1 Outline Define social determinants and health disparities







- Slides: 46
1

Outline • Define social determinants and health disparities • Measures of Health Disparities and Quality • Tipping Health Care in the Right Direction - Collecting race/ethnicity data - Public Reporting - Identifying Social Determinants - Population Health
Defining Social Determinants* Conditions in which people are born, grow, live, work, and age that are shaped by distribution of money, power, and resources at all levels* *World Health Organization. Social Determinants of Health. www. who. int/social_determinants/sdh_definition/en.
Social Determinants - Wealth • White median family wealth $171, 000 • 10 X more than blacks ($17, 600) • 8 X more than Hispanics ($20, 700) • 40% of black retirees and 50% of Hispanic retirees indicate that poor health contributed to decision about when to retire, compared to 26% of whites *https: //www. federalreserve. gov/publications/files/2016 -report-economic-well-being-us-households 201705. pdf 4
Health Disparities* Preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations *CDC. Community Health and Program Services (CHAPS): Health Disparities Among Racial/Ethnic Populations. Atlanta: U. S. Department of Health and Human Services; 2008
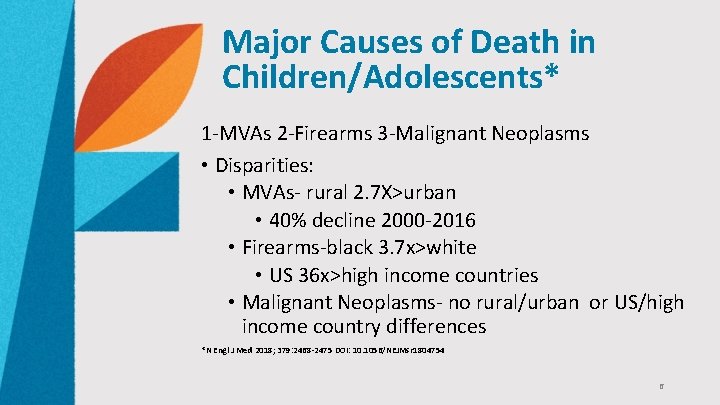
Major Causes of Death in Children/Adolescents* 1 -MVAs 2 -Firearms 3 -Malignant Neoplasms • Disparities: • MVAs- rural 2. 7 X>urban • 40% decline 2000 -2016 • Firearms-black 3. 7 x>white • US 36 x>high income countries • Malignant Neoplasms- no rural/urban or US/high income country differences *N Engl J Med 2018; 379: 2468 -2475 DOI: 10. 1056/NEJMsr 1804754 6
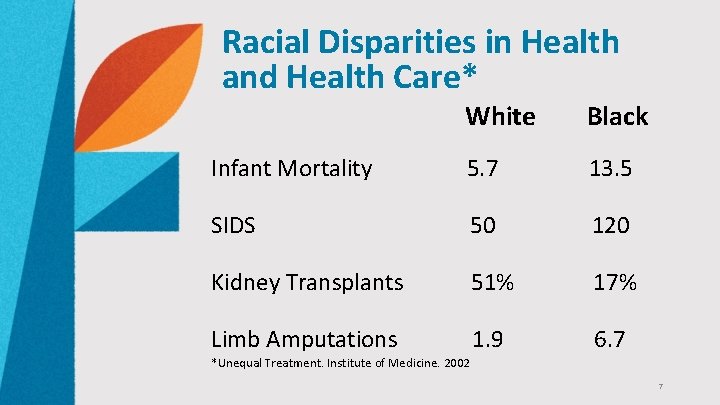
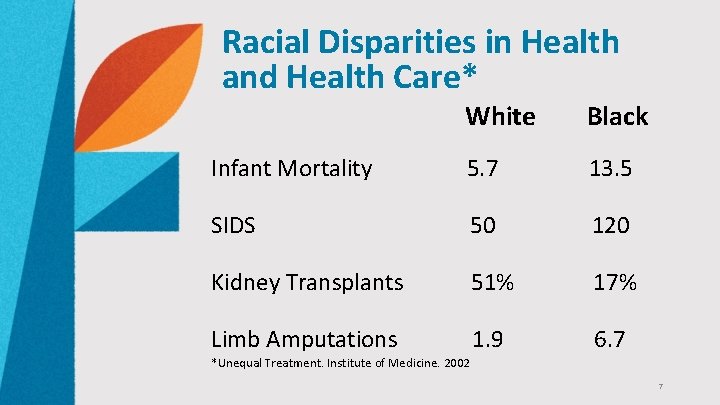
Racial Disparities in Health and Health Care* White Black Infant Mortality 5. 7 13. 5 SIDS 50 120 Kidney Transplants 51% 17% Limb Amputations 1. 9 6. 7 *Unequal Treatment. Institute of Medicine. 2002 7
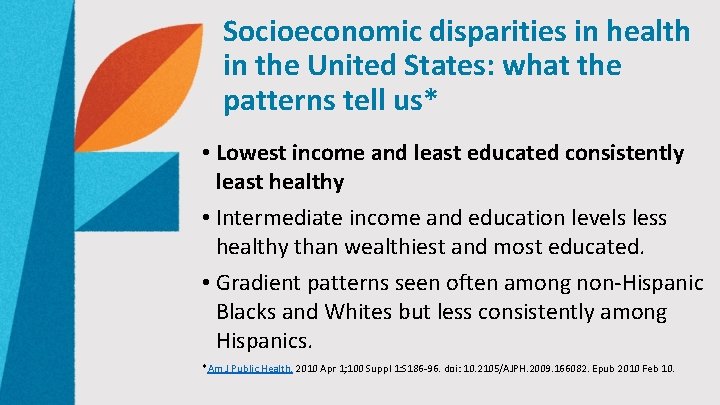
Socioeconomic disparities in health in the United States: what the patterns tell us* • Lowest income and least educated consistently least healthy • Intermediate income and education levels less healthy than wealthiest and most educated. • Gradient patterns seen often among non-Hispanic Blacks and Whites but less consistently among Hispanics. *Am J Public Health. 2010 Apr 1; 100 Suppl 1: S 186 -96. doi: 10. 2105/AJPH. 2009. 166082. Epub 2010 Feb 10.
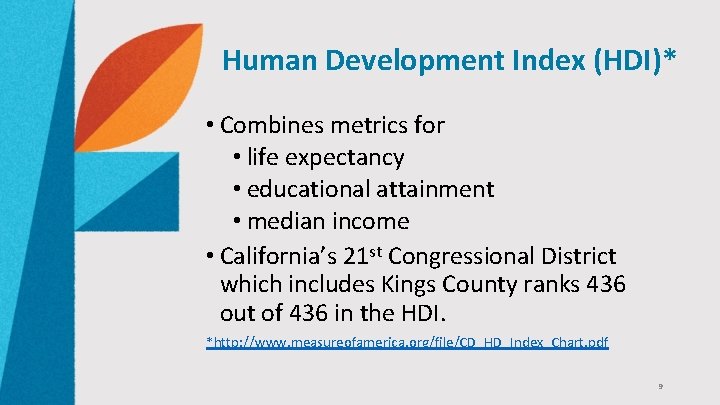
Human Development Index (HDI)* • Combines metrics for • life expectancy • educational attainment • median income • California’s 21 st Congressional District which includes Kings County ranks 436 out of 436 in the HDI. *http: //www. measureofamerica. org/file/CD_HD_Index_Chart. pdf 9
National Healthcare Disparities Report (NHDR)* • Agency for Healthcare Research and Quality (AHRQ) • Disparities in access, quality, and health outcomes • Associated with race, ethnicity, and income *Internet Citation: 2017 National Healthcare Quality and Disparities Report. Content last reviewed September 2018. Agency for Healthcare Research and Quality, Rockville, MD. http: //www. ahrq. gov/research/findings/nhqrdr/nhqdr 17/index. html

Health Equity Report 2017* *Health Resources and Services Administration , Office of Health Equity Report 2017. Rockville, Maryland: U. S. Department of Health and Human Services; 2018. Marked disparities found in health indicators, including: • infant mortality • Disability • life expectancy • mental health • cardiovascular disease • Cancer • Diabetes • COPD • HIV/AIDS • health care access and utilization • health insurance • Leading causes of death • preventive health services such as cervical, breast, and colorectal cancer screening • Smoking • Obesity • substance use • Suicide • Homicide • unintentional injuries

Defining Quality* • Timely • Safe • Effective • Efficient • Patient centered • Equitable-aka no disparities! * IOM. Crossing the Quality Chasm. 2001
Triple Aim of Health Care* • Improving experience of individual • Quality • Patient Satisfaction • Improving health of population • Reducing cost per capita • *Health Aff (Millwood). 2008 May-Jun; 27(3): 759 -69. doi: 10. 1377/hlthaff. 27. 3. 759. The triple aim: care, health, and cost. Berwick DM(1), Nolan TW, Whittington J.
HEDIS • Health Plan and Employer Data and Information Set • Set of performance measures developed by NCQA • Used in NCQA voluntary accreditation process • Enables HMOs to be compared at state, regional and national level • Does not account for social determinants of health • Collects demographics/race/ethnicity for Medicare programs • Not commercial markets
HEDIS Disparities in Medicare* • HEDIS outcome measures for black enrollees 6. 8% to 14. 4% <white enrollees Conclusions: • Disparities weakly correlated with overall quality. • Plan-specific performance reports of racial disparities on outcome measures would provide useful information not currently conveyed by standard HEDIS reports. *Relationship Between Quality of Care and Racial Disparities in Medicare Health Plans Amal N. Trivedi; Alan M. Zaslavsky; Eric C. Schneider; John Z. Ayanian JAMA. 2006; 296: 1998 -2004
Impact of Access on HEDIS Scores • Access measures associated with higher quality* • Primary doctor • Number of visits *Zaslavsky AM. Med Care. 2000; 38(10): 981 -992 • HEDIS quality measures*: • Positively correlated with outpatient care • Negatively associated with inpatient days *Scholle et al. The Relationship Between Quality and Utilization in Managed Care. Am J Managed Care. 2005; 11: 521 -527
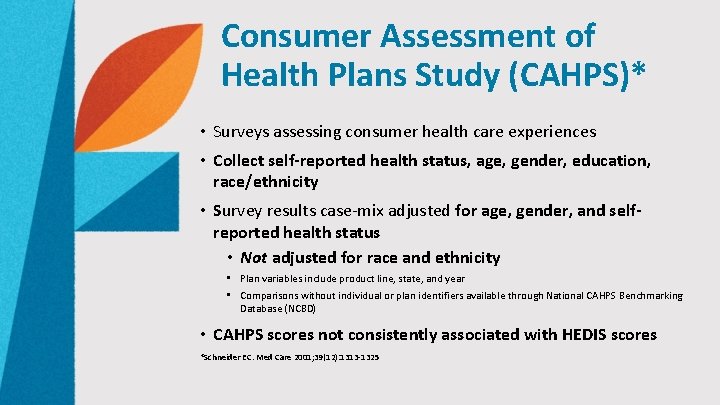
Consumer Assessment of Health Plans Study (CAHPS)* • Surveys assessing consumer health care experiences • Collect self-reported health status, age, gender, education, race/ethnicity • Survey results case-mix adjusted for age, gender, and selfreported health status • Not adjusted for race and ethnicity • Plan variables include product line, state, and year • Comparisons without individual or plan identifiers available through National CAHPS Benchmarking Database (NCBD) • CAHPS scores not consistently associated with HEDIS scores *Schneider EC. Med Care 2001; 39(12): 1313 -1325
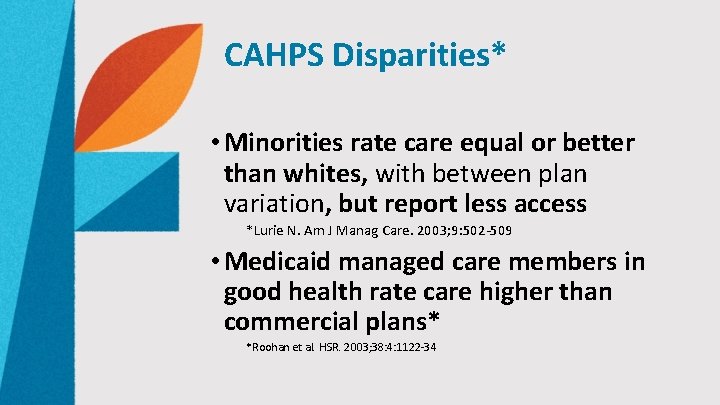
CAHPS Disparities* • Minorities rate care equal or better than whites, with between plan variation, but report less access *Lurie N. Am J Manag Care. 2003; 9: 502 -509 • Medicaid managed care members in good health rate care higher than commercial plans* *Roohan et al. HSR. 2003; 38: 4: 1122 -34
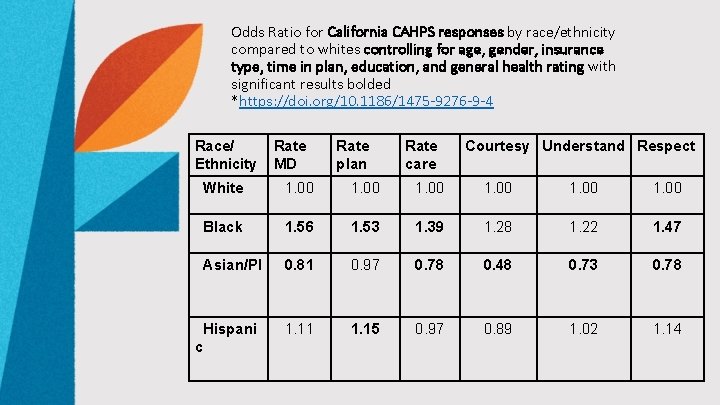
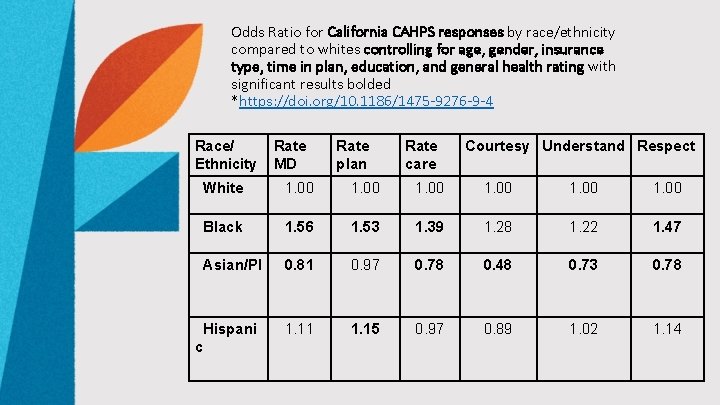
Odds Ratio for California CAHPS responses by race/ethnicity compared to whites controlling for age, gender, insurance type, time in plan, education, and general health rating with significant results bolded *https: //doi. org/10. 1186/1475 -9276 -9 -4 Race/ Ethnicity Rate MD Rate plan Rate care Courtesy Understand Respect White 1. 00 Black 1. 56 1. 53 1. 39 1. 28 1. 22 1. 47 Asian/PI 0. 81 0. 97 0. 78 0. 48 0. 73 0. 78 1. 11 1. 15 0. 97 0. 89 1. 02 1. 14 Hispani c
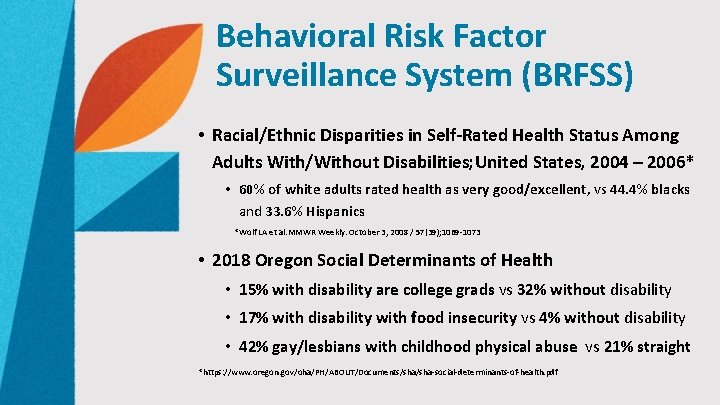
Behavioral Risk Factor Surveillance System (BRFSS) • Racial/Ethnic Disparities in Self-Rated Health Status Among Adults With/Without Disabilities; United States, 2004 – 2006* • 60% of white adults rated health as very good/excellent, vs 44. 4% blacks and 33. 6% Hispanics *Wolf LA et al. MMWR Weekly. October 3, 2008 / 57(39); 1069 -1073 • 2018 Oregon Social Determinants of Health • 15% with disability are college grads vs 32% without disability • 17% with disability with food insecurity vs 4% without disability • 42% gay/lesbians with childhood physical abuse vs 21% straight *https: //www. oregon. gov/oha/PH/ABOUT/Documents/sha-social-determinants-of-health. pdf
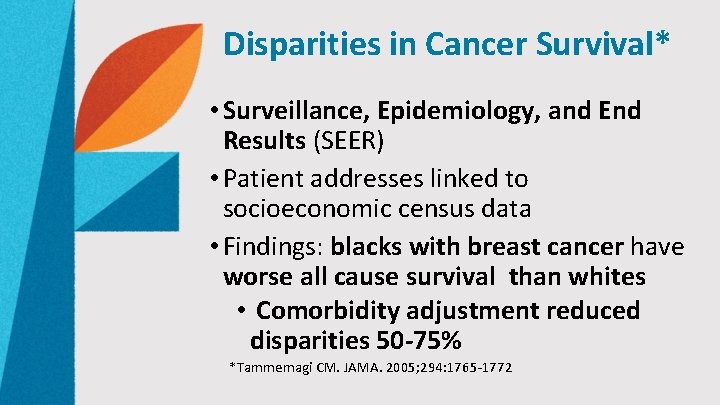
Disparities in Cancer Survival* • Surveillance, Epidemiology, and End Results (SEER) • Patient addresses linked to socioeconomic census data • Findings: blacks with breast cancer have worse all cause survival than whites • Comorbidity adjustment reduced disparities 50 -75% *Tammemagi CM. JAMA. 2005; 294: 1765 -1772
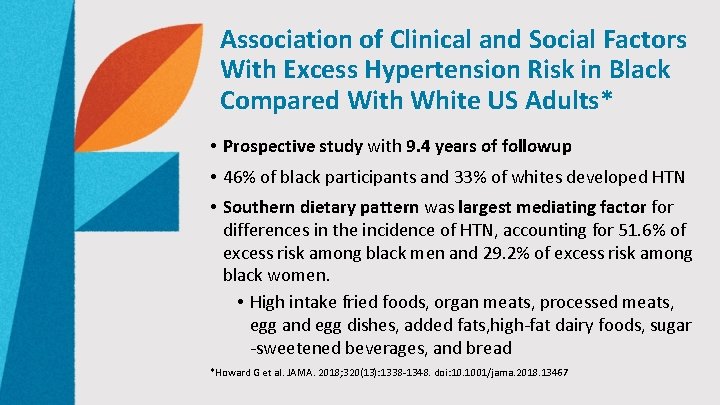
Association of Clinical and Social Factors With Excess Hypertension Risk in Black Compared With White US Adults* • Prospective study with 9. 4 years of followup • 46% of black participants and 33% of whites developed HTN • Southern dietary pattern was largest mediating factor for differences in the incidence of HTN, accounting for 51. 6% of excess risk among black men and 29. 2% of excess risk among black women. • High intake fried foods, organ meats, processed meats, egg and egg dishes, added fats, high-fat dairy foods, sugar -sweetened beverages, and bread *Howard G et al. JAMA. 2018; 320(13): 1338 -1348. doi: 10. 1001/jama. 2018. 13467
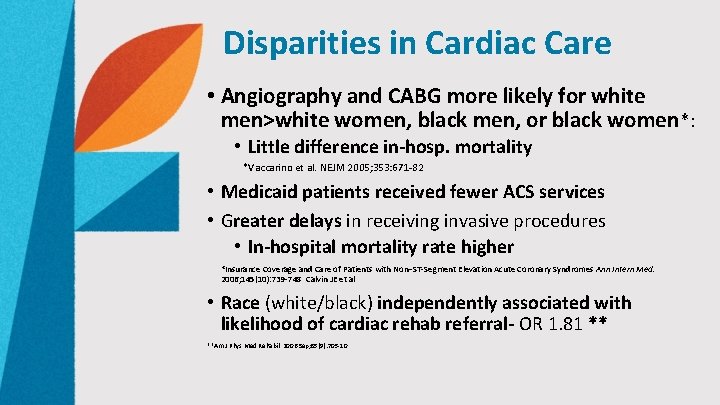
Disparities in Cardiac Care • Angiography and CABG more likely for white men>white women, black men, or black women*: • Little difference in-hosp. mortality *Vaccarino et al. NEJM 2005; 353: 671 -82 • Medicaid patients received fewer ACS services • Greater delays in receiving invasive procedures • In-hospital mortality rate higher *Insurance Coverage and Care of Patients with Non–ST-Segment Elevation Acute Coronary Syndromes Ann Intern Med. 2006; 145(10): 739 -748 Calvin JE et al • Race (white/black) independently associated with likelihood of cardiac rehab referral- OR 1. 81 ** **Am J Phys Med Rehabil. 2006 Sep; 85(9): 705 -10
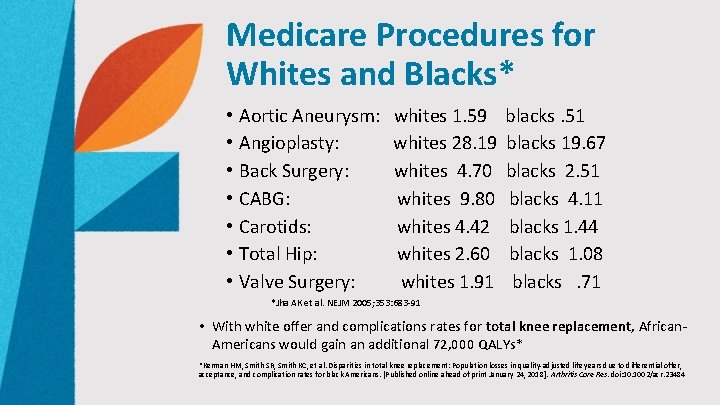
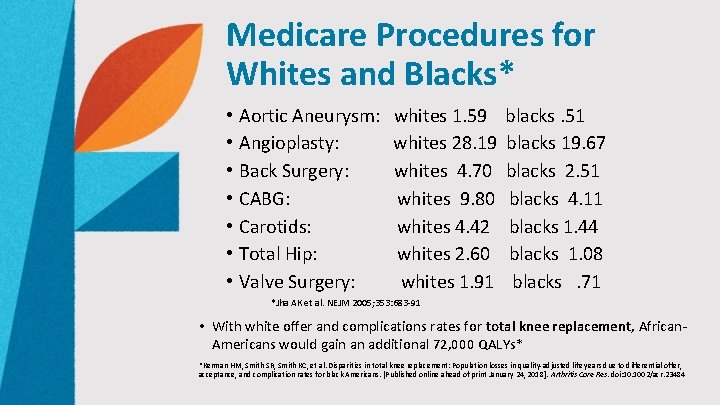
Medicare Procedures for Whites and Blacks* • • Aortic Aneurysm: whites 1. 59 blacks. 51 Angioplasty: whites 28. 19 blacks 19. 67 Back Surgery: whites 4. 70 blacks 2. 51 CABG: whites 9. 80 blacks 4. 11 Carotids: whites 4. 42 blacks 1. 44 Total Hip: whites 2. 60 blacks 1. 08 Valve Surgery: whites 1. 91 blacks . 71 *Jha AK et al. NEJM 2005; 353: 683 -91 • With white offer and complications rates for total knee replacement, African. Americans would gain an additional 72, 000 QALYs* *Kerman HM, Smith SR, Smith KC, et al. Disparities in total knee replacement: Population losses in quality-adjusted life years due to differential offer, acceptance, and complication rates for black Americans. [Published online ahead of print January 24, 2018]. Arthritis Care Res. doi: 10. 1002/acr. 23484
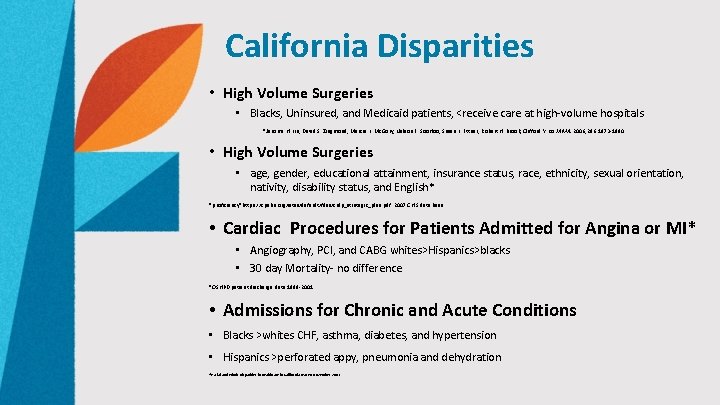
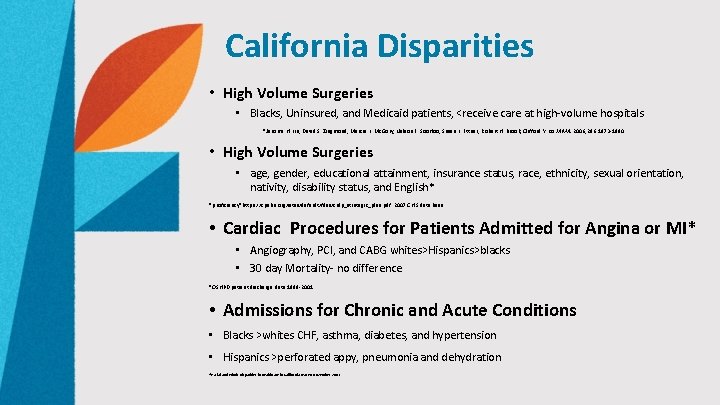
California Disparities • High Volume Surgeries • Blacks, Uninsured, and Medicaid patients, <receive care at high-volume hospitals *Jerome H. Liu; David S. Zingmond; Marcia L. Mc. Gory; Nelson F. Soo. Hoo; Susan L. Ettner; Robert H. Brook; Clifford Y. Ko JAMA. 2006; 296: 1973 -1980 • High Volume Surgeries • age, gender, educational attainment, insurance status, race, ethnicity, sexual orientation, nativity, disability status, and English* *proficiency*https: //cpehn. org/sites/default/files/crdp_strategic_plan. pdf 2007 CHIS data base • Cardiac Procedures for Patients Admitted for Angina or MI* • Angiography, PCI, and CABG whites>Hispanics>blacks • 30 day Mortality- no difference *OSHPD patient discharge data 1999 -2001 • Admissions for Chronic and Acute Conditions • Blacks >whites CHF, asthma, diabetes, and hypertension • Hispanics >perforated appy, pneumonia and dehydration *Racial and Ethnic Disparities in Healthcare in California. OSHPD November, 2003
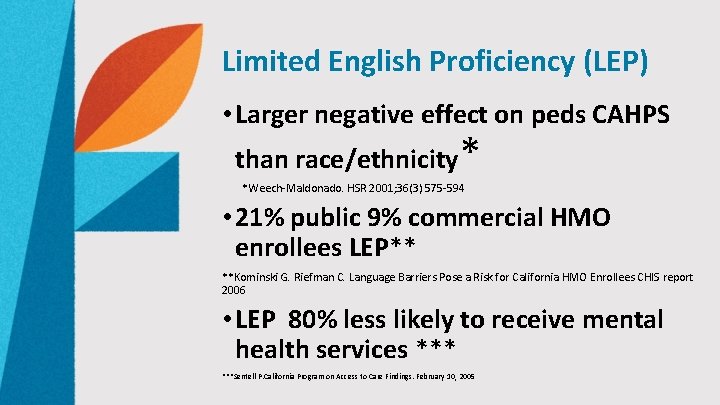
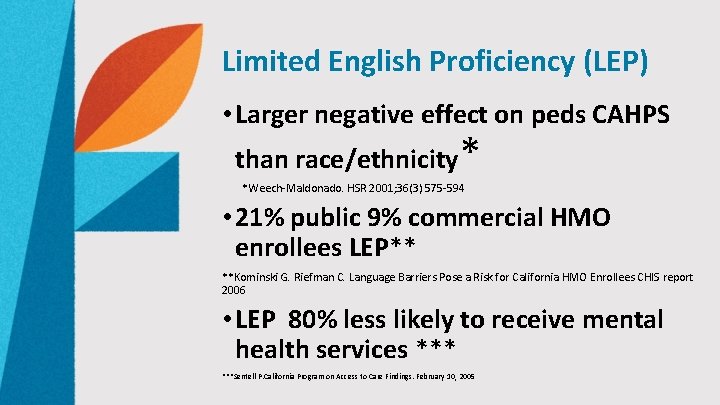
Limited English Proficiency (LEP) • Larger negative effect on peds CAHPS than race/ethnicity * *Weech-Maldonado. HSR 2001; 36(3) 575 -594 • 21% public 9% commercial HMO enrollees LEP** **Kominski G. Riefman C. Language Barriers Pose a Risk for California HMO Enrollees CHIS report 2006 • LEP 80% less likely to receive mental health services ***Sentell P. California Program on Access to Care Findings. February 10, 2005

HHS National Culturally and Linguistically Appropriate Services (CLAS)* • Intended to advance health equity, improve quality, and help eliminate health care disparities • responsive to diverse cultural health beliefs and practices, preferred languages, health literacy, and other communication needs * https: //www. thinkculturalhealth. hhs. gov/
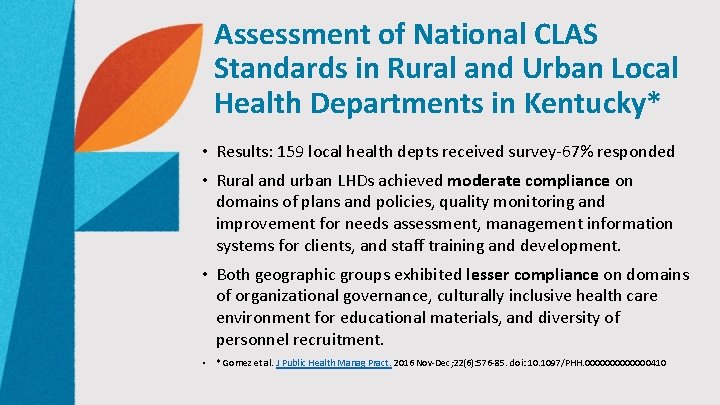
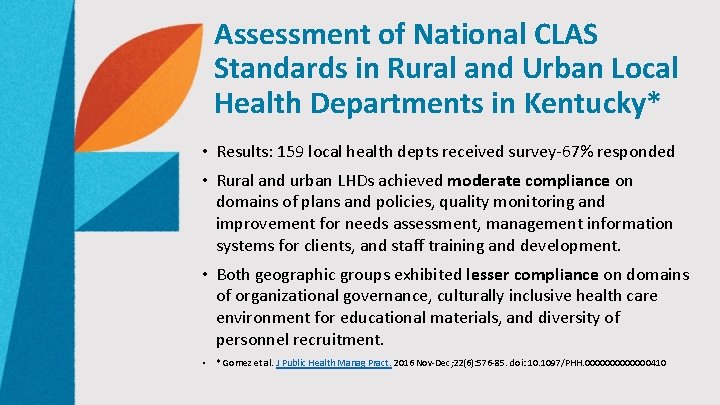
Assessment of National CLAS Standards in Rural and Urban Local Health Departments in Kentucky* • Results: 159 local health depts received survey-67% responded • Rural and urban LHDs achieved moderate compliance on domains of plans and policies, quality monitoring and improvement for needs assessment, management information systems for clients, and staff training and development. • Both geographic groups exhibited lesser compliance on domains of organizational governance, culturally inclusive health care environment for educational materials, and diversity of personnel recruitment. • * Gomez et al. J Public Health Manag Pract. 2016 Nov-Dec; 22(6): 576 -85. doi: 10. 1097/PHH. 0000000410
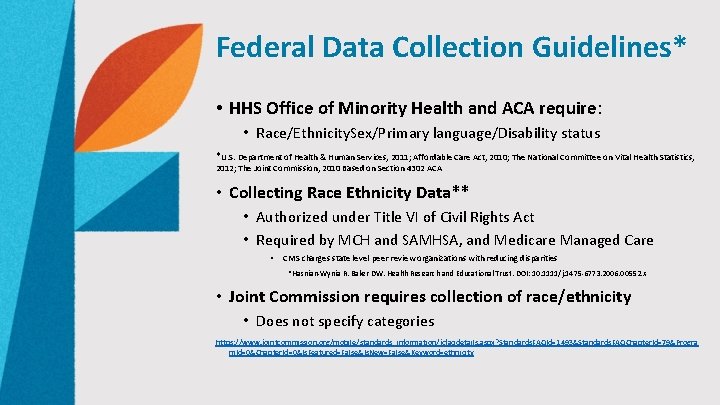
Federal Data Collection Guidelines* • HHS Office of Minority Health and ACA require: • Race/Ethnicity. Sex/Primary language/Disability status *U. S. Department of Health & Human Services, 2011; Affordable Care Act, 2010; The National Committee on Vital Health Statistics, 2012; The Joint Commission, 2010 Based on Section 4302 ACA • Collecting Race Ethnicity Data** • Authorized under Title VI of Civil Rights Act • Required by MCH and SAMHSA, and Medicare Managed Care • CMS charges state level peer review organizations with reducing disparities *Hasnian-Wynia R. Baker DW. Health Research and Educational Trust. DOI: 10. 1111/j. 1475 -6773. 2006. 00552. x • Joint Commission requires collection of race/ethnicity • Does not specify categories https: //www. jointcommission. org/mobile/standards_information/jcfaqdetails. aspx? Standards. FAQId=1493&Standards. FAQChapter. Id=79&Progra m. Id=0&Chapter. Id=0&Is. Featured=False&Is. New=False&Keyword=ethnicity
AHIP Collection and Use of Race and Ethnicity Data for Quality Improvement* • Barriers • No good method for data collection • Costs, IT capability • Not commonly collected or enrollee resistance • Recommendation: Develop comprehensive standards on collecting race, ethnicity and primary language data from enrollees and providers *Gazmararian J. AHIP November 2006
State CLAS Standards* • California-Health Plans must create demographic profiles, survey linguistic needs, and report threshold languages *https: //www. dmhc. ca. gov/Portals/0/Licensing. And. Reporting/Submitting. Health. Plan. Filings/ccr 130067 22. pdf • Massachusetts-Acute care hospitals required to collect and report race and ethnicity *https: //www. dmhc. ca. gov/Portals/0/Licensing. And. Reporting/Submitting. Health. Plan. Filings /ccr 13006722. pdf


Why Public Reporting? * • Promote accountability • Promote competition • Aid consumers in decision making • Promulgate standards *Performance Measurement: Accelerating Improvement. Committee on Redesigning Health Insurance Performance Measures, Payment, and Performance Improvement Programs, Board on Health Care Services. Institute of Medicine. The National Academies Press. Washington, DC. 2006
Unintended Consequences of Public Reporting* • Physicians avoiding sick patients • Discounting patient preferences and clinical judgment • Encouraging physicians to achieve "target rates" even if may be inappropriate *The Unintended Consequences of Publicly Reporting Quality Information Rachel M. Werner, MD, Ph. D; David A. Asch, MD, MBA JAMA. 2005; 293: 1239 -1244 • PCI for AMI lower in states with public reporting • Future Directions • Disease-based reporting • Non-public reporting *JAMA Cardiol. 2018; 3(7): 635 -640. doi: 10. 1001/jamacardio. 2018. 0947. Published online May 9, 2018
Highlight Meaningful Disparities • Significant disparities, driven by social determinants, not reflected in star ratings § Identify disparities by empathetically collecting race/ethnicity and socio-economic data § Publicly report meaningful health care metrics • Adjust for known variables • Acknowledge the unknown
Health Disparity Interventions in Community Health Centers* • Based on HRSA Health Disparities Collaborative • Premise was to reduce disparities by improving all care in settings caring for large numbers of underserved patients • Intervention included 2 day training in QI techniques, disease registry software, and instruction in the Chronic Care Model • Found improvements in process measures for diabetes and asthma, not hypertension • No improvements in outcome measures found *Landon BE et al. N Engl J Med 2007: 356: 921 -34
Standardized Screening for Health. Related Social Needs in Clinical Settings* • 10 -item “Accountable Health Communities Screening Tool” covers 5 domains • Each can be addressed through community services • • • Housing instability Food insecurity Transportation needs Utility assistance needs Interpersonal safety *Billioux, A. , K. Verlander, S. Anthony, and D. Alley. 2017. Standardized screening for health‐related social needs in clinical settings: The accountable health communities screening tool. Discussion Paper, National Academy of Medicine, Washington, DC. https: //nam. edu/wp-content/uploads/2017/05/ Standardized-Screening-for-Health. Related-Social-Needs-in-Clinical-Settings. pdf. • Behavioral health • Substance use
Standardized Screening for Health. Related Social Needs in Clinical Settings • housing instability • What is your housing situation today? • Do you have problems with bugs, mold, lead paint, inadequate heat, no smoke detectors or water leaks • food insecurity • Within the past 12 months, you worried that your food would run out before you got money to buy more. • Within the past 12 months, the food you bought just didn’t last and you didn’t have money to get more.
Standardized Screening for Health. Related Social Needs in Clinical Settings • transportation needs • In the past 12 months, has lack of transportation kept you from medical appointments, meetings, work or from getting things needed for daily living? • utility assistance needs • In the past 12 months has the electric, gas, oil, or water company threatened to shut off services in your home? • interpersonal safety • How often does anyone, including family, physically hurt you?
Additional Social Determinants Behavioral Health • PHQ-2 • Over the past 2 weeks, how often have you been bothered by any of the following problems? • Little interest or pleasure in doing things • Feeling down, depressed, or hopeless
Additional Social Determinants- Substance Use Drug Abuse Screening Test, DAST-10* *Drug Abuse Screening Test (DAST‐ 10). (Copyright 1982 by the Addiction Research Foundation. ) • Referenced in SAMHSA list of resources of substance use screens, and is noted to be a screen that is short, nonproprietary, and effective* • Detects nearly 80% of young and middle-aged patients • In the last year, have you ever drunk or used drugs more than you meant to? • Have you felt you wanted or needed to cut down on your drinking or drug use in the last year? *Brown RL et al. JABFP March–April 2001 Vol. 14 No. 2
Tipping Point: Value Based Care • Health care organizations responsible for cost and quality • Capitation vs fee-for-service • Proactive vs reactive • Transitions of care • Team-based care • Health plan vs accountable care organizations
Tipping Point: Improving Digital Access • Telehealth • E-consults • Phone • E-mail • Texts
Tipping Point: Population Health • A holistic approach to care encompassing social determinants: • Public Health • Chronic Care Management • Case Management • Coordination with community organizations • Team-based care

Improving Star Ratings by Addressing Social Determinants: A Population Health Approach • Recognize health disparities- strive for equity • Provide access to care • Screen for social determinants • Partner with community agencies • Improve health services for rising risk/high risk patients • Chronic care management • Case management- virtual care • Team-based approach to quality improvement
46
 Chapter 3 health wellness and health disparities
Chapter 3 health wellness and health disparities Maternal and infant health disparities
Maternal and infant health disparities 30-30-30 model of health disparities
30-30-30 model of health disparities Health disparity definition
Health disparity definition Health disparities meaning
Health disparities meaning Non malficence
Non malficence What are the 6 main social determinants of health?
What are the 6 main social determinants of health? Define personality and its determinants
Define personality and its determinants Health and social care component 3
Health and social care component 3 Physical environment determinants of health
Physical environment determinants of health Social determinants of personality
Social determinants of personality Social determinants of aggression
Social determinants of aggression Social gospel vs social darwinism
Social gospel vs social darwinism Topic sentence outline example
Topic sentence outline example Social thinking and social influence
Social thinking and social influence Social thinking social influence social relations
Social thinking social influence social relations Occupational health and safety course outline
Occupational health and safety course outline Occupational health and safety course outline
Occupational health and safety course outline 3 by 3 matrix
3 by 3 matrix Applications of matrices and determinants
Applications of matrices and determinants Matrices formula
Matrices formula Determinants of consumption
Determinants of consumption What is appraisal in health and social care
What is appraisal in health and social care Verna and sam case study
Verna and sam case study What are the determinants of market structure
What are the determinants of market structure Chapter 6 section 1 combining supply and demand answers
Chapter 6 section 1 combining supply and demand answers Non price determinants of supply
Non price determinants of supply Non price determinants of supply
Non price determinants of supply Determinants of demand
Determinants of demand Examples of substitute goods
Examples of substitute goods What are the determinants of market structure
What are the determinants of market structure Les déterminants synthèse
Les déterminants synthèse Determinants of pes
Determinants of pes Organizational behaviour meaning
Organizational behaviour meaning Roi indicators for calculating international assignments
Roi indicators for calculating international assignments What are the 5 determinants of price elasticity of demand
What are the 5 determinants of price elasticity of demand Demand analysis example
Demand analysis example What are the 5 determinants of price elasticity of demand
What are the 5 determinants of price elasticity of demand Cytoplasmic determinants
Cytoplasmic determinants Determinants of gait cycle
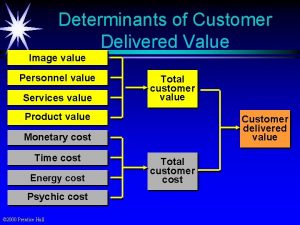
Determinants of gait cycle Customer delivered value definition
Customer delivered value definition What are the determinants of market structure
What are the determinants of market structure Functional cost
Functional cost Experiental readiness
Experiental readiness Determinants of attribution
Determinants of attribution Cofactor matrix
Cofactor matrix Chapter 16 determinants of the money supply
Chapter 16 determinants of the money supply