Advances in the Treatment of AgeRelated Macular Degeneration
- Slides: 22
Advances in the Treatment of Age-Related Macular Degeneration (AMD) Michael E. Helm, PA-S Spring 2007 Advisor: Sam Powdrill, MPhil, PA-C
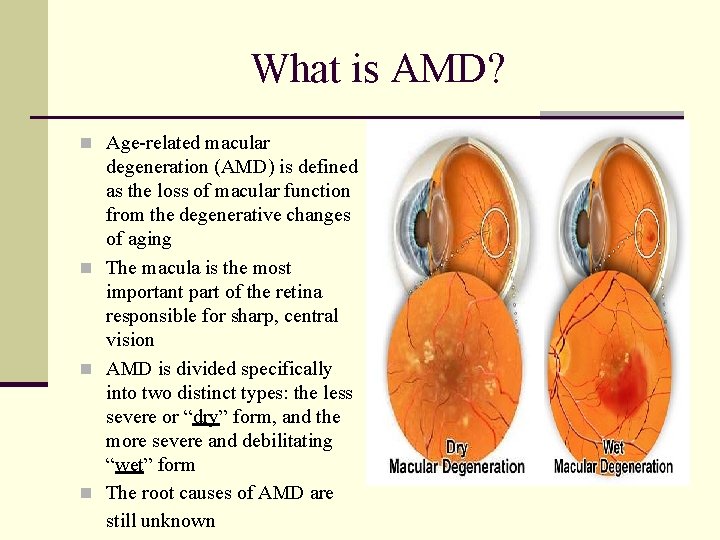
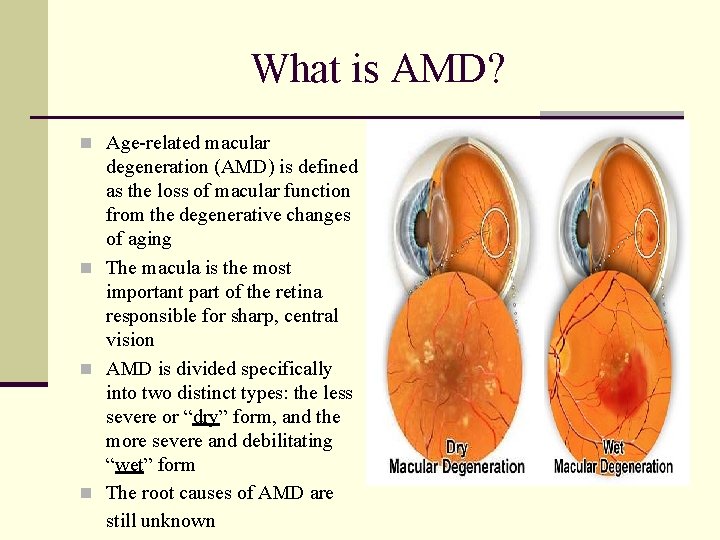
What is AMD? n Age-related macular degeneration (AMD) is defined as the loss of macular function from the degenerative changes of aging n The macula is the most important part of the retina responsible for sharp, central vision n AMD is divided specifically into two distinct types: the less severe or “dry” form, and the more severe and debilitating “wet” form n The root causes of AMD are still unknown
Who is at Risk for AMD? n AMD is the leading cause of irreversible vision loss and blindness in persons over 65 years of age, the fastest growing segment of the United States population n Over a 5 -year time span, it is estimated that 1 in 3 people over the age of 70 years will develop signs of AMD n Caucasians > African Americans n Women > Men
What are the Risk Factors for AMD? n There are currently 5 specific risk factors that are strongly associated with the development of AMD: 1. Caucasian Ancestry 2. Genetic Component 3. Hypertension 4. Aging 5. Smoking (SO QUIT NOW!!!!)
How is AMD Diagnosed? n As with many other medical conditions, the approach to diagnosing AMD requires the integration of both the patient history and the physical exam n Commonly patients will complain of visual symptoms such as blurred or distorted vision, a need for increased lighting, an increase in fatigue when reading, blind spots in central vision, and reports of utility poles being curved or bent when driving
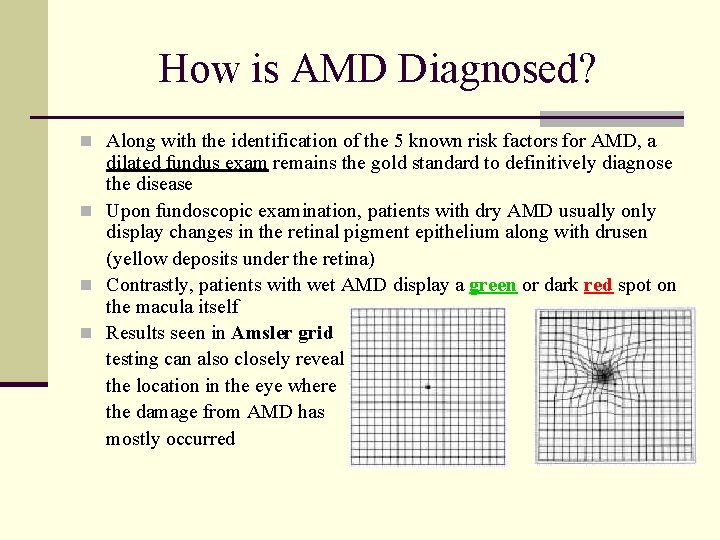
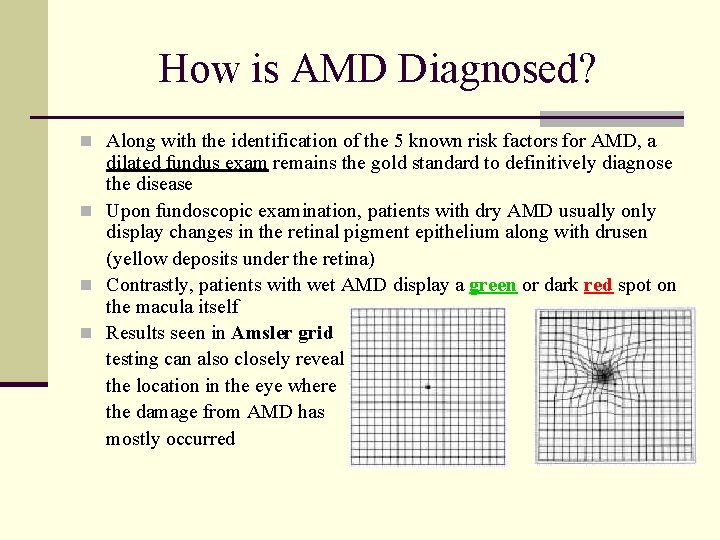
How is AMD Diagnosed? n Along with the identification of the 5 known risk factors for AMD, a dilated fundus exam remains the gold standard to definitively diagnose the disease n Upon fundoscopic examination, patients with dry AMD usually only display changes in the retinal pigment epithelium along with drusen (yellow deposits under the retina) n Contrastly, patients with wet AMD display a green or dark red spot on the macula itself n Results seen in Amsler grid testing can also closely reveal the location in the eye where the damage from AMD has mostly occurred
Preventative Approaches for AMD n Age-Related Eye Disease Study (AREDS) Formulation: The specific daily amounts of antioxidants and zinc used by the study researchers were 500 milligrams of vitamin C, 400 International Units of vitamin E, 15 milligrams of beta-carotene (often labeled as equivalent to 25, 000 International Units of vitamin A), 80 milligrams of zinc as zinc oxide, and two milligrams of copper as cupric oxide. Copper was added to the AREDS formulation containing zinc to prevent copper deficiency anemia, a condition associated with high levels of zinc intake This has been the standard of preventative treatment for AMD since the AREDS study was done in 2001
Preventative Approaches for AMD n The AREDS formulation should only be taken when n n n prescribed by a physician or a P. A. AREDS is the treatment of choice for “dry” AMD Eating fresh fruits and dark green, leafy vegetables Maintaining a low fat & low cholesterol diet Exercising regularly Wearing sunglasses with UV protection Avoiding exposure to second-hand smoke Getting an eye exam regularly
Current Treatments for AMD n Laser Photocoagulation n Used to prevent further vision loss from wet AMD n Developed in the 1980’s n Was the only available treatment for wet AMD prior to the 21 st century n The laser procedure basically destroys the new, leaky blood vessels that cause the substantial vision loss in wet AMD n This type of treatment for AMD can be very destructive to the eye itself if the laser is used too close to the macula, causing immediate and permanent vision loss
Current Treatments for AMD n Verteporfin Photodynamic Therapy (PDT) n Used to prevent further vision loss from wet AMD n Developed in 2000, this treatment uses a photoactivated drug, Verteporfin, and an activating nonthermal laser n This was the first drug therapy developed for AMD n Verteporfin is a photoexcitable dye that is retained mainly in the wet tissues of the retina and is activated by the light from the laser n Once activated, the drug thromboses the new blood vessels in the area and leads to a much slower rate of vision loss in the AMD patient
Current Treatments for AMD Pegaptanib Sodium (MACUGEN®) Used to prevent further vision loss from wet AMD Was first introduced in 2004 Was the first intravitreal injectable drug developed to treat wet AMD, and requires monthly dosing n In the VISION (VEGF Inhibition Studies in Ocular Neovascularization) clinical trials in 2003 and 2004, 70% of patients treated with a small dose of Macugen (0. 3 mg) injected every 6 weeks had < 15 letters of vision loss at the primary end point analysis, compared to only 55% of the control group n Macugen has less adverse effects and a better safety profile than either laser photocoagulation or PDT n n
Current Treatments for AMD n Ranibizumab (LUCENTIS®) n Approved by the FDA on June 30 th, 2006 n Intravitreal injection that requires monthly dosing n The only FDA-approved drug that not only drastically slows vision loss due to AMD, but it also seems to actually restore some visual acuity that has already been lost due to wet AMD destruction n In the MARINA study in 2004 -2005 researching Lucentis, out of 716 patients enrolled, at 12 months 94. 5% of the group given 0. 3 mg of Lucentis and 94. 6% of those given 0. 5 mg lost < 15 letters, as compared with 62. 2% of patients receiving the control injections
Current Treatments for AMD n Mean increases in visual acuity were 6. 5 letters in the 0. 3 mg group and 7. 2 letters in the 0. 5 mg group, as compared with a decrease of 10. 4 letters in the control injection group n Numbers seen in a similar study (ANCHOR) comparing Lucentis against Verteporfin PDT were nearly identical to the MARINA study, favoring Lucentis n Lucentis had no long-term effect on intraocular pressure, and very few instances (<1%) of detached retina or uveitis were reported n Endopthalmitis was also reported in <1% of the patients, but this adverse effect was concluded to be caused by the injection procedure alone
Investigational Treatments for AMD n Bevacizumab (AVASTIN®) n Avastin was approved by the FDA in February 2004 for the treatment of metastatic colorectal cancer in combination with chemotherapy n Incidentally, ranibizumab (Lucentis) is a chemically modified product of bevacizumab (Avastin) that is affinity-matured to have a higher affinity for VEGF, and it is made by the same laboratory, Genetech, that also produces Avastin n After initial results in 2005 from clinical trials with Lucentis became available, ophthalmologists began using Avastin to treat AMD because of its similar chemical structure to Lucentis
Investigational Treatments for AMD n Avastin requires monthly intravitreal injections n Outcomes in patients treated thus far with Avastin have been virtually identical to Lucentis, with no serious ocular effects reported n It must be noted though that intravitreal treatment with Avastin has not been proven effective and safe in controlled clinical trials like Lucentis
Barriers to AMD Treatment n Most Treatments are EXPENSIVE!!!!! n Macugen = ~$900 per injection (per eye) n Lucentis = ~$1, 950 per injection (per eye) n In the United States, under Medicare, Macugen or Lucentis is covered through Part B; patients are responsible for a 20% co-payment for each injection n This would still require nearly $400 per month (or $800 if both eyes were significantly affected) that the patient would be required to pay out-of-pocket per injection, unless they had a Medicare supplemental insurance or qualified for a support program like Medicaid
A More Affordable Option? n Avastin n Not nearly as expensive as drugs specifically designed for treatment of AMD n ~$6 → $10 per injection (per eye) n Already is used widely by ophthalmologists around the world n However, it does not have randomized, clinical trials to back up the efficacy and safety of its use in AMD
A More Affordable Option? n Fortunately, most national insurance carriers cover intravitreal injections of Avastin, given with the patient’s informed consent, just as they do Lucentis even though a national policy supporting this practice has never been officially adopted n Currently, there appears to be a global consensus that the treatment strategy using intravitreal Avastin is logical, the potential risks to patients are minimal, and the cost-effectiveness is so obvious that the treatment should not be withheld due to lack of clinical trial evidence (Rosenfeld, 2006)
Conclusion n While AMD continues to afflict a vast number of individuals over the age of 65 each year, treatments are now being utilized that finally counteract the most debilitating aspects of this disease n It is imperative for people who are at risk for developing AMD to understand preventative measures they can employ such as implementing smoking cessation and controlling hypertension which can have huge impact on the initial development of the disease n Recognize as primary care providers that AMD is seen commonly in practice today, and there are now methods of treatment that can be used to help these patients n Do not hesitate to refer to an ophthalmologist for tx!!!!
References n n n n n n n 1. Augustin AJ, Offermann I. Emerging drugs for age-related macular degeneration. Expert Opin Emerg Drugs 2006; 11(4): 725 -740. 2. Bashshur ZF, Bazarbachi A, Schakal A, Haddad ZA, El Haibi CP, Noureddin BN Intravitreal bevacizumab for the management of choroidal neovascularization in age-related macular degeneration. Am J Opthalmol 2006; 142(1): 1 -9. 3. Brown DM, Kaiser PK, Michels M, Soubrane G, Heier JS, Kim RY, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 2006; 355(14): 1432 -1444. 4. D’Amico DJ, Patel M, Adamis AP, Cunningham ET Jr, Guyer DR, Katz B. Pegaptanib sodium for neovascular age-related macular degeneration: two-year safety results of the two prospective, multicenter, controlled clinical trials. Opthalmology 2006; 113(6): 1001. e 1 -6. 5. Eter N, Krohne TU, Holz FG. New pharmacologic approaches to therapy for age-related macular degeneration. Biodrugs 2006; 20(3): 167 -179. 6. Freeman WR, Falkenstein I. Avastin and new treatments for AMD: where are we? Retina 2006; 26(8): 853 -858. 7. Heier JS, Antoszyk AN, Pavan PR, Leff SR, Rosenfeld PJ, Ciulla TA, et al. Ranibizumab for treatment of neovascular age-related macular degeneration: a phase I/II multicenter, controlled, multidose study. Opthalmology 2006; 113(4): 642. e 1 -4. 8. Kourlas H, Schiller DS. Pegaptanib sodium for the treatment of neovascular age-related macular degeneration: a review. Clin Ther 2006; 28(1): 36 -44. 9. Michels S, Schmidt-Erfurth U, Rosenfeld PJ. Promising new treatments for neovascular age-related macular degeneration. Expert Opin Investing Drugs 2006; 15(7): 779 -793. 10. National Institutes of Health, National Eye Institute. Age-related macular degeneration. November 2006. Available at: macular degeneration. Exp Eye Res 2006; 83(3): 615 -619. http: //www. nei. nih. gov/health/maculardegen/armd_facts. asp. Accessed November 10, 2006.
References n n n n n n 11. Ng EW, Adamis AP. Targeting angiogenesis, the underlying disorder in neovascular age-related macular degeneration. Can J Opthalmol 2005; 40(3): 352 -368. 12. Pieramici DJ, Avery RL. Ranibizumab: treatment in patients with neovascular age-related macular degeneration. Expert Opin Emerg Drugs 2006; 6(11): 1237 -1245. 13. Rosenfeld PJ. Intravitreal avastin: the low cost alternative to lucentis? Am J Opthalmol 2006; 142(1): 141 -143. 14. Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006; 355(14): 1419 -1431. 15. Slakter JS. Anecortave acetate for treating or preventing choroidal neovascularization. Opthalmol Clin North Am 2006; 19(3): 373 -380. 26 16. Spaide RF, Laud K, Fine HF, Klancnik JM Jr, Meyerle CB, Yannuzzi LA, et al. Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina 2006; 26(4): 383 -390. 17. Steinbrook R. The price of sight—ranibizumab, bevacizumab, and the treatment of macular degeneration. N Engl J Med 2006; 355(14): 1409 -1412. 18. Vavvas D, D’Amico DJ. Pegaptanib (Macugen): treating neovascular age-related macular degeneration and current role in clinical practice. Opthalmol Clin North Am 2006; 19(3): 353 -360. 19. Wiggins MN, Uwaydat SH. Age-related macular degeneration: options for earlier detection and improved treatment. J Fam Pract 2006; 55(1): 22 -27. 20. Zhou B, Wang B. Pegaptanib for the treatment of age-related
Questions? ? Thank you!!
 Sue strachan
Sue strachan Anders brevik
Anders brevik Macular scar
Macular scar Macula sparing
Macula sparing Macular hole stages
Macular hole stages Transneuronal degeneration
Transneuronal degeneration Lattice degeneration
Lattice degeneration Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Myoma degeneration
Myoma degeneration Beaded dentinal tubules
Beaded dentinal tubules Cg amp
Cg amp Lattice degeneration
Lattice degeneration Subacute combined degeneration of the cord
Subacute combined degeneration of the cord Terrien marginal degeneration
Terrien marginal degeneration Necrotic cell
Necrotic cell Input motor
Input motor Cornea verticillata
Cornea verticillata Classification of advances as per rbi
Classification of advances as per rbi Advances in technology during wwii
Advances in technology during wwii Short term loans and advances
Short term loans and advances Global oncology trends 2017 advances complexity and cost
Global oncology trends 2017 advances complexity and cost Intellectual development of infants chapter 9
Intellectual development of infants chapter 9 Opto-electronic advances
Opto-electronic advances