Assisting in Orthopedic Medicine Chapter 43 Copyright 2011
- Slides: 51
Assisting in Orthopedic Medicine Chapter 43 Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 1
Learning Objectives Define, spell, and pronounce the terms listed in the vocabulary. Apply critical thinking skills in performing patient assessment and care. Describe the principal structures of the musculoskeletal system and their functions. Differentiate among tendons, bursae, and ligaments. Summarize the major muscular disorders. Identify and describe the common types of fractures. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 2
Learning Objectives Explain the difference between osteomalacia and osteoporosis. Classify typical spinal column disorders. Differentiate among the various joint disorders. Summarize the medical assistant’s role in assisting with orthopedic procedures. Explain the common diagnostic procedures used in orthopedics. Compare and contrast therapeutic modalities used in orthopedic medicine. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 3
Learning Objectives Apply cold therapy to an injury. Assist with hot moist heat application to an orthopedic injury. Properly apply therapeutic ultrasound. Explain the use of common ambulatory devices. Properly fit a patient with crutches, and explain the correct mechanics of crutch walking. Prepare for and assist with cast application. Prepare for and assist with cast removal. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 4
Physician Specialists Orthopedic physician Rheumatologist Osteopath Chiropractor Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 5
Functions of the Musculoskeletal System Protection of internal organs Support Movement Hemopoiesis Mineral storage Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 6
Musculoskeletal System Muscles include: skeletal—voluntary; attach to bones Ø cardiac—involuntary Ø smooth—involuntary; line organs, blood vessels, GI tract, etc. Ø The main structures include: skeletal muscles that provide movement Ø tendons that connect muscles to bones Ø bones that provide support, protection, mineral storage Ø ligaments that connect bone to bone Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 7
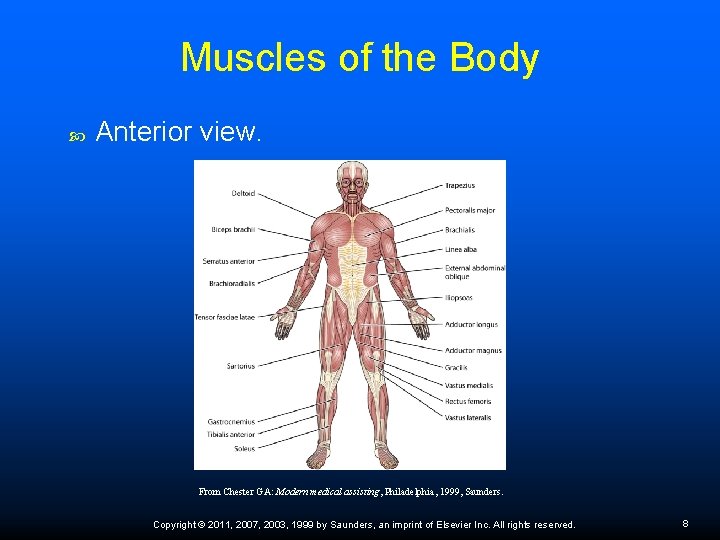
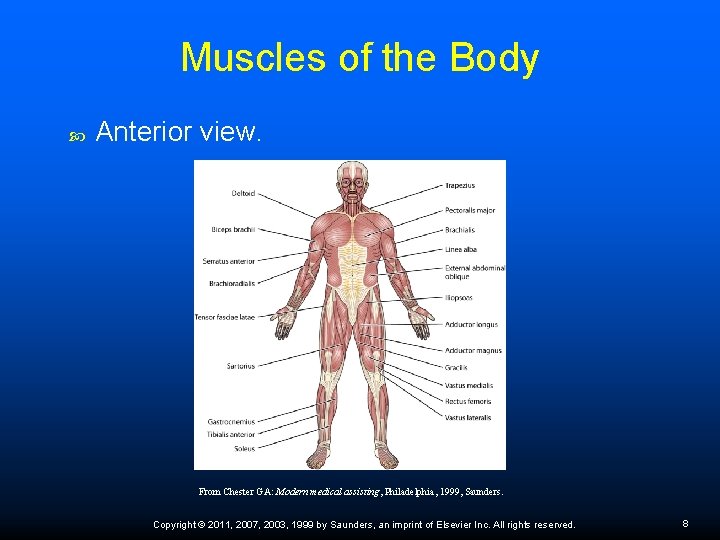
Muscles of the Body Anterior view. From Chester GA: Modern medical assisting, Philadelphia, 1999, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 8
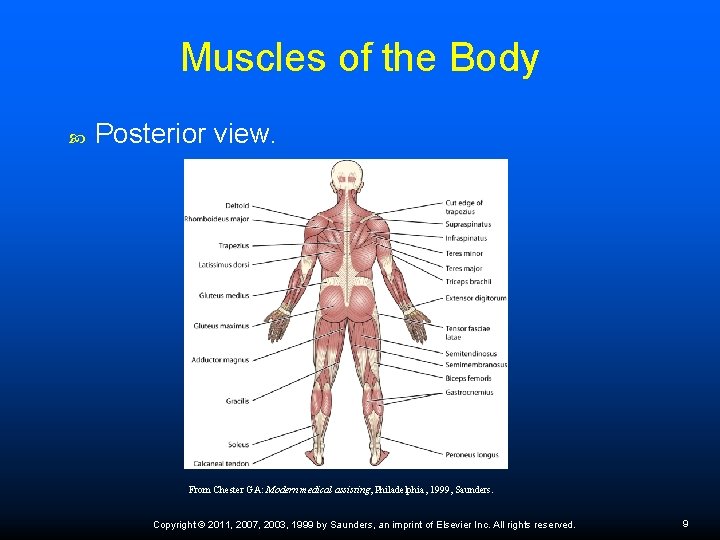
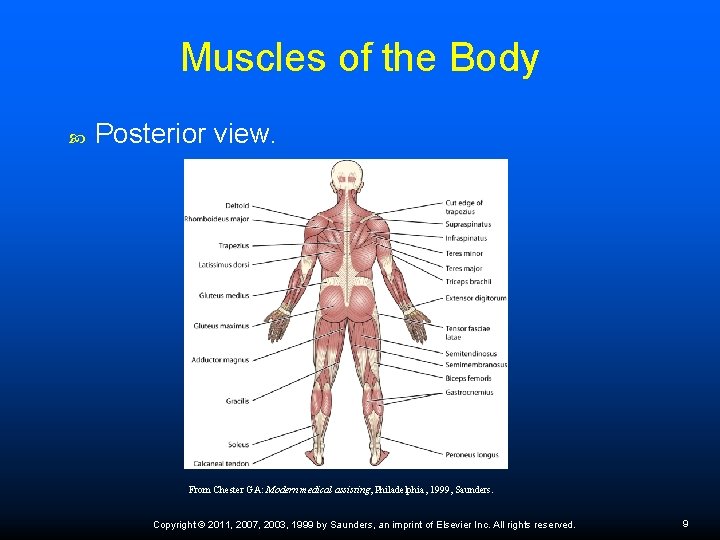
Muscles of the Body Posterior view. From Chester GA: Modern medical assisting, Philadelphia, 1999, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 9
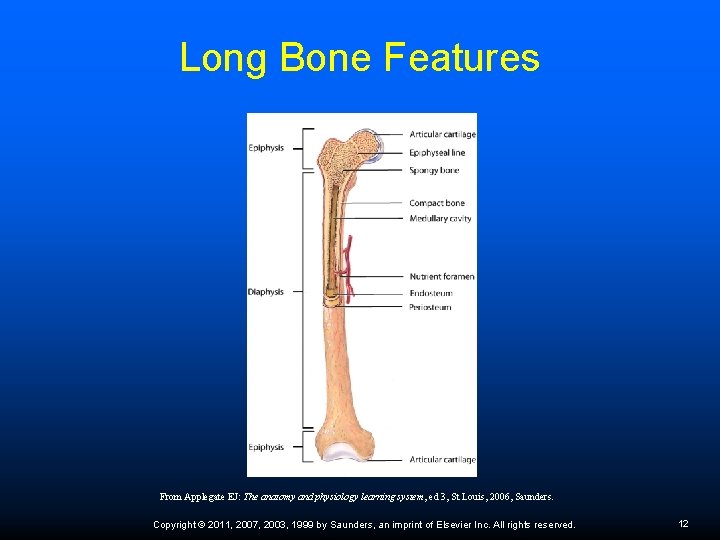
Skeletal Structure Categorized by shape Long bone Diaphysis—shaft Ø Epiphysis—ends Ø Periosteum—membrane covers bones; contains vascular and nervous tissue Ø Red bone marrow—proximal epiphysis of humerus, femur, sternum, ribs, vertebrae; produces blood cells Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 10
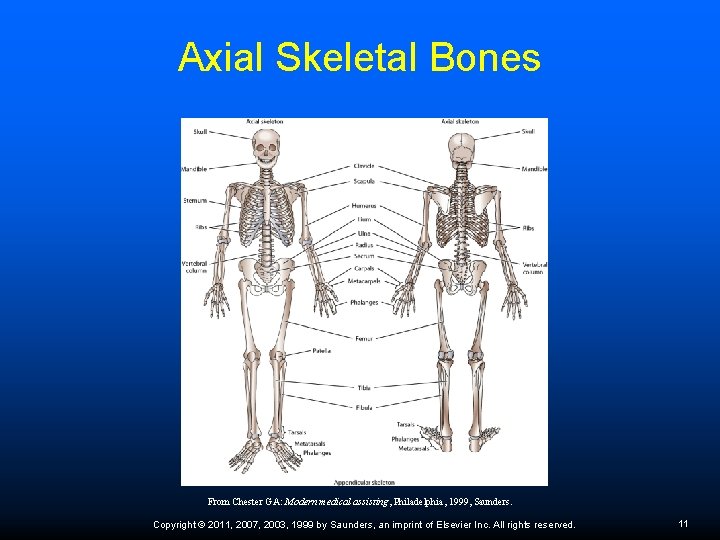
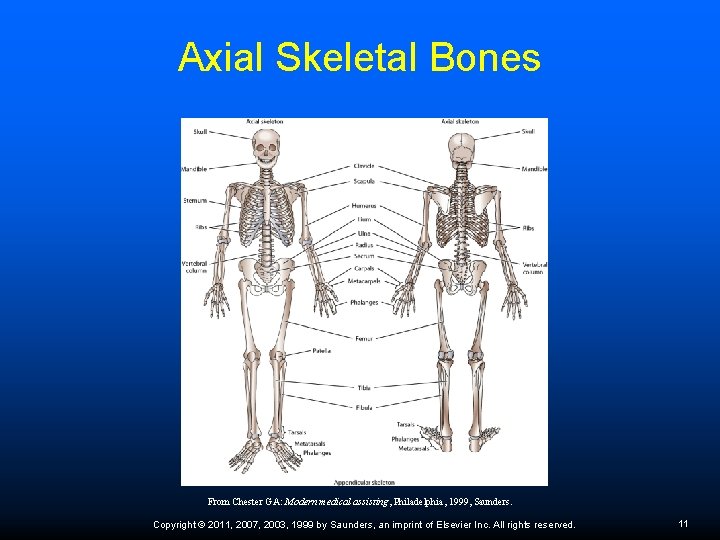
Axial Skeletal Bones From Chester GA: Modern medical assisting, Philadelphia, 1999, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 11
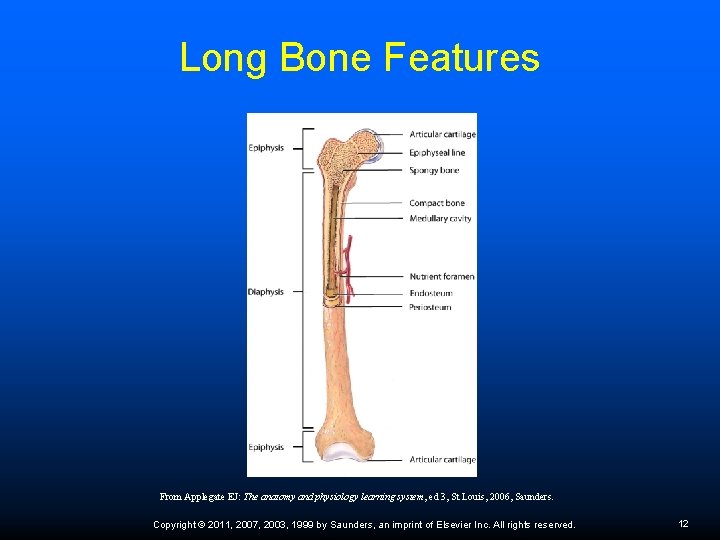
Long Bone Features From Applegate EJ: The anatomy and physiology learning system, ed 3, St Louis, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 12
Telephone Screening Presence of severe pain; inability to bear weight Crooked appearance of injured area or unusual lumps Inability to move injured joint Attempts to use the joint cause limb to buckle or give way Numbness in any part of injured area Inflammation that spreads out from the injured area History of injury to this particular joint Pain, swelling, or inflammation over a bony prominence Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 13
Joints Junctions where bones connect Nonsynovial Synovial fluid Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 14
Types of Joints Classified by the way they are shaped or by their ability to move Sutures Hinged Gliding Ball-and-socket Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 15
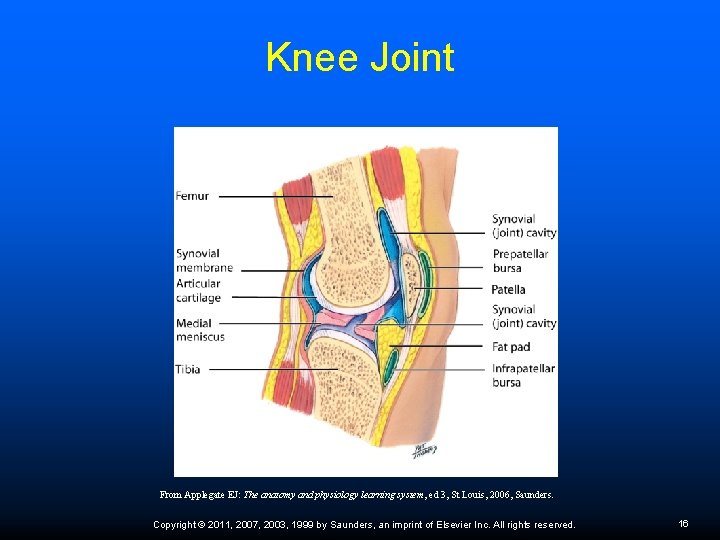
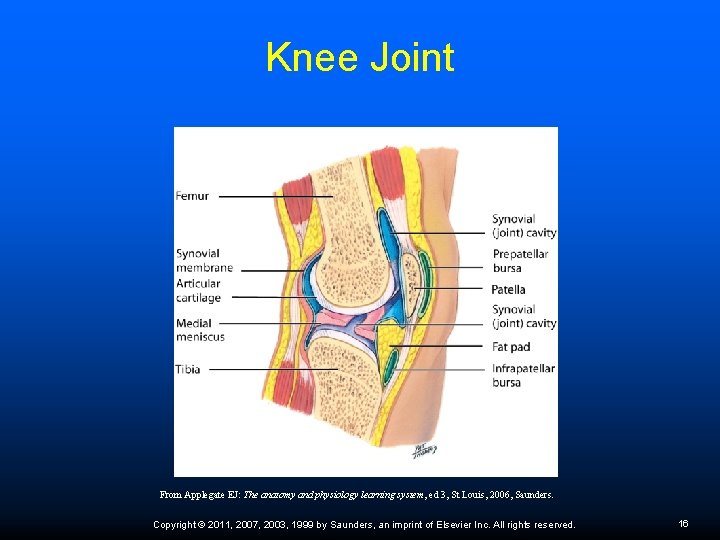
Knee Joint From Applegate EJ: The anatomy and physiology learning system, ed 3, St Louis, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 16
Types of Body Movement: Table 43 -1 Flexion Extension Abduction Adduction Pronation Supination Dorsiflexion Plantar flexion Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 17
Tendons and Ligaments Tendons—tough bands that connect muscles to bones. Ligaments—provide support by connecting bone to bone and preventing a joint from moving beyond its normal range of motion (ROM). Ligament injury occurs when a joint is forced beyond its ROM. Bursae prevent friction between different tissues. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 18
Musculoskeletal Disorders After injury—RICE Maintaining musculoskeletal health — dietary intake of foods rich in calcium and vitamin D, avoid smoking, and weight-bearing exercise Musculoskeletal system disorders account for more missed days at work and more physicians’ office visits than nearly any other medical problem. Trauma Ø Bacteria, fungi, or viruses Ø Autoimmune disorders Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 19
Fibromyalgia Widespread connective tissue, muscular pain and fatigue More frequently in women than in men Pain described as burning, shooting, throbbing, aching, piercing, or stabbing Associated conditions can include sleep disorders, irritable bowel syndrome, chronic headaches, TMJ problems, increased chemical sensitivity, and other musculoskeletal complaints Is often seen in patients with RA, lupus, or hypothyroidism Diagnosis — 11 of 18 specific points to be extremely tender to palpation (Figure 43 -5) Treatment goals include reducing pain, enhancing sleep, and decreasing anxiety and stress Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 20
Restless Leg Syndrome Patient complains of tingling, aching, and twitching of the legs during periods of inactivity, especially at night Overwhelming need to move legs to gain relief Nighttime leg twitching is diagnosed with periodic limb movements of sleep (PLMS), which causes involuntary flexion and extension of legs while sleeping Treatment – relaxation exercises, soaking in a warm bath, cutting back on caffeine, and moderate exercise; medications for Parkinson's disease, anticonvulsants, and muscle relaxants Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 21
Myasthenia Gravis Chronic autoimmune neuromuscular disease Affects voluntary muscle contractions Symptoms – ptosis, diplopia, unstable or waddling gait, altered facial expressions, difficulty swallowing, shortness of breath, dysarthria Caused by defect in transmission of nerve impulses to muscles Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 22
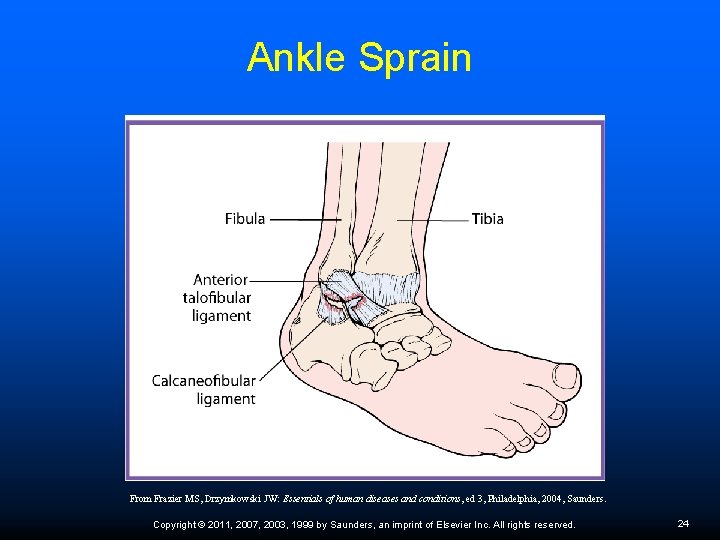
Sprains, Strains, and Spasms Sprain – wrenching or twisting of joint in an abnormal plane of motion or beyond its normal ROM; causes stretching and/or tearing of a ligament Strain – overstretching of muscle or tendon, or a partial or complete tear of the tissue away from the bone Muscle spasms occur spontaneously and may persist for hours; typically caused by heavy exercise and muscle fatigue Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 23
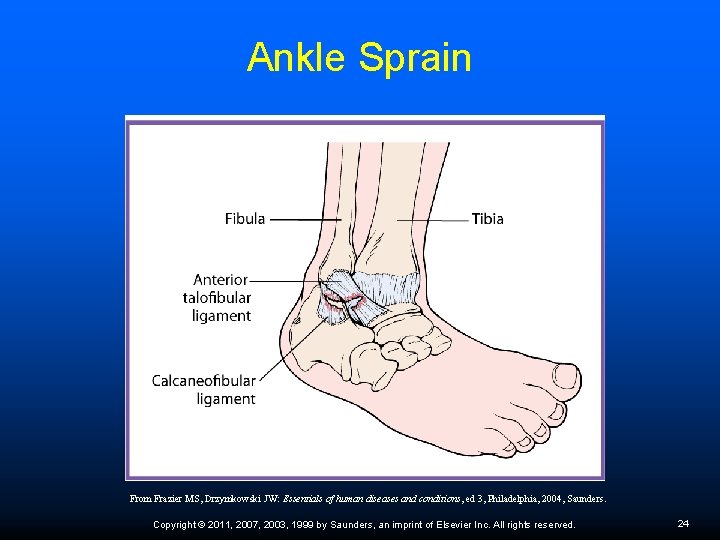
Ankle Sprain From Frazier MS, Drzymkowski JW: Essentials of human diseases and conditions, ed 3, Philadelphia, 2004, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 24
Skeletal Disorders Fractures—see Table 43 -3 Osteomalacia—in children called rickets, from lack of vitamin D; in adults bones soften because of inability to absorb fat and vitamin D or defective kidney function Osteoporosis—progressive loss of bone density Osteopenia – mild bone loss Family history; slight build; amenorrhea; low dietary calcium intake; inactivity; smoking; alcohol abuse Ø Diagnosis: DEXA scan; bone density study (BMD) Ø Treatment: increase vitamin D and calcium, weight-bearing exercise; Fosamax, Didronel, Actonel, Evista, Miacalcin Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 25
Bone Density Recommendations Patients with long-term treatment with medications that can cause osteoporosis, such as prednisone Have type 1 diabetes, liver disease, kidney disease, or a family history of osteoporosis Experienced early menopause (in the early 40 s) Are postmenopausal, older than 50, and have at least one risk factor for osteoporosis Are postmenopausal, older than 65, and have never had a bone density test Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 26
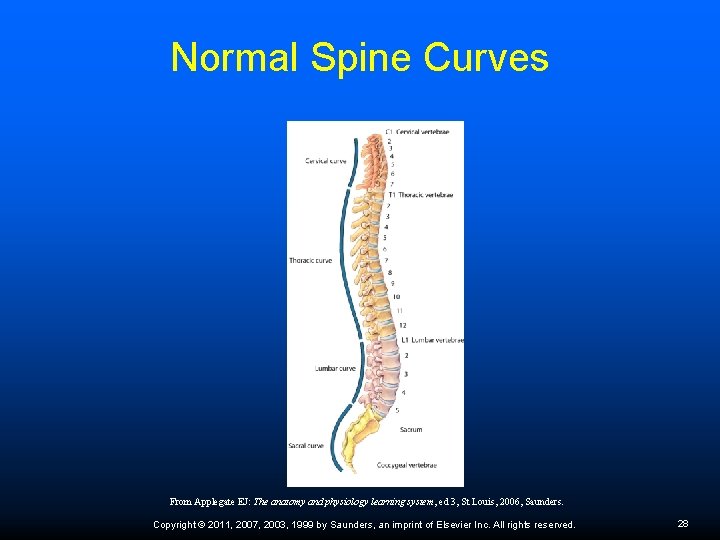
Spinal Disorders Abnormal curvatures Scoliosis Ø Lordosis—swayback Ø Kyphosis—hunchback Ø Herniated disk—nucleus of intervertebral disk protrudes; occurs from trauma or sudden strain on spine; symptoms depend on location and pressure on nerves in the area; diagnosed with MRI, CT, EMG; treatment depends on severity of herniation Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 27
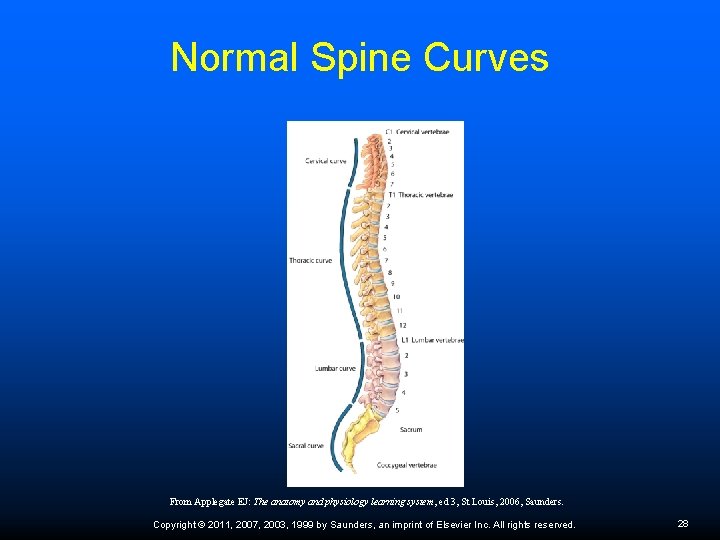
Normal Spine Curves From Applegate EJ: The anatomy and physiology learning system, ed 3, St Louis, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 28
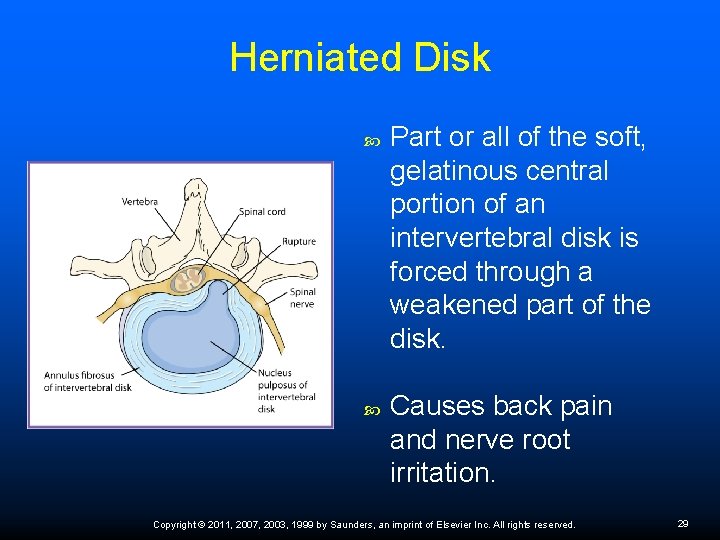
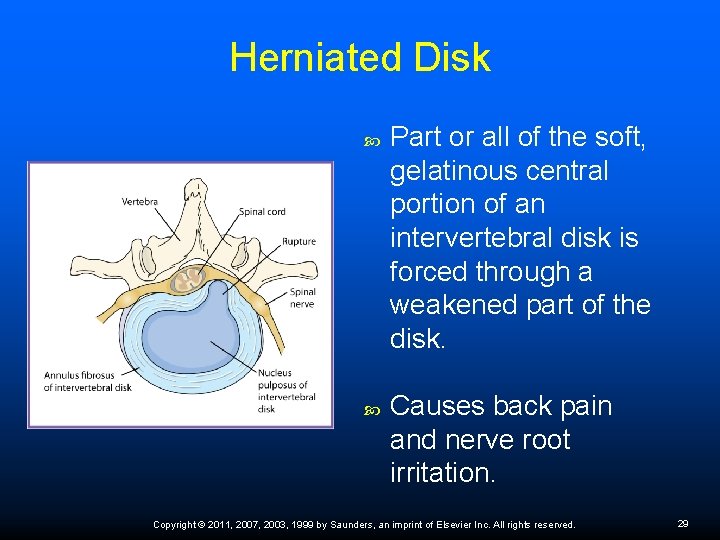
Herniated Disk Part or all of the soft, gelatinous central portion of an intervertebral disk is forced through a weakened part of the disk. Causes back pain and nerve root irritation. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 29
Sciatic Pain Sciatic nerve is the main nerve traveling down the leg. Pain from sciatic nerve originates higher along the spinal cord when nerve roots become compressed or damaged from narrowing of the vertebral column or from a slipped disk. Symptoms can include tingling, numbness, or pain that radiates to the buttocks, legs, and feet. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 30
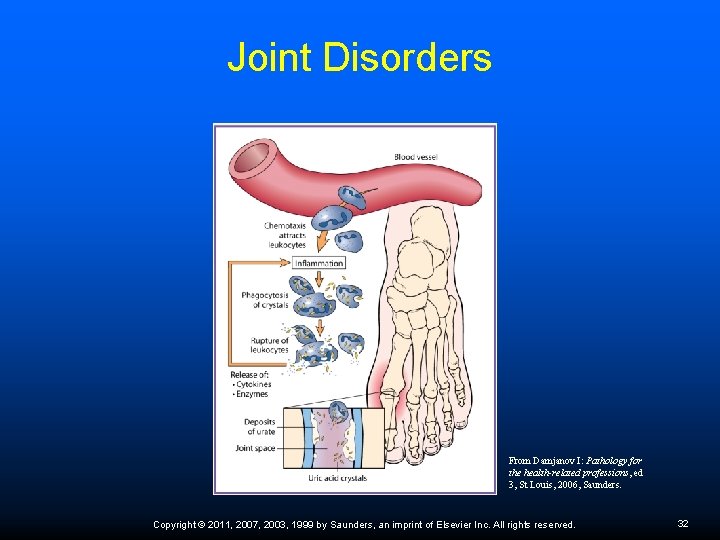
Joint Disorders: Gout Gout—deposit of uric acid crystals into affected joint; remission and exacerbation; diet modification and medication Uric acid is a waste product formed from the breakdown of purines Dietary sources – organ meats, anchovies, herring, asparagus, mushrooms, cold cuts, sausage, and alcohol Treatment – Zyloprim, Aloprim, and Benemid slow rate of uric acid production and enhance its elimination from the body Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 31
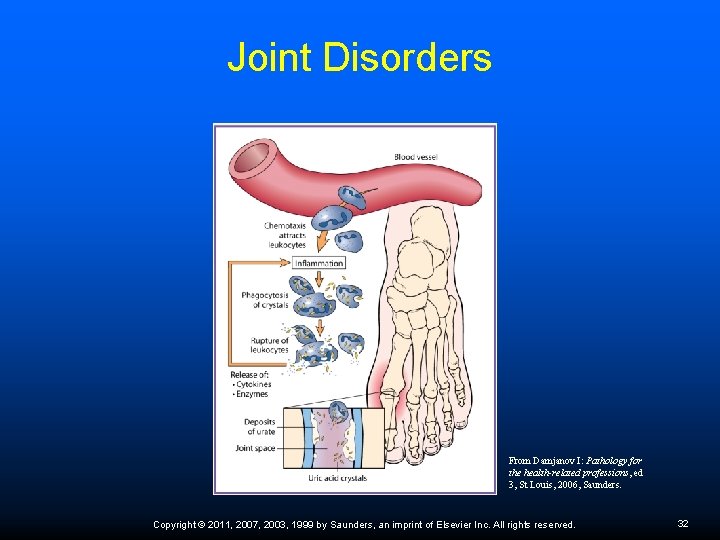
Joint Disorders From Damjanov I: Pathology for the health-related professions, ed 3, St Louis, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 32
Systemic Lupus Erythematosus (SLE) Autoimmune disease of unknown cause; occurs primarily in women 20 to 50 years of age Difficult to diagnose; can affect multiple organs No known cure; goal is to maintain patient function as much as possible; goes through remission and relapse Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 33
Lupus Diagnosis Malar rash—a butterfly-shaped rash across nose and cheeks Discoid rash—raised, scaly patches that may cause scarring Marked sensitivity to sunlight Oral ulcers Arthritis that involves two or more peripheral joints Inflammation of the lining of the heart or lung Renal disease Seizures or psychosis Hematologic disorder – anemia, thrombocytopenia, or leukopenia Elevated antinuclear antibody blood levels (an indicator of an autoimmune disease) Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 34
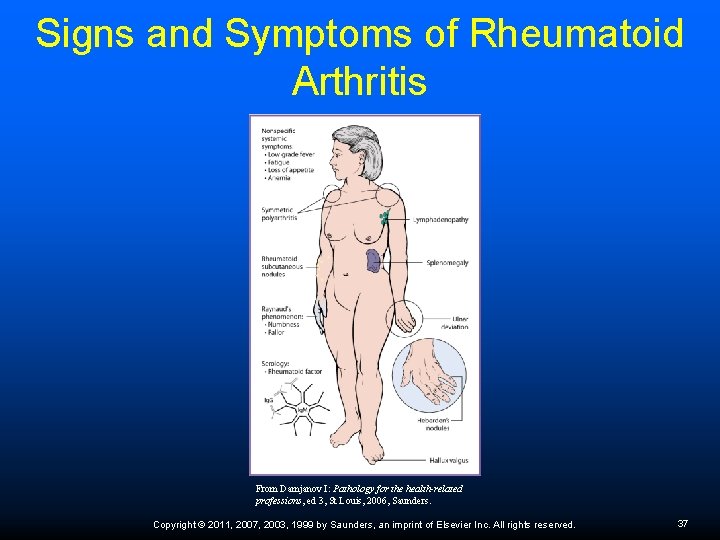
Joint Disorders Lyme disease—caused by bacteria from tick bite; causes fatigue, fever, myalgia, polyarthritis; can invade circulatory and nervous system; treatment is with antibiotics Osteoarthritis—degeneration of articular cartilage; may require joint prosthesis Rheumatoid arthritis—autoimmune attack on synovial membrane; causes pain, edema, damage, deformity of affected joints; treatment includes therapeutic exercise, NSAIDs (Indocin, Naprosyn), ASA Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 35
Lyme Disease Patient Education Wear pants tucked into socks and long-sleeved shirts Use insect repellents that contain DEET Tick-proof yard by clearing brush and leaves Check yourself, children, and pets for ticks; deer ticks are no bigger than the head of a pin or a grain of pepper; shower immediately after being in wooded areas Lyme disease can occur in the same person more than once. Remove a tick with tweezers by gently grasping it near the head or mouth; do not squeeze or crush the tick; pull straight out carefully and steadily; after removal apply antiseptic to area Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 36
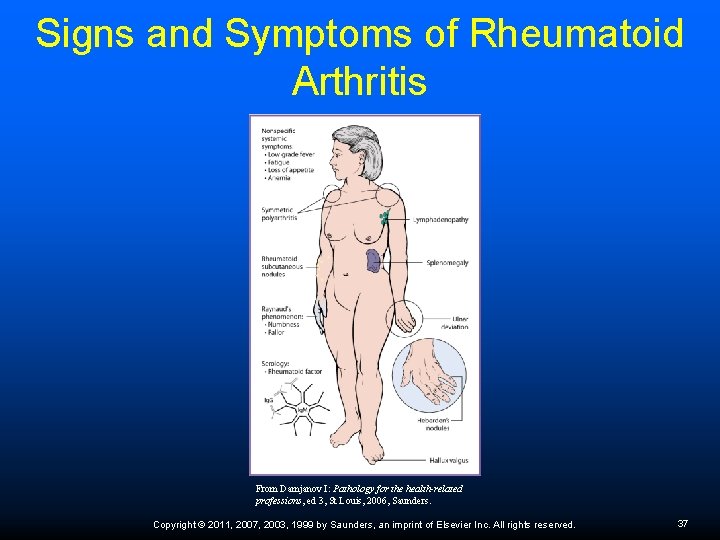
Signs and Symptoms of Rheumatoid Arthritis From Damjanov I: Pathology for the health-related professions, ed 3, St Louis, 2006, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 37
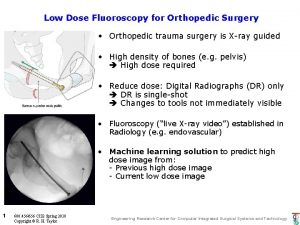
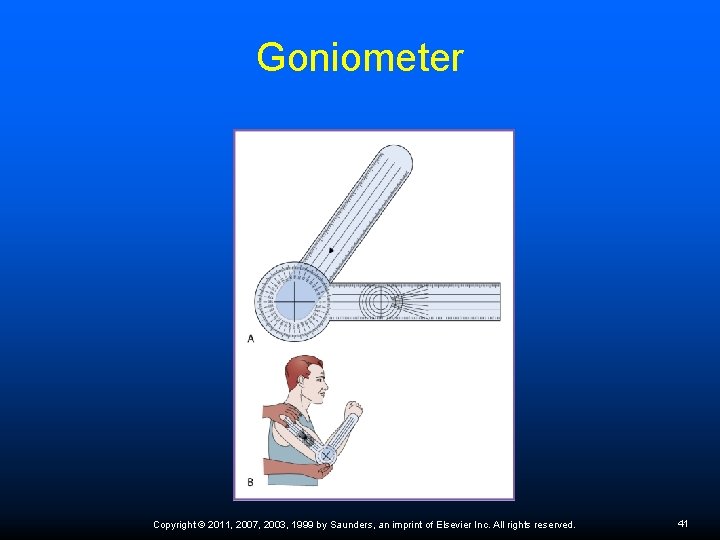
Diagnosis of Musculoskeletal Disorders Common diagnostic procedures include inspection, palpation, percussion, and x-ray studies. It is necessary to rule out bone fractures in many traumatic injuries with radiographs of the injured area. Other diagnostic tools include computed tomography (CT), magnetic resonance imaging (MRI), and diagnostic ultrasound. A goniometer is used to measure ROM of joints. Gait analysis—observe patient walking for abnormalities. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 38
Orthopedic Imaging Arthrograms: Visualizes joints Bone scans: Evaluates areas of bone growth, bone density, and bone tumors, as well as other bone disease patterns Computed tomography (CT) scans: Visualize soft tissue such as tumors, lesions, or some spine injuries Electromyography and nerve conduction velocity studies: Evaluate muscle response to stimulus Biopsies of bone and muscle: Identify cancerous tumors and other neoplasms and pathogens Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 39
Range of Motion ROM—natural distance and direction of movement of a joint; limited ROM indicates a specific joint or body part cannot move through its normal and full movement. Motion may be limited by a mechanical problem within the joint that prevents it from moving beyond a certain point, by edema of tissue around the joint, by muscle spasms, or by pain. Diseases that prevent a joint from fully extending may, over time, produce contractures, causing permanent inability to extend the joint beyond a certain fixed position. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 40
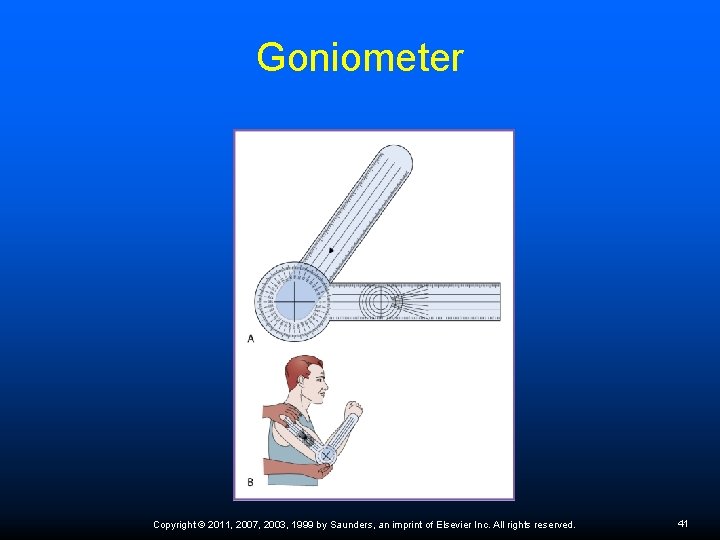
Goniometer Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 41
ROM Assessment In active ROM assessment or exercise, the patient provides and controls the movement. In passive ROM assessment or exercise, therapist provides and controls the movement. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 42
Assistive Devices The most common ambulatory assistive devices are crutches, canes, walkers, and wheelchairs. Fit them properly to the patient, and give the patient adequate instruction on how to use them. Crutches—arm rest should be 2 inches below armpit; elbow bent about 30 degrees; bear weight on good leg, move crutches ahead of good foot and repeat. Review Procedure 43 -4 Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 43
Cold and Heat Application Cold should always be used immediately after an injury to help decrease pain and inflammation and to inhibit additional swelling. Heat after 48 hours promotes circulation and healing, decreases swelling, and causes soft-tissue relaxation. Safety precautions must be followed to prevent possible tissue damage. Review Procedures 43 -1 and 43 -2. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 44
Contraindications for Heat Packs Frst 48 hours of an inflammation In persons with severe circulatory problems; decreased or abnormal sensation Over areas containing encapsulated pus On blisters from previous burns Over scar tissue, because it does not have a normal blood supply and easily overheats In body areas that contain cancerous tumors Over inflamed skin because the initial erythema caused by a burn cannot be detected Over any metal jewelry and over any area containing metal implants Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 45
Paraffin Baths Useful in treating chronic joint inflammation Combine 7 parts paraffin and 1 part mineral oil; heat to 125°F (52°C) Dip body part into warm paraffin mixture and remove immediately; repeat dipping numerous times until there is a thick coating of paraffin on the body part Wrap area with plastic and a towel to allow the heat to penetrate into the tissues Paraffin is kept on for 30 minutes Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 46
Ultrasonography Ultrasound waves cause tissue to vibrate, generating heat as they penetrate superficial tissues and speeding up circulation Increases metabolism in the local area; speeds healing process and helps with pain relief Waves penetrate deeper into body tissues that have a high water content, such as muscles Must be used very carefully around bony areas; waves may concentrate and cause damage Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 47
Physical Therapy Physical therapy can restore normal ROM, muscle strength, and function of the injured part. Other goals include decreasing pain and preserving muscle mass. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 48
Therapeutic Massage Terminology Effleurage: A light, gentle, stroking movement Friction: Deep stroking that affects the deeper soft tissues, traditionally used for back massage Pétrissage: Kneading or rolling with pressing of the muscles Tapotement: Rapid, light percussion done with the sides of the hands Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 49
Cast and Splint Precautions Contact the physician’s office if any of the following occurs: Increased pain and/or a feeling that the splint or cast is too tight Numbness and tingling in the affected hand or foot Burning and stinging because of pressure on the skin Excessive swelling below the cast Loss of active movement of toes or fingers Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 50
Patient Education on Cast Care Keep cast dry Do not walk on “walking cast” until it is completely dry and hard Keep dirt, sand, and powder away from the inside Do not pull out the padding Do not stick objects inside Do not break off rough edges of the cast If skin is red or raw around the cast contact the physician Inspect the cast regularly; report any cracked or soft spots Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 51
 Chapter 42 assisting in other medical specialties
Chapter 42 assisting in other medical specialties Inspection auscultation percussion palpation
Inspection auscultation percussion palpation Chapter 6 general anatomy
Chapter 6 general anatomy Chapter 5 assisting with the nursing process
Chapter 5 assisting with the nursing process Chapter 31 assisting in a medical emergency
Chapter 31 assisting in a medical emergency Chapter 41 assisting in geriatrics
Chapter 41 assisting in geriatrics Chapter 2 dental assisting
Chapter 2 dental assisting Chapter 41 assisting in geriatrics
Chapter 41 assisting in geriatrics Chapter 42 assisting in other medical specialties
Chapter 42 assisting in other medical specialties Dugas test procedure
Dugas test procedure Rop medical assisting
Rop medical assisting Bechterew's test
Bechterew's test Welcoming and greeting the guest procedure
Welcoming and greeting the guest procedure Uva powerpoint template
Uva powerpoint template 2 minute orthopedic exam
2 minute orthopedic exam Search engine optimization for orthopedic practices
Search engine optimization for orthopedic practices Orthopedic history
Orthopedic history Schepelmann test
Schepelmann test Advertise verb form
Advertise verb form Dr. craig shank orthopedic surgery
Dr. craig shank orthopedic surgery Assisting in microbiology and immunology
Assisting in microbiology and immunology Icats nhs
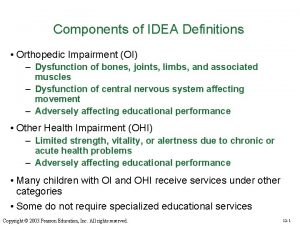
Icats nhs Causes of orthopedic impairment
Causes of orthopedic impairment Orthopedic case presentation
Orthopedic case presentation Orthopedic case presentation
Orthopedic case presentation Idea orthopedic impairment
Idea orthopedic impairment Lokmanya hospitals private limited
Lokmanya hospitals private limited Emory pediatric orthopedics
Emory pediatric orthopedics Pearson's comprehensive medical assisting
Pearson's comprehensive medical assisting Dr todd wilcox
Dr todd wilcox Five historical periods of pharmacy
Five historical periods of pharmacy Chapter 11 complementary and alternative medicine
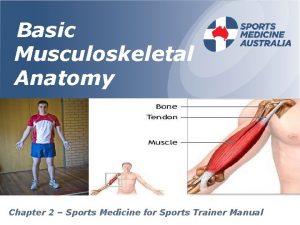
Chapter 11 complementary and alternative medicine Chapter 2 sports medicine
Chapter 2 sports medicine I am a god of medicine chapter 11
I am a god of medicine chapter 11 Wyd 2011 madrid
Wyd 2011 madrid Small business server 2010
Small business server 2010 Small business server 2011 essentials
Small business server 2011 essentials The practice of public relations fraser p. seitel pdf
The practice of public relations fraser p. seitel pdf Uma equipe de cientistas lançará
Uma equipe de cientistas lançará Per-30/pb/2011
Per-30/pb/2011 Kidush shavuot
Kidush shavuot Everson gillmouth
Everson gillmouth Sage act 2011
Sage act 2011 Chemistry regents 2011
Chemistry regents 2011 2011-1989
2011-1989 There names
There names Perfil de egreso de 1 de primaria
Perfil de egreso de 1 de primaria Pergub 140 tahun 2011
Pergub 140 tahun 2011 Perbedaan pp 46 2011 dan pp 30 2019
Perbedaan pp 46 2011 dan pp 30 2019 Usa infotehnoloog 1955-2011
Usa infotehnoloog 1955-2011 Kiraan gaji pekerja
Kiraan gaji pekerja Paradise hotel 2011
Paradise hotel 2011