Womens Health Update Contraception Management Pamela J Keller



- Slides: 60
Women’s Health Update Contraception Management Pamela J Keller MSN, CRNP September 29, 2017
Contraception Practice of contraception is as old as human existence Earliest forms of contraception involved such things as a pessary of crocodile dung and fermented dough which created a hostile environment to sperm Today, voluntary control of fertility is importance to modern society Countries face crisis of population growth For women in general, control of reproduction can allow women to achieve individual goals and contribute to their own personal well being
Contraception June 2013 CDC issued selected practice recommendations for contraceptive use in US Most notable from these recommendations No labs needed before contraception initiated No PE other than BP check needed before COCP Cervical CA screening not necessary prior to IUD insertion IUD removal not needed for PID, Antibiotics sufficient
Contraception Decisions regarding a patients choice for contraception's options involves Efficacy Safety Non contraceptive benefits Cost Personal considerations Culture
Periodic Abstinence Coitus interruptus Withdrawal of entire penis from vagina before ejaculation Very dependent on mans ability to withdrawal prior to ejaculation Failure rate 4% in first year of perfect use, typical failure rate is 22% Advantage Immediate availability No cost No chemical involvement Theoretical reduced risk of STI Disadvantage High risk of pregnancy with incorrect or inconsistent use
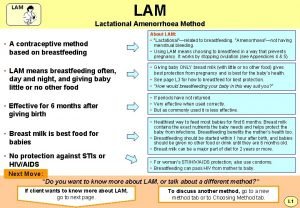
Periodic Abstinence Lactational Amenorrhea Elevated prolactin levels and reduction of gonadotropin releasing hormone from the hypothalamus during lactation suppress ovulation. Leads to reduction in LH release and inhibition of follicular maturation Duration of this suppression varies depends on duration of breastfeeding and length of time since birth Requires BF Q 4 hr during day, Q 6 hr at HS No supplementation No return of menses Baby less than 6 mo old Failure rate- perfect use 1 st 6 months is 0. 5%, typical use is 2%
Periodic Abstinence Lactational amenorrhea Advantage Can be used immediately after childbirth Facilitates PP weight loss Disadvantage Return of fertility is uncertain Frequent BF may be inconvenient Cannot be used in HIV + mom
Periodic Abstinence Natural family planning One of the most widely used methods Especially for religious and cultural beliefs do not permit devices or drugs Involves periodic abstinence Need to determine the fertile period using calendar method, cervical mucus method symptothermal method Failure rate in typical use is 25% Method requires discipline for effectiveness No protection against STD
Mechanical Barriers Male condom Most population barrier method Most effective protection of STI Failure rate if used correctly and consistently is 3% True failure rate is 14% Failure rate is related to errors in use Improper lubricant use Incorrect placement Poor withdrawal technique
Mechanical Barriers Adv Readily available inexpensive Disadv Decrease enjoyment of sex latex allergy Breakage
Mechanical Barriers Female condom Polyurethane sheath intended for one time use, closed ring inside, open end outside vaginal canal after insertion Prevents against pregnancy by barrier to passage of semen Not recommended to use male and female condom together Less than 1% use in US, 15% pregnancy rate Can be used as long as 8 hours prior to intercourse Does not contain spermicide Difficult to place in vagina, cumbersome, can cause UTI if left too long.
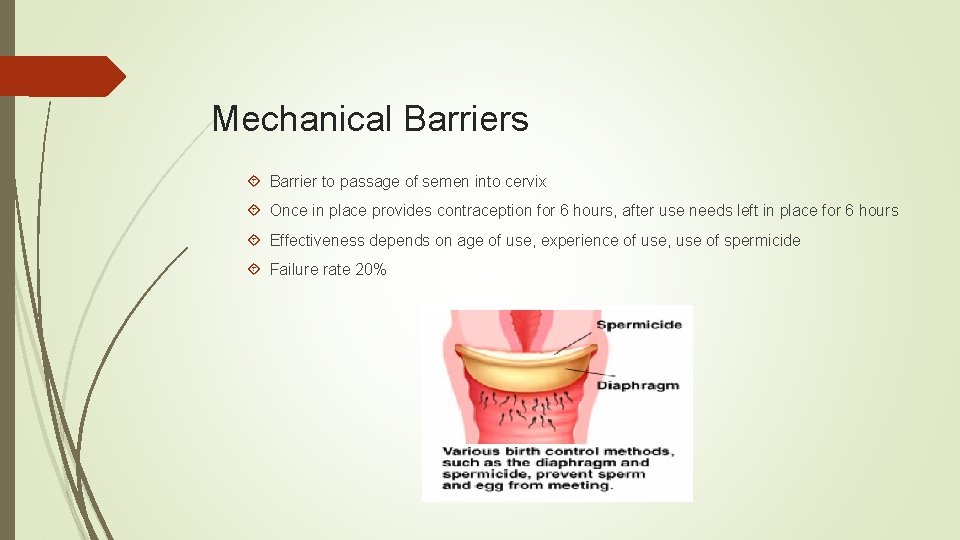
Mechanical Barriers Diaphragm Shallow latex cup with a spring mechanism to hold it in place Different diameters Requires a pelvic exam and measurement of diagonal length of vaginal canal Inserted before intercourse so posterior rim fits in posterior fornix Spermicidal cream or jelly used
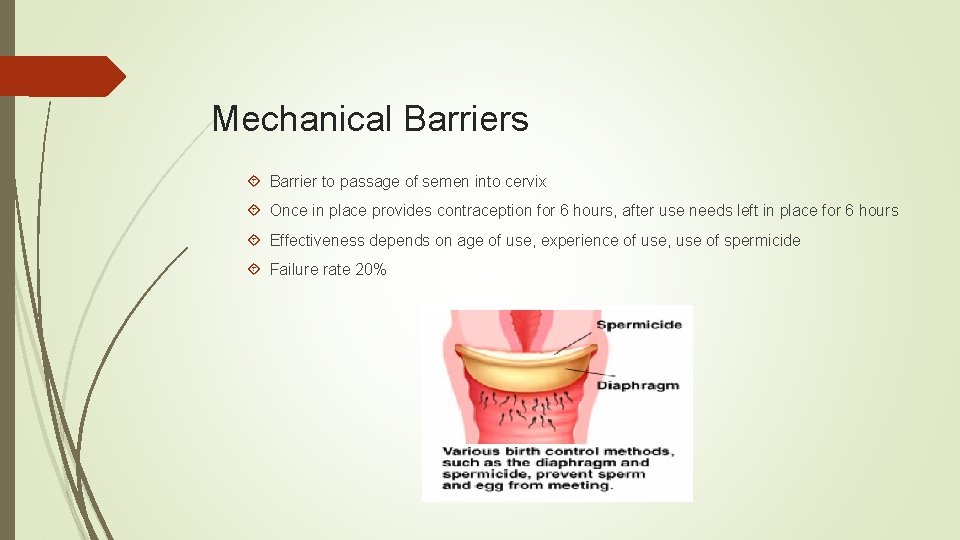
Mechanical Barriers Barrier to passage of semen into cervix Once in place provides contraception for 6 hours, after use needs left in place for 6 hours Effectiveness depends on age of use, experience of use, use of spermicide Failure rate 20%
Hormonal Contraceptions Implants First one approved was the Norplant in 1990, removed due to adverse events in 2002 2001 , Implanon was approved with fewer side effects. 2011 , Newest version is the Nexplanon, which is radiopaque for easier diagnostic testing
Hormonal Contraception Contains 68 mg of Etonogesterel Contraception occurs within 24 hrs of insertion if inserted during 1 st week of menstrual cycle Inserted subcutaneously Upper non dominant arm Visible under skin Palpable Works by suppression of LH surge, ovulation, development of mucus to prevent sperm penetration, prevent endometrial growth and development
Hormonal Contraception More effective than surgical sterilization Pregnancy rates with proper insertion 0. 05% for at least 3 years No exogenous estrogen Prompt return of fertility when removed Surgery needed for removal Menstrual irregularities are common HA, Breast tenderness, moodiness
Hormonal Contraception Depo Provera- DMPA Depomedroxyprogesterone Acetate Suspension of microcrystals of synthetic progestin that is injected IM Levels maintained for 3 months Can become undetectable in 7 -9 months Inhibition of ovulation with suppression of FSH and LH and eliminate of LH surge. Results in hypoestrogenic state 150 mg is good for as long as 15 weeks, 1 dose every 3 month
Depo Advantages Extremely effective option Does not produce serious side effects as with estrogen Decrease thromboembolism, dysmenorrhea, decreased anemia risk of endometrial ovarian ca Safe for breastfeeding
Depo Disadvantages Disruption of menstrual cycle occurs in 50% women Persistent irregular bleeding Can result in delay of return of fertility because of its persistence in body Weight gain Depression Weight gain can be indicative of future weight gain Black box warning in 2004 Bone loss may not be totally reversible
Hormonal Contraception Progestin only Oral contraceptives Minipill- Nor QD Not widely used in US Less than 1% of users use them as sole birth control BF moms Women with contraindication to estrogen use
Hormonal Contraception POP Suppression of ovulation Variable dampening effects of midcycle peaks of FSH LH Increase in cervical mucus viscosity Reduction in number and size of endometrial glands, leading to decreased endometrium Reduce cilia motility, slowing transport
Hormonal Contraception Progestin levels peak at about 2 hours after administration Best with consistent use Failure rates 7% Minimal risk of thromboembolism Decreased dysmenorrhea, decreased menstrual bleeding Fertility is immediately re established after cessation of use Continuous use needed for compliance Back up method needed if pills missed or late
Combined Oral contraception Marketed since 1962 Dose has significantly decrease in last 40 yrs Ethinyl estradiol used in all preparations less than 35 mcg of estrogen in US Progestin component contains norethindrone, levonorgestrel, norgestimate, desogestrel, drospirenone. Newest one Yasmin More than 30 preparations are available Monophasic Biphasic Triphasic
COCP Missed pill take as soon as remembered If missed longer than 2, use back up method Prevents ovulation is Mechanism of action Failure rates correlates to compliance 0. 1 -5%
COCP Used to treat menstrual irregularities Used to decrease anemia by controlling cycle Can manipulate cycle to avoid cycle or skip cycle Works by Suppression of ovarian stimulation by FSH and LH reduces functional cysts
COCP Cessation of ovulation prevent ectopic pregnancies Prevents ovarian carcinoma by 40% Endometrial CA by 50%- and protection continues for at least 15 years following discontinuing use SE Nausea, Breast tenderness, BTB, amenorrhea, HA, no STI prevention

COCP Metabolic effects Venous thrombosis estrogen component of COCP has the capability of activating the blood clotting mechanism Greater risk in smokers Hyperlipidemia Diabetes HTN Obesity Hypertension Dose related effect on BP Related to estrogen increase in renin substrate in susceptible individuals Surveillance of BP advised POP is recommended
COCP Metabolic effects Atherogenesis and stroke Habits are more significant than the pills themselves sedentary Obesity Smoker HTN DM If has hypercholesteremia = more risk
Hepatocellular adenoma Benign liver tumors danger lies in the rupture of the capsule, leading to extensive bleeding and death New lower dose ocp’s are equal to lower risks Cancer Association with breast cancer is controversial Association with cervical cancer also controversial Risks of early sexual intercourse Exposure to HPV Pap smear screening recommended
91 day COCP Seasonale Menses every 3 months 12 weeks of active pills/ 1 week of placebo Ethinyl estradiol/ levonorgestrel Can have intermittent bleeding and spotting Seasonique Developed to counter act the unplanned bleeding Eliminates the hormone free interval 84 active pills/ 7 more active pills- no hormone free weeks Benefits include decreased bleeding
91 day COCP All COCP can be dosed continuously. No need to have a menses except for fertility. May need to have a cyclic bleeding depending on breakthrough bleeding
Combination Patch Available since 2001 Each patch contains 1 week of hormone Failure rate 1 pregnancy in 100 women Decreased nausea Greater compliance Skin irritation Less effective for women who weight more than 200 lbs
Combination Patch New studies indicate that Patch has a higher steady state of concentration of estrogen in the patch, up to 60% higher in women who use the patch New back box warning in 2005 Increased estrogen exposure increases the clot risk Though new studies have found similar risks with use of oral products
Nuvaring First developed in 1970’s Approved by FDA in 2001 In for 3 weeks, out for 1 If expelled should be rinsed and replaced Increased compliance with ring Results in complete suppression of ovulation Presumed to be more effective than OCP
Nuvaring Advantages Return of fertility after d/c of use is rapid Highly acceptable for women and partners Nausea and vomiting is avoided Disadvantages Headaches Vaginal irritation Feeling ring during intercourse
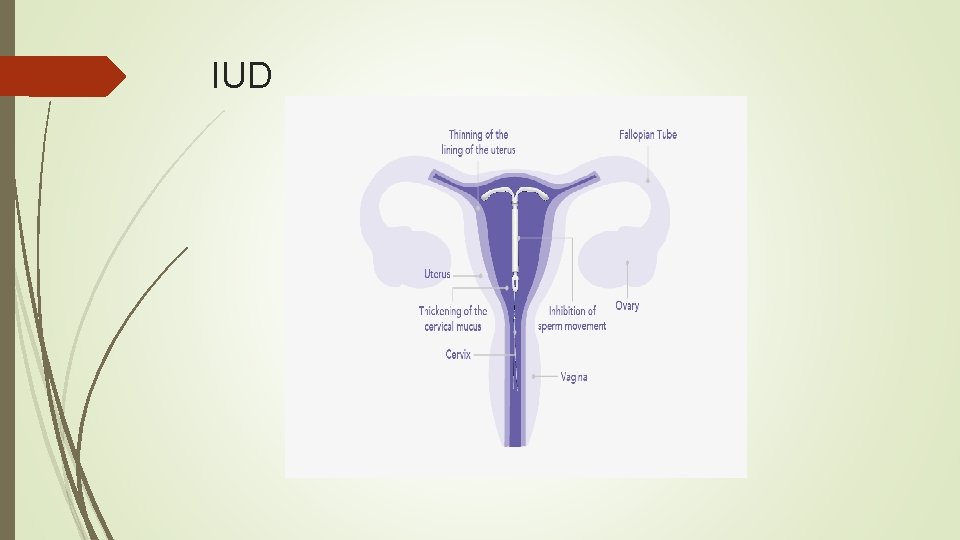
IUDS Most effective contraceptive devices available Pregnancy rates <1% CDC recommends screening for GC/C at time of placement to prevent PID Gaining popularity Especially in the 15 -44 year old age group
Paragard Copper IUD Introduced in 1988 Made of polyethylene and fine copper wire wrapped around vertical stem Foreign body reaction creates toxic intrauterine environment Prevents fertilization Effectiveness good for 10 years Failure rate 0. 6%
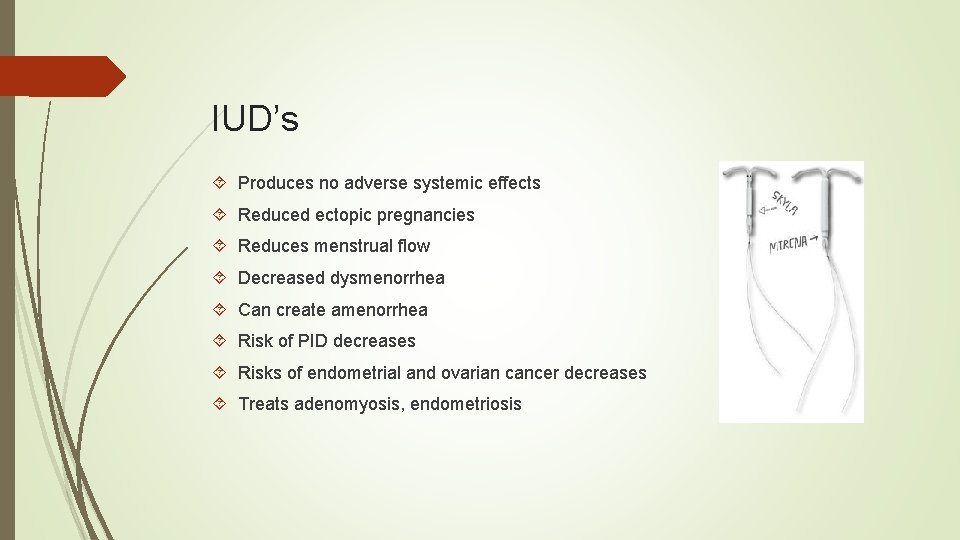
IUD’s Mirena approved in December 2000 Similar in shape to Paragard, but contains levonorgestrel, a progesterone Cylinder is coated with a membrane that regulates the release of the hormone Good for 5 years Visible on x-rays Treats menorrhagia as well Failure rate 0. 1%

IUD’s Liletta- approved 2015 - 5 years of use Skyla- approved in 2013, 3 years of use, smaller in size, but less hormone can create increased risk of spotting Kyleena- approved 2016, 5 years of use, smaller like Skyla
IUD’s Produces no adverse systemic effects Reduced ectopic pregnancies Reduces menstrual flow Decreased dysmenorrhea Can create amenorrhea Risk of PID decreases Risks of endometrial and ovarian cancer decreases Treats adenomyosis, endometriosis
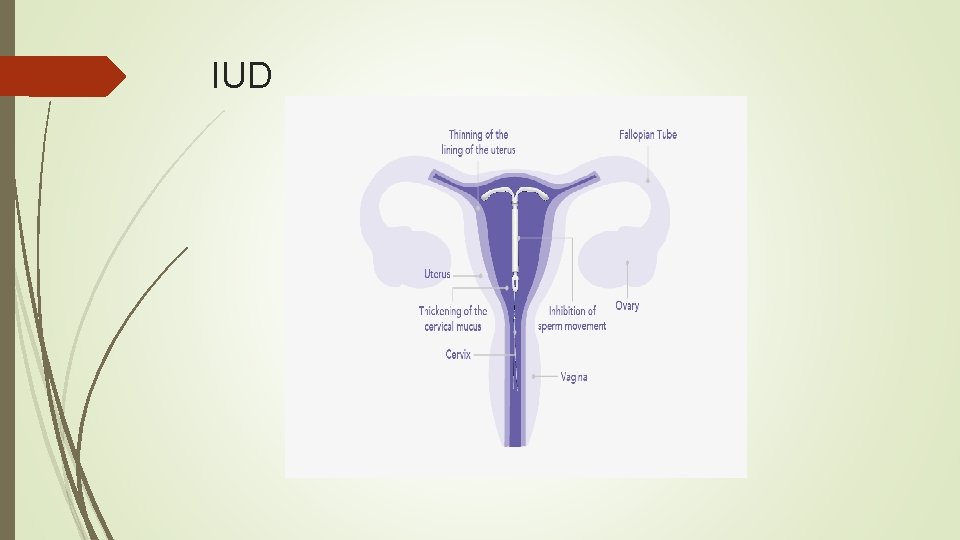
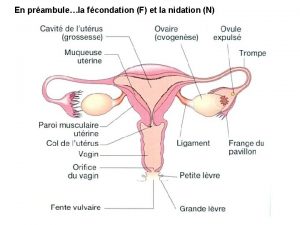
IUD
IUDS Risk of uterine perforation at insertion No protection of STD Contraindicated abnormal uterine cavity Undiagnosed genital bleeding Uterine malignancy Cervical malignancy Wilson disease Pregnancy Active infection
Sterilization Choices Elective permanent method of sterilization Can be reversed surgically, but more difficult than the original procedure may not be successful Success greater with tubal reanastomosis than vas deferens Failure rate depends on how the tubal is done Essures Met with a lot of controversy lately, litigation
Contraception Vasectomy Involves incision of scrotal sac, transsection of vas deferens and occlusion of severed ends by suture or fulguration Local anesthesia Out patient Sperm can remain in ejaculatory ducts after procedure Semen analysis needed to document sperm free ejaculate Require 15 -20 ejaculates to clear the ducts
Future of contraception Research in US has slowed, but outside had continued at rapid pace Goal is to produce new options with fewer adverse effects, safer and more efficacious Most notable is the hormonal contraceptive for men Male pill manipulates steroid hormones to decrease sperm production and testosterone secretion Biodegradable implant to eliminate the need for removal. Pellets Vaginal sponge Pregnancy vaccine- most exciting and controversial
Good Resource in Primary care Good resource book- Managing Contraceptive Pill/Drug Patients, by Richard Dickey MD.
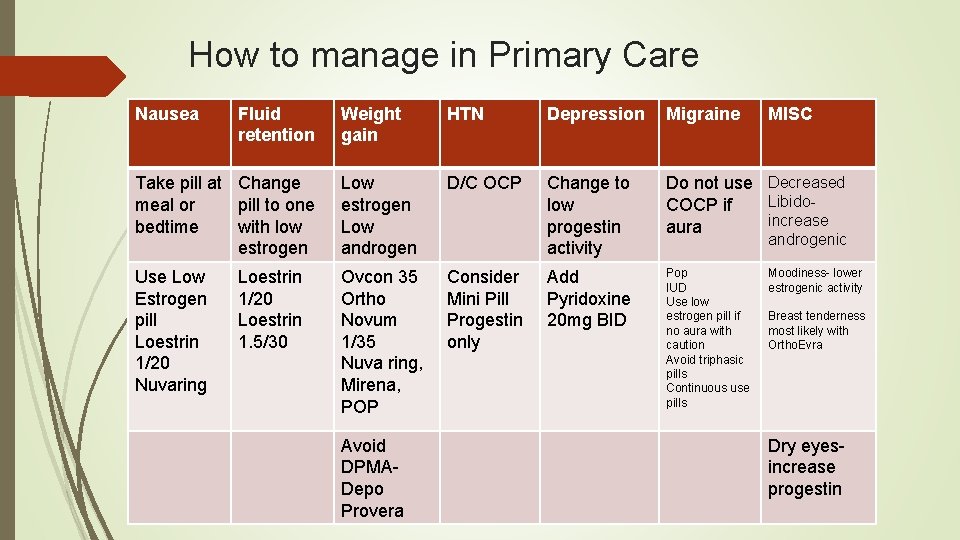
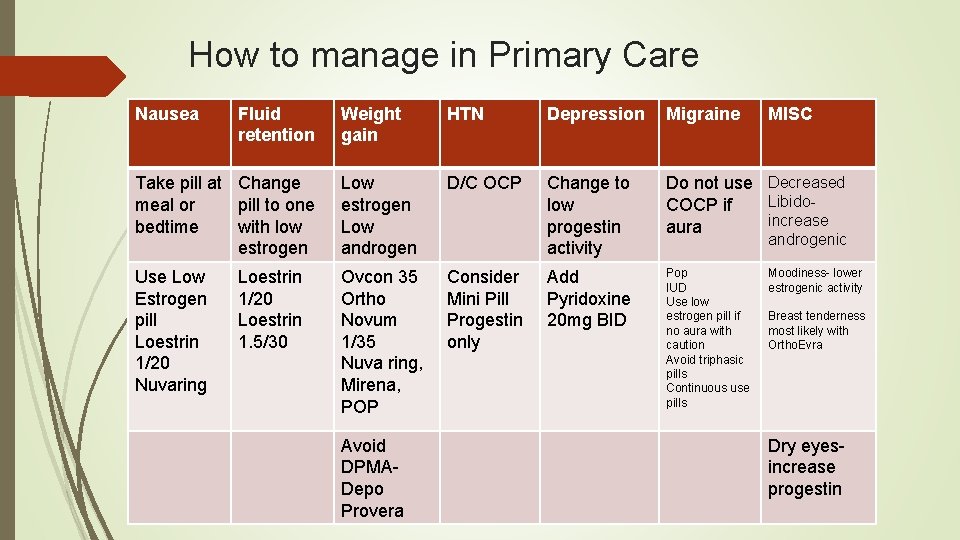
How to manage in Primary Care Nausea Fluid retention Weight gain HTN Depression Migraine Take pill at Change meal or pill to one bedtime with low estrogen Low androgen D/C OCP Change to low progestin activity Do not use Decreased Libido. COCP if increase aura Use Low Estrogen pill Loestrin 1/20 Nuvaring Ovcon 35 Ortho Novum 1/35 Nuva ring, Mirena, POP Consider Mini Pill Progestin only Add Pyridoxine 20 mg BID Pop IUD Use low estrogen pill if no aura with caution Avoid triphasic pills Continuous use pills Loestrin 1/20 Loestrin 1. 5/30 Avoid DPMADepo Provera MISC androgenic Moodiness- lower estrogenic activity Breast tenderness most likely with Ortho. Evra Dry eyesincrease progestin
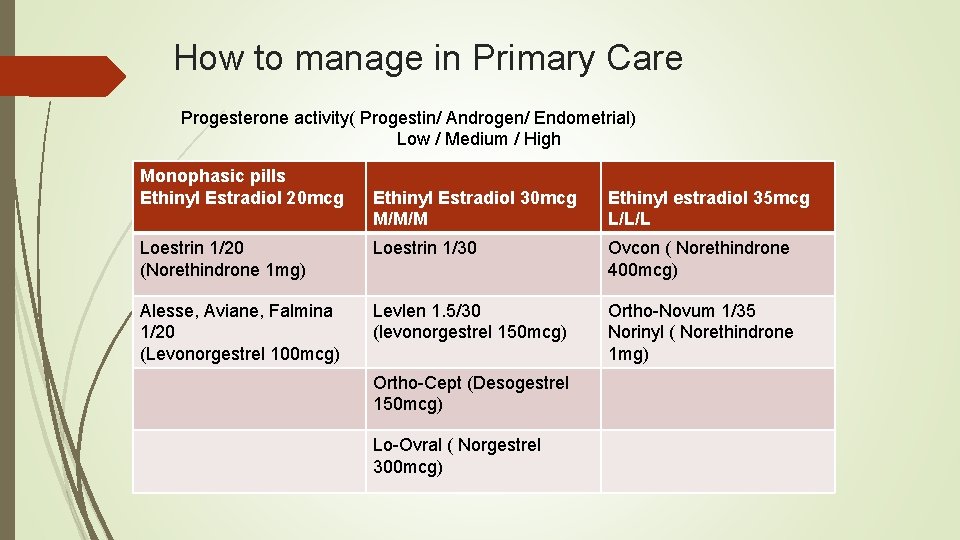
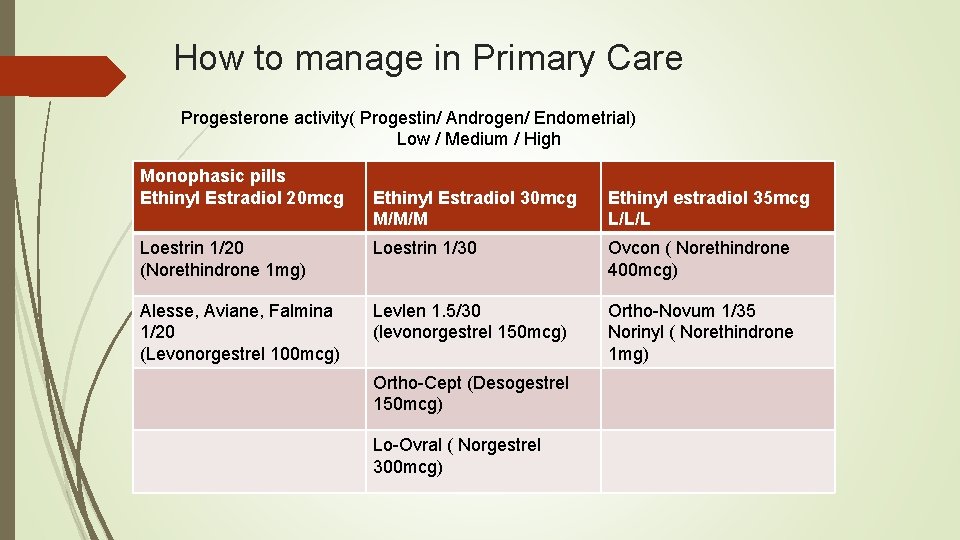
How to manage in Primary Care Progesterone activity( Progestin/ Androgen/ Endometrial) Low / Medium / High Monophasic pills Ethinyl Estradiol 20 mcg Ethinyl Estradiol 30 mcg M/M/M Ethinyl estradiol 35 mcg L/L/L Loestrin 1/20 (Norethindrone 1 mg) Loestrin 1/30 Ovcon ( Norethindrone 400 mcg) Alesse, Aviane, Falmina 1/20 (Levonorgestrel 100 mcg) Levlen 1. 5/30 (levonorgestrel 150 mcg) Ortho-Novum 1/35 Norinyl ( Norethindrone 1 mg) Ortho-Cept (Desogestrel 150 mcg) Lo-Ovral ( Norgestrel 300 mcg)
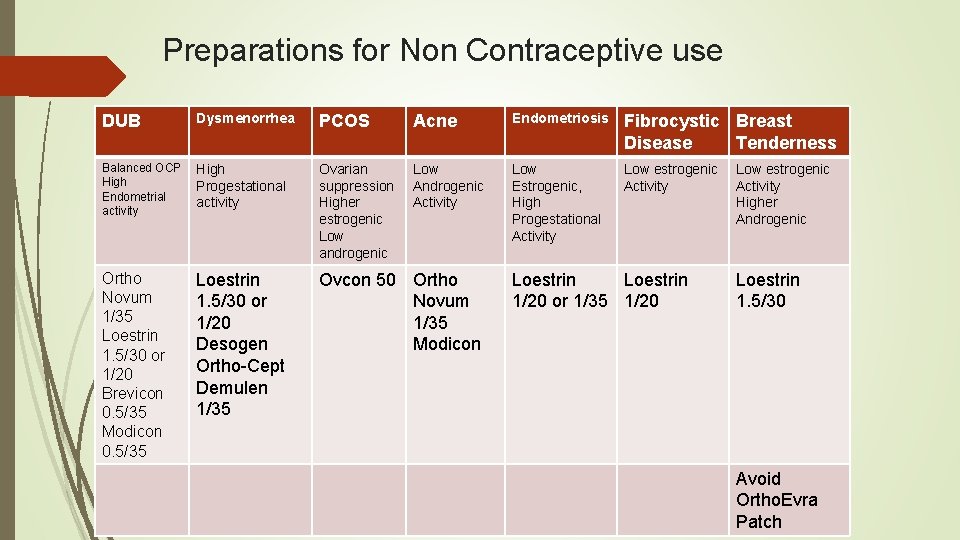
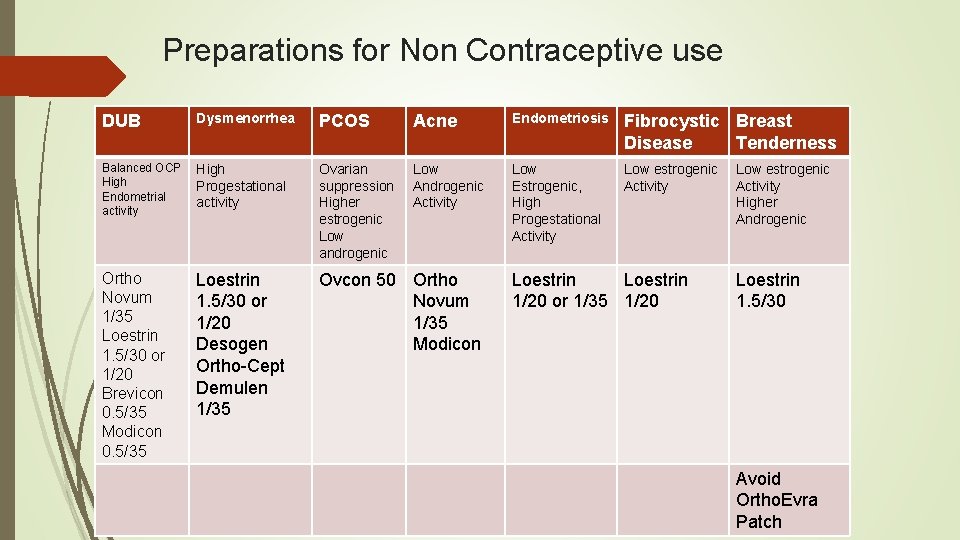
Preparations for Non Contraceptive use DUB Dysmenorrhea PCOS Acne Endometriosis Fibrocystic Breast Disease Tenderness Balanced OCP High Endometrial activity High Progestational activity Ovarian suppression Higher estrogenic Low androgenic Low Androgenic Activity Low Estrogenic, High Progestational Activity Low estrogenic Activity Ortho Novum 1/35 Loestrin 1. 5/30 or 1/20 Brevicon 0. 5/35 Modicon 0. 5/35 Loestrin 1. 5/30 or 1/20 Desogen Ortho-Cept Demulen 1/35 Ovcon 50 Ortho Novum 1/35 Modicon Loestrin 1/20 or 1/35 1/20 Low estrogenic Activity Higher Androgenic Loestrin 1. 5/30 Avoid Ortho. Evra Patch
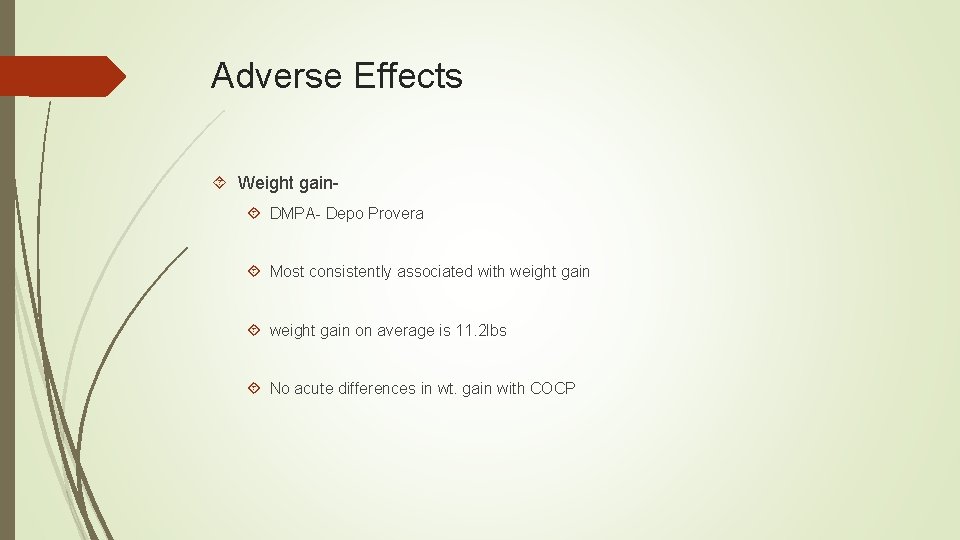
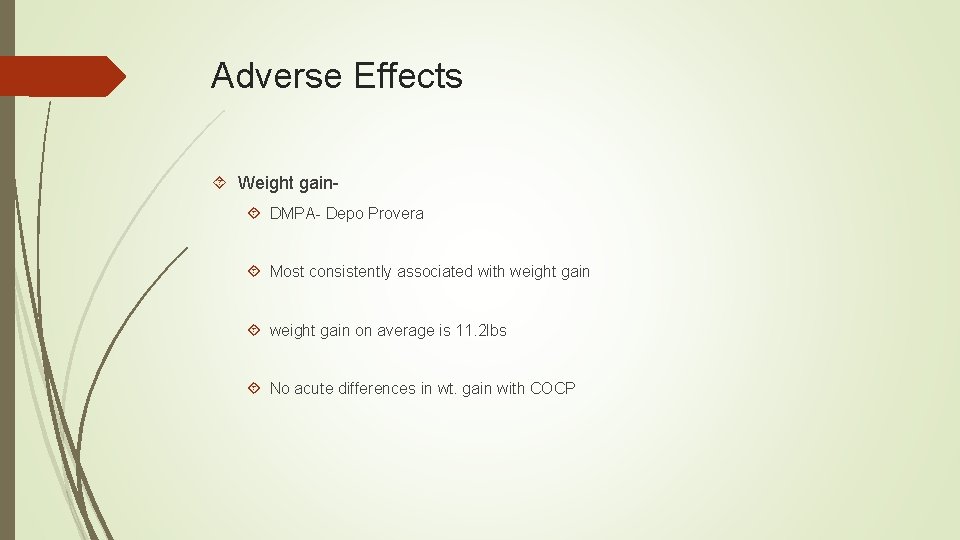
Adverse Effects Weight gain DMPA- Depo Provera Most consistently associated with weight gain on average is 11. 2 lbs No acute differences in wt. gain with COCP
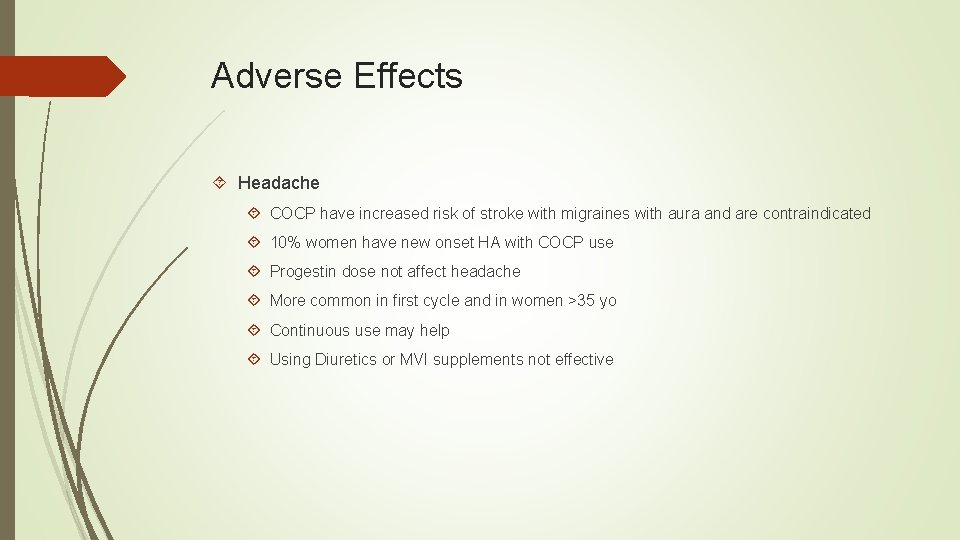
Adverse Effects Headache COCP have increased risk of stroke with migraines with aura and are contraindicated 10% women have new onset HA with COCP use Progestin dose not affect headache More common in first cycle and in women >35 yo Continuous use may help Using Diuretics or MVI supplements not effective
Adverse Effects Breast Tenderness Use of COCP decreases breast tenderness after 18 mo. of use No significant differences in formulations More common in women who use patch due to increase hormonal concentration
Adverse Effects Breakthrough Bleeding Common in first months of use Patients need reassurance this will happen Variations in estrogen dose does not always make a difference Women with norethindrone regimens more amenorrhea than those with levonorgestrel If BTB on extended cycle dosing, patients should be instructed to take a break at next end of pack for 3 -4 days then resume dosing
Adverse Effects Irregular Bleeding Often d/c use of pills for menstrual cycle disorders POP and Low Dose COCP < 20 Mcg a day are most commonly associated with bleeding disturbances Depo Provera most common NSAIDs may be helpful in helping with bleeding If using Implant, pt. need counseled that only 11% of women having normal bleeding pattern Can use double suppression
Adverse Effects Sexual Effects Studies have been inconsistent Pharmacologic basis is unclear Bioavailable testosterone is lower in women who use COCP than non users Many studies have been done comparing all forms of contraception with non being more disrupting than other. Sexual function is very multifactorial- A good History is the key to most problems Talk to your patients
Adverse Effects Skin Changes Acne worsens with Progestin only products- ( nexplanon, IUD’s) Can improve with COCP, after 6 mo. Nuvaring users in Cochrane review reported less acne
Adverse Effects Nausea Emergency contraception the worst culprit Pretreatment with Reglan or Meclizine can reduce nausea WHO recommends this pretreatment For non emergency use, no specific differences in tolerance

References Barr, N. G. , M. D. (2010, December 14). Managing adverse effects of contraceptives. American Family Physician, 82(12), 1499 -1565. hormonal Casey, F. E. , & Lucidi, R. S. (2016, December 7). Contraception. Retrieved from http: //emedicine. Medscape. com/article/258507/- overview. August 8, 2017, Dean, G. , MD, MPH, & Goldberg, A. , MD, MPH. (2017, September 12). Intrauterine contraception: Devices, candidates, and selection. Retrieved August 8, 2017, from https: //www. uptodate. com/contents/intrauterine-contraception-devicescandidates-and-selection? source=see_link Kaunitz, A. , M. D. (2016, December 14). Progestin Only Pills. Retrieved August from https: //www. uptodate. com/contents/progestin-only-pillspops-forcontraception? source=see_link Kaunitz, A. , M. D. (2017, August 21). Depot medroxyprogesterone acetate for contraception. Retrieved August 8, 2017, from https: //www. uptodate. com/contents/depot-medroxyprogesterone-acetate-forcontraception? source=see_link 8, 2017,
References Kaunitz, A. , MD. (2017, April 21). Contraceptive counseling and selection. Retrieved August 8, 2017, from https: //www. uptodate. com/contents/contraceptive-counseling-andselection? source=search_result&search=contraceptives&selected. Title=1~150 Martin , K. A. , M. D. , & Barbieri, R. L. , M. D. (2016, August 17). Overview of the of estrogen-progestin contraceptives. Retrieved August 8, 2017, from https: //www. uptodate. com/contents/overview-of-the-use-of-estrogenprogestin-contraceptives? source=see_link Moses, S. , M. D. (2017, August 6). Oral contraceptive selection. Retrieved August 8, 2017, from http: //www. fpnotebook. com/gyn/Pharm/Orlcntrcptv. Sd. Efct. Mngmnt. htm Moses, S. , M. D. (2017, September 3). Oral contraceptive Side Effect management. Retrieved August 8, 2017, from http: //www. fpnotebook. com/gyn/Pharm/Orlcntrcptv. Sd. Efct. Mngmnt. htm use
 Database backup and recovery techniques
Database backup and recovery techniques How to use calendar method of family planning
How to use calendar method of family planning French envelope contraception
French envelope contraception Cape cervicale caya
Cape cervicale caya Contraception for over 40s
Contraception for over 40s Contraception
Contraception Diaphragme contraception caya
Diaphragme contraception caya Voluntary surgical contraception
Voluntary surgical contraception What is lam contraception
What is lam contraception Mode d'action de la pilule contraceptive
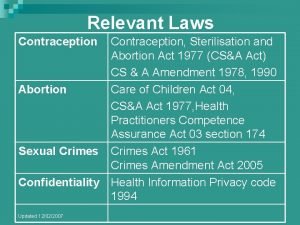
Mode d'action de la pilule contraceptive Contraception sterilisation and abortion act 1977
Contraception sterilisation and abortion act 1977 Alvin isd insurance
Alvin isd insurance Needs of adolescence
Needs of adolescence Womens rights
Womens rights Late night womens hour
Late night womens hour Claire paine
Claire paine Womens right
Womens right Differences between men's and women's soccer
Differences between men's and women's soccer Womens college kumbakonam
Womens college kumbakonam Womens college kumbakonam
Womens college kumbakonam Womens right
Womens right Womens shelter edmonton
Womens shelter edmonton Womens rights
Womens rights Virginia of a woman
Virginia of a woman Womens history month door
Womens history month door Womens community shelters
Womens community shelters Ballybeen womens centre
Ballybeen womens centre Scarborough womens centre
Scarborough womens centre Girls lacrosse helmets
Girls lacrosse helmets Bristol womens voice
Bristol womens voice Kotler and keller
Kotler and keller Triangulo del bullying
Triangulo del bullying Dra pamela santos
Dra pamela santos Pamela thielman
Pamela thielman Pamela tossati
Pamela tossati Pamela goldberg
Pamela goldberg La mia citta'
La mia citta' La famiglia di sara
La famiglia di sara Pamela nicoara
Pamela nicoara Pamela aray
Pamela aray Snapshot
Snapshot Dr pamela beck
Dr pamela beck Pamela guest
Pamela guest Pam nicholson net worth
Pam nicholson net worth Pamela schwartz
Pamela schwartz Pamela fishman gender theory
Pamela fishman gender theory Pamela harman
Pamela harman Christy henrich
Christy henrich Bianka bella bryant pam bryant
Bianka bella bryant pam bryant Pamela weber harris
Pamela weber harris Pamela ralf
Pamela ralf Pamela masajes
Pamela masajes What is vignette-style mcqs
What is vignette-style mcqs Euclideon unlimited detail
Euclideon unlimited detail Pamela hines science
Pamela hines science Daniele zullino
Daniele zullino Ego dystonic
Ego dystonic Pamela knapp
Pamela knapp Condiciones subestandar ejemplos
Condiciones subestandar ejemplos Pamela caillens
Pamela caillens Sinus
Sinus