5 2 1 Almost None Lets Make Delawares













- Slides: 67
5 -2 -1 -Almost None Let’s Make Delaware’s Kids the Healthiest in the Nation
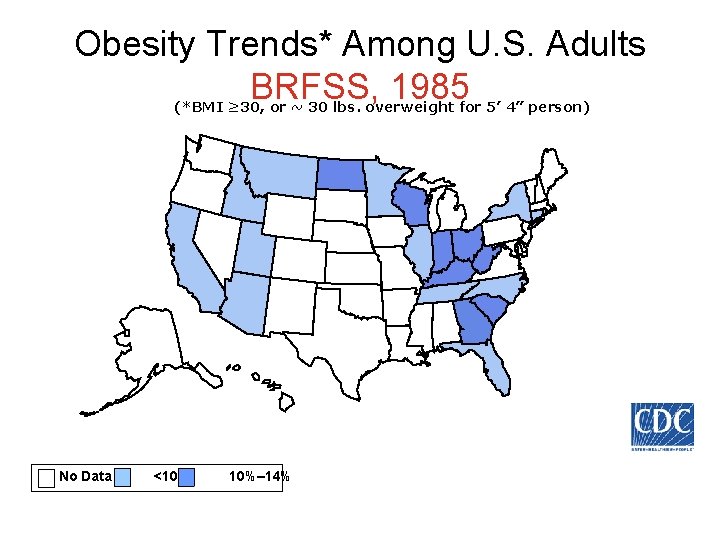
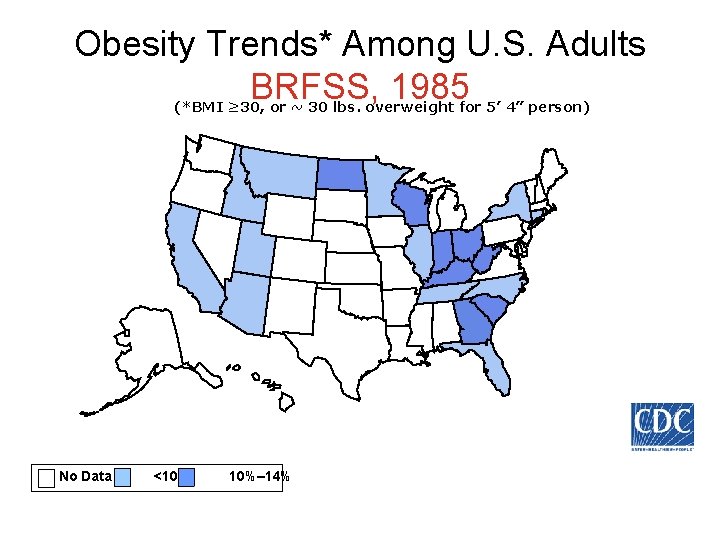
Obesity Trends* Among U. S. Adults BRFSS, 1985 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
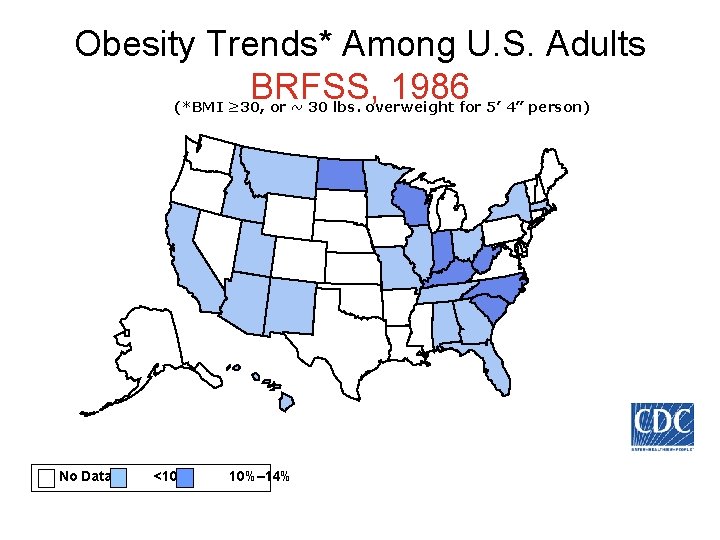
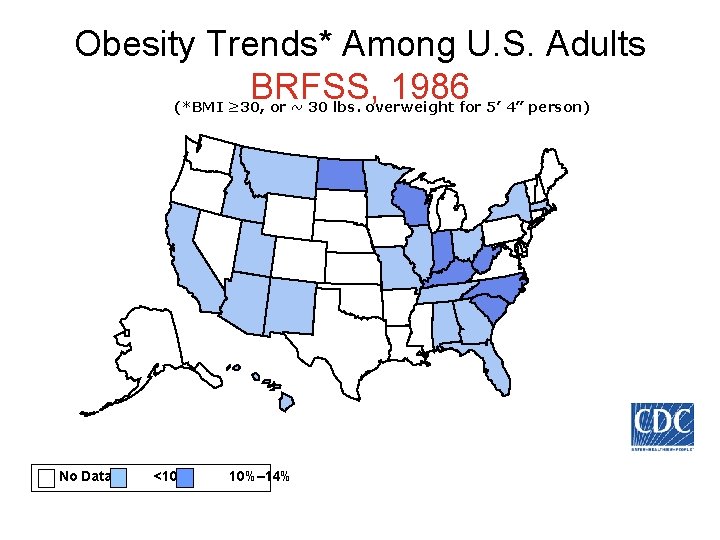
Obesity Trends* Among U. S. Adults BRFSS, 1986 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
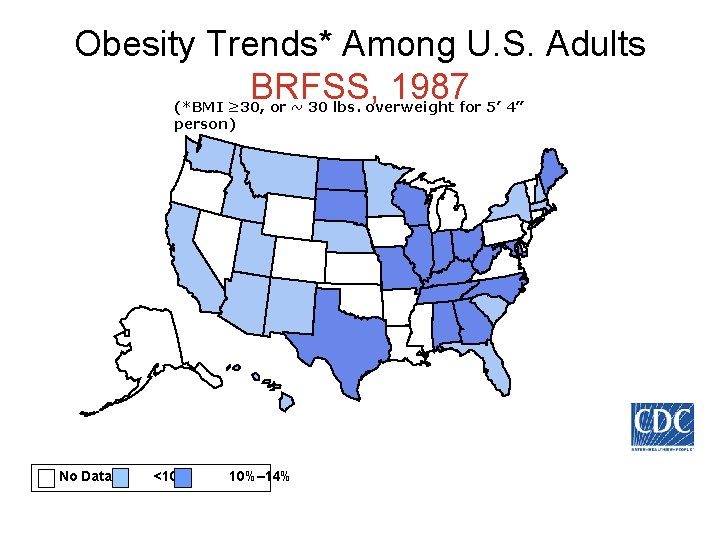
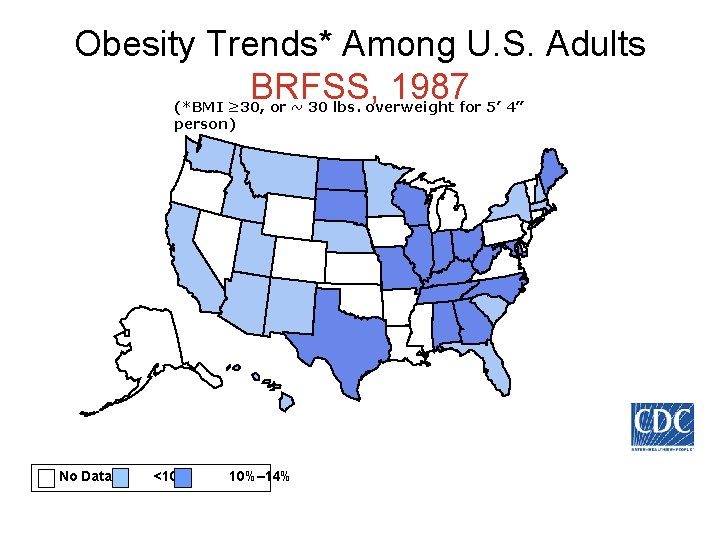
Obesity Trends* Among U. S. Adults BRFSS, 1987 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
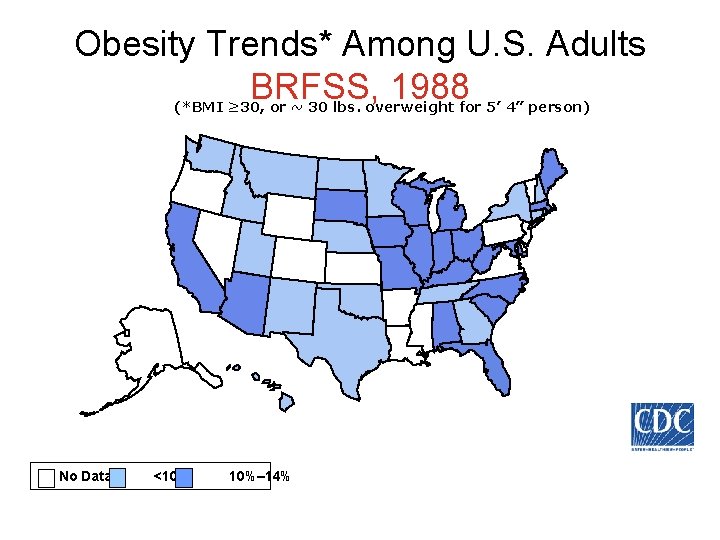
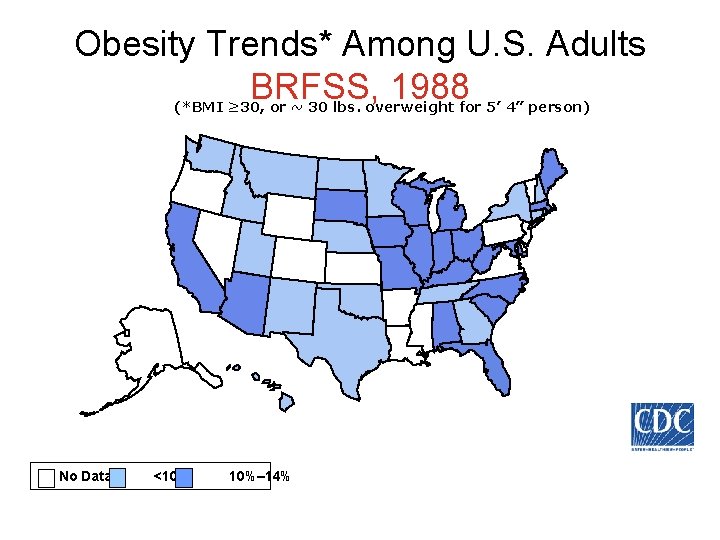
Obesity Trends* Among U. S. Adults BRFSS, 1988 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
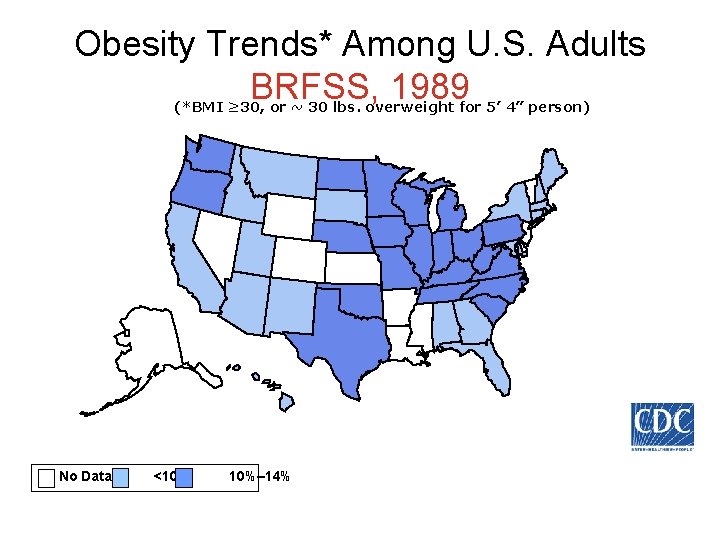
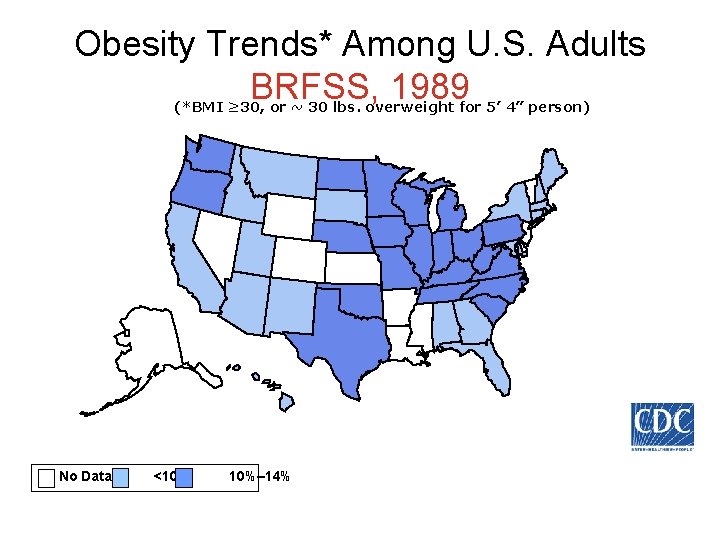
Obesity Trends* Among U. S. Adults BRFSS, 1989 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
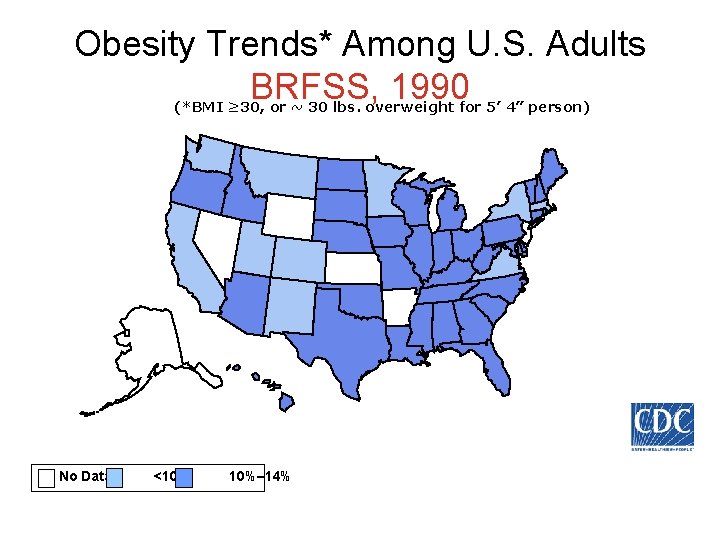
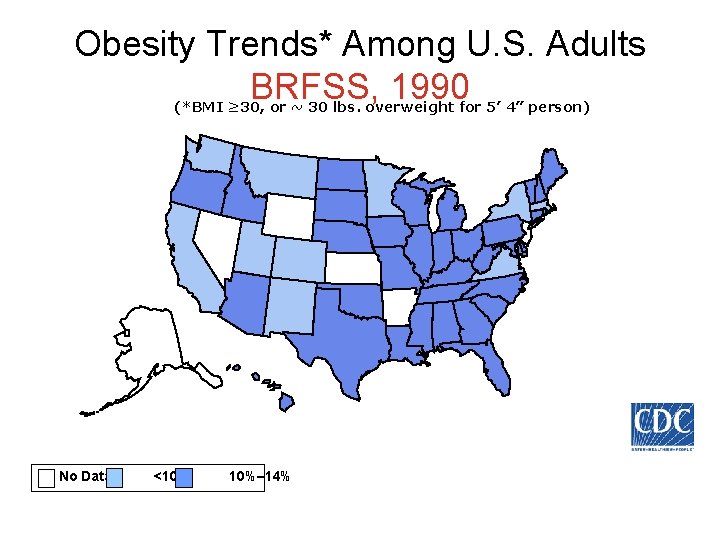
Obesity Trends* Among U. S. Adults BRFSS, 1990 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14%
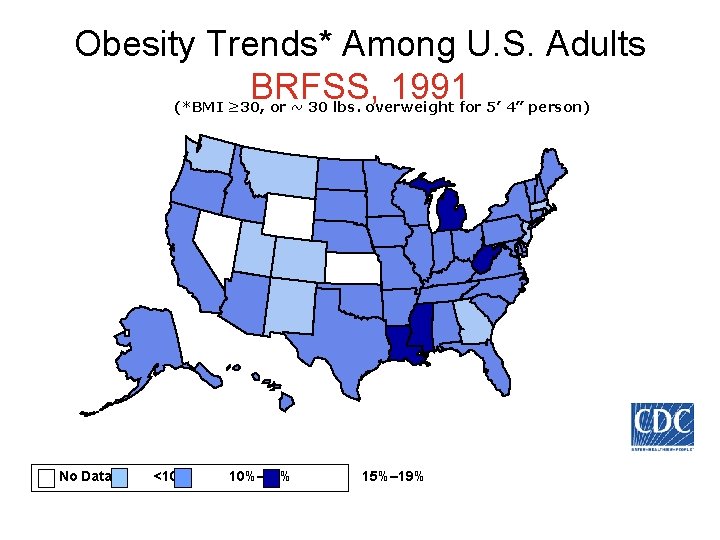
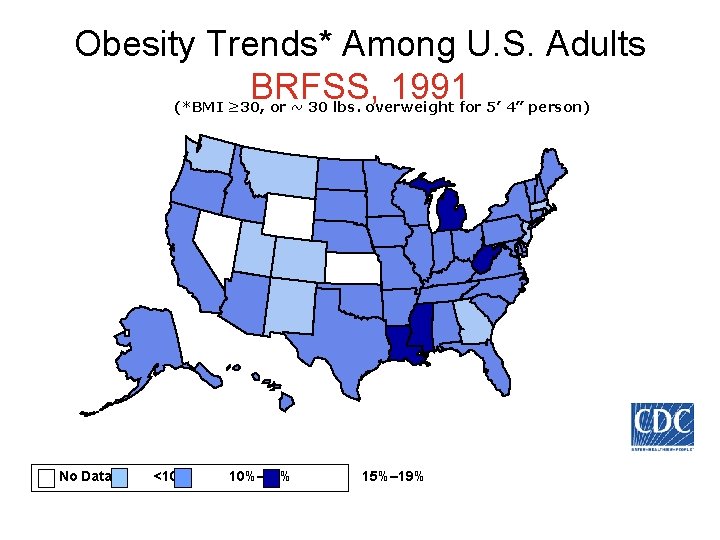
Obesity Trends* Among U. S. Adults BRFSS, 1991 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
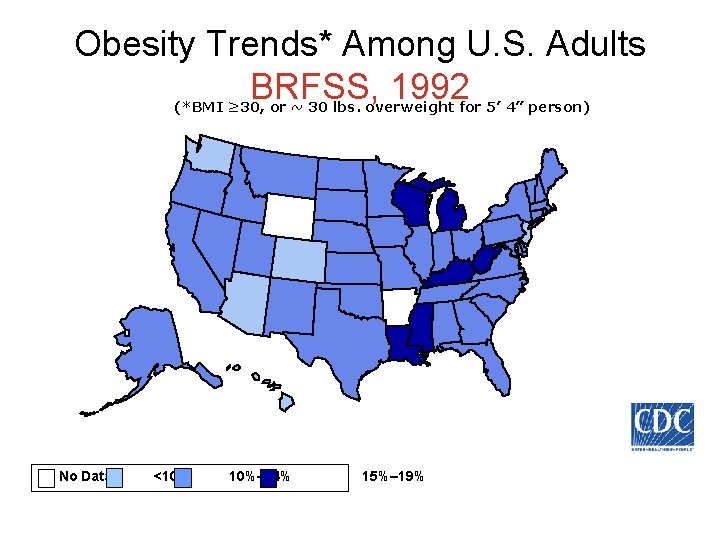
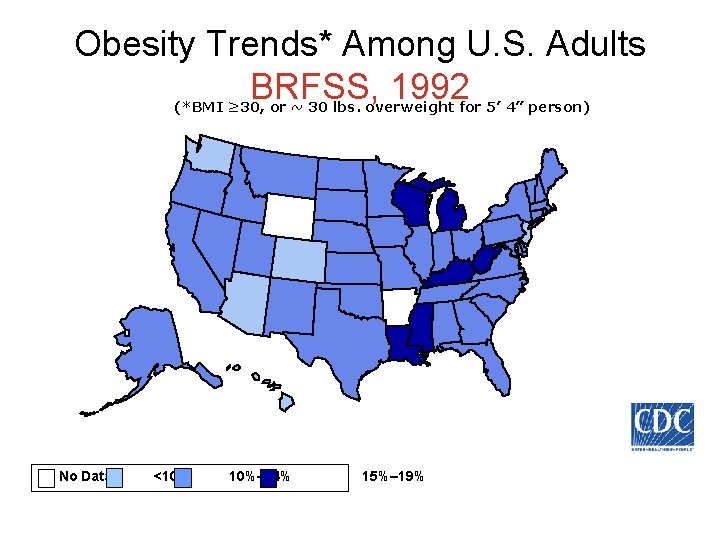
Obesity Trends* Among U. S. Adults BRFSS, 1992 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
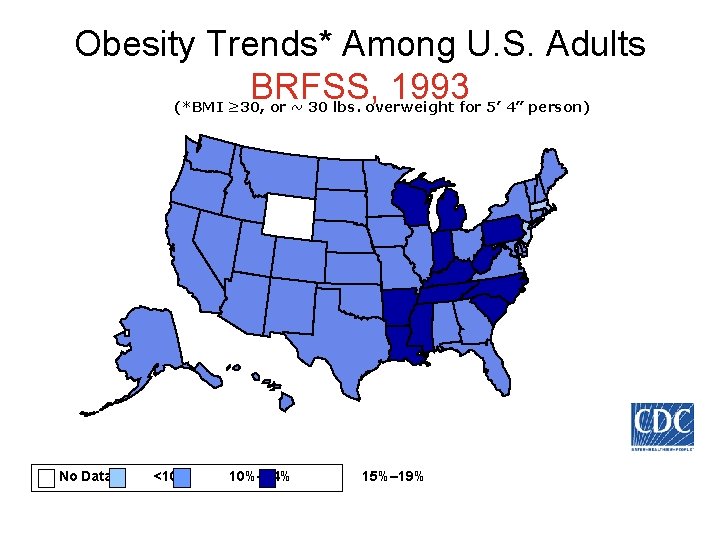
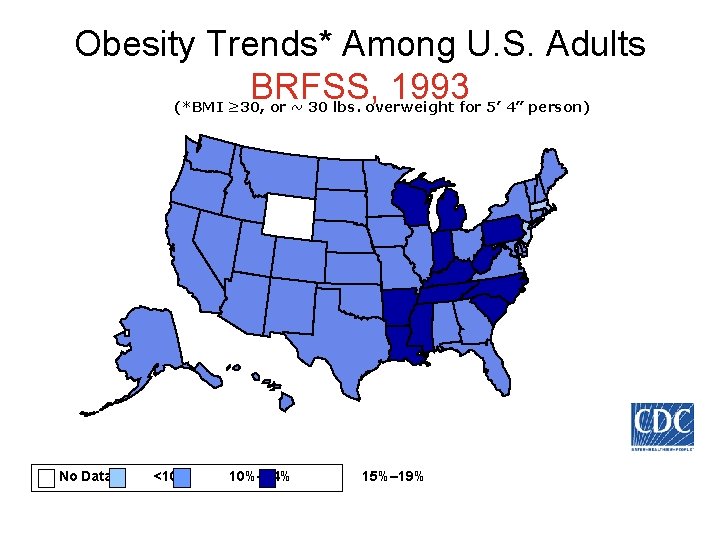
Obesity Trends* Among U. S. Adults BRFSS, 1993 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
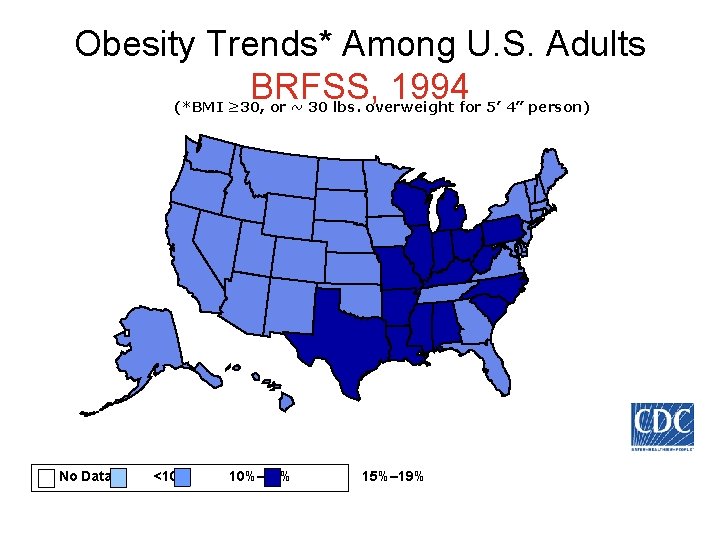
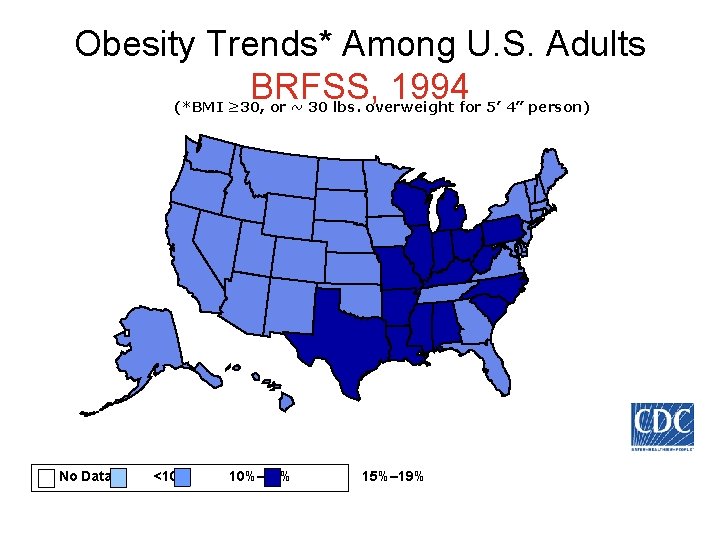
Obesity Trends* Among U. S. Adults BRFSS, 1994 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
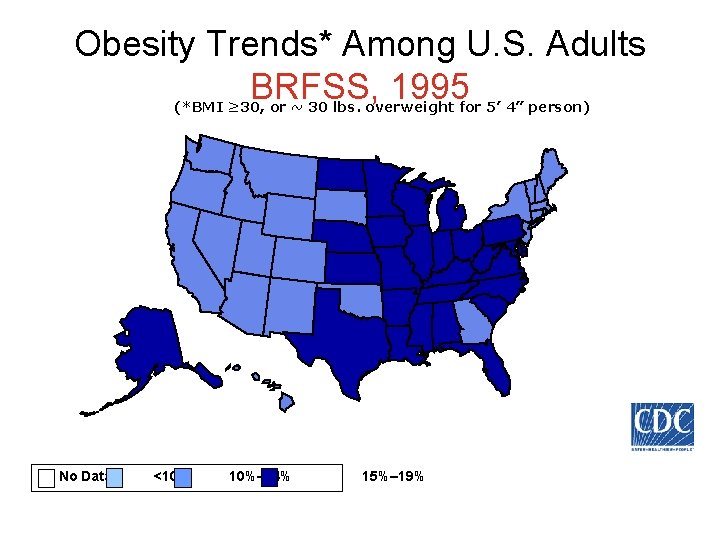
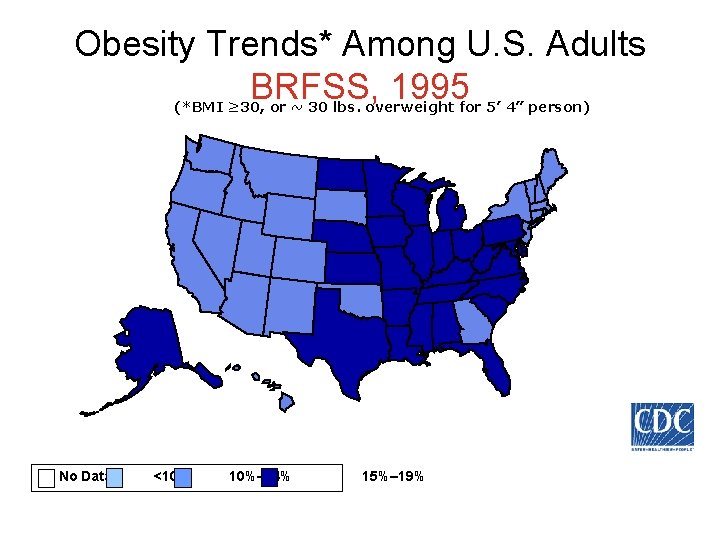
Obesity Trends* Among U. S. Adults BRFSS, 1995 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
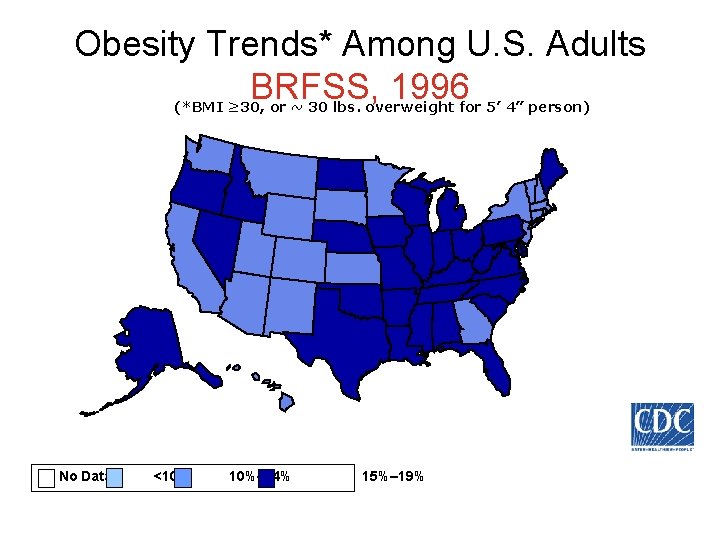
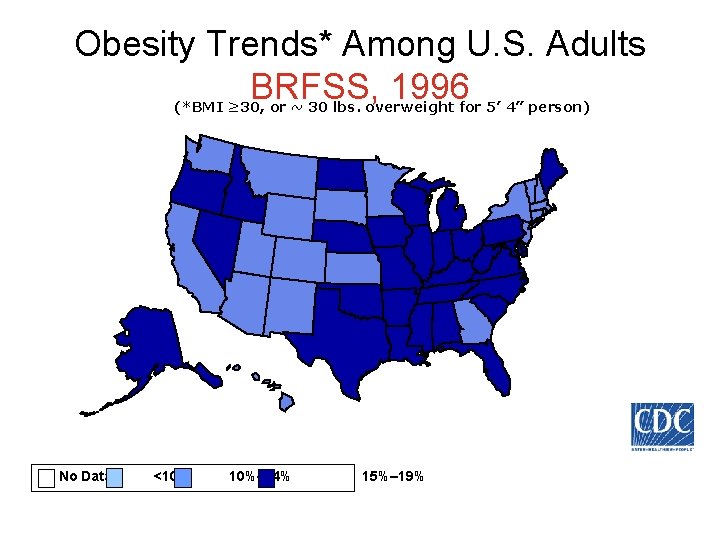
Obesity Trends* Among U. S. Adults BRFSS, 1996 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19%
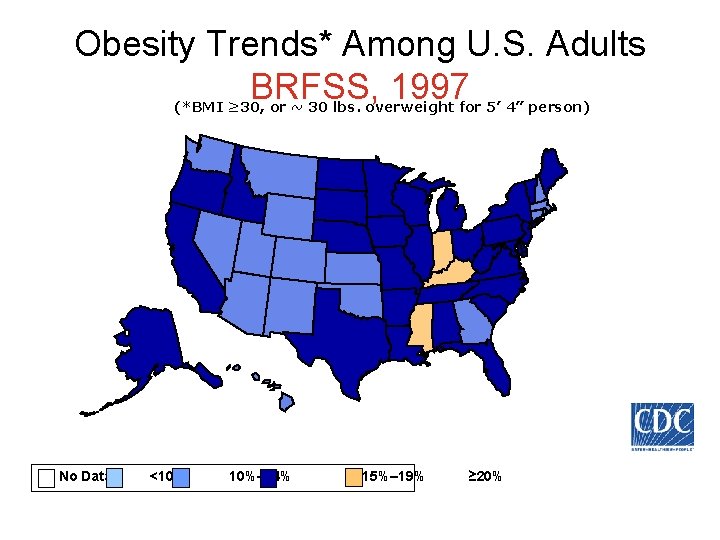
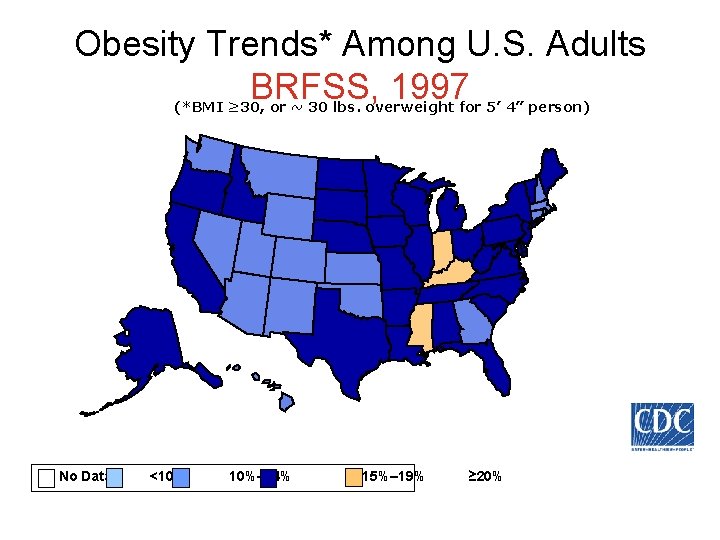
Obesity Trends* Among U. S. Adults BRFSS, 1997 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
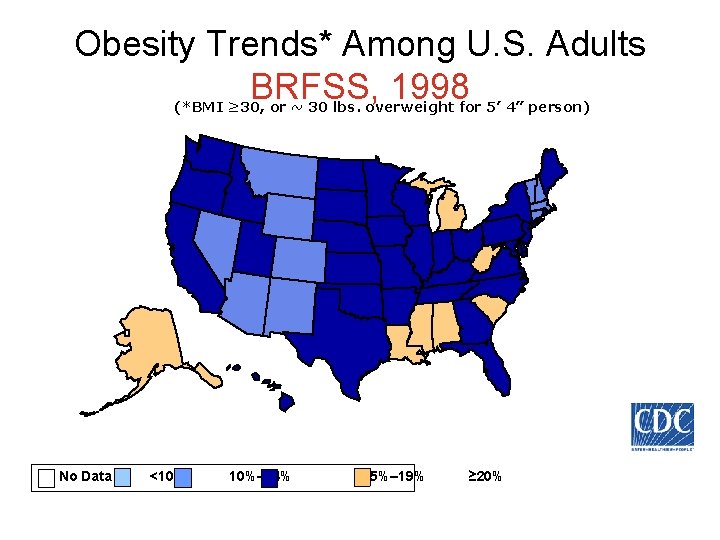
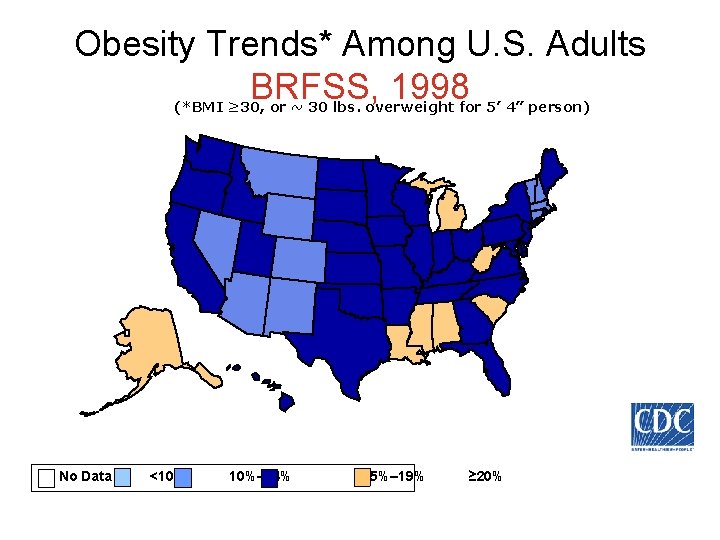
Obesity Trends* Among U. S. Adults BRFSS, 1998 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
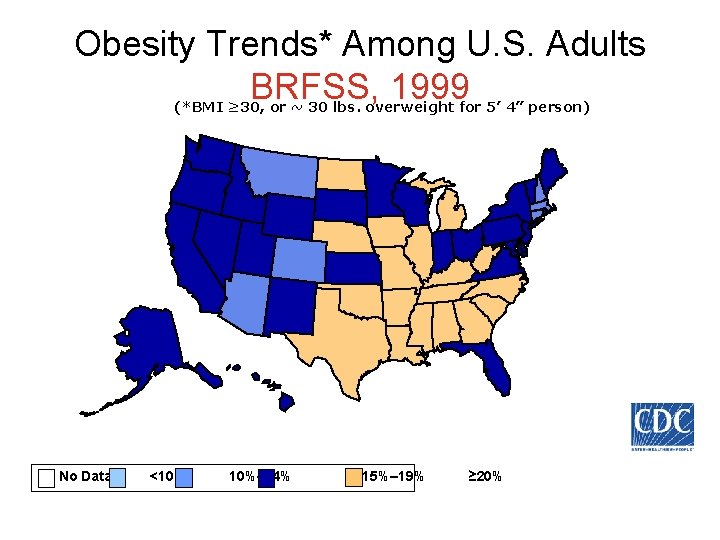
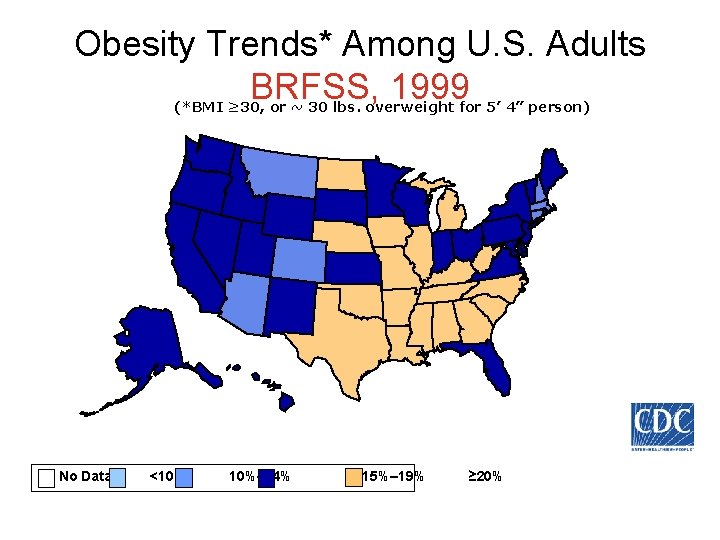
Obesity Trends* Among U. S. Adults BRFSS, 1999 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
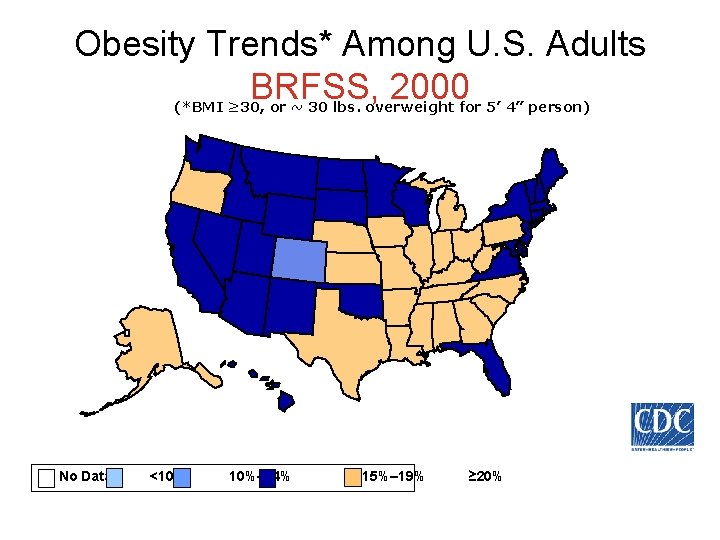
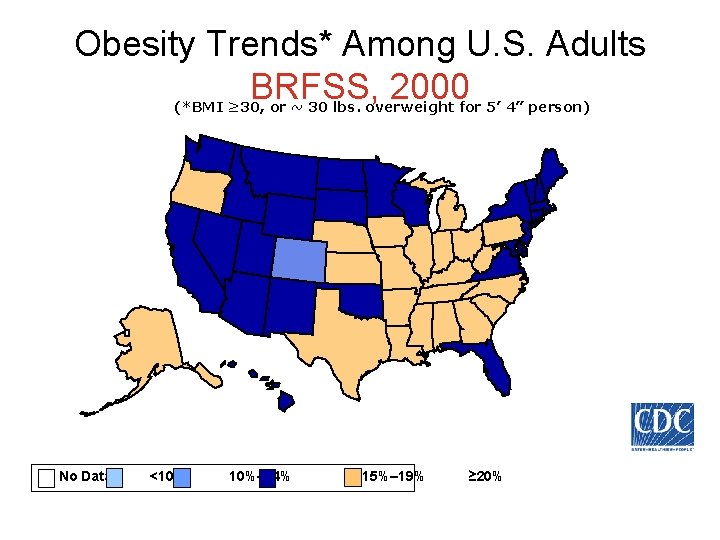
Obesity Trends* Among U. S. Adults BRFSS, 2000 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% ≥ 20%
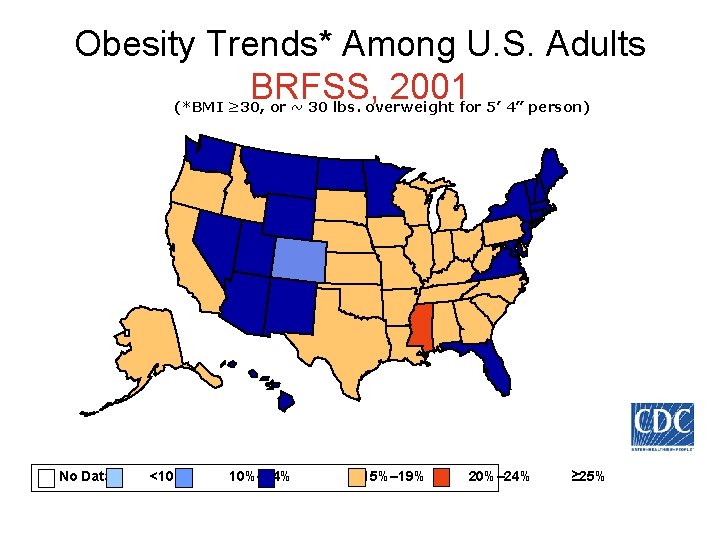
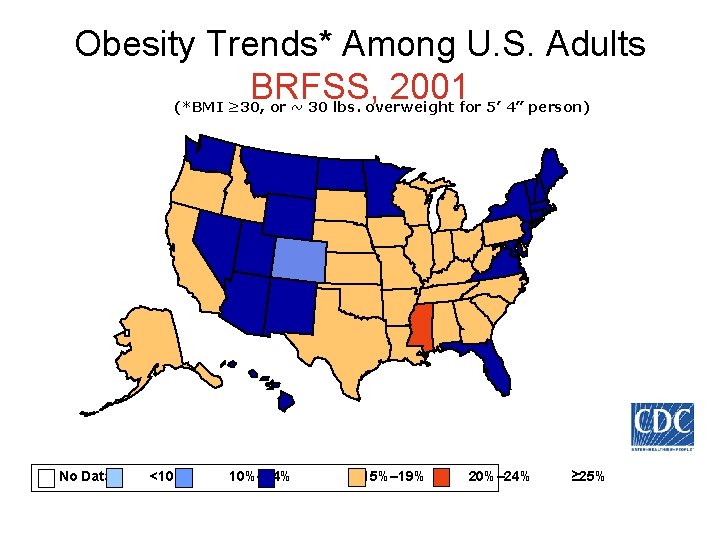
Obesity Trends* Among U. S. Adults BRFSS, 2001 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
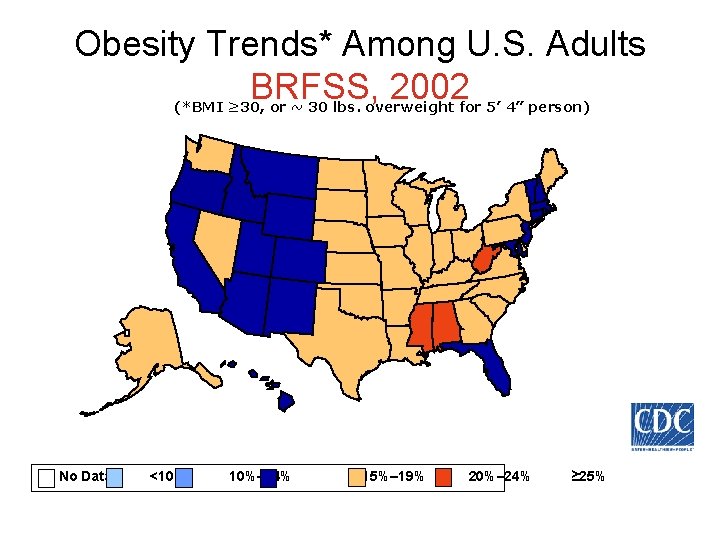
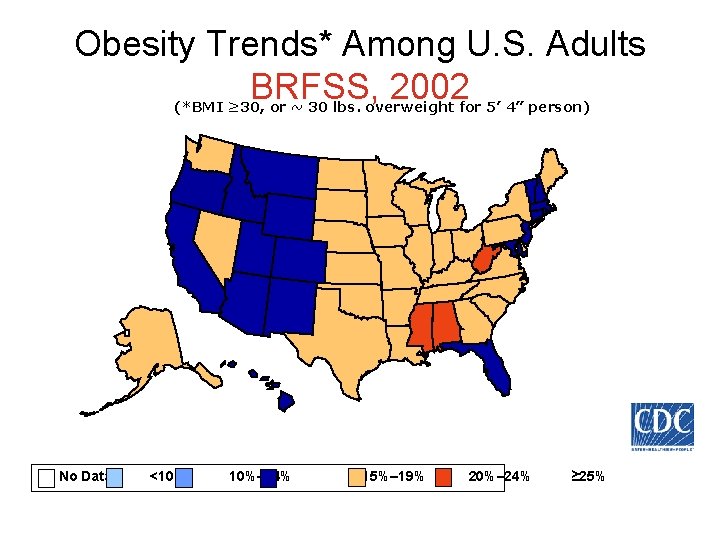
Obesity Trends* Among U. S. Adults BRFSS, 2002 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
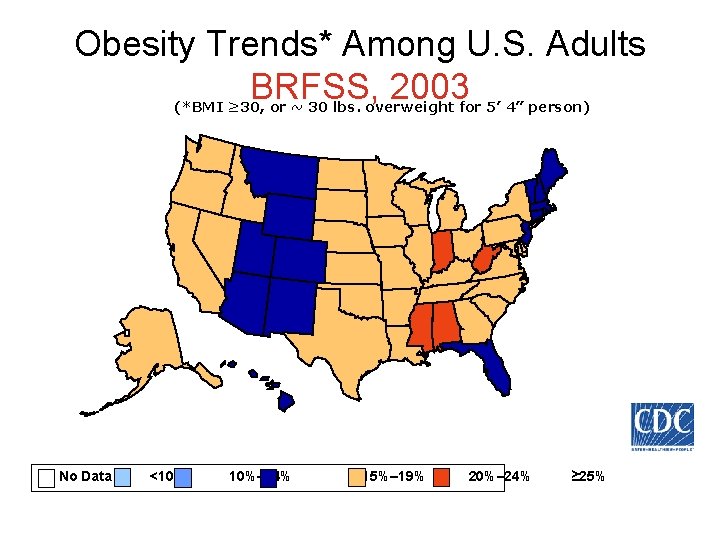
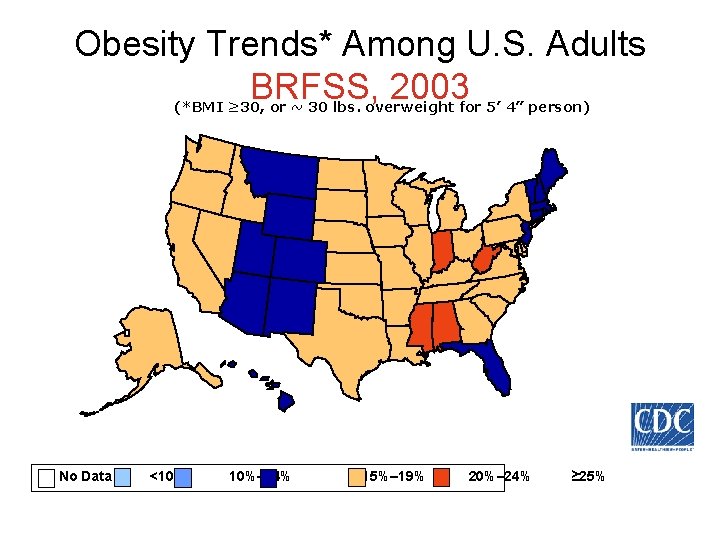
Obesity Trends* Among U. S. Adults BRFSS, 2003 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
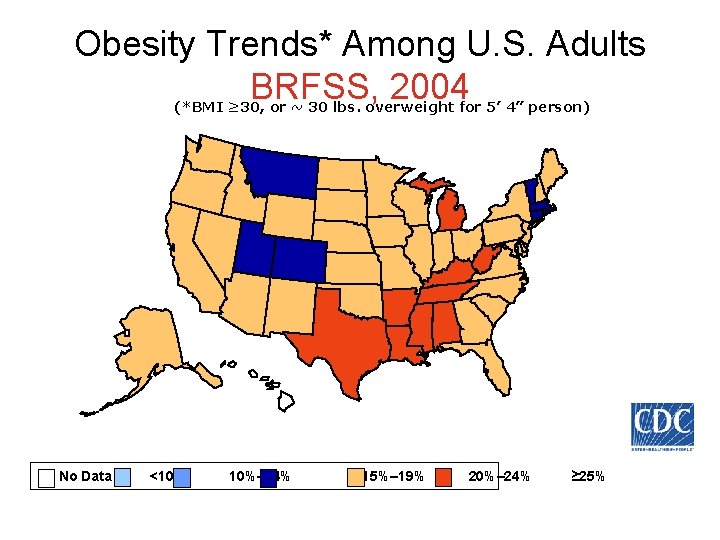
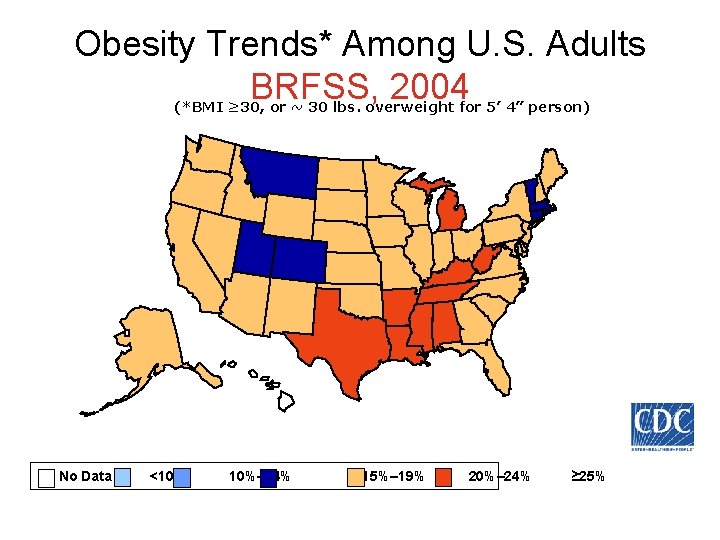
Obesity Trends* Among U. S. Adults BRFSS, 2004 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 10%– 14% 15%– 19% 20%– 24% ≥ 25%
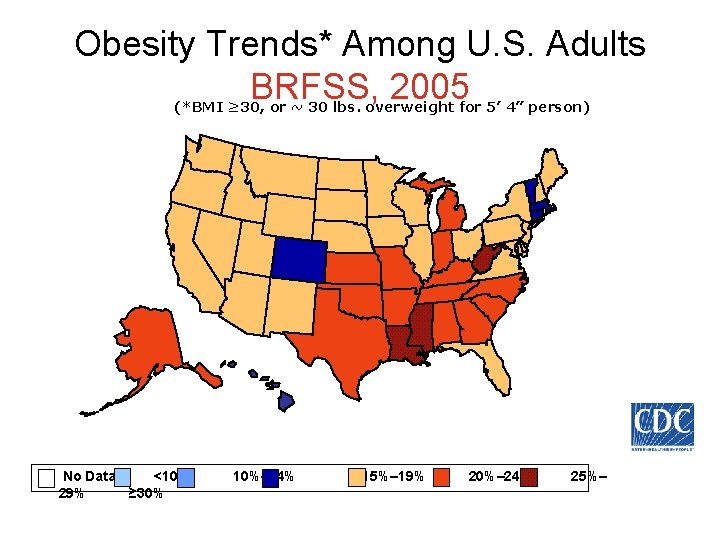
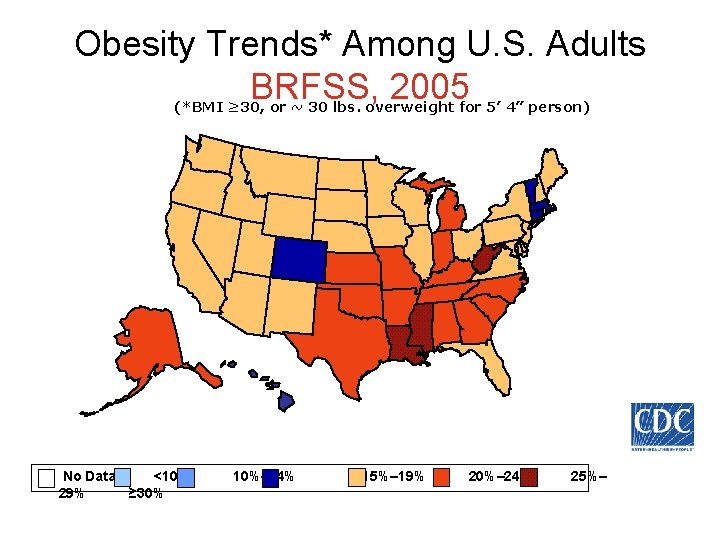
Obesity Trends* Among U. S. Adults BRFSS, 2005 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–
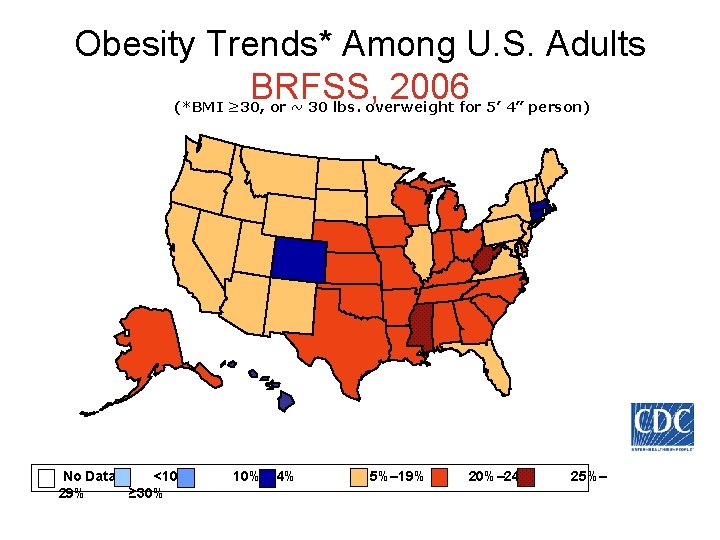
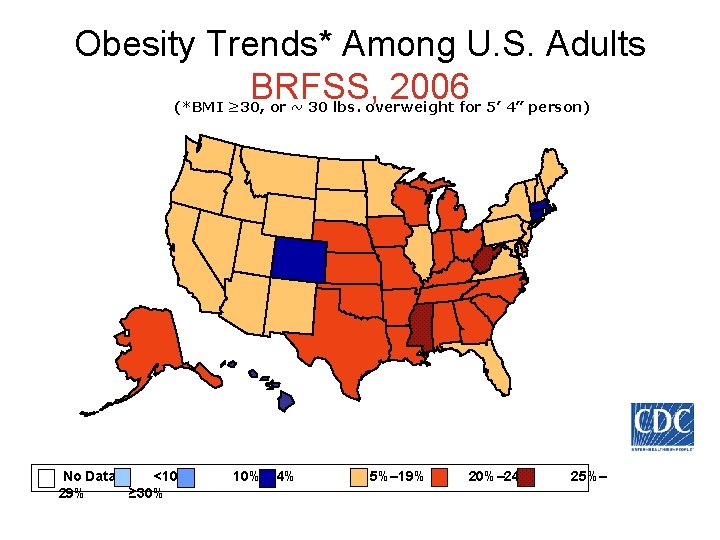
Obesity Trends* Among U. S. Adults BRFSS, 2006 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–
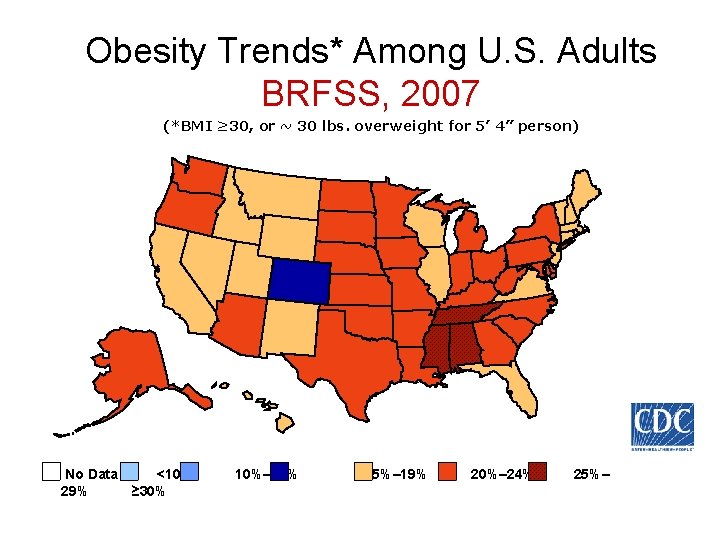
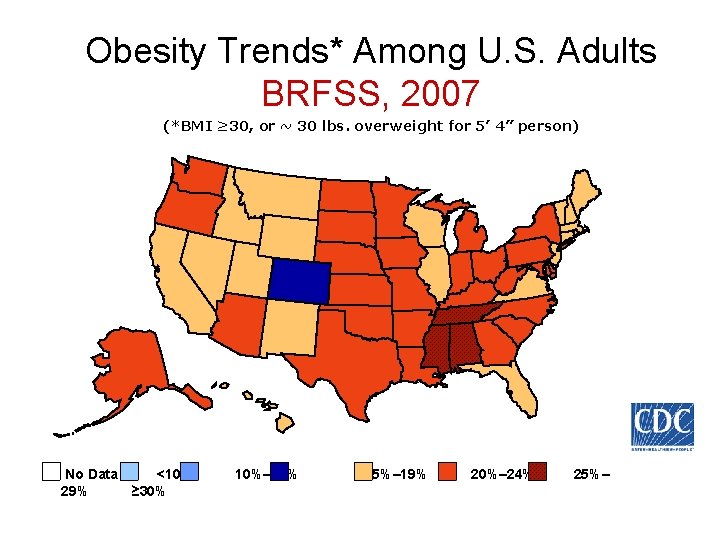
Obesity Trends* Among U. S. Adults BRFSS, 2007 (*BMI ≥ 30, or ~ 30 lbs. overweight for 5’ 4” person) No Data <10% 29% ≥ 30% 10%– 14% 15%– 19% 20%– 24% 25%–
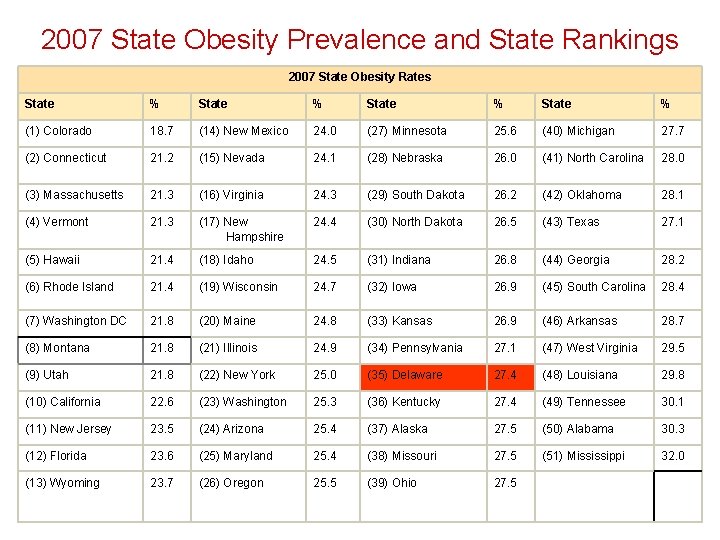
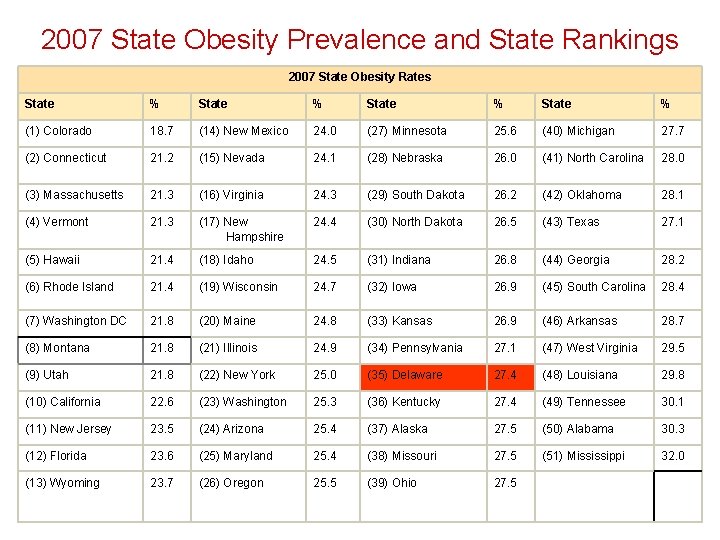
2007 State Obesity Prevalence and State Rankings 2007 State Obesity Rates State % (1) Colorado 18. 7 (14) New Mexico 24. 0 (27) Minnesota 25. 6 (40) Michigan 27. 7 (2) Connecticut 21. 2 (15) Nevada 24. 1 (28) Nebraska 26. 0 (41) North Carolina 28. 0 (3) Massachusetts 21. 3 (16) Virginia 24. 3 (29) South Dakota 26. 2 (42) Oklahoma 28. 1 (4) Vermont 21. 3 (17) New Hampshire 24. 4 (30) North Dakota 26. 5 (43) Texas 27. 1 (5) Hawaii 21. 4 (18) Idaho 24. 5 (31) Indiana 26. 8 (44) Georgia 28. 2 (6) Rhode Island 21. 4 (19) Wisconsin 24. 7 (32) Iowa 26. 9 (45) South Carolina 28. 4 (7) Washington DC 21. 8 (20) Maine 24. 8 (33) Kansas 26. 9 (46) Arkansas 28. 7 (8) Montana 21. 8 (21) Illinois 24. 9 (34) Pennsylvania 27. 1 (47) West Virginia 29. 5 (9) Utah 21. 8 (22) New York 25. 0 (35) Delaware 27. 4 (48) Louisiana 29. 8 (10) California 22. 6 (23) Washington 25. 3 (36) Kentucky 27. 4 (49) Tennessee 30. 1 (11) New Jersey 23. 5 (24) Arizona 25. 4 (37) Alaska 27. 5 (50) Alabama 30. 3 (12) Florida 23. 6 (25) Maryland 25. 4 (38) Missouri 27. 5 (51) Mississippi 32. 0 (13) Wyoming 23. 7 (26) Oregon 25. 5 (39) Ohio 27. 5
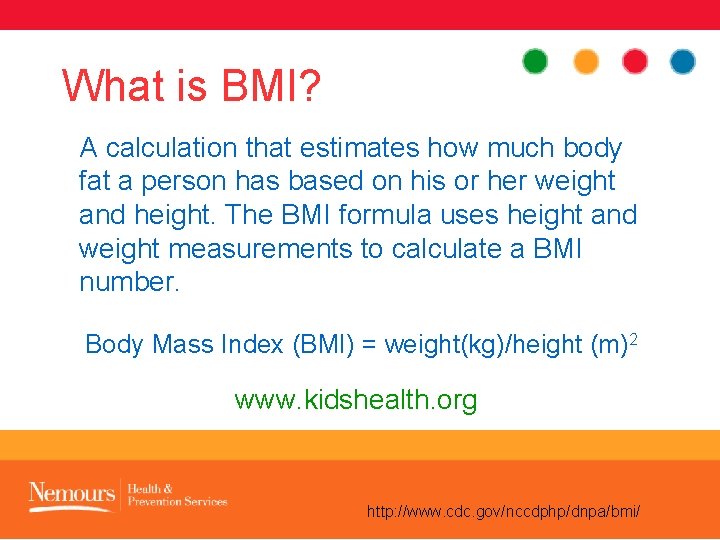
What is BMI? A calculation that estimates how much body fat a person has based on his or her weight and height. The BMI formula uses height and weight measurements to calculate a BMI number. Body Mass Index (BMI) = weight(kg)/height (m)2 www. kidshealth. org http: //www. cdc. gov/nccdphp/dnpa/bmi/
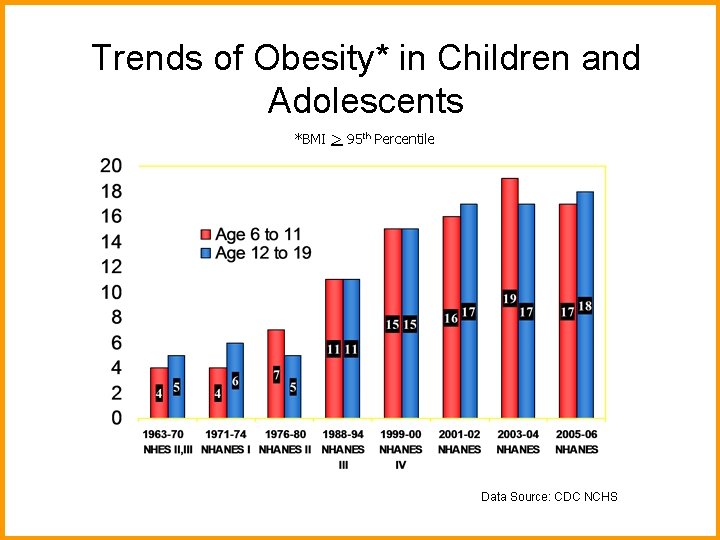
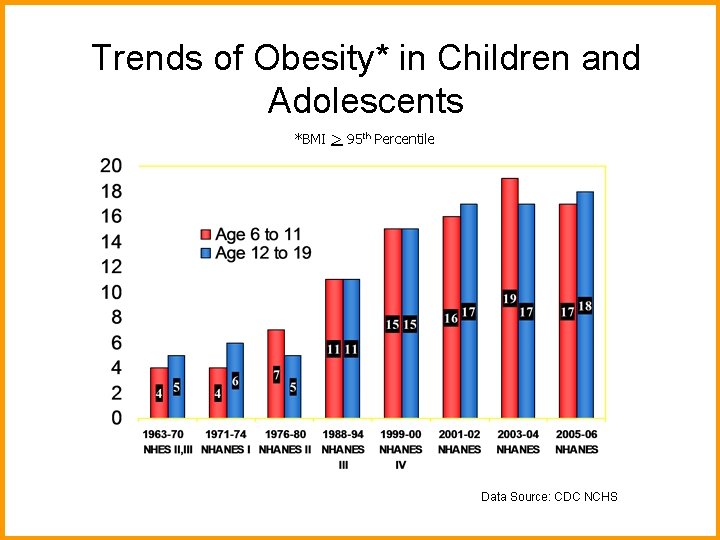
Trends of Obesity* in Children and Adolescents *BMI > 95 th Percentile Data Source: CDC NCHS
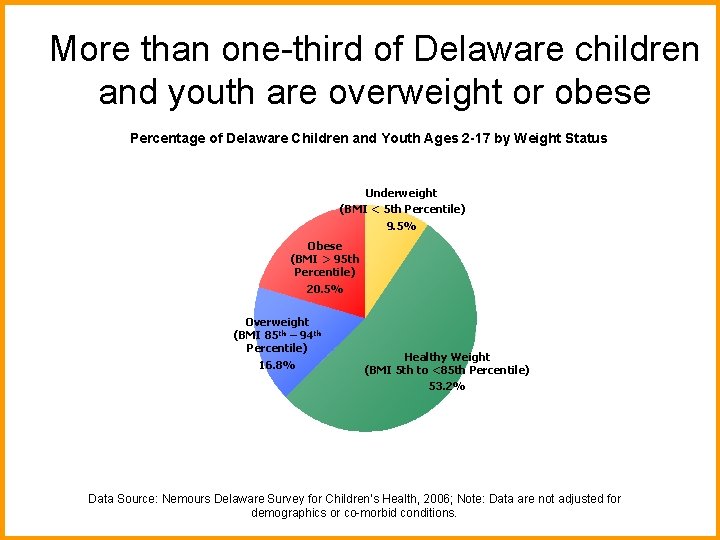
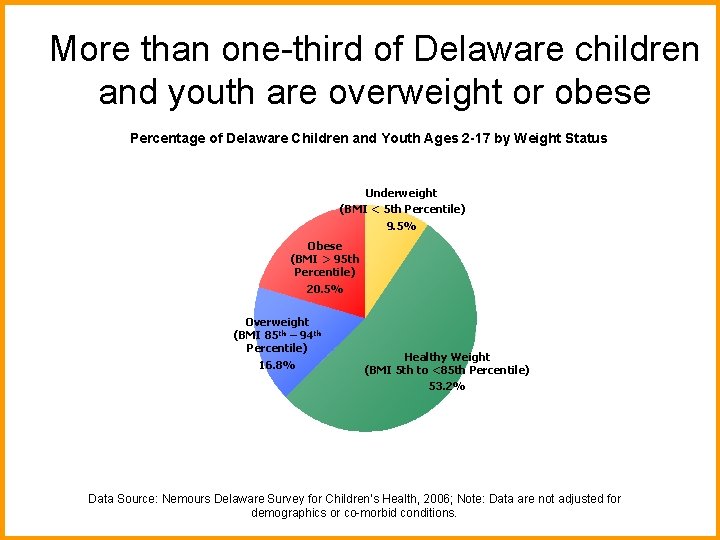
More than one-third of Delaware children and youth are overweight or obese Percentage of Delaware Children and Youth Ages 2 -17 by Weight Status Underweight (BMI < 5 th Percentile) 9. 5% Obese (BMI > 95 th Obese Percentile) (BMI 20. 5% > 95 th Percentile) 19. 9% Overweight (BMI 85 th – 94 th Percentile) 16. 8% Healthy Weight (BMI 5 th to <85 th Percentile) 53. 2% Healthy Weight (BMI 5 th to <85 th Percentile) 60. 6% Data Source: Nemours Delaware Survey for Children’s Health, 2006; Note: Data are not adjusted for demographics or co-morbid conditions.
What is BMI? A calculation that estimates how much body fat a person has based on his or her weight and height. The BMI formula uses height and weight measurements to calculate a BMI number. Body Mass Index (BMI) = weight(kg)/height (m)2 www. kidshealth. org http: //www. cdc. gov/nccdphp/dnpa/bmi/
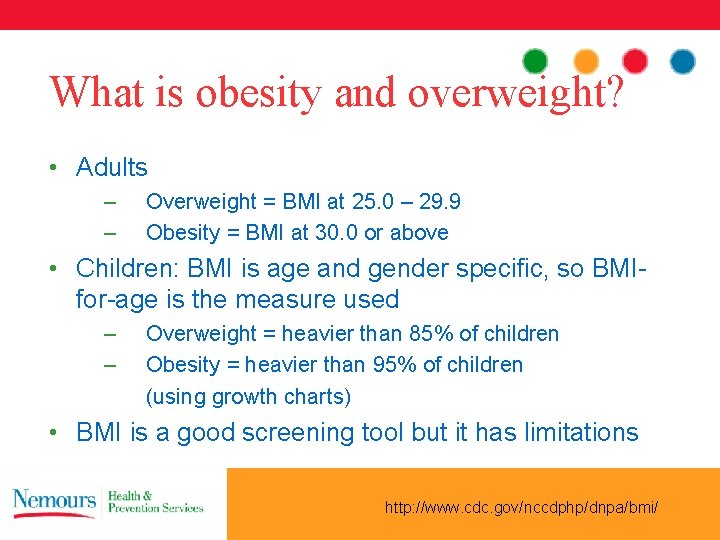
What is obesity and overweight? • Adults – – Overweight = BMI at 25. 0 – 29. 9 Obesity = BMI at 30. 0 or above • Children: BMI is age and gender specific, so BMIfor-age is the measure used – – Overweight = heavier than 85% of children Obesity = heavier than 95% of children (using growth charts) • BMI is a good screening tool but it has limitations http: //www. cdc. gov/nccdphp/dnpa/bmi/

Consequences of childhood and adolescent obesity • Discrimination • Anxiety • Persistence into adulthood • Asthma • Abnormal cholesterol • Sleep problems • High Blood Pressure • Earlier maturation • Type 2 diabetes • Reproductive problems • Liver and Gallbladder Disease • Bone complications • Depression
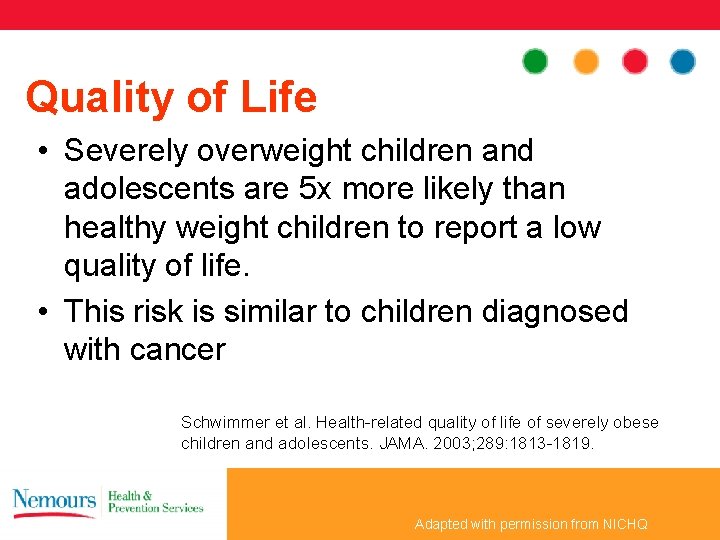
Quality of Life • Severely overweight children and adolescents are 5 x more likely than healthy weight children to report a low quality of life. • This risk is similar to children diagnosed with cancer Schwimmer et al. Health-related quality of life of severely obese children and adolescents. JAMA. 2003; 289: 1813 -1819. Adapted with permission from NICHQ
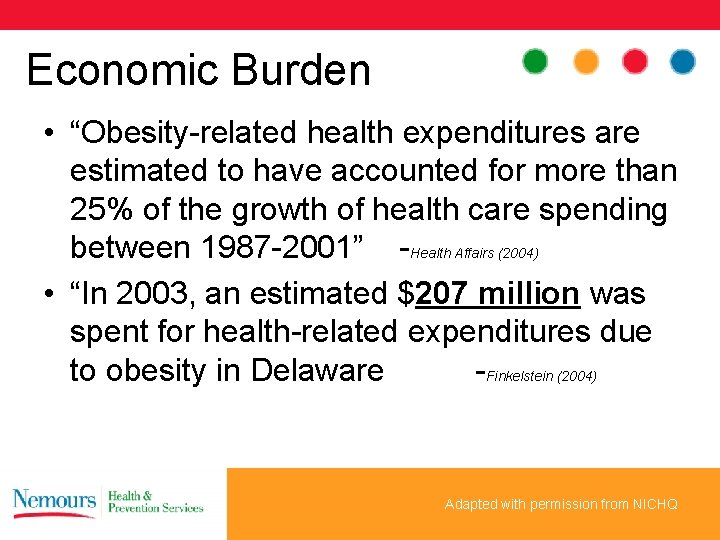
Economic Burden • “Obesity-related health expenditures are estimated to have accounted for more than 25% of the growth of health care spending between 1987 -2001” -Health Affairs (2004) • “In 2003, an estimated $207 million was spent for health-related expenditures due to obesity in Delaware -Finkelstein (2004) Adapted with permission from NICHQ

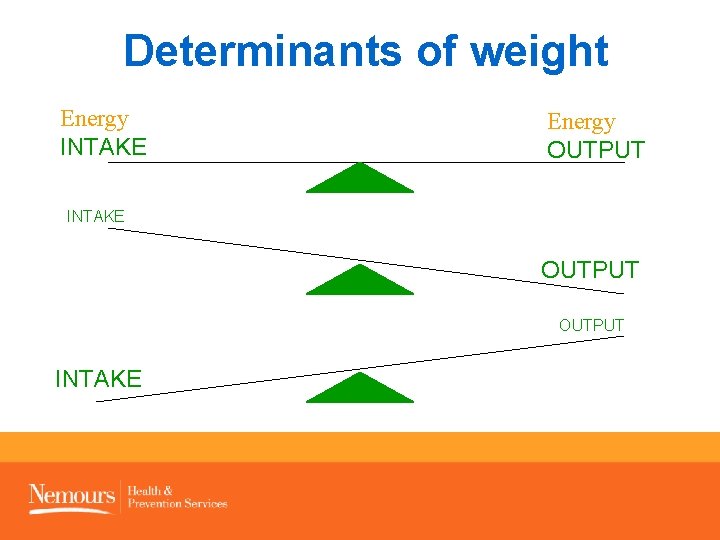
What are the causes of obesity? • More calories eaten • Less physical activity • More inactivity
The New Social Norm?
Sugar and fat: cheap and abundant
Food environment

Vending Machines

Fast Food

Food marketing to children
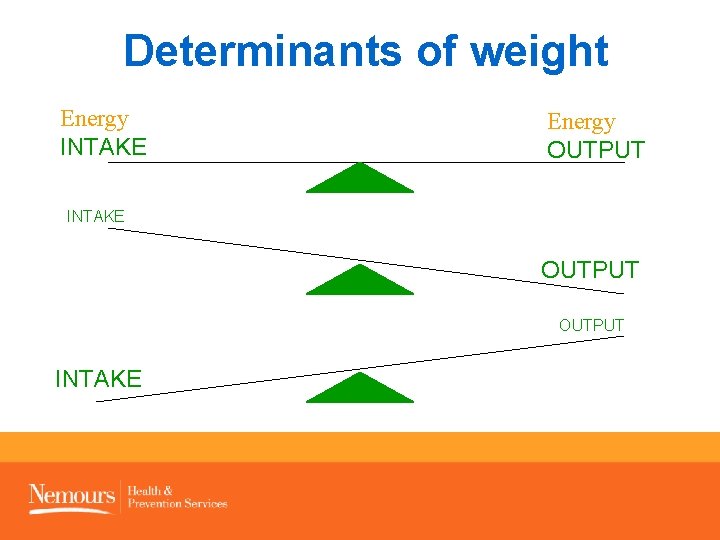
Determinants of weight Energy INTAKE Energy OUTPUT INTAKE
What do we know? • No single culprit • No magic bullet • MODERATION—such a boring word! • There are some things we can do…

Children could reduce their risk of preventable disease if: They consumed 5 or more servings of fruits and vegetables each day. They reduced screen time to fewer than 2 hours each day. They engaged in a total of at least 1 hour of physical activity each day. They limited drinks with added sugars, specifically soft drinks, non-100% fruit drinks and sports drinks.

5 -2 -1 -Almost None

5 or more servings of fruits and vegetables per day
What’s a serving? • Fruit: 1 medium whole fruit, ½ cup of cut fruit, ½ cup 100% juice or ¼ cup of dried fruit • Vegetable: 1 cup of leafy vegetables, ½ cup of raw or cooked vegetables or 100% juice • Fresh, frozen or canned? • It is important to eat a variety of colors
Fruits and vegetables: • May help your stomach feel full. • May decrease the chance of becoming overweight • Decrease chance of chronic disease: – Cancer – Heart Disease Dietary Guidelines for Americans, 2005; Rolls, 2004.

Nationwide, only 21. 4% of teens eat 5 fruits and vegetables a day. Source: Youth Risk Behavior Surveillance System, 2007.

Poor dietary patterns are beginning at early stages. • Fruit and vegetable intake in infants and toddlers does not meet national nutrition recommendations. • French fries are one of three most common vegetables fed to infants 9 -11 months. • By 15 -18 months, French fries become the most common vegetable consumed. Fox MK, Pac S, Devaney B, Jankowski L. Feeding infants and toddlers study: what foods are infants and toddlers eating? J Am Diet Assoc. 2004; 104: S 22 -S 30.
2 hours or less of screen time per day
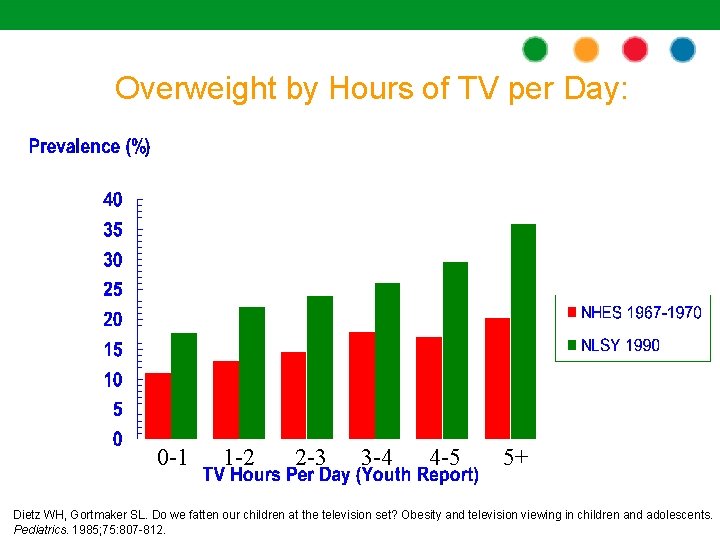
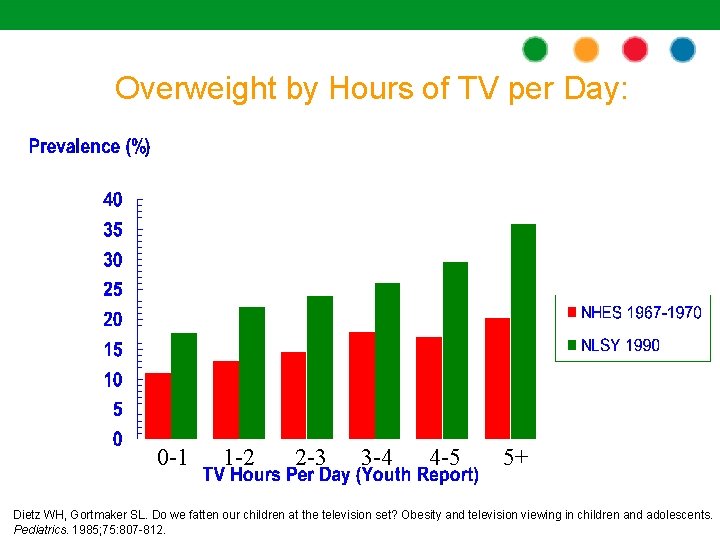
Overweight by Hours of TV per Day: 0 -1 1 -2 2 -3 3 -4 4 -5 5+ Dietz WH, Gortmaker SL. Do we fatten our children at the television set? Obesity and television viewing in children and adolescents. Pediatrics. 1985; 75: 807 -812.
Screen Time and Obesity • Increased snacking and consumption of high caloric foods • Increased exposure to food and beverage advertising • Displacement of physical activity Dietz, 1985; Gortmaker, 1996; Robinson, 2001.
Sedentary Behaviors of Delaware Youth (2007) • 28% played video games, computer games, or used a computer for 3 or more hours a day • 39% watched television for 3 or more hours a day Youth Risk Behavior Surveillance Survey (2007).
TV Can Have Negative Affects On: • Violent and aggressive behavior • Substance use • Sexual activity • Body image • Academic performance American Academy of Pediatrics. Children, adolescents, and television. Pediatrics. 2001; 107: 423 -426.
1 or more hours of physical activity per day
What is physical activity? • Any movement that uses energy • Wide range of physical activities including: – Household: cleaning, raking leaves – Transportation: walking or biking to work – Occupational: lifting boxes – Leisure time: team sports, exercise classes, walking, biking
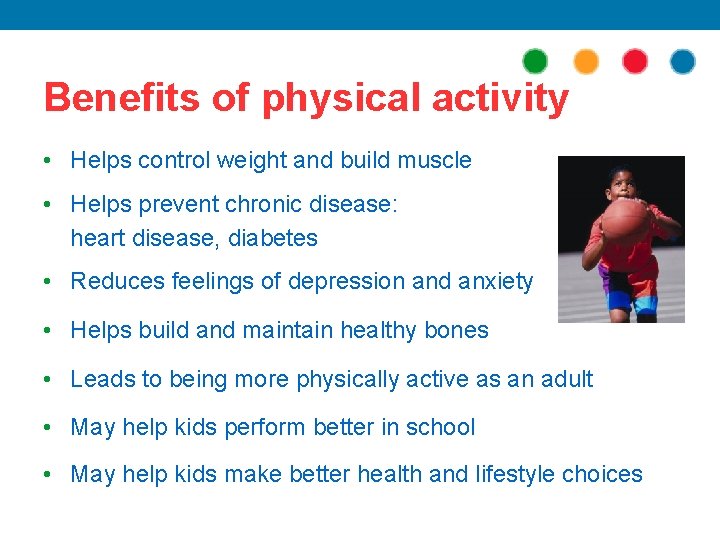
Benefits of physical activity • Helps control weight and build muscle • Helps prevent chronic disease: heart disease, diabetes • Reduces feelings of depression and anxiety • Helps build and maintain healthy bones • Leads to being more physically active as an adult • May help kids perform better in school • May help kids make better health and lifestyle choices
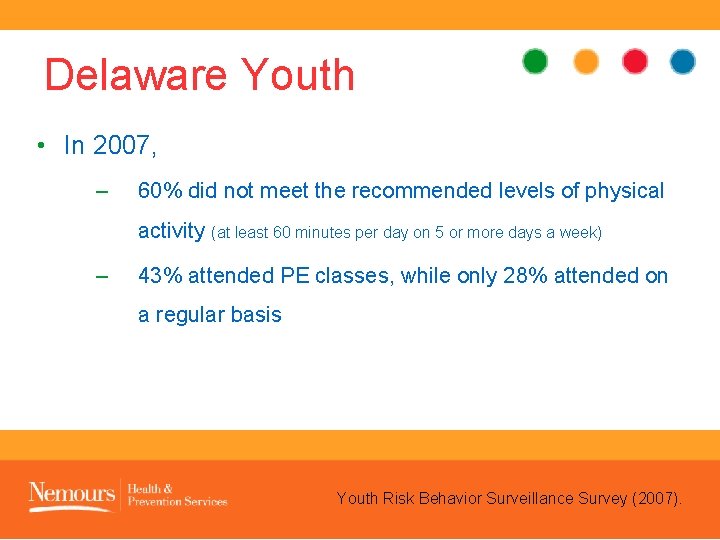
Delaware Youth • In 2007, – 60% did not meet the recommended levels of physical activity (at least 60 minutes per day on 5 or more days a week) – 43% attended PE classes, while only 28% attended on a regular basis Youth Risk Behavior Surveillance Survey (2007).
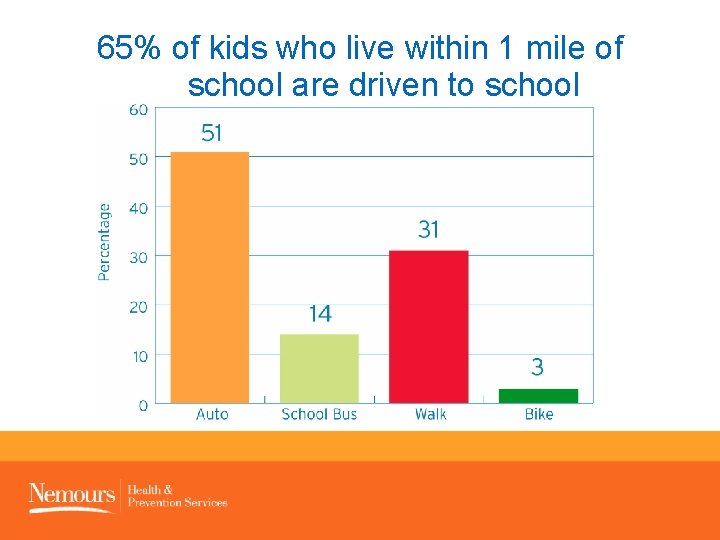
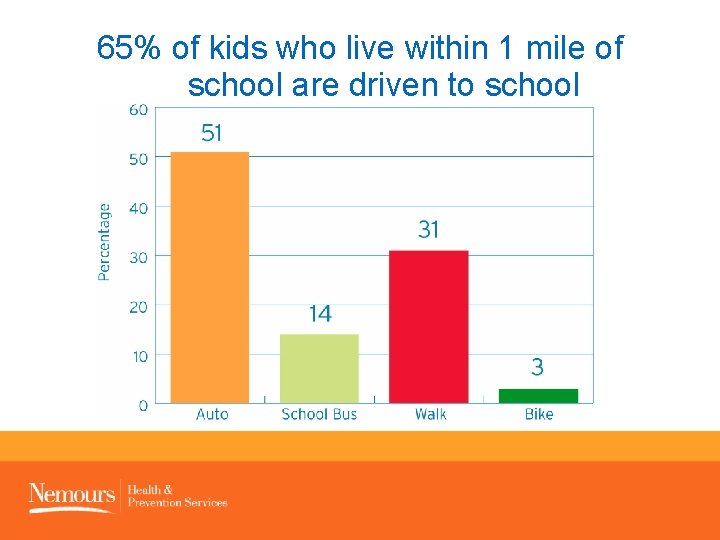
65% of kids who live within 1 mile of school are driven to school


Almost no sugary beverages
Sugary Beverages • Drinks with added sugars – Regular soft drinks, fruit drinks, sweetened teas, and sports drinks. • Contribute to childhood obesity because they are high in sugar and calories • Displace more nutritious drinks that children need to grow, like low-fat milk • Contribute to dental cavities
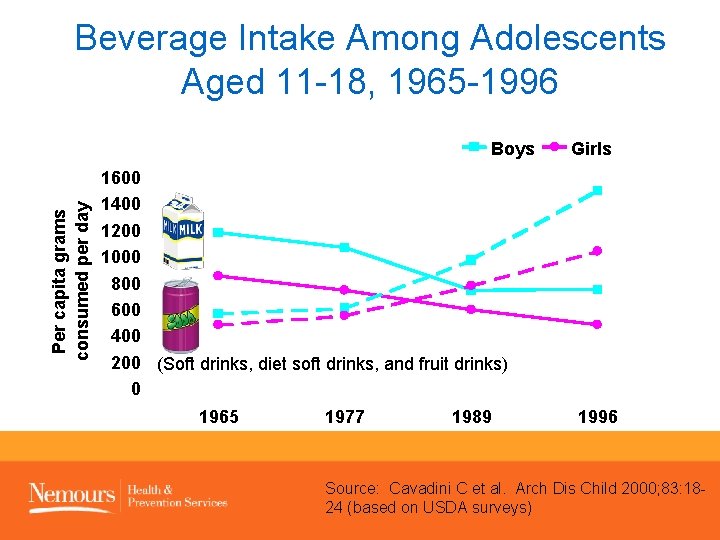
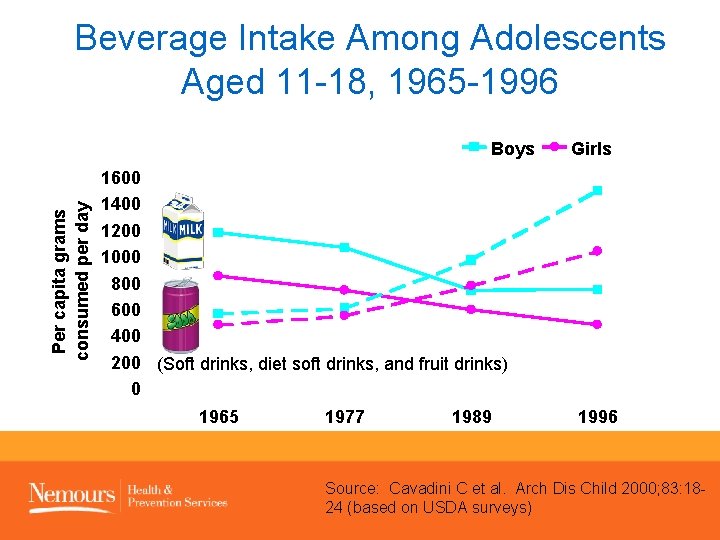
Beverage Intake Among Adolescents Aged 11 -18, 1965 -1996 Per capita grams consumed per day Boys Girls 1600 1400 1200 1000 800 600 400 200 (Soft drinks, diet soft drinks, and fruit drinks) 0 1965 1977 1989 1996 SOURCE: Cavadini C et al. Arch Dis Child 2000; 83: 18 -24 (based on USDA surveys) Source: Cavadini C et al. Arch Dis Child 2000; 83: 1824 (based on USDA surveys)
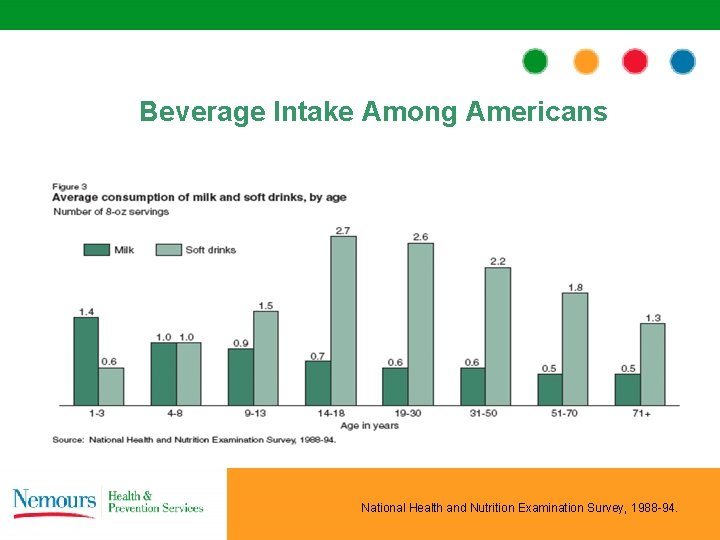
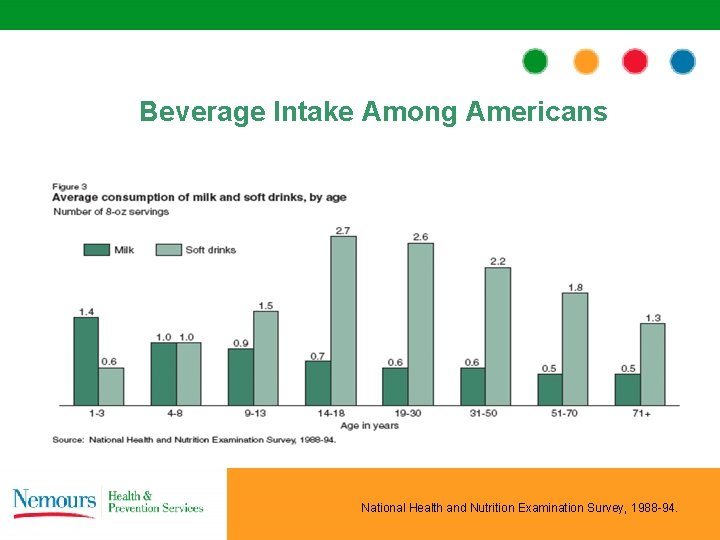
Beverage Intake Among Americans National Health and Nutrition Examination Survey, 1988 -94.
Poor dietary patterns are beginning at early stages For children 12 -24 months, the top 3 sources of total energy were reported to be: – Milk – 100% juice – Sugar Sweetened Beverages Source: Fox, MK, Reidy K, Novak T, Ziegler P. Sources of energy and nutrients in the diets of infants and toddlers. J Am Diet Assoc. 2006; 106: 1992 -2000.
Why limit juice? Excessive juice intake in children may be associated with: – Obesity or persistence of obesity in childhood – Dental cavities Welsh, 2005; Konig, 1995

5 -2 -1 -Almost None