2017 CPT Codes and Outcome Measures LAURA SAKER
- Slides: 21
2017 CPT Codes and Outcome Measures LAURA SAKER, SOT BRENAU UNIVERSITY MSOT CLASS OF 2017 BETHANY DIAMOND, SPT, ATC CLEVELAND STATE UNIVERSITY DPT CLASS OF 2017
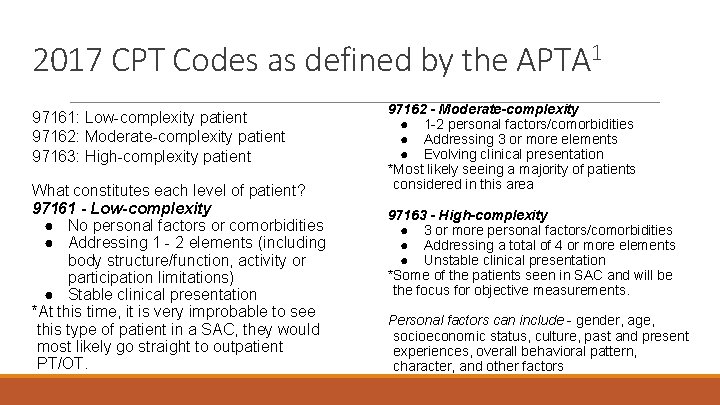
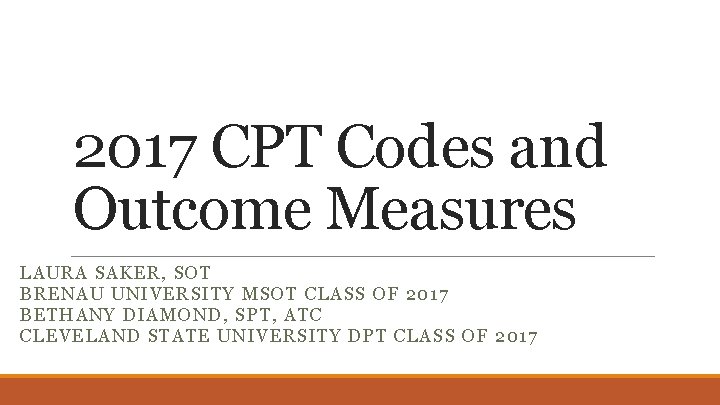
2017 CPT Codes as defined by the APTA 1 97161: Low-complexity patient 97162: Moderate-complexity patient 97163: High-complexity patient What constitutes each level of patient? 97161 - Low-complexity ● No personal factors or comorbidities ● Addressing 1 - 2 elements (including body structure/function, activity or participation limitations) ● Stable clinical presentation *At this time, it is very improbable to see this type of patient in a SAC, they would most likely go straight to outpatient PT/OT. 97162 - Moderate-complexity ● 1 -2 personal factors/comorbidities ● Addressing 3 or more elements ● Evolving clinical presentation *Most likely seeing a majority of patients considered in this area 97163 - High-complexity ● 3 or more personal factors/comorbidities ● Addressing a total of 4 or more elements ● Unstable clinical presentation *Some of the patients seen in SAC and will be the focus for objective measurements. Personal factors can include - gender, age, socioeconomic status, culture, past and present experiences, overall behavioral pattern, character, and other factors
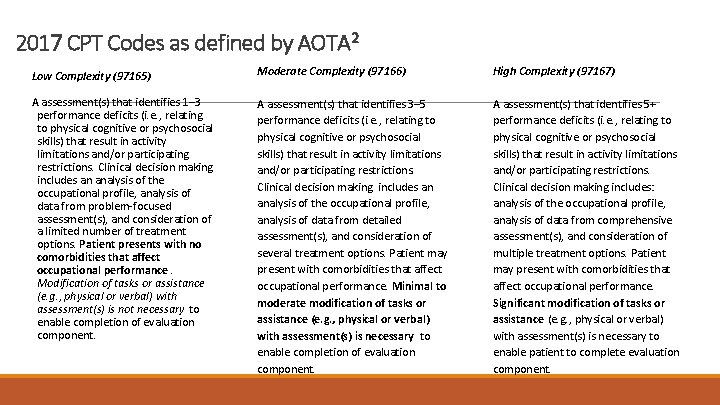
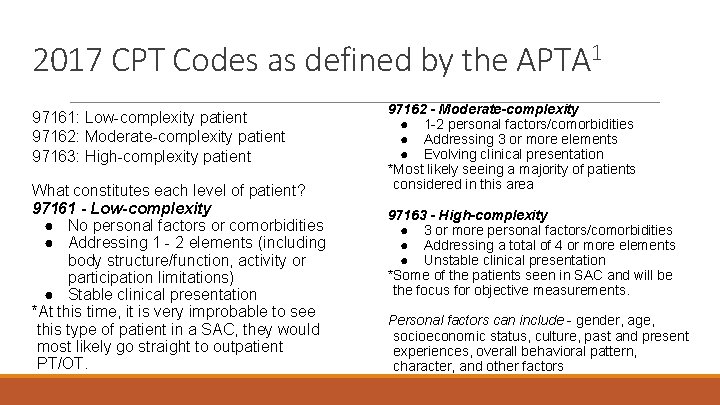
2017 CPT Codes as defined by AOTA 2 Low Complexity (97165) Moderate Complexity (97166) High Complexity (97167) A assessment(s) that identifies 1– 3 performance deficits (i. e. , relating to physical cognitive or psychosocial skills) that result in activity limitations and/or participating restrictions. Clinical decision making includes an analysis of the occupational profile, analysis of data from problem-focused assessment(s), and consideration of a limited number of treatment options. Patient presents with no comorbidities that affect occupational performance. Modification of tasks or assistance (e. g. , physical or verbal) with assessment(s) is not necessary to enable completion of evaluation component. A assessment(s) that identifies 3– 5 performance deficits (i. e. , relating to physical cognitive or psychosocial skills) that result in activity limitations and/or participating restrictions. Clinical decision making includes an analysis of the occupational profile, analysis of data from detailed assessment(s), and consideration of several treatment options. Patient may present with comorbidities that affect occupational performance. Minimal to moderate modification of tasks or assistance (e. g. , physical or verbal) with assessment(s) is necessary to enable completion of evaluation component. A assessment(s) that identifies 5+ performance deficits (i. e. , relating to physical cognitive or psychosocial skills) that result in activity limitations and/or participating restrictions. Clinical decision making includes: analysis of the occupational profile, analysis of data from comprehensive assessment(s), and consideration of multiple treatment options. Patient may present with comorbidities that affect occupational performance. Significant modification of tasks or assistance (e. g. , physical or verbal) with assessment(s) is necessary to enable patient to complete evaluation component.
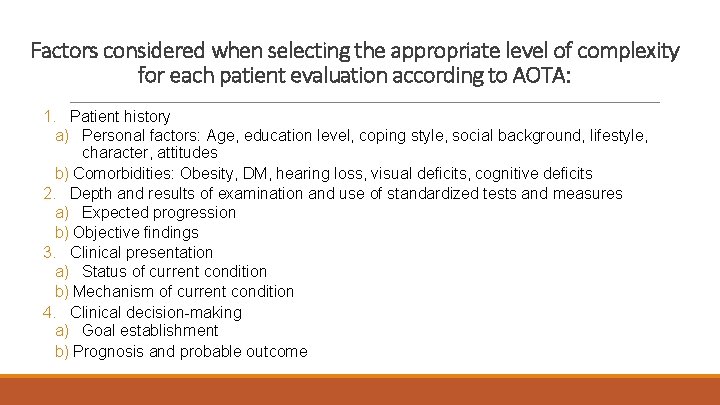
Factors considered when selecting the appropriate level of complexity for each patient evaluation according to AOTA: 1. Patient history a) Personal factors: Age, education level, coping style, social background, lifestyle, character, attitudes b) Comorbidities: Obesity, DM, hearing loss, visual deficits, cognitive deficits 2. Depth and results of examination and use of standardized tests and measures a) Expected progression b) Objective findings 3. Clinical presentation a) Status of current condition b) Mechanism of current condition 4. Clinical decision-making a) Goal establishment b) Prognosis and probable outcome
Why outcome measures? 1. For objective, measurable data to verify patient’s level of functioning and record changes in functioning over time. 2. REIMBURSEMENT - With the new evaluation codes, this will need to be addressed with verified data even more so
APTA recommends these balance outcome measures 3 1. 2. 3. 4. 5. 6. Walking speed 6 MWT TUG 5 x Sit to Stand BERG Etc. These are suggested outcome measures due to generalizability, ease of application, and strong evidence supporting each
Why these aren’t always applicable Low-level, nonambulatory patients are not going to be able to complete these tasks and cannot objectively demonstrate a patient’s level of function Most current sitting balance assessments are completed using a likert scale: ◦ Poor - Fair - Good Normal ◦ This does not have established reliability or validity
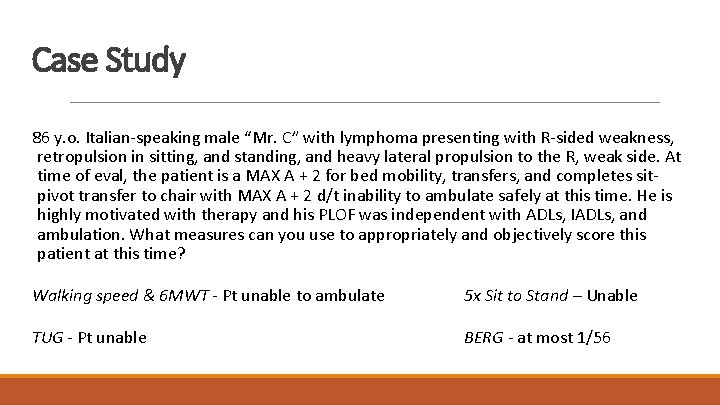
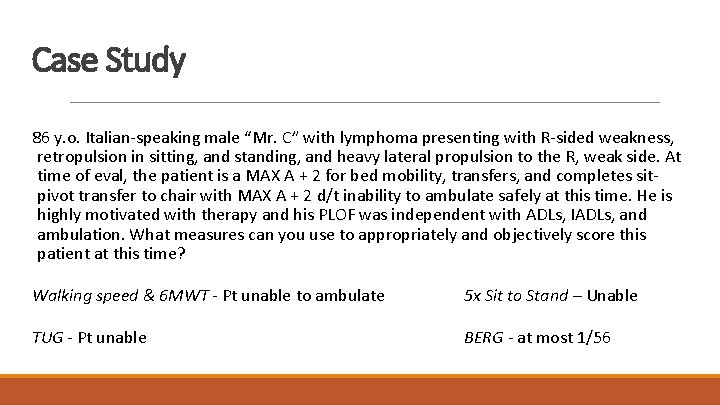
Case Study 86 y. o. Italian-speaking male “Mr. C” with lymphoma presenting with R-sided weakness, retropulsion in sitting, and standing, and heavy lateral propulsion to the R, weak side. At time of eval, the patient is a MAX A + 2 for bed mobility, transfers, and completes sitpivot transfer to chair with MAX A + 2 d/t inability to ambulate safely at this time. He is highly motivated with therapy and his PLOF was independent with ADLs, IADLs, and ambulation. What measures can you use to appropriately and objectively score this patient at this time? Walking speed & 6 MWT - Pt unable to ambulate 5 x Sit to Stand – Unable TUG - Pt unable BERG - at most 1/56
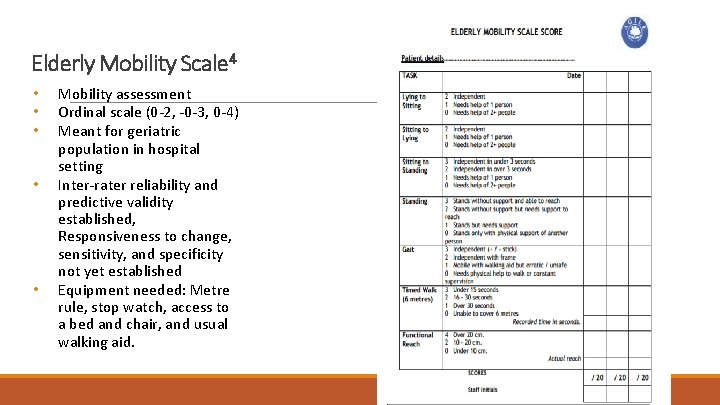
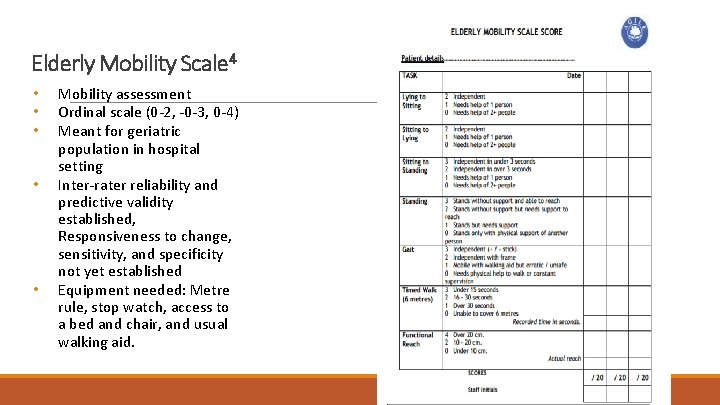
Elderly Mobility Scale 4 • • • Mobility assessment Ordinal scale (0 -2, -0 -3, 0 -4) Meant for geriatric population in hospital setting Inter-rater reliability and predictive validity established, Responsiveness to change, sensitivity, and specificity not yet established Equipment needed: Metre rule, stop watch, access to a bed and chair, and usual walking aid.
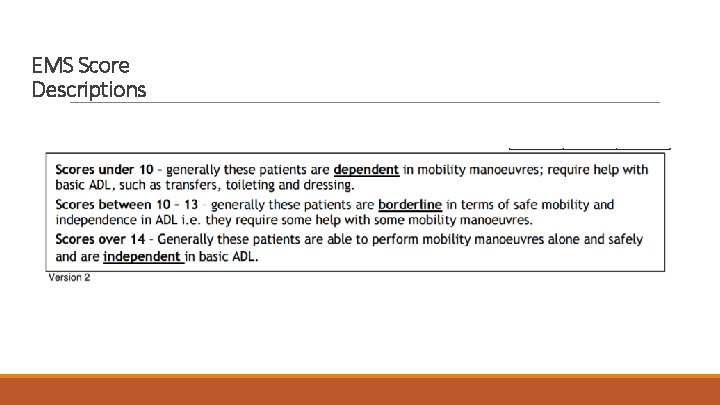
EMS Score Descriptions
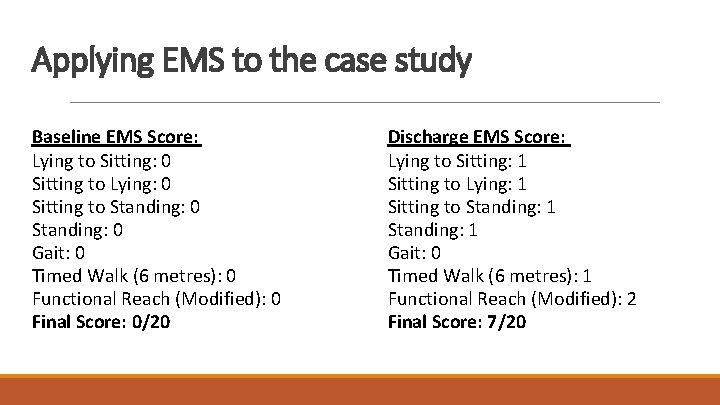
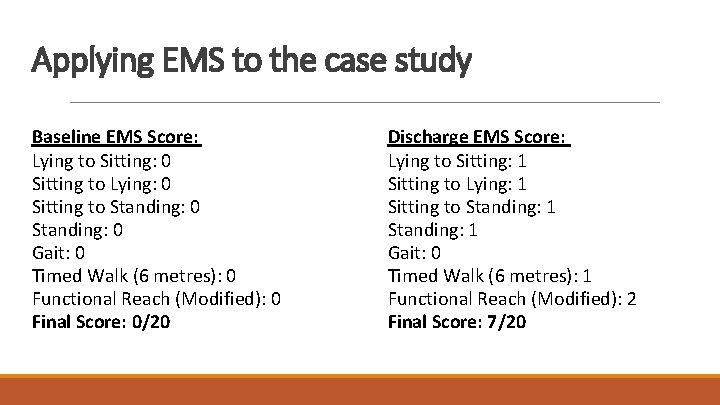
Applying EMS to the case study Baseline EMS Score: Lying to Sitting: 0 Sitting to Lying: 0 Sitting to Standing: 0 Gait: 0 Timed Walk (6 metres): 0 Functional Reach (Modified): 0 Final Score: 0/20 Discharge EMS Score: Lying to Sitting: 1 Sitting to Lying: 1 Sitting to Standing: 1 Gait: 0 Timed Walk (6 metres): 1 Functional Reach (Modified): 2 Final Score: 7/20
Limitations in EMS • Difficult to use in community environments • Ceiling effect for more able patients • Not sensitive for patients with issues of poor confidence • Sensitivity and specificity not yet established
What other outcome measure can be utilized in the clinic for non-ambulatory patients like Mr. C who may “bottom out” on measures such as Berg Balance/TUG/ functional reach?
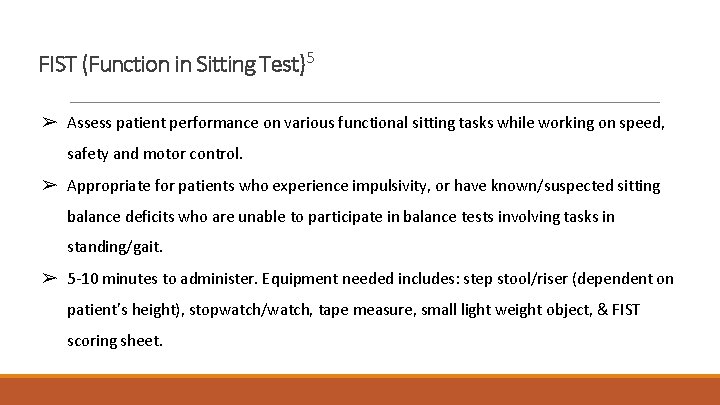
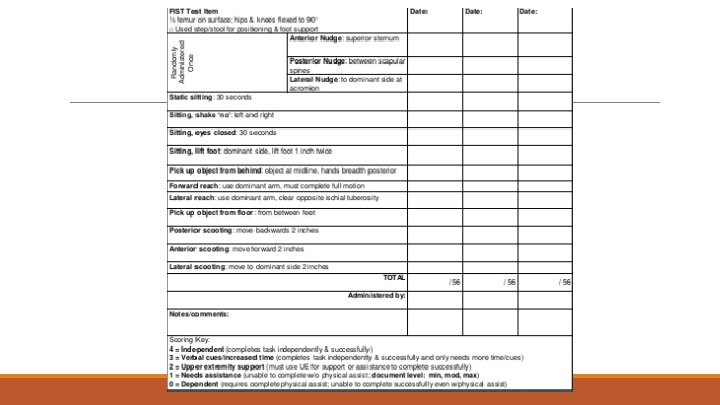
FIST (Function in Sitting Test)5 ➢ Assess patient performance on various functional sitting tasks while working on speed, safety and motor control. ➢ Appropriate for patients who experience impulsivity, or have known/suspected sitting balance deficits who are unable to participate in balance tests involving tasks in standing/gait. ➢ 5 -10 minutes to administer. Equipment needed includes: step stool/riser (dependent on patient’s height), stopwatch/watch, tape measure, small light weight object, & FIST scoring sheet.
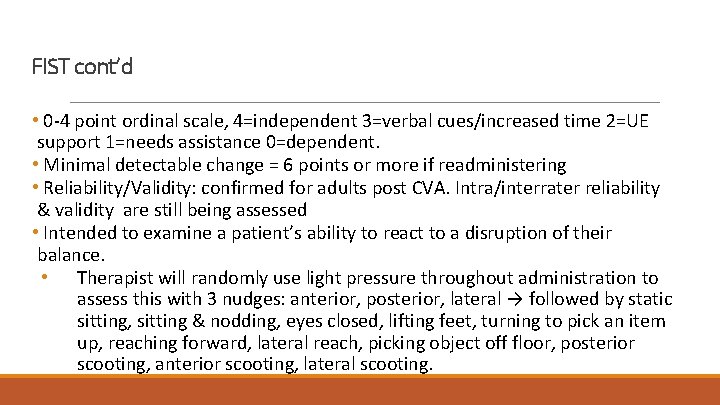
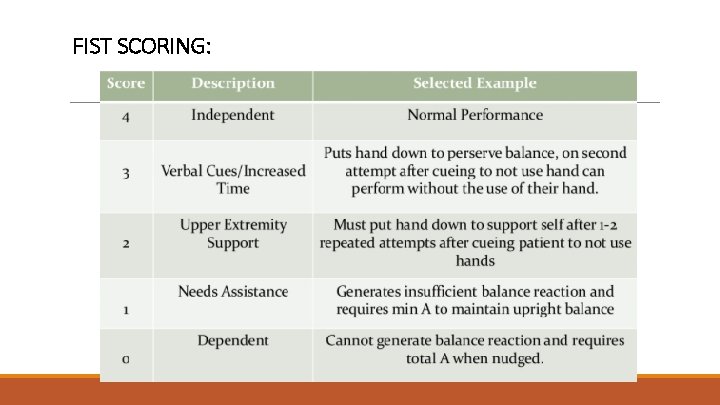
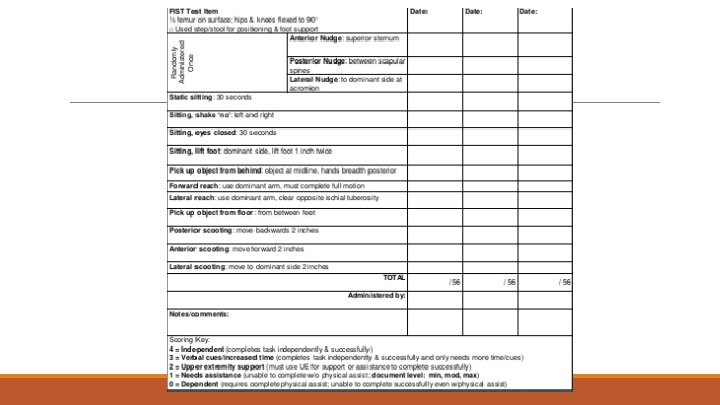
FIST cont’d • 0 -4 point ordinal scale, 4=independent 3=verbal cues/increased time 2=UE support 1=needs assistance 0=dependent. • Minimal detectable change = 6 points or more if readministering • Reliability/Validity: confirmed for adults post CVA. Intra/interrater reliability & validity are still being assessed • Intended to examine a patient’s ability to react to a disruption of their balance. • Therapist will randomly use light pressure throughout administration to assess this with 3 nudges: anterior, posterior, lateral → followed by static sitting, sitting & nodding, eyes closed, lifting feet, turning to pick an item up, reaching forward, lateral reach, picking object off floor, posterior scooting, anterior scooting, lateral scooting.
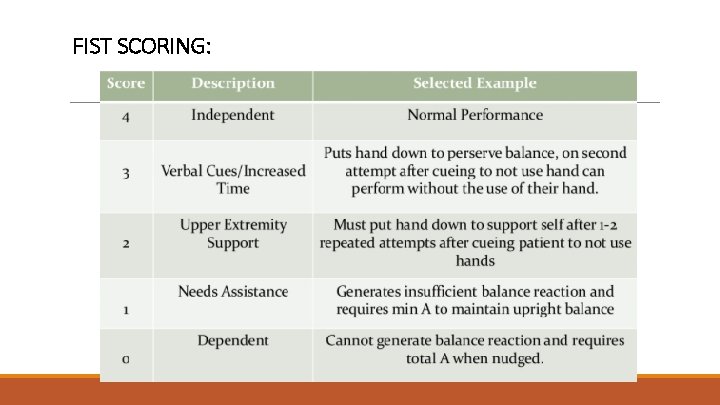
FIST SCORING:
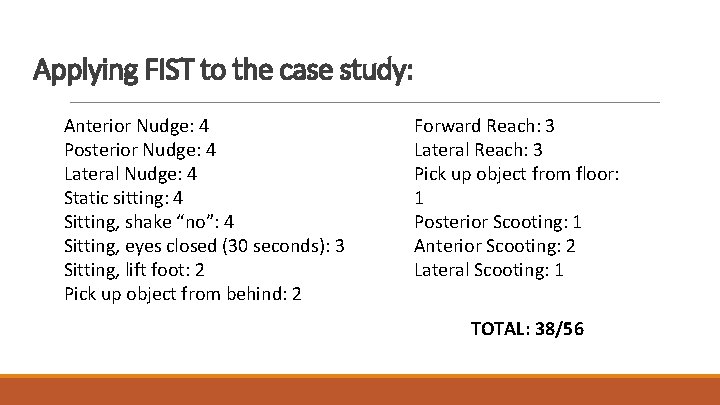
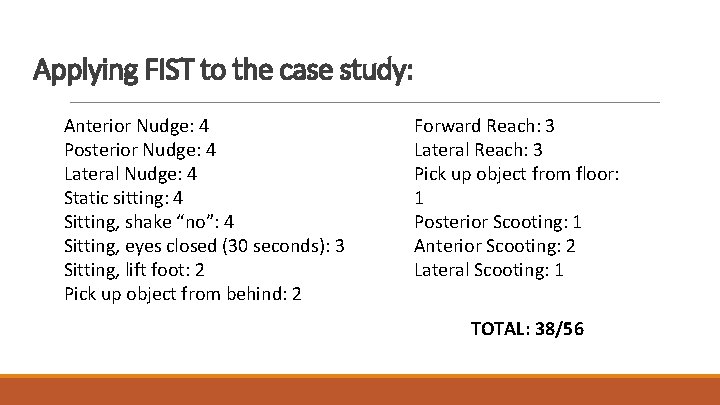
Applying FIST to the case study: Anterior Nudge: 4 Posterior Nudge: 4 Lateral Nudge: 4 Static sitting: 4 Sitting, shake “no”: 4 Sitting, eyes closed (30 seconds): 3 Sitting, lift foot: 2 Pick up object from behind: 2 Forward Reach: 3 Lateral Reach: 3 Pick up object from floor: 1 Posterior Scooting: 1 Anterior Scooting: 2 Lateral Scooting: 1 TOTAL: 38/56
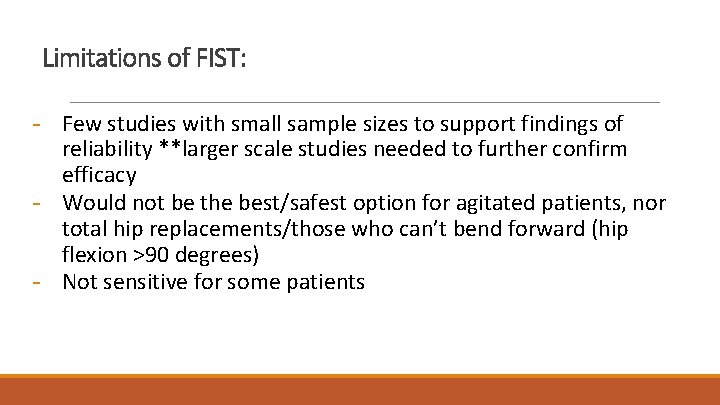
Limitations of FIST: - Few studies with small sample sizes to support findings of reliability **larger scale studies needed to further confirm efficacy - Would not be the best/safest option for agitated patients, nor total hip replacements/those who can’t bend forward (hip flexion >90 degrees) - Not sensitive for some patients
General Considerations for High Complexity Pts: - Shorten phrases 1 step directions Modeling Hand gestures Picture boards Repeat/reiterate phrases Stand in front when speaking to those HOH Allow time for pt to ask questions Always be aware of body language
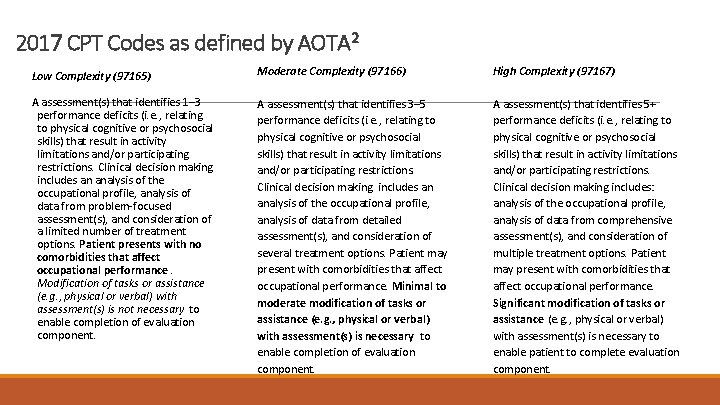
References 1. APTA. Physical Therapy Evaluation Reference Table. American Physical Therapy Association. http: //www. apta. org/uploaded. Files/APTAorg/Payment/Reform/New. Eval. Codes. Quick. Guide. pdf. Published 2016. Accessed February 13, 2017. 2. New Occupational Therapy Evaluation Coding Overview. American Occupational Therapy Association. https: //www. aota. org/~/media/Corporate/Files/Advocacy/Federal/Evaluation. Codes-Overview-2016. pdf. Published 2016. Accessed February 2017. 3. Hartley G, Strunk E, Lusardi M. Section on Geriatrics Recommended Outcome Measures for Medicare Functional Limitation/Severity Reporting. Geriatric Toolkit. http: //geriatrictoolkit. missouri. edu/So. G-Joint-Report-2013 -GCode-Tests. pdf. Published 2013. Accessed February 2017. 4. Rajendran V, Jeevanantham D. The Elderly Mobility Scale. Journal of Acute Care Physical Therapy. 2016; 7(1): 3 -4. doi: 10. 1097/jat. 000000016. 5. “Function in Sitting Test (FIST), ” Samuel Meritt University. N. p. , n. d. Web. 06 Nov. 2013. <http: //www. samuelmerritt. edu/fist>.