1 Maryam Tohidi Associate professor of anatomical clinical

![Ø Presence of vascular invasion [OPTIONAL: perform IHC for endothelial markers if needed] Ø Ø Presence of vascular invasion [OPTIONAL: perform IHC for endothelial markers if needed] Ø](https://slidetodoc.com/presentation_image_h2/738a36ff6ee5b40191209ed131904c7e/image-37.jpg)
- Slides: 40

1
Maryam Tohidi Associate professor of anatomical & clinical pathology Research Institute for Endocrine Sciences Shahid Beheshti University of Medical Sciences November 2018 Tehran, Iran
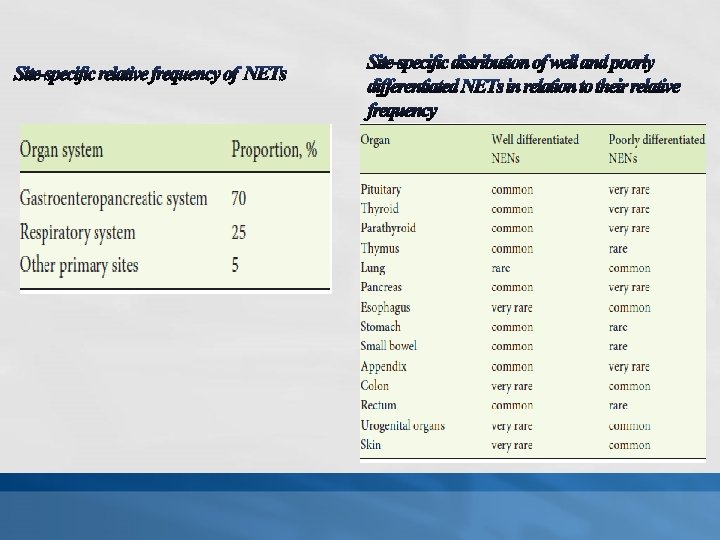
v Neuroendocrine neoplasia (NEN) is an obscure family of tumors originating from epithelial or non-epithelial neoplasm with predominant neuroendocrine differentiation. v Neuroendocrine- programmed cells are: ü Widely distributed in the body ü From different embryologic origin 3
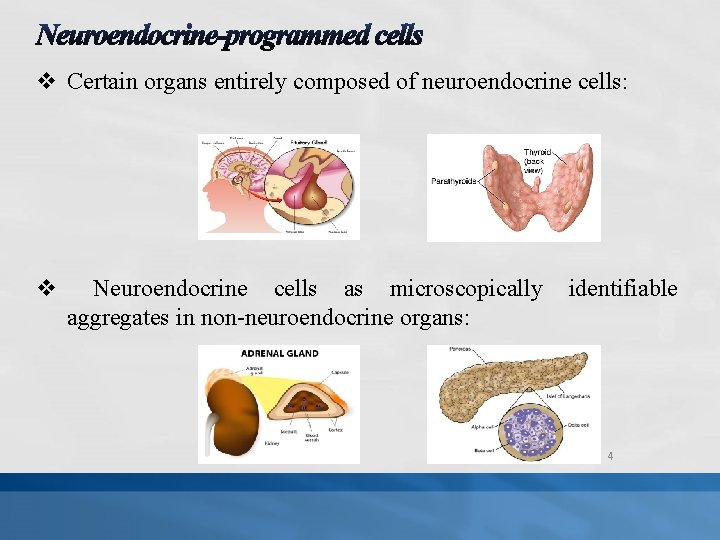
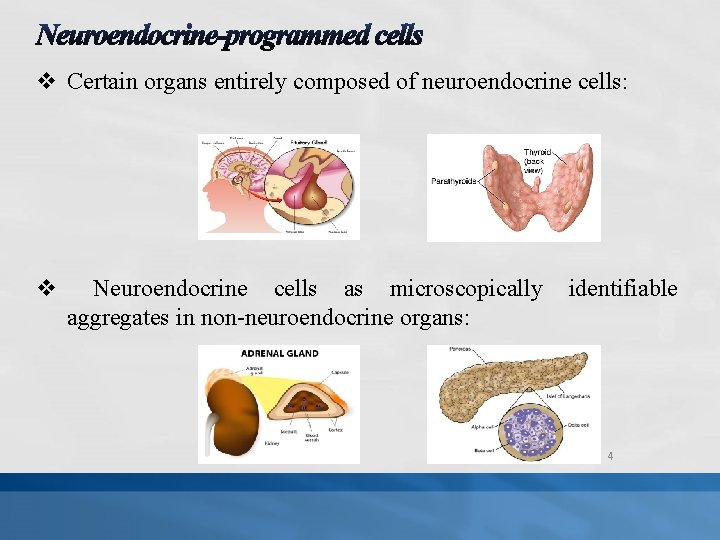
v Certain organs entirely composed of neuroendocrine cells: v Neuroendocrine cells as microscopically aggregates in non-neuroendocrine organs: identifiable 4
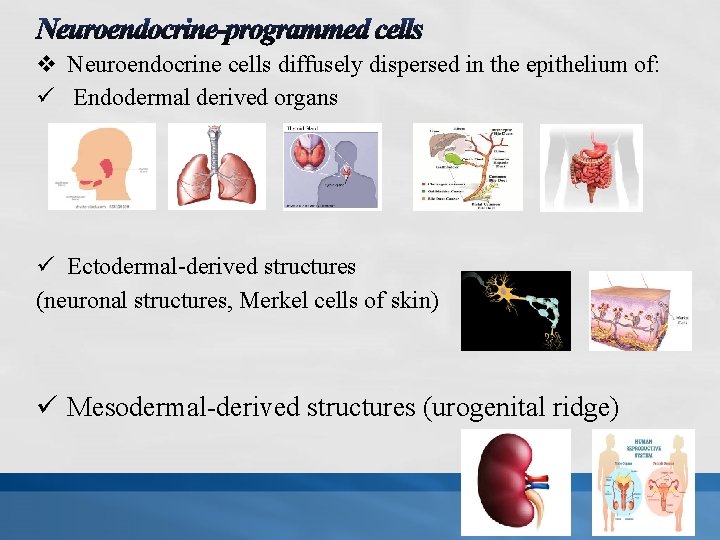
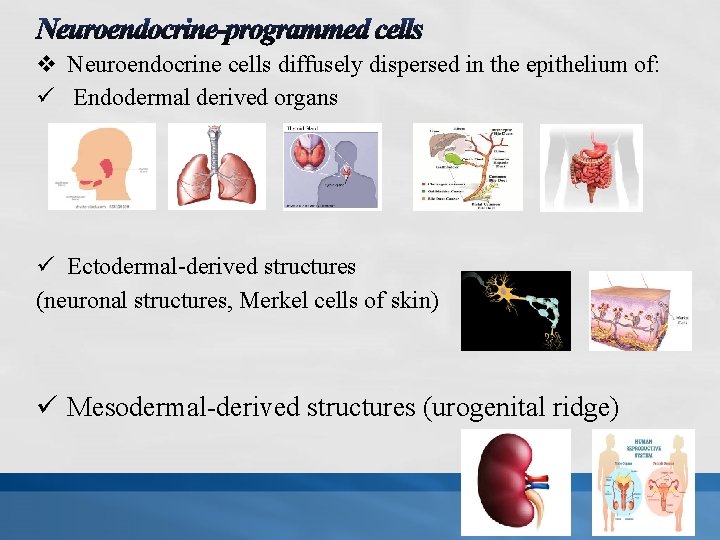
v Neuroendocrine cells diffusely dispersed in the epithelium of: ü Endodermal derived organs ü Ectodermal-derived structures (neuronal structures, Merkel cells of skin) ü Mesodermal-derived structures (urogenital ridge) 5
v NENs arise at almost any anatomical site v NENs share major morphological and protein expression signatures depending on differentiation. v NENs express a variable spectrum of proteins, shared with their normal cell of origin at specific anatomical locations q Markers of general neuroendocrine differentiation such as chromogranin A, chromogranin B, and synaptophysin q Site-specific markers such as hormones and transcription factors 6
v Neoplasia versus Tumor ü Neoplasm is a more accurate term than tumor (means only a mass). ü Neuroendocrine tumor (NET) has achieved widespread acceptance in many nomenclature & classification systems and is used more than correct but less accepted alternative, neuroendocrine neoplasm (NEN). 7
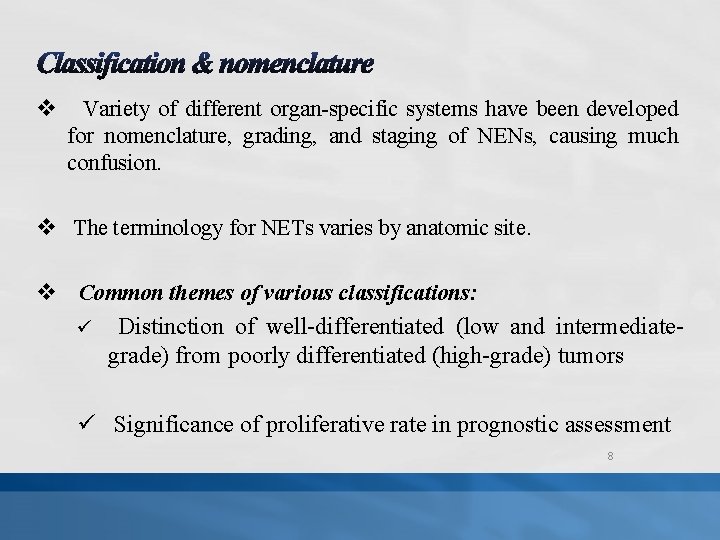
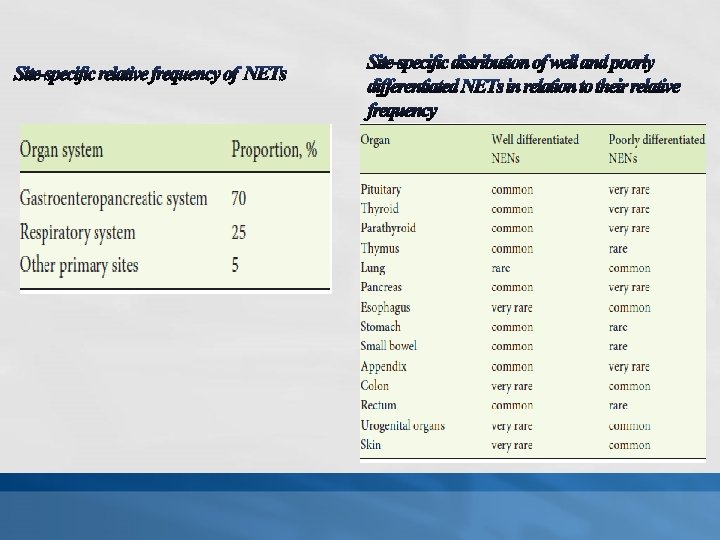
v Variety of different organ-specific systems have been developed for nomenclature, grading, and staging of NENs, causing much confusion. v The terminology for NETs varies by anatomic site. v Common themes of various classifications: ü Distinction of well-differentiated (low and intermediategrade) from poorly differentiated (high-grade) tumors ü Significance of proliferative rate in prognostic assessment 8
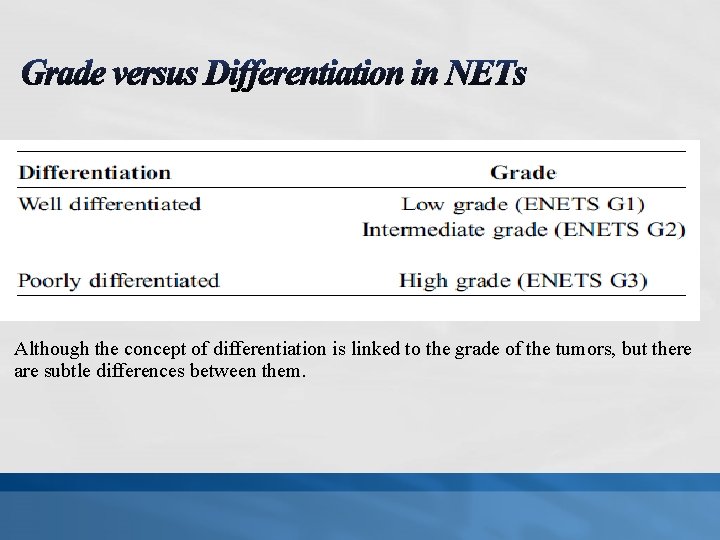
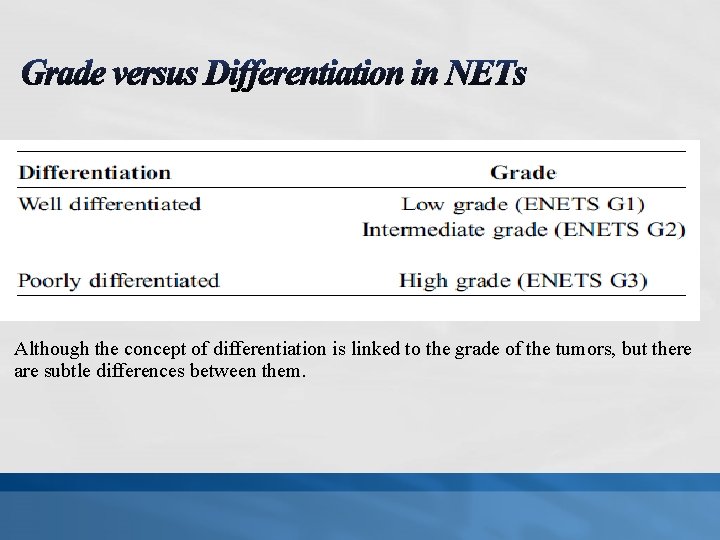
Although the concept of differentiation is linked to the grade of the tumors, but there are subtle differences between them.
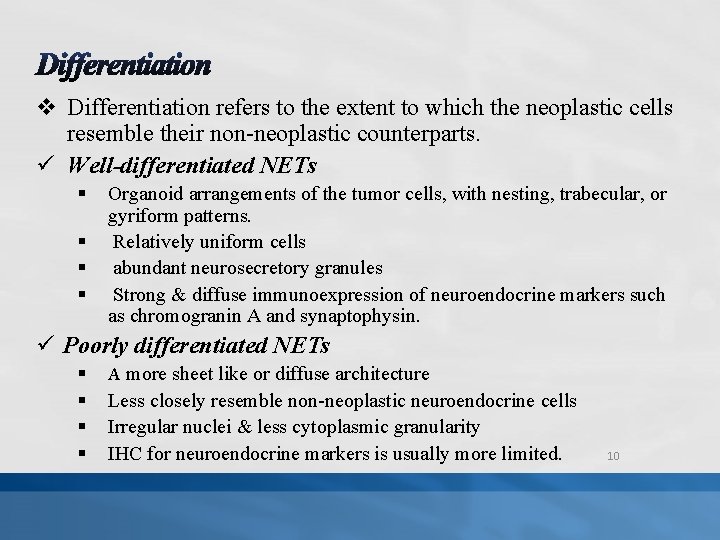
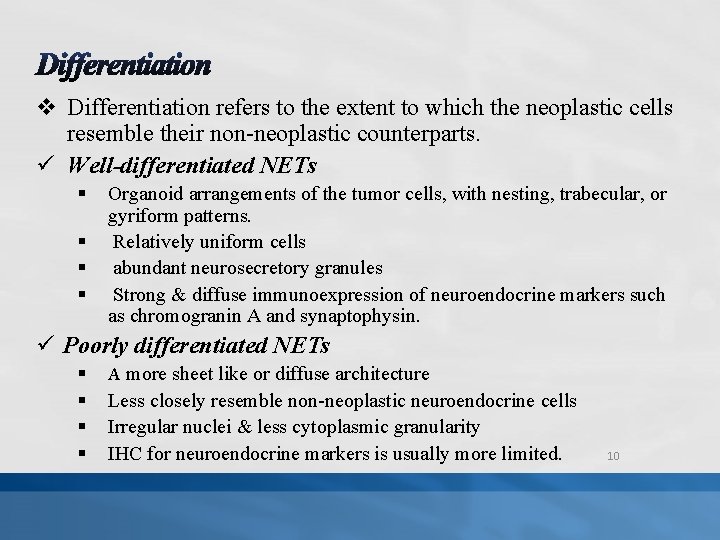
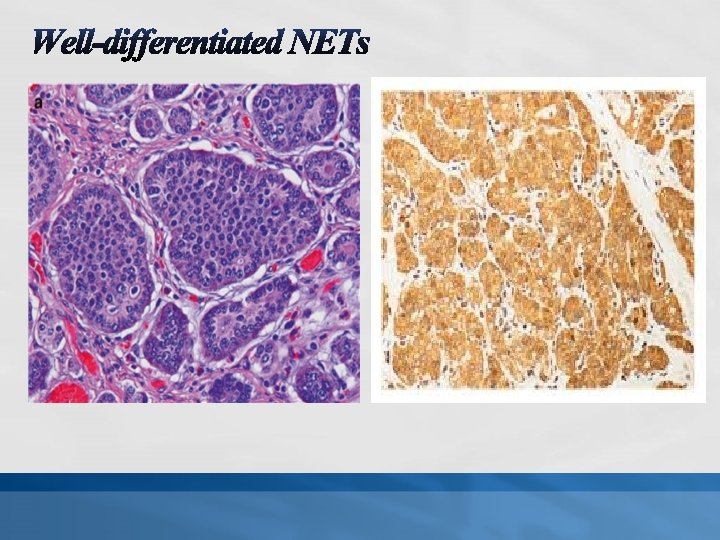
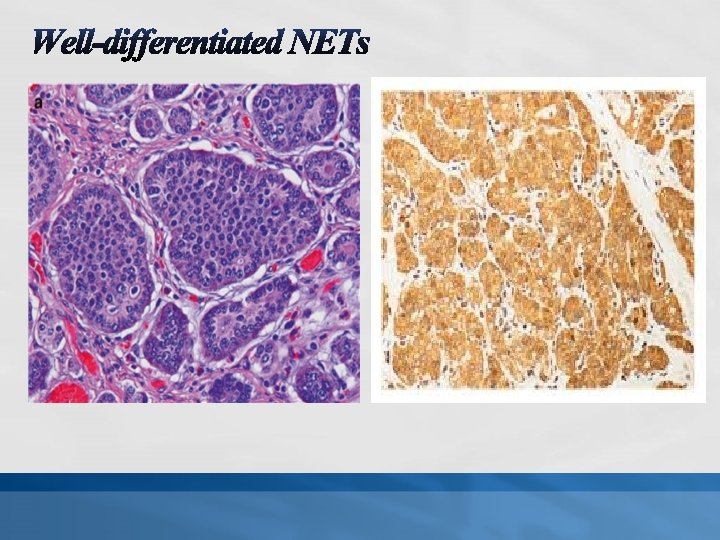
v Differentiation refers to the extent to which the neoplastic cells resemble their non-neoplastic counterparts. ü Well-differentiated NETs § § Organoid arrangements of the tumor cells, with nesting, trabecular, or gyriform patterns. Relatively uniform cells abundant neurosecretory granules Strong & diffuse immunoexpression of neuroendocrine markers such as chromogranin A and synaptophysin. ü Poorly differentiated NETs § A more sheet like or diffuse architecture § § § Less closely resemble non-neoplastic neuroendocrine cells Irregular nuclei & less cytoplasmic granularity IHC for neuroendocrine markers is usually more limited. 10
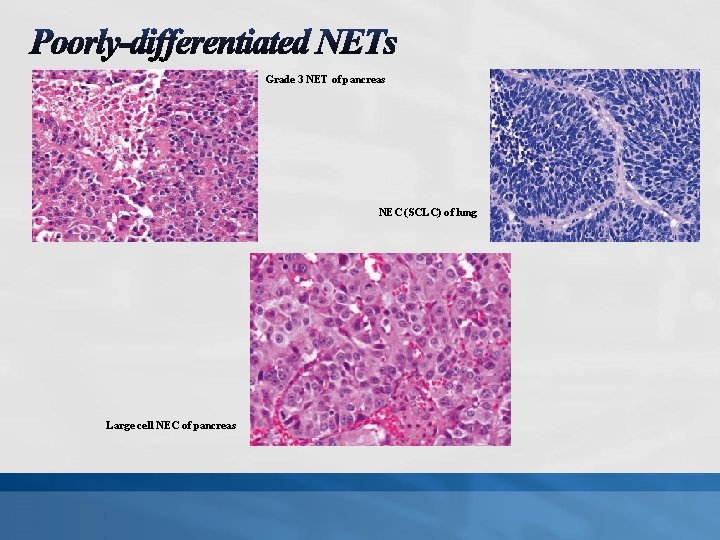
Grade 3 NET of pancreas NEC (SCLC) of lung Large cell NEC of pancreas
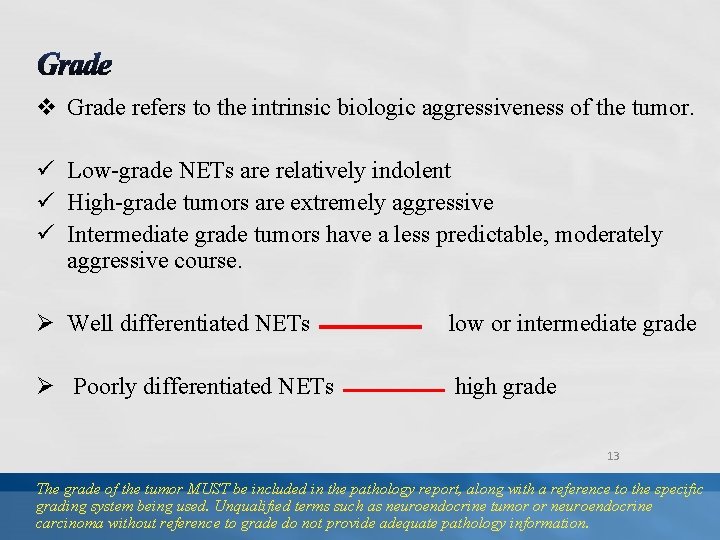
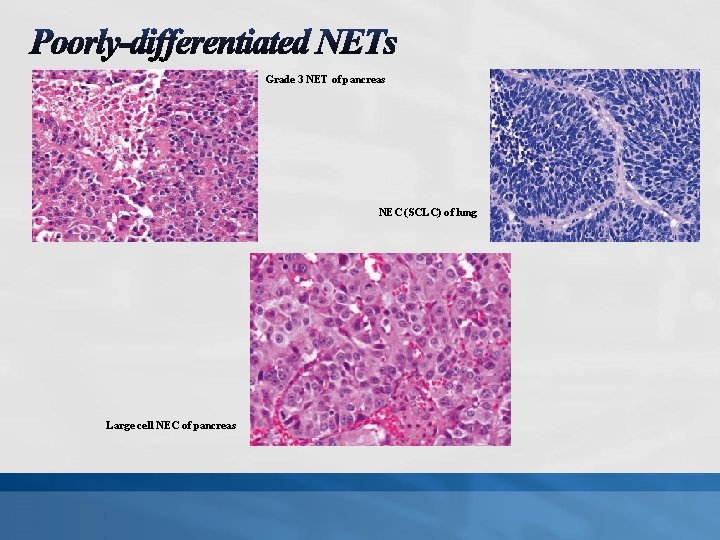
v Grade refers to the intrinsic biologic aggressiveness of the tumor. ü Low-grade NETs are relatively indolent ü High-grade tumors are extremely aggressive ü Intermediate grade tumors have a less predictable, moderately aggressive course. Ø Well differentiated NETs low or intermediate grade Ø Poorly differentiated NETs high grade 13 The grade of the tumor MUST be included in the pathology report, along with a reference to the specific grading system being used. Unqualified terms such as neuroendocrine tumor or neuroendocrine carcinoma without reference to grade do not provide adequate pathology information.
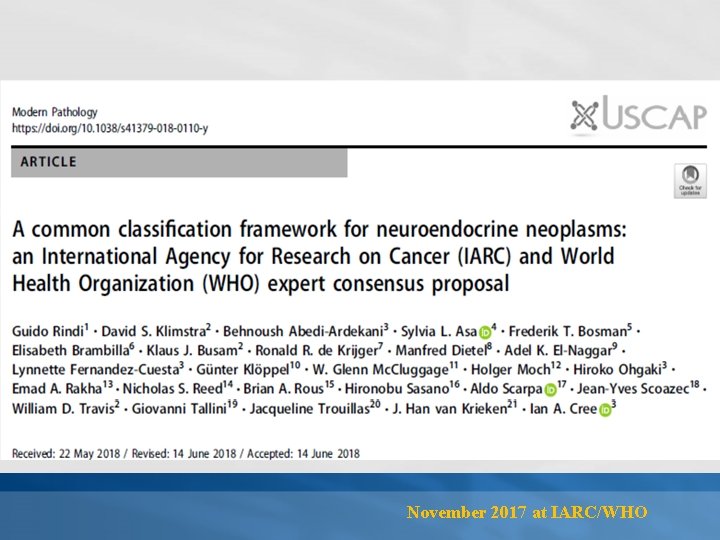
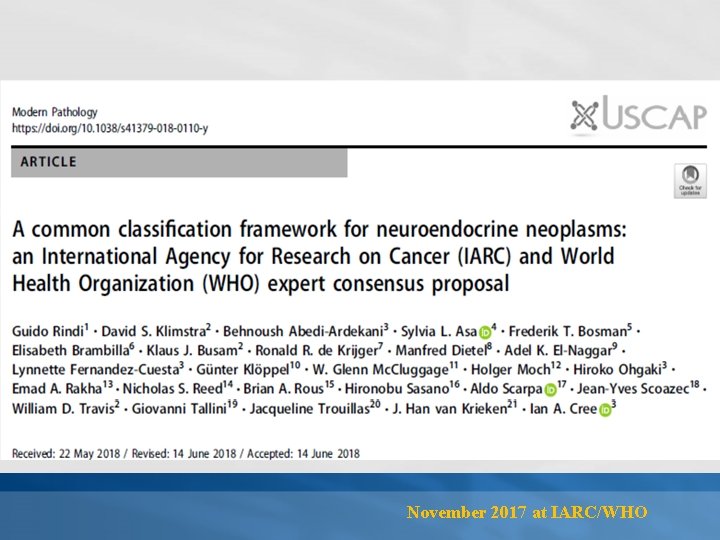
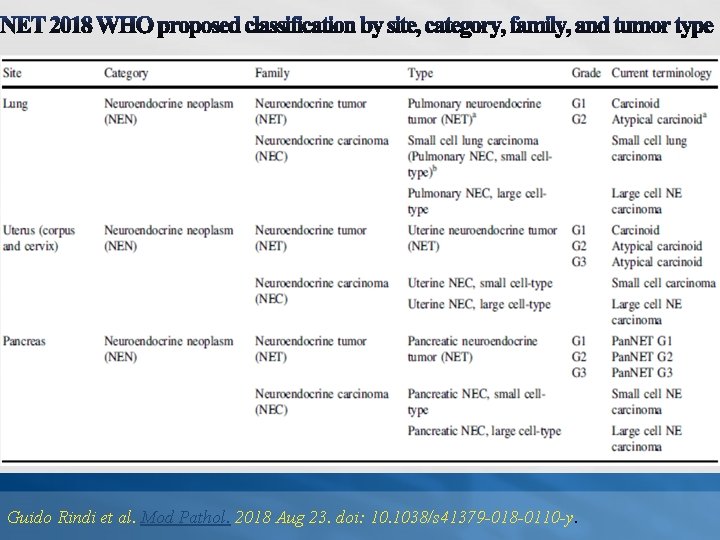
November 2017 at IARC/WHO
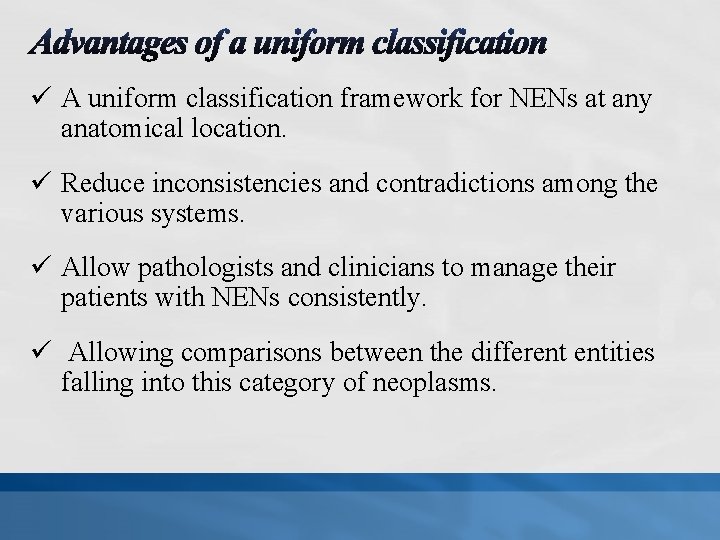
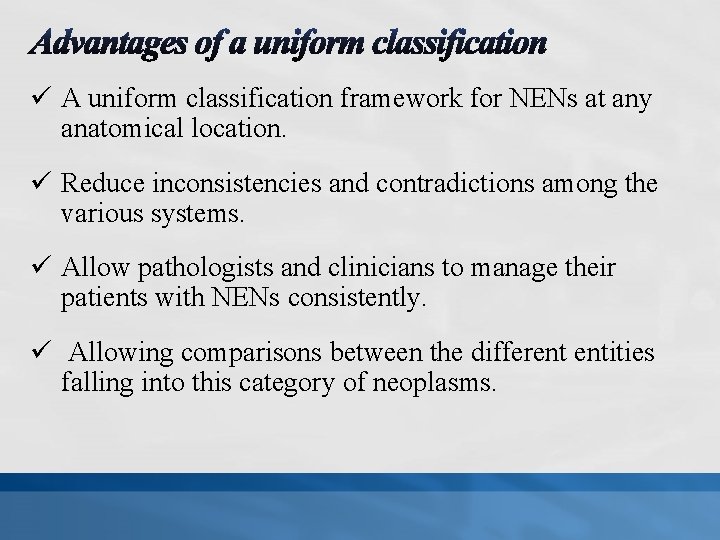
ü A uniform classification framework for NENs at any anatomical location. ü Reduce inconsistencies and contradictions among the various systems. ü Allow pathologists and clinicians to manage their patients with NENs consistently. ü Allowing comparisons between the different entities falling into this category of neoplasms.
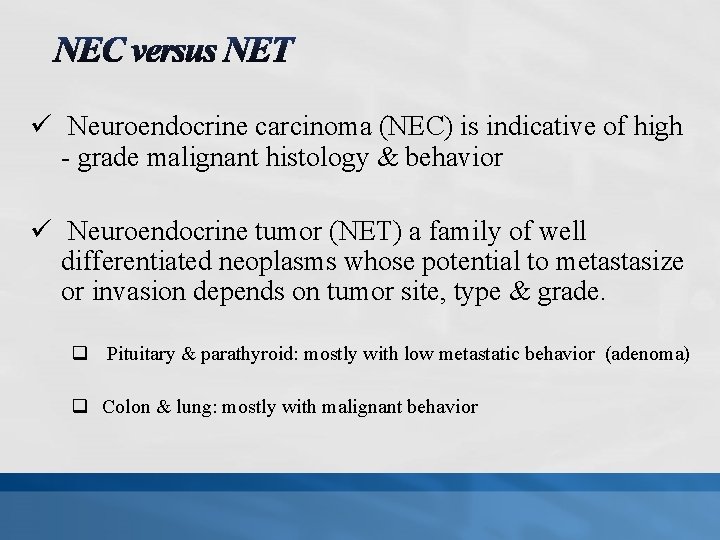
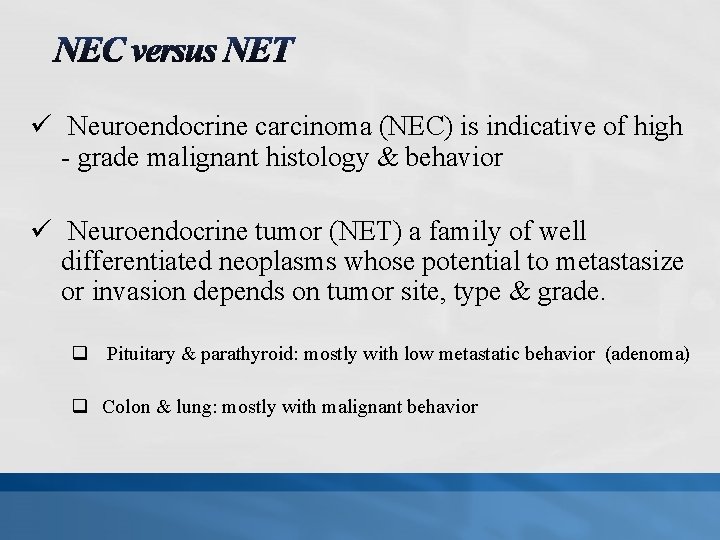
ü Neuroendocrine carcinoma (NEC) is indicative of high - grade malignant histology & behavior ü Neuroendocrine tumor (NET) a family of well differentiated neoplasms whose potential to metastasize or invasion depends on tumor site, type & grade. q Pituitary & parathyroid: mostly with low metastatic behavior (adenoma) q Colon & lung: mostly with malignant behavior
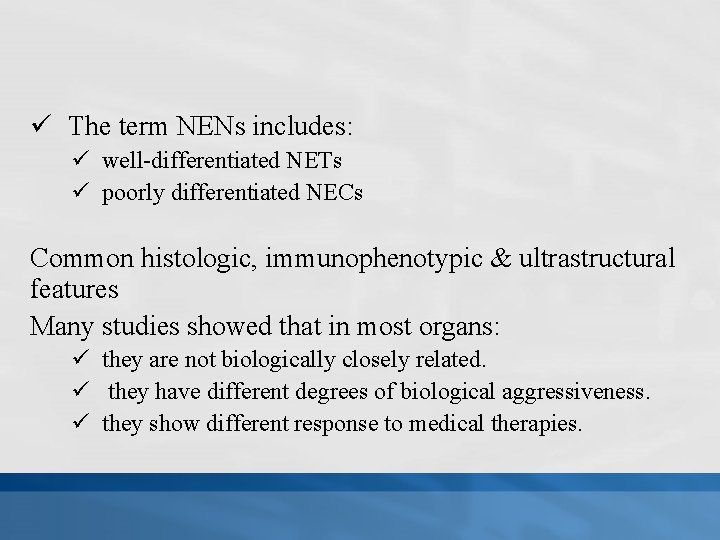
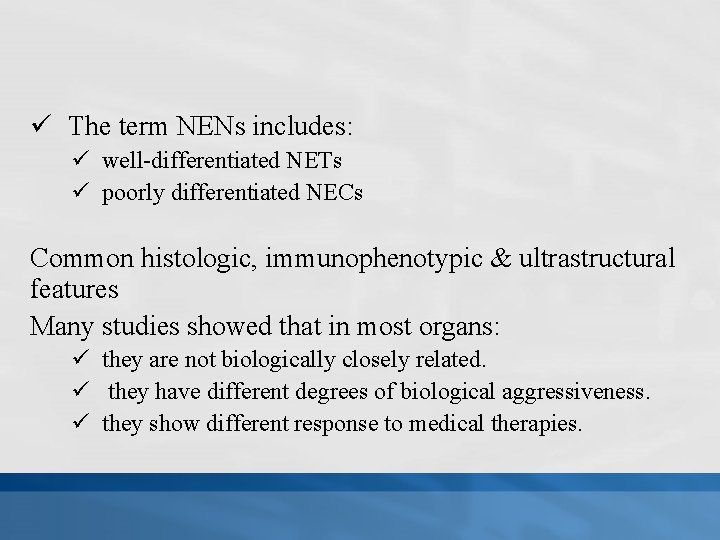
ü The term NENs includes: ü well-differentiated NETs ü poorly differentiated NECs Common histologic, immunophenotypic & ultrastructural features Many studies showed that in most organs: ü they are not biologically closely related. ü they have different degrees of biological aggressiveness. ü they show different response to medical therapies.
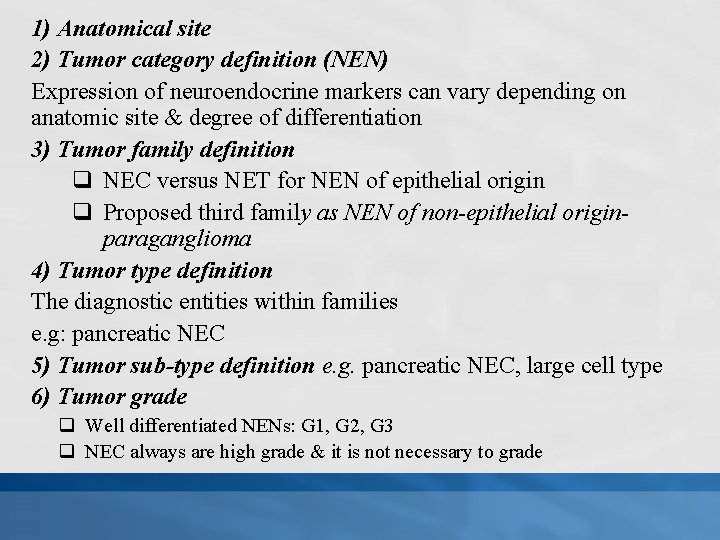
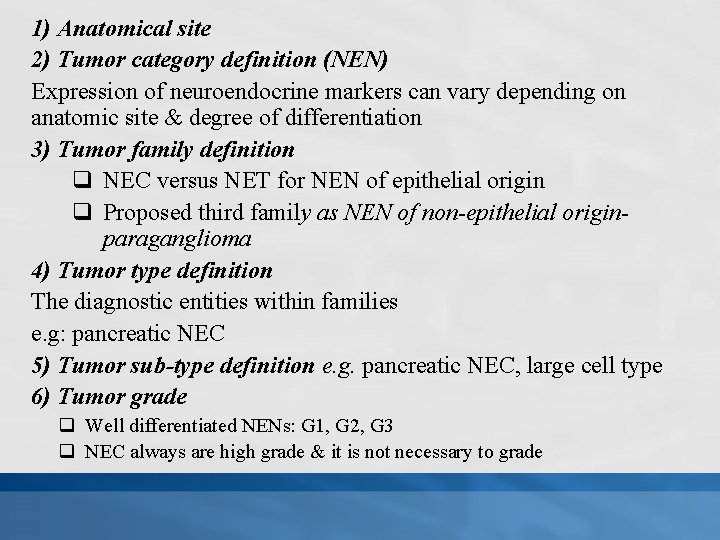
1) Anatomical site 2) Tumor category definition (NEN) Expression of neuroendocrine markers can vary depending on anatomic site & degree of differentiation 3) Tumor family definition q NEC versus NET for NEN of epithelial origin q Proposed third family as NEN of non-epithelial originparaganglioma 4) Tumor type definition The diagnostic entities within families e. g: pancreatic NEC 5) Tumor sub-type definition e. g. pancreatic NEC, large cell type 6) Tumor grade q Well differentiated NENs: G 1, G 2, G 3 q NEC always are high grade & it is not necessary to grade
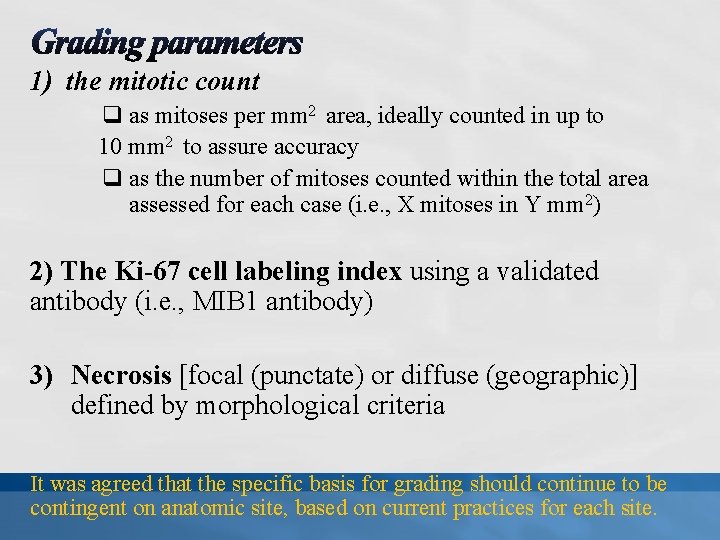
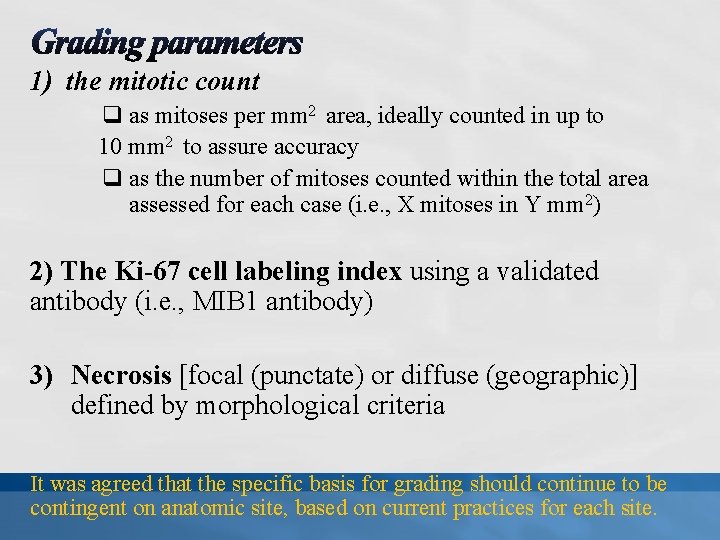
1) the mitotic count q as mitoses per mm 2 area, ideally counted in up to 10 mm 2 to assure accuracy q as the number of mitoses counted within the total area assessed for each case (i. e. , X mitoses in Y mm 2) 2) The Ki-67 cell labeling index using a validated antibody (i. e. , MIB 1 antibody) 3) Necrosis [focal (punctate) or diffuse (geographic)] defined by morphological criteria It was agreed that the specific basis for grading should continue to be contingent on anatomic site, based on current practices for each site.
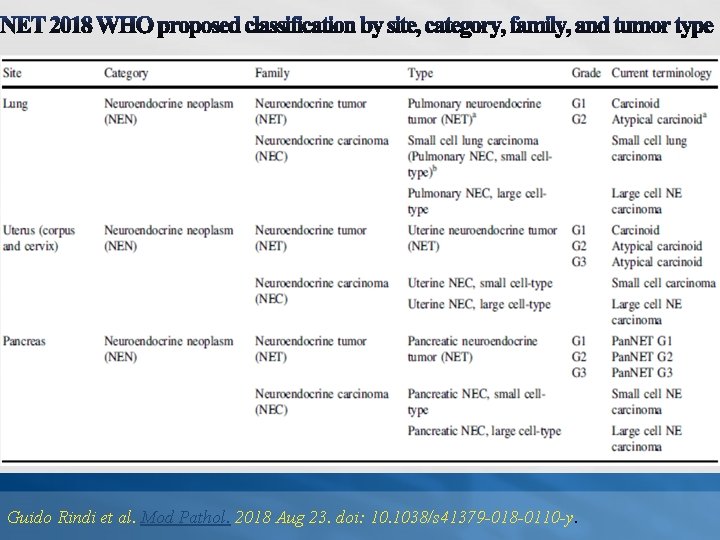
Guido Rindi et al. Mod Pathol. 2018 Aug 23. doi: 10. 1038/s 41379 -018 -0110 -y.
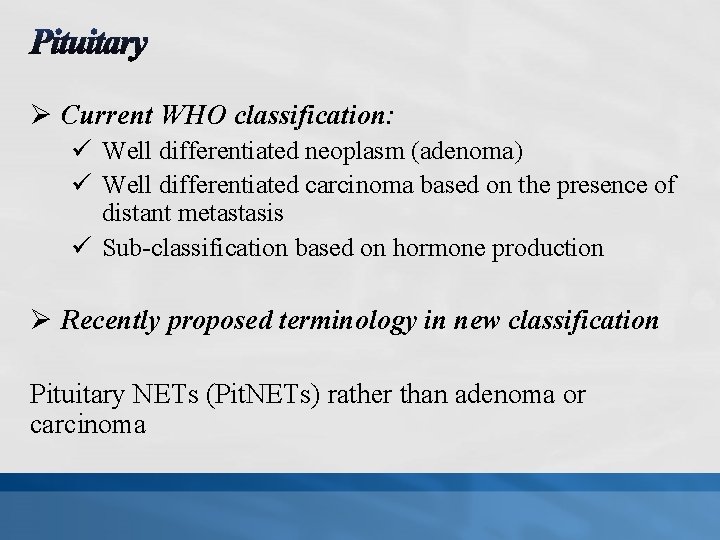
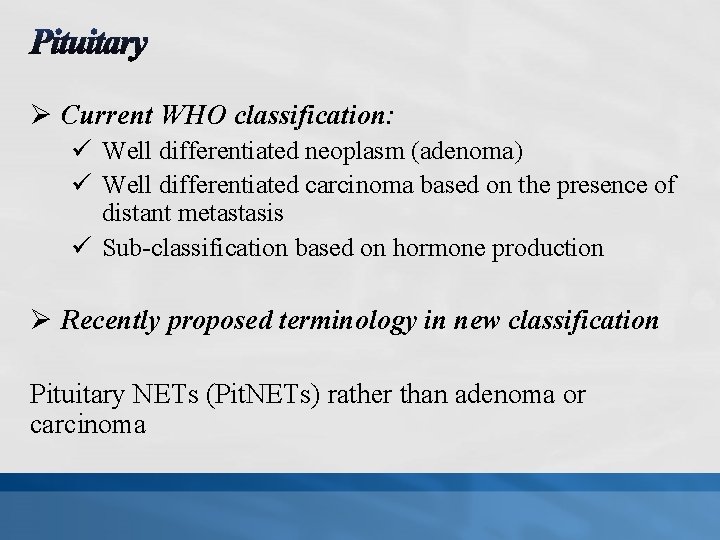
Ø Current WHO classification: ü Well differentiated neoplasm (adenoma) ü Well differentiated carcinoma based on the presence of distant metastasis ü Sub-classification based on hormone production Ø Recently proposed terminology in new classification Pituitary NETs (Pit. NETs) rather than adenoma or carcinoma
Ø Pit. NET prognosis and prediction relies more on cell type and degree of cell differentiation than on proliferative markers. Ø Mitoses are uncommon in these tumors. Ø Necrosis is rare and related to vascular thrombosis. Ø Impact of mitotic count and/or Ki-67 index on Pit. NET prognosis is controversial. Ø Grading of these tumors as G 1, G 2, and G 3 is currently not possible based on available data. Ø Poorly differentiated NECs do not occur in the pituitary.
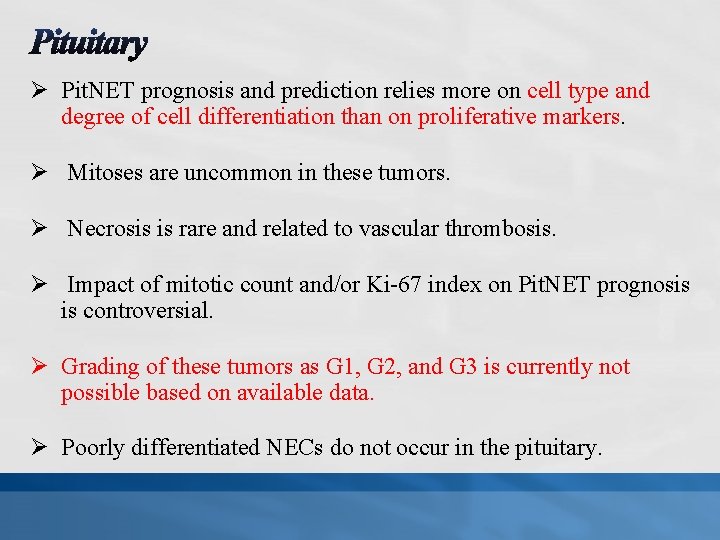
ü The vast majority of thyroid NENs are tumors of C-cells (parafollicular cells), medullary thyroid carcinoma (MTC) ü Most MTCs are well-differentiated NETs, based on the expression of calcitonin and TTF-I. ü Aggressive, poorly differentiated NECs represent less than 1% of MTCs, and include a small cell variant. § DD with small cell carcinoma metastatic to the thyroid gland. § Small cell carcinomas of many anatomic sites express TTF-1
Ø The Ki-67 labeling index in MTC is often <1% and therefore difficult to assess. Ø Limited evidence indicates that Ki-67 -based grading may be of prognostic significance. Ø Mitotic count, necrosis and/or Ki-67 labeling index may be used as markers of aggressive behavior but they are not currently part of any validated grading system. Ø There is evidence that IHC loss of calcitonin expression with retention of CEA is considered an unfavorable sign.
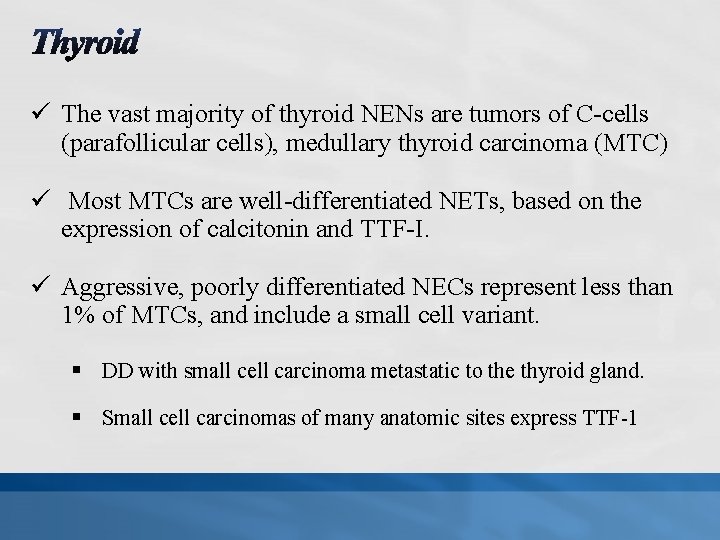
Ø Current classification includes: ü well-differentiated neoplasms classified as adenomas , atypical adenomas, or carcinomas (parathyroid NETs) Ø Poorly differentiated aggressive carcinomas (NECs) are extremely unusual. Ø The diagnosis of malignancy is based on: ü invasive growth ü vascular invasion ü full penetration of the tumor capsule with extension into the surrounding non-neoplastic tissues ü metastases
ü Potential signs of malignancy: ü ü ü Mitoses atypical mitoses Macronucleoli thick intersecting fibrous bands necrosis Ø The Ki-67 labeling index is often >5% in carcinomas compared with adenomas and hyperplastic nodules. ü There is a significant overlap in some equivocal cases. ü Although the Ki-67 index, mitotic counts, and necrosis are often used as markers of aggressive behavior, they are not part of a formally defined diagnostic grading scheme.
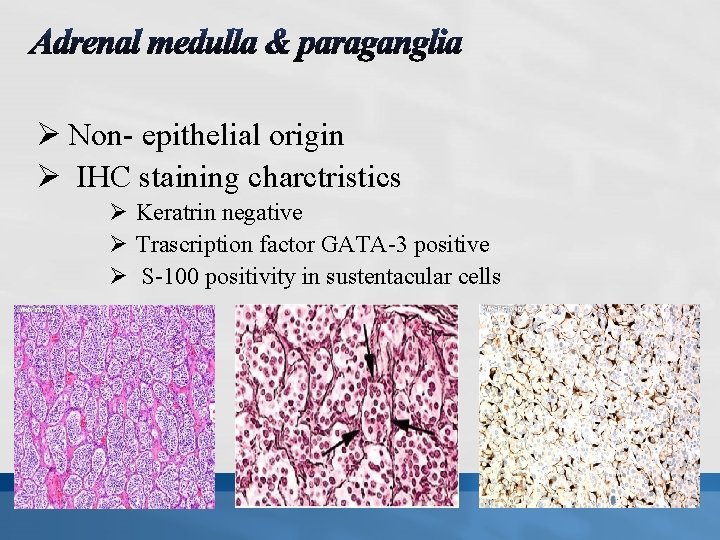
Ø NENs may be derived from the neurectoderm of the neural crest. Ø Tumors can occur throughout the body. Ø In adrenal medulla: Pheochromocytomas Ø In all other locations: Paragangliomas. Ø Based on the new proposed classification framework, all of these neoplasms are regarded to be welldifferentiated and therefore NETs Ø Poorly differentiated NECs do not occur in the adrenal or in paragangliae.
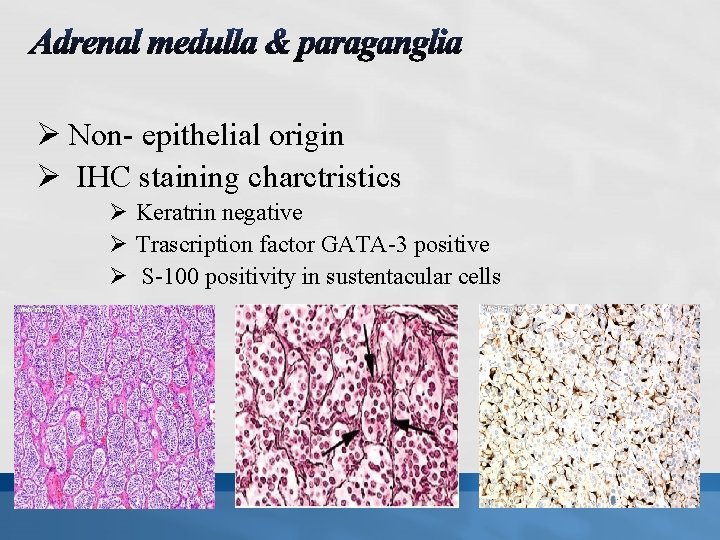
Ø Non- epithelial origin Ø IHC staining charctristics Ø Keratrin negative Ø Trascription factor GATA-3 positive Ø S-100 positivity in sustentacular cells.
Ø All tumors should be considered potentially malignant. Ø In the recent new edition of the WHO volume on endocrine tumors, it was concluded that there is no wide acceptance of any grading system. Ø The Thompson (2002), pheochromocytoma of the adrenal gland scaled score (PASS): Ø A 20 score system based on 12 histologic criteria Ø Score ≥ 4 indicate adverse clinical behavior of the tumor
Ø The Kimura (2014) 3 -tiered grading system: Ø 4 histological characteristics Ø Ki-67 labeling index (cut-offs of <1%, 1– 3%, and >3% in 500– 2000 cells in 2 of the most highly labeled areas) Ø biochemistry (catecholamine secretion pattern). Ø Well, moderately, and poorly differentiated categories would correspond to low, intermediate, and high-grade categories in the newly proposed classification framework. Ø IHC staining for Succinate Dehydrogenase Subunit B (SDHB) potentially had additional value in predicting metastasis. The value of these scoring systems remains unclear.
Klimstra DS et al. Am J Surg Pathol. 2010; 34: 300 -313.
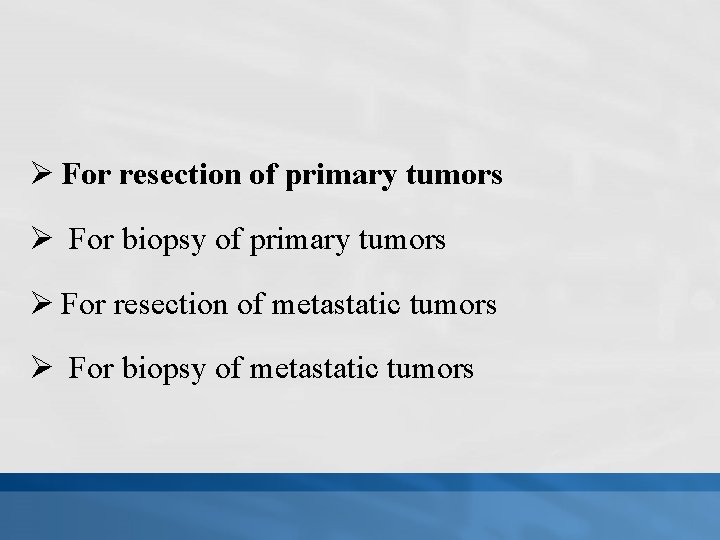
Ø For resection of primary tumors Ø For biopsy of primary tumors Ø For resection of metastatic tumors Ø For biopsy of metastatic tumors
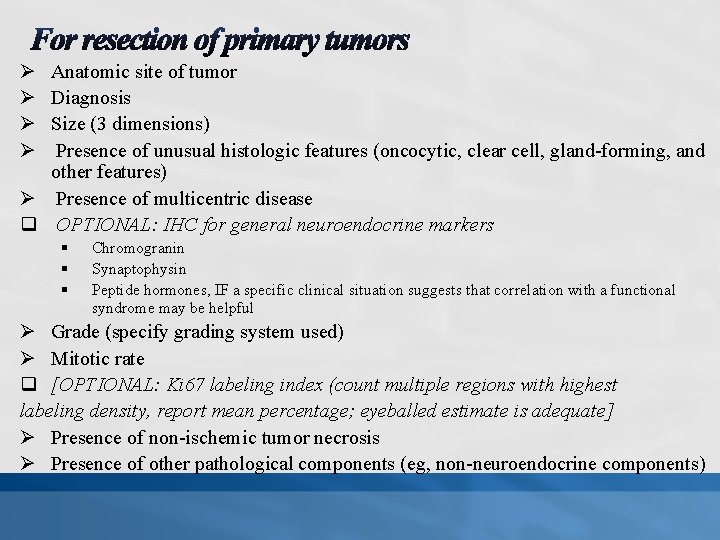
Ø Ø Anatomic site of tumor Diagnosis Size (3 dimensions) Presence of unusual histologic features (oncocytic, clear cell, gland-forming, and other features) Ø Presence of multicentric disease q OPTIONAL: IHC for general neuroendocrine markers § § § Chromogranin Synaptophysin Peptide hormones, IF a specific clinical situation suggests that correlation with a functional syndrome may be helpful Ø Grade (specify grading system used) Ø Mitotic rate q [OPTIONAL: Ki 67 labeling index (count multiple regions with highest labeling density, report mean percentage; eyeballed estimate is adequate] Ø Presence of non-ischemic tumor necrosis Ø Presence of other pathological components (eg, non-neuroendocrine components)
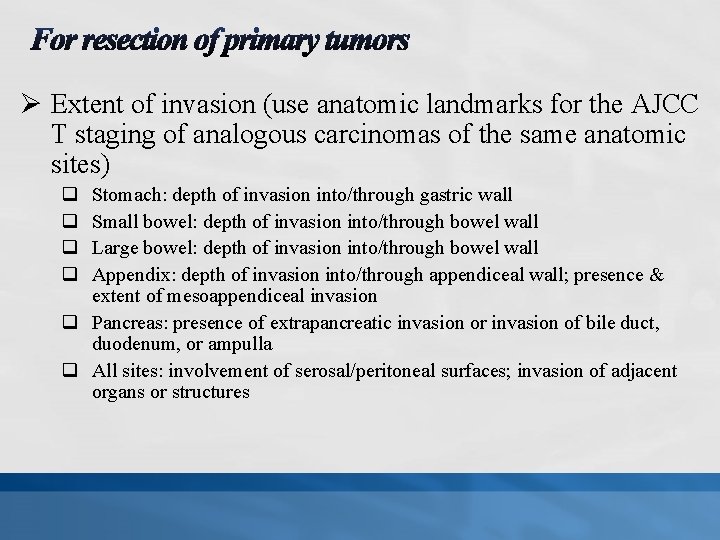
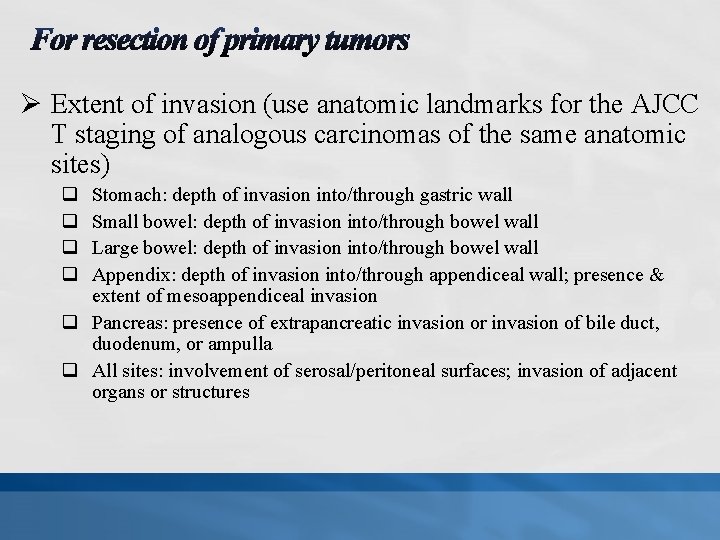
Ø Extent of invasion (use anatomic landmarks for the AJCC T staging of analogous carcinomas of the same anatomic sites) q q Stomach: depth of invasion into/through gastric wall Small bowel: depth of invasion into/through bowel wall Large bowel: depth of invasion into/through bowel wall Appendix: depth of invasion into/through appendiceal wall; presence & extent of mesoappendiceal invasion q Pancreas: presence of extrapancreatic invasion or invasion of bile duct, duodenum, or ampulla q All sites: involvement of serosal/peritoneal surfaces; invasion of adjacent organs or structures
![Ø Presence of vascular invasion OPTIONAL perform IHC for endothelial markers if needed Ø Ø Presence of vascular invasion [OPTIONAL: perform IHC for endothelial markers if needed] Ø](https://slidetodoc.com/presentation_image_h2/738a36ff6ee5b40191209ed131904c7e/image-37.jpg)
Ø Presence of vascular invasion [OPTIONAL: perform IHC for endothelial markers if needed] Ø Presence of perineural invasion Ø Lymph node metastases q Number of positive nodes q Total number of nodes examined Ø TNM staging (specify staging system used) Ø Resection margins (positive/negative/close) [OPTIONAL: measure distance from margin if within 0. 5 cm] Ø Proliferative changes or other abnormalities in non-neoplastic neuroendocrine cells
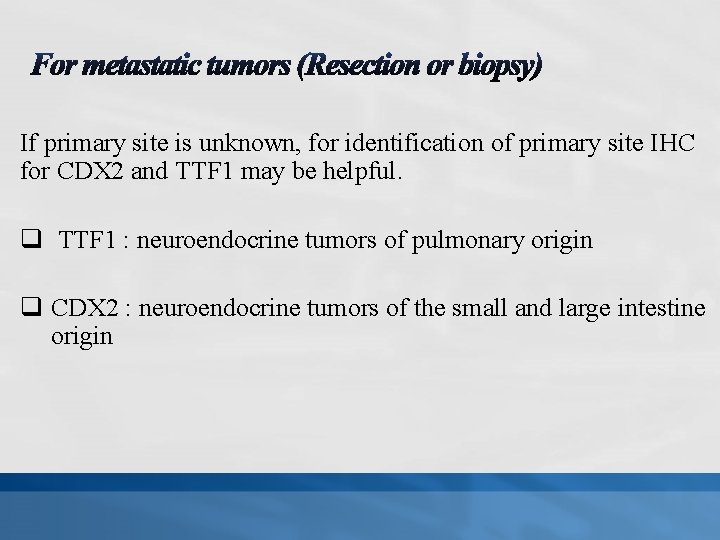
If primary site is unknown, for identification of primary site IHC for CDX 2 and TTF 1 may be helpful. q TTF 1 : neuroendocrine tumors of pulmonary origin q CDX 2 : neuroendocrine tumors of the small and large intestine origin
It was proposed by IARC/WHO that in the pathology report: Ø Parameters of grading (mitotic count, Ki-67 labeling index [%] and necrosis) be stated clearly. Ø The site-specific tumor nomenclature according to current WHO classifications be stated first. Ø The novel uniform standard classification framework be added in brackets, i. e. , (NEN-WHO 2018).
40 Thank you for attention
 Promotion from assistant to associate professor
Promotion from assistant to associate professor Anahita vondráková age
Anahita vondráková age Maryam nazir
Maryam nazir Maryam majedi
Maryam majedi Josyl barchue
Josyl barchue Räkna ut volymen på en cylinder
Räkna ut volymen på en cylinder Djevojčica iz afganistana fabula
Djevojčica iz afganistana fabula Maryam.h2009
Maryam.h2009 Maryam saeri
Maryam saeri Maryam merrikhpour
Maryam merrikhpour Dr. maryam zahedi clinic
Dr. maryam zahedi clinic Gmail
Gmail Dr maryam ebrahimi
Dr maryam ebrahimi Parvana's dad
Parvana's dad Maryam khodabakhsh
Maryam khodabakhsh Iitb
Iitb Dr maryam ghasemi
Dr maryam ghasemi Maryam kamgarpour
Maryam kamgarpour When a driver's awareness and focus drift from
When a driver's awareness and focus drift from دکتر مریم زاهدی
دکتر مریم زاهدی Lone star college nursing program deadlines
Lone star college nursing program deadlines Marine corps league uniform regulations
Marine corps league uniform regulations Hea associate fellowship
Hea associate fellowship Customer kpi
Customer kpi Why is critical thinking an active process? *
Why is critical thinking an active process? * Associate degree in the netherlands
Associate degree in the netherlands Rcog eportfolio
Rcog eportfolio Bcs membership benefits
Bcs membership benefits Mhp associate partner gehalt
Mhp associate partner gehalt Cincinnati state associate degrees
Cincinnati state associate degrees Iter project associate
Iter project associate Associate systems engineering professional
Associate systems engineering professional Experience assessment
Experience assessment Associate consultant in capgemini
Associate consultant in capgemini Delta chi flag
Delta chi flag Rekenhulp tegemoetkoming scholieren
Rekenhulp tegemoetkoming scholieren Associate consulting engineers
Associate consulting engineers Tecniche associate al pensiero computazionale
Tecniche associate al pensiero computazionale Ruckus certification training
Ruckus certification training Imeche associate membership
Imeche associate membership Safety associate
Safety associate