Acute otitis media Acute inflammation in middle ear


- Slides: 25
Acute otitis media Acute inflammation in middle ear < 3 weeks (month) Often associated with a viral upper respiratory infection Most common reason for medical therapy for children younger than 5 years Recurrent otitis media: At � least 4 episodes/ year At least 3 episodes/ 6 months � (with adequate therapy)
Epidemiology Most children have at least one episode of AOM (by age 3, 50 -85%) Peak incidence age 6 -15 months Increased incidence in the fall and winter Only 20% are adults >700 milion cases/year
Causes Eustachian tube is lined with respiratory mucosa Responds together with nasopharynx mucosa Edema > narrowed > negative middle lumen ear pressure Influx of pathogens from nasopharynx is possible
Causes Inflammatory response in middle ear worsens the obstruction Trigger: Allergies � Upper � respiratory tract infections GER (especially children) � Adenoid hypertrophy � Other �
Causes Viral (30 -70%) RSV � Rhinovirus � Coronavirus � Influenza, � parainfluenza Bacterial (55%) (44%) Haemophilus influenzae (41%) � Moraxella catarrhalis (14%) � Gram negative enteric bacteria � S. Aureus � � Streptococcus pneumoniae • Combined (15%)
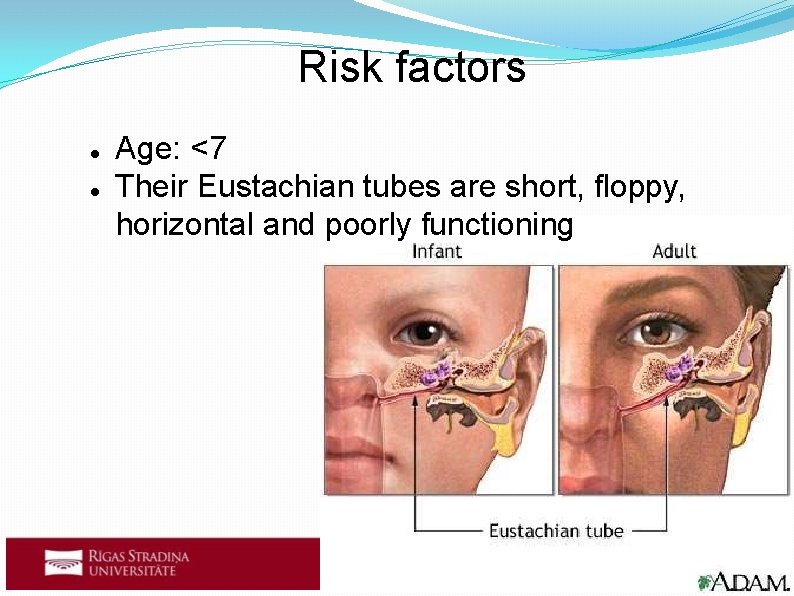
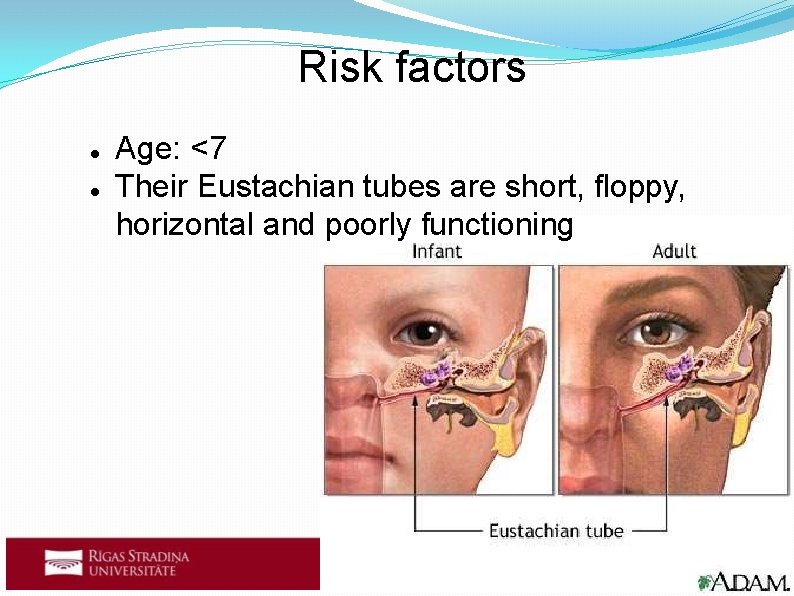
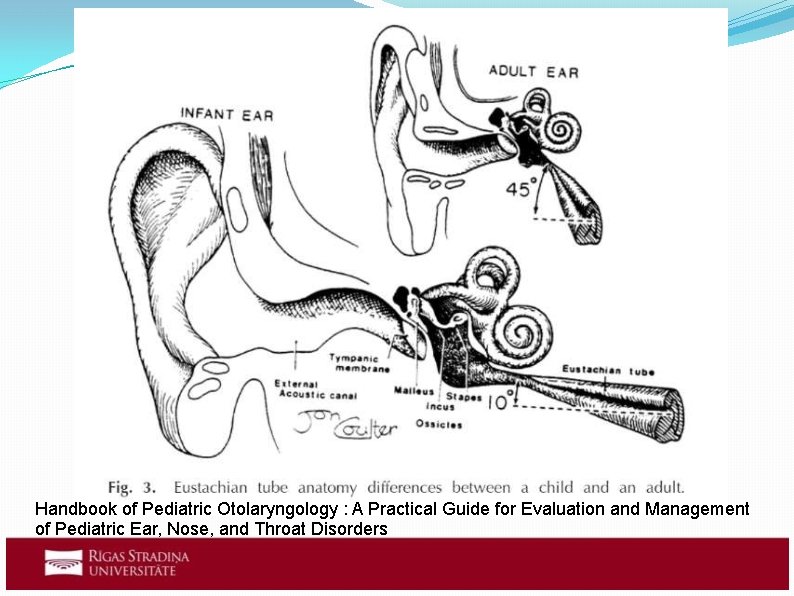
Risk factors Age: <7 Their Eustachian tubes are short, floppy, horizontal and poorly functioning
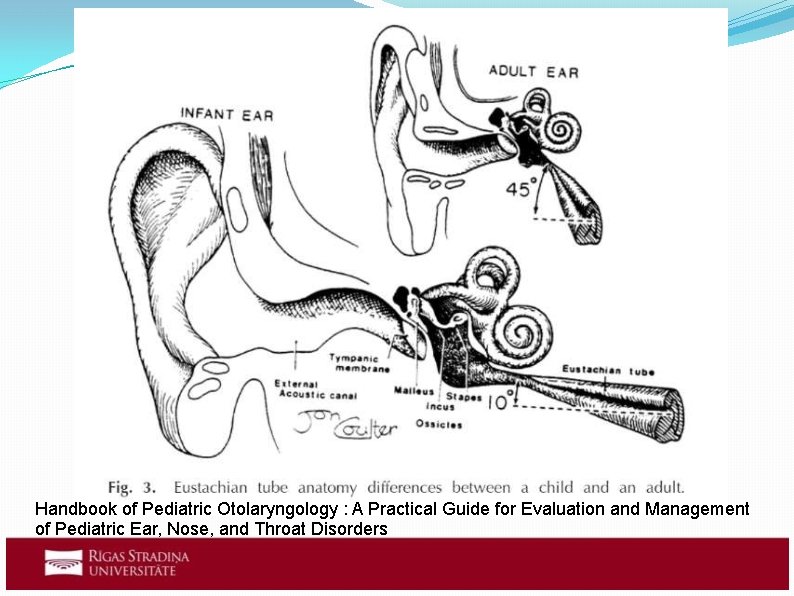
Handbook of Pediatric Otolaryngology : A Practical Guide for Evaluation and Management of Pediatric Ear, Nose, and Throat Disorders
Risk factors Genetic predisposition Eustachian � tube dysfunction Allergic tendencies � Bottle feeding (first 3 months) (breast milk contains lactoferrin, oligosaccharide and surface immunoglobulin A that inhibit bacterial colonization) (sucking generates negative pressure) Incorrect posture while breastfeeding
Risk factors Underlying pathology Unrepaired � cleft palate Parental smoking Large familys/attending daycare Immunocompromised states

Signs and symptoms Otalgia (not always) Fever Hearing loss (speech delay for children) Headache Nausea Cough Rhinitis Conjunctivitis
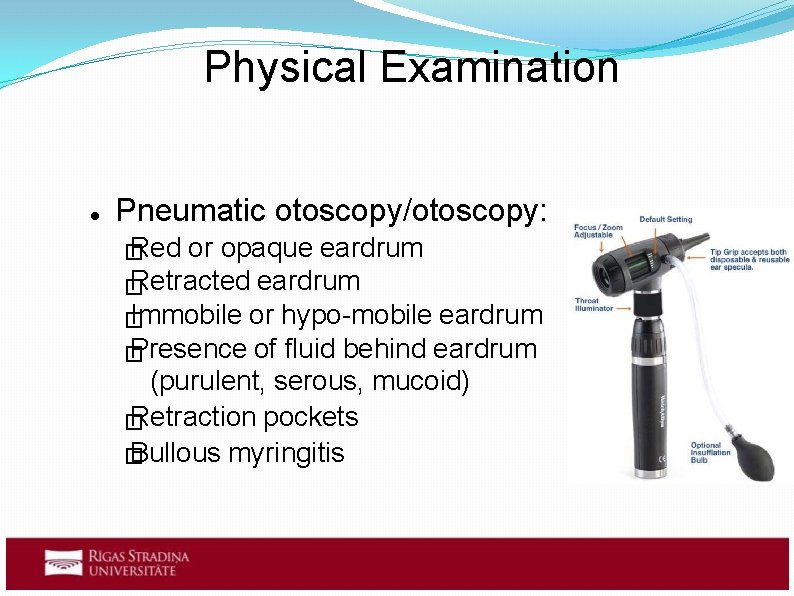
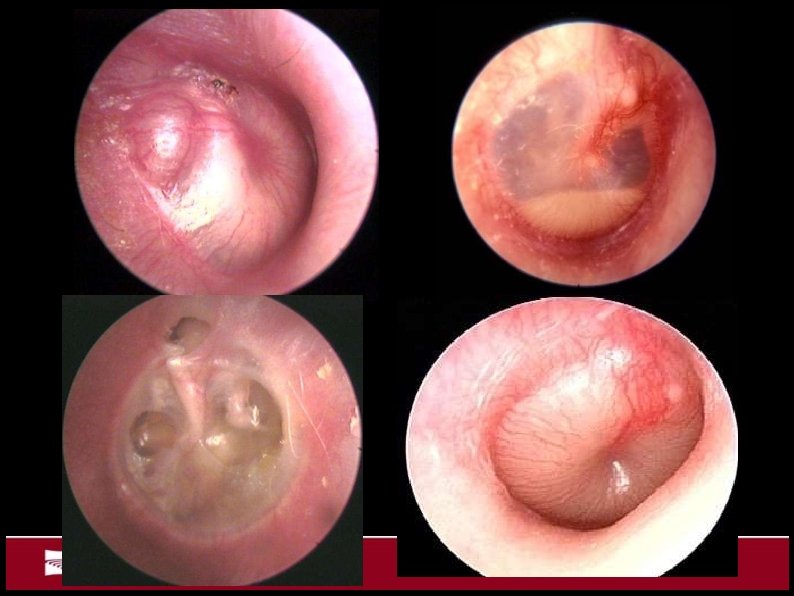
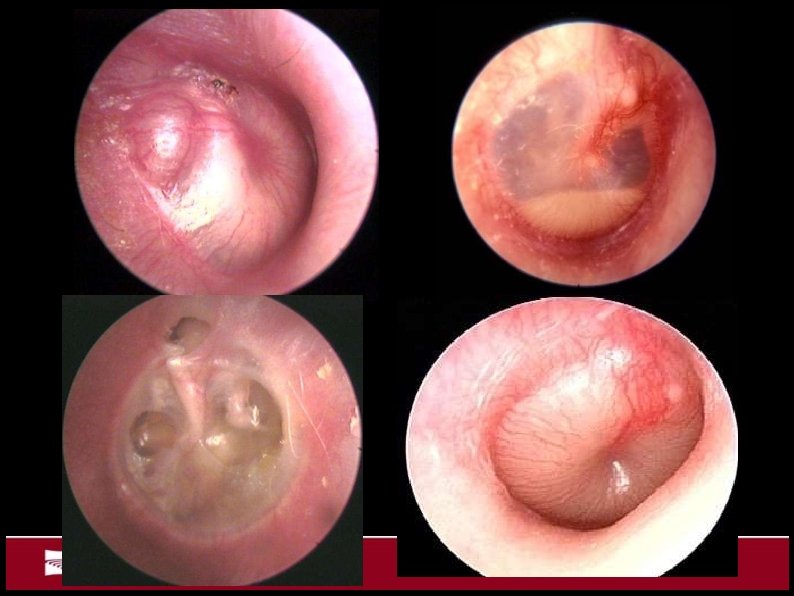
Physical Examination Pneumatic otoscopy/otoscopy: Red � or opaque eardrum Retracted eardrum � Immobile or hypo-mobile eardrum � Presence of fluid behind eardrum � (purulent, serous, mucoid) Retraction pockets � Bullous myringitis �

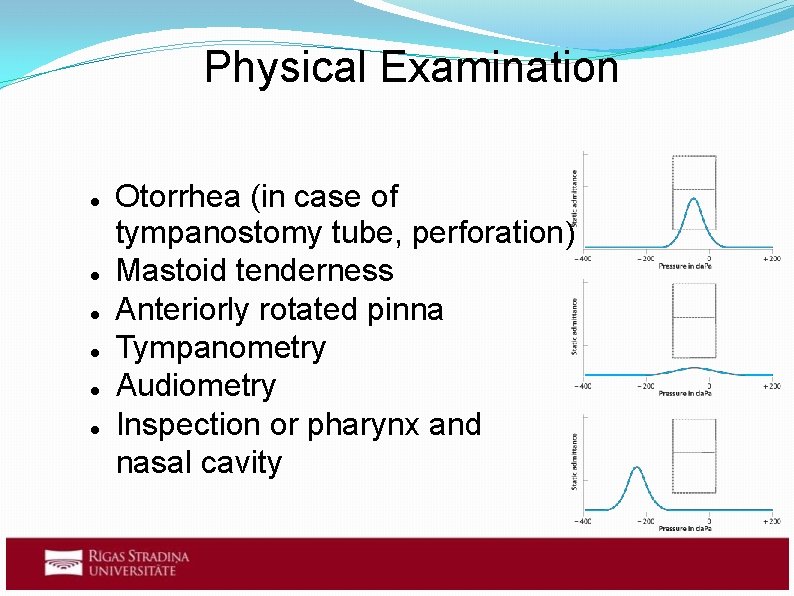
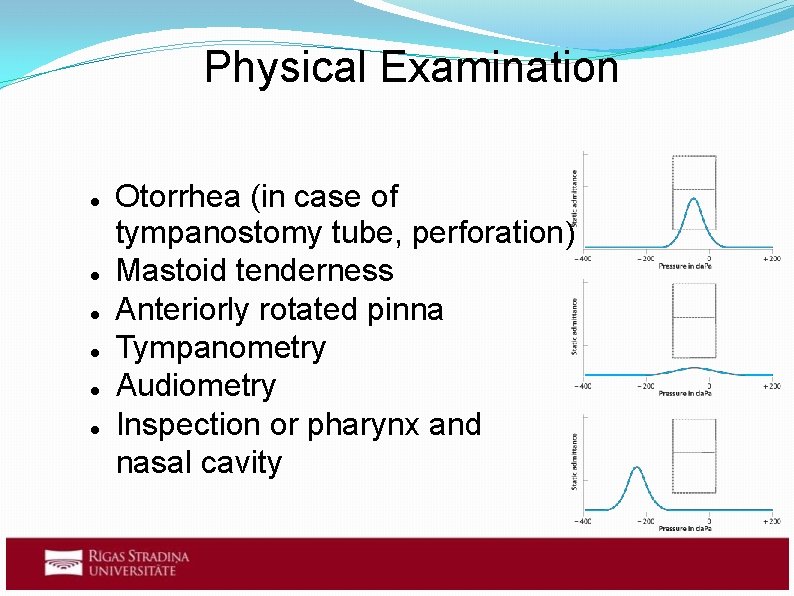
Physical Examination Otorrhea (in case of tympanostomy tube, perforation) Mastoid tenderness Anteriorly rotated pinna Tympanometry Audiometry Inspection or pharynx and nasal cavity
Diagnosis Acute onset of signs and syptoms The presence of middle ear effusion (hypomobile eardrum, air-fluid level) Signs and symptoms of middle ear inflamation (erythema, otalgia)
Complications Acute mastoiditis Abscess formation Facial paralysis Otitis media with effusion Persistent AOM Recurrent AOM Hearing loss Perforation of eardrum
Complications (rare) Lateral sinus thrombosis Otitic hydrocephalus Septic shock Meningitis Encephalitis Extradural abscess Labyrinthitis
Treatment Antibacterial therapy for: Children � of age <6 months 6 months to 2 years with severe illness � Recurrent or billateral AOM � Immunocompromised patients � Patients with a perforated tympanic membrane � Pain management (Ibuprofen, Diclofenac, paracetamol) Decongestants and/or antihistamines, nasal steroids
After 24 -48 h (48 -72 h) If no improvemants: No antibiotics > antibiotics � Antibiotics > change to a different � antibiotics
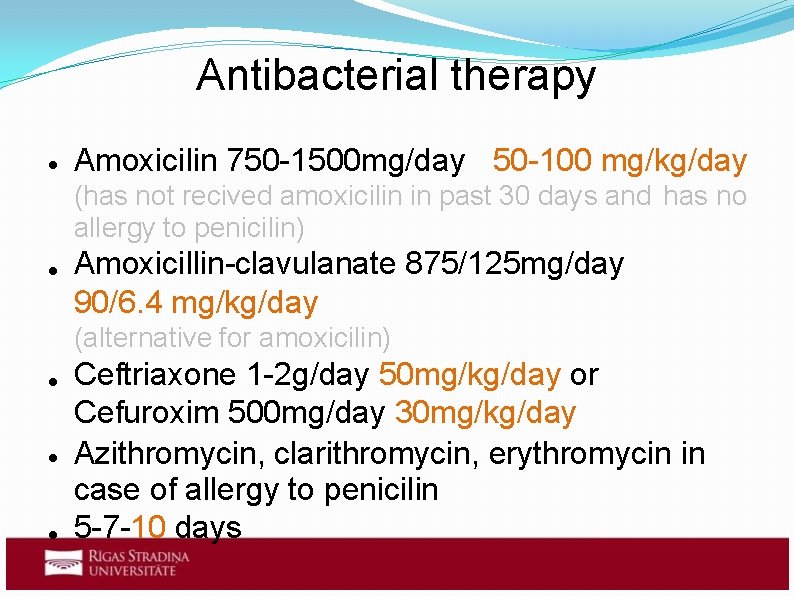
Antibacterial therapy Amoxicilin 750 -1500 mg/day 50 -100 mg/kg/day (has not recived amoxicilin in past 30 days and has no allergy to penicilin) Amoxicillin-clavulanate 875/125 mg/day 90/6. 4 mg/kg/day (alternative for amoxicilin) Ceftriaxone 1 -2 g/day 50 mg/kg/day or Cefuroxim 500 mg/day 30 mg/kg/day Azithromycin, clarithromycin, erythromycin in case of allergy to penicilin 5 -7 -10 days
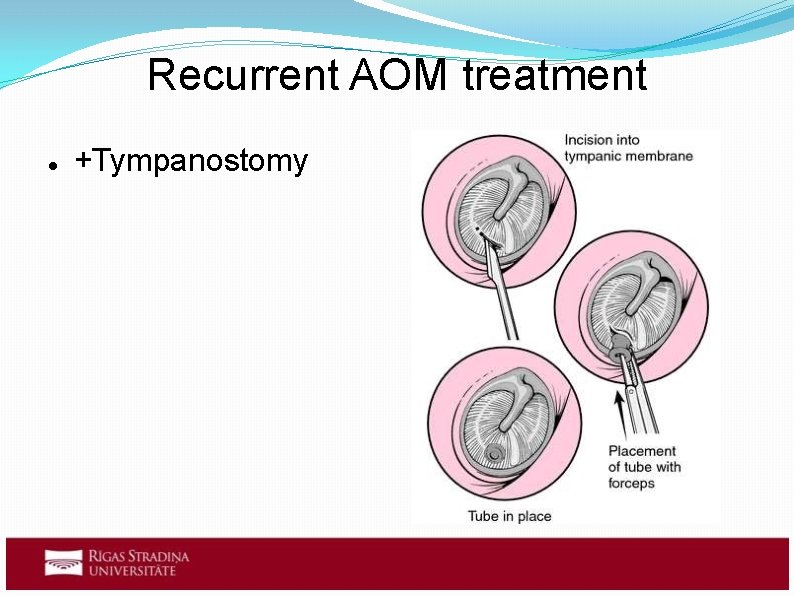
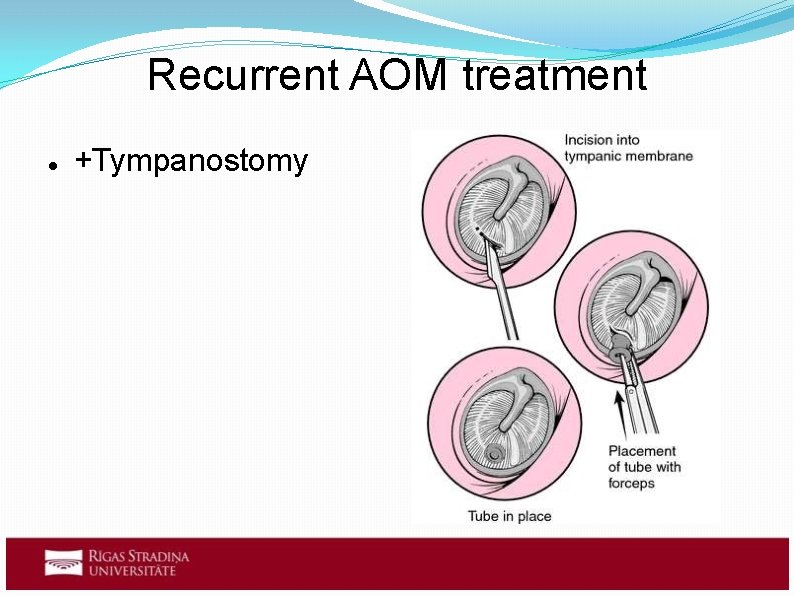
Recurrent AOM treatment +Tympanostomy
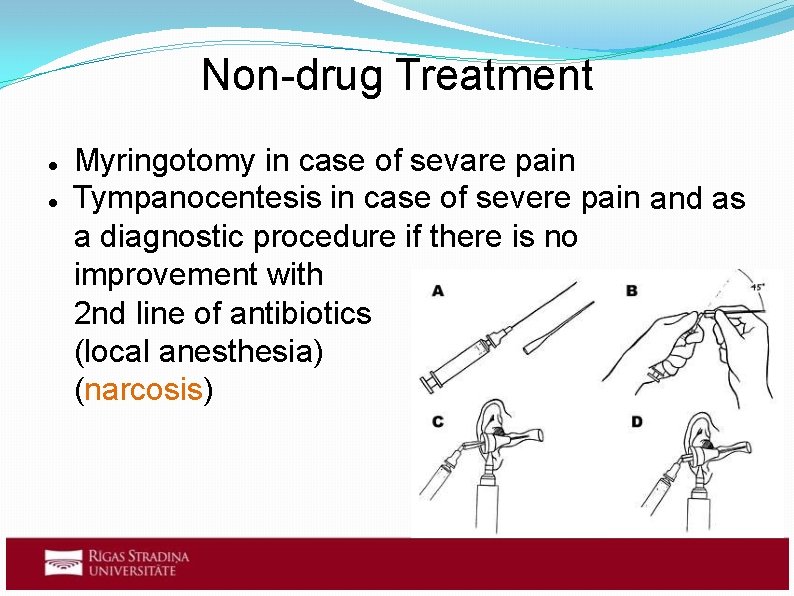
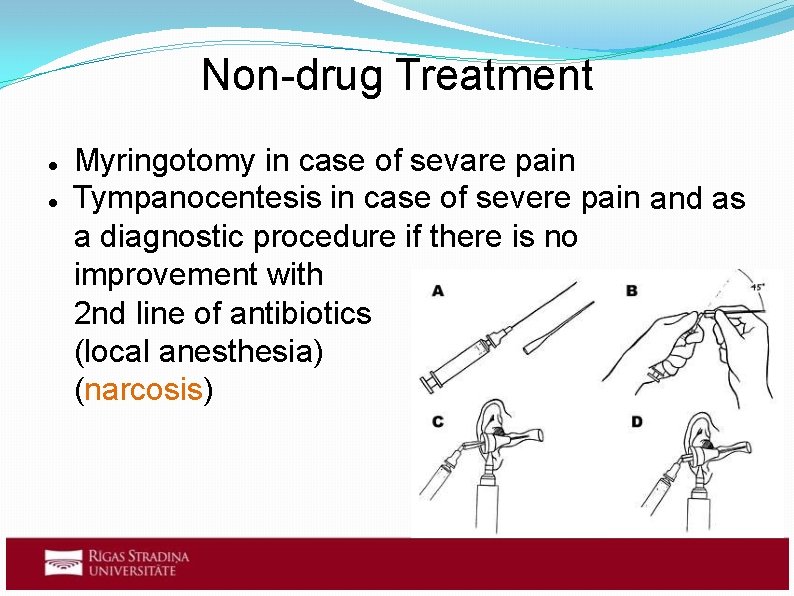
Non-drug Treatment Myringotomy in case of sevare pain Tympanocentesis in case of severe pain and as a diagnostic procedure if there is no improvement with 2 nd line of antibiotics (local anesthesia) (narcosis)
Preventive measures Avoiding risk factors if possible Vaccination: ? S. Pneumonia � Influenza � • • (PCV-7) Adenoidectomy Polipectomy
Differential diagnosis Otitis externa Impacted cerumen or foreign body in ear Tympanosclerosis Otitis media with effusion Injury of the ear
Sources Shapiro, Nina L. Handbook Of Pediatric Otolaryngology : A Practical Guide For Evaluation And Management Of Pediatric Ear, Nose, And Throat Disorders. Singapore: World Scientific Publishing Company, 2012. e. Book Academic Collection (EBSCOhost). Web. 5 Mar. 2016. https: //www. clinicalkey. com. db. rsu. lv/#!/content/medical_topic/21 -s 2. 01014193? scroll. To=%23 heading 0 http: //web. a. ebscohost. com. db. rsu. lv/dynamed/detail? vid=2&sid=74 b 4 f a 24 -4 f 97 -43 f 1 -a 411581 c 0 fcc 826 e%40 sessionmgr 4003&hid=4204&bdata=Jn. Npd. GU 9 ZHlu YW 1 l. ZC 1 sa. XZl. Jn. Njb 3 Bl. PXNpd. GU%3 d#AN=116345&db=dme https: //www. clinicalkey. com. db. rsu. lv/#!/content/book/3 -s 2. 0 B 9780323079327000247? scroll. To=%23 hl 0001072 https: //www. clinicalkey. com. db. rsu. lv/#!/content/book/3 -s 2. 0 B 9780323280471005540 http: //www. aafp. org/afp/2007/1201/p 1650. html http: //journals. plos. org/plosone/article? id=10. 1371/journal. pone. 00362 26 http: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 153141/