ATORVA 20 mgd LDL CHOL 90 mgdl ROSUVA



























- Slides: 48






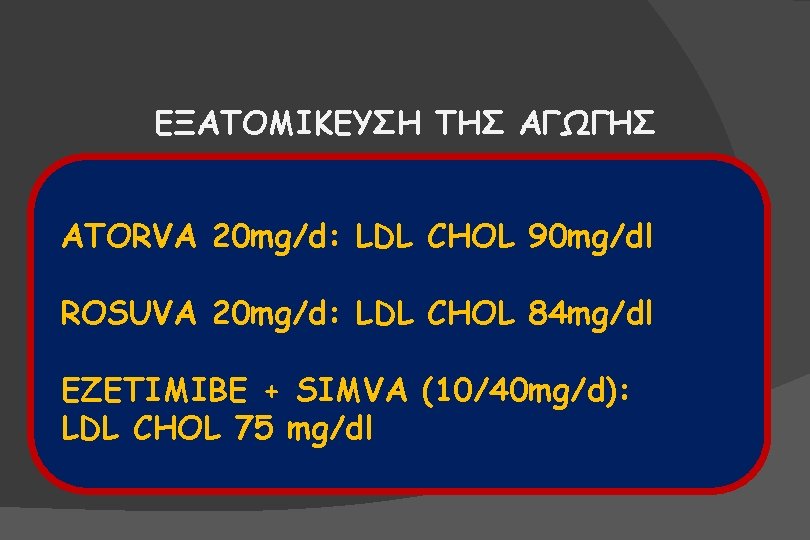
ΕΞΑΤΟΜΙΚΕΥΣΗ ΤΗΣ ΑΓΩΓΗΣ ATORVA 20 mg/d: LDL CHOL 90 mg/dl ROSUVA 20 mg/d: LDL CHOL 84 mg/dl EZETIMIBE + SIMVA (10/40 mg/d): LDL CHOL 75 mg/dl


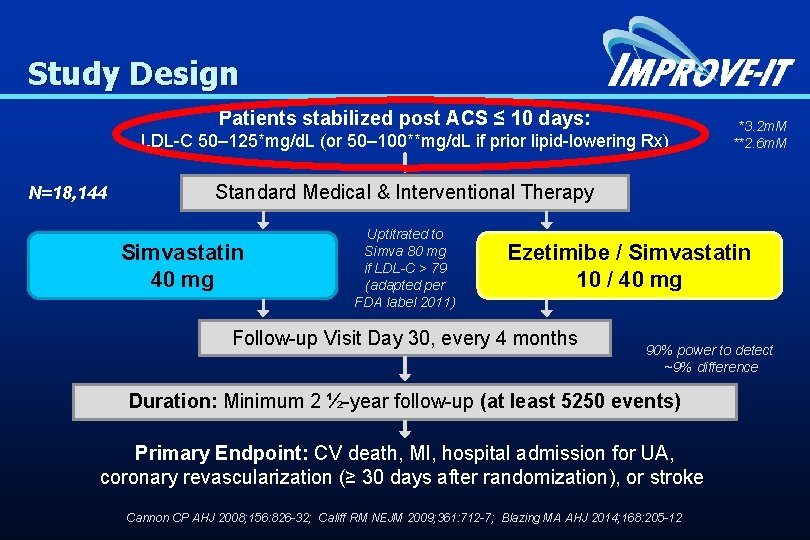
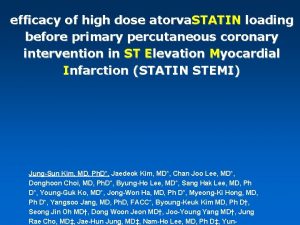
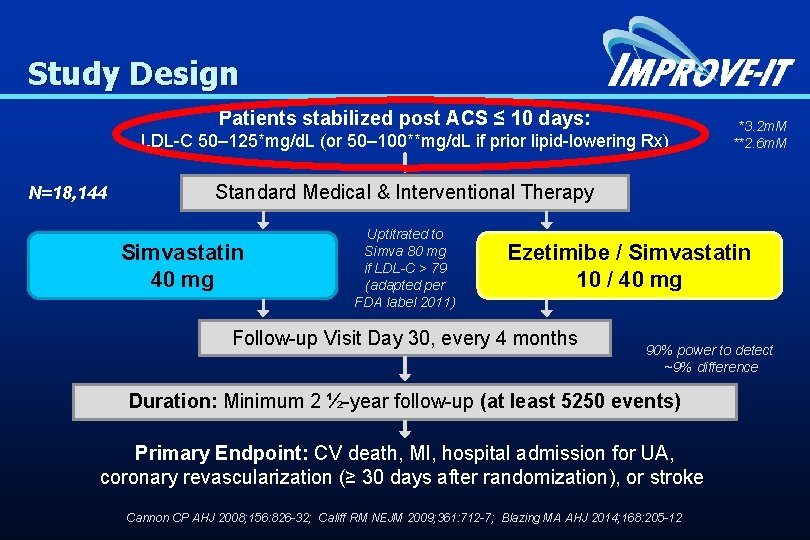
Study Design Patients stabilized post ACS ≤ 10 days: LDL-C 50– 125*mg/d. L (or 50– 100**mg/d. L if prior lipid-lowering Rx) N=18, 144 *3. 2 m. M **2. 6 m. M Standard Medical & Interventional Therapy Simvastatin 40 mg Uptitrated to Simva 80 mg if LDL-C > 79 (adapted per FDA label 2011) Ezetimibe / Simvastatin 10 / 40 mg Follow-up Visit Day 30, every 4 months 90% power to detect ~9% difference Duration: Minimum 2 ½-year follow-up (at least 5250 events) Primary Endpoint: CV death, MI, hospital admission for UA, coronary revascularization (≥ 30 days after randomization), or stroke Cannon CP AHJ 2008; 156: 826 -32; Califf RM NEJM 2009; 361: 712 -7; Blazing MA AHJ 2014; 168: 205 -12
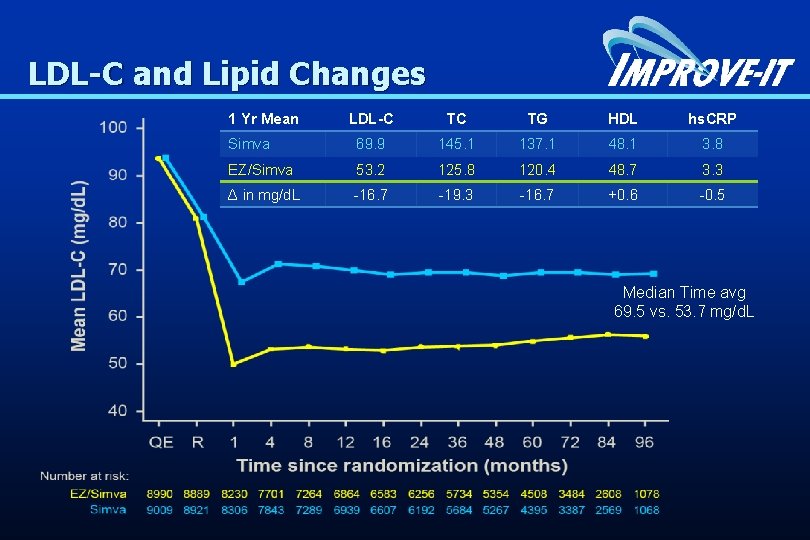
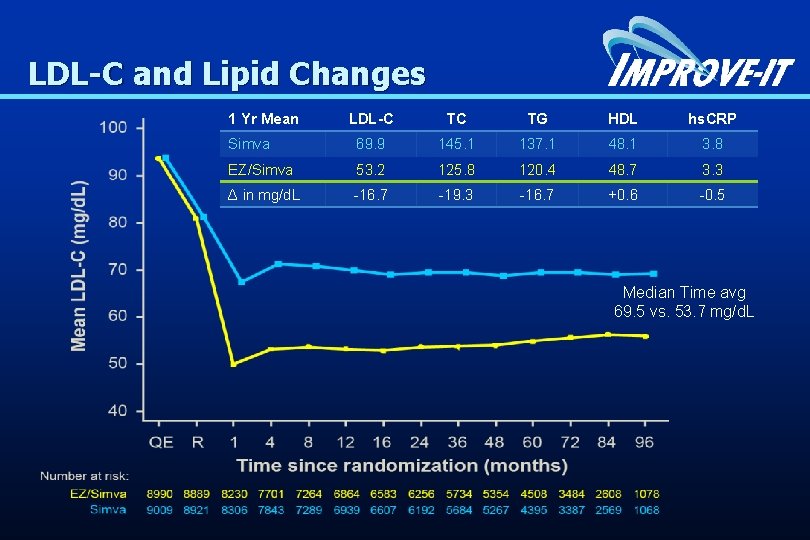
LDL-C and Lipid Changes 1 Yr Mean LDL-C TC TG HDL hs. CRP Simva 69. 9 145. 1 137. 1 48. 1 3. 8 EZ/Simva 53. 2 125. 8 120. 4 48. 7 3. 3 Δ in mg/d. L -16. 7 -19. 3 -16. 7 +0. 6 -0. 5 Median Time avg 69. 5 vs. 53. 7 mg/d. L
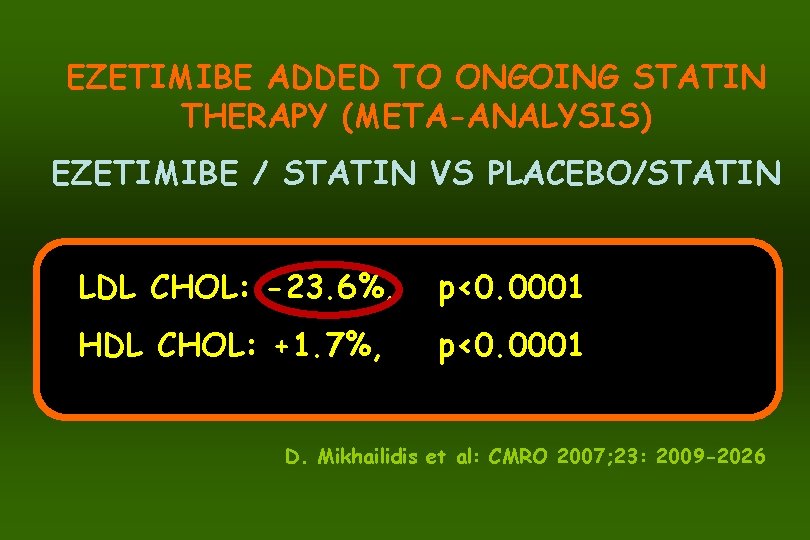
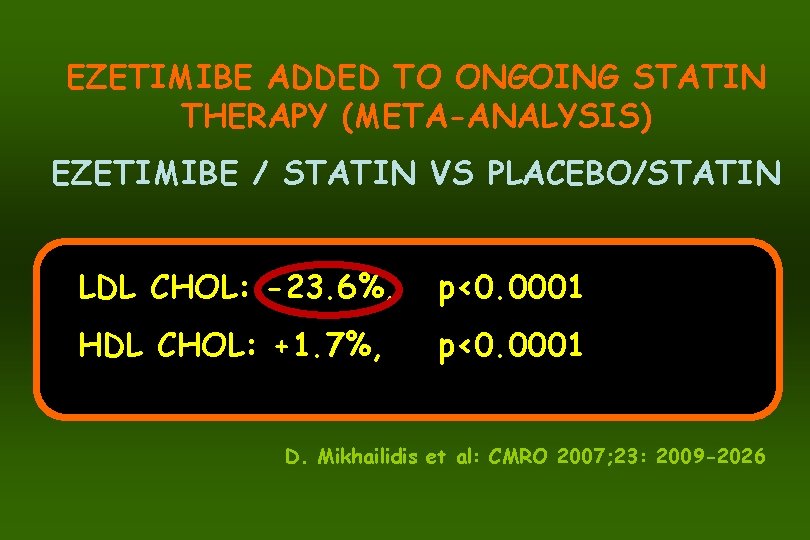
EZETIMIBE ADDED TO ONGOING STATIN THERAPY (META-ANALYSIS) EZETIMIBE / STATIN VS PLACEBO/STATIN LDL CHOL: -23. 6%, p<0. 0001 HDL CHOL: +1. 7%, p<0. 0001 D. Mikhailidis et al: CMRO 2007; 23: 2009 -2026
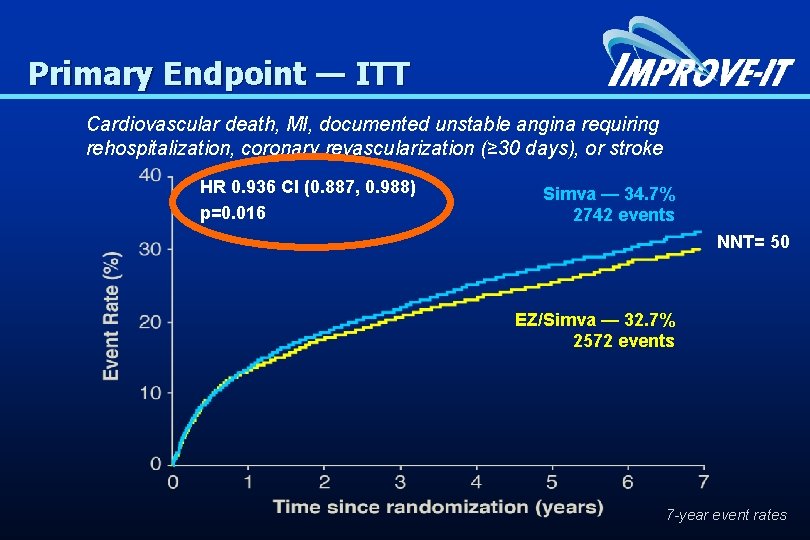
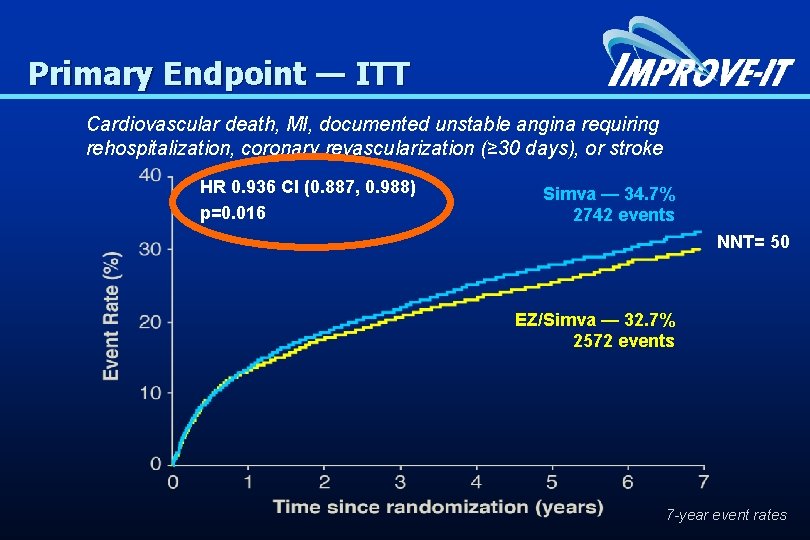
Primary Endpoint — ITT Cardiovascular death, MI, documented unstable angina requiring rehospitalization, coronary revascularization (≥ 30 days), or stroke HR 0. 936 CI (0. 887, 0. 988) p=0. 016 Simva — 34. 7% 2742 events NNT= 50 EZ/Simva — 32. 7% 2572 events 7 -year event rates
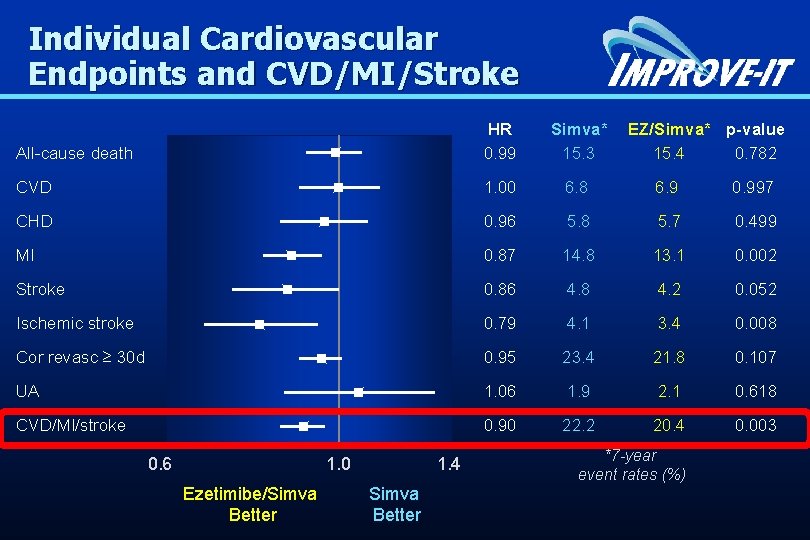
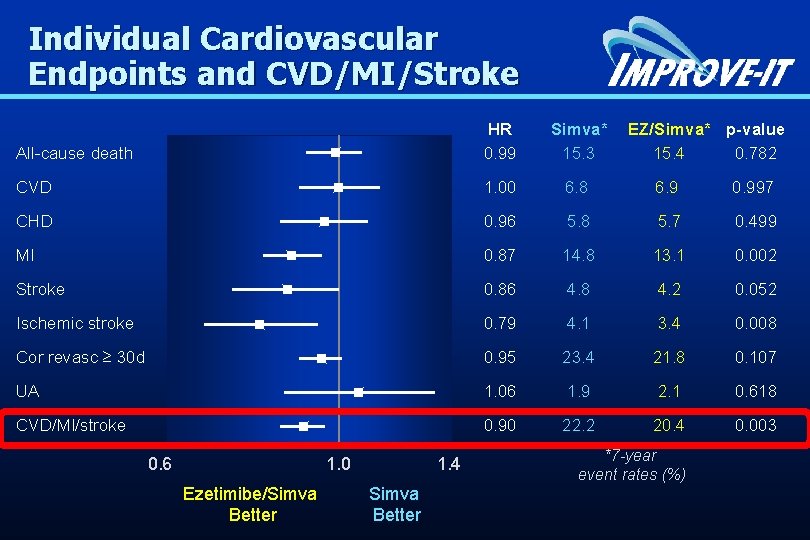
Individual Cardiovascular Endpoints and CVD/MI/Stroke HR 0. 99 Simva* 15. 3 1. 00 6. 8 6. 9 0. 997 0. 96 0. 87 5. 8 14. 8 5. 7 13. 1 0. 499 0. 002 Stroke 0. 86 4. 8 4. 2 0. 052 Ischemic stroke 0. 79 4. 1 3. 4 0. 008 Cor revasc ≥ 30 d 0. 95 23. 4 21. 8 0. 107 UA 1. 06 1. 9 2. 1 0. 618 CVD/MI/stroke 0. 90 22. 2 20. 4 0. 003 All-cause death CVD CHD MI 0. 6 1. 0 Ezetimibe/Simva Better 1. 4 Simva Better EZ/Simva* p-value 15. 4 0. 782 *7 -year event rates (%)
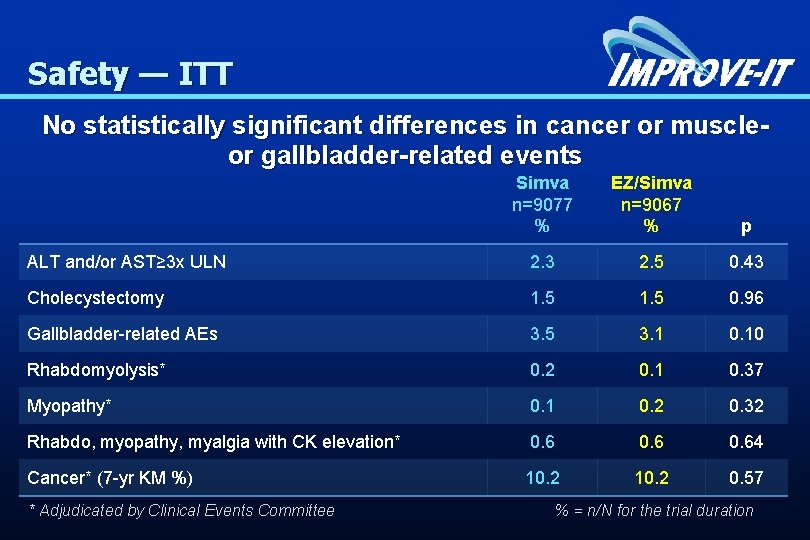
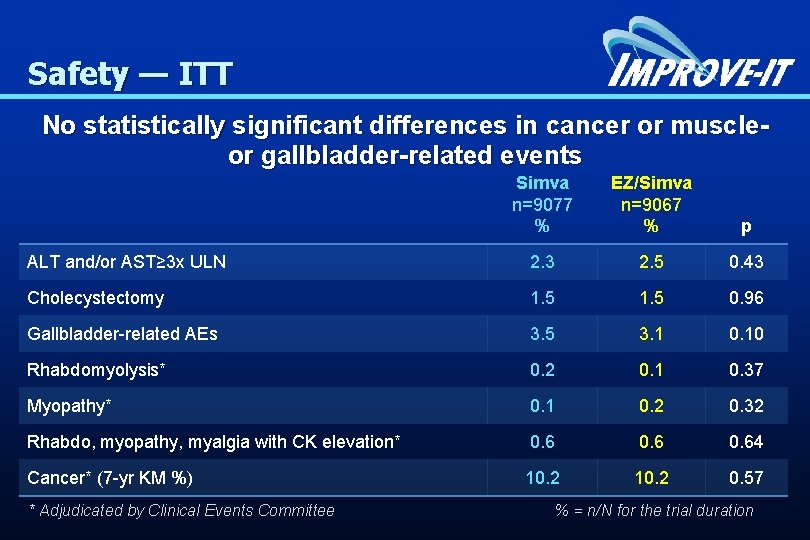
Safety — ITT No statistically significant differences in cancer or muscle- or gallbladder-related events Simva n=9077 % EZ/Simva n=9067 % p ALT and/or AST≥ 3 x ULN 2. 3 2. 5 0. 43 Cholecystectomy 1. 5 0. 96 Gallbladder-related AEs 3. 5 3. 1 0. 10 Rhabdomyolysis* 0. 2 0. 1 0. 37 Myopathy* 0. 1 0. 2 0. 32 Rhabdo, myopathy, myalgia with CK elevation* 0. 64 Cancer* (7 -yr KM %) 10. 2 0. 57 * Adjudicated by Clinical Events Committee % = n/N for the trial duration






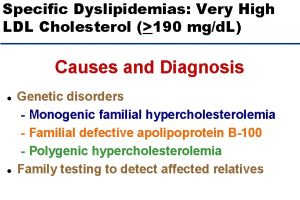
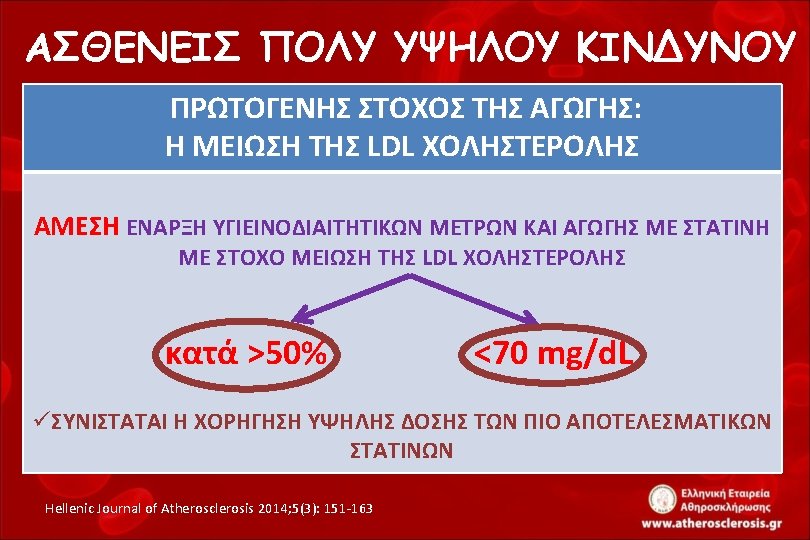
v. ACHIEVEMENT OF THE LDL CHOL GOALS: DOUBLING THE DOSE OR COMBINATION THERAPY?





IMPROVE-IT RESULTS LOWER IS BETTER


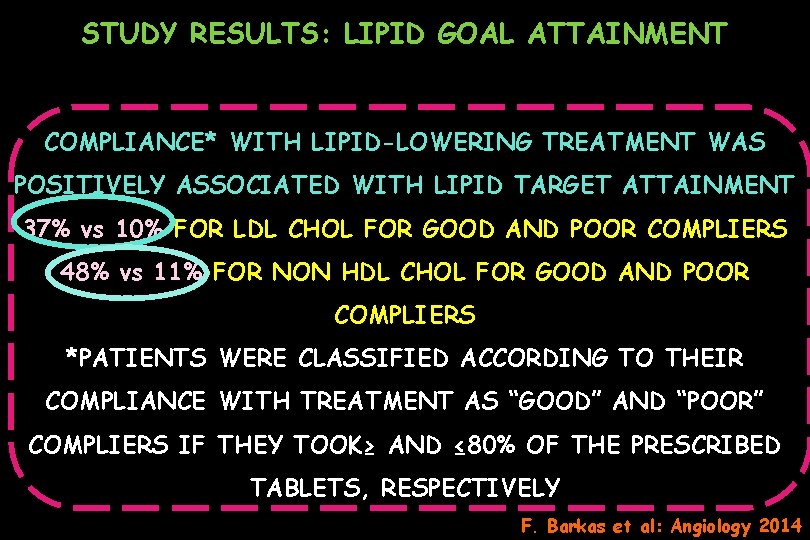
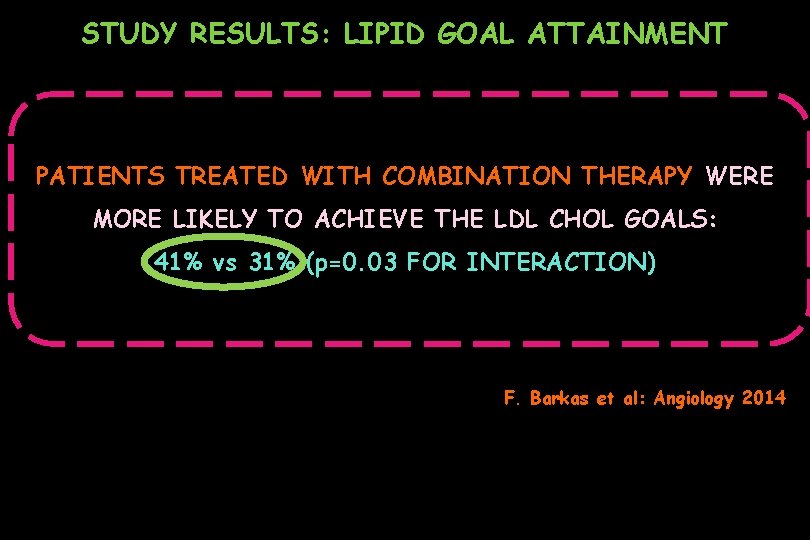
STUDY RESULTS: LIPID GOAL ATTAINMENT COMPLIANCE* WITH LIPID-LOWERING TREATMENT WAS POSITIVELY ASSOCIATED WITH LIPID TARGET ATTAINMENT 37% vs 10% FOR LDL CHOL FOR GOOD AND POOR COMPLIERS 48% vs 11% FOR NON HDL CHOL FOR GOOD AND POOR COMPLIERS *PATIENTS WERE CLASSIFIED ACCORDING TO THEIR COMPLIANCE WITH TREATMENT AS “GOOD” AND “POOR” COMPLIERS IF THEY TOOK≥ AND ≤ 80% OF THE PRESCRIBED TABLETS, RESPECTIVELY F. Barkas et al: Angiology 2014
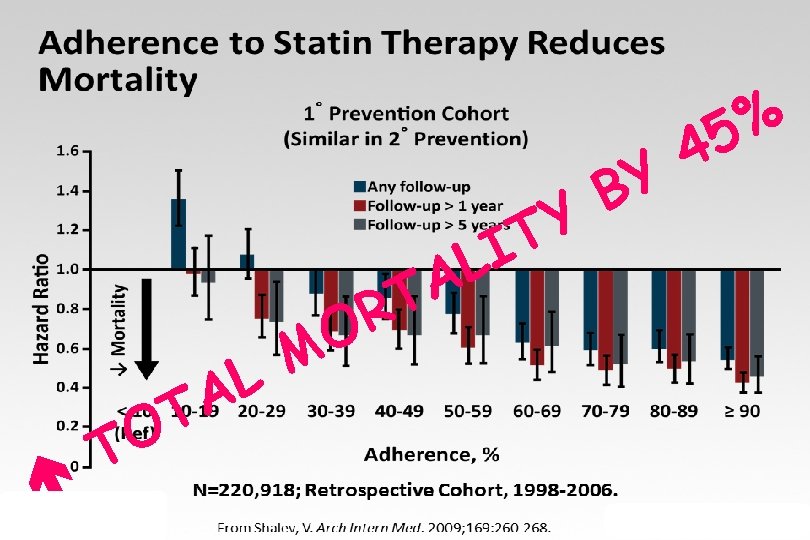
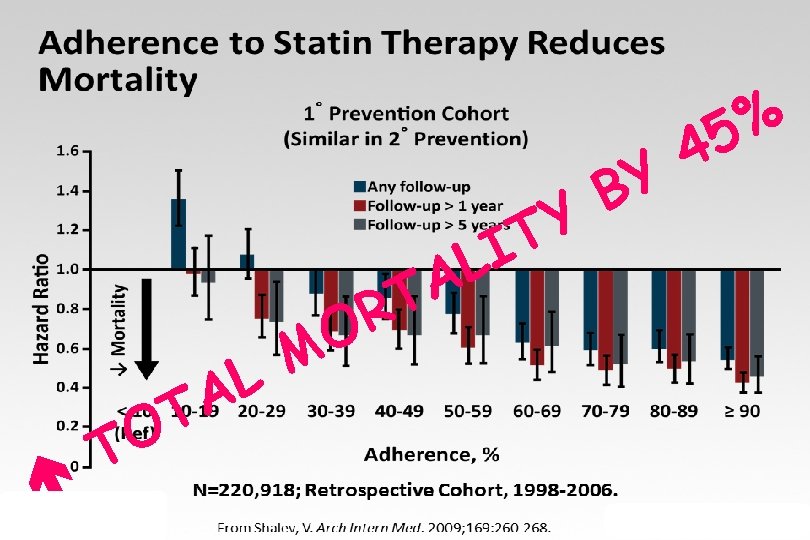
4 Y B Y T I L A T R O M L A T O T % 5
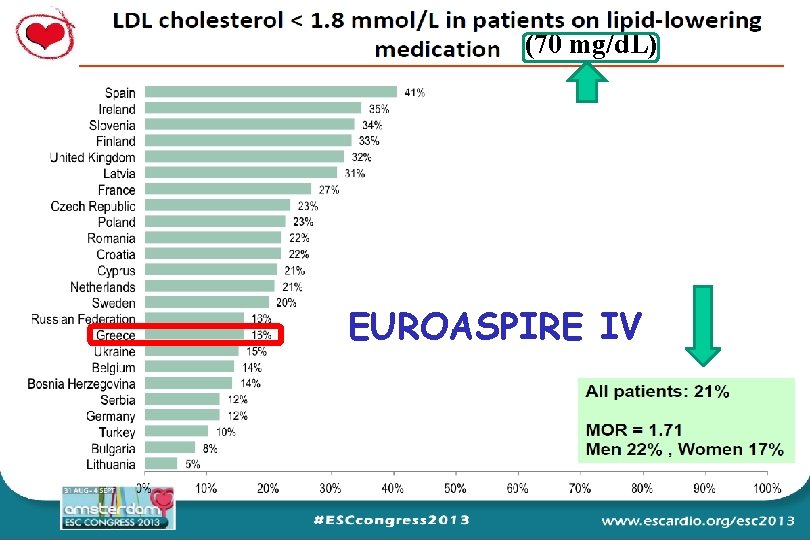
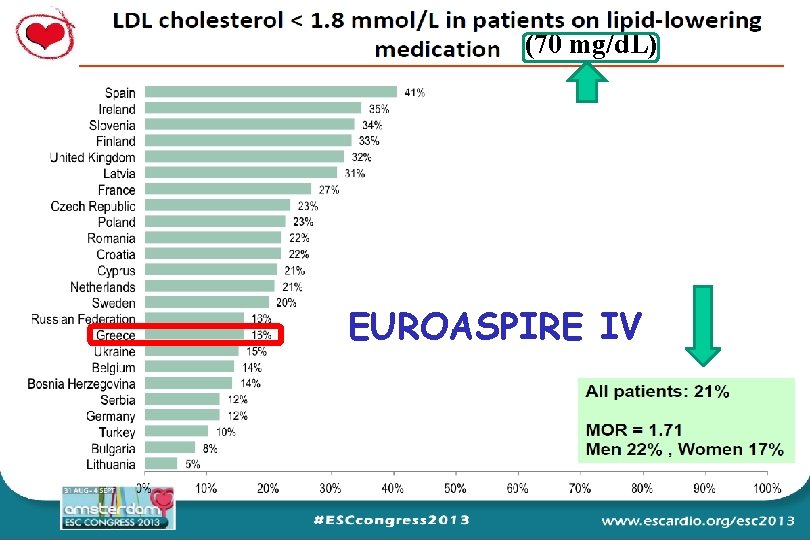
(70 mg/d. L) EUROASPIRE IV
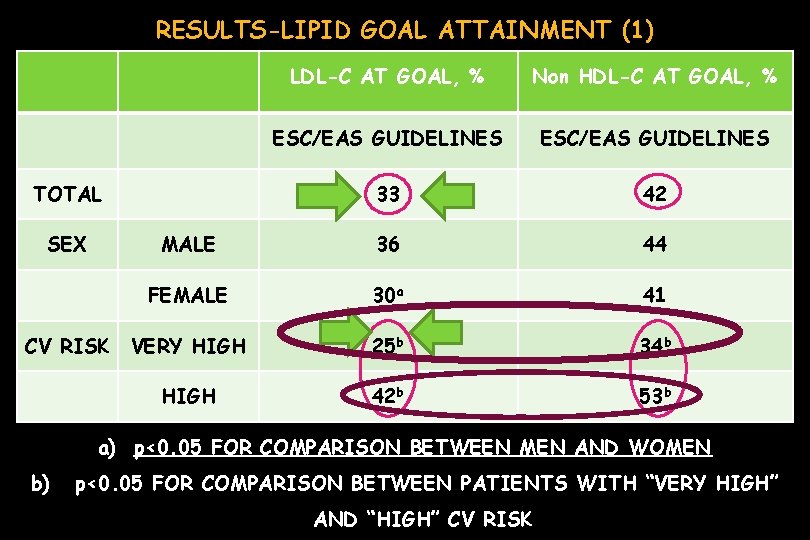
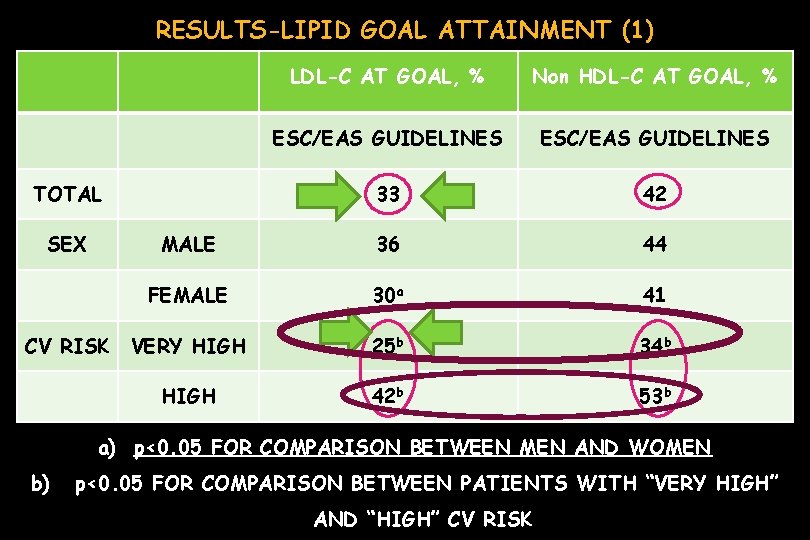
RESULTS-LIPID GOAL ATTAINMENT (1) LDL-C AT GOAL, % Non HDL-C AT GOAL, % ESC/EAS GUIDELINES 33 42 MALE 36 44 FEMALE 30 a 41 VERY HIGH 25 b 34 b HIGH 42 b 53 b TOTAL SEX CV RISK a) p<0. 05 FOR COMPARISON BETWEEN MEN AND WOMEN b) p<0. 05 FOR COMPARISON BETWEEN PATIENTS WITH “VERY HIGH” AND “HIGH” CV RISK
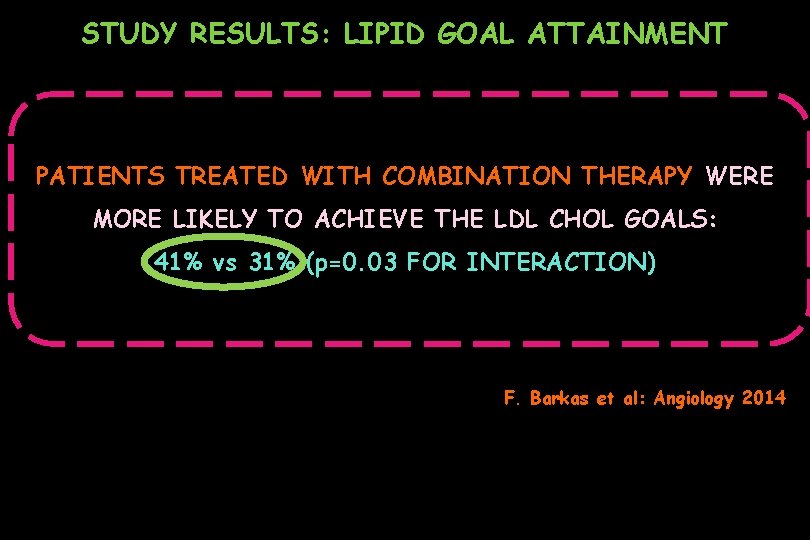
STUDY RESULTS: LIPID GOAL ATTAINMENT PATIENTS TREATED WITH COMBINATION THERAPY WERE MORE LIKELY TO ACHIEVE THE LDL CHOL GOALS: 41% vs 31% (p=0. 03 FOR INTERACTION) F. Barkas et al: Angiology 2014

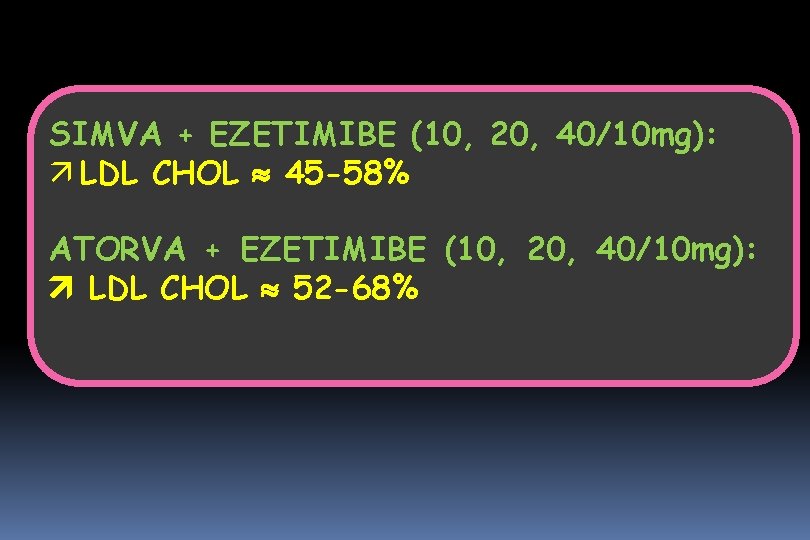
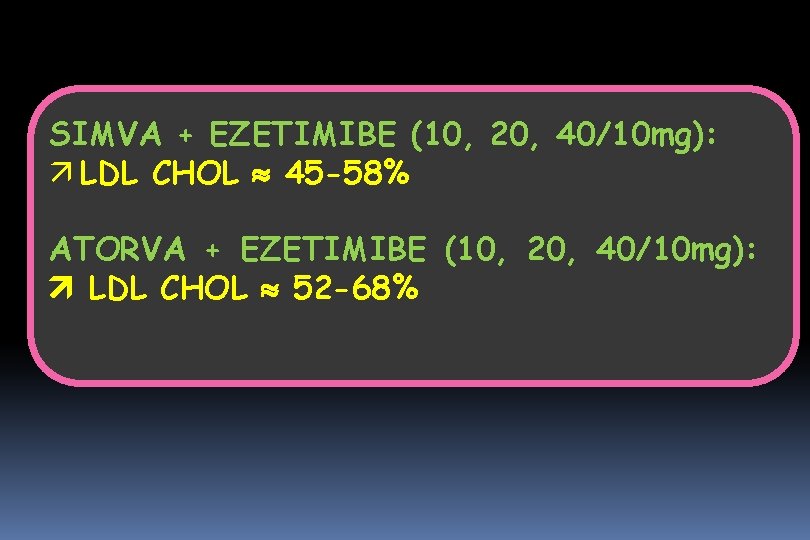
SIMVA + EZETIMIBE (10, 20, 40/10 mg): ä LDL CHOL 45 -58% ATORVA + EZETIMIBE (10, 20, 40/10 mg): LDL CHOL 52 -68%



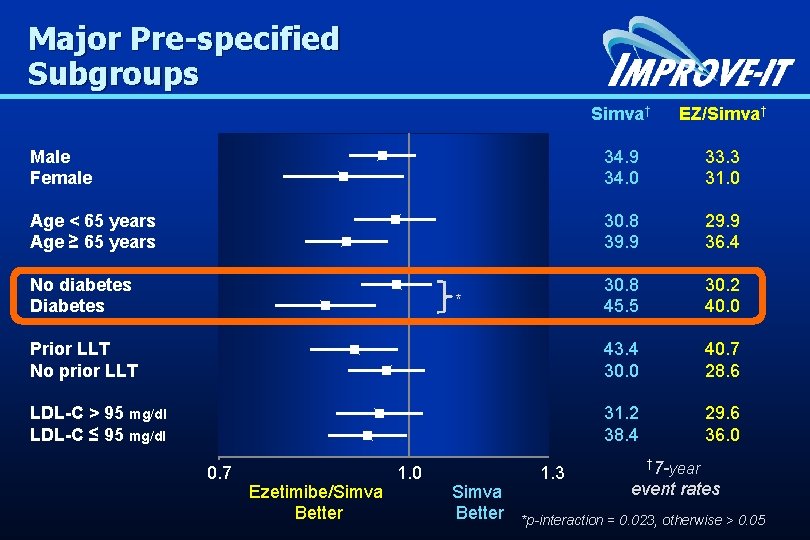
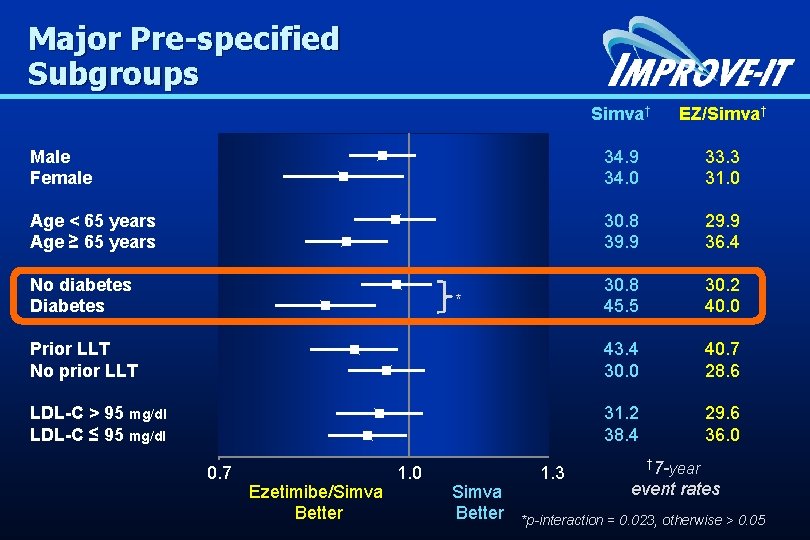
Major Pre-specified Subgroups Simva† 34. 9 34. 0 30. 8 39. 9 30. 8 45. 5 43. 4 30. 0 31. 2 38. 4 Male Female Age < 65 years Age ≥ 65 years No diabetes Diabetes * Prior LLT No prior LLT LDL-C > 95 mg/dl LDL-C ≤ 95 mg/dl 0. 7 Ezetimibe/Simva Better 1. 0 Simva Better 1. 3 EZ/Simva† 33. 3 31. 0 29. 9 36. 4 30. 2 40. 0 40. 7 28. 6 29. 6 36. 0 † 7 -year event rates *p-interaction = 0. 023, otherwise > 0. 05

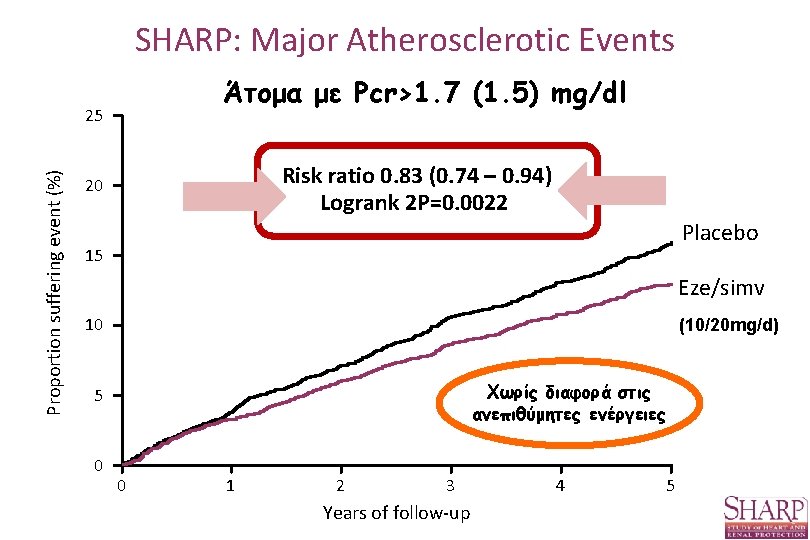
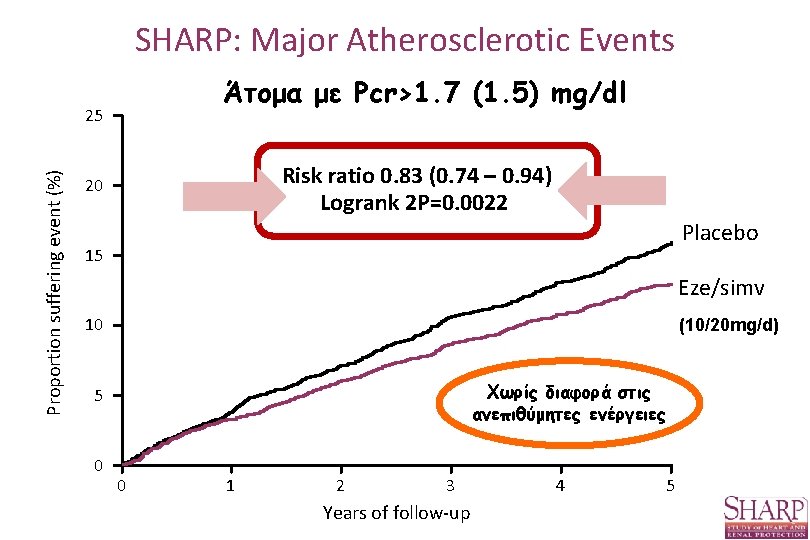
SHARP: Major Atherosclerotic Events Άτομα με Pcr>1. 7 (1. 5) mg/dl Proportion suffering event (%) 25 Risk ratio 0. 83 (0. 74 – 0. 94) Logrank 2 P=0. 0022 20 Placebo 15 Eze/simv 10 (10/20 mg/d) Χωρίς διαφορά στις ανεπιθύμητες ενέργειες 5 0 0 1 2 3 Years of follow-up 4 5

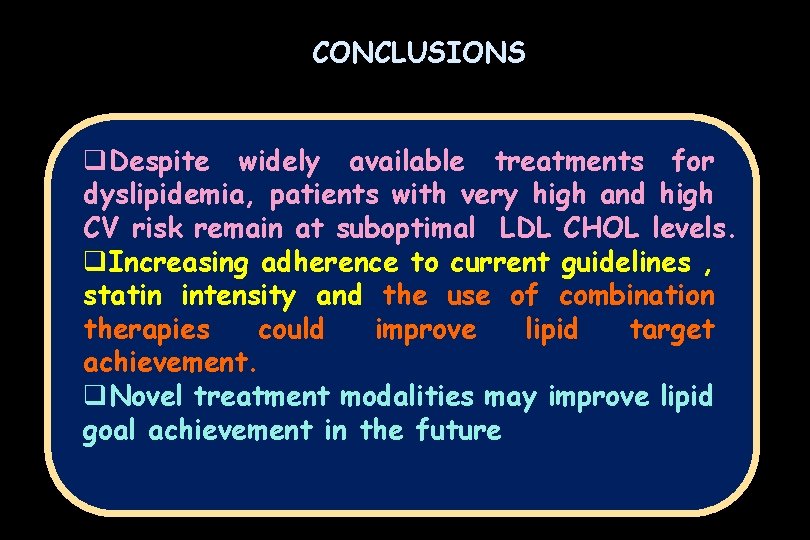
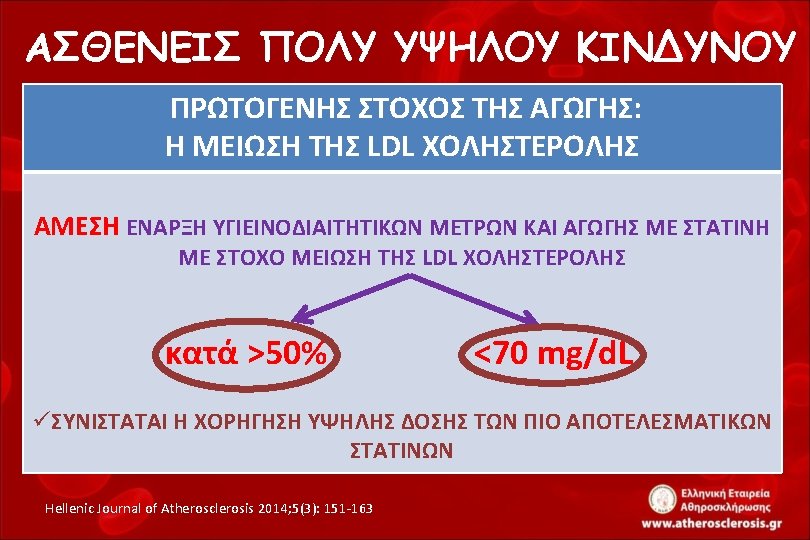
CONCLUSIONS q. Despite widely available treatments for dyslipidemia, patients with very high and high CV risk remain at suboptimal LDL CHOL levels. q. Increasing adherence to current guidelines , statin intensity and the use of combination therapies could improve lipid target achievement. q. Novel treatment modalities may improve lipid goal achievement in the future