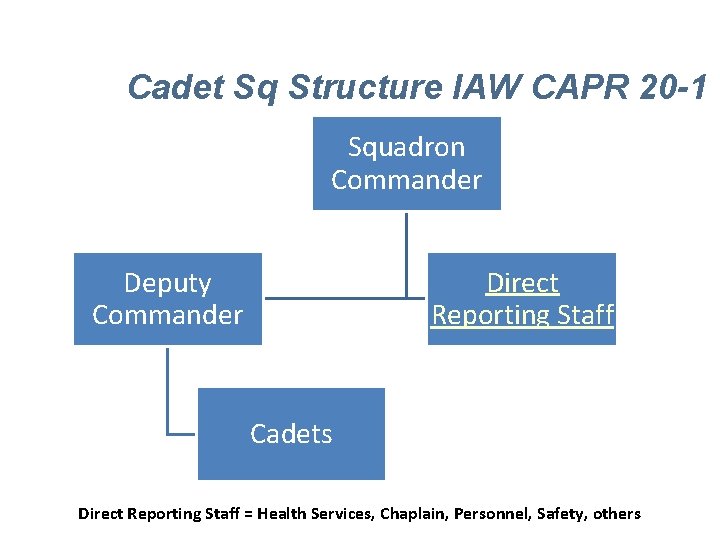
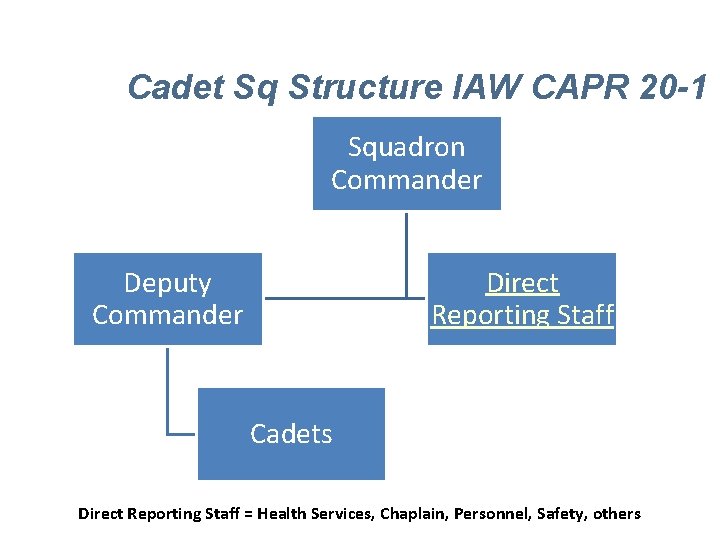
Cadet Sq Structure IAW CAPR 20 -1 Squadron Commander Deputy Commander Direct Reporting Staff Cadets Direct Reporting Staff = Health Services, Chaplain, Personnel, Safety, others
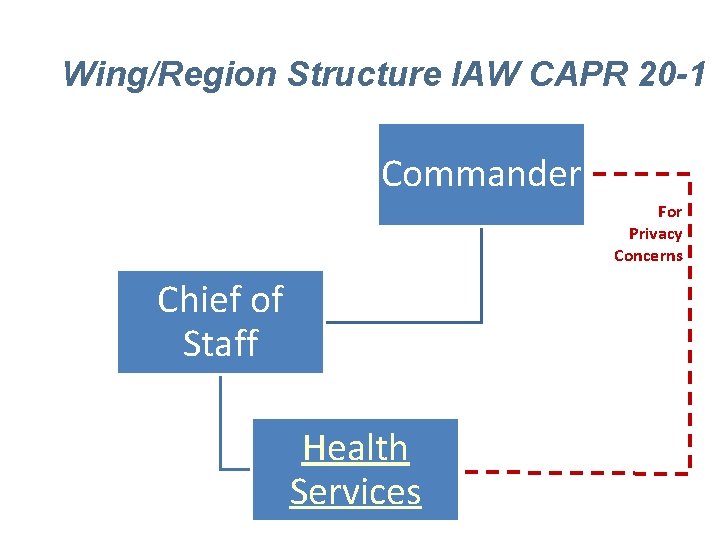
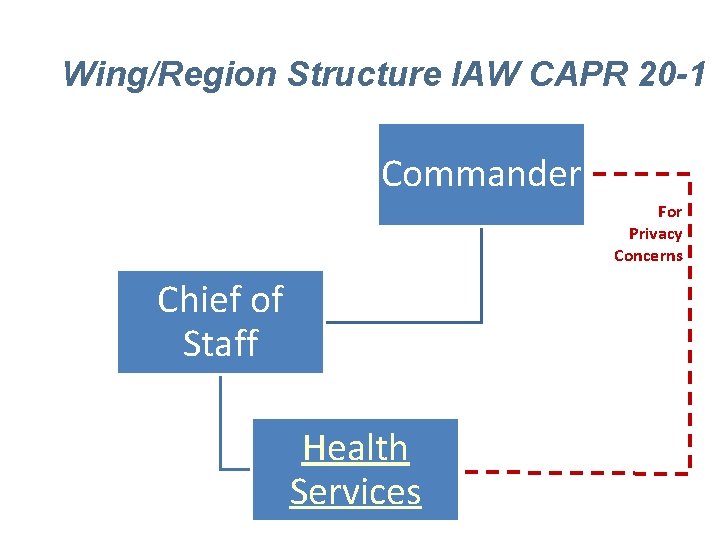
Wing/Region Structure IAW CAPR 20 -1 Commander For Privacy Concerns Chief of Staff Health Services
General Medical Planning Support • Step 1 -Mission analysis (e. g. , who, what, where, when, and how). Essentially, what are the mission requirements and potential challenges from a health perspective? • Step 2 -Evaluation of health & safety factors: • General factors - environment (terrain, temperature, humidity, weather, accessibility of roads/trails for helicopters, ATVs, litter teams, ground ambulances); • Population-at-risk - number of people, general ages, fitness level, amount of and security of food/water); https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 558384/
Medical Planning – Emergency Services • Step 2 -Evaluation of factors - continued: • Medical factors—estimation of injury/illness risk and type; first-aid capabilities within CAP groups/teams/units; location of civilian medical facilities and capabilities; location of casualty collection points / fire stations / ambulance facilities; • Complete ICS 206 in conjunction with Safety Officer; https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 558384/
Medical Planning – Emergency Services • Step 3—Consideration of courses of action: • Identify different plans that will inform Command based on Light, Medium and Heavy resource availability; • Step 4—Brief the Commander on possible courses of action; • Step 5—Commander's decision; • Step 6—Implementing the plan. • Step 7—After Action review and analysis
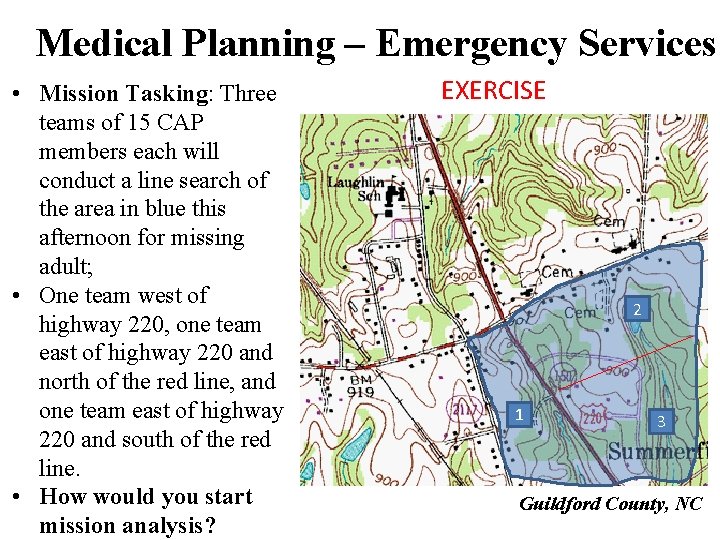
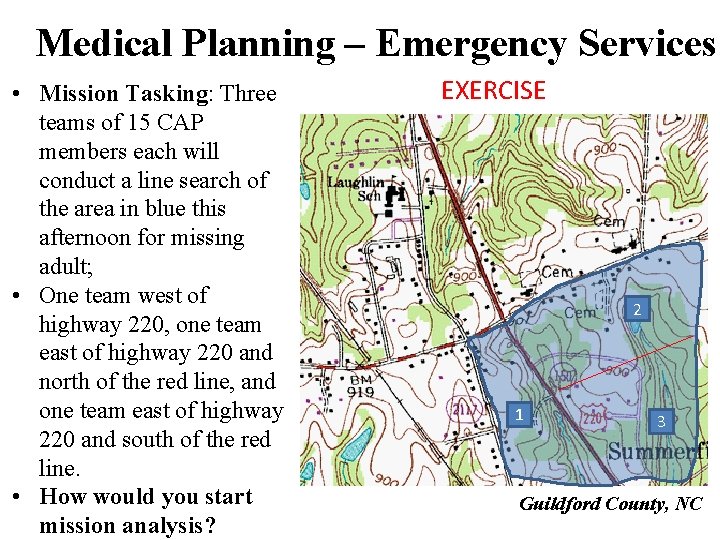
Medical Planning – Emergency Services • Mission Tasking: Three teams of 15 CAP members each will conduct a line search of the area in blue this afternoon for missing adult; • One team west of highway 220, one team east of highway 220 and north of the red line, and one team east of highway 220 and south of the red line. • How would you start mission analysis? EXERCISE 2 1 3 Guildford County, NC
General Medical Planning Support • Step 1 -Mission analysis (e. g. , who, what, where, when, and how). Essentially, what are the mission requirements and potential gaps from a health perspective? • Who: (3) CAP ground teams of 15 each; • What: performing line searches in three distinct areas for a missing adult person; • Where: 3 distinct areas along RT 220; hilly area; temperature is 90’s; rain forecasted this evening; • When: Afternoon; potentially into evening/night; • How: Walking-based search.
General Medical Planning Support • Step 1 -Mission Receipt / analysis – Potential mission gaps include hilly terrain, nightfall, temp in 90’s, rain, 45 CAP members in dispersed area; • Step 2 -Evaluation of Health & Safety factors • General factors – identify environmental factors to consider; • Population-at-risk - number of people, general ages, fitness level, amount of and security of food/water); https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 558384/
Medical Planning – Emergency Services • Step 2 -Evaluation of Health & Safety factors continued: • Medical factors – estimation of health risks for CAP members and civilian population, consider preplanning location of casualty collection points and communicating with fire stations / ambulance facilities so they know CAP is operating in the area (ICS-206); • Feasability – estimation of the Command team’s appetite for the level of health services support. • Requirements – identify the ultimate requirements needed to meet the identified factors above.
Medical Planning – Emergency Services • Step 3 – Courses of action analysis: • Light level COA – estimation of the minimal levels of resources that will generally meet the requirements. • Medium level COA – estimation of the medium level of resources that will meet the requirements and sufficiently mitigate the Commander’s risk. • Heavy level COA – estimation of the heavy level of resources that will meet the requirements and fully mitigate the Commander’s risk. • Areas of Risk – estimate the risk level that the Commander’s will have to accept for each course of action.
Medical Planning – Emergency Services • Step 2 - 3 – Strategic Exercise / Comparison; Place a map of your area of operations on a table and roll 3 -6 die. Where the dice land will be the geographical areas and types of injury/illness to identify potential medical planning shortfalls using the following numerical assignments for your dice: • • • 1 – Adult: chest pain in an adult with a weight of 256 lbs. 2 – Adult: stroke-like symptoms 190 lbs. 3 – Cadet: ankle injury highly suspect for fracture 200 lbs. 4 – Cadet: fall from 8 feet with loss of consciousness 190 lbs. 5 – Adults: accident with 2 adults in a vehicle 6 – Adult: requiring CPR
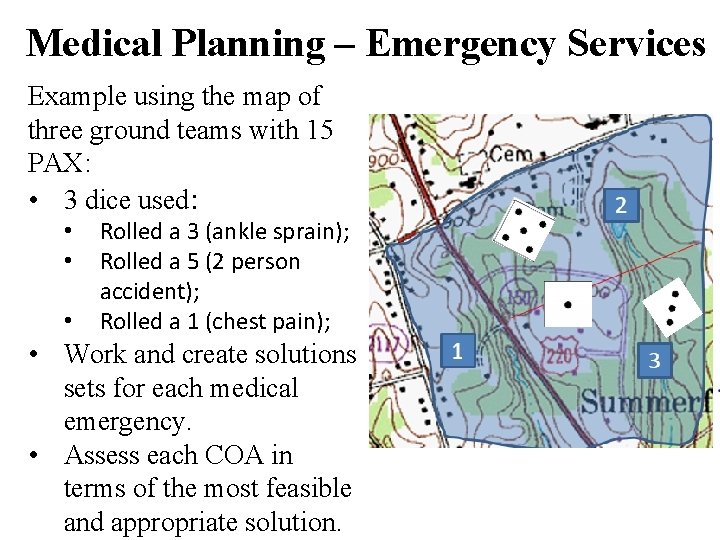
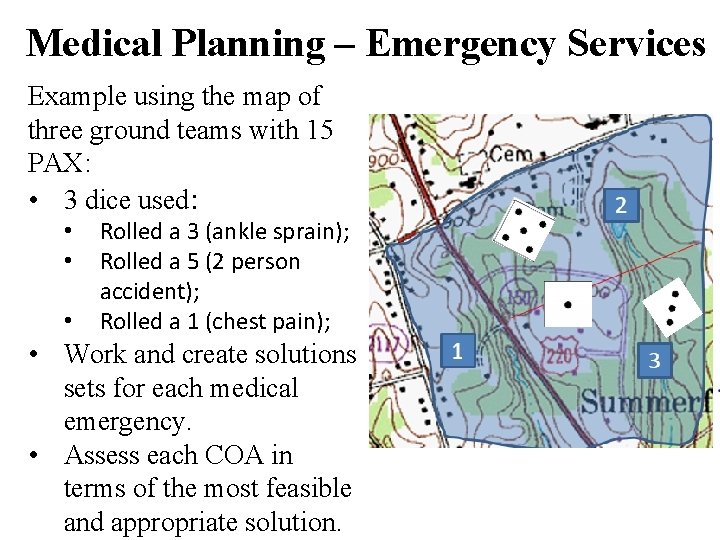
Medical Planning – Emergency Services Example using the map of three ground teams with 15 PAX: • 3 dice used: • • • Rolled a 3 (ankle sprain); Rolled a 5 (2 person accident); Rolled a 1 (chest pain); • Work and create solutions sets for each medical emergency. • Assess each COA in terms of the most feasible and appropriate solution.
Medical Planning – Emergency Services • Step 4 – Brief Commander on potential COA. • Your goal is to mitigate risk and preserve the health of the force. • Within the context of the entire mission/incident/activity, choose the course of action that: • Fulfills the Commanders requirements; • Fulfills the mission/incident/activities requirements, and; • Fulfills the feasibility requirements • As a reminder, the Commander chooses the course of action…you job is to communicate your methodology, assessment of risk, and recommendation.
Medical Planning – Emergency Services Step 4 – Brief Commander on potential COA - cont. • As with all healthcare operations, clear written documentation of your recommendations is required. • Commanders are busy people and will likely want to know the “BLUF” (pronounced “bluff”) or bottom line up front – a single sentence about your recommendation.
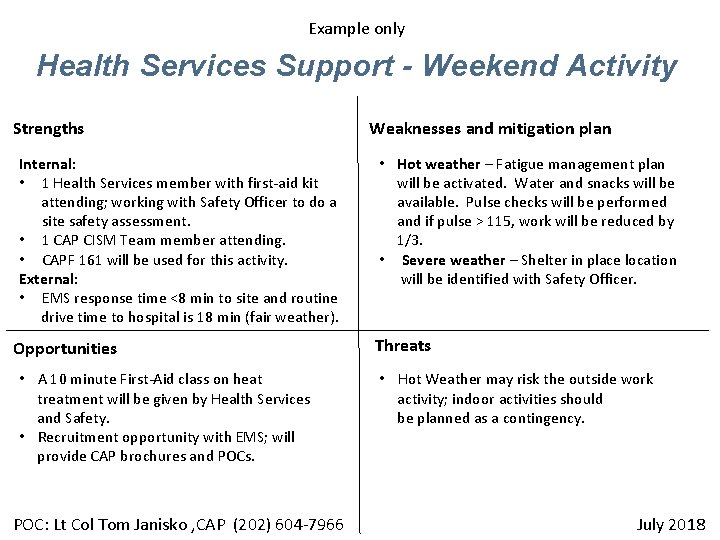
Medical Planning – Emergency Services Step 4 – Brief Commander on potential COA - cont. • Commanders will likely be familiar with the military decision making process (MDMP), so you should frame your decision making in a similar fashion. • Use a Strength, Weakness, Opportunity, and Threat or “SWOT” slide to visually explain what your thought process was for your conclusion (an example is on the next page).
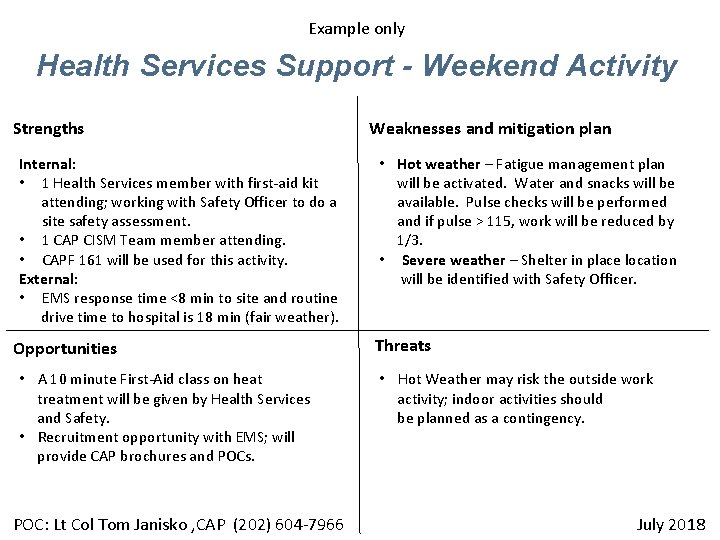
Example only Health Services Support - Weekend Activity Strengths Internal: • 1 Health Services member with first-aid kit attending; working with Safety Officer to do a site safety assessment. • 1 CAP CISM Team member attending. • CAPF 161 will be used for this activity. External: • EMS response time <8 min to site and routine drive time to hospital is 18 min (fair weather). Opportunities • A 10 minute First-Aid class on heat treatment will be given by Health Services and Safety. • Recruitment opportunity with EMS; will provide CAP brochures and POCs. POC: Lt Col Tom Janisko , CAP (202) 604 -7966 Weaknesses and mitigation plan • Hot weather – Fatigue management plan will be activated. Water and snacks will be available. Pulse checks will be performed and if pulse > 115, work will be reduced by 1/3. • Severe weather – Shelter in place location will be identified with Safety Officer. Threats • Hot Weather may risk the outside work activity; indoor activities should be planned as a contingency. July 2018
Medical Planning – Emergency Services Sample BLUF: “Sir, to meet your requirement of hosting a weekend activity, health services will have one Health Service Officer present with a first-aid kit, perform an assessment of the site with the Safety Officer, ensure the local EMS system knows our location, and actively monitor the heat; no showstoppers from a health perspective, but I recommend a contingency plan for indoor activities in the case of excessively hot or severe weather”.
Medical Planning – Emergency Services Step 5: Commander’s Decision Step 6: COA Implementation and follow-up Step 7: After Action review and analysis • Work together with the activity Safety Officer to review the COA and the outcome of the implementation of that COA; • Look for opportunities to improve COA planning in the future.
Resources CAP HSO Webpage on e. Services • Requirements for HSO Specialty Track; • Health & Wellness Presentations for your use; • HSO training materials; • Best practices; • And more.
Good Luck Planning and ensure our force is healthy and safe A F S C IP 214 5 D#20 -g 05 -03 -95
 Cap stem badge
Cap stem badge Civil air patrol national conference
Civil air patrol national conference Malcolm kyser
Malcolm kyser Civil air patrol kahoot
Civil air patrol kahoot Cap ncsa
Cap ncsa Civil air patrol model rocketry badge
Civil air patrol model rocketry badge Civil air patrol aerospace module 1
Civil air patrol aerospace module 1 Civil air patrol missouri
Civil air patrol missouri Civil air patrol strategic plan
Civil air patrol strategic plan Civil air patrol frequencies
Civil air patrol frequencies Civil air patrol powerpoint template
Civil air patrol powerpoint template Cap blues
Cap blues Civil air patrol cppt
Civil air patrol cppt Split-force patrol
Split-force patrol Split force patrol
Split force patrol Top auxiliary view
Top auxiliary view Civil rights webquest
Civil rights webquest Air higroskopis air kapiler dan air gravitasi
Air higroskopis air kapiler dan air gravitasi Ski apache web
Ski apache web Patrol tactics training
Patrol tactics training Patrol base activities
Patrol base activities Home fire safety patrol
Home fire safety patrol Clint eastwood highway patrol
Clint eastwood highway patrol Motor carrier safety assistance program
Motor carrier safety assistance program Scout method
Scout method Nissan patrol vibration problems
Nissan patrol vibration problems School crossing patrol coat
School crossing patrol coat Ics patrol
Ics patrol Nebraska state patrol concealed carry
Nebraska state patrol concealed carry