2012 11 16 Glaucoma conference Ap R 3
- Slides: 36
2012. 11. 16 Glaucoma conference Ap. 박혜영 / R 3 박창현
2012. 11. 16 GLAUCOMAS ASSOCIATED WITH CORNEAL PROCEDURES
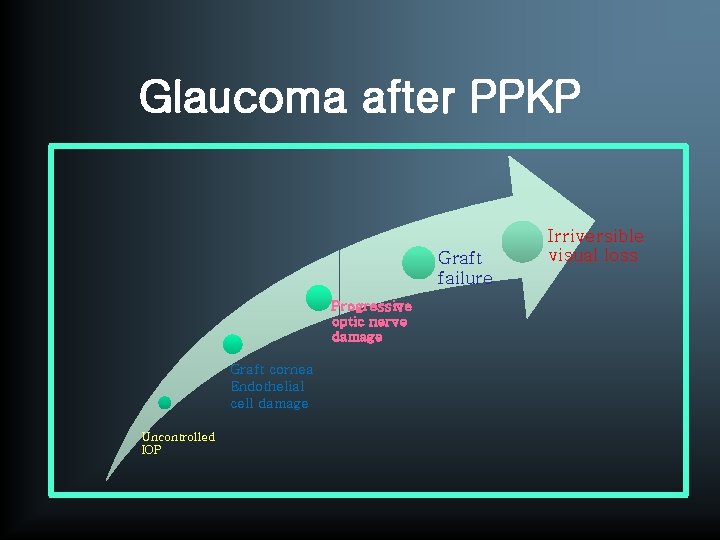
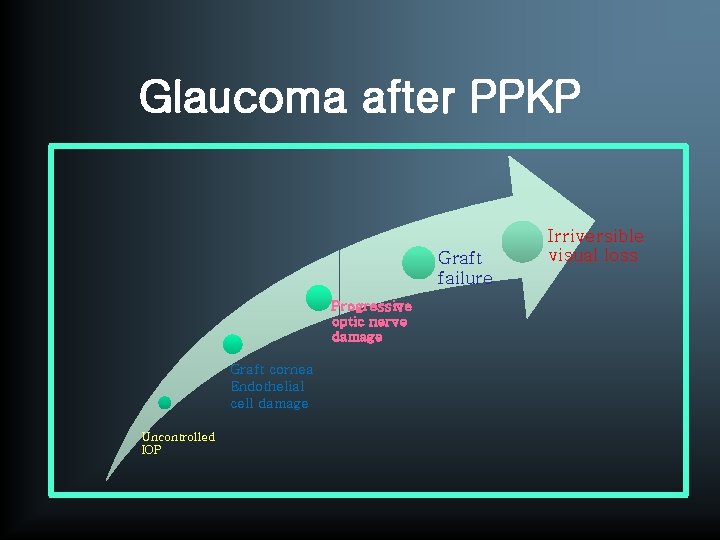
Glaucoma after PPKP Graft failure Progressive optic nerve damage Graft cornea Endothelial cell damage Uncontrolled IOP Irriversible visual loss
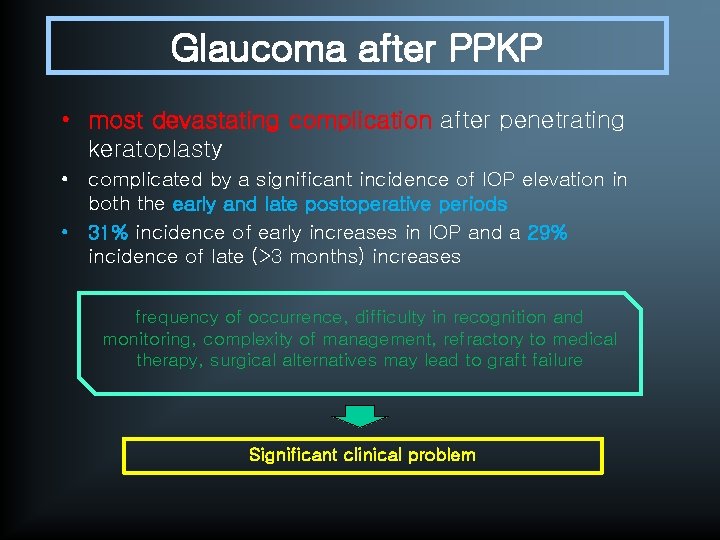
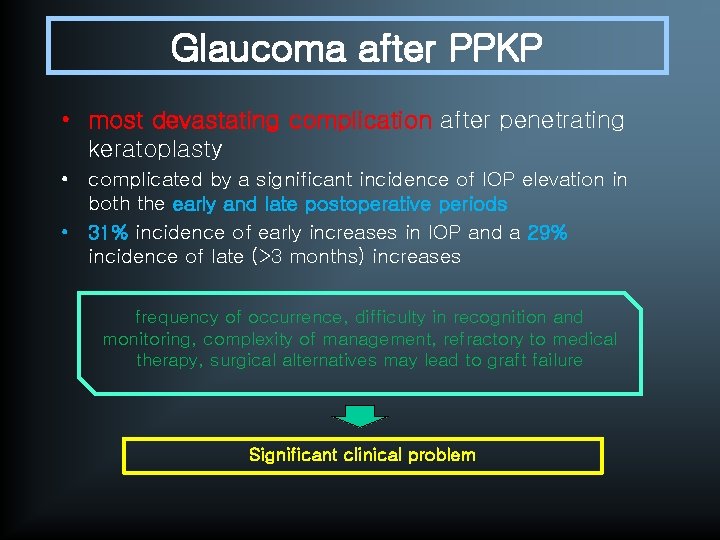
Glaucoma after PPKP • most devastating complication after penetrating keratoplasty • complicated by a significant incidence of IOP elevation in both the early and late postoperative periods • 31% incidence of early increases in IOP and a 29% incidence of late (>3 months) increases frequency of occurrence, difficulty in recognition and monitoring, complexity of management, refractory to medical therapy, surgical alternatives may lead to graft failure Significant clinical problem
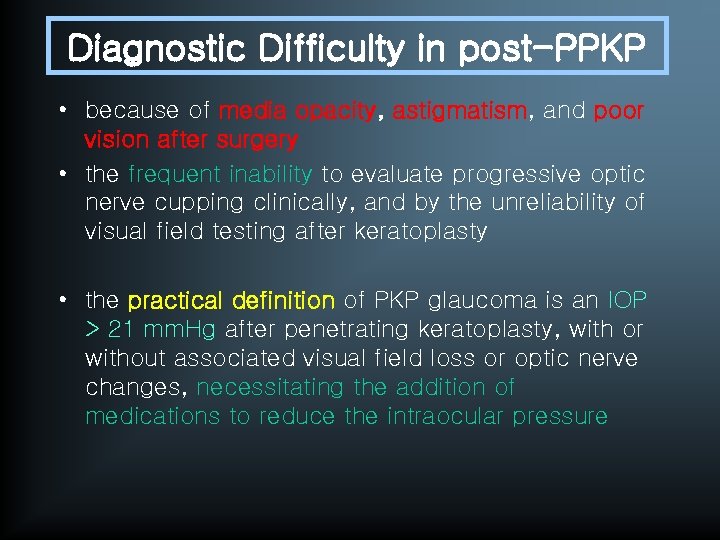
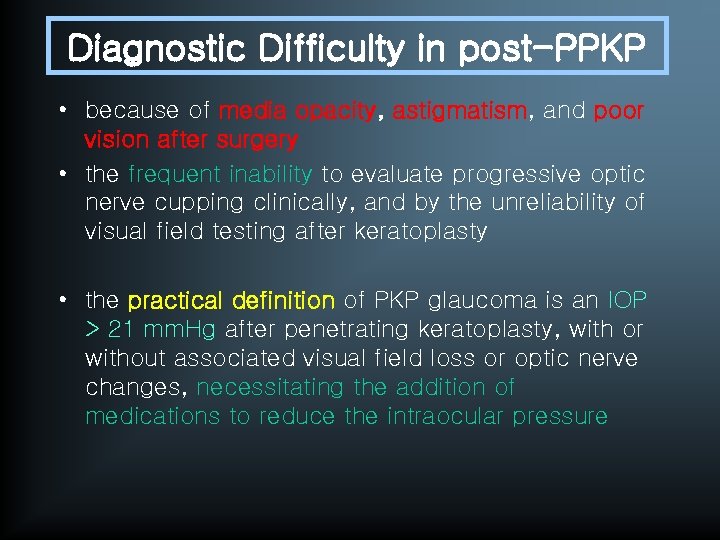
Diagnostic Difficulty in post-PPKP • because of media opacity, astigmatism, and poor vision after surgery • the frequent inability to evaluate progressive optic nerve cupping clinically, and by the unreliability of visual field testing after keratoplasty • the practical definition of PKP glaucoma is an IOP > 21 mm. Hg after penetrating keratoplasty, with or without associated visual field loss or optic nerve changes, necessitating the addition of medications to reduce the intraocular pressure
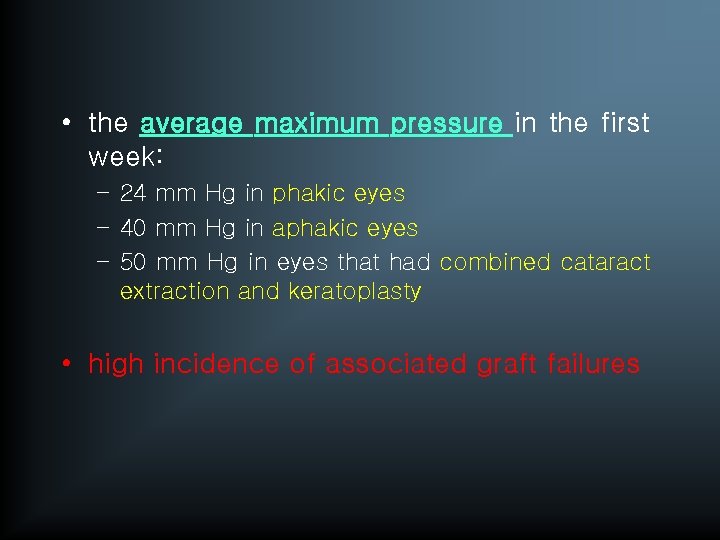
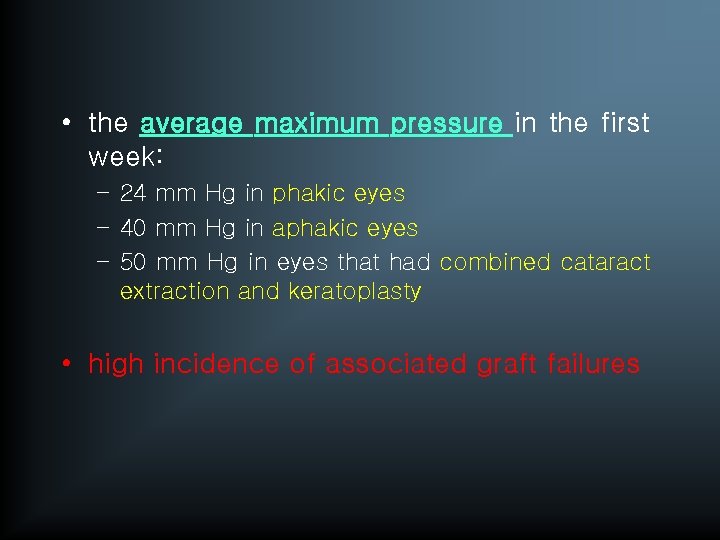
• the average maximum pressure in the first week: – 24 mm Hg in phakic eyes – 40 mm Hg in aphakic eyes – 50 mm Hg in eyes that had combined cataract extraction and keratoplasty • high incidence of associated graft failures
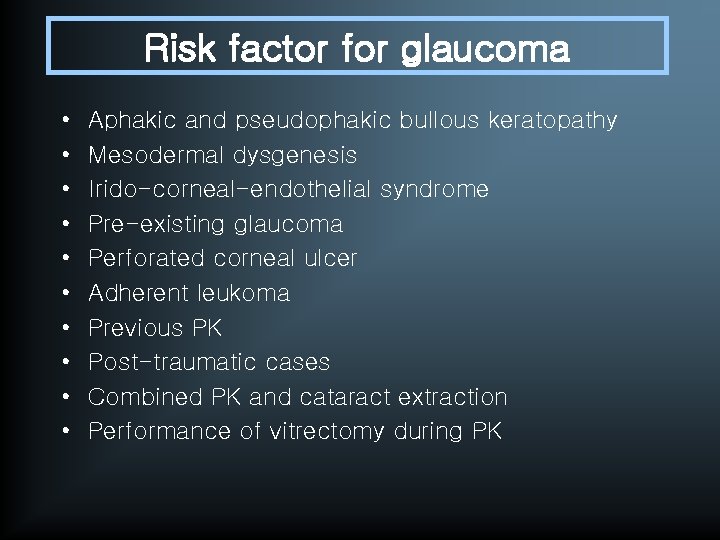
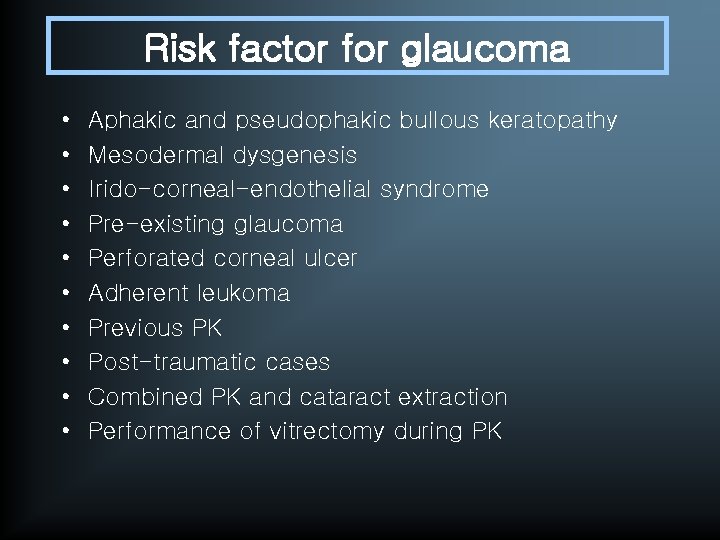
Risk factor for glaucoma • • • Aphakic and pseudophakic bullous keratopathy Mesodermal dysgenesis Irido-corneal-endothelial syndrome Pre-existing glaucoma Perforated corneal ulcer Adherent leukoma Previous PK Post-traumatic cases Combined PK and cataract extraction Performance of vitrectomy during PK
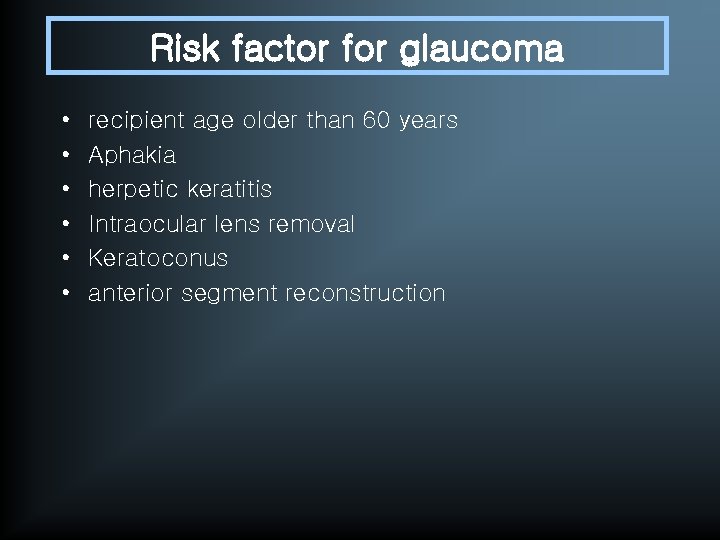
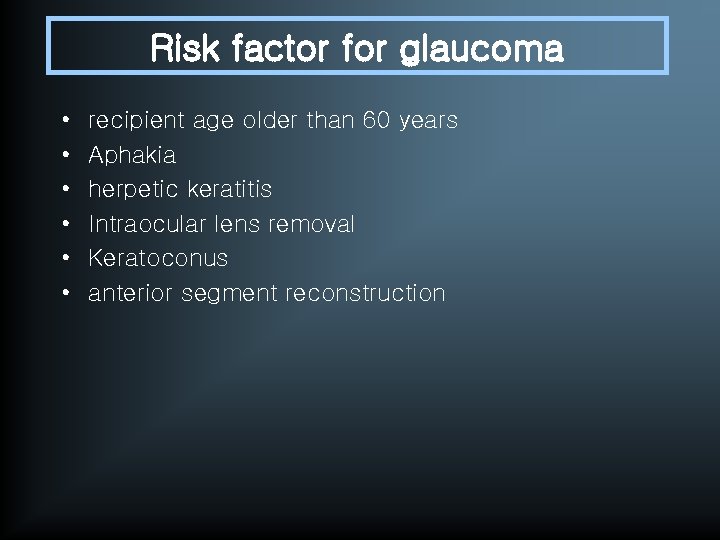
Risk factor for glaucoma • • • recipient age older than 60 years Aphakia herpetic keratitis Intraocular lens removal Keratoconus anterior segment reconstruction
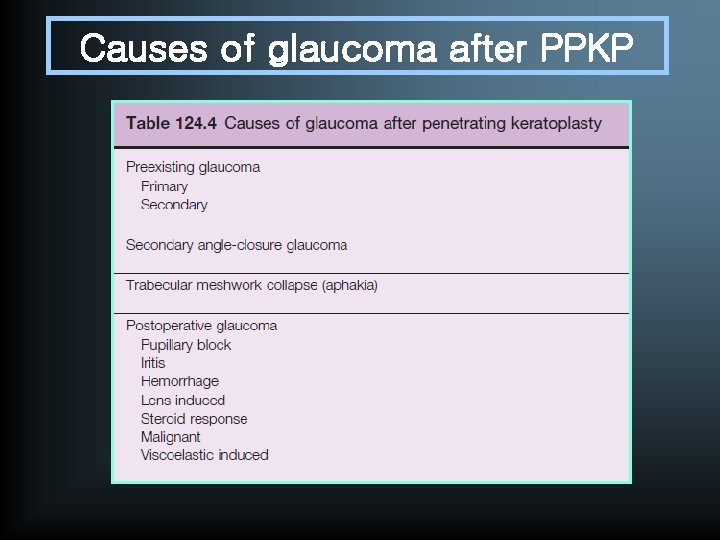
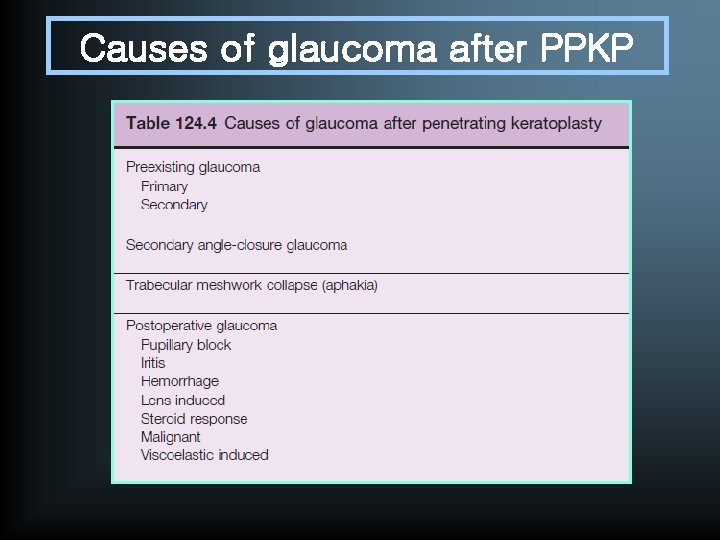
Causes of glaucoma after PPKP
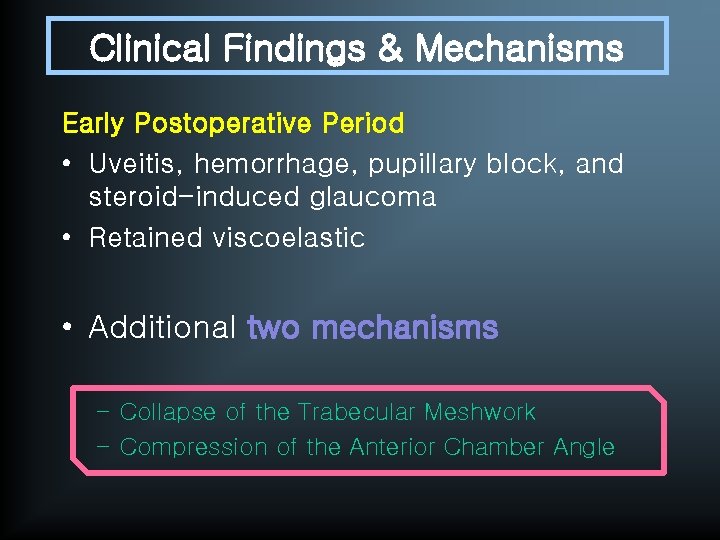
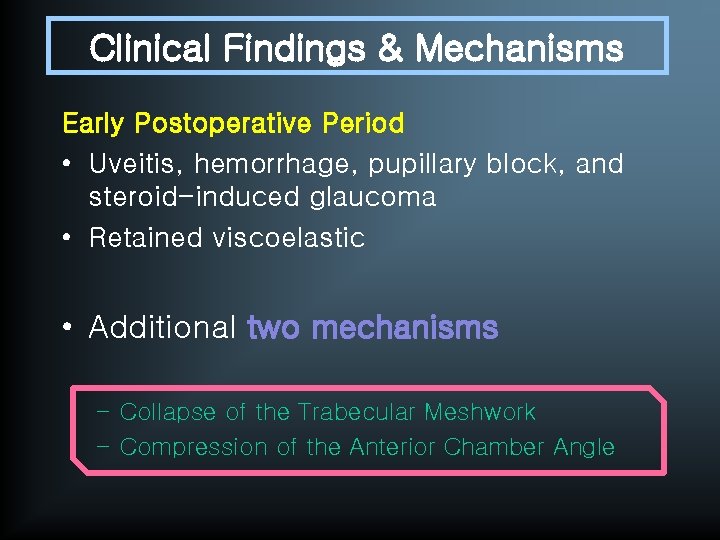
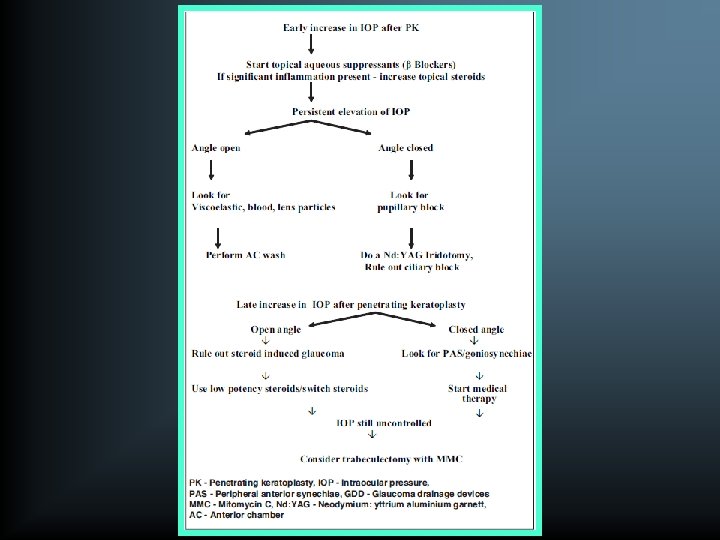
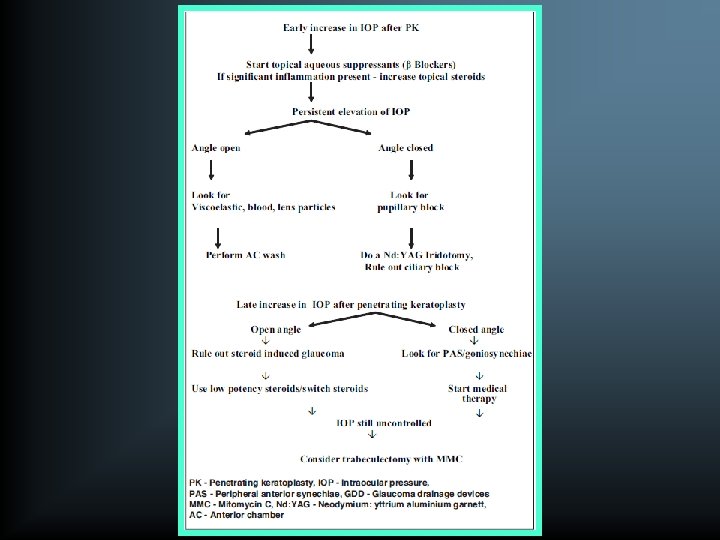
Clinical Findings & Mechanisms Early Postoperative Period • Uveitis, hemorrhage, pupillary block, and steroid-induced glaucoma • Retained viscoelastic • Additional two mechanisms – Collapse of the Trabecular Meshwork – Compression of the Anterior Chamber Angle
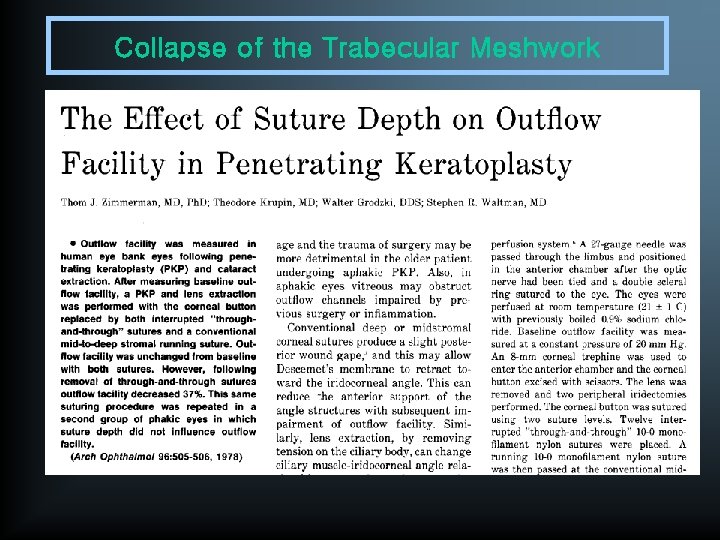
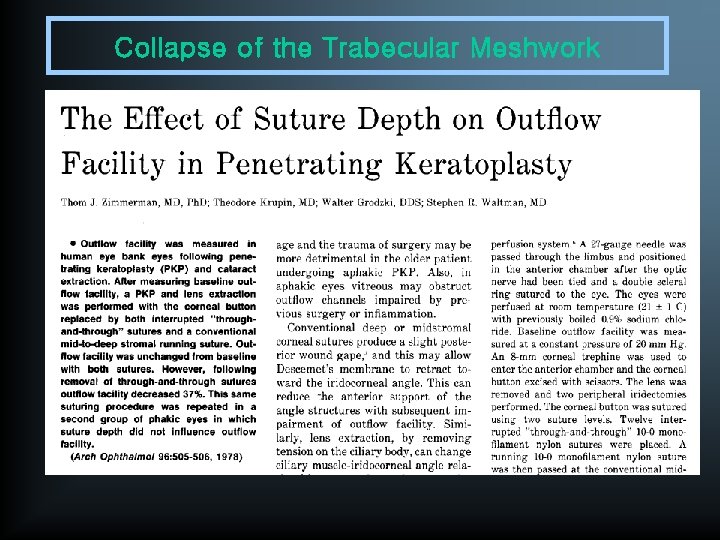
Collapse of the Trabecular Meshwork • loss of anterior support due to the incision in the Descemet membrane • compounded in the aphakic eye by a reduction in posterior support from the loss of zonular tension • through-and-through suturing: lower early postoperative IOP, compared with conventional mid-stromal suturing
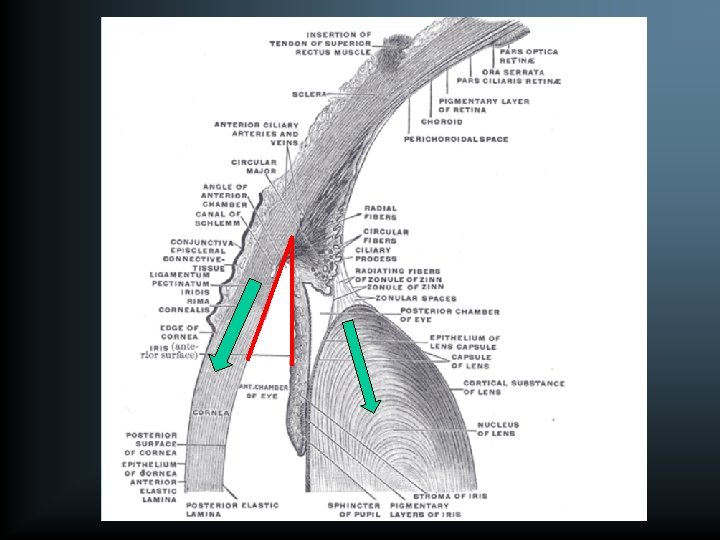
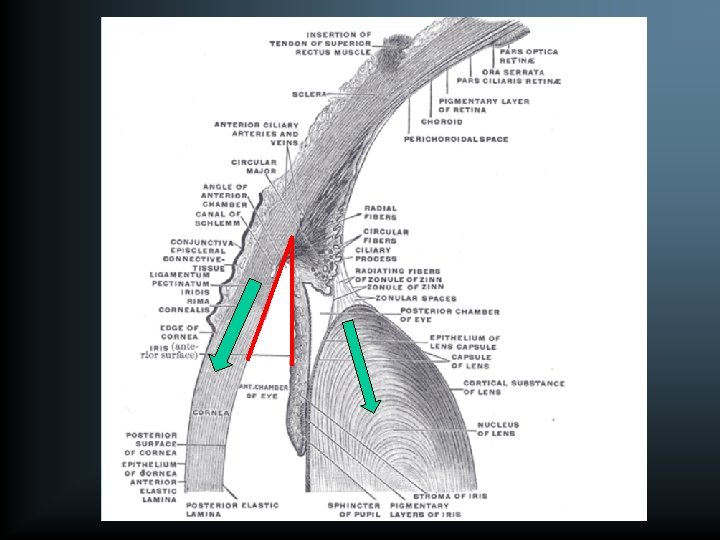
Compression of the Anterior Chamber Angle • caused by the conventional techniques of penetrating keratoplasty • causing an early postoperative IOP rise • subsequent chronic glaucoma due to peripheral anterior synechiae
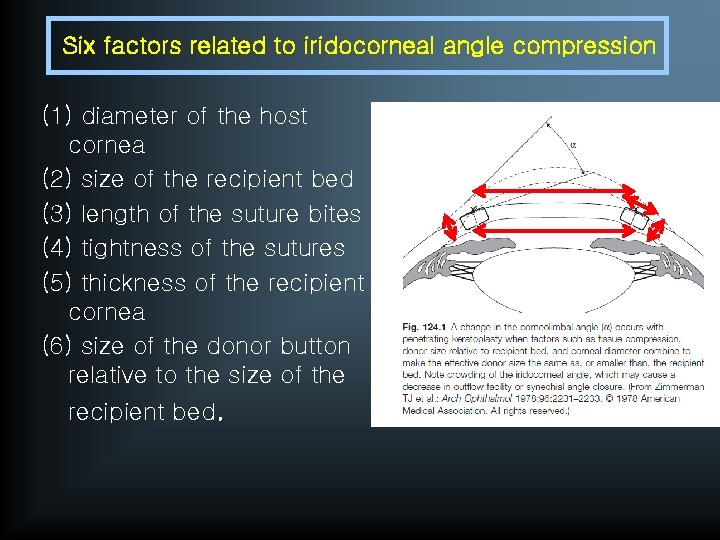
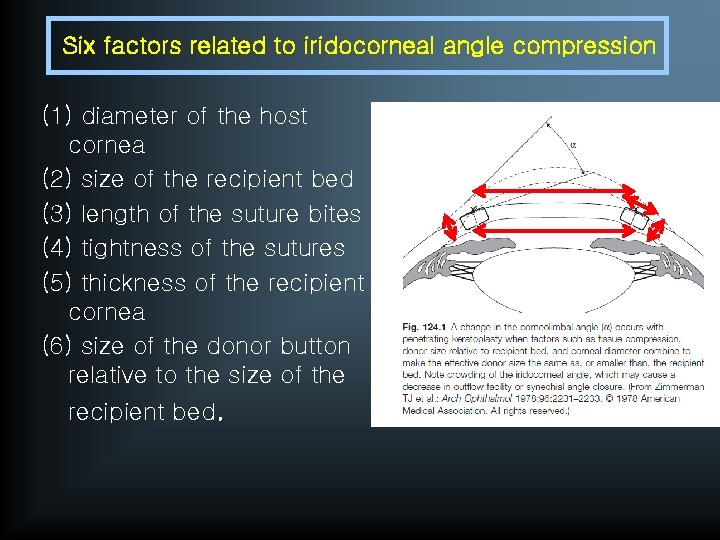
Six factors related to iridocorneal angle compression (1) diameter of the host cornea (2) size of the recipient bed (3) length of the suture bites (4) tightness of the sutures (5) thickness of the recipient cornea (6) size of the donor button relative to the size of the recipient bed.
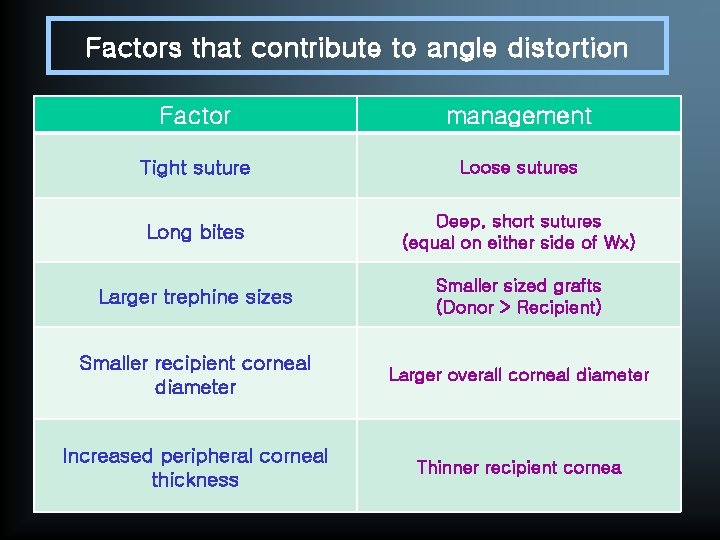
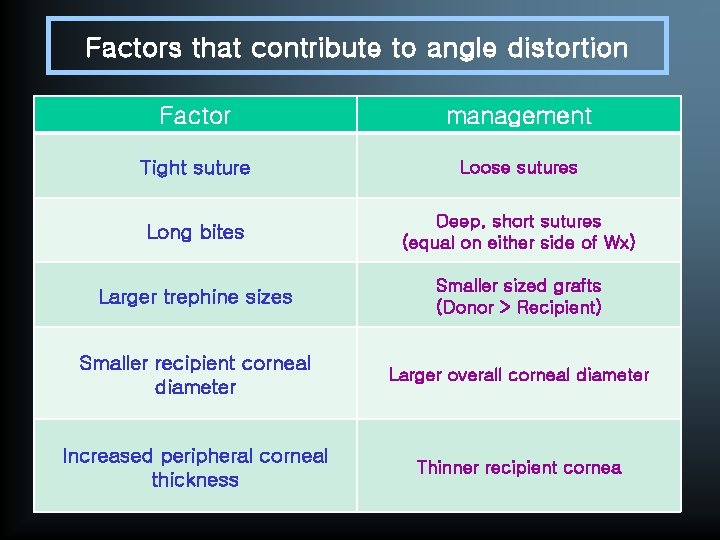
Factors that contribute to angle distortion Factor management Tight suture Loose sutures Long bites Deep, short sutures (equal on either side of Wx) Larger trephine sizes Smaller sized grafts (Donor > Recipient) Smaller recipient corneal diameter Larger overall corneal diameter Increased peripheral corneal thickness Thinner recipient cornea
Clinical Findings & Mechanisms Late Postoperative Period • synechial angle closure is probably the dominant cause of chronic PKP glaucoma • Gradual flattening of the anterior chamber several months after aphakic keratoplasty : intact anterior vitreous face -> prophylactic vitrectomy • graft rejection, which may require long-term steroid antiglaucoma therapy • pigment dispersion syndrome may also be seen with pseudophakic eyes • keratoplasty for congenitally opaque corneas • peripheral anterior synechiae • long-term use of steroids, or epithelial ingrowth
Tonometry • biomechanical assumptions underlying all tonometry techniques are violated in such eyes – – the cornea is not spherical usually has significant astigmatism corneal thickness is abnormal mechanical linkage of the grafted cornea to the host is not continuous • the Mackay-Marg electronic applanation Tonometer, the pneumatic applanation tonometer, tono-pen • The Dynamic Contour Tonometer (DCT) : with a digital piezoelectric pressure transducer that couples to the contour of the ocular surface and measures transcorneal pressure directly
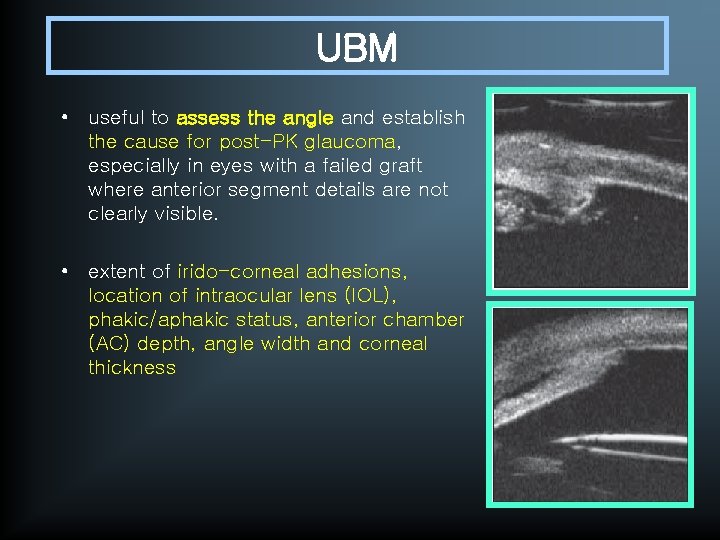
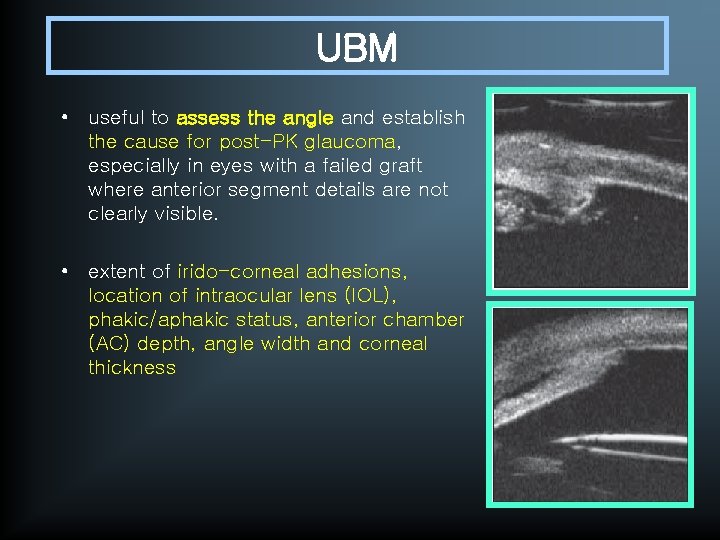
UBM • useful to assess the angle and establish the cause for post-PK glaucoma, especially in eyes with a failed graft where anterior segment details are not clearly visible. • extent of irido-corneal adhesions, location of intraocular lens (IOL), phakic/aphakic status, anterior chamber (AC) depth, angle width and corneal thickness
Prophylaxis Management Preventive Measures during PPKP • larger than the recipient trephine • looser or shorter suture bites compression • smaller trephine size • a thinner peripheral host cornea • larger host corneal diameter to minimize tissue • use of oversized grafts is associated with deeper anterior chamber depths, a lower incidence of progressive angle closure, and significantly lower postoperative pressures, compared with use of same-sized grafts • Oversized grafts, however, are contraindicated in treating keratoconus because they cause a significant increase in myopia
Prophylaxis Management • placement of sutures near the pupillary portion of a flaccid iris to create a taut iris • meticulous wound closure • extensive postoperative steroids : control the inflammation and prevent PAS formation. • Cytoplegics : keep the pupil mobile and prevent pupillary block.
Medical Treatment • first-line treatment : unless a specific, treatable condition, such as pupillary block, is apparent. • frequently unsuccessful. • Indication – known or suspected glaucomatous optic nerve damage or IOP high enough to cause corneal graft failure
Medical Treatment • Beta adrenergic blocking agents : not very effective and cause, chronic conjunctival inflammation • Brimonidine tartarate 0. 2% or 0. 15% with preservative can be used (thrice daily as monotherapy and twice daily as combination therapy • Apraclonidine (0. 5%) is a potent vasoconstrictor and is useful both to prevent AC bleeding during the operation and to treat resultant IOP spikes
Medical Treatment • Systemic carbonic anhydrase inhibitors are very useful as a short-term therapy in the early postoperative period to control the IOP • Topical carbonic anhydrase inhibitors (dorzolamide and brinzolamide) should be used with caution as they also suppress the carbonic anhydrase enzyme in the corneal endothelium and long-term use can lead to graft decompensation • Prostaglandin analogs can also be used to decrease IOP by increasing uveoscleral outflow and can be used in conjunction with beta blockers.
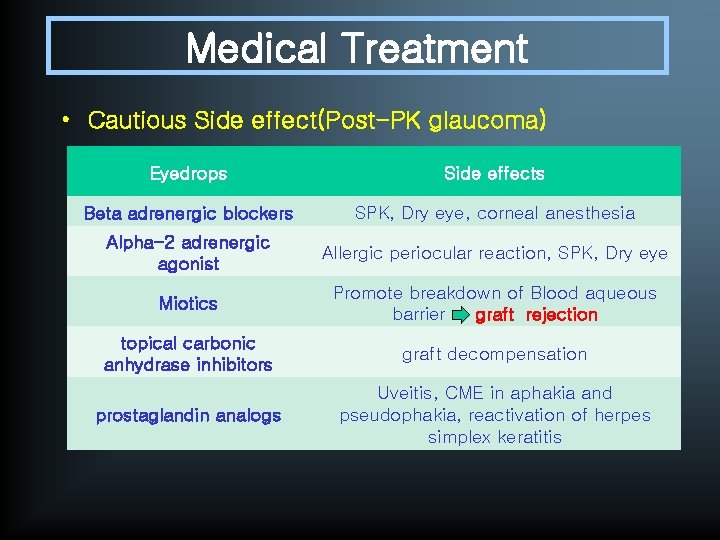
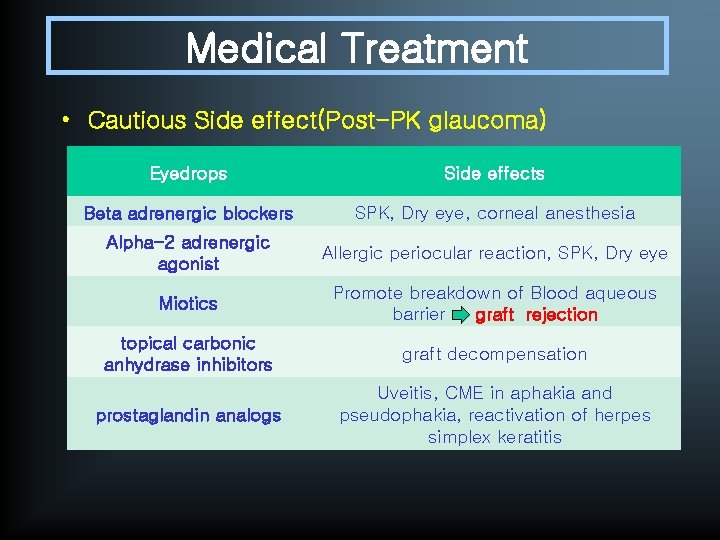
Medical Treatment • Cautious Side effect(Post-PK glaucoma) Eyedrops Side effects Beta adrenergic blockers SPK, Dry eye, corneal anesthesia Alpha-2 adrenergic agonist Allergic periocular reaction, SPK, Dry eye Miotics Promote breakdown of Blood aqueous barrier graft rejection topical carbonic anhydrase inhibitors graft decompensation prostaglandin analogs Uveitis, CME in aphakia and pseudophakia, reactivation of herpes simplex keratitis
Target IOP. In an eye with no discernable glaucoma damage: in the upper teens and low 20 s In the Advanced Glaucoma Intervention Study (AGIS), only those patients with IOPs < 18 mm. Hg at every follow-up visit demonstrated visual field stability; among this group, the average IOP was 14. 1 mm. Hg. the results of the AGIS and other studies strongly support aggressive IOP lowering in patients with established disease, with targets set in the mid to low teens.
Surgical Treatment • Indication : when the optic nerve head or the graft is threatened by a persistently elevated IOP – – Laser trabeculoplasty Laser iridoplasty/iridotomy Trabeculectomy with antimetabolites GDDs • No glaucoma operation has been found to be entirely suitable for controlling IOP and preserving graft clarity
Laser trabeculoplasty • open angles, clear grafts, and moderately elevated IOP (20 -25 mm. Hg) on glaucoma medications. • post-operative IOP spikes and uveitis, which can trigger graft rejection Laser iridotomy • Pupillary block is suspected • Gonioplasty can be done for PAS, which has been present for less than one year
Trabeculectomy • usually not effective due to dense perilimbal scarring and fibrosis with an increased risk of failure. • Antimetabolites (5 -fluorouracil and mitomycin-C) must be used (high rate of corneal epithelial toxicity) • aphakic eyes : mandatory to do a vitrectomy to prevent any vitreous from blocking the trabeculectomy ostium • success rate in IOP control with mitomycin trabeculectomy in patients with post-PK glaucoma is 67 -91%, and that of graft failure is 12 -18%.
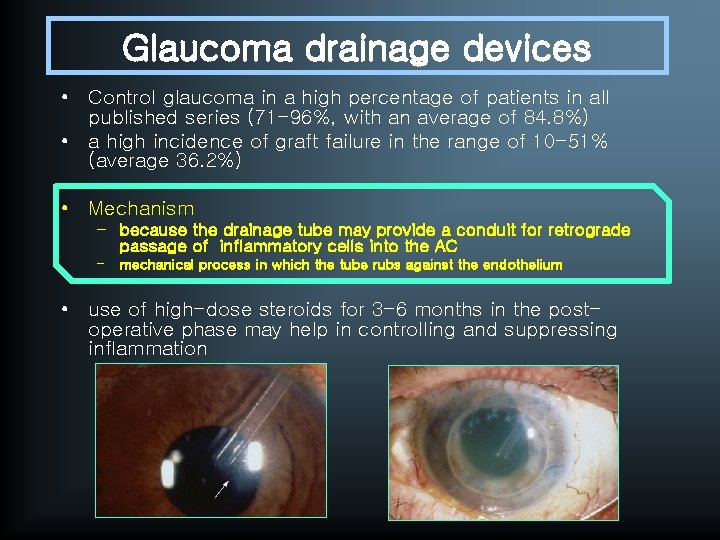
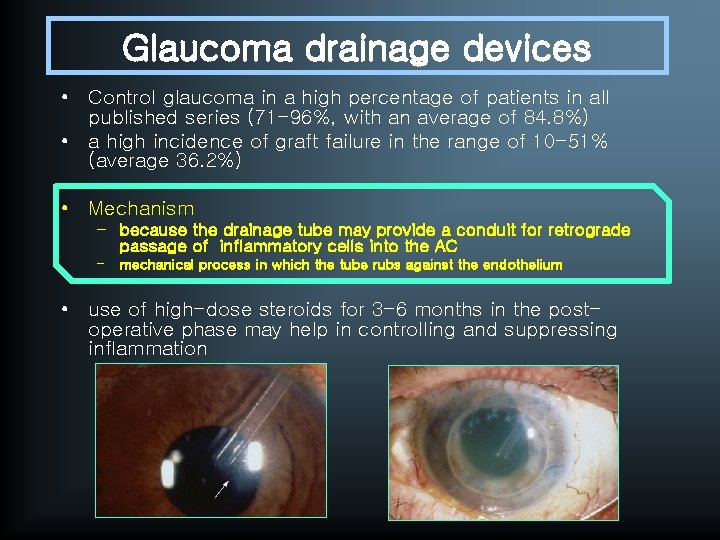
Glaucoma drainage devices • Control glaucoma in a high percentage of patients in all published series (71 -96%, with an average of 84. 8%) • a high incidence of graft failure in the range of 10 -51% (average 36. 2%) • Mechanism – because the drainage tube may provide a conduit for retrograde passage of inflammatory cells into the AC – mechanical process in which the tube rubs against the endothelium • use of high-dose steroids for 3 -6 months in the postoperative phase may help in controlling and suppressing inflammation
Cyclodestructive Procedures • Ablating the cilliary processes to lower IOP by reducing aqueous production – – Cyclocryotherapy Nd: YAG laser cyclophotocoagulation Diode laser cyclophotocoagulation Transpupillary argon laser photocoagulation • Despite numerous published case series, the best choice among these three surgical approaches (trabeculectomy with MMC, GDD, or cyclophotocoagulation) is not clear
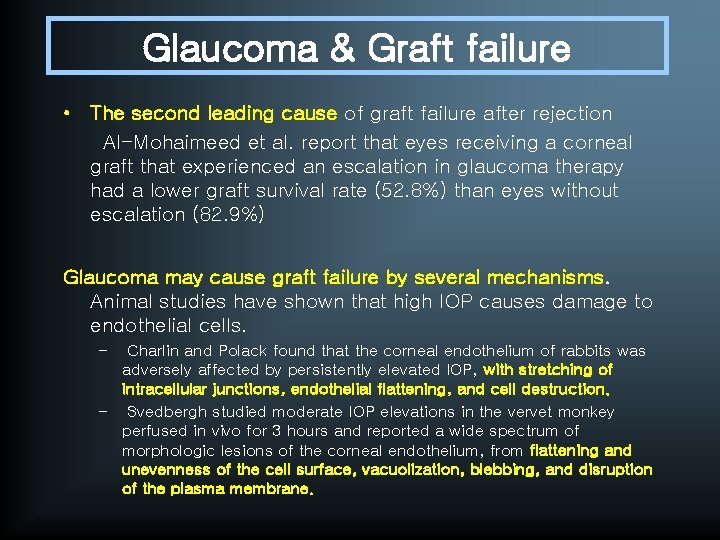
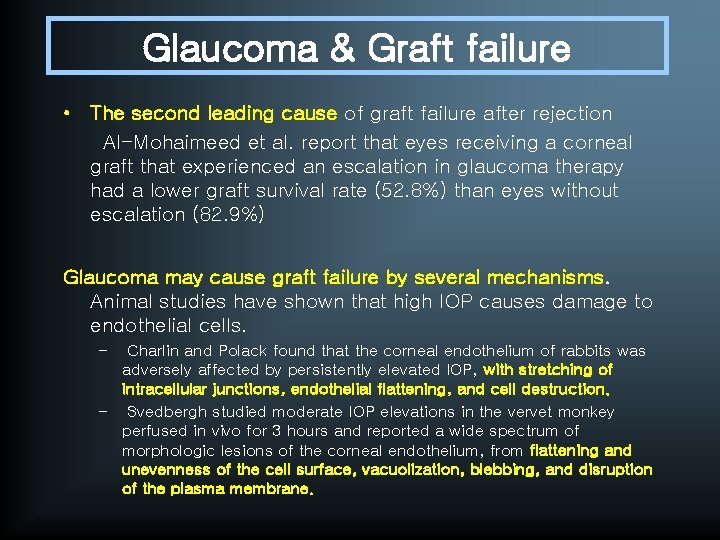
Glaucoma & Graft failure • The second leading cause of graft failure after rejection Al-Mohaimeed et al. report that eyes receiving a corneal graft that experienced an escalation in glaucoma therapy had a lower graft survival rate (52. 8%) than eyes without escalation (82. 9%) Glaucoma may cause graft failure by several mechanisms. Animal studies have shown that high IOP causes damage to endothelial cells. – Charlin and Polack found that the corneal endothelium of rabbits was adversely affected by persistently elevated IOP, with stretching of intracellular junctions, endothelial flattening, and cell destruction. – Svedbergh studied moderate IOP elevations in the vervet monkey perfused in vivo for 3 hours and reported a wide spectrum of morphologic lesions of the corneal endothelium, from flattening and unevenness of the cell surface, vacuolization, blebbing, and disruption of the plasma membrane.
Glaucoma & Graft failure Preservative benzalkonium chloride (BAK) • a cause of graft failure • accumulation of inflammatory cells and mediators in conjunctival tissue • researchers have postulated that this increases the likelihood of immunologic graft rejection
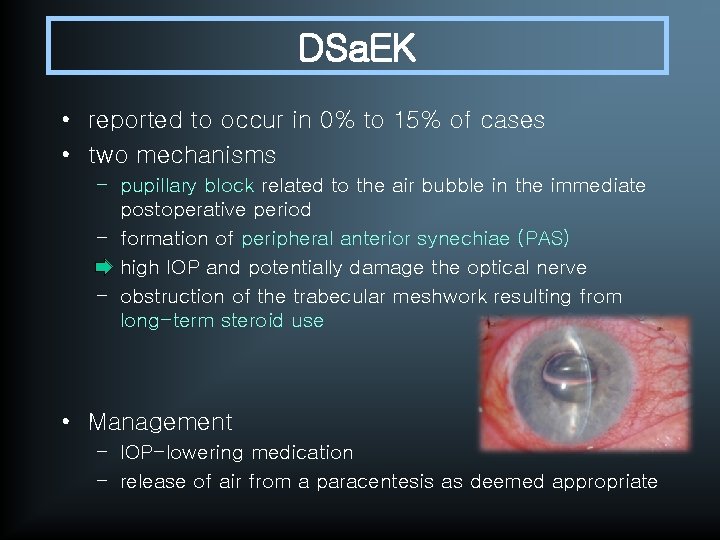
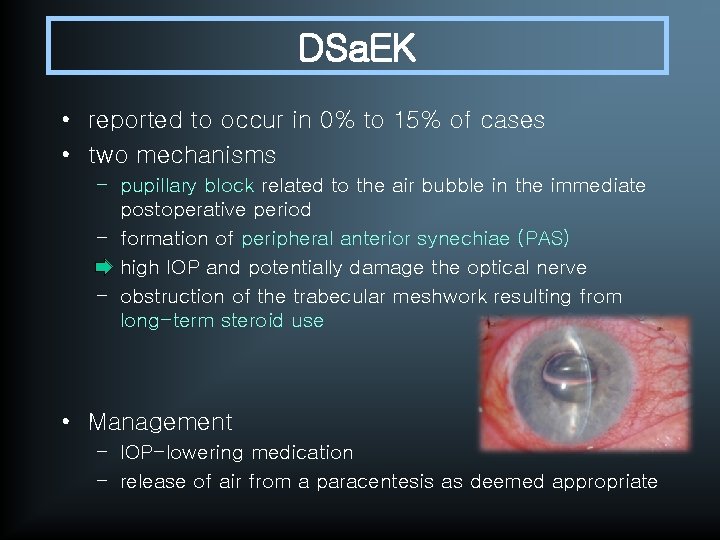
DSa. EK • reported to occur in 0% to 15% of cases • two mechanisms – pupillary block related to the air bubble in the immediate postoperative period – formation of peripheral anterior synechiae (PAS) – high IOP and potentially damage the optical nerve – obstruction of the trabecular meshwork resulting from long-term steroid use • Management – IOP-lowering medication – release of air from a paracentesis as deemed appropriate
• Terry et al. reported no cases of pupillary block glaucoma in a series of 200 eyes undergoing DSEK as a result of placing a mobile air bubble occupying less than 50% of the anterior chamber volume • Price et al. analyzed risk factors for graft rejection with DSEK and found that preexisting glaucoma (eyes with and without glaucoma surgery) and steroid-induced ocular hypertension had 1. 8 times the relative risk of experiencing an initial rejection episode than eyes that did not have these conditions.
Reference • Shields Textbook of Glaucoma, 6 th ed. • Krachmer: Cornea, 3 rd ed. • Post-penetrating keratoplasty glaucoma, Indian J Ophthalmol 2008; 56: 269 -77