CANCER RESEARCH UK UPDATE CERVICAL SCREENING UPTAKE PACK










- Slides: 28

CANCER RESEARCH UK UPDATE

CERVICAL SCREENING UPTAKE PACK


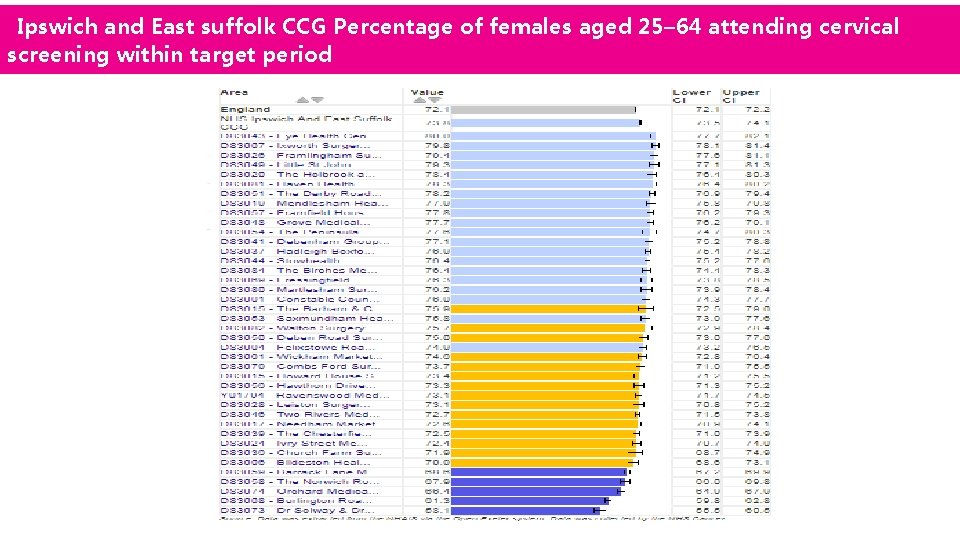
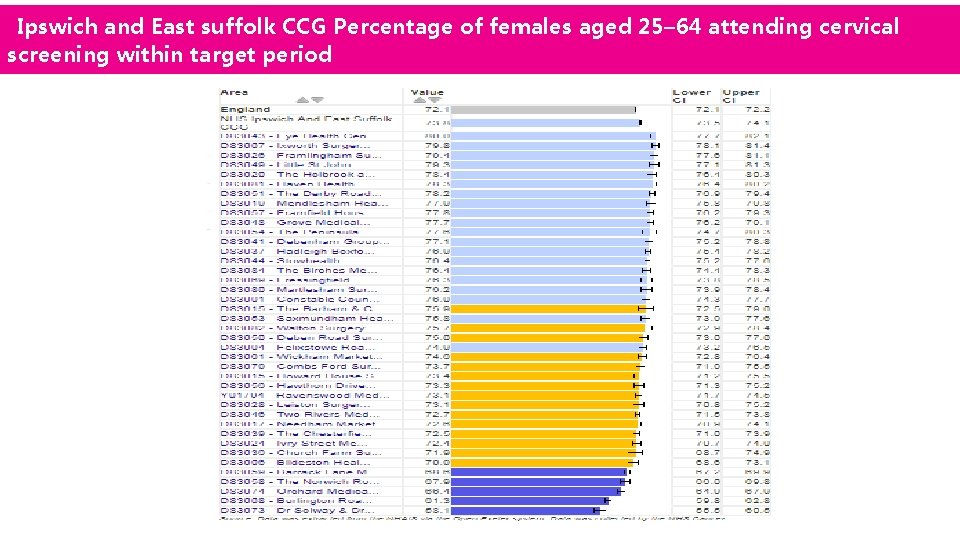
Ipswich and East suffolk CCG Percentage of females aged 25– 64 attending cervical screening within target period





PRIMARY CARE CANCER UPTAKE PACK
PRIMARY CARE CANCER UPDATE PACK 2017/18 MENDLESHAM HEALTH CENTRE Donna Reeve (CRUK Facilitator Manager East of England) E: donna. reeve@cancer. org. uk T: 07979 926403 Dr Andrew Yager Macmillan GP E: a. yager@nhs. net T: 07917454535
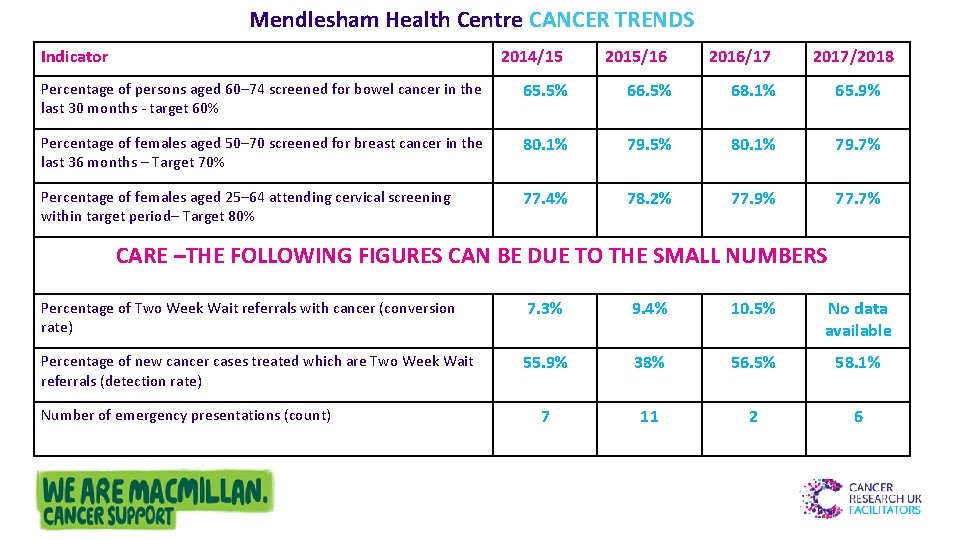
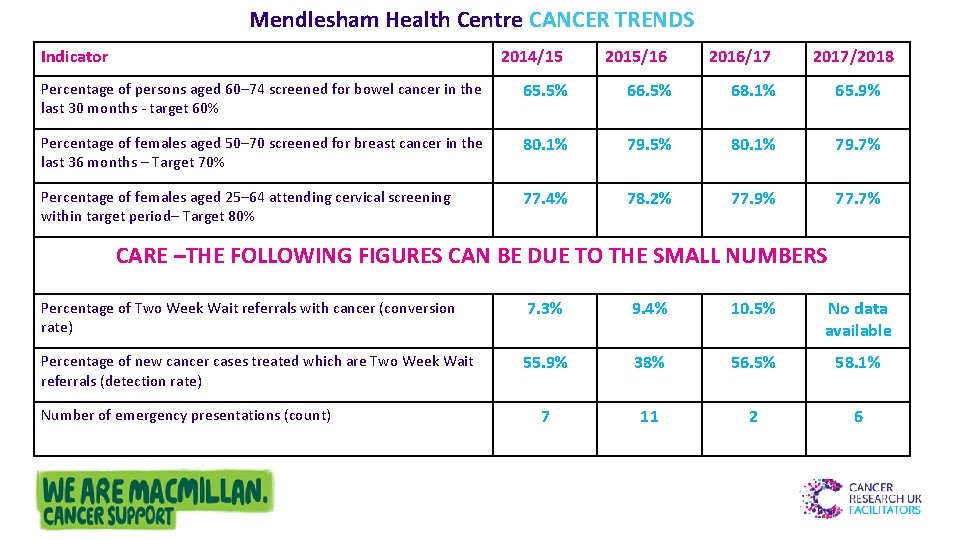
Mendlesham Health Centre CANCER TRENDS Indicator 2014/15 2015/16 2016/17 2017/2018 Percentage of persons aged 60– 74 screened for bowel cancer in the last 30 months - target 60% 65. 5% 66. 5% 68. 1% 65. 9% Percentage of females aged 50– 70 screened for breast cancer in the last 36 months – Target 70% 80. 1% 79. 5% 80. 1% 79. 7% Percentage of females aged 25– 64 attending cervical screening within target period– Target 80% 77. 4% 78. 2% 77. 9% 77. 7% CARE –THE FOLLOWING FIGURES CAN BE DUE TO THE SMALL NUMBERS Percentage of Two Week Wait referrals with cancer (conversion rate) 7. 3% 9. 4% 10. 5% No data available Percentage of new cancer cases treated which are Two Week Wait referrals (detection rate) 55. 9% 38% 56. 5% 58. 1% 7 11 2 6 Number of emergency presentations (count)
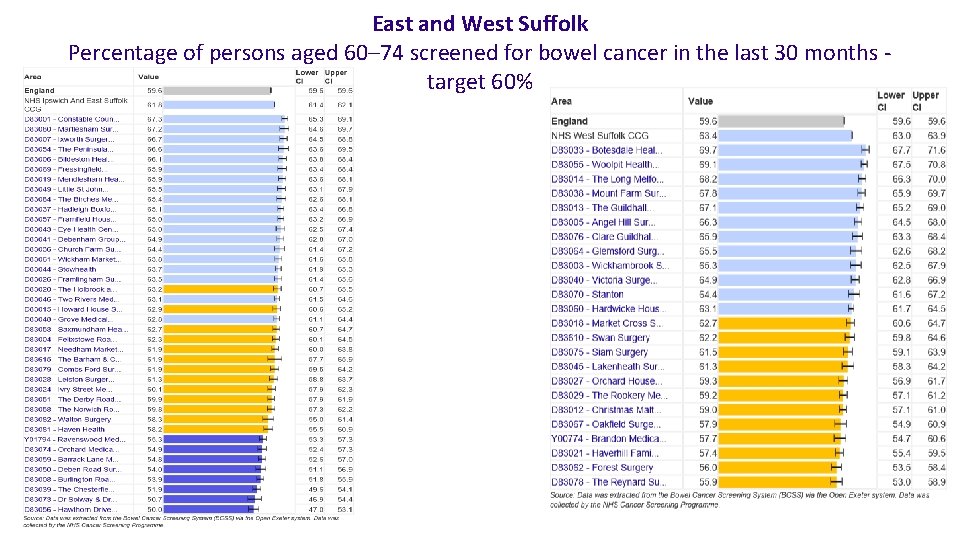
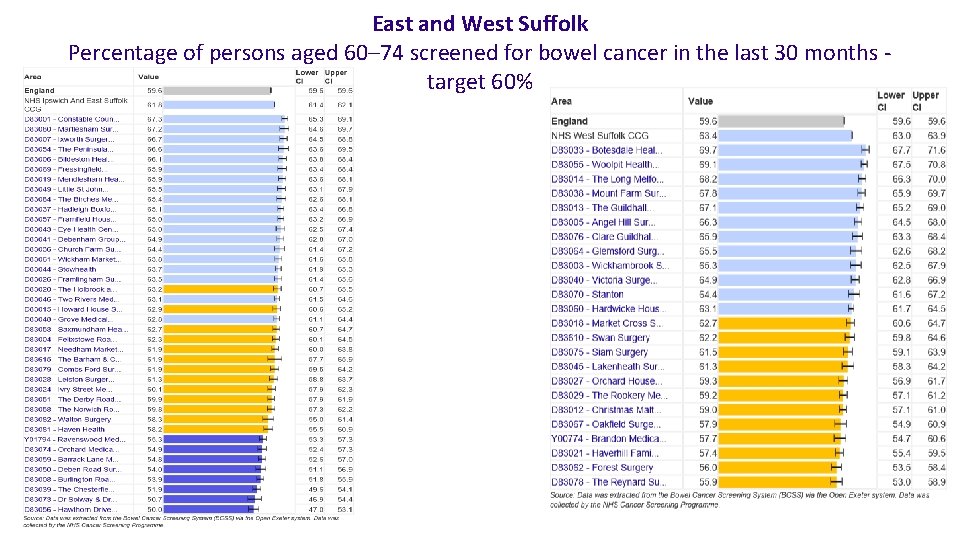
East and West Suffolk Percentage of persons aged 60– 74 screened for bowel cancer in the last 30 months target 60%
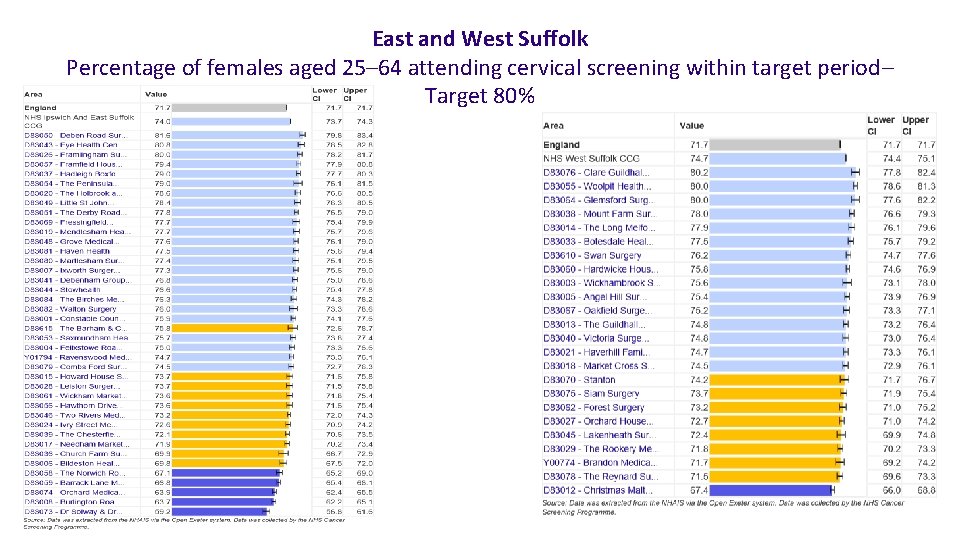
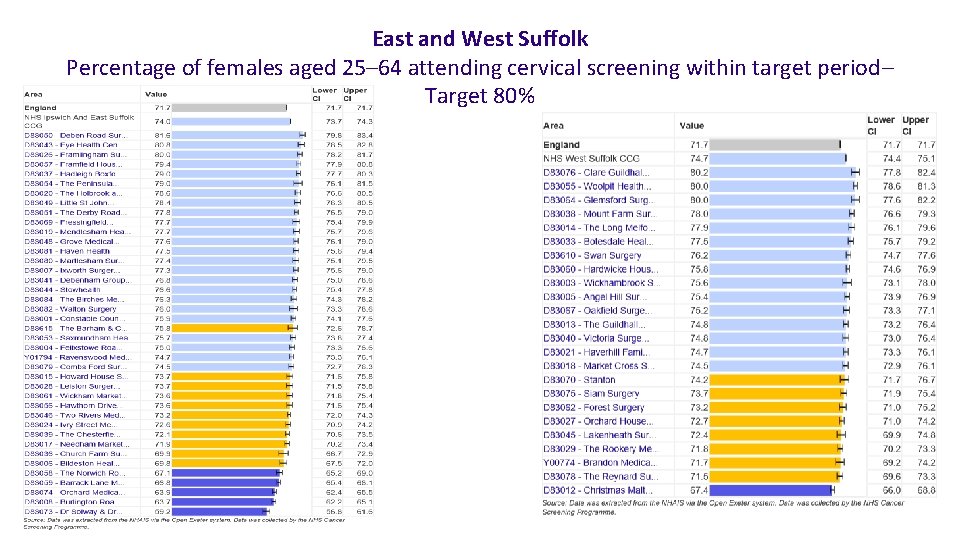
East and West Suffolk Percentage of females aged 25– 64 attending cervical screening within target period– Target 80%
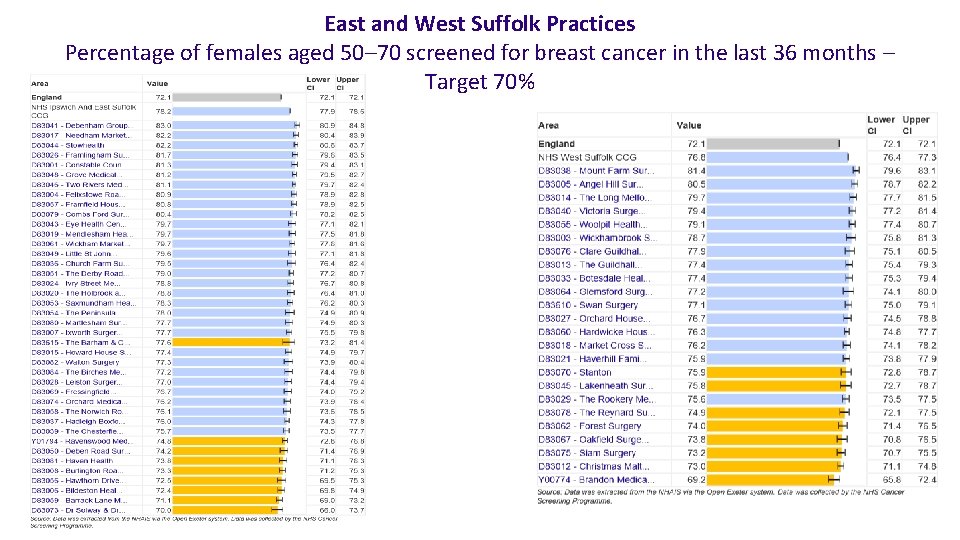
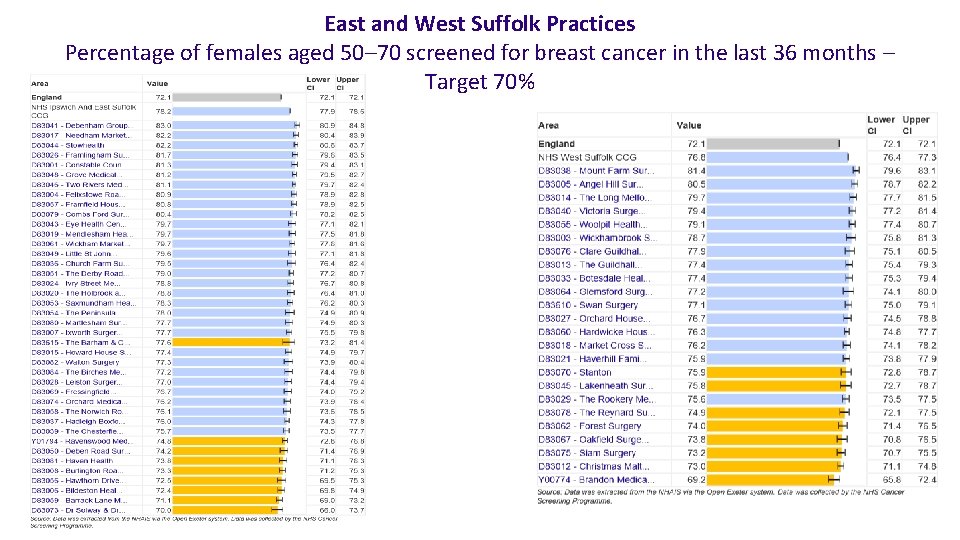
East and West Suffolk Practices Percentage of females aged 50– 70 screened for breast cancer in the last 36 months – Target 70%
SCREENING TOP T IPS • All practice staff are trained so they can discuss bowel screening with patients? • Does the practice use system alerts • Does practice regularly review defaulter lists? • Does the practice try to contact screening defaulters? • Is the practice aware of patients who may need more assistance? • Is ‘easy read’ literature available and embedded in service delivery? • Is bowel, cervical, and breast screening promoted on practice screens and noticeboards? • Does practice take part in national campaigns?
URGENT 2 WW REFERRAL TOP T IPS • Are all GPs familiar with new NICE cancer guidance (NG 12)? • Does the practice use the update regional 2 ww forms? • Do GPs use referral decision support tools? • Does practice ensure patients given information leaflet/card with 2 ww referral? • Does practice carry out any audits on cancer cases eg SEA? • Does practice keep a record of 2 ww referrals and review progress? • Does practice have a standardised safety netting protocol in place?
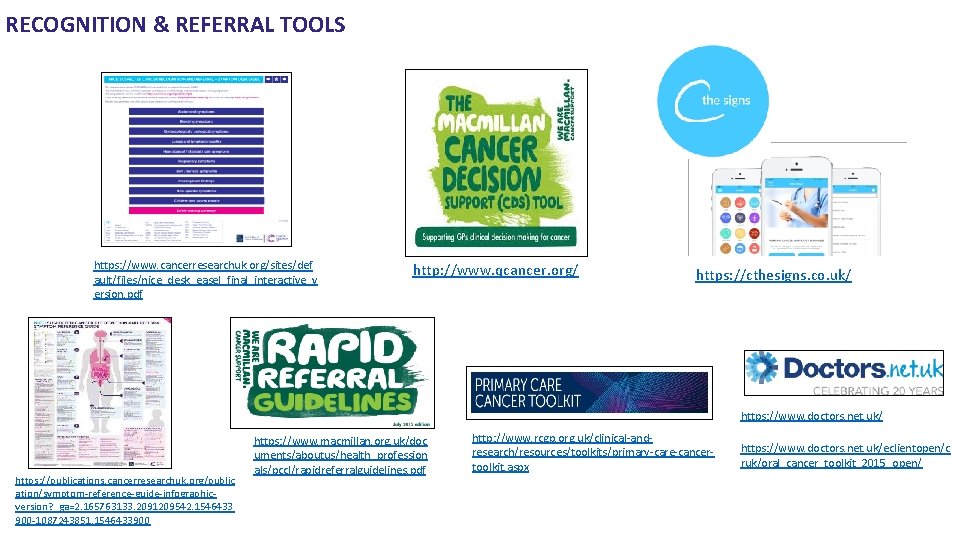
RECOGNITION & REFERRAL TOOLS https: //www. cancerresearchuk. org/sites/def ault/files/nice_desk_easel_final_interactive_v ersion. pdf http: //www. qcancer. org/ https: //cthesigns. co. uk/ https: //www. doctors. net. uk/ https: //publications. cancerresearchuk. org/public ation/symptom-reference-guide-infographicversion? _ga=2. 165763133. 2091209542. 1546433 900 -1087243851. 1546433900 https: //www. macmillan. org. uk/doc uments/aboutus/health_profession als/pccl/rapidreferralguidelines. pdf http: //www. rcgp. org. uk/clinical-andresearch/resources/toolkits/primary-care-cancertoolkit. aspx https: //www. doctors. net. uk/eclientopen/c ruk/oral_cancer_toolkit_2015_open/
BANANA SKINS LUNG COPD patients have an increased risk x 4 – 1% risk per annum Atypical presentations – often vague – haemoptysis is most specific indicator PPV at 2. 4% (NG 15 3%) Thrombocytosis – cancer risk increased - mainly lung and CR Negative CXRs – BJGP 2006 – 164 patients 3/12 before diagnosis – 90% abnormal 10% no suspicion of malignancy 1 year before 23% missed PANCREAS Easily missed - abdominal and back pain – jaundice late presentation NB new onset diabetes Around 10 % 2 ww Emergency presentation 50% Ultrasound - remember does not have a 100% sensitivity – around 75 -89% Lancet – if still worried further Ix needed OVARY Remember new presentation urinary frequency/urgency / change in bowel habit / new onset IBS >50 Do a Ca 125 – Ca Ovary 1: 500 symptoms/signs dropping to 1: 150 if Ca 125 > 35 Ca 125 most reliable tumour marker at the moment – elevates in up to 90% cases, but only 50% elevated stage 1 +
BANANA SKINS HAEMATURIA Trace haematuria on dipstick can be ignored – 1+ and above Care with stick storage 2. 5 – 20% of population have NVH – 1. 5% have pathology Visible haematuria has a PPV of around 5% for bladder/renal ca NICE 2 WW age 45 Anaemia in males PPV 1. 4% for urological cancer - do not forget urine in Ix of anaemia Symptomatic NVH / raised WBC is significant NICE 2 WW age 60 Bladder cancer in females easily missed – NB recurrent UTIs NICE 2 ww age 45 2 -3, 1+dipsticks done on different days in asymptomatic NVH is significant LYMPHOMA 6 th most common cancer - increasing incidence PPVs over 60 are; - Unexplained LN = 18. 6%; Head and neck mass = 4. 6%; mass anywhere else in body 1. 1% Non Hodgkins 70% occur > 60 years
LOCAL PREVENTION SERVICE PROVIDERS There are many local and national partner organisations that offer services and initiatives and training providers that are available for GP’s to sign post or refer patients to. Stop smoking services https: //onelifesuffolk. co. uk/our-services/quit-smoking/ Weight management https: //onelifesuffolk. co. uk/adult-weight-management-groups/ Exercise referral (West Suffolk and Felixstowe) http: //acleisure. com/health-wellbeing/exercise-on-referral (All Suffolk) https: //onelifesuffolk. co. uk/our-services/gh 2 ga/ Healthwatch https: //www. healthwatchsuffolk. co. uk/ Alcohol and drug service http: //wellbeing. turning-point. co. uk/suffolk/ One You self management https: //www. nhs. uk/oneyou/ Change for Life self management https: //www. nhs. uk/change 4 life Macmillan Cancer Support https: //www. macmillan. org. uk/about-us/health-professionals
PRIMARY CARE CANCER EDUCATION IN SUFFOLK PRIMARY CARE NURSE CANCER COURSE EVERY SIX MONTHS 5 -10 NURSES EACH TIME 30+ PRACTICES COMPLETED 3 DAYS FACE TO FACE & DISTANCE LEARNING PRIMARY CARE CANCER UPDATE EVERY SIX MONTHS FREE 1 DAY UPDATE FOR ALL PRACTICE CLINICAL STAFF NEXT ONE 6 TH JUNE 2019 Topics included November 2018 – breast cancer, FIT testing, Immunotherapy
CANCER EDUCATION CRUK Talking About Cancer: Reducing Risk, Early Detection and Myth busting- FREE online training https: //www. futurelearn. com/courses/talking-about-cancer (Can also organize a training session for health professionals) Macmillan E-learning courses- FREE https: //learnzone. org. uk/courses/index. php? a=4 RCGP Behaviour change E-Learning course- FREE This module is aimed at healthcare professionals who would like to promote behaviour change in their patients to reduce their cancer risk. http: //elearning. rcgp. org. uk/course/info. php? id=211 Other CRUK CPD training- FREE https: //www. cancerresearchuk. org/health-professional/learning-and-ways-we-can-supportyou/continual-professional-development-cpd CRUK Facilitator and Macmillan GP led training- FREE Delivery of training for primary care professionals on a variety of topics such as prevention, early diagnosis, screening and safetynetting Donna Reeve (CRUK Facilitator Dr Andrew Yager Macmillan GP donna. reeve@cancer. org. uk a. yager@nhs. net 07979 926403 07917454535
National Cancer Diagnosis Audit https: //www. cancerresearchuk. org/healthprofessional/diagnosis/national-cancerdiagnosis-audit
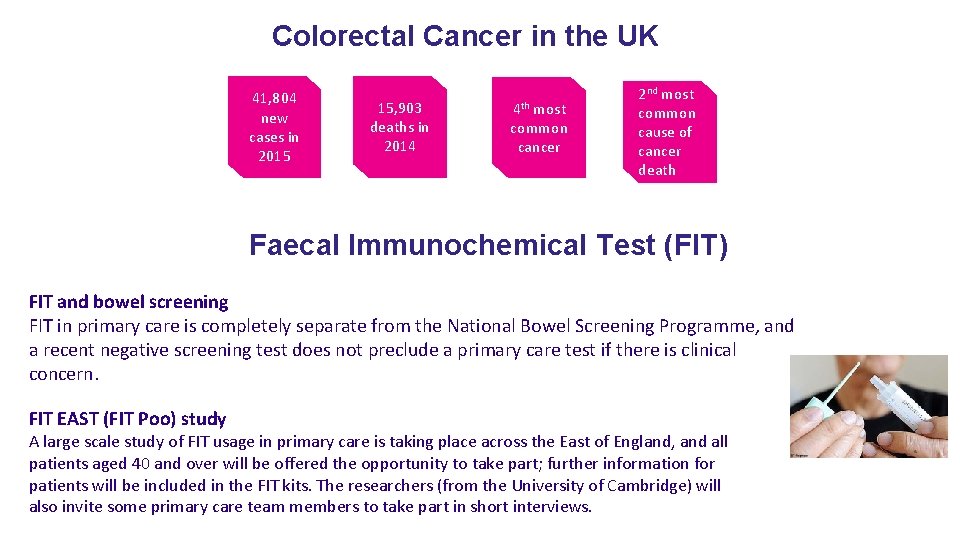
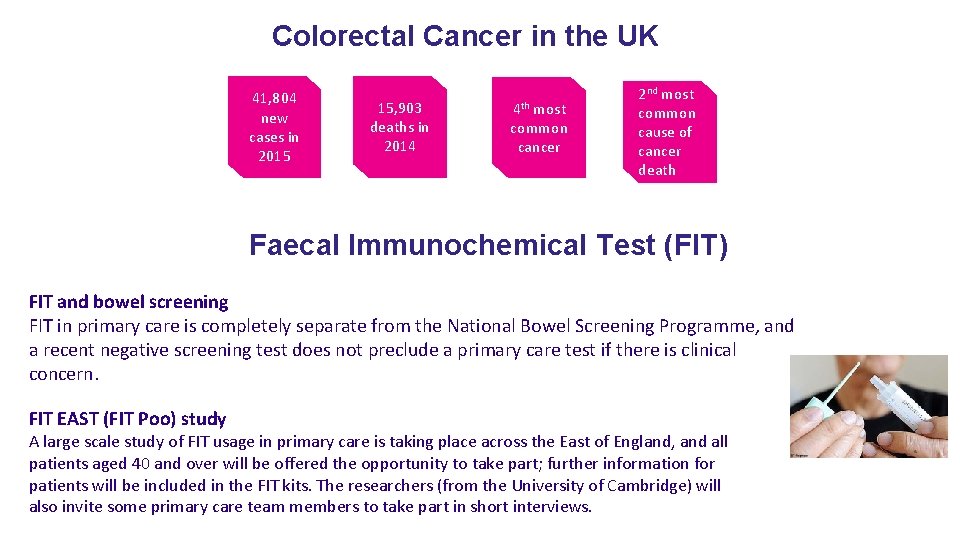
Colorectal Cancer in the UK 41, 804 new cases in 2015 15, 903 deaths in 2014 4 th most common cancer 2 nd most common cause of cancer death Faecal Immunochemical Test (FIT) FIT and bowel screening FIT in primary care is completely separate from the National Bowel Screening Programme, and a recent negative screening test does not preclude a primary care test if there is clinical concern. FIT EAST (FIT Poo) study A large scale study of FIT usage in primary care is taking place across the East of England, and all patients aged 40 and over will be offered the opportunity to take part; further information for patients will be included in the FIT kits. The researchers (from the University of Cambridge) will also invite some primary care team members to take part in short interviews.
FIT testing in primary care What is FIT? FIT stands for Faecal Immunochemical Test and is an antibody test for the presence of human globin in faeces. It is a highly sensitive, quantitative test performed on a single sample, unaffected by diet. A positive test (>10 ug/g) indicates lower GI bleeding and the need for further referral. Who should be offered the test? NICE has produced guidance (DG 30) on which patients should be offered FIT: https: //www. nice. org. uk/guidance/dg 30. Primary care clinicians are, however, encouraged to offer FIT testing to those patients whose symptoms may represent colorectal cancer but do not meet existing 2 WW criteria. The suggested management pathway is overleaf, which also summarises NICE guidance. How is the test arranged? Practices will be supplied with FIT kits by their local laboratories and the test is ordered and reported on ICE just like any other primary care test. A recent FBC is also needed. FIT and fast-track referral pathways NG 12 guidance and current 2 WW colorectal pathways are unaffected and these patients do not need a FIT test. The small print A negative FIT test effectively rules out current colorectal cancer but clinical judgement is still needed for safety netting and follow-up.

This is to certify that has Participated in a Cancer Update Insert name. Health Professional Engagement Facilitator Insert STP Cancer Research UK Tel : Insert Email on Insert date