Adrenal hormones The adrenal gland consists of the


- Slides: 28
Adrenal hormones

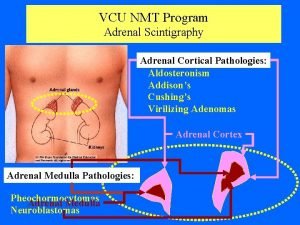
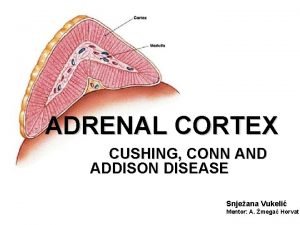
• The adrenal gland consists of the cortex and the medulla. • The medulla secretes catecholamines. • the cortex secretes two types of corticosteroids (glucocorticoids and mineralocorticoids|) and the adrenal androgens. • The adrenal cortex has three zones, and each zone synthesizes a different type of steroid hormone from cholesterol.
• The outer zona glomerulosa produces mineralocorticoids (aldosterone) that are responsible for regulating salt and water metabolism. • Production of aldosterone is regulated primarily by the renin–angiotensin system. • The middle zona fasciculata synthesizes glucocorticoids (cortisol) that are involved with metabolism and response to stress. • The inner zona reticularis secretes adrenal androgens.
A. Glucocorticoids • Cortisol is the principal human glucocorticoid. • its production is diurnal, with a peak early in the morning followed by a decline and then a secondary, smaller peak in the late afternoon. • Factors such as stress and levels of the circulating steroid influence secretion.
The effects of cortisol 1. Promote normal intermediary metabolism: • Glucocorticoids favor gluconeogenesis through increasing amino acid uptake by the liver and kidney and elevating activities of gluconeogenic enzymes. • They stimulate protein catabolism (except in the liver) and lipolysis, thereby providing the building blocks and energy that are needed for glucose synthesis. • [Note: Glucocorticoid insufficiency may result in hypoglycemia (for example, during stressful periods or fasting). ]
2. Increase resistance to stress: • By raising plasma glucose levels, glucocorticoids provide the body with energy to combat stress caused by trauma, fright, infection, bleeding, or debilitating disease. 3. Alter blood cell levels in plasma: • Glucocorticoids cause a decrease in eosinophils, basophils, monocytes, and lymphocytes by redistributing them from the circulation to lymphoid tissue. • Glucocorticoids also increase hemoglobin, erythrocytes, platelets, and polymorphonuclear leukocytes.
4. Have anti-inflammatory action: • The most important therapeutic properties of the glucocorticoids are their potent anti-inflammatory and immunosuppressive activities. • These therapeutic effects of glucocorticoids are the result of a number of actions. 1. The lowering of circulating lymphocytes. 2. these agents inhibit the ability of leukocytes and macrophages to respond to mitogens and antigens. 3. Glucocorticoids also decrease the production and release of proinflammatory cytokines.
1. They inhibit phospholipase A 2, which blocks the release of arachidonic acid (the precursor of the prostaglandins and leukotrienes) from membrane-bound phospholipid. The decreased production of prostaglandins and leukotrienes is believed to be central to the antiinflammatory action. 2. these agents influence the inflammatory response by stabilizing mast cell and basophil membranes, resulting in decreased histamine release.
5. Affect other systems: • glucocorticoids serve as feedback inhibitors of ACTH production and affect the endocrine system by suppressing further synthesis of glucocorticoids and thyroid-stimulating hormone. • adequate cortisol levels are essential for normal glomerular filtration. • The effects of corticosteroids on other systems are mostly associated with adverse effects of the hormones.
B. Mineralocorticoids • Mineralocorticoids help to control fluid status and concentration of electrolytes, especially sodium and potassium. • Aldosterone acts on distal tubules and collecting ducts in the kidney, causing reabsorption of sodium, bicarbonate, and water. • aldosterone decreases reabsorption of potassium, which, with H+, is then lost in the urine. Enhancement of sodium reabsorption by aldosterone also occurs in gastrointestinal mucosa and in sweat and salivary glands.
C. Therapeutic uses of the corticosteroids • Several semisynthetic derivatives of corticosteroids are available. These agents vary in anti-inflammatory potency, mineralocorticoid activity, and duration of action. • Shortto medium-acting glucocorticoids : Hydrocortisone (cortisol), Cortisone, Prednisolone, Methylprednisolone. • Intermediate-acting glucocorticoids: Triamcinolone. • Long-acting glucocorticoids: Betamethasone, Dexamethasone.
1. Replacement therapy for primary adrenocortical insufficiency (Addison disease): Addison disease is caused by adrenal cortex dysfunction. Hydrocortisone is given to correct the deficiency. 2. Replacement therapy for secondary or tertiary adrenocortical insufficiency: These disorders are caused by a defect in CRH production by the hypothalamus or in ACTH production by the pituitary. Hydrocortisone is used for treatment of these deficiencies.
5. Relief of inflammatory symptoms: • Corticosteroids significantly reduce the manifestations of inflammation associated with: • rheumatoid arthritis and inflammatory skin conditions, including redness, swelling, heat, and tenderness. • symptom control in persistent asthma, as well as management of asthma exacerbations and active inflammatory bowel disease. • In osteoarthritis, intra-articular corticosteroids may be used for treatment of a disease flare. Corticosteroids are not curative in these disorders. • In Infections as acute respiratory distress syndrome, sepsis.
6. Treatment of allergies: Corticosteroids are beneficial in the treatment of: • allergic rhinitis, as well as drug, serum, and transfusion allergic reactions. • other Allergic reactions: asthma, bee stings, contact dermatitis, urticaria. • in organ transplants for prevention and treatment of rejection (immunosuppression).
Pharmacokinetics 1. Absorption and fate: • Orally administered corticosteroid are readily absorbed. • can also be administered intravenously, intramuscularly, intra-articularly (into arthritic joints), topically, or via inhalation or intranasal delivery. • All topical and inhaled glucocorticoids are absorbed to some extent and, therefore, have the potential to cause hypothalamic–pituitary–adrenal (HPA) axis suppression.
• Greater than 90% of absorbed glucocorticoids are bound to plasma proteins (CBG). • Corticosteroids are metabolized by the liver microsomal oxidizing enzymes. • Prednisone is preferred in pregnancy because it minimizes steroid effects on the fetus. • It is a prodrug that is not converted to the active compound, prednisolone, in the fetal liver. Any prednisolone formed in the mother is biotransformed to prednisone by placental enzymes.
2. Dosage: • Many factors: • including glucocorticoid versus mineralocorticoid activity, duration of action, type of preparation, and time of day when the drug is administered. • When large doses of the hormone are required for more than 2 weeks, suppression of the HPA axis occurs. • Alternate-day administration of the corticosteroid may prevent this adverse effect by allowing the HPA axis to recover/function on days the hormone is not taken.
E. Adverse effects • These are extension of the pharmacological action that become prominent with prolonged therapy, and are a great limitation to the use of corticoids in chronic diseases. • Cushing-like syndrome (redistribution of body fat (obesity of trunk with relatively thin limbs), puffy face, hirsutism, and increased appetite[Note: Increased appetite is not necessarily an adverse effect. In fact, it is one of the reasons for the use of prednisone in cancer chemotherapy. ] • Fragile skin, purple striae—easy bruising, telengiectasis, hirsutism. Cutaneous atrophy occurs with topical use also.
• Hyperglycaemia, precipitation of diabetes. • Muscular weakness; myopathy occurs occasionally. • Susceptibility to infection; opportunistic infections with low-grade pathogens (Candida, etc. ). • Delayed healing of wounds. • Peptic ulceration. • Osteoporosis is the most common adverse effect due to the ability of glucocorticoids to suppress intestinal Ca 2+ absorption, inhibit bone formation, and decrease sex hormone synthesis. Patients are advised to take calcium and vitamin D supplements.
• Growth retardation: in children occurs even with small doses if given for long periods. • Fetal abnormalities: cleft palate and other defects are produced in animals, but have not been encountered in pregnant women. • Psychiatric disturbances.
F. Discontinuation • Sudden discontinuation of these drugs can be a serious problem if the patient has suppression of the HPA axis. In this case, abrupt removal of corticosteroids causes acute adrenal insufficiency that can be fatal. • This risk, coupled with the possibility that withdrawal might cause an exacerbation of the disease, means that the dose must be tapered slowly according to individual tolerance.
• Suppression of hypothalamo-pituitaryadrenal (HPA) axis: occurs depending both on dose and duration of therapy. • In time, adrenal cortex atrophies and stoppage of exogenous steroid precipitates a withdrawal syndrome and reactivation of the disease. Subjected to stress, these patients may go into acute adrenal insufficiency.
B. Contraindications • Glucocorticoids must be used with great caution in patients with peptic ulcer, heart disease or hypertension with heart failure, certain infectious illnesses such as varicella and tuberculosis, psychoses, diabetes, osteoporosis. •

Individual adrenal steroids • Glucocorticoid preparations differ with respect to relative anti-inflammatory and mineralocorticoid effect, duration of action, cost, and dosage forms available and these factors should be taken into account in selecting the drug to be used. • 1. Hydrocortisone (cortisol) In addition to primary glucocorticoid, it has significant mineralocorticoid activity with rapid and short lasting action. can be given intravenously for rapid effect in emergency whether due to deficiency, allergy or inflammatory disease.
2. Prednisolone It is 4 times more potent than hydrocortisone; also more selective glucocorticoid, but fluid retention does occur with high doses. Has intermediate duration of action: • causes less pituitary-adrenal suppression when a single morning dose or alternate day treatment is given. It is used for allergic, inflammatory, autoimmune diseases and in malignancies.
3. Methylprednisolone Slightly more potent and more selective than prednisolone. Pulse therapy with high dose methylprednisolone (1 g infused i. v. every 6 – 8 weeks) has been tried in nonresponsive active rheumatoid • arthritis, renal transplant, etc.
4. Triamcinolone Slightly more potent than prednisolone but highly selective glucocorticoid. 5. Dexamethasone Very potent and highly selective glucocorticoid. Long acting, causes marked pituitaryadrenal suppression, but fluid retention and hypertension are not a problem. It is used for inflammatory and allergic conditions, shock, cerebral edema, etc.
6. Betamethasone Similar to dexamethasone. Dexamethasone or betamethasone are preferred in cerebral edema and other states in which fluid retention must be avoided.
 Adrenal gland hormones
Adrenal gland hormones Adrenal gland epithelium
Adrenal gland epithelium Ectocrine
Ectocrine Betoderm
Betoderm Nerve ganglia
Nerve ganglia Coelomic epithelium
Coelomic epithelium Adrenal gland hormone
Adrenal gland hormone Adrenal gland regions
Adrenal gland regions Relation of suprarenal gland
Relation of suprarenal gland Adrenal gland regions
Adrenal gland regions Adrenal gland
Adrenal gland Summary of adrenal gland
Summary of adrenal gland Left ureter
Left ureter Pituitary gland hormones
Pituitary gland hormones Pineal gland pituitary gland
Pineal gland pituitary gland Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual A multicellular exocrine gland consists of ______.
A multicellular exocrine gland consists of ______. Adrenal glands
Adrenal glands Adrenal cushing
Adrenal cushing Medulla
Medulla Adrenal hormone pathway
Adrenal hormone pathway All systems of the body
All systems of the body Mineralocorticoid function
Mineralocorticoid function Adrenal cortex develops from
Adrenal cortex develops from Thyroid
Thyroid Estadiamento de tanner
Estadiamento de tanner Adrenal bezin hipofonksiyonu sonucu gelişen tablo
Adrenal bezin hipofonksiyonu sonucu gelişen tablo Addison's vs conn's
Addison's vs conn's Congenital adrenal hyperplasia genitalia
Congenital adrenal hyperplasia genitalia