Acute Postoperative Pain A revolution in the management


![Chronic Effects • Chronic postsurgical pain [CPSP] is a largely unrecognized problem that may Chronic Effects • Chronic postsurgical pain [CPSP] is a largely unrecognized problem that may](https://slidetodoc.com/presentation_image/ead3b04776ed4c499b26b489f66b6195/image-7.jpg)















- Slides: 33


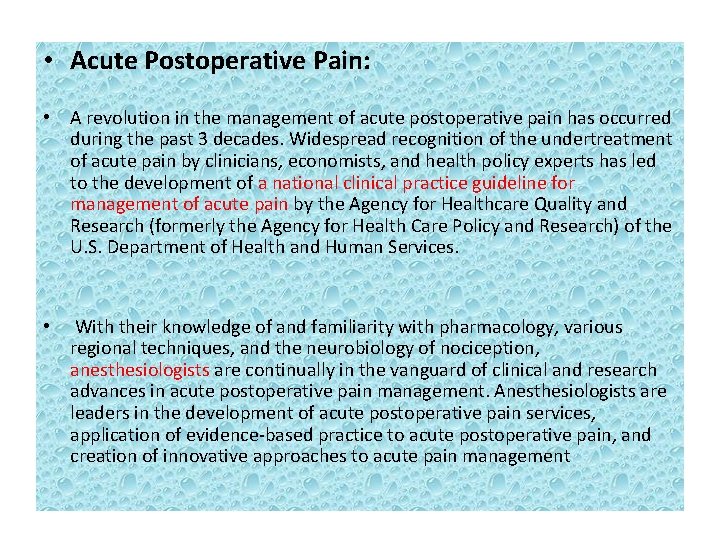
• Acute Postoperative Pain: • A revolution in the management of acute postoperative pain has occurred during the past 3 decades. Widespread recognition of the undertreatment of acute pain by clinicians, economists, and health policy experts has led to the development of a national clinical practice guideline for management of acute pain by the Agency for Healthcare Quality and Research (formerly the Agency for Health Care Policy and Research) of the U. S. Department of Health and Human Services. • With their knowledge of and familiarity with pharmacology, various regional techniques, and the neurobiology of nociception, anesthesiologists are continually in the vanguard of clinical and research advances in acute postoperative pain management. Anesthesiologists are leaders in the development of acute postoperative pain services, application of evidence-based practice to acute postoperative pain, and creation of innovative approaches to acute pain management
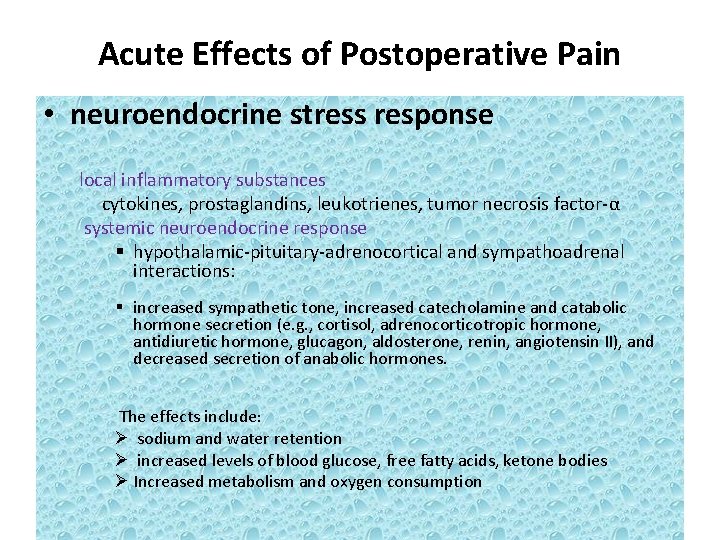
Acute Effects of Postoperative Pain • neuroendocrine stress response local inflammatory substances cytokines, prostaglandins, leukotrienes, tumor necrosis factor-α systemic neuroendocrine response § hypothalamic-pituitary-adrenocortical and sympathoadrenal interactions: § increased sympathetic tone, increased catecholamine and catabolic hormone secretion (e. g. , cortisol, adrenocorticotropic hormone, antidiuretic hormone, glucagon, aldosterone, renin, angiotensin II), and decreased secretion of anabolic hormones. The effects include: Ø sodium and water retention Ø increased levels of blood glucose, free fatty acids, ketone bodies Ø Increased metabolism and oxygen consumption
• The stress response may be an important factor in the postoperative development of hypercoagulability. • The stress response may also potentiate postoperative immunosuppression. – Hyperglycemia from the stress response may contribute to poor wound healing and depression of immune function. • increase myocardial oxygen consumption • delay return of postoperative gastrointestinal motility – Although postoperative ileus is the result of a combination of inhibitory input from central and local factors, such as from uncontrolled pain
• Postoperative respiratory function is markedly decreased, especially after upper abdominal and thoracic surgery. – Spinal reflex inhibition of phrenic nerve activity is an important component of this decreased postoperative pulmonary function. – However, control of postoperative pain is also important because patients with poor pain control may breathe less deeply, have an inadequate cough, and be more susceptible to the development of postoperative pulmonary complications
![Chronic Effects Chronic postsurgical pain CPSP is a largely unrecognized problem that may Chronic Effects • Chronic postsurgical pain [CPSP] is a largely unrecognized problem that may](https://slidetodoc.com/presentation_image/ead3b04776ed4c499b26b489f66b6195/image-7.jpg)
Chronic Effects • Chronic postsurgical pain [CPSP] is a largely unrecognized problem that may occur in 10% to 65% of postoperative patients (depending on the type of surgery). • Control of acute postoperative pain may improve long-term recovery or patient-reported outcomes (e. g. , quality of life). – Patients whose pain is controlled in the early postoperative period (especially with the use of continuous epidural or peripheral catheter techniques) may be able to actively participate in postoperative rehabilitation, which may improve short- and long-term recovery after surgery.
Treatment Methods Many options are available for the treatment of postoperative pain, including systemic (i. e. , opioid and nonopioid) analgesics and regional (i. e. , neuraxial and peripheral) analgesic techniques. Opioids : • These agents generally exert their analgesic effects through μ-receptors in the CNS, although there is evidence that opioids may also act at peripheral opioid receptors. • opioids are administered parenterally (intravenously or intramuscularly), intravenous patient-controlled analgesia (PCA) optimizes delivery of analgesic opioids and minimizes the effects of pharmacokinetic and pharmacodynamic variability in individual patients. • side effects : nausea, vomiting, respiratory depression and sedation
• Nonsteroidal Anti-inflammatory Agents: – The primary mechanism by which NSAIDs exert their analgesic effect is through inhibition of cyclooxygenase (COX) and synthesis of prostaglandins, which are important mediators of peripheral sensitization and hyperalgesia. – side effects: including decreased hemostasis, renal dysfunction, gastrointestinal hemorrhage, and deleterious effects on bone healing and osteogenesis. • Ketamine • tramadol
Regional Analgesic Techniques • In general, the analgesia provided by epidural and peripheral techniques (particularly when local anesthetics are used) is superior to that with systemic opioids, and use of these techniques may even reduce morbidity and mortality. • However, there are risks associated with the use of such techniques, and the clinician should evaluate the risks and benefits of these techniques on an individual basis in determining the appropriateness of neuraxial or peripheral regional techniques for each patient, especially in light of some of the controversies about the use of these techniques in the presence of various anticoagulants
• Administration of a single dose of opioid administered intrathecally or epidurally. • Epidural infusion of local anesthetic alone may be used for postoperative analgesia – but in general it is not as effective in controlling pain as local anesthetic–opioid epidural analgesic combinations are. • Side Effects of Neuraxial Analgesic Drugs: – HYPOTENSION. MOTOR BLOCK. NAUSEA AND VOMITING. PRURITUS. RESPIRATORY DEPRESSION. URINARY RETENTION.
Intercostal block: • Patient Selection: – Chest trauma such as rib fractures – Post surgical pain after Chest and upper abdominal surgery • The intercostalblock can also be used when chest tubes (thoracostomy tubes) are placed or when feeding gastrostomy tubes are inserted • Pharmacologic Choice: – If sensory analgesia is all that is necessary from the block, 0. 25% bupivacaine, 0. 2% ropivacaine, 1% lidocaine, or 1% mepivacaine is appropriate. • Position: – the patient ideally is placed in the prone position, its preferred location just lateral to the paraspinous muscles at the angle of the ribs. A pillow is placed under the patient's mid-abdomen to reduce lumbar lordosis and to accentuate the intercostal space sposteriorly. The arms are allowed to hang down from the edge of the block table to permit the scapula to rotate as far laterally as possible.

• Technique of Intercostal Block: – A line is drawn along the posterior vertebral spines. Nearly parallel lines are drawn along the posterior angles of the rib, which can be palpated 6 to 8 cm from the midline. These lines angle medially at the upper levels to prevent overlying of the scapula. – The inferior edge of each rib is palpated and marked on a line intersecting the posterior angle of the rib. After appropriate skin preparation, skin wheals are raised at each of these points. – A 22 -gauge, short-beveled 4 -cm needle is attached to a 10 -m. L syringe. Beginning at the lowest rib, the index finger of the left hand displaces the skin up over the patient's rib. The needle is inserted at the tip of the finger until it rests on the rib. The fingers of the left hand are shifted to grasp the needle hub firmly. The left hand then walks the needle 3 to 5 mm off the lower rib edge, where 3 to 5 m. L of local anesthetic is injected. – This process is repeated at each rib.

Side Effects and Complications • The major complication feared with intercostal blockade is pneumothorax. The actual incidence, however, was as low as 0. 07% in a large series performed by anesthesiologists at all levels of training. Routine postoperative chest radiographs showed a 0. 42% incidence of nonsymptomatic pneumothorax. If this unusual complication occurs, treatment is usually limited to observation, administration of oxygen, or needle aspiration. Rarely, chest tube drainage is required when these treatments are unsuccessful. • A risk of systemic local anesthetic toxicity is present with multiple intercostal blocks because of the large volumes and rapid absorption of the solutions. Use of epinephrine has been shown to decrease blood levels. Patients should be monitored and observed carefully during the block and for at least 20 to 30 minutes afterward.
Interpleural block • Patient Selection: – Patients undergoing upper abdominal or flank surgery or those recovering from fractured ribs have been the patients most frequently selected for interpleural anesthesia. – Also has used for chronic pain(metastasis, etc) • Pharmacologic Choice: – Most commonly, 20 to 30 m. L of local anesthetic solution is injected via an interpleural needle or catheter. – The most common local anesthetic concentrations used have been 0. 25% to 0. 5% bupivacaine and 0. 2% to 0. 5% ropivacaine.
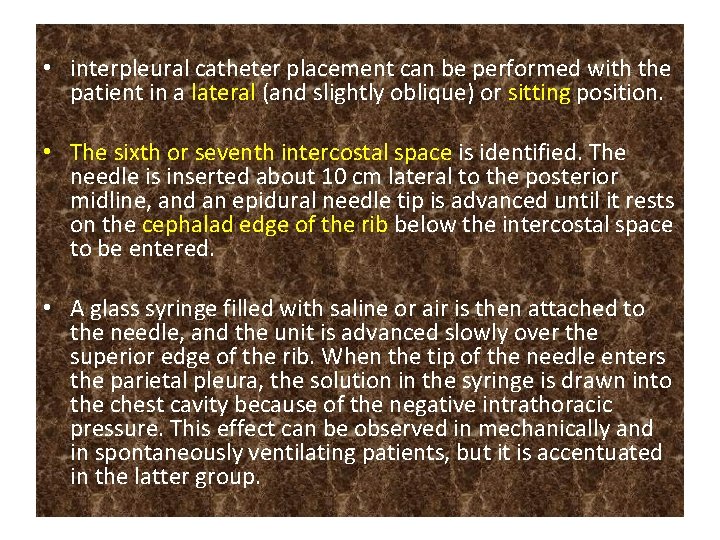
• interpleural catheter placement can be performed with the patient in a lateral (and slightly oblique) or sitting position. • The sixth or seventh intercostal space is identified. The needle is inserted about 10 cm lateral to the posterior midline, and an epidural needle tip is advanced until it rests on the cephalad edge of the rib below the intercostal space to be entered. • A glass syringe filled with saline or air is then attached to the needle, and the unit is advanced slowly over the superior edge of the rib. When the tip of the needle enters the parietal pleura, the solution in the syringe is drawn into the chest cavity because of the negative intrathoracic pressure. This effect can be observed in mechanically and in spontaneously ventilating patients, but it is accentuated in the latter group.

• Side effects: – Pneumothorax – Systemic toxicity – Cholestasis – Phernic nerve palsy












 Nursing care plan for cataract patient
Nursing care plan for cataract patient Causes of acute abdominal pain
Causes of acute abdominal pain Madpain
Madpain Period-like cramps during early pregnancy
Period-like cramps during early pregnancy Is pregnancy pain same as period pain
Is pregnancy pain same as period pain Data klinis
Data klinis Postoperative shock
Postoperative shock Post operative nursing management
Post operative nursing management Russian revolution vs french revolution
Russian revolution vs french revolution You should hope this game will be over soon
You should hope this game will be over soon Green revolution vs third agricultural revolution
Green revolution vs third agricultural revolution Pancreatitis nursing interventions
Pancreatitis nursing interventions Pain management okc soonercare
Pain management okc soonercare Pico format question
Pico format question Stony brook pain management
Stony brook pain management Iu pain management
Iu pain management Chapter 7 nursing management of pain during labor and birth
Chapter 7 nursing management of pain during labor and birth Gonzalez vallina
Gonzalez vallina Nonpharmacologic pain management nursing
Nonpharmacologic pain management nursing Prizm pain management
Prizm pain management Matrifen
Matrifen Pain definition nursing
Pain definition nursing Dr danko pain management
Dr danko pain management Triangle conclusion paragraph
Triangle conclusion paragraph Dr. mehdi pain management
Dr. mehdi pain management Pain management ehr
Pain management ehr Cervical facet referral patterns
Cervical facet referral patterns Pain res manage
Pain res manage Dr lascarides pain management
Dr lascarides pain management Pain management synonym
Pain management synonym Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em