Adult Nursing I Topic Care of clients with
- Slides: 47
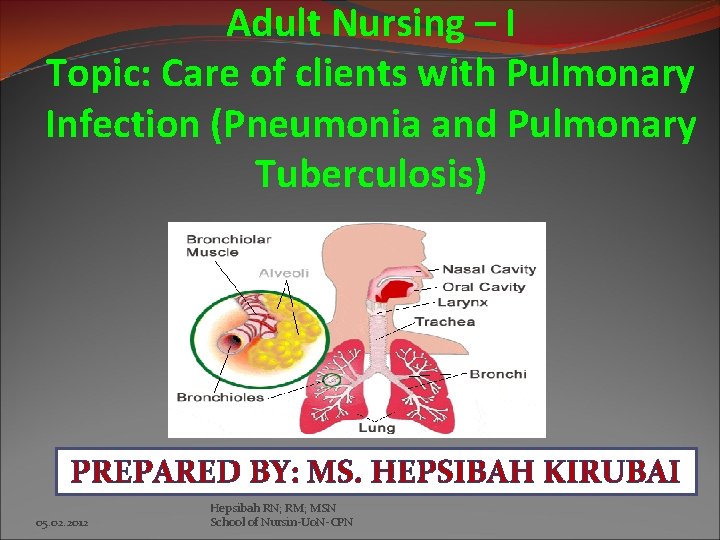
Adult Nursing – I Topic: Care of clients with Pulmonary Infection (Pneumonia and Pulmonary Tuberculosis) PREPARED BY: MS. HEPSIBAH KIRUBAI 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Learning Outcome �Describe the causes, pathophysiology, clinical manifestations, treatment (drug and surgery) and the nursing care for individuals with pulmonary infections (Pneumonia & Pulmonary Tuberculosis) �Demonstrate beginning skills in the care of clients/patients with pulmonary infections. (Pneumonia & Pulmonary Tuberculosis) �Develop beginning skills in giving health education to clients/patients with pulmonary infections (Pneumonia & Pulmonary Tuberculosis). 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
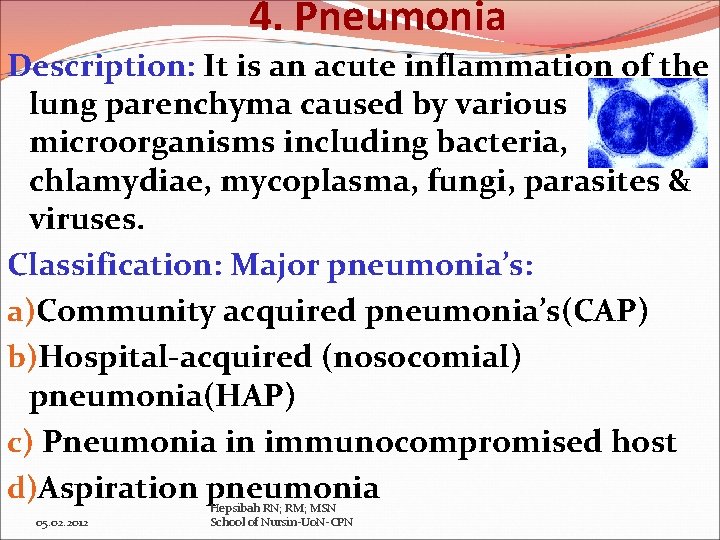
4. Pneumonia Description: It is an acute inflammation of the lung parenchyma caused by various microorganisms including bacteria, chlamydiae, mycoplasma, fungi, parasites & viruses. Classification: Major pneumonia’s: a)Community acquired pneumonia’s(CAP) b)Hospital-acquired (nosocomial) pneumonia(HAP) c) Pneumonia in immunocompromised host d)Aspiration pneumonia 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
4. Pneumonia: Classification a) Community-Acquired Pneumonia (CAP): CAP occurs in the community setting or within the first 48 hours after hospitalization or institutionalization. b) Hospital-Acquired Pneumonia (HAP) or Nosocomial pneumonia: Defined as the onset of pneumonia symptoms more than 48 hours after admission in patients with no evidence of infection at the time of admission. c) Pneumonia in the Immuno-compromised Hosts includes Pneumocystis pneumonia (PCP), fungal pneumonias & mycobacterium tuberculosis d) Aspiration Pneumonia: Refers to the pulmonary consequences resulting from entry of endogenous or exogenous substances into the lower airway. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
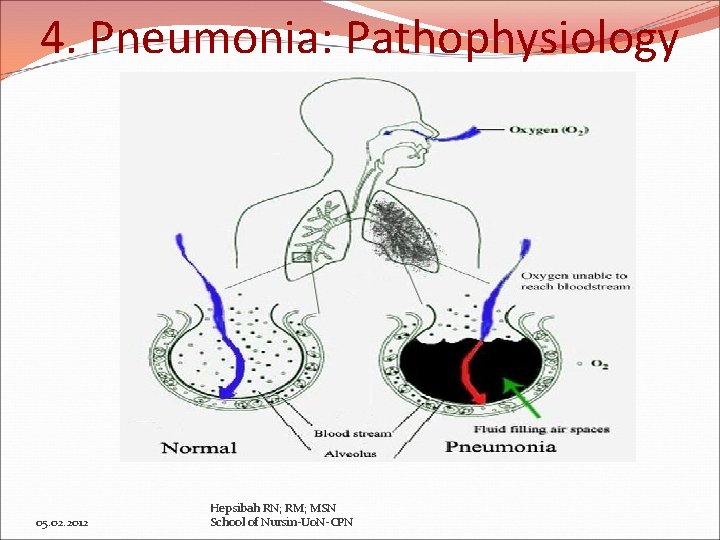
4. Pneumonia: Pathophysiology Inflammatory reaction occurs in alveoli exudate interferes with diffusion of O 2 & CO 2. ↓ Neutrophils migrate into the alveoli & fill the normally air-containing spaces ↓ Secretions & mucosal edema causes partial occlusion of bronchi/alveoli ↓ O 2 tension ↓ Ventilation-perfusion mismatch in the affected lung arterial hypoxemia Pneumonia (Bronchopneumonia more common than lobar pneumonia) Hepsibah RN; RM; MSN 05. 02. 2012 School of Nursin-Uo. N-CPN
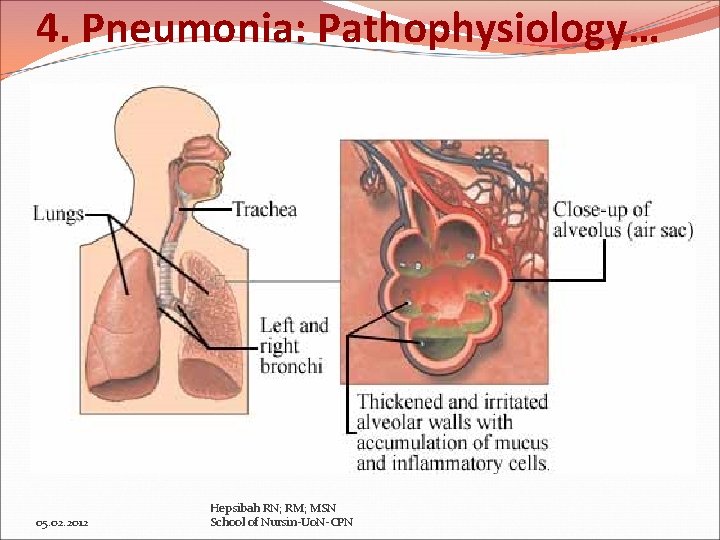
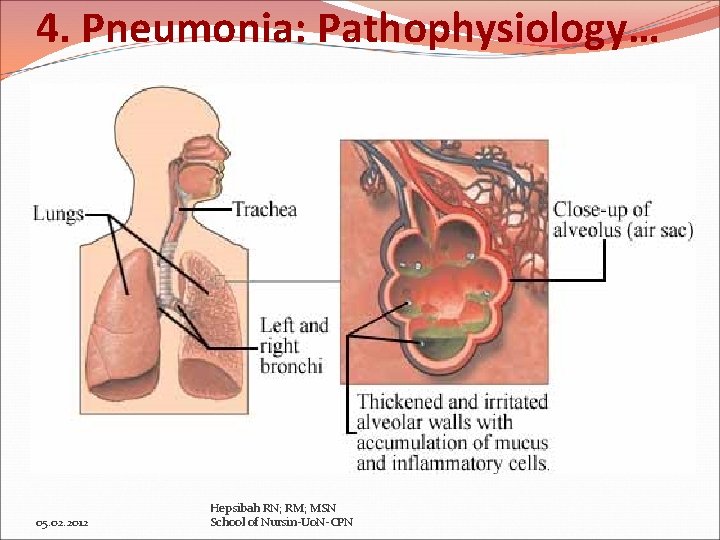
4. Pneumonia: Pathophysiology… 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
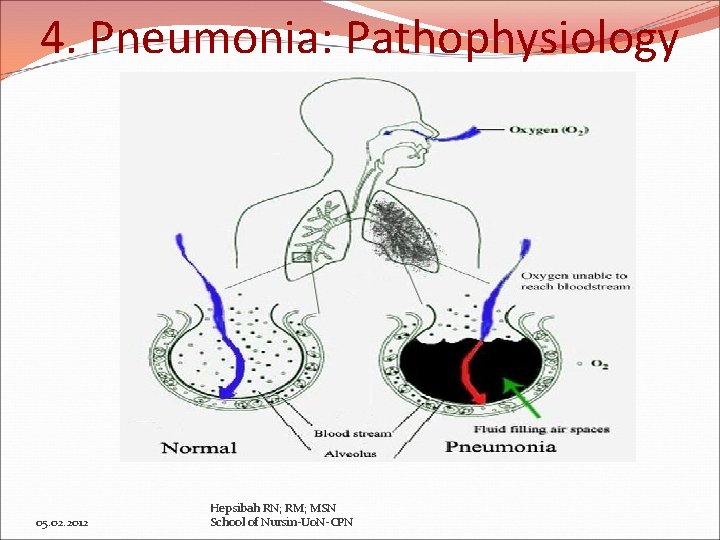
4. Pneumonia: Pathophysiology 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
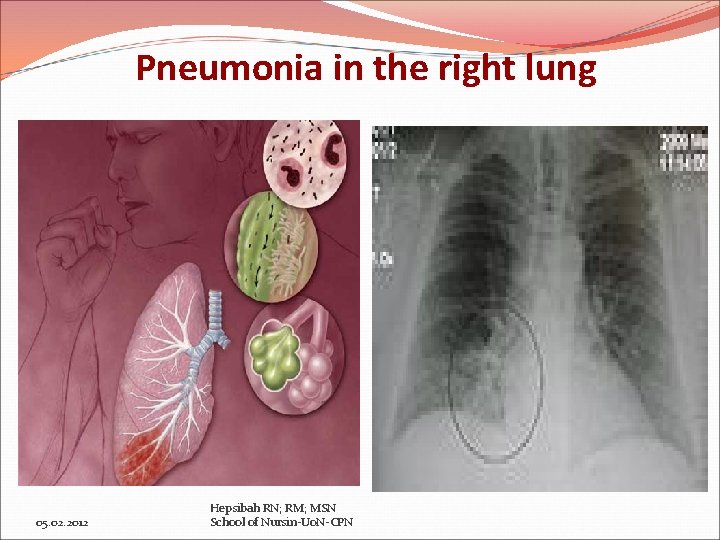
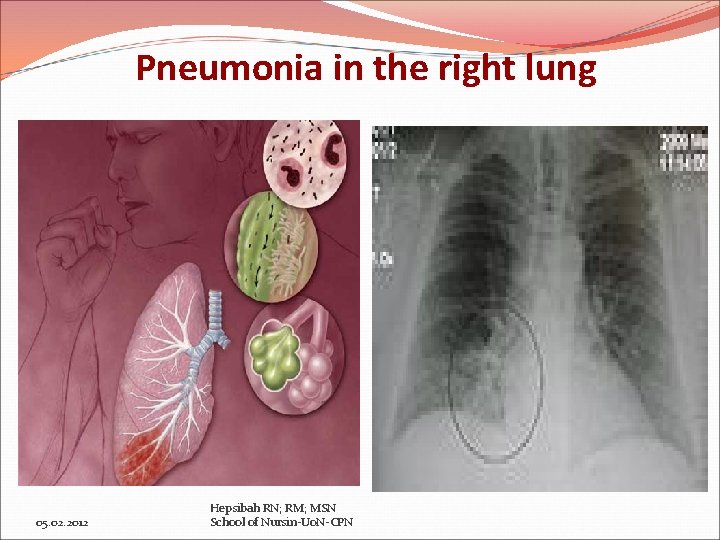
Pneumonia in the right lung 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Risk factors for Pneumonia Conditions producing mucus or bronchial obstruction ( Cancer, cigarette smoking, COPD) Immunosupressed patients with neutropenia, prolonged immobility Depressed cough reflex, NPO status Prolonged supine positioning, antibiotic therapy, alcohol intoxication, general anesthetics, sedatives or opiod preparations Advanced age, improperly cleaned respiratory equipments. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Clinical Manifestations for Pneumonia Signs & Symptoms (s/s) vary depending on the causal organism & underlying disease condition A patient with streptococcal (pneumococcal) pneumonia has sudden onset of chills, fever (38. 5 – 40. 5 0 C; pleuritic chest pain aggravated by deep breathing & coughing; may have tachypnea (25 -45 breaths/mt) with respiratory distress (SOB, use of accessory muscles); rapid & bounding pulse A relative bradycardia with fever viral; mycoplasma or legionella organism 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Clinical Manifestations for Pneumonia Some may exhibit URT infection (nasal congestion, sore throat): headache; low-grade fever; pleuritic chest pain, myalgia, rash & pharyngitis, later mucopurulent sputum & in severe pneumonia cheeks flush, lips & nail beds have central cyanosis (hypoxemia) Patient may exhibit orthopnea (SOB when reclining) preferring to be propped up or sitting in bed leaning forward (orthopneic position), poor appetite & diaphoretic & tires easily, purulent sputum. Rusty, blood tinged sputum with streptococcal (pneumococcal), staphylococcal & klebsiella pneumonia. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Assessment & Diagnostic Findings for PTB History and Physical Examination Chest x-ray Gram’s stain of sputum Sputum culture and sensitivity test (transtracheal aspiration or bronchoscopy with aspiration if unable to obtain via cough or induced production of sputum • ABGs or pulse oximetry • Complete blood count • Blood cultures • • 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Medical Management for Pneumonia � Prompt administration of antibiotics in whom CAP is strongly suspected or confirmed is a key treatment measure. Examples: Patients with no cardiopulmonary(CP) disease azithromycin (Zithromax); or clarithromycin (Biaxin); doxycycline (Vibramycin) or fluoroquinolone (Gatifloxacin), levofloxacin (Levaquin) for S. pneumoniae If CP disorder exists: beta-lactam agent cefpodoxime; cefuroxime; high dose amoxycillin or amoxycillin/clavulanate + a macrolide or doxycycline 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Medical Management for Pneumonia A patient with HAP is usually initiated with a broadspectrum IV antibiotic or monotherapy/combination therapy If pseudomonas infection: second generation cephalosporins (cefuroxime, cefamandole) or third generation cephalosporins (ceftriaxone, cefotaxime, ampicillin sulbacctam, fluoroquinolones (ciprofloxacin; levofloxacin) or carbapenem (meropenam) High risk for pseudomonas: Penicillin + aminoglycoside (amikacin; gentamycin) or betalactamase inhibitor (ampicillin/ sulbactam or ticarcillin/clavulanate) 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Medical Management for Pneumonia � Patients with MRSA infection, vancomycin or linezolid is used � Patients with atypical pneumonia (legionella, M. pneumnoniae) are usually treated for 10 -21 days) Other Therapeutic Regimens: Antibiotics are not ineffective in viral upper respiratory & pneumonia except for secondary bacterial pneumonia, bronchitis or sinusitis For viral pneumonia, treatment is primarily supportive (hydration; antipyretics; antitussive; warm, moist inhalation; antihistamines; , nasal decongestants, bed rest) Hepsibah RN; RM; MSN 05. 02. 2012 School of Nursin-Uo. N-CPN
Medical Management for Pneumonia Other Therapeutic Regimens… If hypoxemia develops, oxygen is administered. Perform ABG & pulse oximeter. ABG: Measures patient’s oxygenation & acid-base status Pulse oximetry: Monitors oxygen saturation A high concentration of oxygen is contra indicated in patients with COPD as it ↓ ventilatory drive respiratory decompensation More aggressive therapy include high concent-rations of oxygen (fraction of inspired oxygen-FIO 2); endotracheal(ET) tube & mechanical ventilation Complications: Shock & respiratory failure; atelectasis & pleural effusion. Hepsibah & superinfection. RN; RM; MSN 05. 02. 2012 School of Nursin-Uo. N-CPN
Nursing Interventions for Pneumonia 1. Ineffective airway clearance related to copious tracheobronchial secretions Improving airway patency: Remove secretions by hydration (2 -3 lts/day) as it thins & loosens secretions Humidification loosen secretions & improve ventilation. High-humidity face mask delivers warm, humidified air which liquefy secretions & relieves tracheobronchial irritation. Encourage coughing, deep breathing with an incentive spirometer. Chest physiotherapy (percussion & postural drainage) loosens & mobilizes secretions. If unable to cough perform suctioning. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Nursing Interventions for Pneumonia 2. Activity Intolerance related to impaired respiratory function Promoting rest and conserving energy: Take rest and avoid overexertion & exacerbation of symptoms Assume comfortable position (semi-Fowler’s) Change position frequently to enhance secretion clearance, ventilation & perfusion in the lungs. Engage only in moderate activity during initial phases of treatment. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Nursing Interventions for Pneumonia 3. Risk for deficient fluid volume related to fever and rapid respiratory rate Promoting fluid intake: Labored breathing & fever increase in insensible fluid loss during exhalation dehydration Encourage increased fluid intake (atleast 2 lts/day), unless contraindicated 4. Imbalanced nutrition less than body requirements Maintaining Nutrition: SOB & fatigue ↓ appetite & consume only fluids. Encourage fluids with electrolytes (gatorade) provide fluid, calories & electrolytes Nutritionally enriched drinks or shakes may help Hepsibah RN; RM; MSN 05. 02. 2012 Administer IV fluids and nutrients School of Nursin-Uo. N-CPN
Nursing Interventions for Pneumonia 5. Deficient knowledge about the treatment regimen and preventive health measure Promoting patients’ knowledge: Instruct about the cause, management of symptoms of pneumonia & report to physician & do follow-up care Give written instructions & information about proper administration of oral antibiotics & potential side-effects. Gradually increase activities once fever subsides Encourage breathing exercises to promote secretion clearance and volume expansion 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Nursing Interventions for Pneumonia Instruct on follow-up chest x-ray & physical examination Encourage to stop smoking as it inhibits tracheobronchial ciliary action, irritates the mucous cells of bronchi & inhibits function of alveo-lar macrophage (scavenger) cells. Avoid stress, fatigue, temperature changes & excess alcohol intake 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
End of Pneumonia! 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
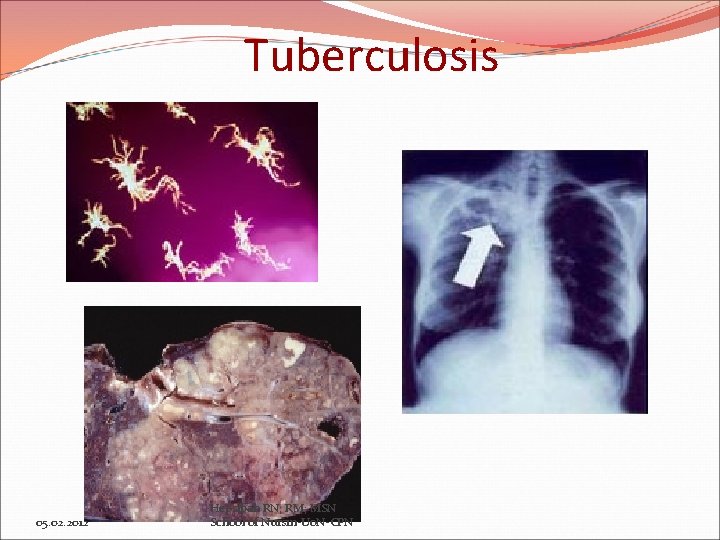
5. Pulmonary Tuberculosis (PTB) Description: Tuberculosis (TB) is an infectious disease that primarily affects the lung parenchyma. It also may be transmitted to other parts of the body, including meninges, kidneys, bones and lymph nodes. Primary infectious agent, Mycobacterium tuberculosis, is a gram positive, an acid-fast bacilli (AFB) TB is a worldwide public health problem and mortality and morbidity rates continue to rise 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
5. Pulmonary Tuberculosis (PTB) The WHO estimates that TB is the cause of death for 11% of all patients with AIDS TB is closely associated with poverty, malnutrition, overcrowding, substandard housing and inadequate health care Transmission and Risk factors: TB spreads from person to person by airborne transmission. An infected person releases droplet nuclei through talking, coughing, sneezing, laughing or singing 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Risk Factors for PTB �Close contact with a person who has active TB �Immunocompromised status �Substance abuse �Any person without adequate health care �Preexisting medical conditions (diabetes, CRF, malnourishment…) �Immigration from countries with a high prevalence of TB �Institutionalization, Living in overcrowded, substandard housing �Being a health care worker performing high -risk activities 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Pathophysiology of PTB Inhalation of mycobacterium bacteria enters through the airway to the alveoli, gets deposited & multiply ↓ Bacilli are transported to other parts like lymph system and blood stream, kidneys, bones, cerebral cortex. ↓ Initiates inflammatory reaction ↓ Phagocytes engulf many of the bacteria & TB specific lymphocytes lyse the bacilli and Hepsibah RN; RM; MSN 05. 02. 2012 School of Nursin-Uo. N-CPN normal tissue
↓ This tissue reaction results in the accumulation of exudate in the alveoli Bronchopneumonia ↓ New tissue masses of live & dead bacilli are surrounded by macrophages forms a protective wall (Granuloma’s) ↓ Center of fibrous tissue mass (Ghon tubercle) ↓ Material becomes necrotic a cheesy mass ↓ Calcified & a collagenous scar is formed & no Hepsibah RN; RM; MSN 05. 02. 2012 School ofprogression Nursin-Uo. N-CPN further of active disease
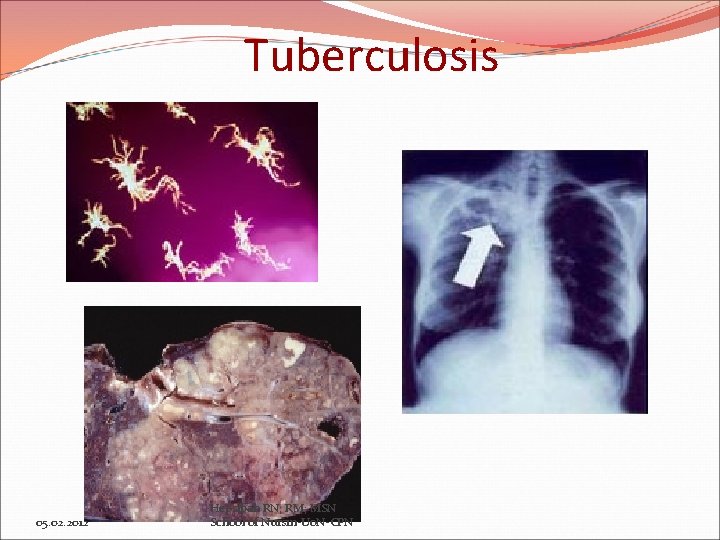
Tuberculosis 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
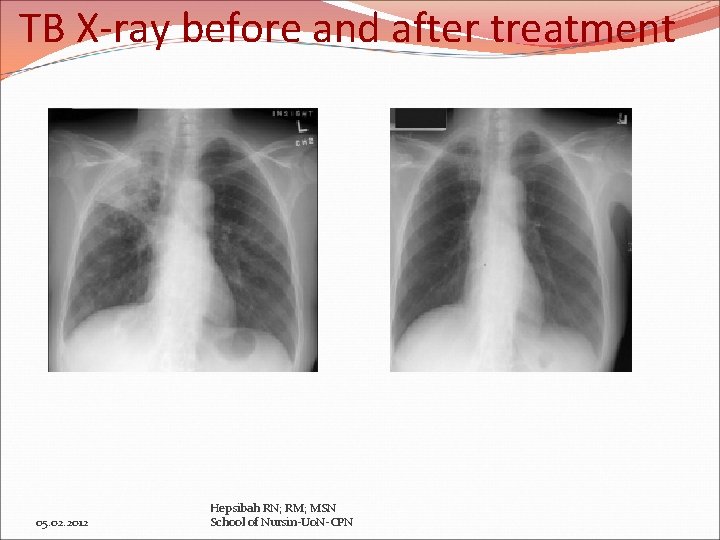
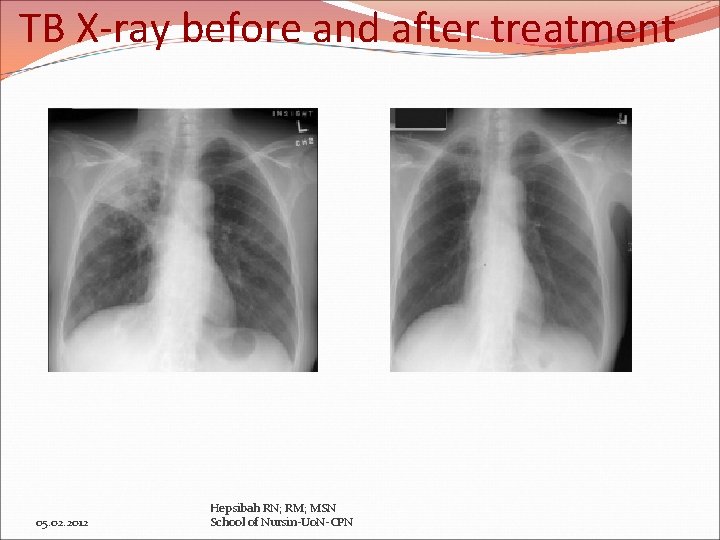
TB X-ray before and after treatment 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
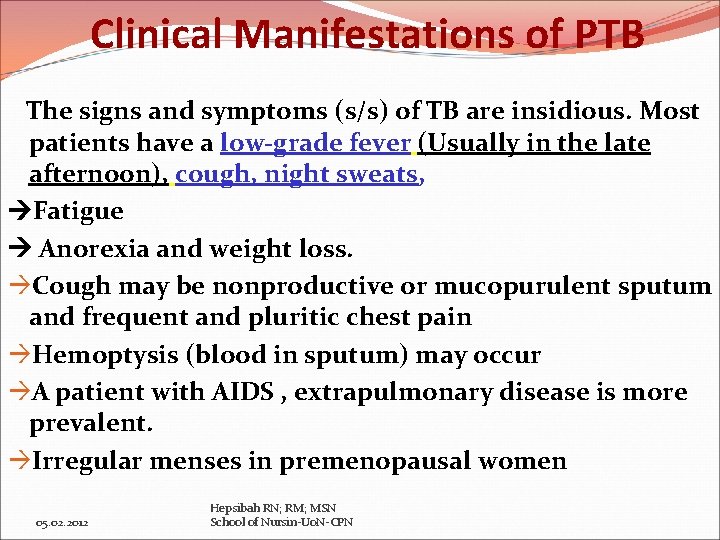
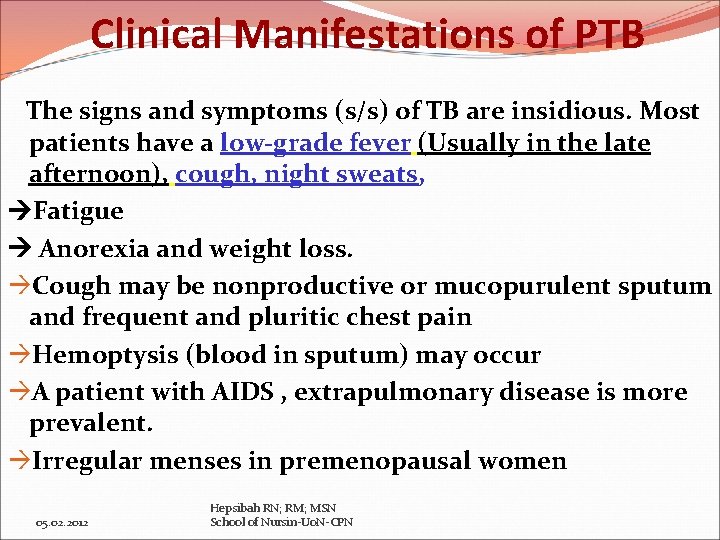
Clinical Manifestations of PTB The signs and symptoms (s/s) of TB are insidious. Most patients have a low-grade fever (Usually in the late afternoon), cough, night sweats, Fatigue Anorexia and weight loss. Cough may be nonproductive or mucopurulent sputum and frequent and pluritic chest pain Hemoptysis (blood in sputum) may occur A patient with AIDS , extrapulmonary disease is more prevalent. Irregular menses in premenopausal women 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
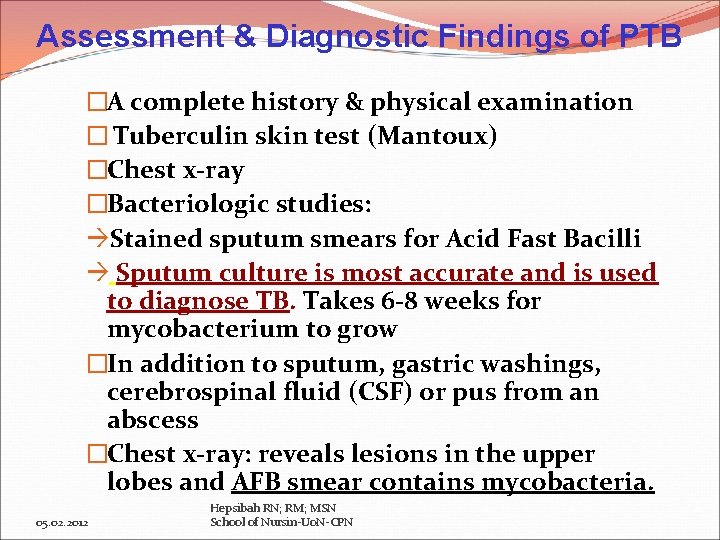
Assessment & Diagnostic Findings of PTB �A complete history & physical examination � Tuberculin skin test (Mantoux) �Chest x-ray �Bacteriologic studies: Stained sputum smears for Acid Fast Bacilli Sputum culture is most accurate and is used to diagnose TB. Takes 6 -8 weeks for mycobacterium to grow �In addition to sputum, gastric washings, cerebrospinal fluid (CSF) or pus from an abscess �Chest x-ray: reveals lesions in the upper lobes and AFB smear contains mycobacteria. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
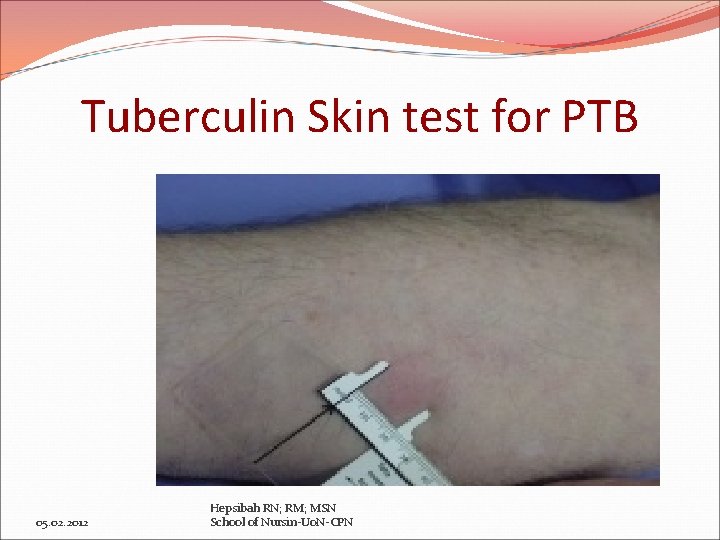
Assessment & Diagnostic Findings for PTB Tuberculin skin testing (TST): The Mantoux test is used to determine whether a person has been infected with the TB bacillus. Procedure? ? ? Tubercle bacilli extract (tuberculin), 0. 1 m. L purified protein derivative (PPD) is injected into the intradermal layer of the inner aspect of the forearm, 4 inches below the elbow creating a wheal or bleb. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
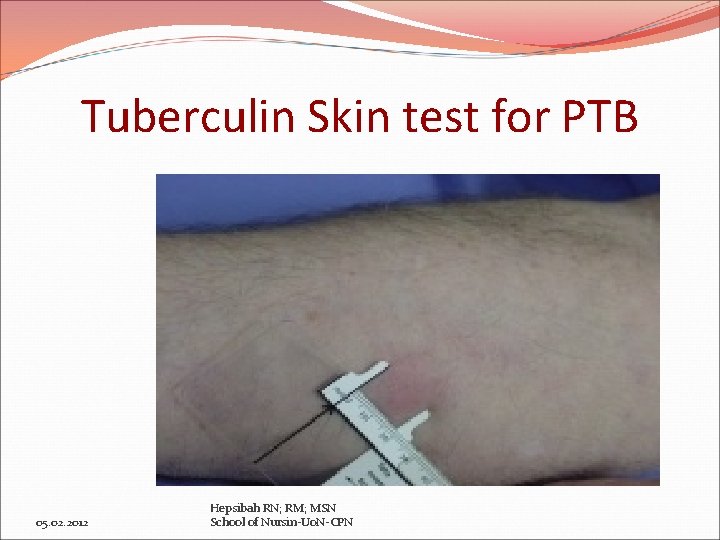
Tuberculin Skin test for PTB 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
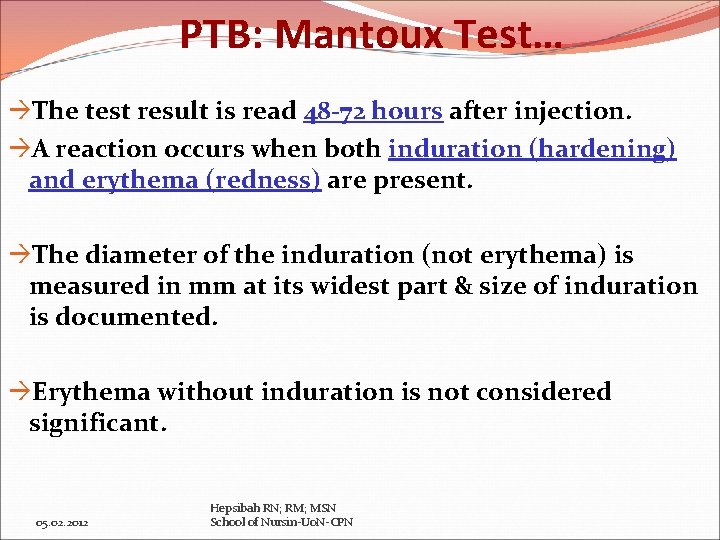
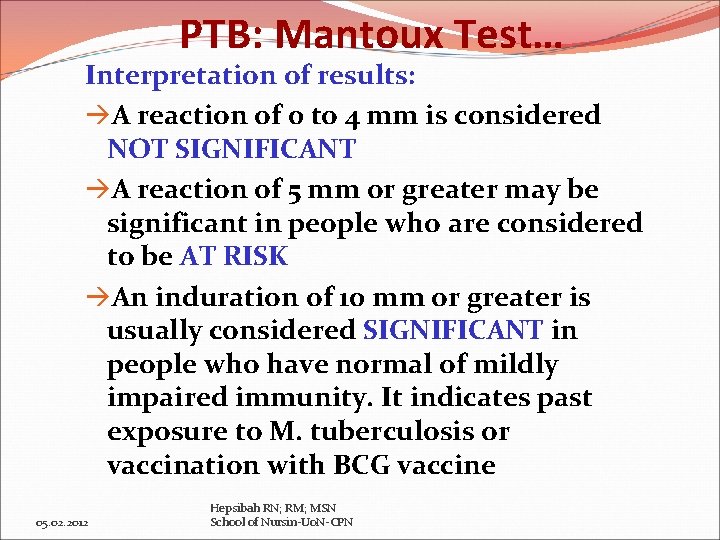
PTB: Mantoux Test… The test result is read 48 -72 hours after injection. A reaction occurs when both induration (hardening) and erythema (redness) are present. The diameter of the induration (not erythema) is measured in mm at its widest part & size of induration is documented. Erythema without induration is not considered significant. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
PTB: Mantoux Test… Interpretation of results: A reaction of 0 to 4 mm is considered NOT SIGNIFICANT A reaction of 5 mm or greater may be significant in people who are considered to be AT RISK An induration of 10 mm or greater is usually considered SIGNIFICANT in people who have normal of mildly impaired immunity. It indicates past exposure to M. tuberculosis or vaccination with BCG vaccine 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
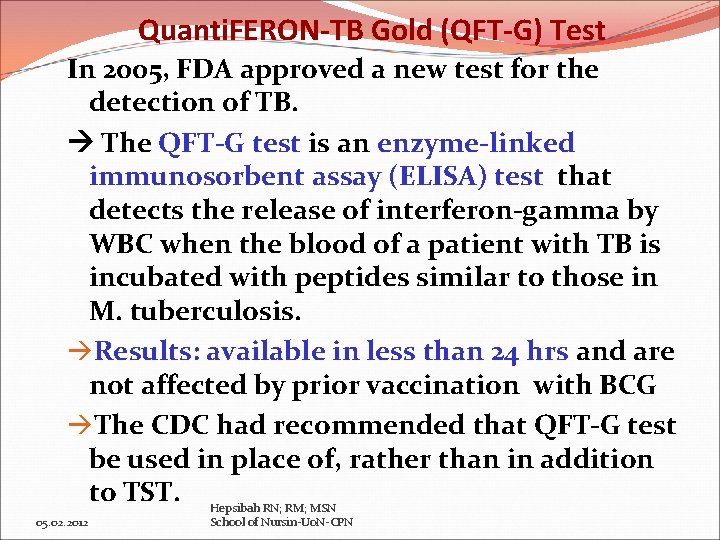
Quanti. FERON-TB Gold (QFT-G) Test In 2005, FDA approved a new test for the detection of TB. The QFT-G test is an enzyme-linked immunosorbent assay (ELISA) test that detects the release of interferon-gamma by WBC when the blood of a patient with TB is incubated with peptides similar to those in M. tuberculosis. Results: available in less than 24 hrs and are not affected by prior vaccination with BCG The CDC had recommended that QFT-G test be used in place of, rather than in addition to TST. Hepsibah RN; RM; MSN 05. 02. 2012 School of Nursin-Uo. N-CPN
Medical Management for PTB TB is primarily treated with chemo-therapeutic agents (Anti-tuberculosis treatment (ATT) for 6 to 12 months to ensure eradication and prevent relapse. Several types of drug resistance can occur 1. Primary drug resistance: Resistance to one of the first-line ATT in people who have not had previous treatment 2. Secondary/acquired drug resistance: Resistance to one or more ATT in patients undergoing therapy 3. Multidrug resistance: Resistance to 2 agents, isoniazid (INH) & rifampin. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Pharmacologic Therapy for PTB In current TB treatment First-line drugs: 5 drugs such as Isoniazid (INH), rifampin, pyrazinamide & ethambutol & Streptomycin. Combination of drugs such as INH & Rifampin; INH, Pyrazinamide & Rifampin or drugs given twice a week (eg: Rifapentine) is available to improve adherance. Second-line drugs: Capreomycin, ethionamide, para-aminosalicylate sodium & cycloserine 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Recommended treatment guidelines: Newly Diagnosed cases of TB I. Initial Phase: Multiple medication regimen – INH, rifampin, pyrazinamide & ethambutol. Administered daily for 8 weeks (2 months) followed by… II. Continuation Phase: INH & Rifampin or INH & Rifapentine. Lasts for an additional 4 to 7 months. Mostly 4 month period is used. * People are considered noninfectious after 2 -3 wks of continuous medication therapy. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Recommended treatment guidelines: 1. Isoniazid (INH) Vitamin-B (pyridoxine) is usually given with INH? ? ? To prevent INH-associated peripheral neuropathy INH prophylaxis (preventive) is given to people who are at risk for significant disease Monitor for liver enzymes (hepatotoxicity) , blood urea nitrogen & creatinine levels monthly Sputum culture results are monitored for AFB to evaluate the effectiveness of treatment & patients adherence 2. Rifampin: Side-effect: Hepatitis, febrile reaction, GI disturbance, peripheral neuropathy & hypersensitivity. Possible orange urine Hepsibah RN; RM; MSN 05. 02. 2012 School of Nursin-Uo. N-CPN
Nursing Management for PTB 1. Ineffective airway clearance related to copious tracheobronchial secretions Promoting airway clearance Copious secretions obstruct the airways in many patients with TB Increasing fluid intake promotes systemic hydration & serves as an effective expectoration Instruct about correct positioning to facilitate airway drainage (postural drainage) 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Nursing Management for PTB 2. Deficient knowledge about treatment regimen and preventive measure Advocating adherence to treatment regimen Instruct the patient that TB is a communicable disease and taking the medications is the most effective means of prevention transmission Main reason for the failure is that patients do not take their medications regularly for the prescribed duration Instruct about hygienic measures like mouth care, covering the mouth & nose while coughing or sneezing, proper disposal of tissues & hand washing. Follow up by positive reinforcement & monitor 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Nursing Management for PTB 3. Activity intolerance related to fatigue, altered nutritional status and fever Promoting activity and adequate nutrition Plan for a progressive activity schedule that focuses on increasing activity tolerance and muscle strength. Anorexia, weight loss and malnutrition are common in patients with TB Patients willingness to eat may be altered by fatigue from excessive coughing, sputum production, chest pain, debilitated state or cost. Plan for small, frequent meals. Liquid nutritional supplements may meet basic caloric requirements. 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Home and Community-based care (PTB) �Assess patients ability to continue therapy at home �Instruct about infection control procedures: proper disposal of tissues, covering the mouth during coughing and frequent hand washing. �Assess adherence to treatment failure to continue Emergence of resistance �If not taking the drug daily refer to out patient clinic for daily medication administration – referred to as directly observed therapy (DOT) 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
References 1. Smeltzer, S. C. et al. (2008). Brunner and Suddarth’s textbook of medical-surgical nursing. 11 th Ed. Philadelphia, Lippincott. 1. Lewis, S. M. et al. (2000). Medical Surgical Nursing: Assessment and Management of Clinical Problems (5 th Ed. ). St. Louis, Mosby 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
Any Questions? 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
End of Tuberculosis 05. 02. 2012 Hepsibah RN; RM; MSN School of Nursin-Uo. N-CPN
 Ocd nursing care plan pdf
Ocd nursing care plan pdf Postoperative nursing management of cataract
Postoperative nursing management of cataract Levels of care primary secondary tertiary quaternary
Levels of care primary secondary tertiary quaternary Bsc hons adult nursing
Bsc hons adult nursing Bsc hons adult nursing
Bsc hons adult nursing Bsc hons adult nursing
Bsc hons adult nursing Adult care sheffield
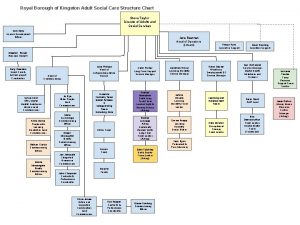
Adult care sheffield Adult social care kingston
Adult social care kingston Broad topic and narrow topic examples
Broad topic and narrow topic examples Tapic about internet
Tapic about internet Todays public relations departments
Todays public relations departments Cold calling script
Cold calling script Déontologie
Déontologie étude de flux
étude de flux Typologie des clients insatisfaits
Typologie des clients insatisfaits Ibm thin clients
Ibm thin clients How to schedule appointments with clients
How to schedule appointments with clients Trauma-informed questions for clients
Trauma-informed questions for clients Open ended questions social work
Open ended questions social work Nudge for clients
Nudge for clients Circles of my multicultural self
Circles of my multicultural self Characteristics of profession
Characteristics of profession Sabre helps its clients through dashboards and analytics
Sabre helps its clients through dashboards and analytics Adlerians view the use of techniques in counseling as
Adlerians view the use of techniques in counseling as Counseling multicultural clients
Counseling multicultural clients Using bird dogs when prospecting for clients refers to
Using bird dogs when prospecting for clients refers to What are two basic requirements for a healthy scalp
What are two basic requirements for a healthy scalp Client needs assessment
Client needs assessment Gnutella clients
Gnutella clients Nachteile thin clients
Nachteile thin clients Web essentials clients servers and communication
Web essentials clients servers and communication Chapter 4 communicating for success
Chapter 4 communicating for success Idt therapy
Idt therapy Ece 450
Ece 450 Ucm service en ligne
Ucm service en ligne Modular nursing method
Modular nursing method Nursing process introduction
Nursing process introduction Nursing process in psychiatric nursing
Nursing process in psychiatric nursing Nursing process steps
Nursing process steps Modular nursing definition
Modular nursing definition Associative looseness
Associative looseness Nursing position definition
Nursing position definition Perioperative definition
Perioperative definition Preoperative checklist definition
Preoperative checklist definition Nursing care of hospitalized child
Nursing care of hospitalized child Post operative nursing care
Post operative nursing care Nail care procedure in nursing
Nail care procedure in nursing Nursing diagnosis for gingivitis
Nursing diagnosis for gingivitis