Acute Pain Management for the Chronic Pain Patient








- Slides: 53
Acute Pain Management for the Chronic Pain Patient Paul S. Tumber, MD FRCPC Assistant Professor of Anesthesiology Toronto Western Hospital Pain Management Consultant UHN / Wasser Pain Clinic, Mt. Sinai Hospital, and WCH Paul. tumber@uhn. ca
Objectives: Understand some of the challenges faced by individuals with chronic pain Review acute pain management principles, and how these need to be modified when dealing with individuals with chronic pain
Ehlers-Danlos and Chronic Pain: Some Key Points Vast majority will have chronic pain Under-diagnosed by clinicians Complex presentation: Incomplete knowledge of mechanisms involved Joint, muscle, proprioreception, small-fiber nerves/CNS Fatigue, headaches, sleep disturbance, anxiety Gastrointestinal, Pelvic pain Autonomic dysfunction ( example POTS ) Chopra, P et al. Pain Management in Ehlers-Danlos Syndromes Am J Med Genetics 175 C: 2017

The Impact of Persistent Pain: Bio-psycho-spiritual not just bio-medical • Psychologic: somatic focus and fear/anxiety, sleep-deprivation, fatigue • • Loss: personal, financial, social, spouse Deconditioning, weight gain Frustration with medical system Enigma and Stigma
http: //www. gb 42. com/ynot_The_Pain_Exhibit. html
The acute pain problem: Millions of surgeries per year 80% will report postoperative pain At least 75% report >= moderate pain
What about acute on chronic pain?
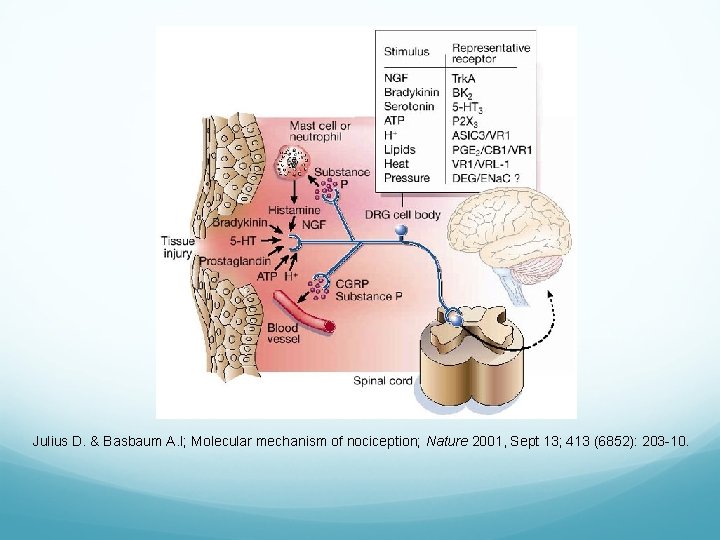
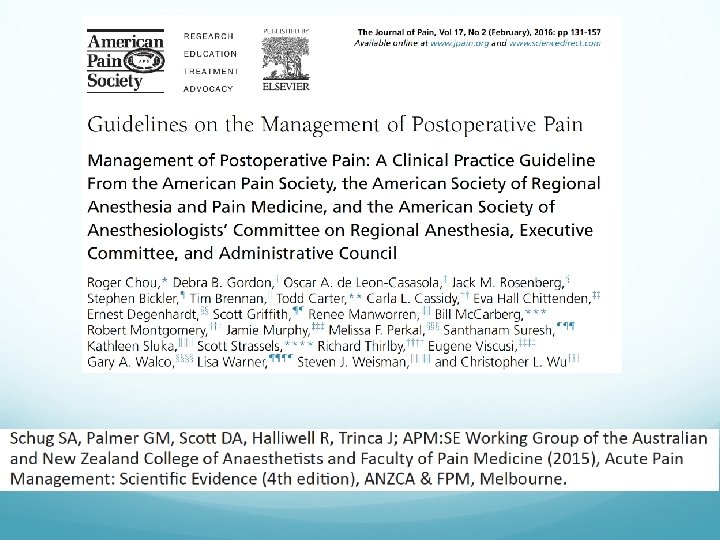
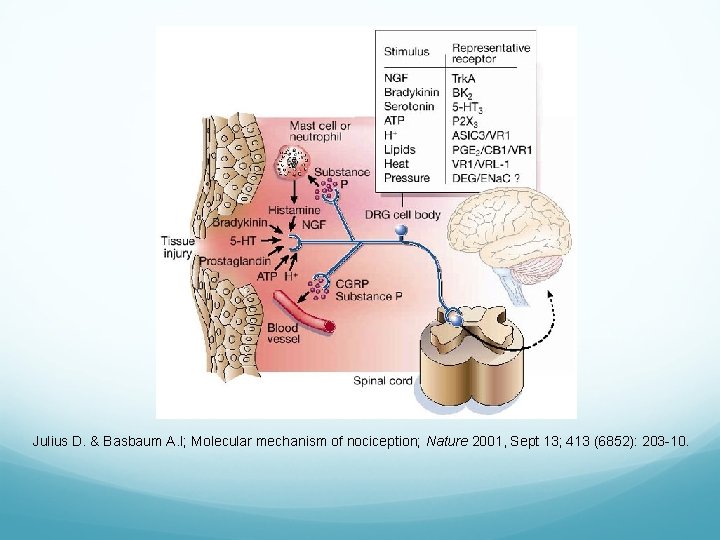
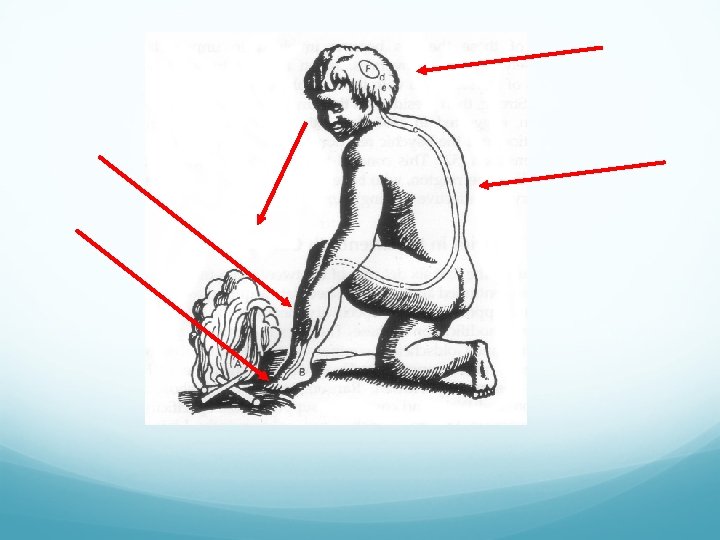
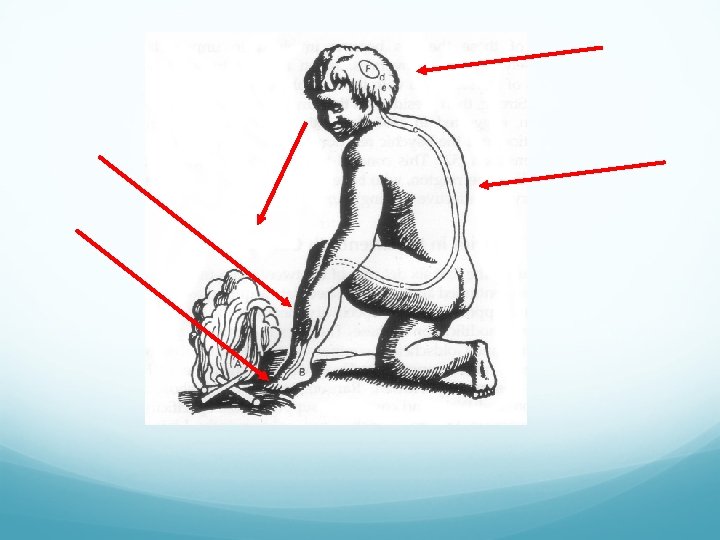
Julius D. & Basbaum A. I; Molecular mechanism of nociception; Nature 2001, Sept 13; 413 (6852): 203 -10.
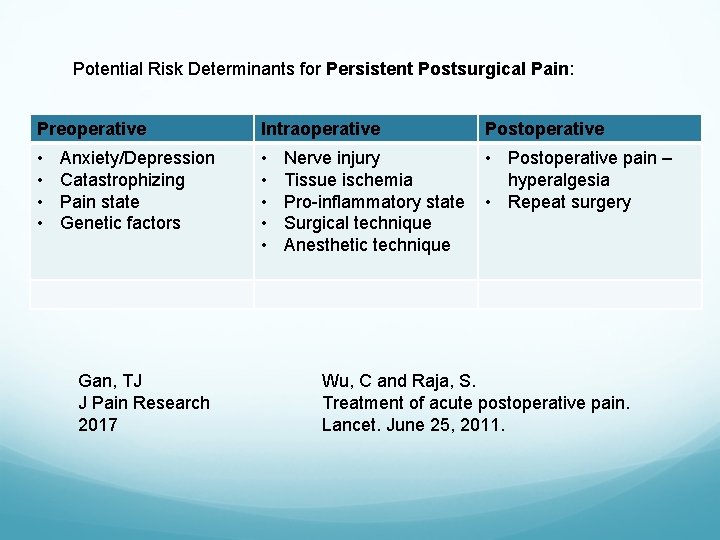
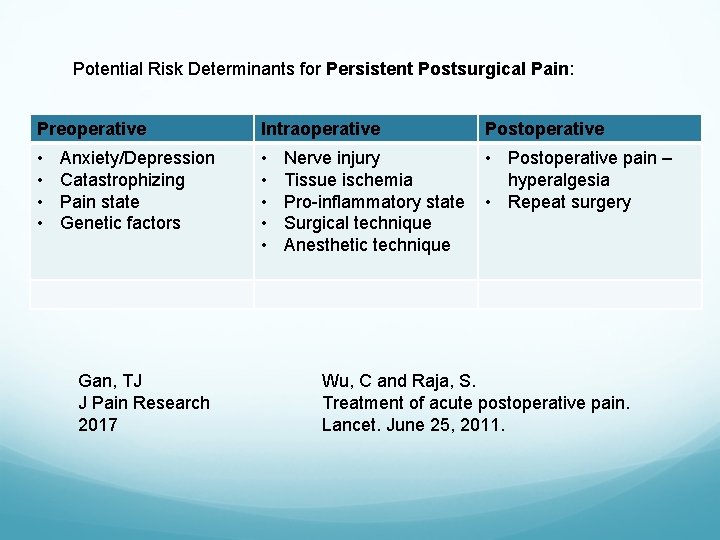
Potential Risk Determinants for Persistent Postsurgical Pain: Preoperative Intraoperative Postoperative • • • Postoperative pain – hyperalgesia • Repeat surgery Anxiety/Depression Catastrophizing Pain state Genetic factors Gan, TJ J Pain Research 2017 Nerve injury Tissue ischemia Pro-inflammatory state Surgical technique Anesthetic technique Wu, C and Raja, S. Treatment of acute postoperative pain. Lancet. June 25, 2011.
Analgesia: The Big Picture
Which Drug to Choose?

The perfect analgesic: what are we looking for? Effective Safe / Non-toxic: No CNS or cardiorespiratory depression No constipation No nausea Easy to order, easy to administer, easy to take No drug interactions Inexpensive No withdrawal, dependence, tolerance, addiction Useful in all patient populations Elderly vs. young, pregnant, hepatic failure, renal failure, CHF Reversible effect Quick onset Acceptable duration of effect (long, short) Different preparations (liquid, sublingual, injectable, transdermal) Better than currently available analgesic of the same class!
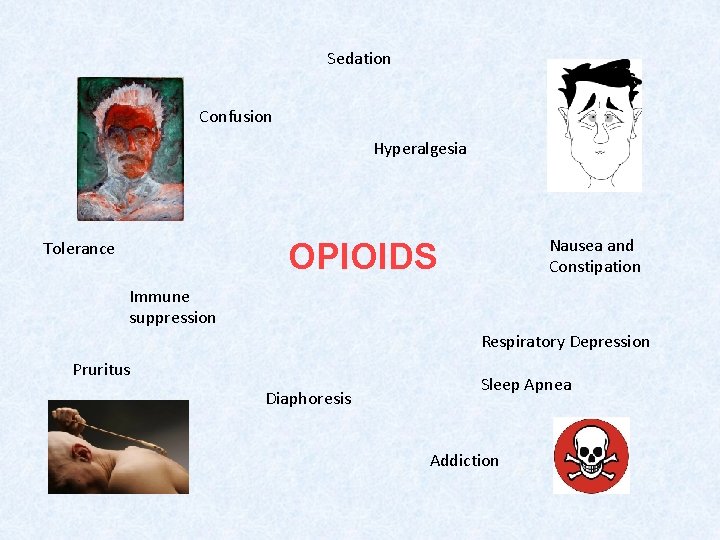
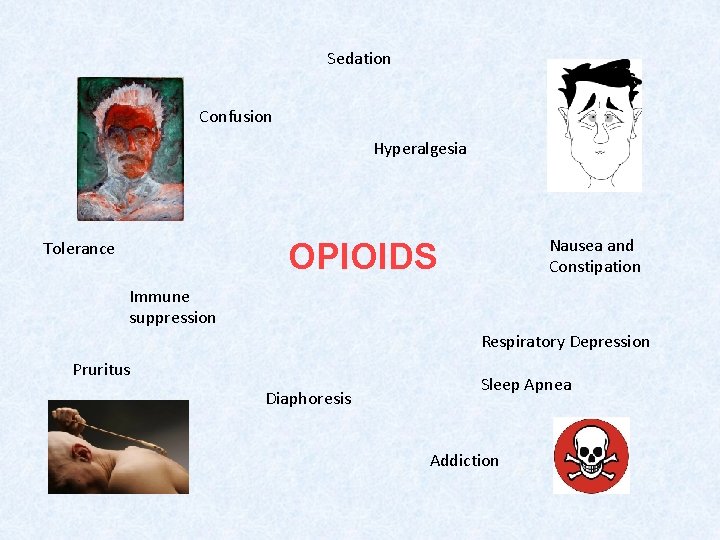
Sedation Confusion Hyperalgesia Nausea and Constipation OPIOIDS Tolerance Immune suppression Respiratory Depression Pruritus Diaphoresis Sleep Apnea Addiction
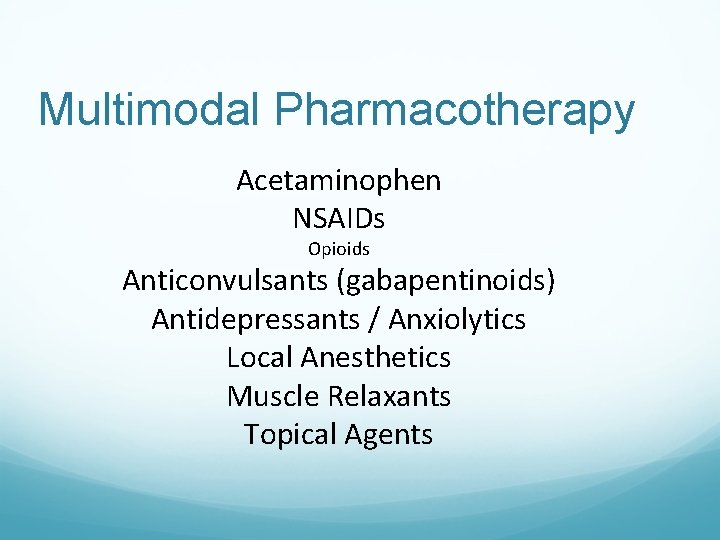
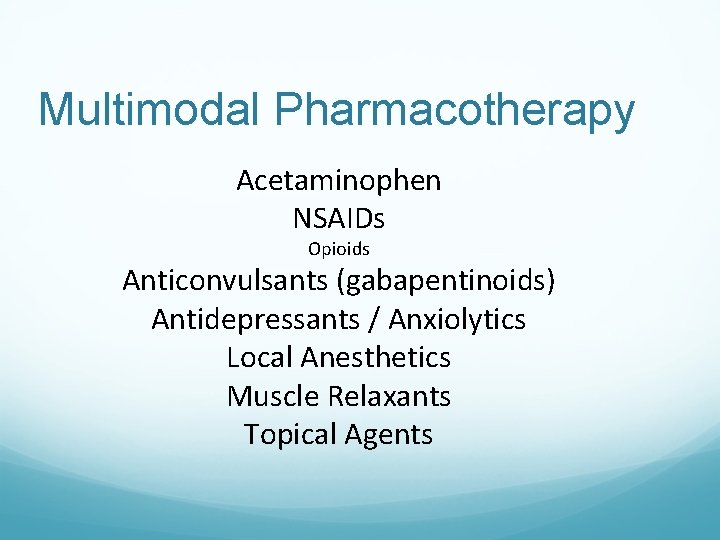
Multimodal Pharmacotherapy Acetaminophen NSAIDs Opioids Anticonvulsants (gabapentinoids) Antidepressants / Anxiolytics Local Anesthetics Muscle Relaxants Topical Agents

Multimodal Analgesia

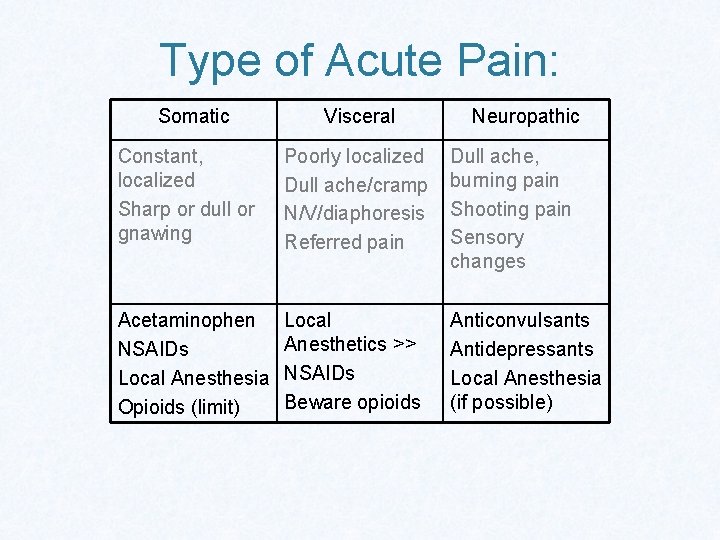
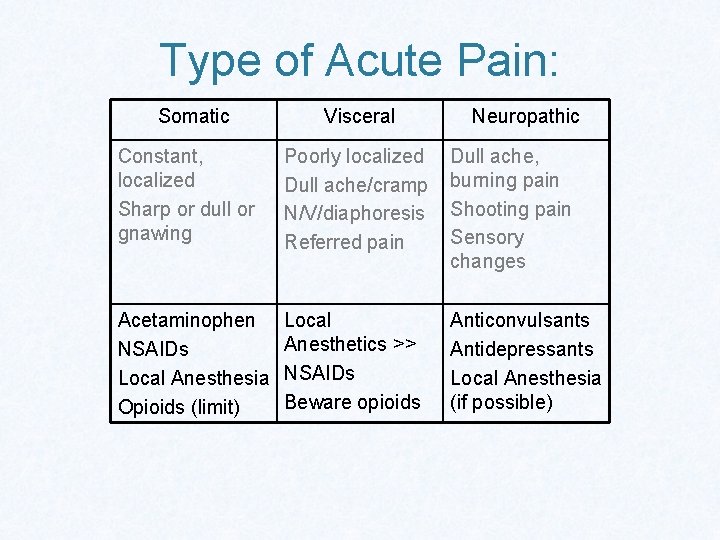
Type of Acute Pain: Somatic Visceral Neuropathic Constant, localized Sharp or dull or gnawing Poorly localized Dull ache/cramp N/V/diaphoresis Referred pain Dull ache, burning pain Shooting pain Sensory changes Acetaminophen NSAIDs Local Anesthesia Opioids (limit) Local Anesthetics >> NSAIDs Beware opioids Anticonvulsants Antidepressants Local Anesthesia (if possible)
Nonspecific Treatment Effects in Pain Medicine Satisfaction with care correlates with the doctor-patient relationship: Trust, mutual respect, communication, enthusiasm. Jamison, Robert Pain Clinical Updates: January 2011
Nonspecific Treatment Effects Patient expectations: feel welcome? Informed? believe their perspective is understood? feel secure that their basic needs have been met? Attention to details specific to the patient? Adequate time spent with the patient? Robert N. Jamison, Ph. D
Team Approach: -Family support -Nursing -Surgery -APS / Anesth -Physical therapy/OT -Pharmacy -Psychology/Psychiatry -Medicine/Dentistry -Dietician/Nutritionists -Addiction Medicine -Social Work -Clergy/Spiritual Guidance
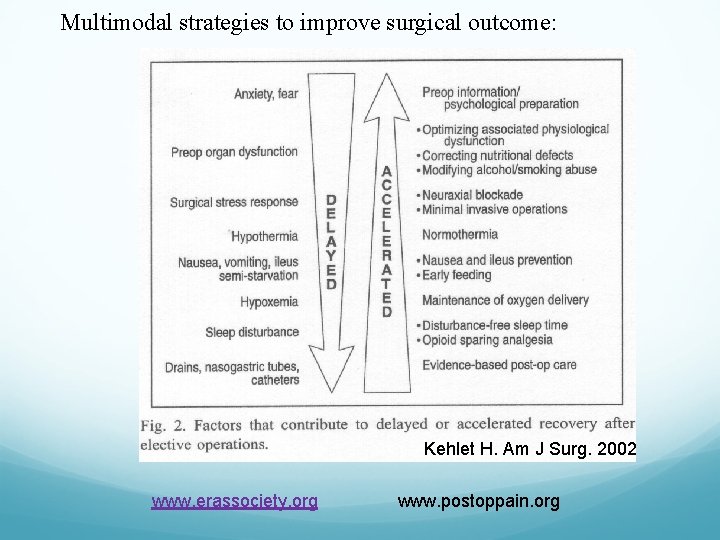
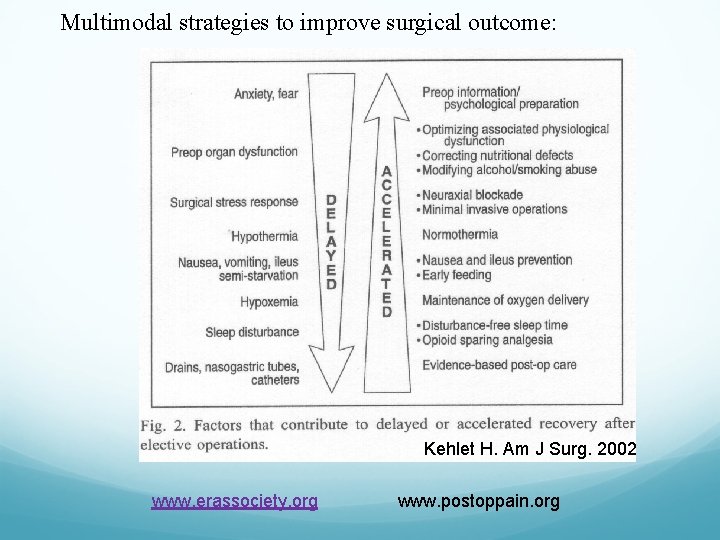
Multimodal strategies to improve surgical outcome: Kehlet H. Am J Surg. 2002 www. erassociety. org www. postoppain. org
How do we treat acute on chronic pain?

Multimodal Analgesia: 1. Preoperative 2. Intraoperative 3. Postoperative
Preoperative Phase: Education and Expectations -- notify A. P. S. Optimize pain control, anxiety/depression • Involve family members Patient-centered care
Preoperative Phase: Premedication: • Nsaid/Coxib; Acetaminophen; • Sustained-release opioid • Anxiolytic: • Lorazepam (Ativan) 1 - 2 mg Clonidine (beware hypotension, bradycardia) Gabapentinoid
Intraoperative Phase
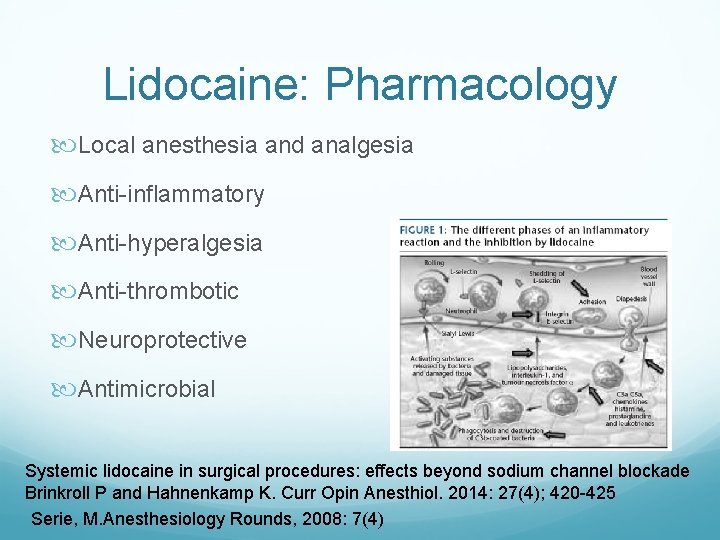
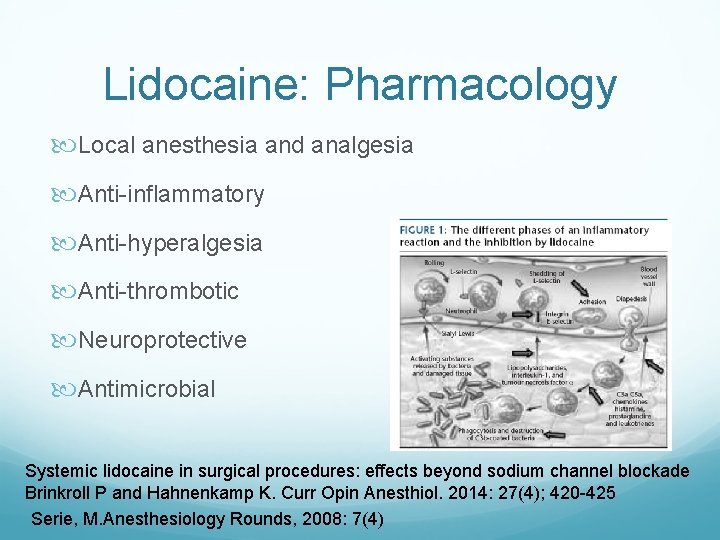
Lidocaine: Pharmacology Local anesthesia and analgesia Anti-inflammatory Anti-hyperalgesia Anti-thrombotic Neuroprotective Antimicrobial Systemic lidocaine in surgical procedures: effects beyond sodium channel blockade Brinkroll P and Hahnenkamp K. Curr Opin Anesthiol. 2014: 27(4); 420 -425 Serie, M. Anesthesiology Rounds, 2008: 7(4)
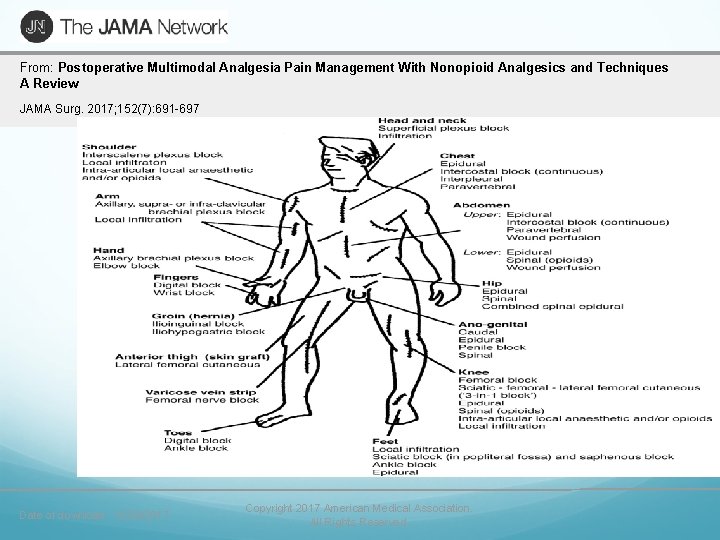
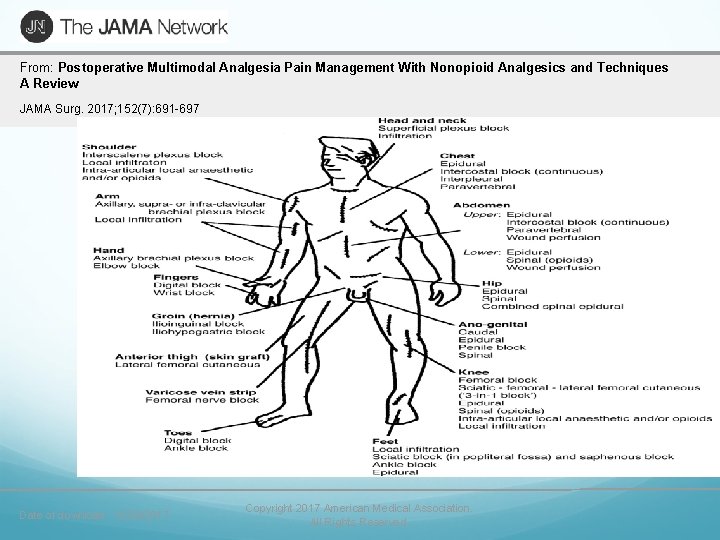
From: Postoperative Multimodal Analgesia Pain Management With Nonopioid Analgesics and Techniques A Review JAMA Surg. 2017; 152(7): 691 -697 Date of download: 10/28/2017 Copyright 2017 American Medical Association. All Rights Reserved.
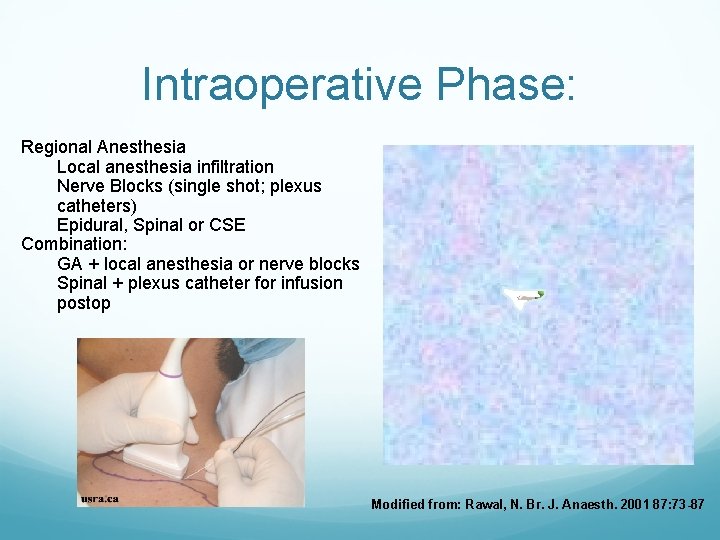
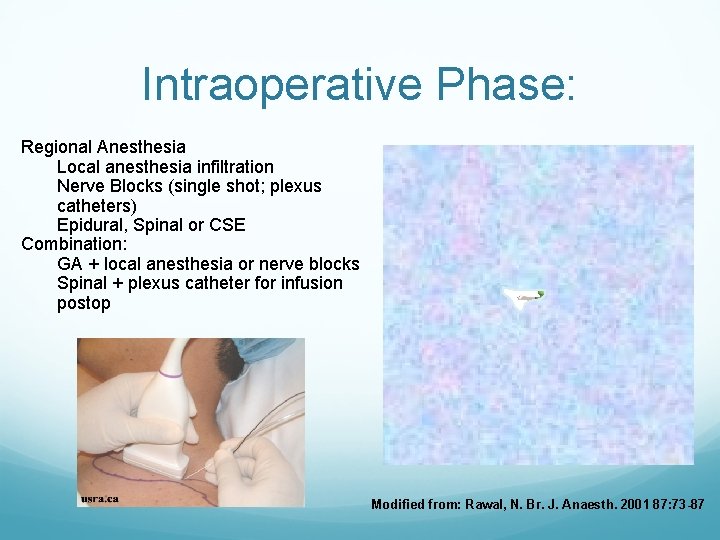
Intraoperative Phase: Regional Anesthesia Local anesthesia infiltration Nerve Blocks (single shot; plexus catheters) Epidural, Spinal or CSE Combination: GA + local anesthesia or nerve blocks Spinal + plexus catheter for infusion postop Modified from: Rawal, N. Br. J. Anaesth. 2001 87: 73 -87
Intraoperative Phase: Consider ketorolac Dexamethasone Lidocaine IV Ketamine Magnesium
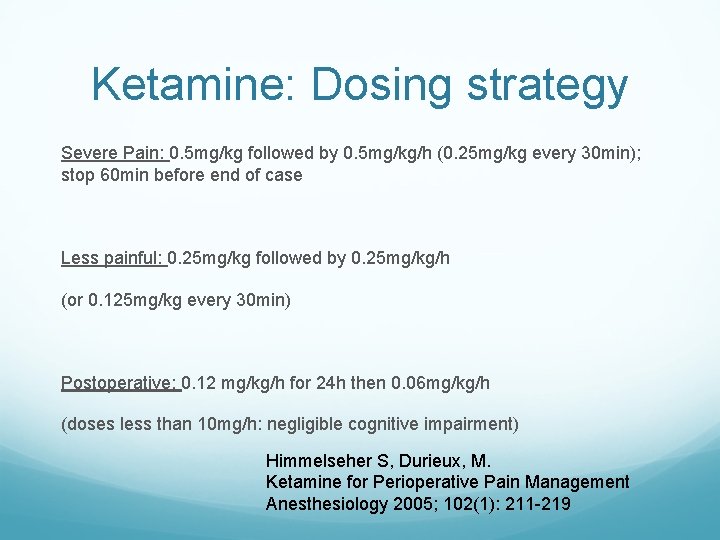
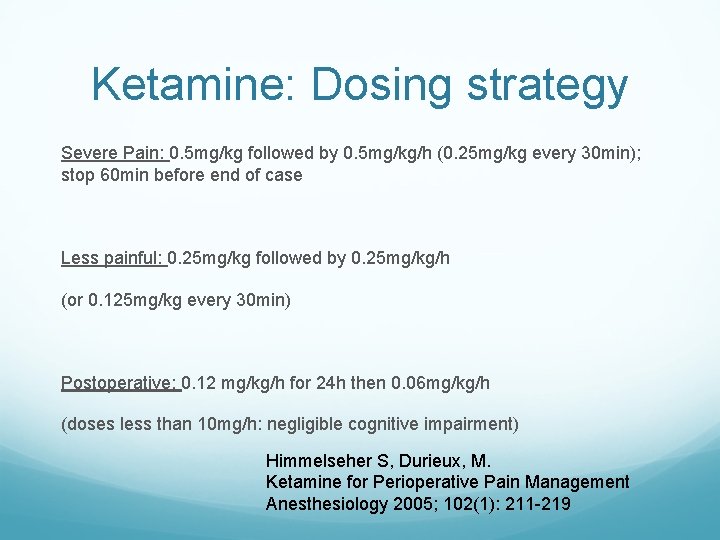
Ketamine: Dosing strategy Severe Pain: 0. 5 mg/kg followed by 0. 5 mg/kg/h (0. 25 mg/kg every 30 min); stop 60 min before end of case Less painful: 0. 25 mg/kg followed by 0. 25 mg/kg/h (or 0. 125 mg/kg every 30 min) Postoperative: 0. 12 mg/kg/h for 24 h then 0. 06 mg/kg/h (doses less than 10 mg/h: negligible cognitive impairment) Himmelseher S, Durieux, M. Ketamine for Perioperative Pain Management Anesthesiology 2005; 102(1): 211 -219
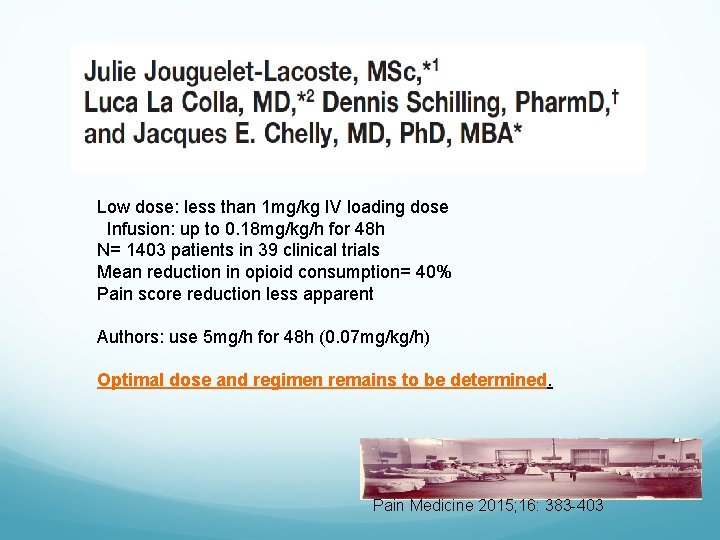
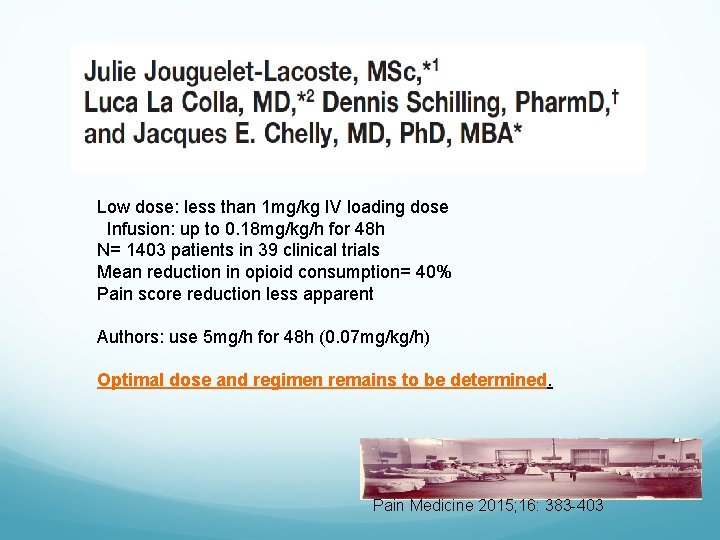
Low dose: less than 1 mg/kg IV loading dose Infusion: up to 0. 18 mg/kg/h for 48 h N= 1403 patients in 39 clinical trials Mean reduction in opioid consumption= 40% Pain score reduction less apparent Authors: use 5 mg/h for 48 h (0. 07 mg/kg/h) Optimal dose and regimen remains to be determined. Pain Medicine 2015; 16: 383 -403
Postoperative Analgesia
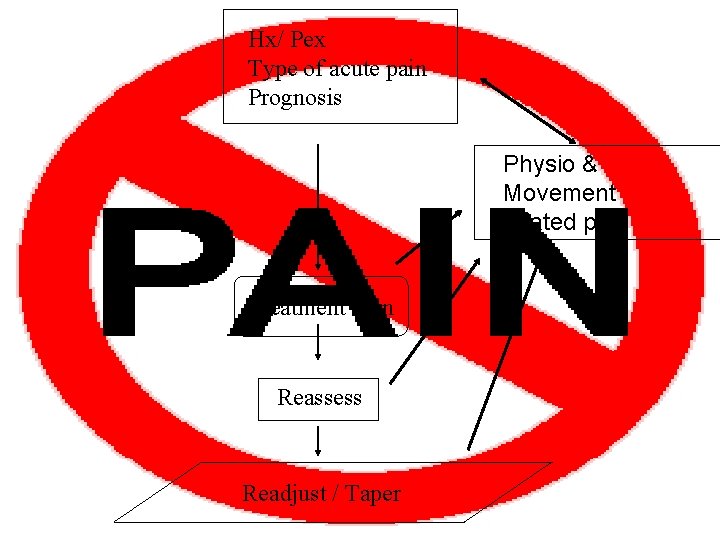
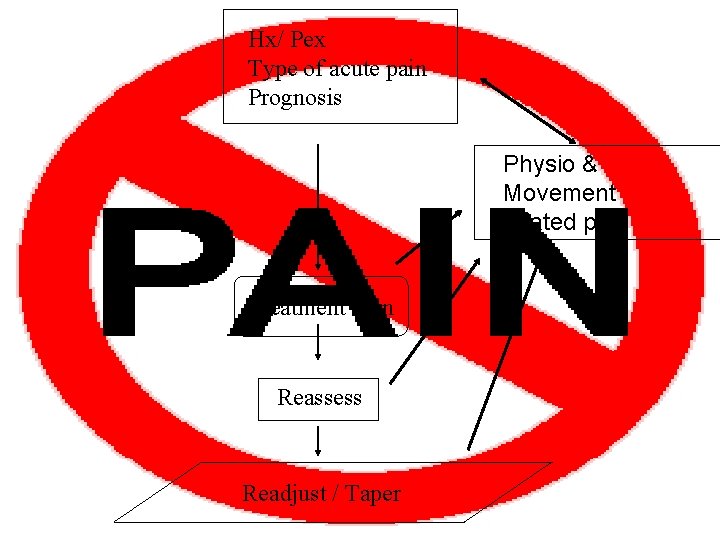
Hx/ Pex Type of acute pain Prognosis Physio & Movement related pain Treatment Plan Reassess Readjust / Taper
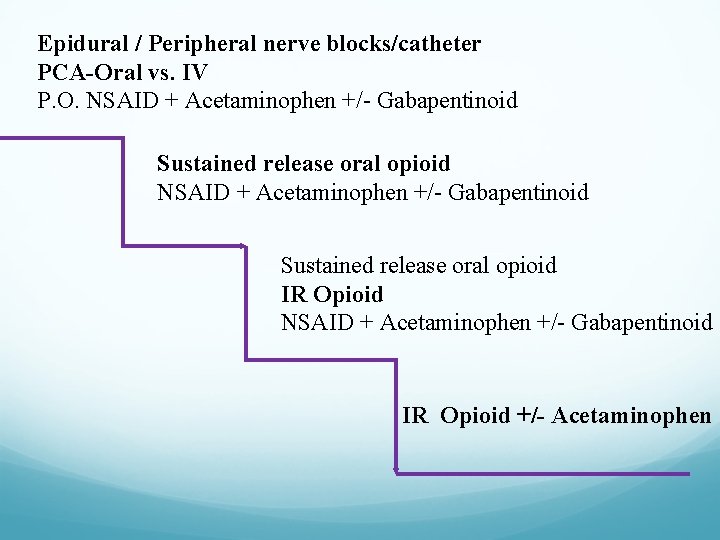
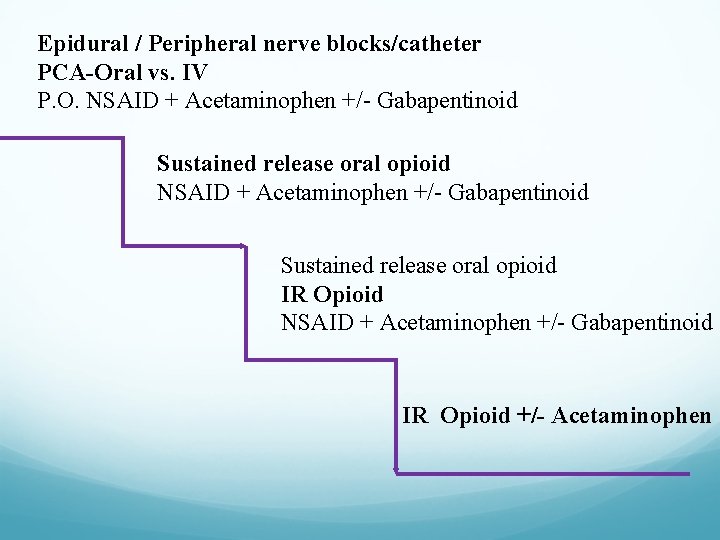
Epidural / Peripheral nerve blocks/catheter PCA-Oral vs. IV P. O. NSAID + Acetaminophen +/- Gabapentinoid Sustained release oral opioid IR Opioid NSAID + Acetaminophen +/- Gabapentinoid IR Opioid +/- Acetaminophen
Postoperative Analgesia: 1. Utilize patient controlled analgesia 2. Other medications round the clock (RTC) 3. Monitor and treat side effects 4. Consider pain as the fifth vital sign
Opioids: Tips Educate patients and caregivers Universal Precautions shared-decision making risk vs. benefit, alternatives, time course, follow-up, expectations: opioid contract Adjust doses according to requirements Example: decrease night time dose of opioid vs. increased daytime doses with physiotherapy Beware polypharmacy (esp. BDZ) Consider opioid rotation Taper sustained release opioids whenever possible
Multimodal Pharmacotherapy Acetaminophen NSAIDs Opioids Anticonvulsants Antidepressants Muscle Relaxants Topical Agents

Multimodal Pharmacotherapy Acetaminophen NSAIDs Opioids Anticonvulsants Antidepressants Muscle Relaxants Topical Agents
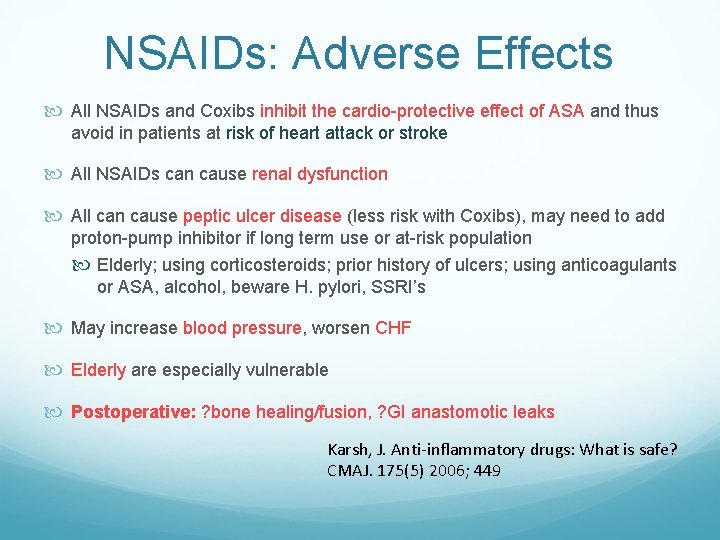
NSAIDs: Adverse Effects All NSAIDs and Coxibs inhibit the cardio-protective effect of ASA and thus avoid in patients at risk of heart attack or stroke All NSAIDs can cause renal dysfunction All can cause peptic ulcer disease (less risk with Coxibs), may need to add proton-pump inhibitor if long term use or at-risk population Elderly; using corticosteroids; prior history of ulcers; using anticoagulants or ASA, alcohol, beware H. pylori, SSRI’s May increase blood pressure, worsen CHF Elderly are especially vulnerable Postoperative: ? bone healing/fusion, ? GI anastomotic leaks Karsh, J. Anti-inflammatory drugs: What is safe? CMAJ. 175(5) 2006; 449
Multimodal Pharmacotherapy Acetaminophen NSAIDs Opioids Anticonvulsants Antidepressants Muscle Relaxants Topical Agents
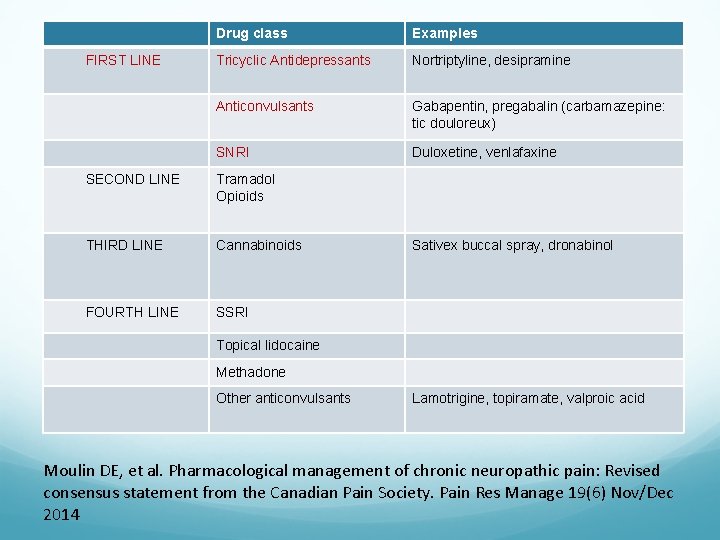
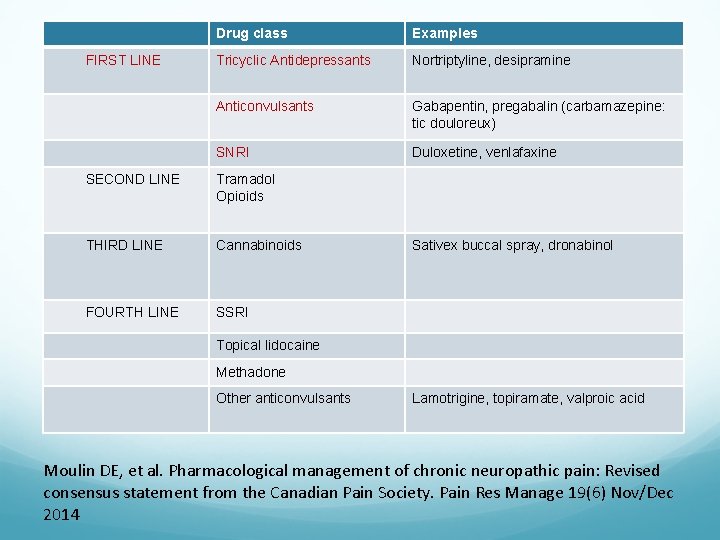
FIRST LINE Drug class Examples Tricyclic Antidepressants Nortriptyline, desipramine Anticonvulsants Gabapentin, pregabalin (carbamazepine: tic douloreux) SNRI Duloxetine, venlafaxine SECOND LINE Tramadol Opioids THIRD LINE Cannabinoids FOURTH LINE SSRI Sativex buccal spray, dronabinol Topical lidocaine Methadone Other anticonvulsants Lamotrigine, topiramate, valproic acid Moulin DE, et al. Pharmacological management of chronic neuropathic pain: Revised consensus statement from the Canadian Pain Society. Pain Res Manage 19(6) Nov/Dec 2014
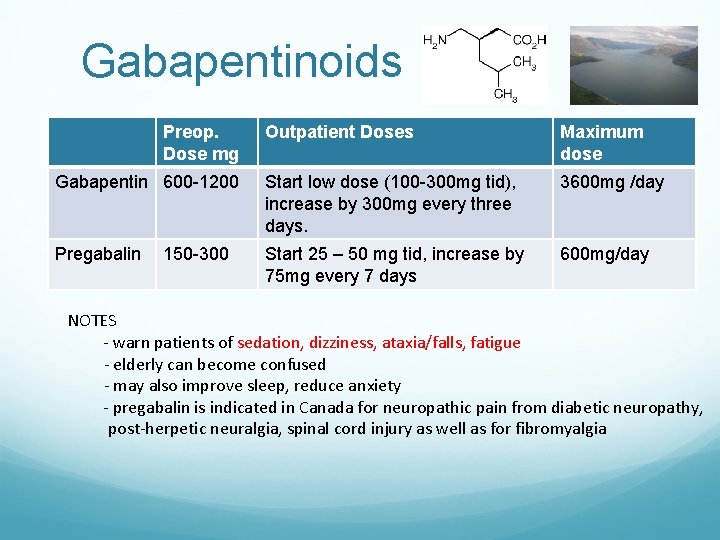
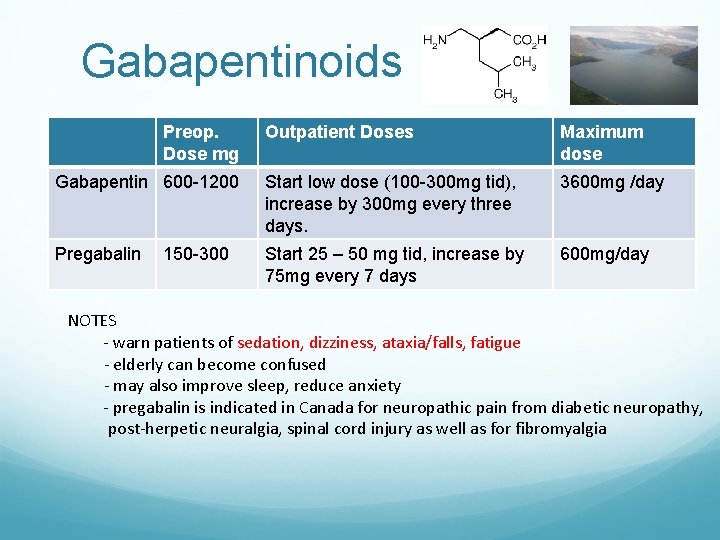
Gabapentinoids Preop. Dose mg Outpatient Doses Maximum dose Gabapentin 600 -1200 Start low dose (100 -300 mg tid), increase by 300 mg every three days. 3600 mg /day Pregabalin Start 25 – 50 mg tid, increase by 75 mg every 7 days 600 mg/day 150 -300 NOTES - warn patients of sedation, dizziness, ataxia/falls, fatigue - elderly can become confused - may also improve sleep, reduce anxiety - pregabalin is indicated in Canada for neuropathic pain from diabetic neuropathy, post-herpetic neuralgia, spinal cord injury as well as for fibromyalgia

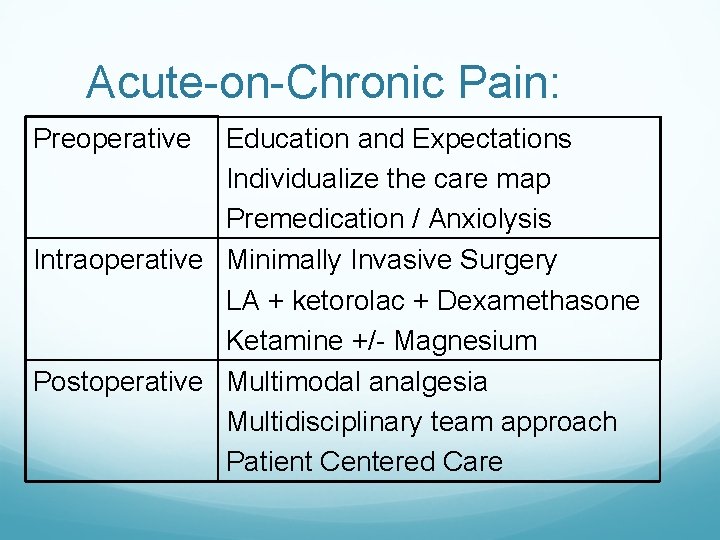
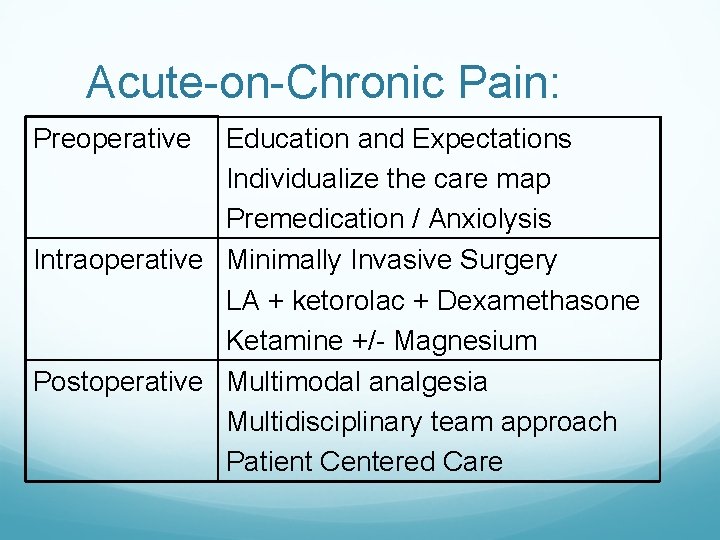
Acute-on-Chronic Pain: Preoperative Education and Expectations Individualize the care map Premedication / Anxiolysis Intraoperative Minimally Invasive Surgery LA + ketorolac + Dexamethasone Ketamine +/- Magnesium Postoperative Multimodal analgesia Multidisciplinary team approach Patient Centered Care
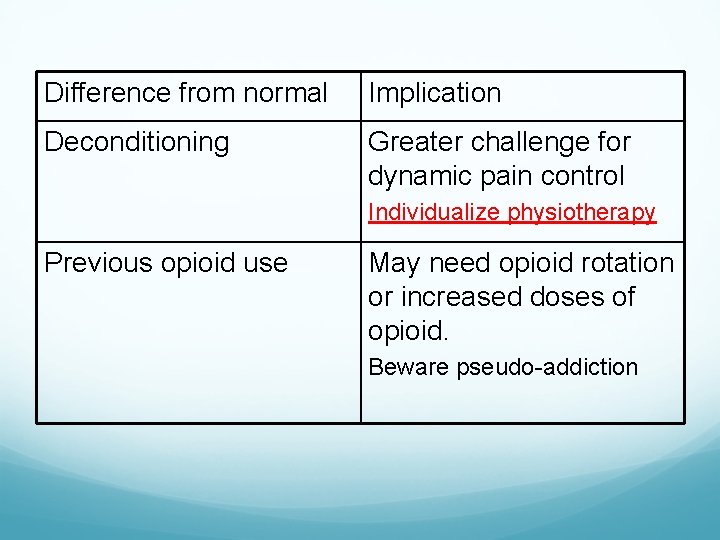
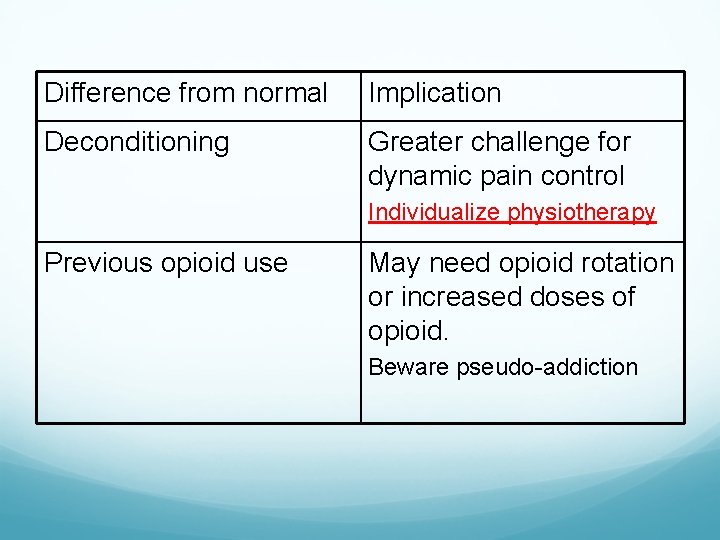
Difference from normal Implication Deconditioning Greater challenge for dynamic pain control Individualize physiotherapy Previous opioid use May need opioid rotation or increased doses of opioid. Beware pseudo-addiction
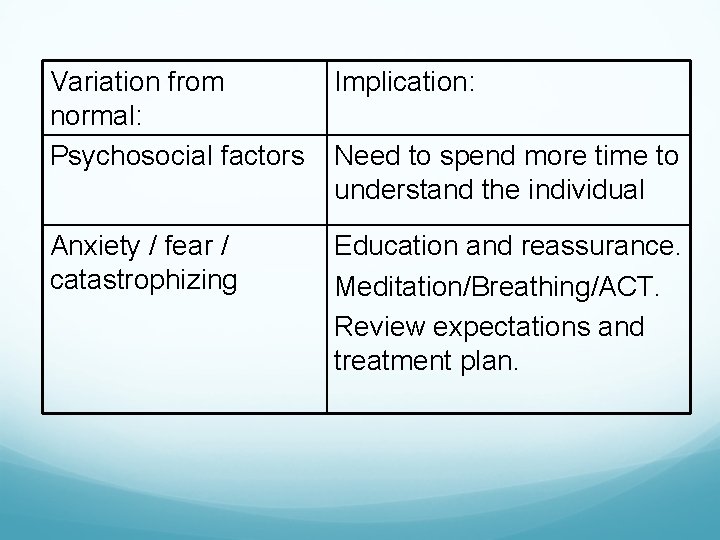
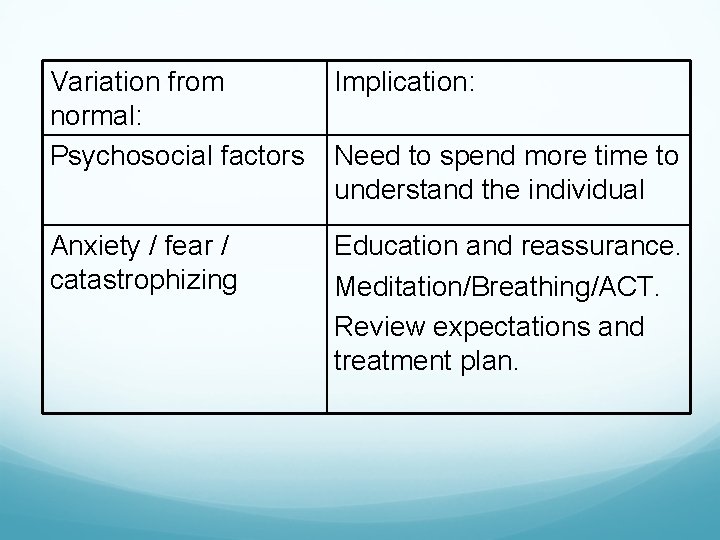
Variation from normal: Psychosocial factors Implication: Anxiety / fear / catastrophizing Education and reassurance. Meditation/Breathing/ACT. Review expectations and treatment plan. Need to spend more time to understand the individual
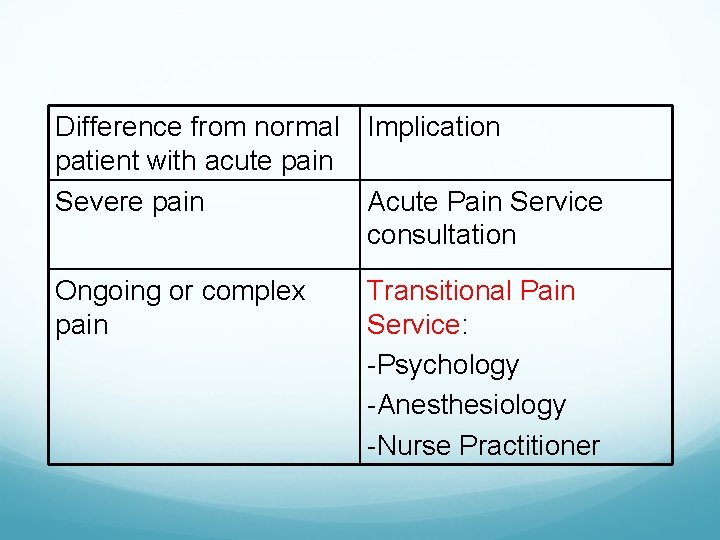
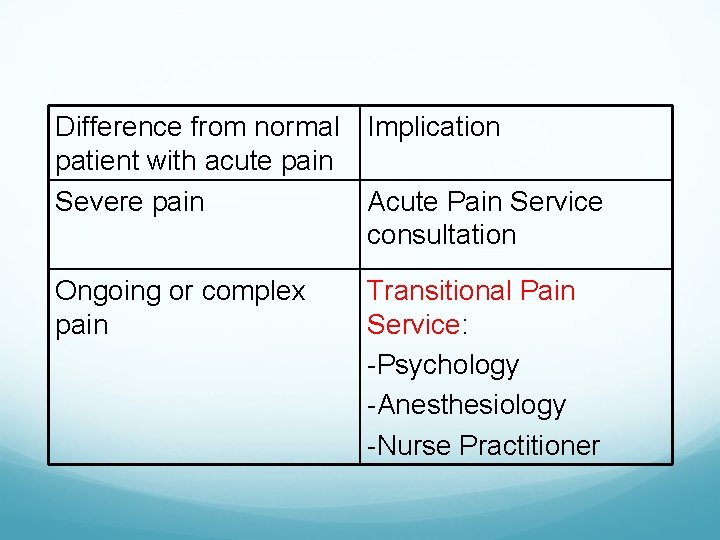
Difference from normal Implication patient with acute pain Severe pain Acute Pain Service consultation Ongoing or complex pain Transitional Pain Service: -Psychology -Anesthesiology -Nurse Practitioner
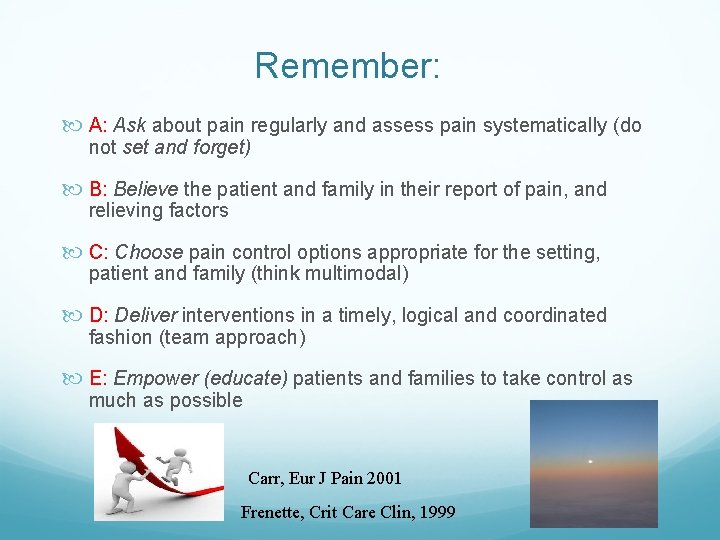
Remember: A: Ask about pain regularly and assess pain systematically (do not set and forget) B: Believe the patient and family in their report of pain, and relieving factors C: Choose pain control options appropriate for the setting, patient and family (think multimodal) D: Deliver interventions in a timely, logical and coordinated fashion (team approach) E: Empower (educate) patients and families to take control as much as possible Carr, Eur J Pain 2001 Frenette, Crit Care Clin, 1999

 Santa fe pain and spine
Santa fe pain and spine Differences between acute and chronic inflammation
Differences between acute and chronic inflammation Acute cholecystitis vs chronic cholecystitis
Acute cholecystitis vs chronic cholecystitis Acute subacute chronic
Acute subacute chronic Pigment gallstones causes
Pigment gallstones causes Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Morphological pattern of inflammation
Morphological pattern of inflammation Acute vs chronic heart failure
Acute vs chronic heart failure Leukemia death rate
Leukemia death rate Classification of periapical diseases
Classification of periapical diseases Chronic pain definition
Chronic pain definition Chronic pain comorbidities
Chronic pain comorbidities Causes of acute abdominal pain
Causes of acute abdominal pain Patient 2 patient
Patient 2 patient Martian pain
Martian pain How to know if your period is coming or your pregnant
How to know if your period is coming or your pregnant Pms vs pregnancy symptoms
Pms vs pregnancy symptoms Flinders model of chronic care self-management limitations
Flinders model of chronic care self-management limitations Kate lorig stanford
Kate lorig stanford Wagner chronic care model
Wagner chronic care model Liver defination
Liver defination Pancreatitis nursing
Pancreatitis nursing Kontinuitetshantering
Kontinuitetshantering Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Varför kallas perioden 1918-1939 för mellankrigstiden?
Varför kallas perioden 1918-1939 för mellankrigstiden? En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Kassaregister ideell förening
Kassaregister ideell förening Personlig tidbok
Personlig tidbok Sura för anatom
Sura för anatom Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Stig kerman
Stig kerman Hur skriver man en tes
Hur skriver man en tes Delegerande ledarstil
Delegerande ledarstil Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Vätsketryck formel
Vätsketryck formel Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Bo bergman jag fryser om dina händer
Bo bergman jag fryser om dina händer Presentera för publik crossboss
Presentera för publik crossboss Teckenspråk minoritetsspråk argument
Teckenspråk minoritetsspråk argument Vem räknas som jude
Vem räknas som jude Treserva lathund
Treserva lathund Luftstrupen för medicinare
Luftstrupen för medicinare Claes martinsson
Claes martinsson Cks
Cks Byggprocessen steg för steg
Byggprocessen steg för steg Mat för unga idrottare
Mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar