The Red Eye for primary healthcare providers DR

- Slides: 35
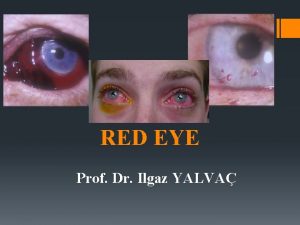
The Red Eye for primary healthcare providers DR CHIN PIK KEE FRCS Ophthal (Edinburgh), M. Med Ophthal (S’pore) Sunway Medical Centre Primary Eye Care Paramedic Workshop, MSJOC 2016; 4 March 2016, Kuching, Sarawak
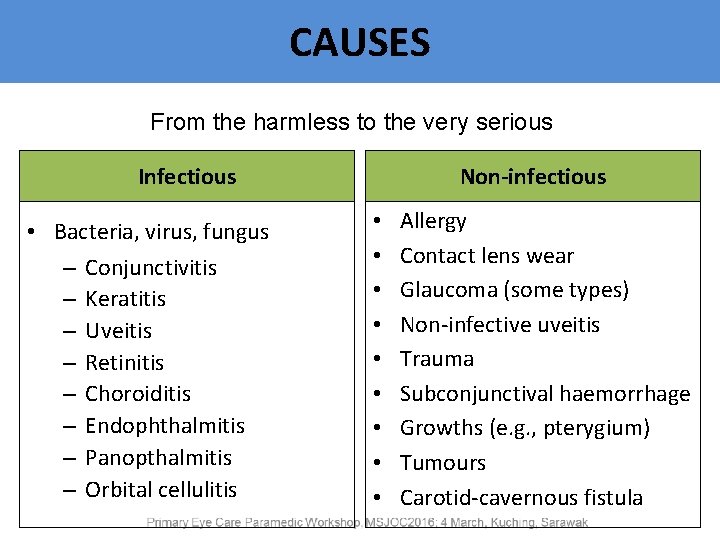
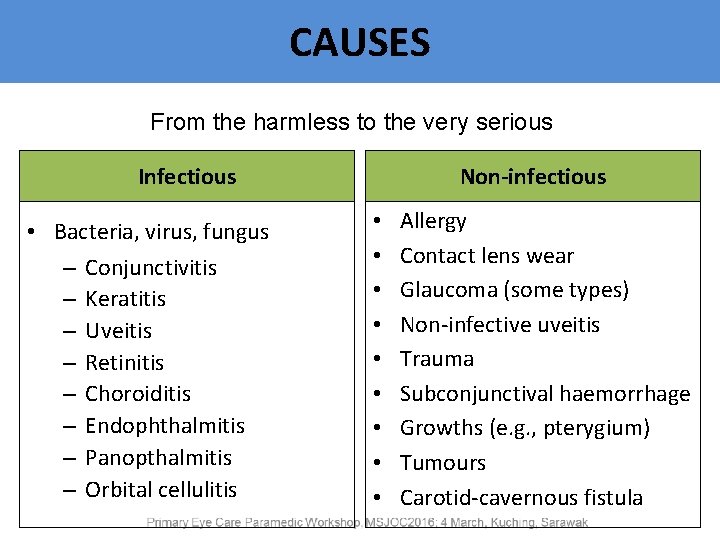
CAUSES From the harmless to the very serious Infectious • Bacteria, virus, fungus – Conjunctivitis – Keratitis – Uveitis – Retinitis – Choroiditis – Endophthalmitis – Panopthalmitis – Orbital cellulitis Non-infectious • • • Allergy Contact lens wear Glaucoma (some types) Non-infective uveitis Trauma Subconjunctival haemorrhage Growths (e. g. , pterygium) Tumours Carotid-cavernous fistula
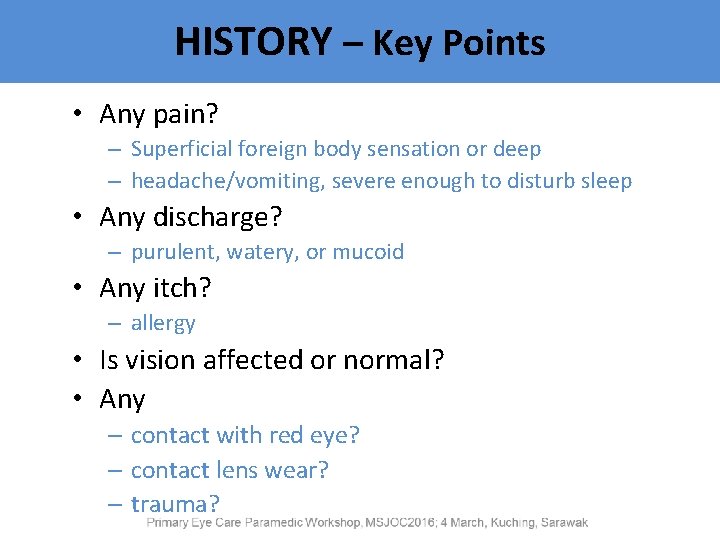
HISTORY – Key Points • Any pain? – Superficial foreign body sensation or deep – headache/vomiting, severe enough to disturb sleep • Any discharge? – purulent, watery, or mucoid • Any itch? – allergy • Is vision affected or normal? • Any – contact with red eye? – contact lens wear? – trauma?
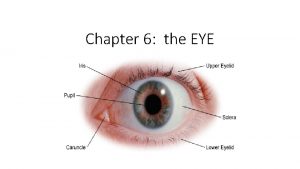
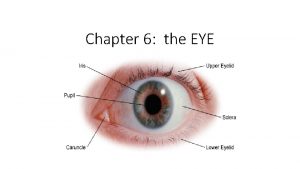
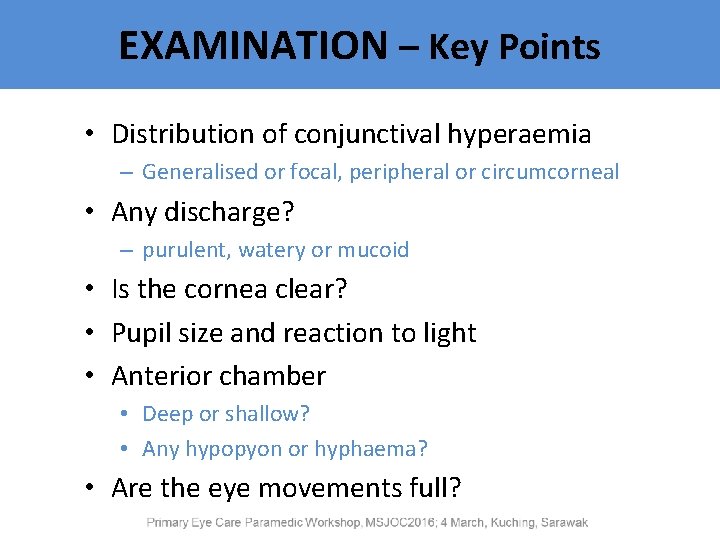
EXAMINATION – Key Points • Distribution of conjunctival hyperaemia – Generalised or focal, peripheral or circumcorneal • Any discharge? – purulent, watery or mucoid • Is the cornea clear? • Pupil size and reaction to light • Anterior chamber • Deep or shallow? • Any hypopyon or hyphaema? • Are the eye movements full?
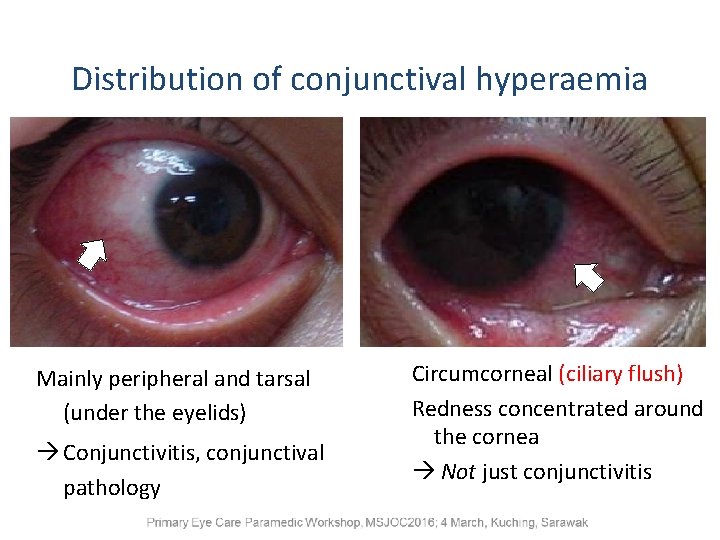
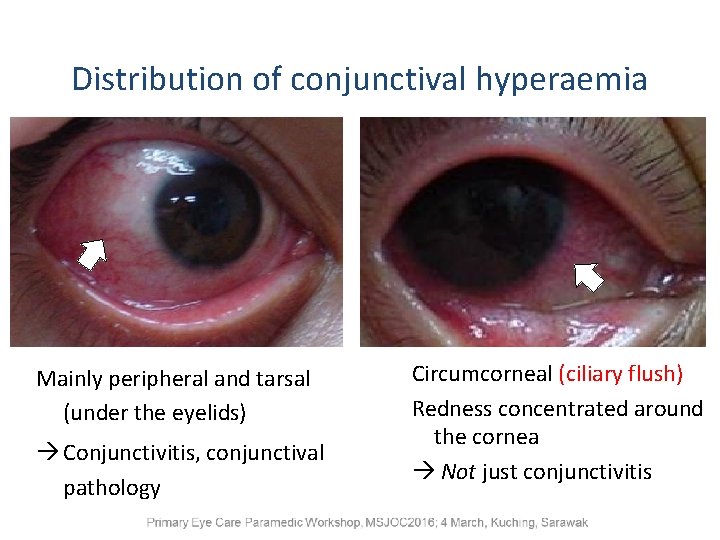
Distribution of conjunctival hyperaemia Mainly peripheral and tarsal (under the eyelids) Conjunctivitis, conjunctival pathology Circumcorneal (ciliary flush) Redness concentrated around the cornea Not just conjunctivitis
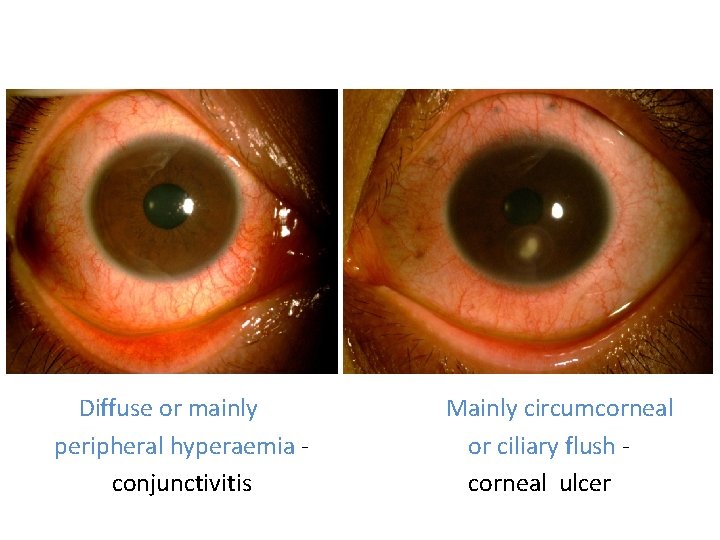
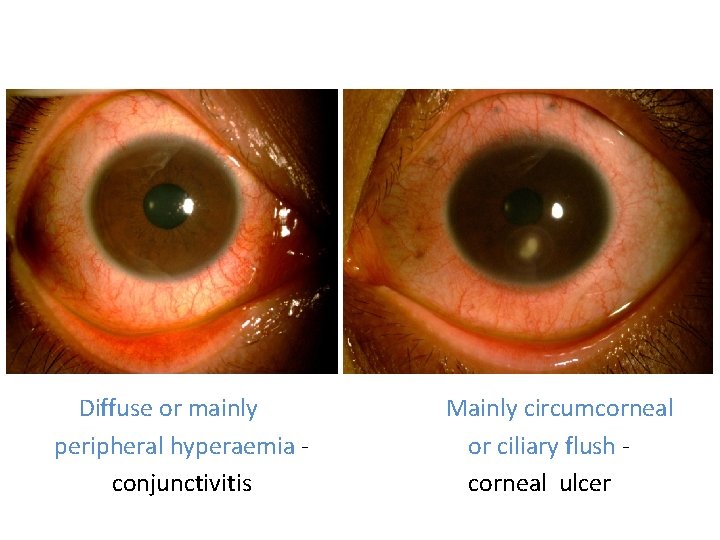
1 Diffuse or mainly peripheral hyperaemia conjunctivitis Mainly circumcorneal or ciliary flush corneal ulcer
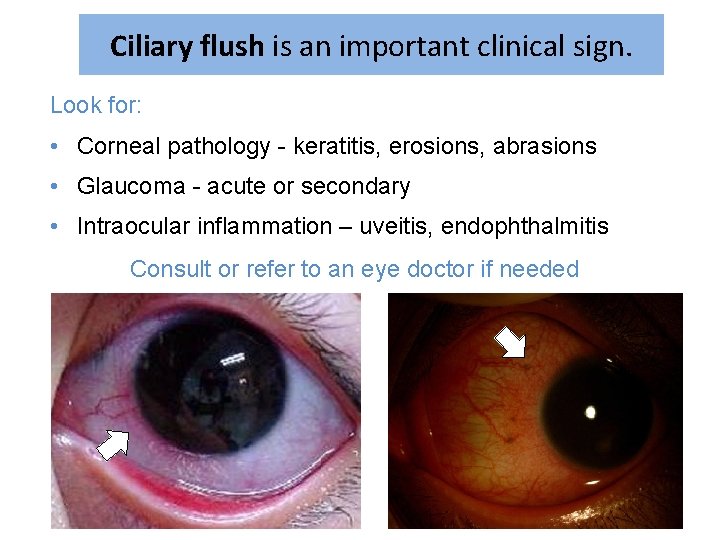
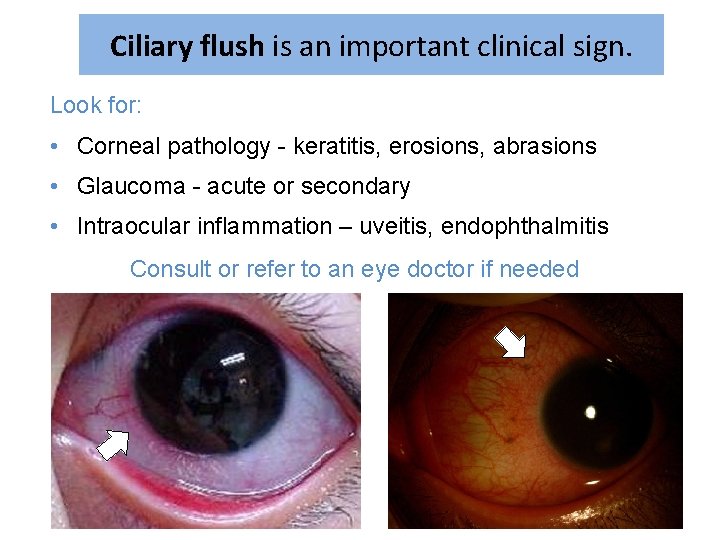
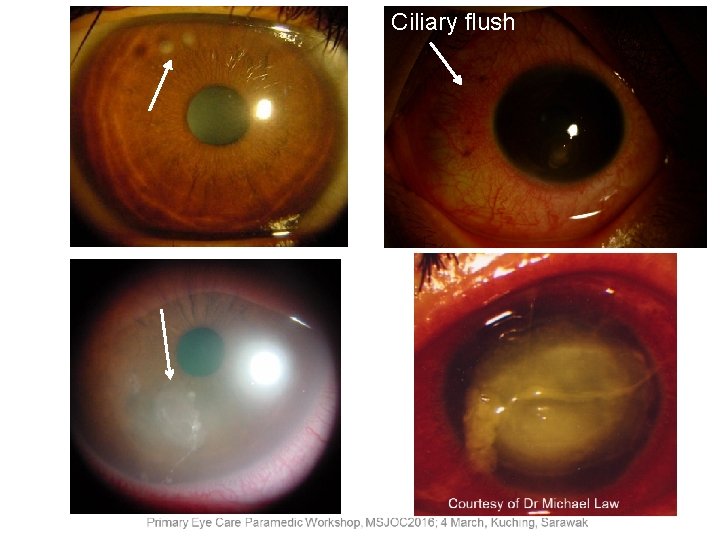
Ciliary flush is an important clinical sign. Look for: • Corneal pathology - keratitis, erosions, abrasions • Glaucoma - acute or secondary • Intraocular inflammation – uveitis, endophthalmitis Consult or refer to an eye doctor if needed
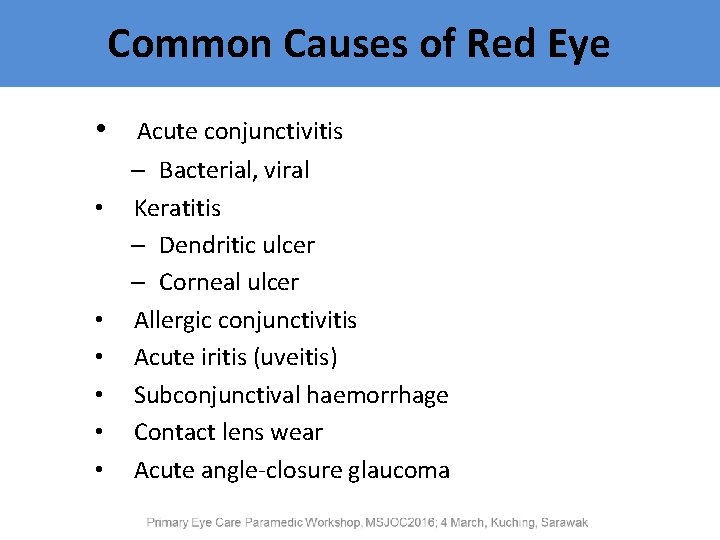
Common Causes of Red Eye • • Acute conjunctivitis – Bacterial, viral Keratitis – Dendritic ulcer – Corneal ulcer Allergic conjunctivitis Acute iritis (uveitis) Subconjunctival haemorrhage Contact lens wear Acute angle-closure glaucoma
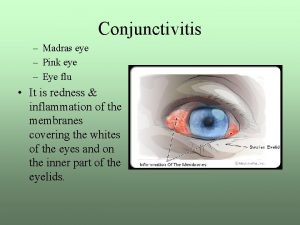
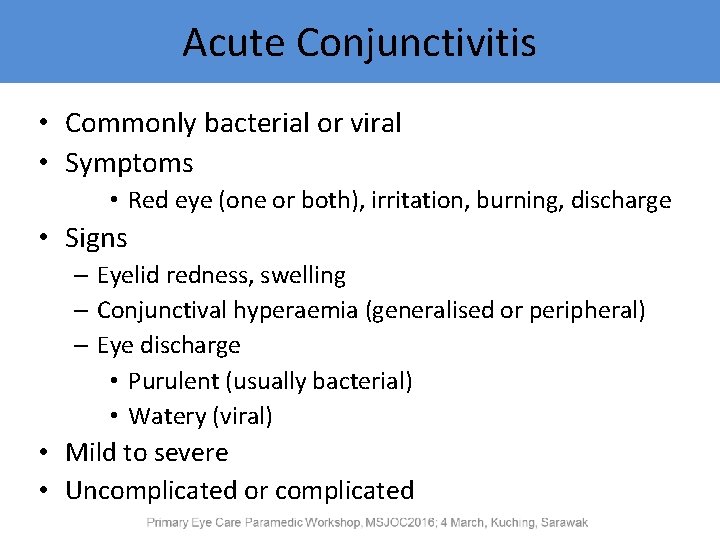
Acute Conjunctivitis • Commonly bacterial or viral • Symptoms • Red eye (one or both), irritation, burning, discharge • Signs – Eyelid redness, swelling – Conjunctival hyperaemia (generalised or peripheral) – Eye discharge • Purulent (usually bacterial) • Watery (viral) • Mild to severe • Uncomplicated or complicated
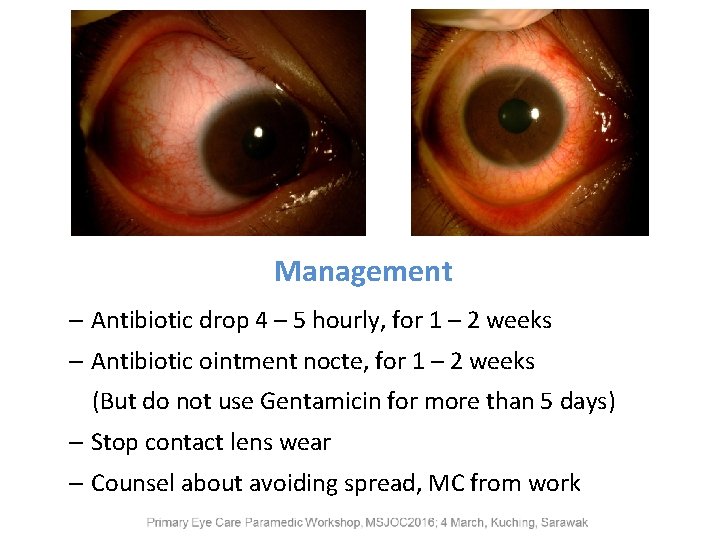
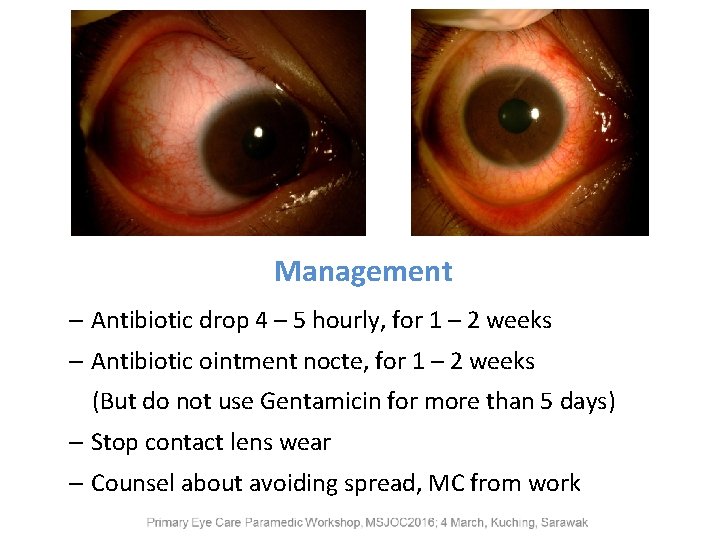
Management – Antibiotic drop 4 – 5 hourly, for 1 – 2 weeks – Antibiotic ointment nocte, for 1 – 2 weeks (But do not use Gentamicin for more than 5 days) – Stop contact lens wear – Counsel about avoiding spread, MC from work
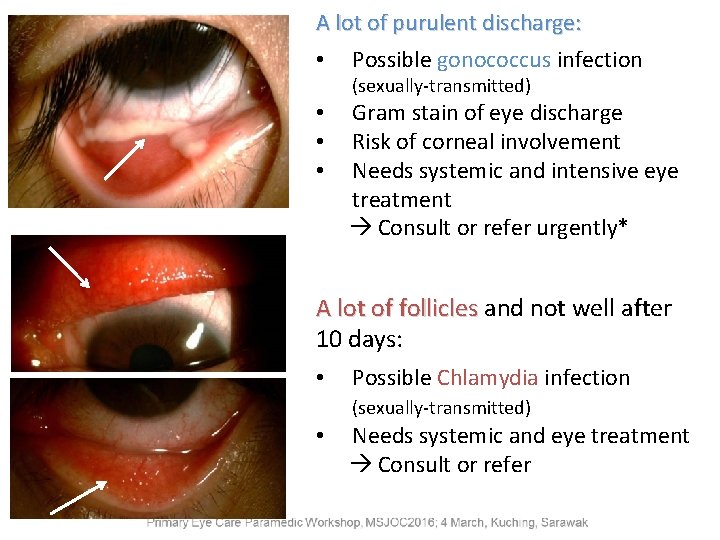
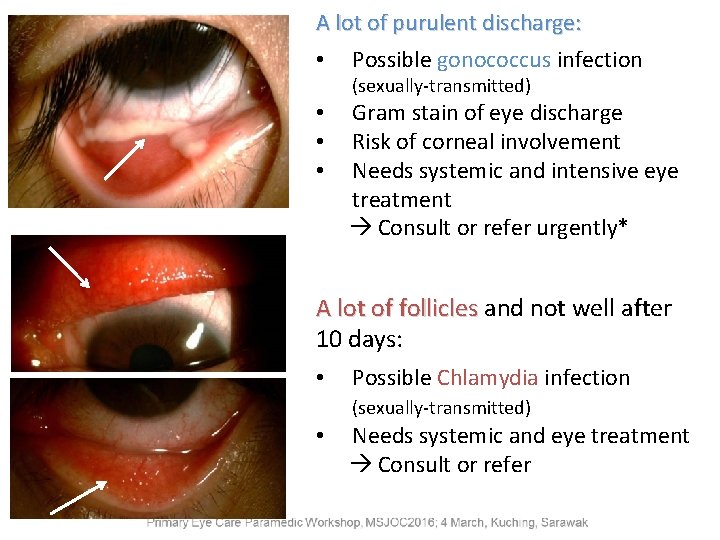
A lot of purulent discharge: • Possible gonococcus infection (sexually-transmitted) • • • Gram stain of eye discharge Risk of corneal involvement Needs systemic and intensive eye treatment Consult or refer urgently* A lot of follicles and not well after 10 days: • Possible Chlamydia infection (sexually-transmitted) • Needs systemic and eye treatment Consult or refer
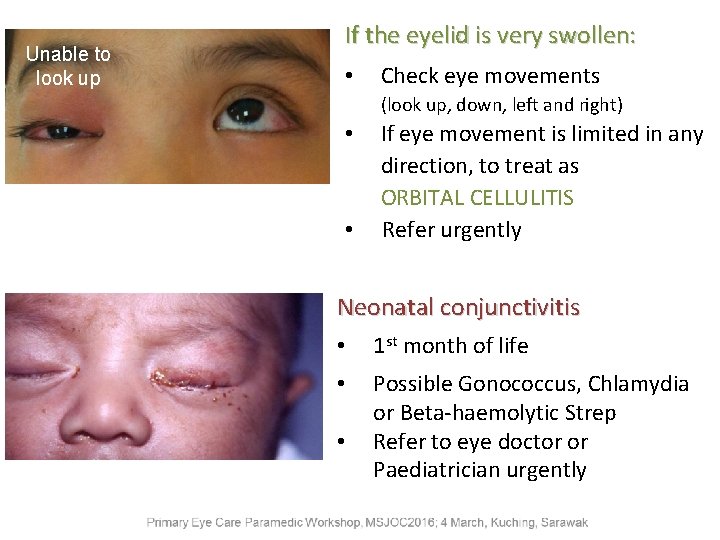
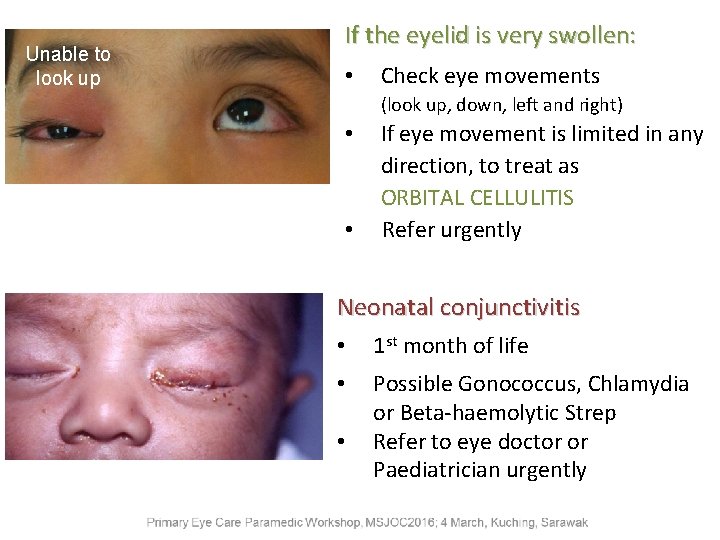
Unable to look up If the eyelid is very swollen: • Check eye movements (look up, down, left and right) • • If eye movement is limited in any direction, to treat as ORBITAL CELLULITIS Refer urgently Neonatal conjunctivitis • 1 st month of life • Possible Gonococcus, Chlamydia or Beta-haemolytic Strep Refer to eye doctor or Paediatrician urgently •
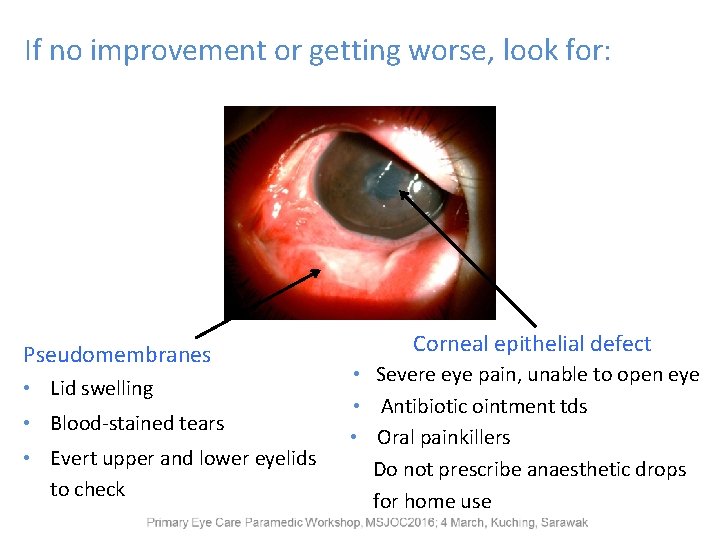
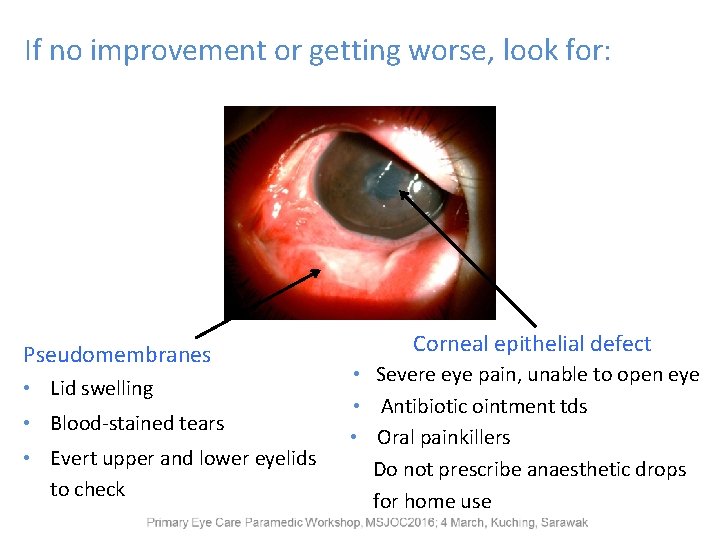
If no improvement or getting worse, look for: Pseudomembranes • Lid swelling • Blood-stained tears • Evert upper and lower eyelids to check Corneal epithelial defect • Severe eye pain, unable to open eye • Antibiotic ointment tds • Oral painkillers Do not prescribe anaesthetic drops for home use
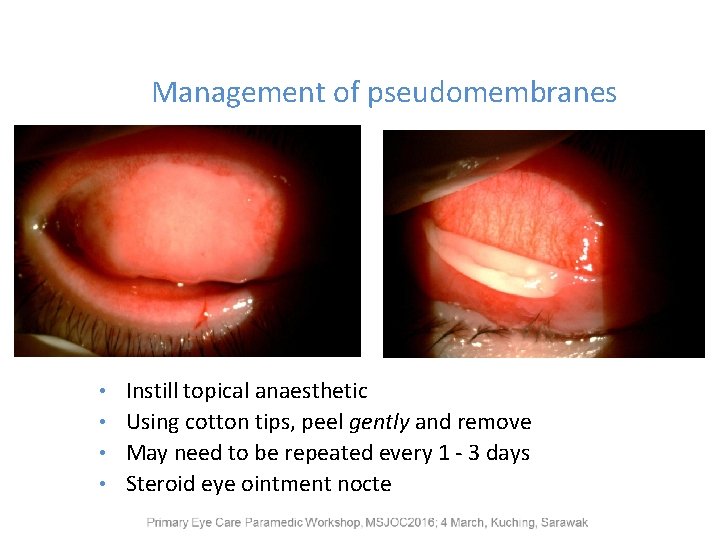
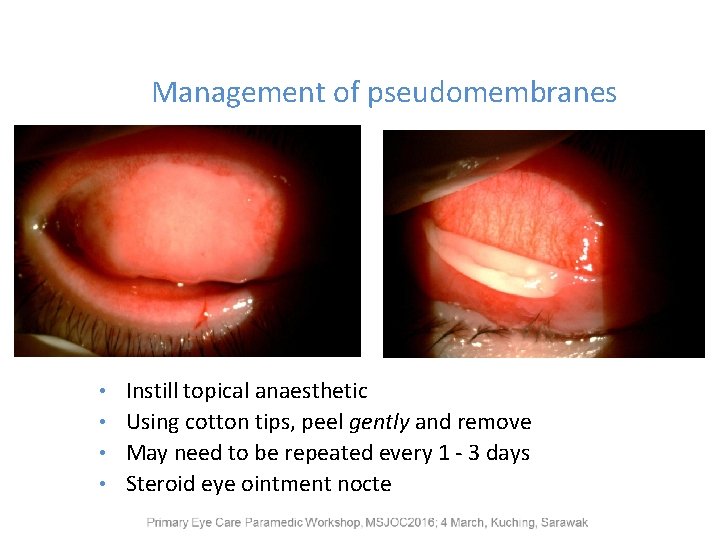
Management of pseudomembranes Instill topical anaesthetic • Using cotton tips, peel gently and remove • May need to be repeated every 1 - 3 days • Steroid eye ointment nocte •
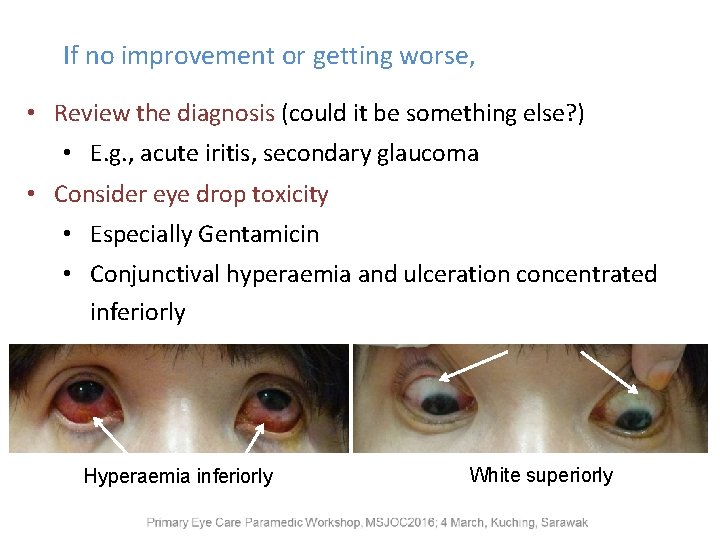
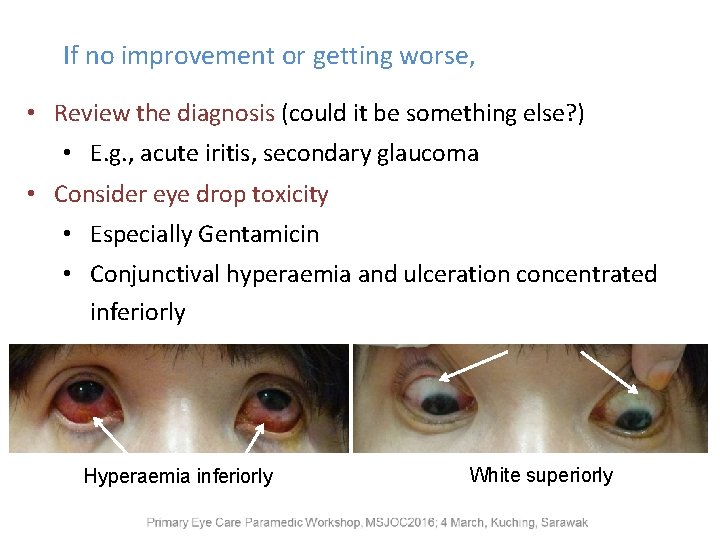
If no improvement or getting worse, • Review the diagnosis (could it be something else? ) • E. g. , acute iritis, secondary glaucoma • Consider eye drop toxicity • Especially Gentamicin • Conjunctival hyperaemia and ulceration concentrated inferiorly Hyperaemia inferiorly White superiorly
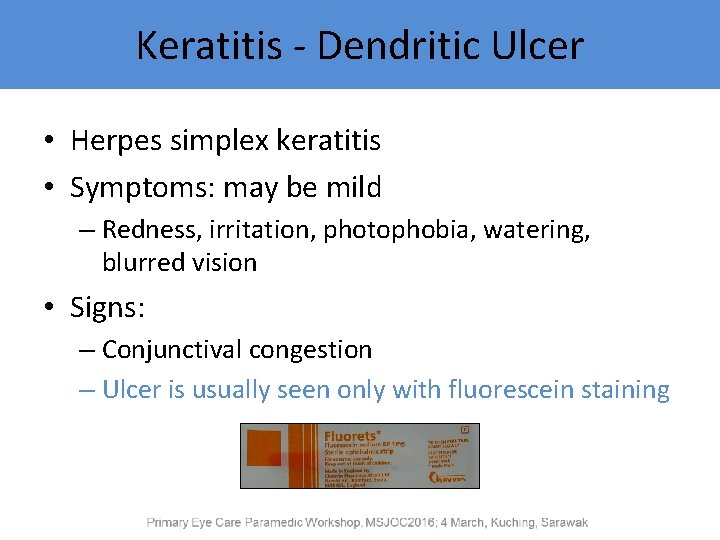
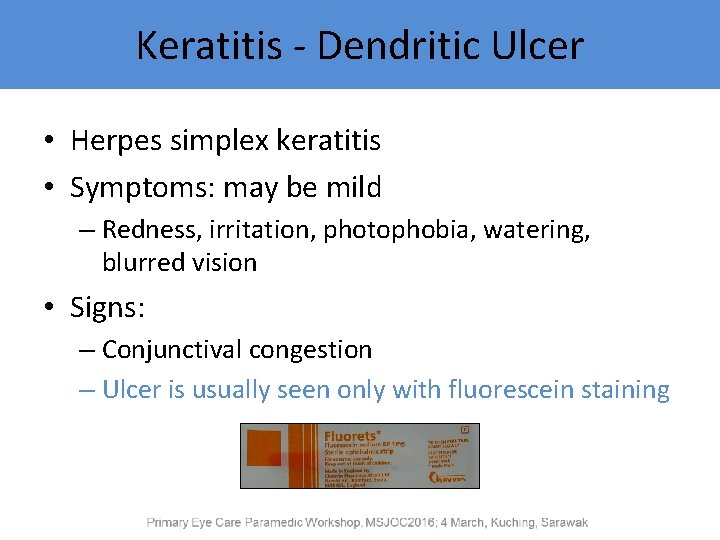
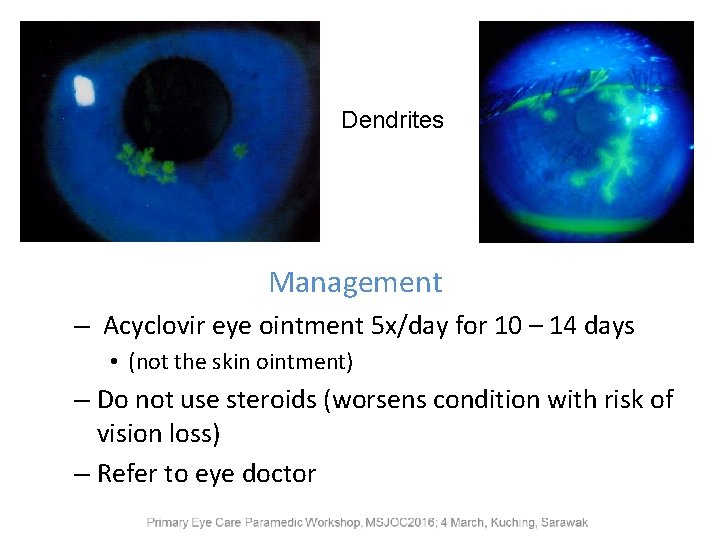
Keratitis - Dendritic Ulcer • Herpes simplex keratitis • Symptoms: may be mild – Redness, irritation, photophobia, watering, blurred vision • Signs: – Conjunctival congestion – Ulcer is usually seen only with fluorescein staining
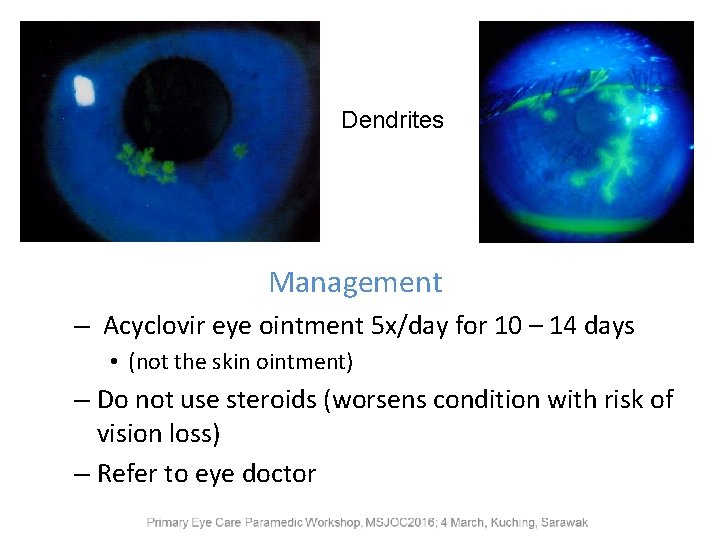
Dendrites Management – Acyclovir eye ointment 5 x/day for 10 – 14 days • (not the skin ointment) – Do not use steroids (worsens condition with risk of vision loss) – Refer to eye doctor
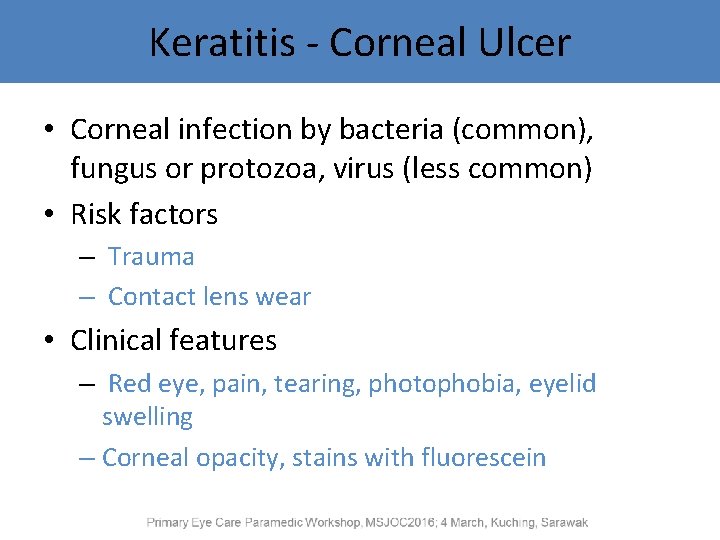
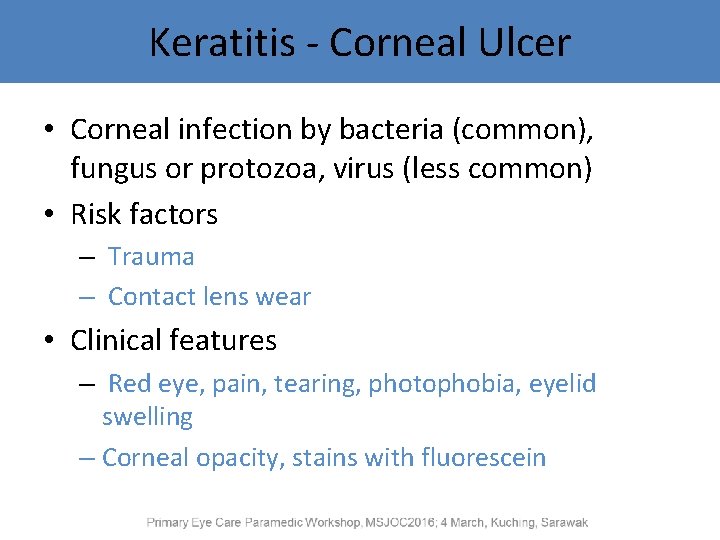
Keratitis - Corneal Ulcer • Corneal infection by bacteria (common), fungus or protozoa, virus (less common) • Risk factors – Trauma – Contact lens wear • Clinical features – Red eye, pain, tearing, photophobia, eyelid swelling – Corneal opacity, stains with fluorescein
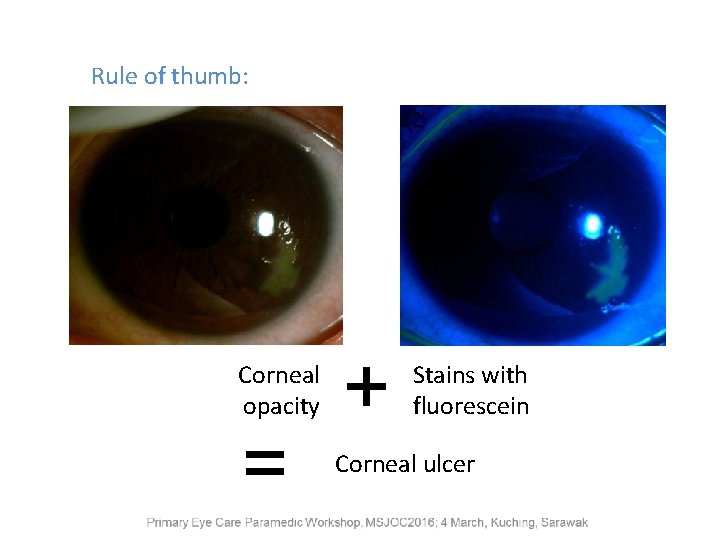
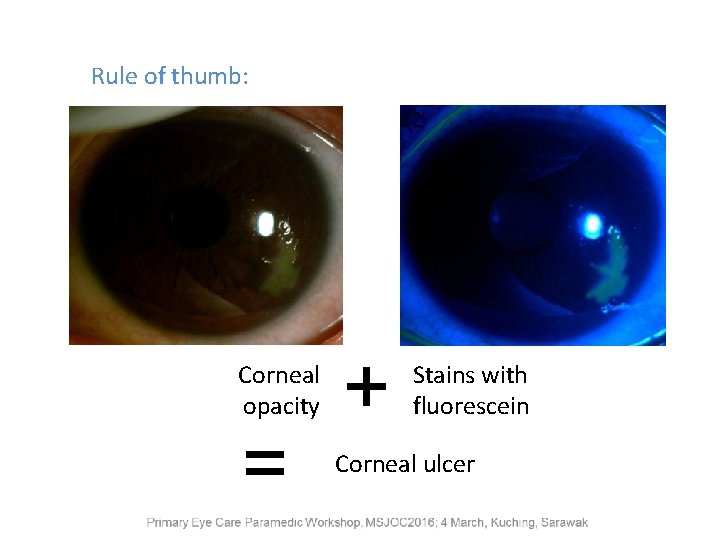
Rule of thumb: Corneal opacity = + Stains with fluorescein Corneal ulcer
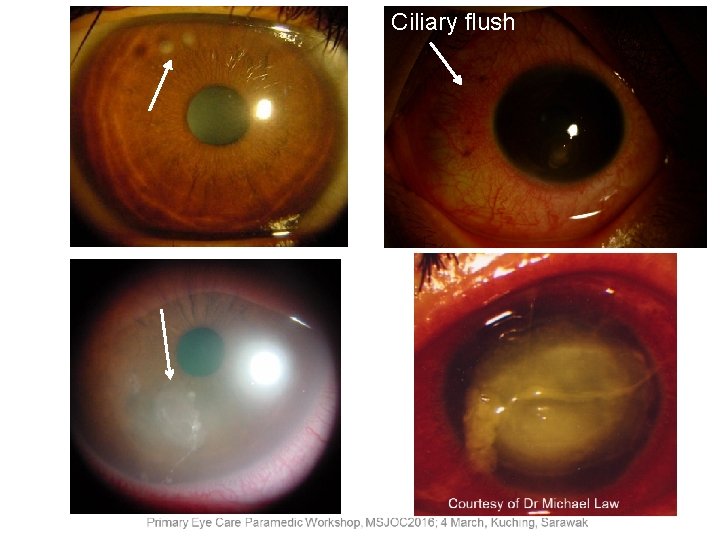
Ciliary flush Courtesy of Dr Michael Law
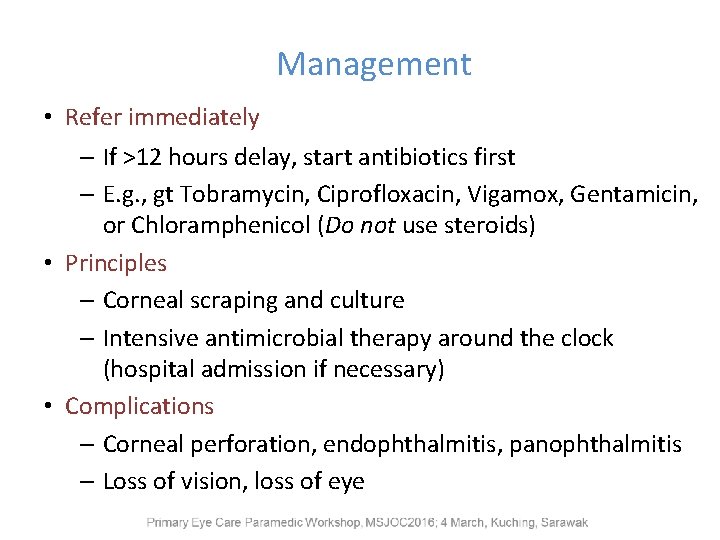
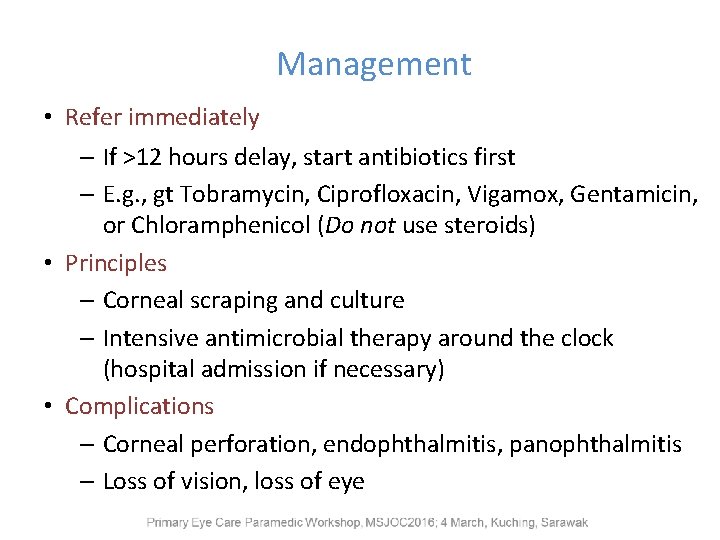
Management • Refer immediately – If >12 hours delay, start antibiotics first – E. g. , gt Tobramycin, Ciprofloxacin, Vigamox, Gentamicin, or Chloramphenicol (Do not use steroids) • Principles – Corneal scraping and culture – Intensive antimicrobial therapy around the clock (hospital admission if necessary) • Complications – Corneal perforation, endophthalmitis, panophthalmitis – Loss of vision, loss of eye
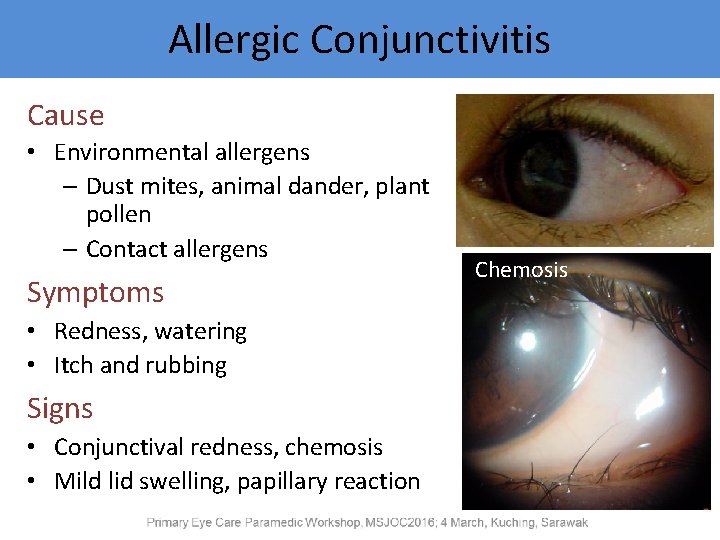
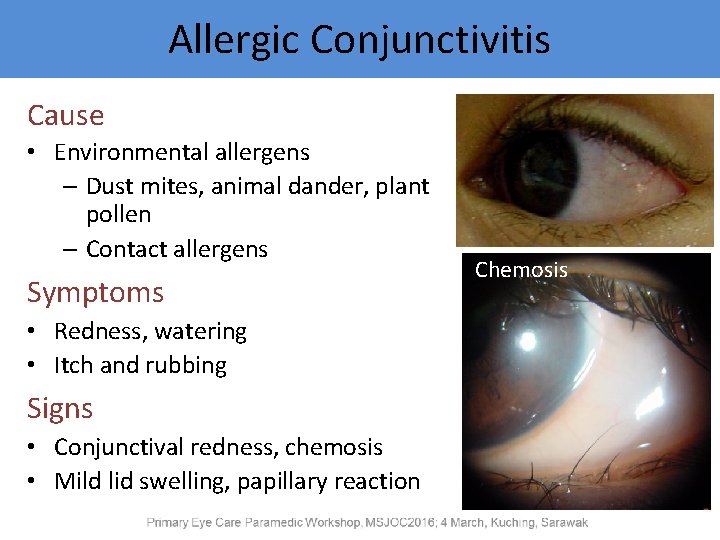
Allergic Conjunctivitis Cause • Environmental allergens – Dust mites, animal dander, plant pollen – Contact allergens Symptoms • Redness, watering • Itch and rubbing Signs • Conjunctival redness, chemosis • Mild lid swelling, papillary reaction Chemosis
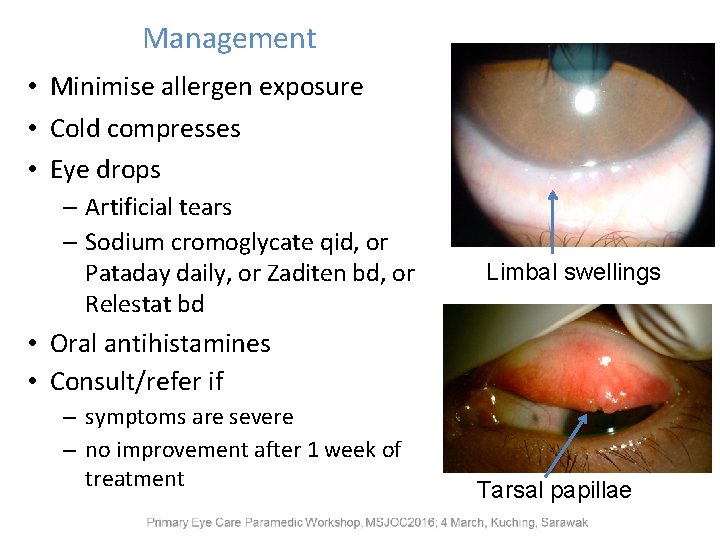
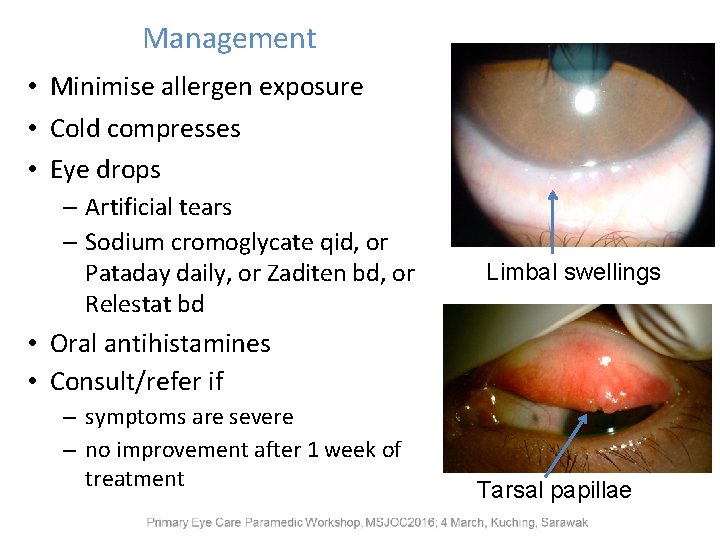
Management • Minimise allergen exposure • Cold compresses • Eye drops – Artificial tears – Sodium cromoglycate qid, or Pataday daily, or Zaditen bd, or Relestat bd Limbal swellings • Oral antihistamines • Consult/refer if – symptoms are severe – no improvement after 1 week of treatment Tarsal papillae
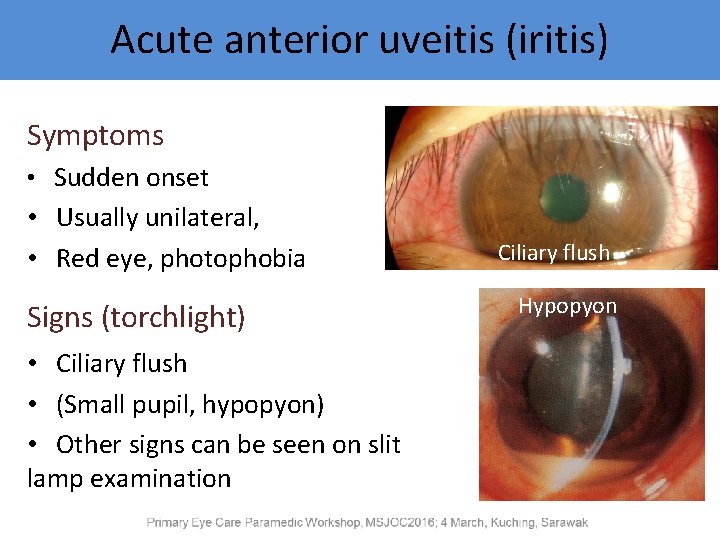
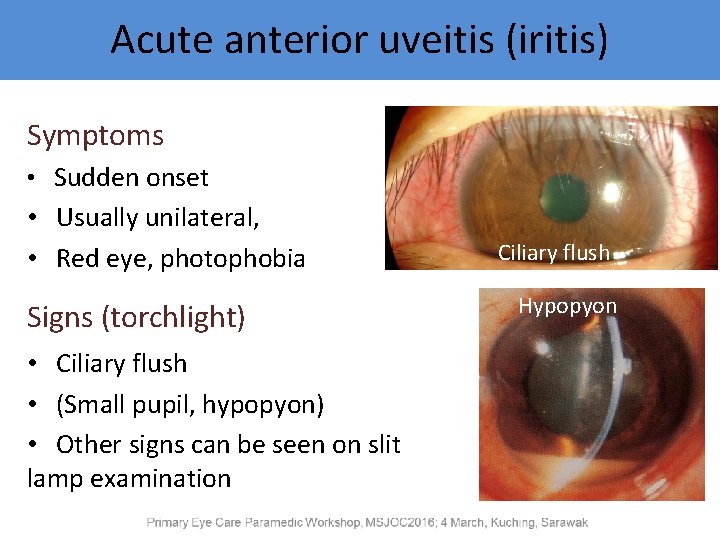
Acute anterior uveitis (iritis) Symptoms • Sudden onset • Usually unilateral, • Red eye, photophobia Signs (torchlight) • Ciliary flush • (Small pupil, hypopyon) • Other signs can be seen on slit lamp examination Ciliary flush Hypopyon
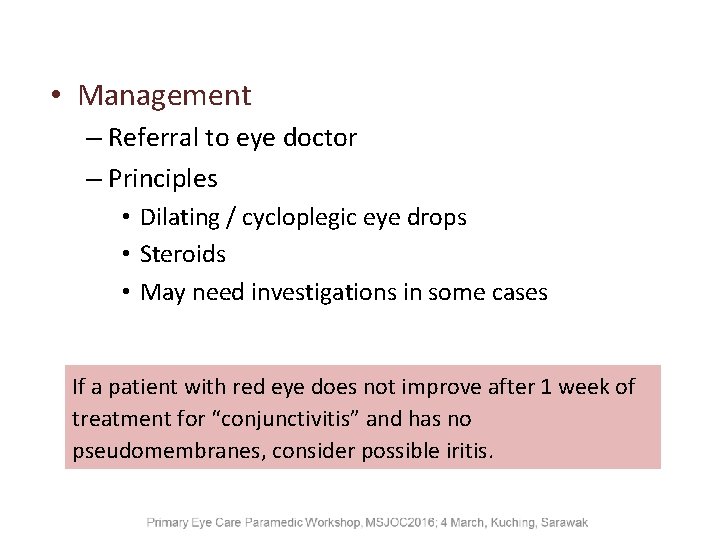
• Management – Referral to eye doctor – Principles • Dilating / cycloplegic eye drops • Steroids • May need investigations in some cases If a patient with red eye does not improve after 1 week of treatment for “conjunctivitis” and has no pseudomembranes, consider possible iritis.
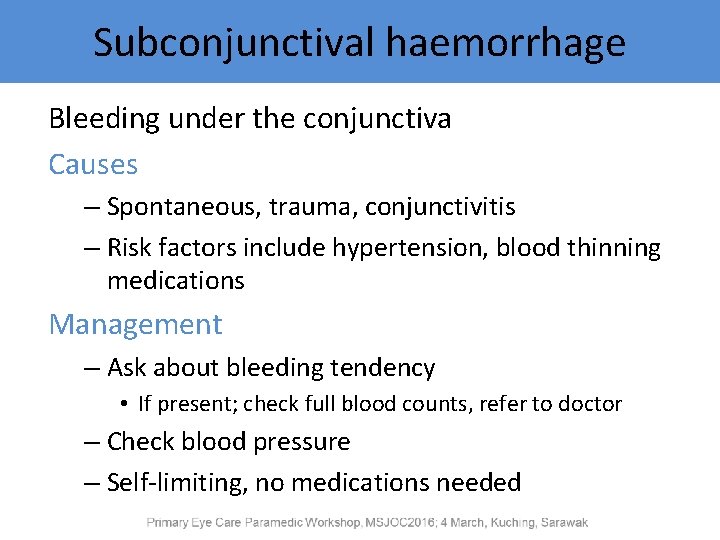
Subconjunctival haemorrhage Bleeding under the conjunctiva Causes – Spontaneous, trauma, conjunctivitis – Risk factors include hypertension, blood thinning medications Management – Ask about bleeding tendency • If present; check full blood counts, refer to doctor – Check blood pressure – Self-limiting, no medications needed
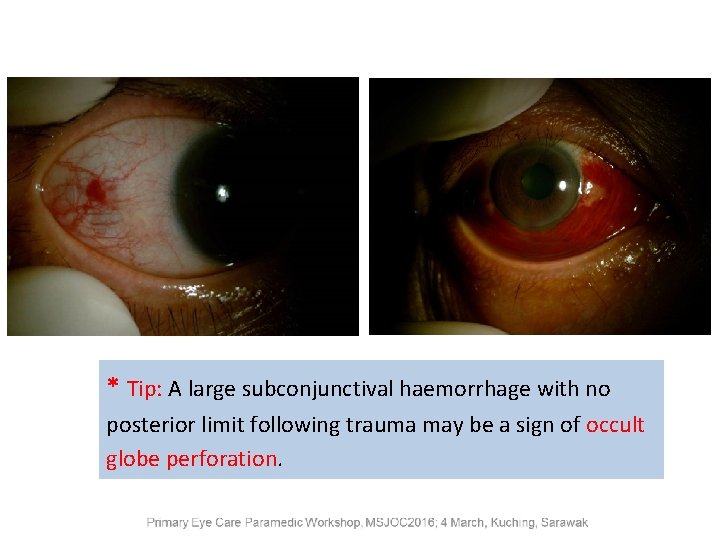
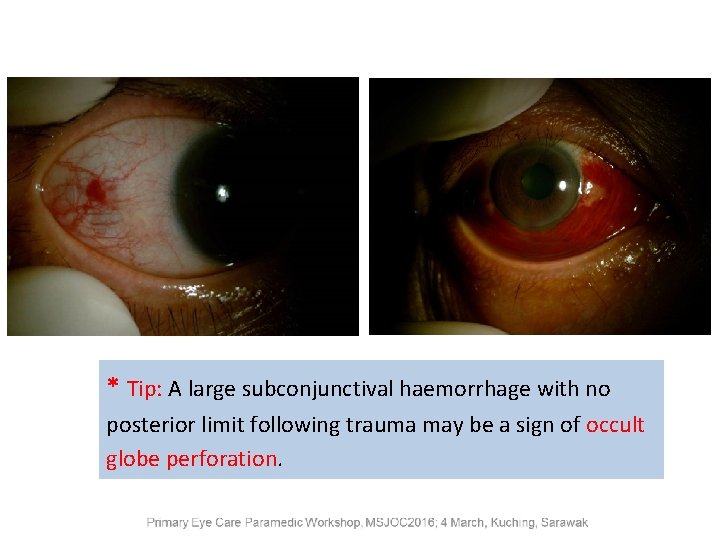
* Tip: A large subconjunctival haemorrhage with no posterior limit following trauma may be a sign of occult globe perforation.
Contact Lens Wear Complications – Poor oxygen transmission to cornea – Mechanical trauma – Allergic reaction – Infection Problems are usually related to: – Chronic wear, long wearing hours – Poor care and cleaning routine – Sleeping with lenses on – Exposure to contaminated water
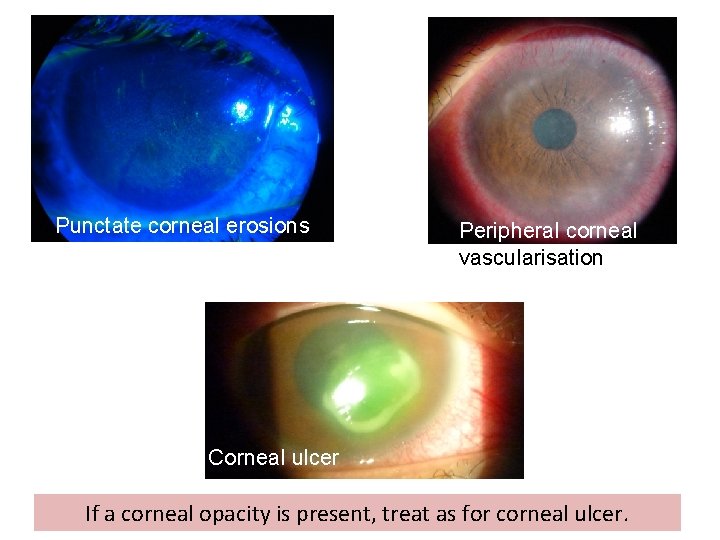
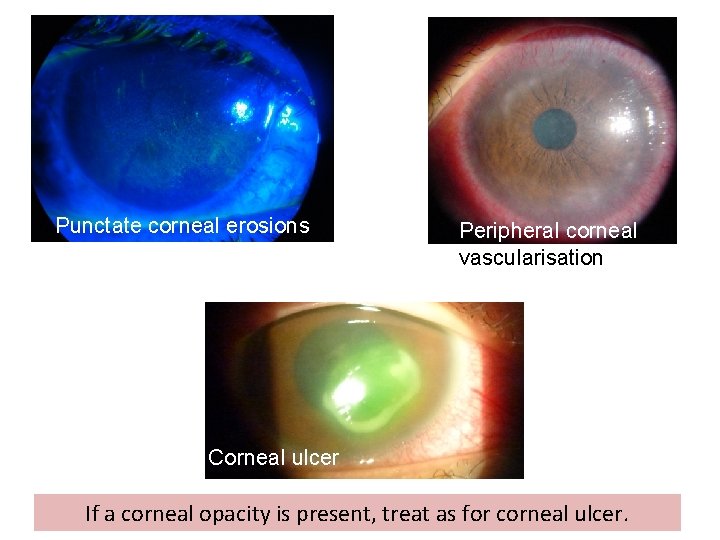
Punctate corneal erosions Peripheral corneal vascularisation Corneal ulcer If a corneal opacity is present, treat as for corneal ulcer.
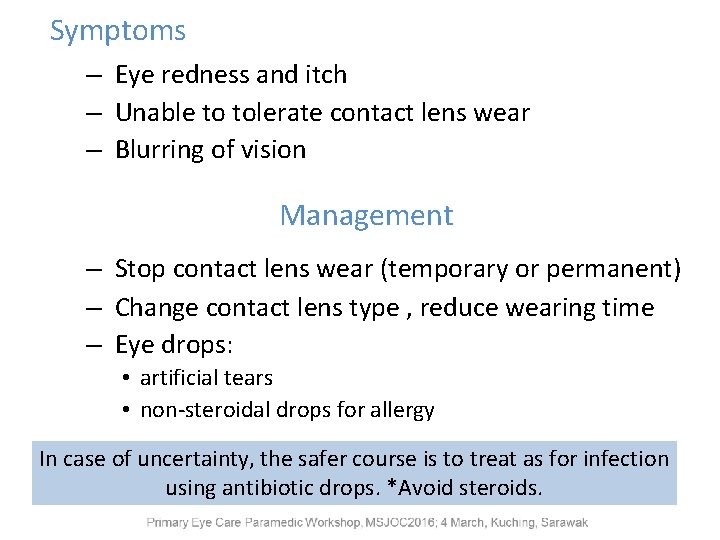
Symptoms – Eye redness and itch – Unable to tolerate contact lens wear – Blurring of vision Management – Stop contact lens wear (temporary or permanent) – Change contact lens type , reduce wearing time – Eye drops: • artificial tears • non-steroidal drops for allergy In case of uncertainty, the safer course is to treat as for infection using antibiotic drops. *Avoid steroids.
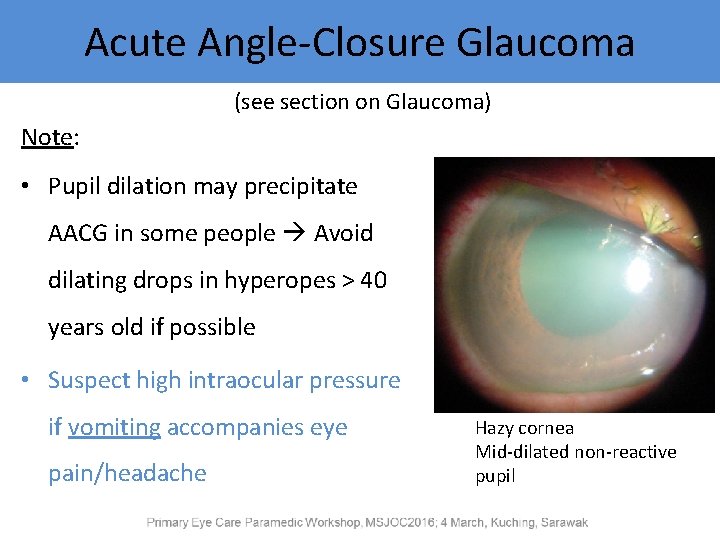
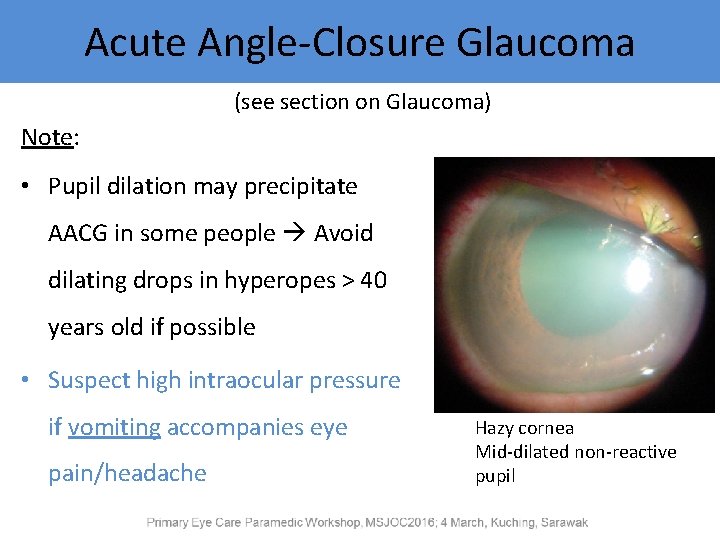
Acute Angle-Closure Glaucoma (see section on Glaucoma) Note: • Pupil dilation may precipitate AACG in some people Avoid dilating drops in hyperopes > 40 years old if possible • Suspect high intraocular pressure if vomiting accompanies eye pain/headache Hazy cornea Mid-dilated non-reactive pupil
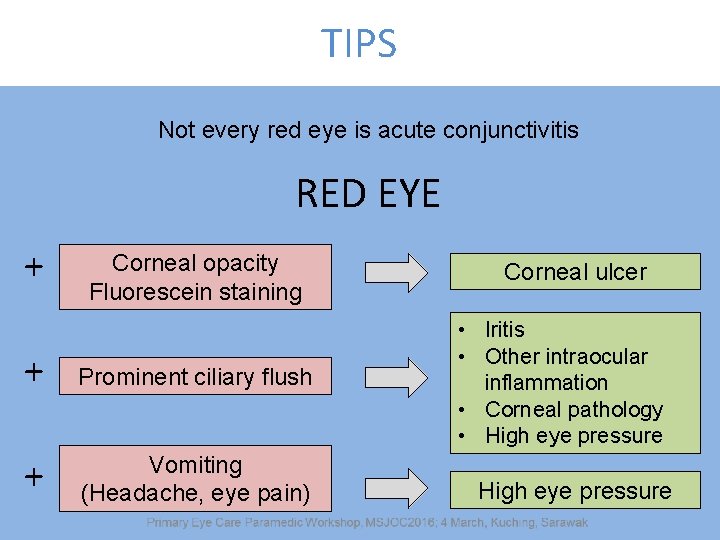
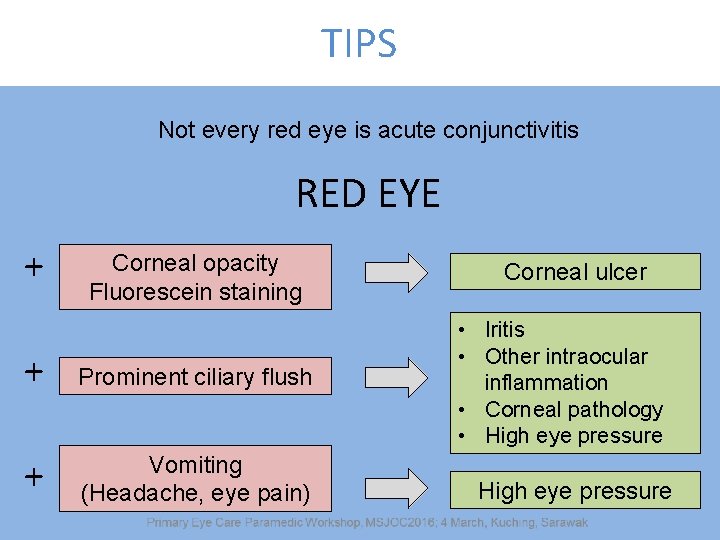
TIPS Not every red eye is acute conjunctivitis RED EYE + Corneal opacity Fluorescein staining + Prominent ciliary flush + Vomiting (Headache, eye pain) Corneal ulcer • Iritis • Other intraocular inflammation • Corneal pathology • High eye pressure
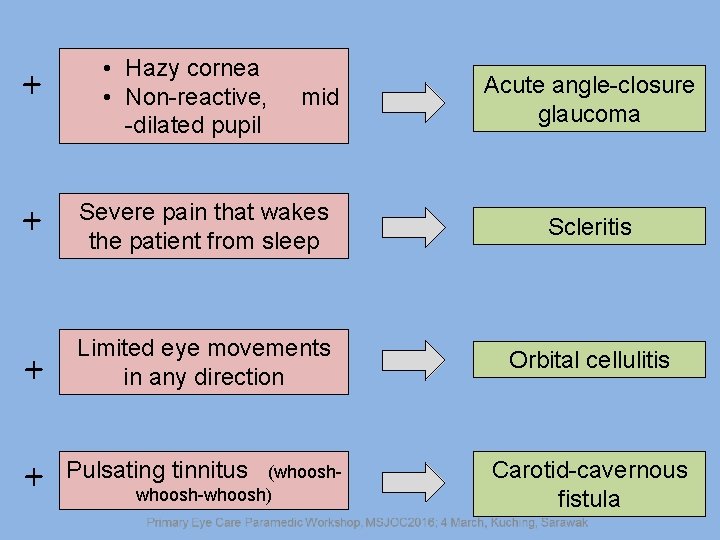
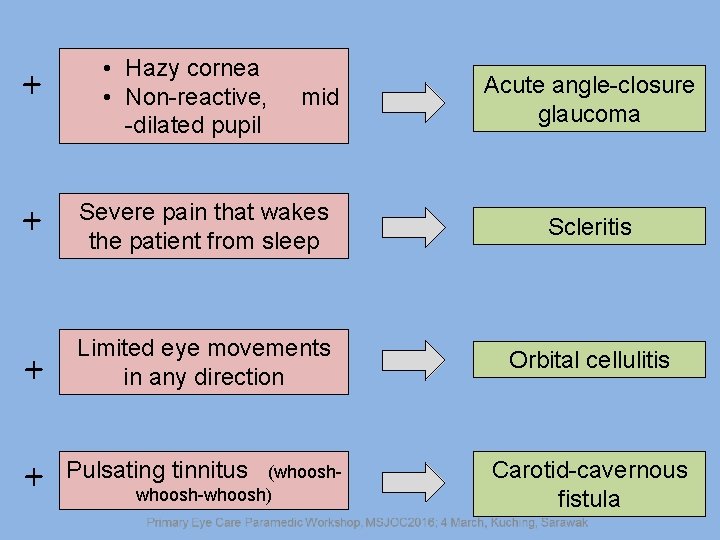
+ • Hazy cornea • Non-reactive, -dilated pupil mid Acute angle-closure glaucoma + Severe pain that wakes the patient from sleep Scleritis + Limited eye movements in any direction Orbital cellulitis + Pulsating tinnitus (whoosh-whoosh) Carotid-cavernous fistula
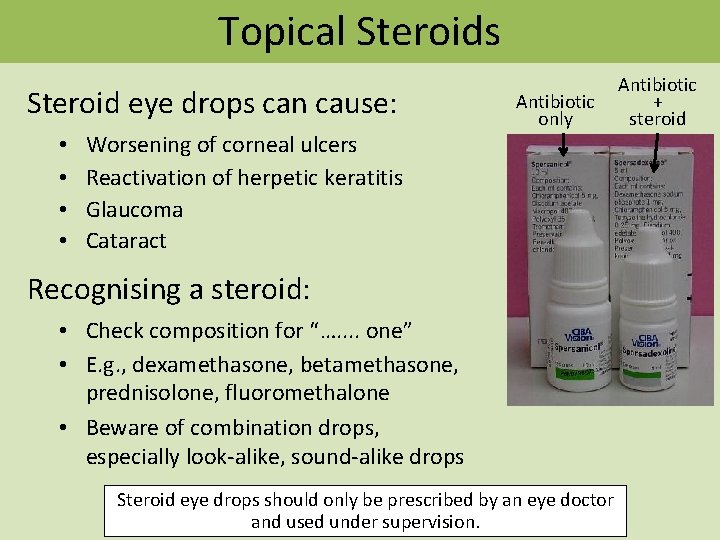
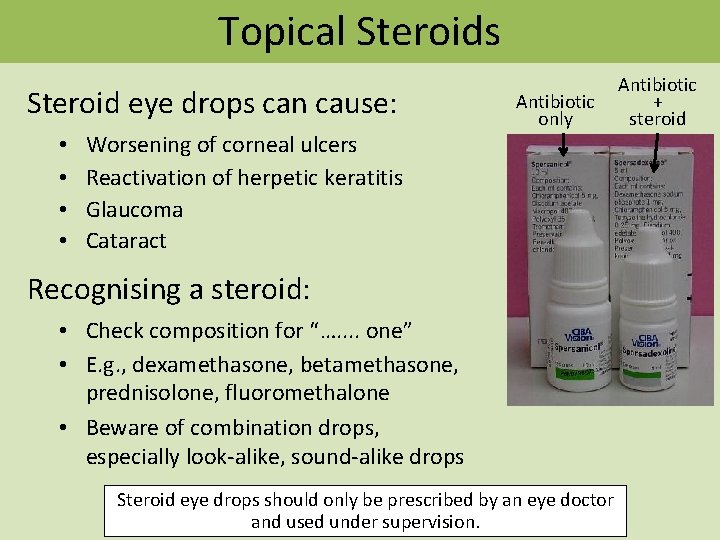
Topical Steroids Steroid eye drops can cause: • • Worsening of corneal ulcers Reactivation of herpetic keratitis Glaucoma Cataract Antibiotic only Recognising a steroid: • Check composition for “…. . one” • E. g. , dexamethasone, betamethasone, prednisolone, fluoromethalone • Beware of combination drops, especially look-alike, sound-alike drops Steroid eye drops should only be prescribed by an eye doctor and used under supervision. Antibiotic + steroid

Thank you
 United healthcare community plan primary care providers
United healthcare community plan primary care providers Neonlab
Neonlab Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine meaning
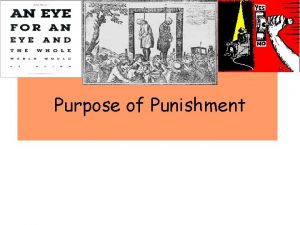
Sports medicine meaning Eye for an eye code
Eye for an eye code Worms eye view example
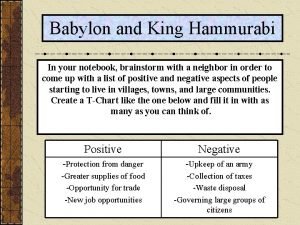
Worms eye view example Hammurabi code eye for an eye
Hammurabi code eye for an eye Healthy eyes vs anemic eyes
Healthy eyes vs anemic eyes Code of hammurabi activity
Code of hammurabi activity An eye for an eye a tooth for a tooth sister act
An eye for an eye a tooth for a tooth sister act Blue eyes genetics
Blue eyes genetics An eye for an eye meaning
An eye for an eye meaning Every eye is an eye
Every eye is an eye Who guidelines for primary eye care
Who guidelines for primary eye care Who guidelines for primary eye care
Who guidelines for primary eye care Differential diagnosis red eye
Differential diagnosis red eye Cojunctivitis
Cojunctivitis Traffic lights afl
Traffic lights afl Loyalty spaarsysteem
Loyalty spaarsysteem Teta offices
Teta offices Local 237 union
Local 237 union Education hub acca
Education hub acca Adit registration
Adit registration Minnesota interlock program
Minnesota interlock program Masshealth dental providers portal
Masshealth dental providers portal Office of government wide policy
Office of government wide policy The basic value proposition of community providers is:
The basic value proposition of community providers is: Tourism service suppliers
Tourism service suppliers 3pi logistics vendors
3pi logistics vendors Digital media content providers
Digital media content providers Wyoming medicaid trust
Wyoming medicaid trust Teacher professional development in kenya
Teacher professional development in kenya My ohio hcp
My ohio hcp Mdu internet providers
Mdu internet providers Register of apprenticeship training providers
Register of apprenticeship training providers Cigna allegiance providers
Cigna allegiance providers