Goals Guidelines A summary of international guidelines for
- Slides: 16
Goals & Guidelines A summary of international guidelines for CHD
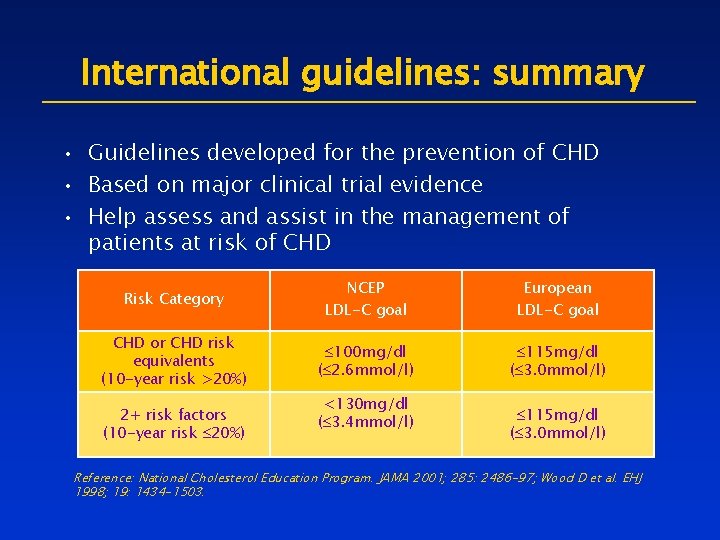
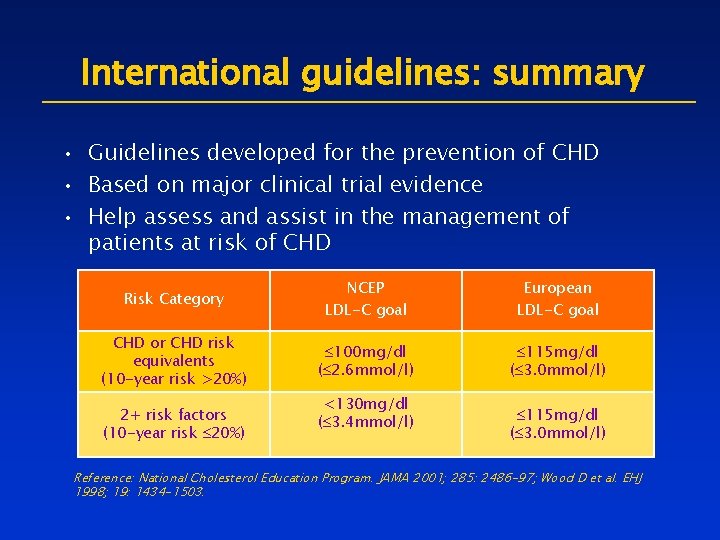
International guidelines: summary • Guidelines developed for the prevention of CHD • Based on major clinical trial evidence • Help assess and assist in the management of patients at risk of CHD Risk Category NCEP LDL-C goal European LDL-C goal CHD or CHD risk equivalents (10 -year risk >20%) 100 mg/dl ( 2. 6 mmol/l) 115 mg/dl ( 3. 0 mmol/l) 2+ risk factors (10 -year risk 20%) <130 mg/dl ( 3. 4 mmol/l) 115 mg/dl ( 3. 0 mmol/l) Reference: National Cholesterol Education Program. JAMA 2001; 285: 2486 -97; Wood D et al. EHJ 1998; 19: 1434 -1503.
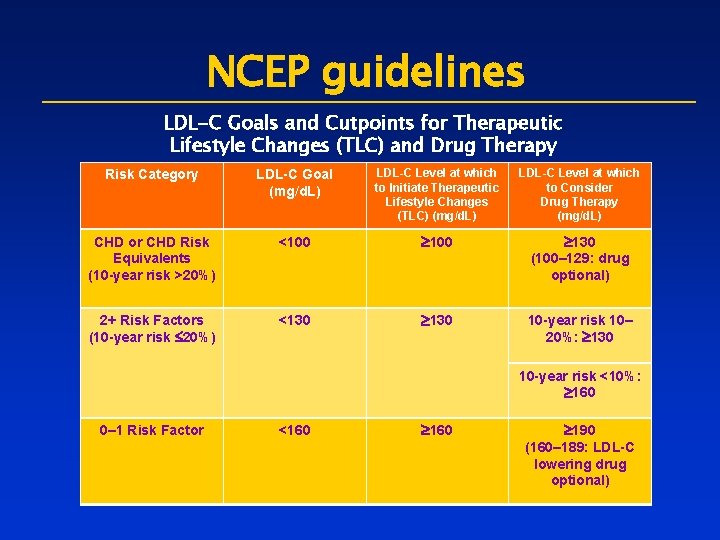
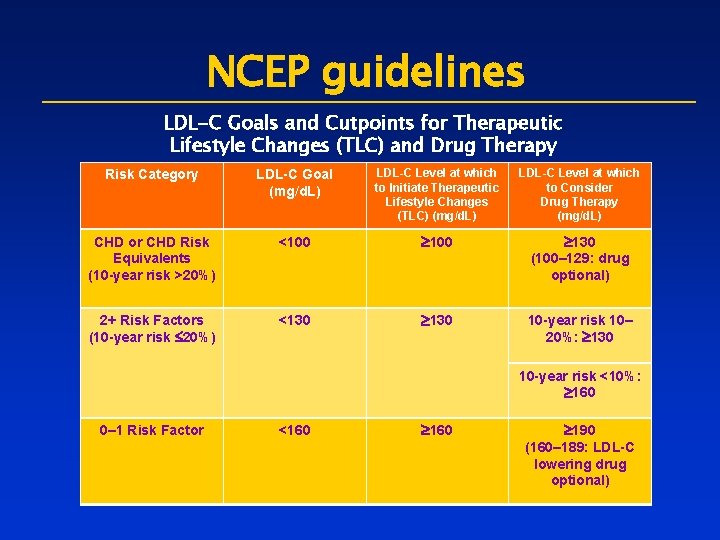
NCEP guidelines LDL-C Goals and Cutpoints for Therapeutic Lifestyle Changes (TLC) and Drug Therapy Risk Category LDL-C Goal (mg/d. L) LDL-C Level at which to Initiate Therapeutic Lifestyle Changes (TLC) (mg/d. L) LDL-C Level at which to Consider Drug Therapy (mg/d. L) CHD or CHD Risk Equivalents (10 -year risk >20%) <100 ³ 130 (100– 129: drug optional) 2+ Risk Factors (10 -year risk £ 20%) <130 ³ 130 10 -year risk 10– 20%: ³ 130 10 -year risk <10%: ³ 160 0– 1 Risk Factor <160 ³ 190 (160– 189: LDL-C lowering drug optional)
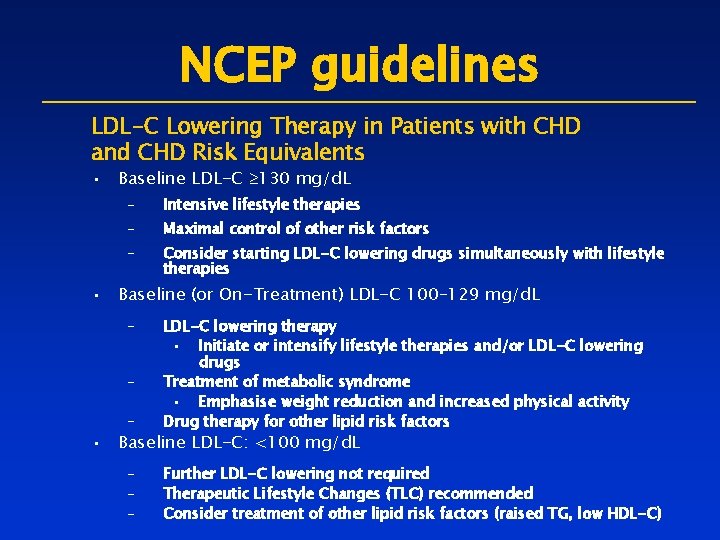
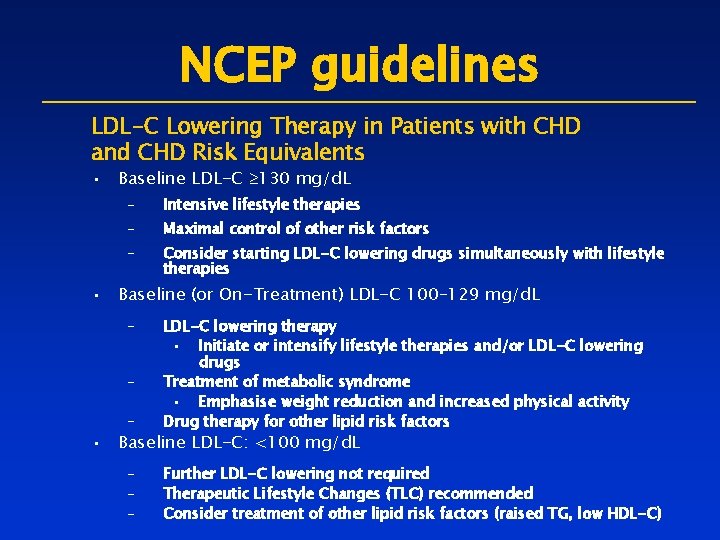
NCEP guidelines LDL-C Lowering Therapy in Patients with CHD and CHD Risk Equivalents • Baseline LDL-C ³ 130 mg/d. L – Intensive lifestyle therapies – Maximal control of other risk factors – Consider starting LDL-C lowering drugs simultaneously with lifestyle therapies • Baseline (or On-Treatment) LDL-C 100– 129 mg/d. L – – LDL-C lowering therapy • Initiate or intensify lifestyle therapies and/or LDL-C lowering drugs Treatment of metabolic syndrome • Emphasise weight reduction and increased physical activity Drug therapy for other lipid risk factors – – – Further LDL-C lowering not required Therapeutic Lifestyle Changes (TLC) recommended Consider treatment of other lipid risk factors (raised TG, low HDL-C) – • Baseline LDL-C: <100 mg/d. L
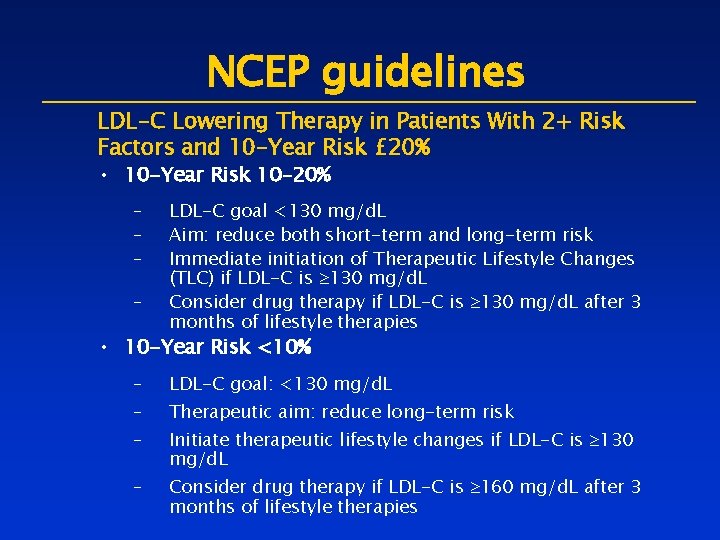
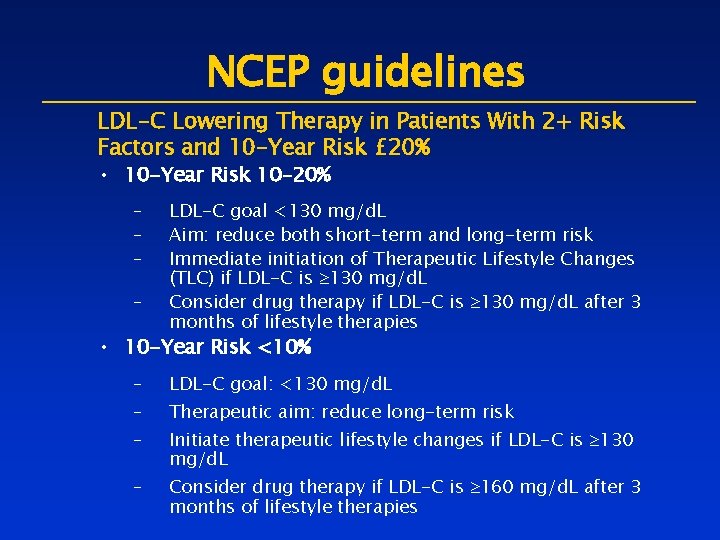
NCEP guidelines LDL-C Lowering Therapy in Patients With 2+ Risk Factors and 10 -Year Risk £ 20% • 10 -Year Risk 10– 20% – – LDL-C goal <130 mg/d. L Aim: reduce both short-term and long-term risk Immediate initiation of Therapeutic Lifestyle Changes (TLC) if LDL-C is ³ 130 mg/d. L Consider drug therapy if LDL-C is ³ 130 mg/d. L after 3 months of lifestyle therapies • 10 -Year Risk <10% – – LDL-C goal: <130 mg/d. L Therapeutic aim: reduce long-term risk Initiate therapeutic lifestyle changes if LDL-C is ³ 130 mg/d. L Consider drug therapy if LDL-C is ³ 160 mg/d. L after 3 months of lifestyle therapies
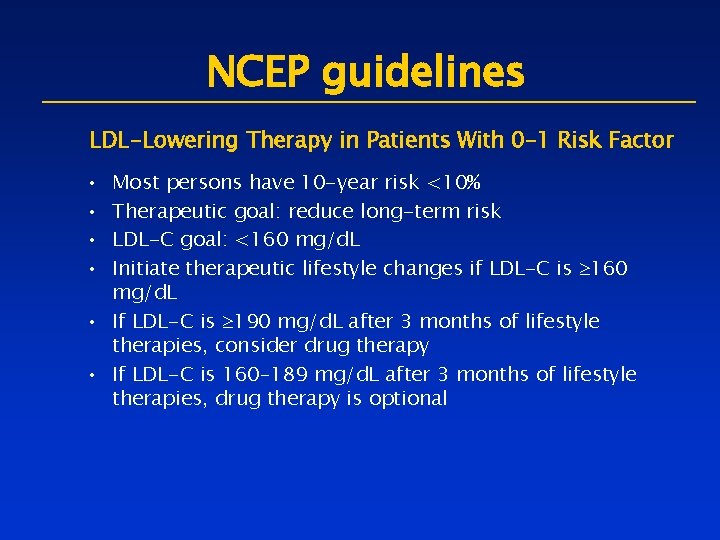
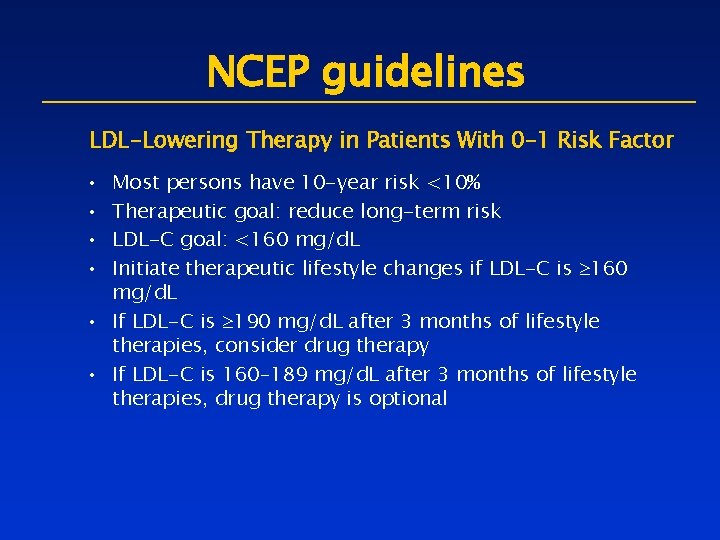
NCEP guidelines LDL-Lowering Therapy in Patients With 0– 1 Risk Factor • • Most persons have 10 -year risk <10% Therapeutic goal: reduce long-term risk LDL-C goal: <160 mg/d. L Initiate therapeutic lifestyle changes if LDL-C is ³ 160 mg/d. L • If LDL-C is ³ 190 mg/d. L after 3 months of lifestyle therapies, consider drug therapy • If LDL-C is 160– 189 mg/d. L after 3 months of lifestyle therapies, drug therapy is optional
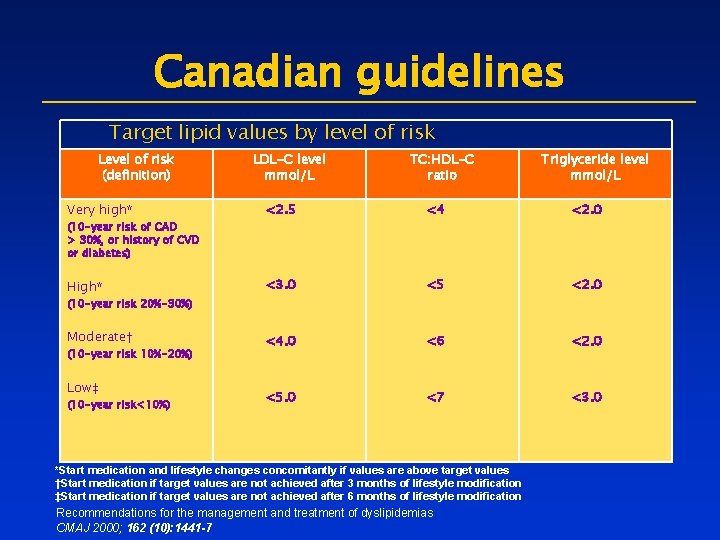
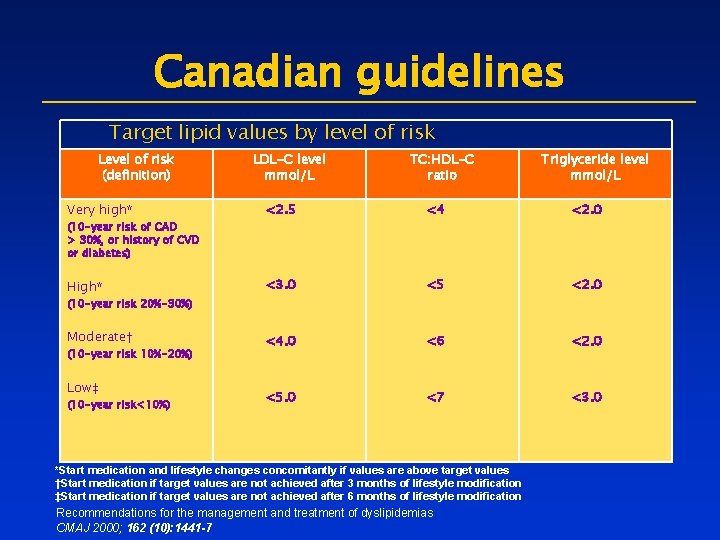
Canadian guidelines Target lipid values by level of risk Level of risk (definition) LDL-C level mmol/L TC: HDL-C ratio Triglyceride level mmol/L Very high* <2. 5 <4 <2. 0 High* <3. 0 <5 <2. 0 Moderate† <4. 0 <6 <2. 0 <5. 0 <7 <3. 0 (10 -year risk of CAD > 30%, or history of CVD or diabetes) (10 -year risk 20%-30%) (10 -year risk 10%-20%) Low‡ (10 -year risk<10%) *Start medication and lifestyle changes concomitantly if values are above target values †Start medication if target values are not achieved after 3 months of lifestyle modification ‡Start medication if target values are not achieved after 6 months of lifestyle modification Recommendations for the management and treatment of dyslipidemias CMAJ 2000; 162 (10): 1441 -7
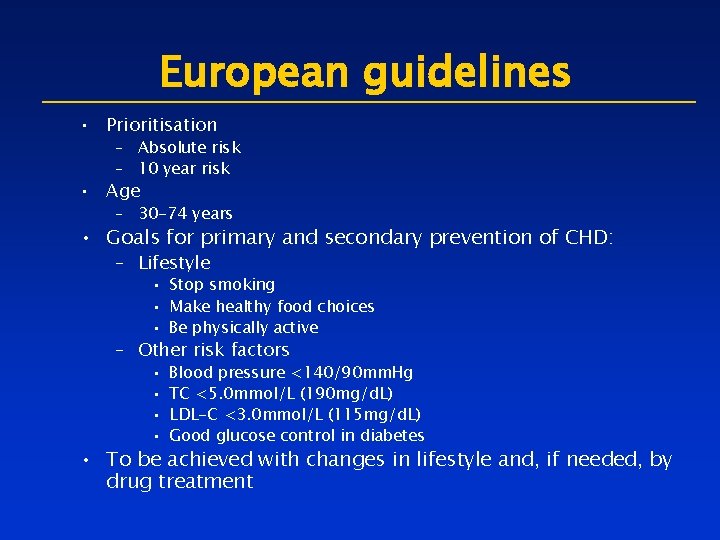
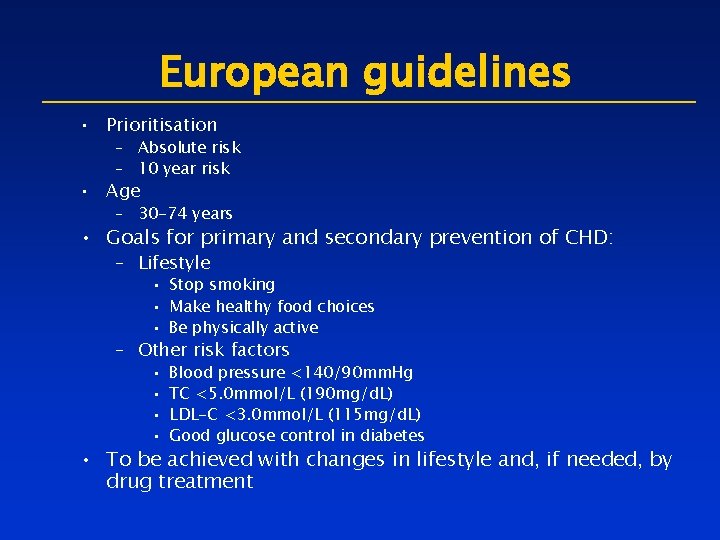
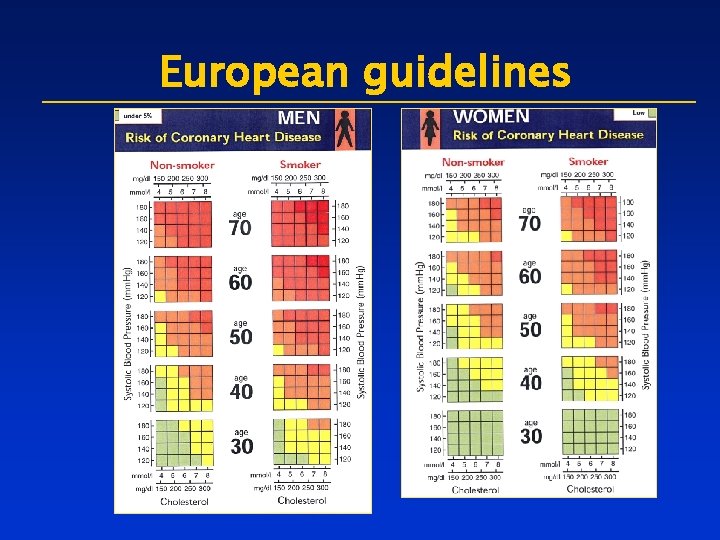
European guidelines • Prioritisation – Absolute risk – 10 year risk • Age – 30 -74 years • Goals for primary and secondary prevention of CHD: – Lifestyle • Stop smoking • Make healthy food choices • Be physically active – Other risk factors • • Blood pressure <140/90 mm. Hg TC <5. 0 mmol/L (190 mg/d. L) LDL-C <3. 0 mmol/L (115 mg/d. L) Good glucose control in diabetes • To be achieved with changes in lifestyle and, if needed, by drug treatment
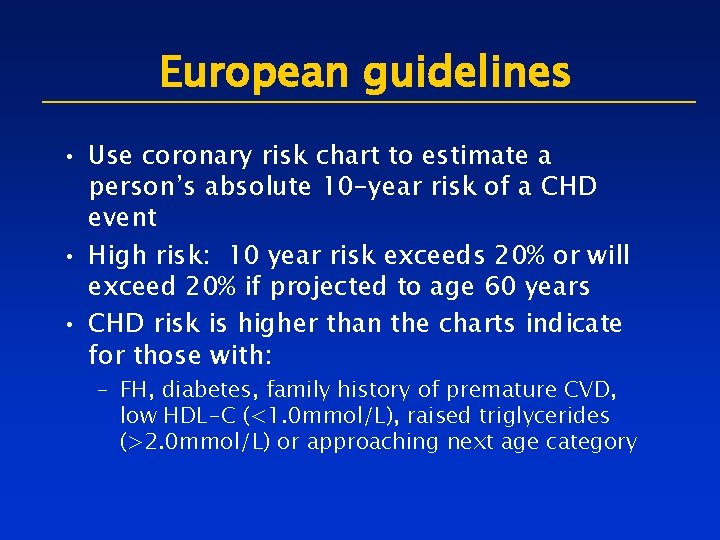
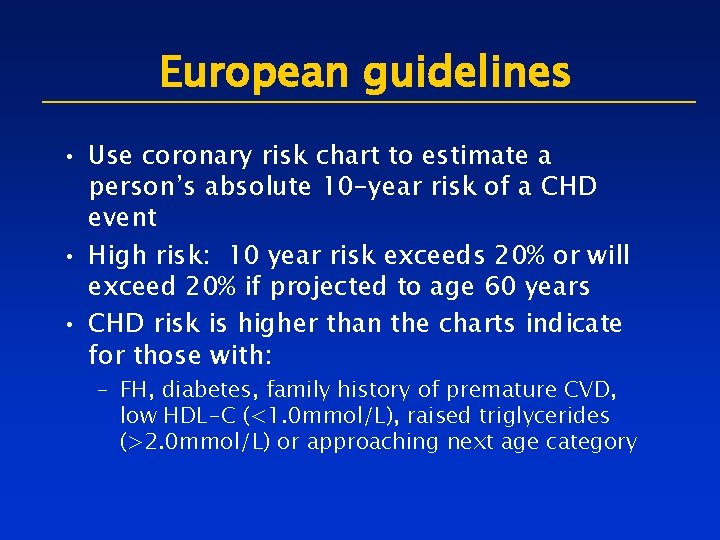
European guidelines • Use coronary risk chart to estimate a person’s absolute 10 -year risk of a CHD event • High risk: 10 year risk exceeds 20% or will exceed 20% if projected to age 60 years • CHD risk is higher than the charts indicate for those with: – FH, diabetes, family history of premature CVD, low HDL-C (<1. 0 mmol/L), raised triglycerides (>2. 0 mmol/L) or approaching next age category
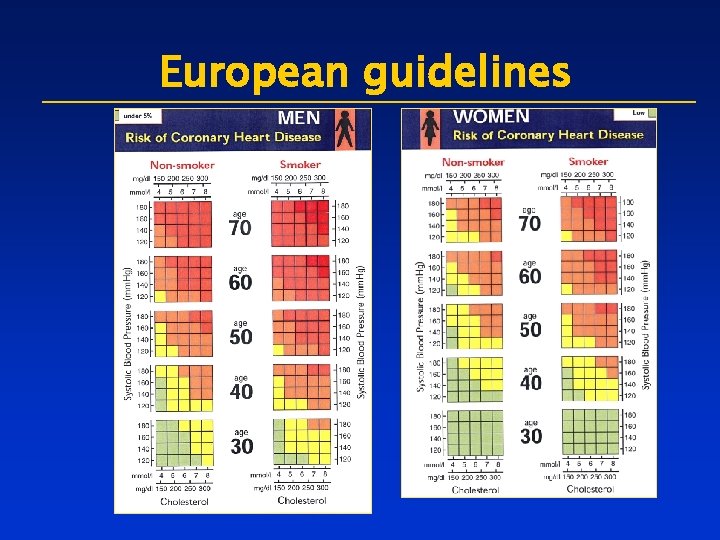
European guidelines
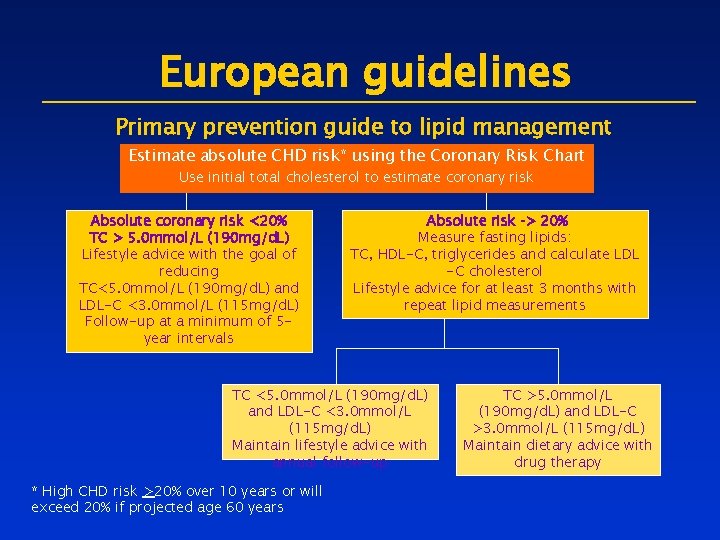
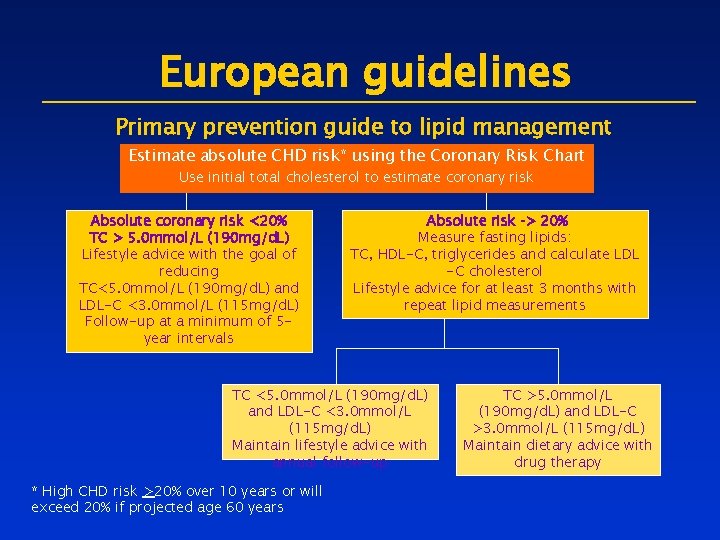
European guidelines Primary prevention guide to lipid management Estimate absolute CHD risk* using the Coronary Risk Chart Use initial total cholesterol to estimate coronary risk Absolute coronary risk <20% TC > 5. 0 mmol/L (190 mg/d. L) Lifestyle advice with the goal of reducing TC<5. 0 mmol/L (190 mg/d. L) and LDL-C <3. 0 mmol/L (115 mg/d. L) Follow-up at a minimum of 5 year intervals Absolute risk > 20% Measure fasting lipids: TC, HDL-C, triglycerides and calculate LDL -C cholesterol Lifestyle advice for at least 3 months with repeat lipid measurements TC <5. 0 mmol/L (190 mg/d. L) and LDL-C <3. 0 mmol/L (115 mg/d. L) Maintain lifestyle advice with annual follow-up * High CHD risk >20% over 10 years or will exceed 20% if projected age 60 years TC >5. 0 mmol/L (190 mg/d. L) and LDL-C >3. 0 mmol/L (115 mg/d. L) Maintain dietary advice with drug therapy
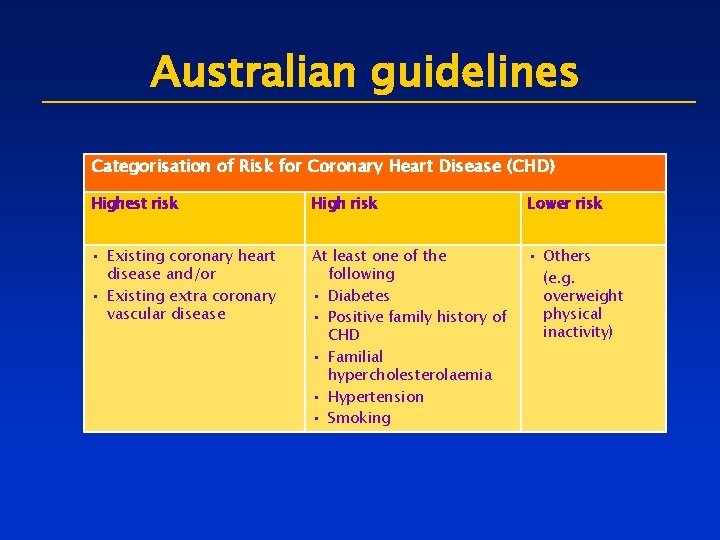
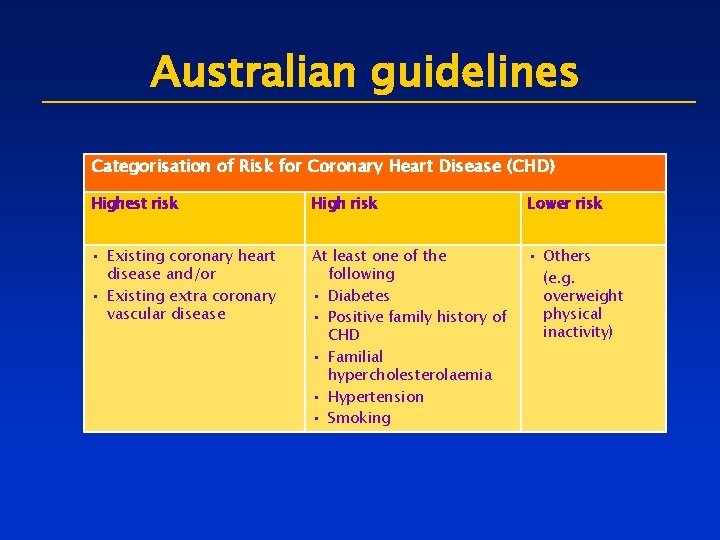
Australian guidelines Categorisation of Risk for Coronary Heart Disease (CHD) Highest risk High risk Lower risk • Existing coronary heart disease and/or • Existing extra coronary vascular disease At least one of the following • Diabetes • Positive family history of CHD • Familial hypercholesterolaemia • Hypertension • Smoking • Others (e. g. overweight physical inactivity)
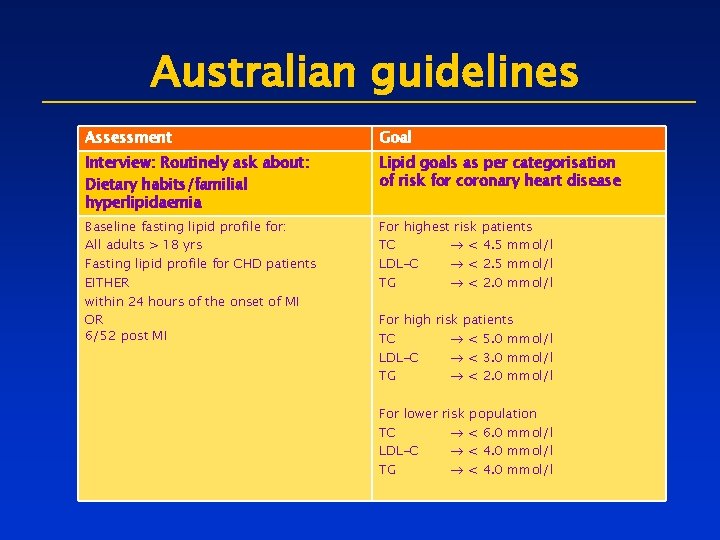
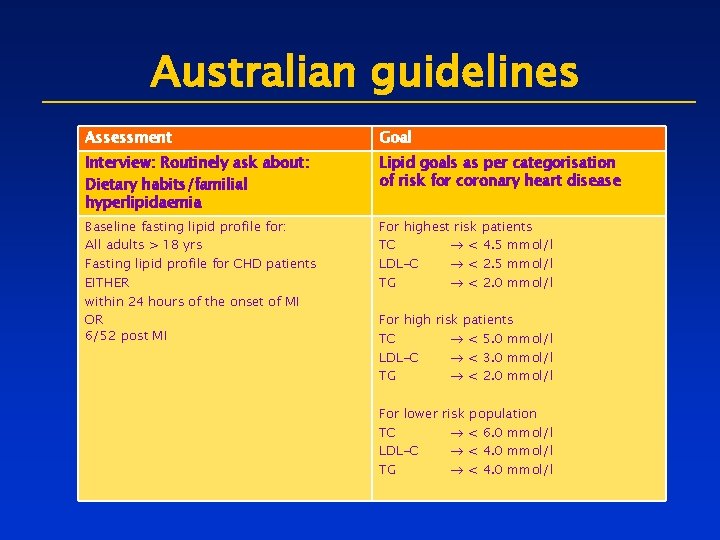
Australian guidelines Assessment Goal Interview: Routinely ask about: Dietary habits/familial hyperlipidaemia Lipid goals as per categorisation of risk for coronary heart disease Baseline fasting lipid profile for: All adults > 18 yrs Fasting lipid profile for CHD patients EITHER within 24 hours of the onset of MI OR 6/52 post MI For highest risk patients TC < 4. 5 mmol/l LDL-C < 2. 5 mmol/l TG < 2. 0 mmol/l For high risk patients TC < 5. 0 mmol/l LDL-C < 3. 0 mmol/l TG < 2. 0 mmol/l For lower risk population TC < 6. 0 mmol/l LDL-C < 4. 0 mmol/l TG < 4. 0 mmol/l
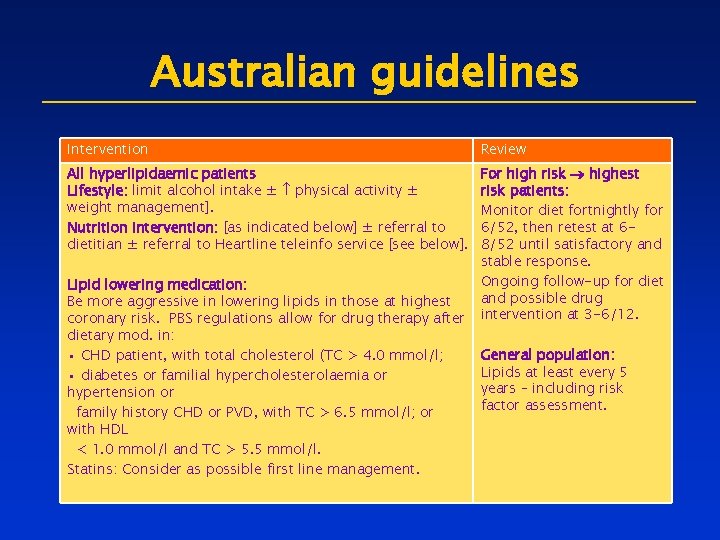
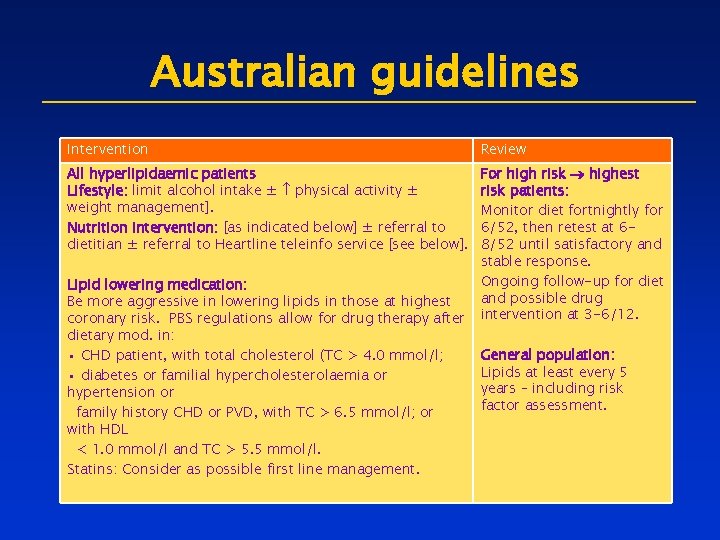
Australian guidelines Intervention Review All hyperlipidaemic patients Lifestyle: limit alcohol intake ± physical activity ± weight management]. Nutrition intervention: [as indicated below] ± referral to dietitian ± referral to Heartline teleinfo service [see below]. For high risk highest risk patients: Monitor diet fortnightly for 6/52, then retest at 68/52 until satisfactory and stable response. Ongoing follow-up for diet and possible drug intervention at 3 -6/12. Lipid lowering medication: Be more aggressive in lowering lipids in those at highest coronary risk. PBS regulations allow for drug therapy after dietary mod. in: • CHD patient, with total cholesterol (TC > 4. 0 mmol/l; • diabetes or familial hypercholesterolaemia or hypertension or family history CHD or PVD, with TC > 6. 5 mmol/l; or with HDL < 1. 0 mmol/l and TC > 5. 5 mmol/l. Statins: Consider as possible first line management. General population: Lipids at least every 5 years – including risk factor assessment.
Issues with guidelines • Goals are not reached resulting in the undertreatment of patients • Guidelines are not implemented resulting in untreated patients
Goals not reached • Evidence shows that patients are failing to reach the goals set in guidelines • 62% of patients failing to reach their goal* • NHANES data show that 82% of CHD patients are not meeting target LDL-C level* • Only 49% of patients with CHD reach total cholesterol targets (EUROASPIRE) References: Pearson TA et al. Arch Intern Med 2000; 160: 458 -67; Hoerger TJ et al. Am J Cardiol; 82: 61 -5; EUROASPIRE. EHJ 2001; 22: 54 -72. *relates to NCEP II ATP goals
 Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals Strategic goals tactical goals operational goals
Strategic goals tactical goals operational goals General goals and specific goals
General goals and specific goals Examples of generic goals and product-specific goals
Examples of generic goals and product-specific goals Ldl goals guidelines
Ldl goals guidelines Expanded opportunity set international finance
Expanded opportunity set international finance Industrial park planning and design
Industrial park planning and design Guidelines international network
Guidelines international network Depuap
Depuap Formuö
Formuö Typiska drag för en novell
Typiska drag för en novell Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Kassaregister ideell förening
Kassaregister ideell förening Tidbok
Tidbok