Why medical students find difficult patients difficult Jody









- Slides: 32
Why medical students find “difficult patients” difficult Jody Steinauer, MD, MAS Patricia O’Sullivan, Ed. D, Felisa Preskill, MPP, Olle Ten Cate, Ph. D, Arianne Teherani, Ph. D
Background • Physicians feel negative emotions toward patients – “Difficult Patients” – 20%1 – Harder to provide empathic, patient-centered care • Physicians trust and like some more than others 2, 3 • They blame some for medical problems 4 • They label some as “bad” or “problem” patients 5 • “Difficult” patients have less satisfaction with care 1 • Higher quality of interaction - better outcomes 3, 6 1. Hinchey, JGIM, 2011; 2. Thom, Ann Fam Med, 2011; 3. Hall, Patient Educ Couns, 2002; 4. Tait, J Behav Med, 2005; 5. Lorber, J Health Soc Behav, 1975; 6. Kim, Eval Health Prof, 2004.
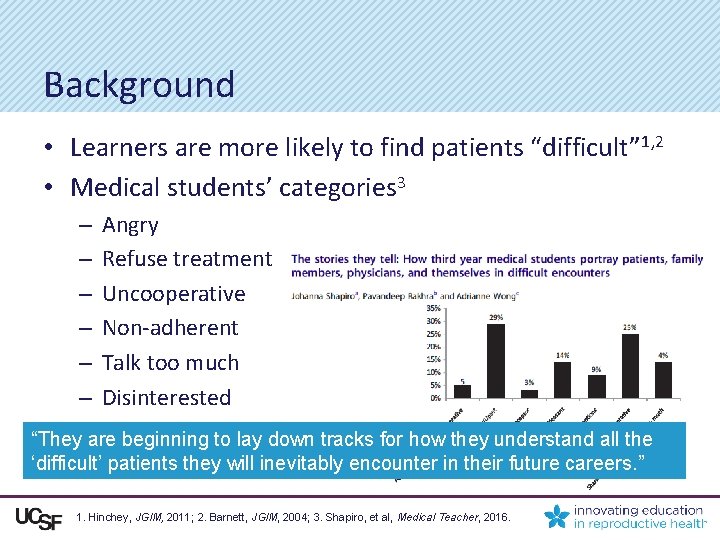
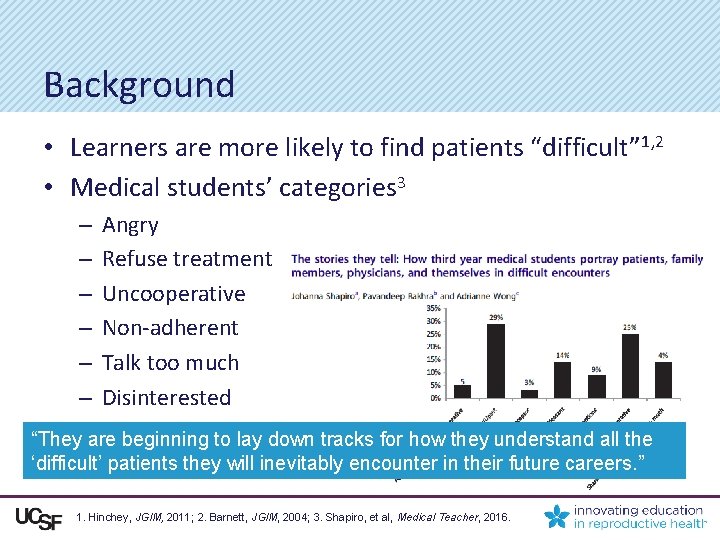
Background • Learners are more likely to find patients “difficult” 1, 2 • Medical students’ categories 3 – – – Angry Refuse treatment Uncooperative Non-adherent Talk too much Disinterested “They are beginning to lay down tracks for how they understand all the ‘difficult’ patients they will inevitably encounter in their future careers. ” 1. Hinchey, JGIM, 2011; 2. Barnett, JGIM, 2004; 3. Shapiro, et al, Medical Teacher, 2016.
Research Question How and why do medical students experience patients who invoke negative feelings? Professional Identity Formation
Methods • Qualitative interview study of 4 th-year UCSF medical students recruited before graduation (after rank list in) • Constructivist Grounded Theory – Methodological orientation • Interview content Describe a time when you felt negative emotions, such as anger or frustration, with a patient. – 2 stories of patients toward whom they felt negative emotions – Additional probes: patterns, strategies Charmaz, Constructing Grounded Theory, Sage Publishing, 2014.
Methods • Constant comparison – Iterative coding with data collection • Codebook – Created by 3 investigators, revised over 5 interviews • Theoretical sufficiency – Stopped interviews when no new patterns identified 1 • Synthesis – Grouped codes into themes, found connections, created theory • Reflexivity – Interviews conducted by me, an ob-gyn clinician educator, and a public policy-trained associate 1. Charmaz, Constructing Grounded Theory, Sage Publishing, 2014.
Results: Learning to Care for Challenging Patients in the Clinical Learning Environment • 180 invited, 44 responded, 26 interviewed – 13 women, mean age 29 • Each described 2 - 8 specific patients • “Difficult patient” categories similar to physicians – – – Angry, mean, manipulative Declined recommended treatments Caused their own problems “Unfixable” problems Many had psychiatric and/or substance use disorders • Students felt frustrated, powerless, disrespected

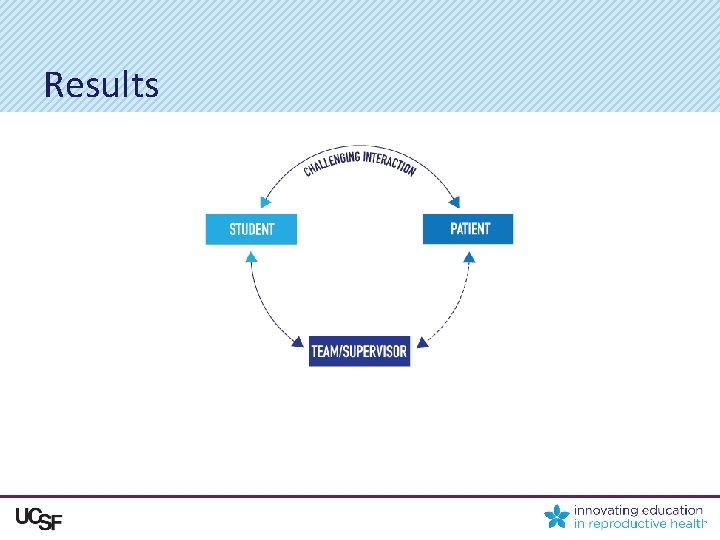
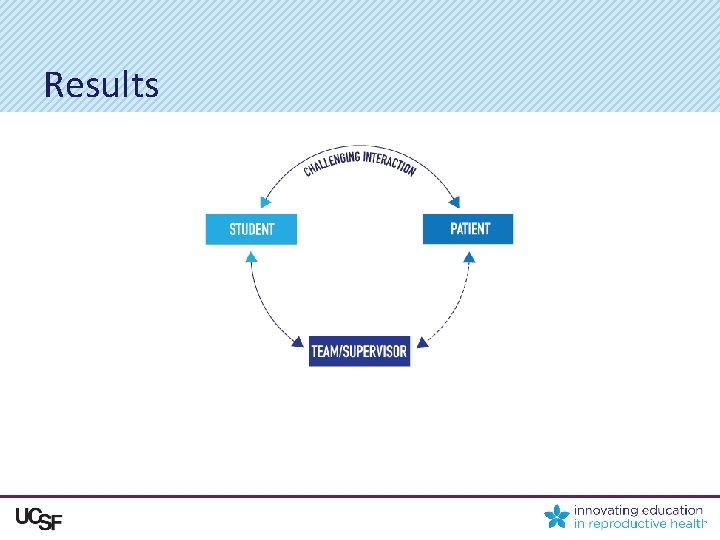
Results
Results
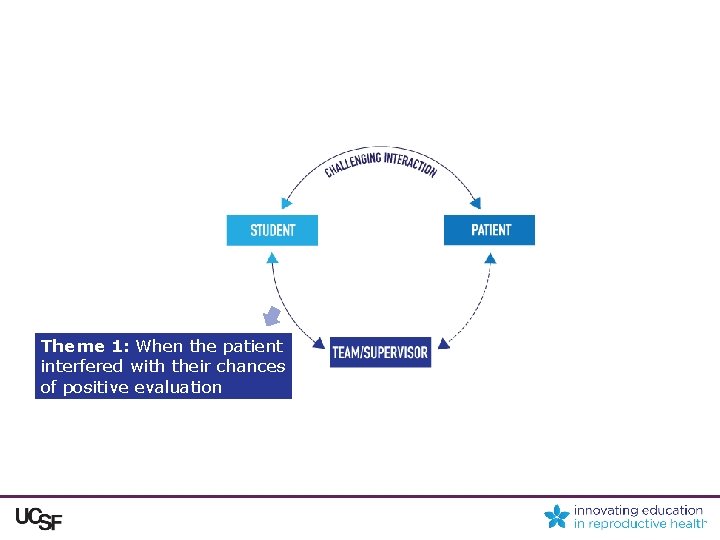
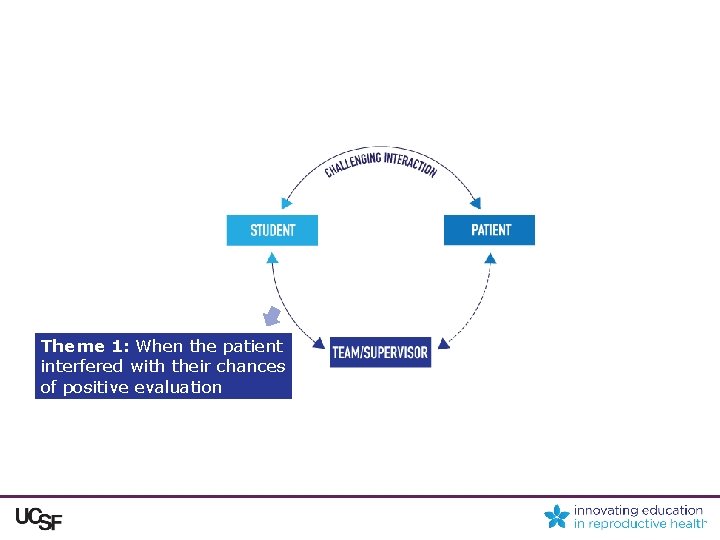
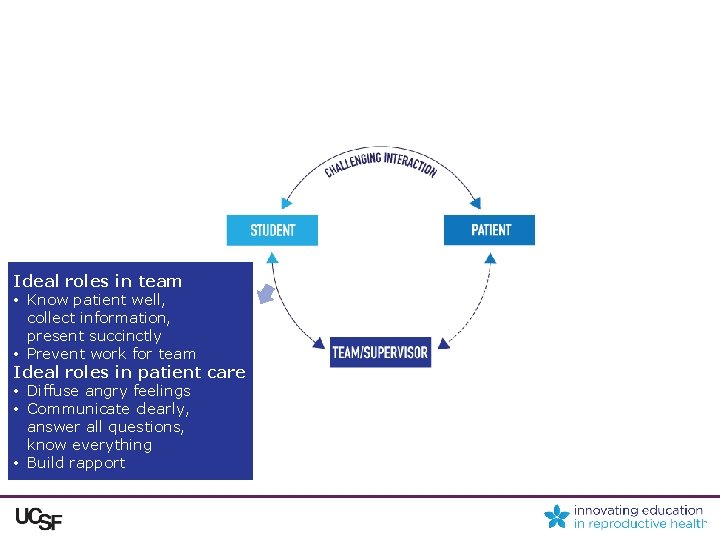
Theme 1: When the patient interfered with their chances of positive evaluation
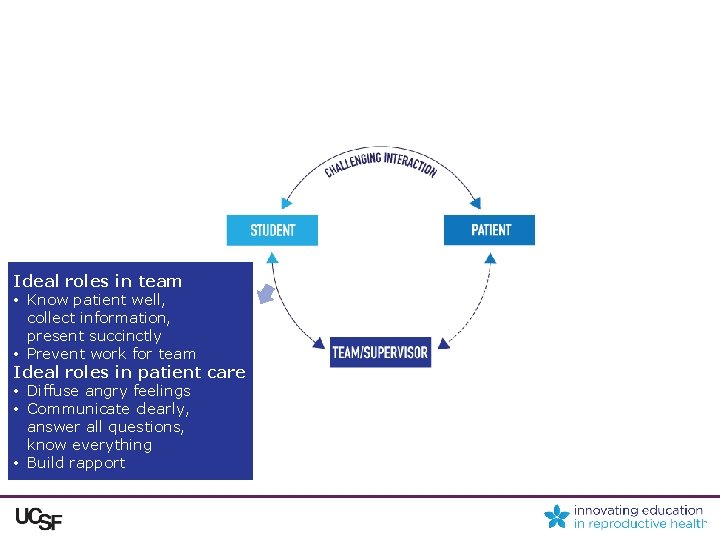
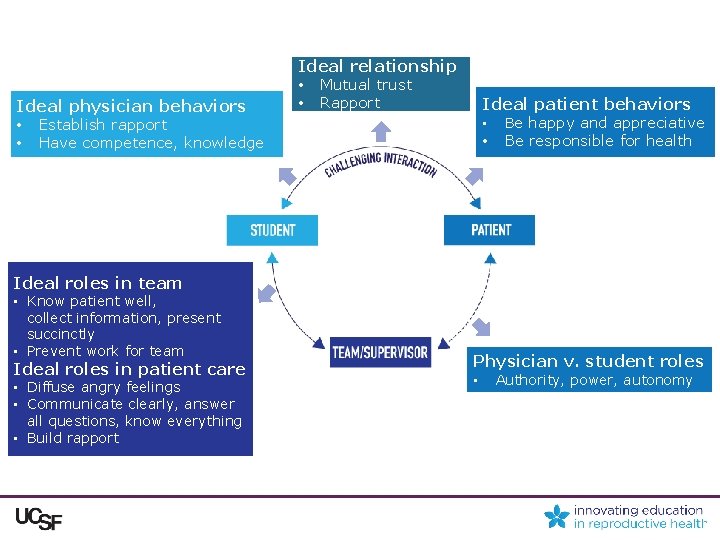
Ideal roles in team • Know patient well, collect information, present succinctly • Prevent work for team Ideal roles in patient care • Diffuse angry feelings • Communicate clearly, answer all questions, know everything • Build rapport

It’s frustrating because I keep thinking, oh, my gosh, I’m only supposed to be in here for maybe 20 minutes at most before I need to go and talk to my preceptor and I can’t get even the most basic information out of her… And when you’re on your third year, you’re pre-rounding and you do your presentation, that’s your time to shine as a student. And if you haven’t gotten the information or you weren’t able to finish whatever your task was, then it’s like, oh, you didn’t do this one job you had. Results
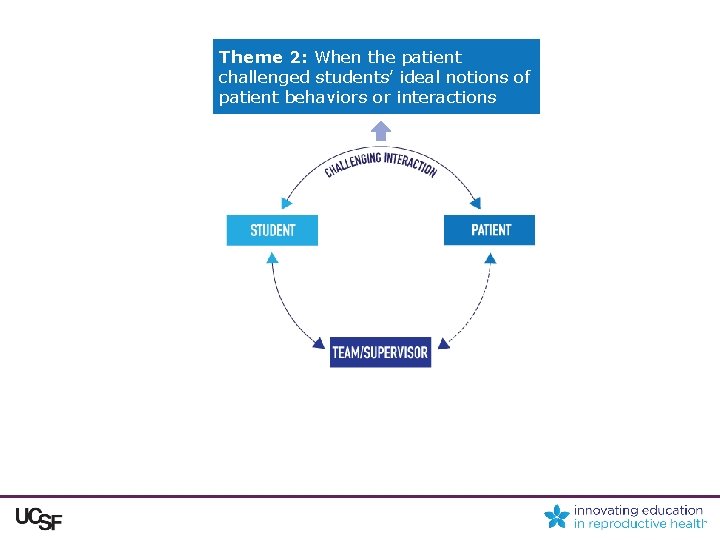
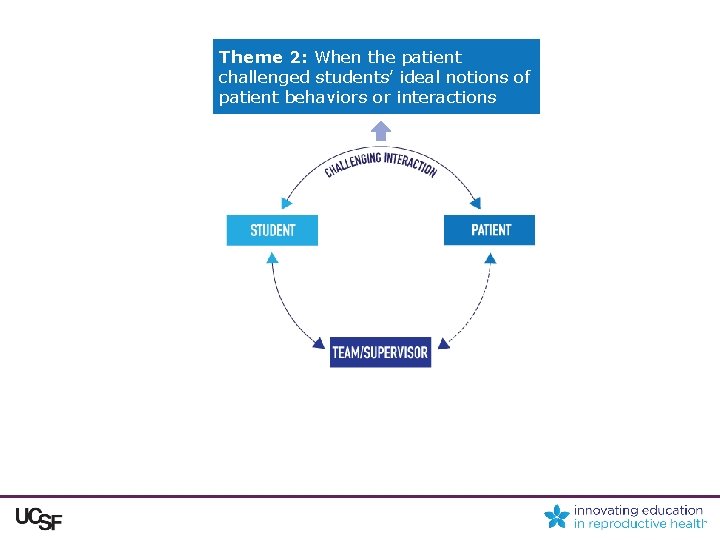
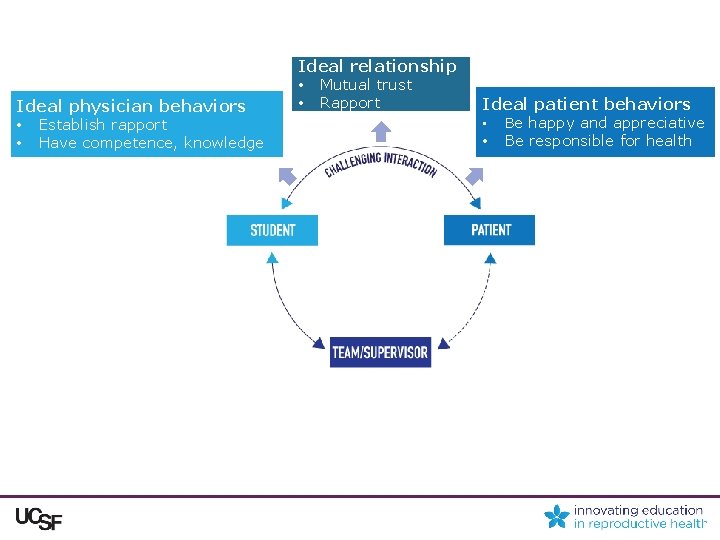
Theme 2: When the patient challenged students’ ideal notions of patient behaviors or interactions
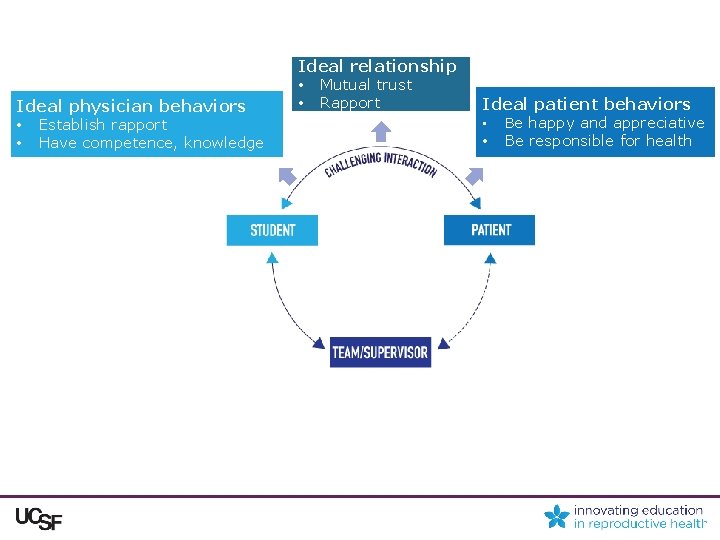
Ideal physician behaviors • Establish rapport • Have competence, knowledge Ideal relationship • Mutual trust • Rapport Ideal patient behaviors • • Be happy and appreciative Be responsible for health
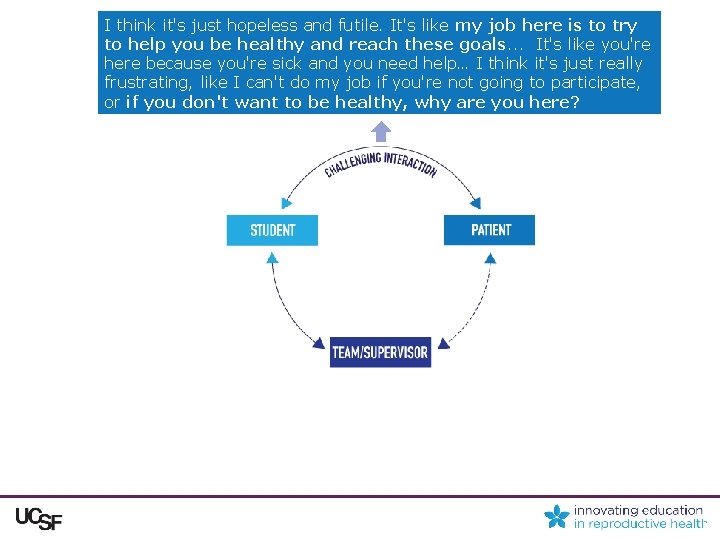
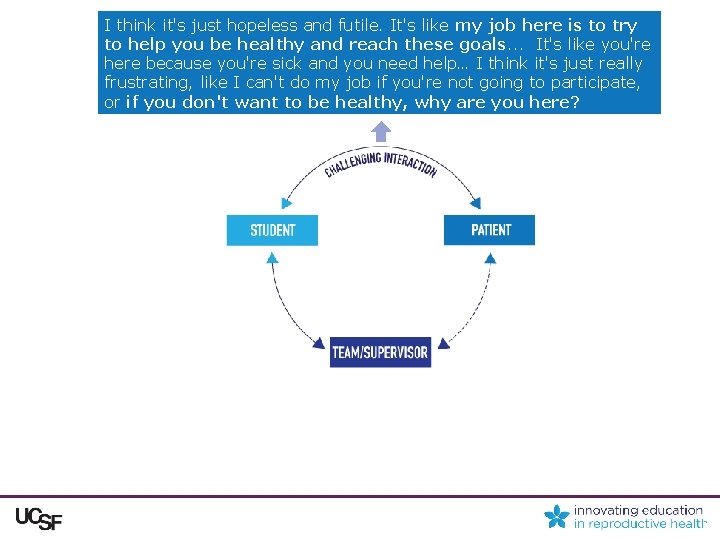
I think it's just hopeless and futile. It's like my job here is to try to help you be healthy and reach these goals. . . It's like you're here because you're sick and you need help… I think it's just really frustrating, like I can't do my job if you're not going to participate, or if you don't want to be healthy, why are you here?
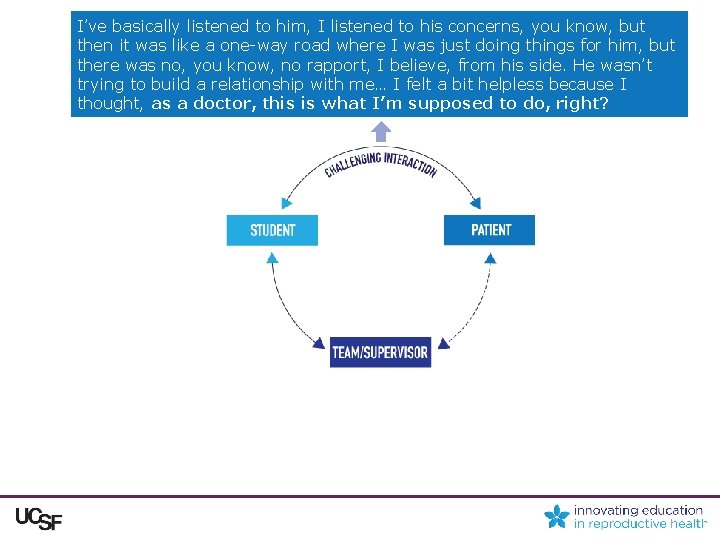
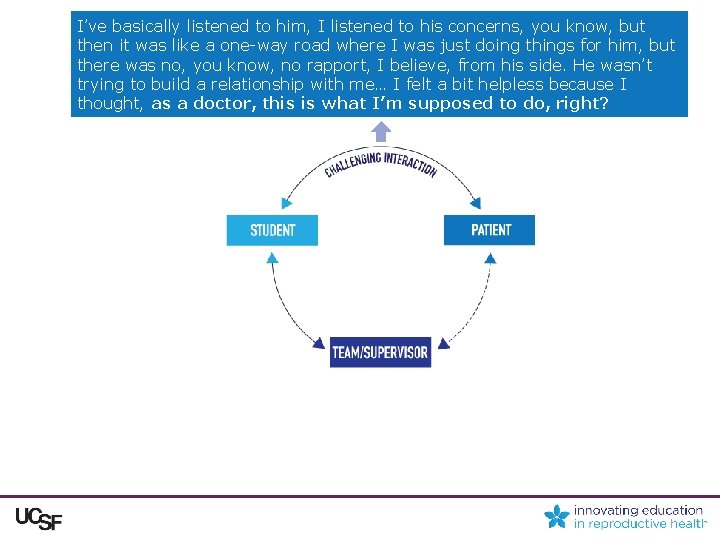
I’ve basically listened to him, I listened to his concerns, you know, but then it was like a one-way road where I was just doing things for him, but there was no, you know, no rapport, I believe, from his side. He wasn’t trying to build a relationship with me… I felt a bit helpless because I thought, as a doctor, this is what I’m supposed to do, right?

Theme 3: When the student lacked competence and authority to provide independent care

Ideal physician roles v. reality of student roles • Authority, power, autonomy
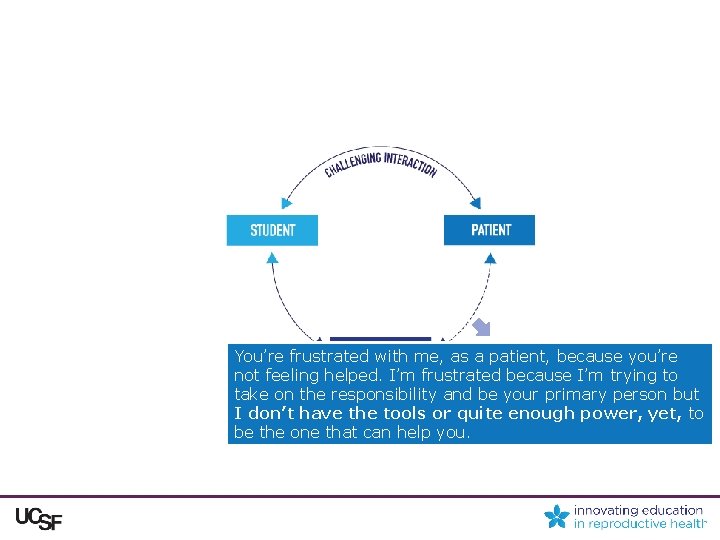
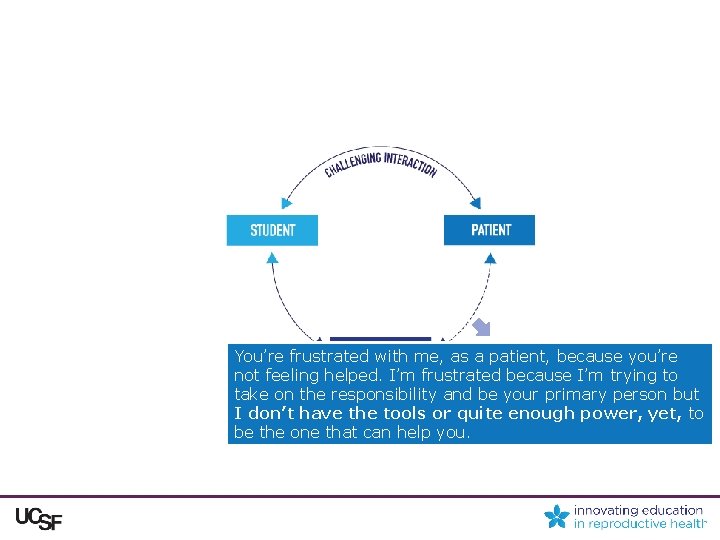
You’re frustrated with me, as a patient, because you’re not feeling helped. I’m frustrated because I’m trying to take on the responsibility and be your primary person but I don’t have the tools or quite enough power, yet, to be the one that can help you.
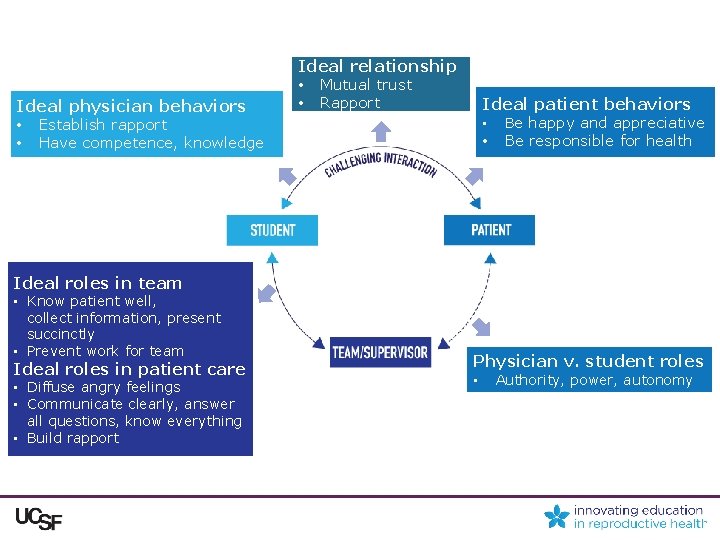
Ideal physician behaviors • Establish rapport • Have competence, knowledge Ideal relationship • Mutual trust • Rapport Ideal patient behaviors • • Be happy and appreciative Be responsible for health Ideal roles in team • Know patient well, collect information, present succinctly • Prevent work for team Ideal roles in patient care • Diffuse angry feelings • Communicate clearly, answer all questions, know everything • Build rapport Physician v. student roles • Authority, power, autonomy
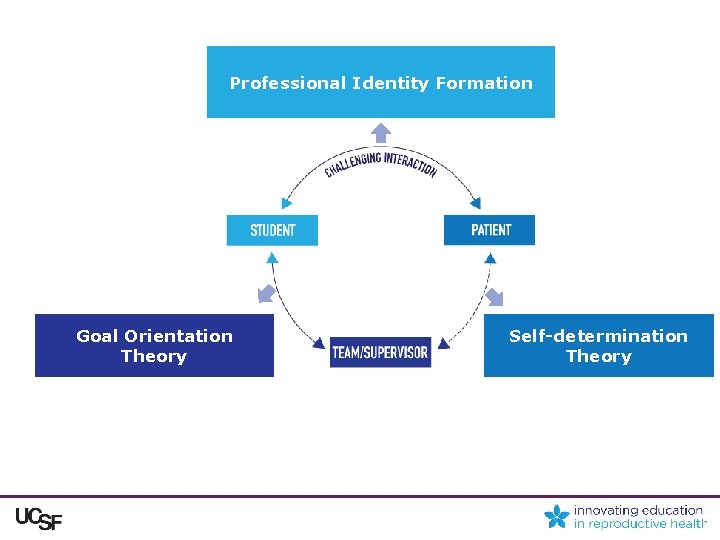
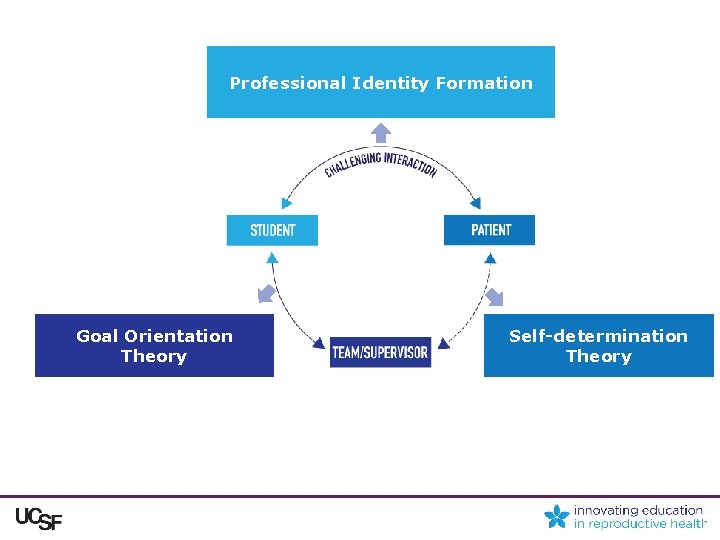
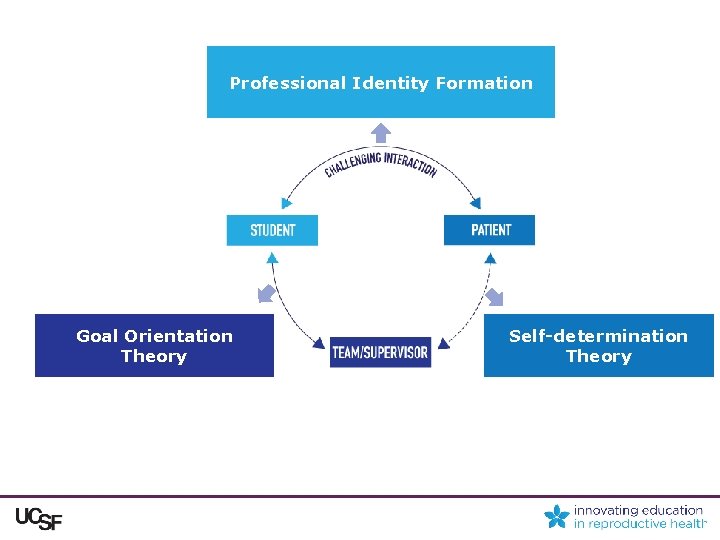
Professional Identity Formation Goal Orientation Theory Self-determination Theory

Discussion • Concerns about evaluation – Goal orientation theory 1 - performance orientation • Ideal notions of patients and physicians – Professional identity formation 2 -4 • Lack of competence, authority – Self-determination theory 5 -autonomy, competence, (relatedness) – Professional identity formation 2, 4 1. Pintrich, Contemp Educ Psychol, 2000; 2. Cruess, Acad Med, 2015; 3. Monrouxe, Med Ed, 2010; 4. Macleod, Adv Health Sci Ed, 2011; 5. Ten Cate, Med Teach, 2011.
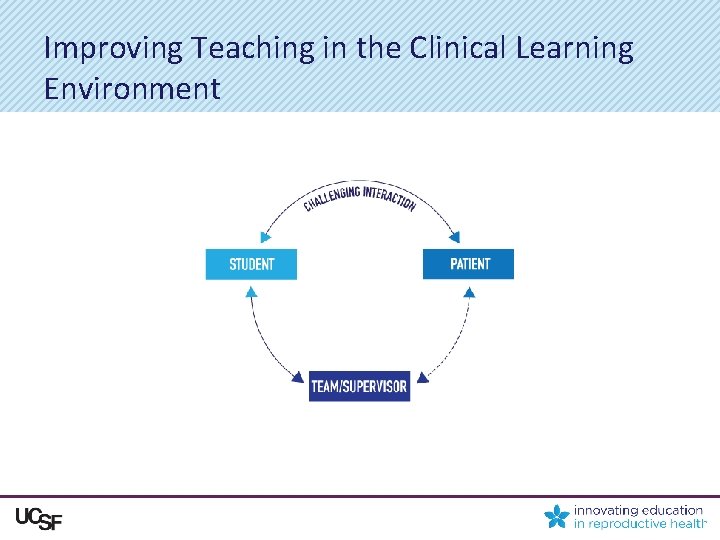
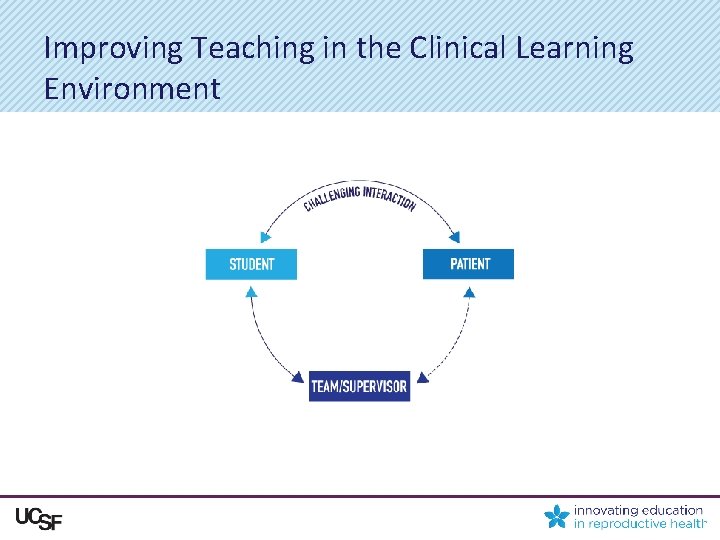
Improving Teaching in the Clinical Learning Environment
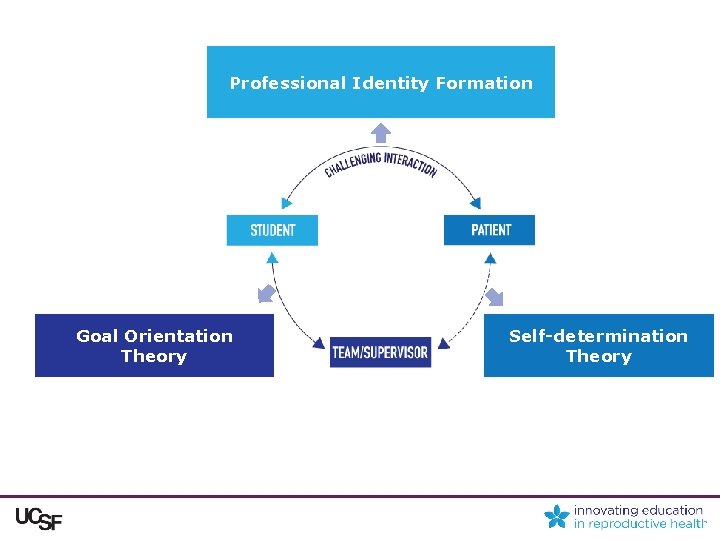
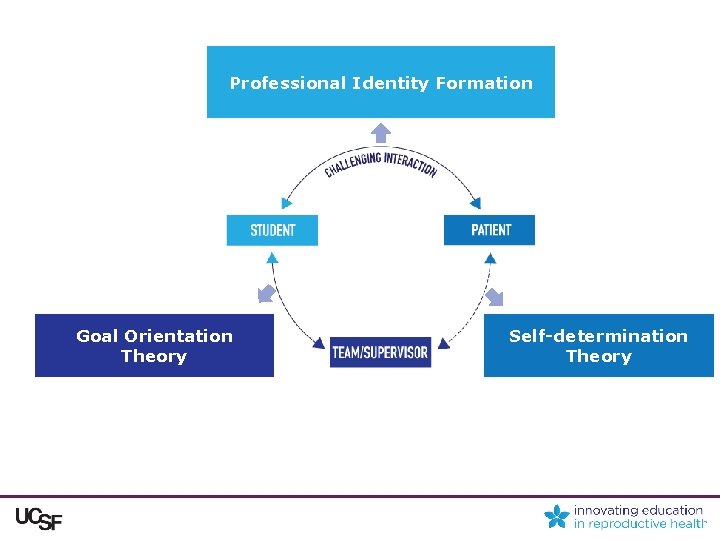
Professional Identity Formation Goal Orientation Theory Self-determination Theory
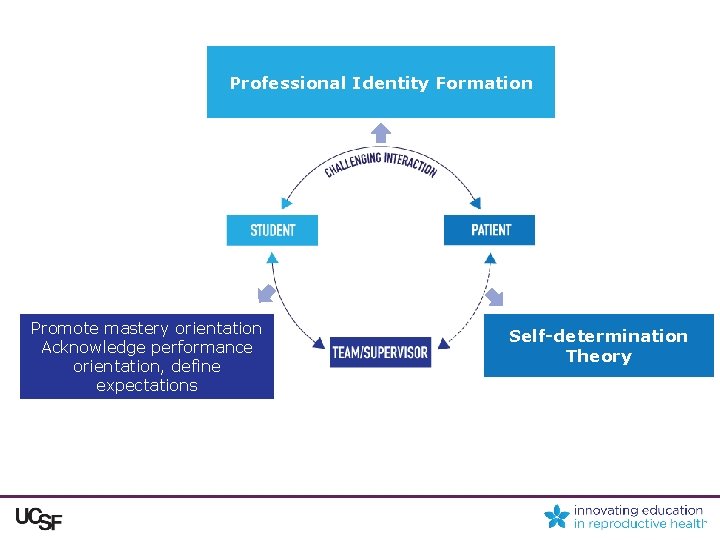
Professional Identity Formation Promote mastery orientation Acknowledge performance orientation, define expectations Self-determination Theory
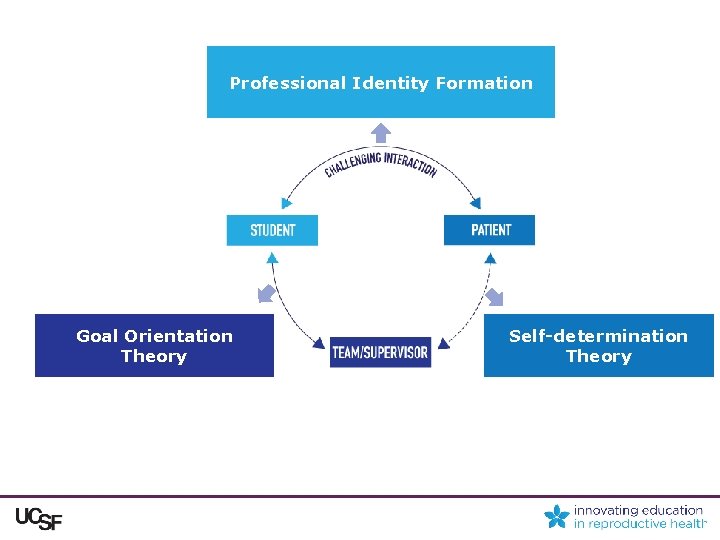
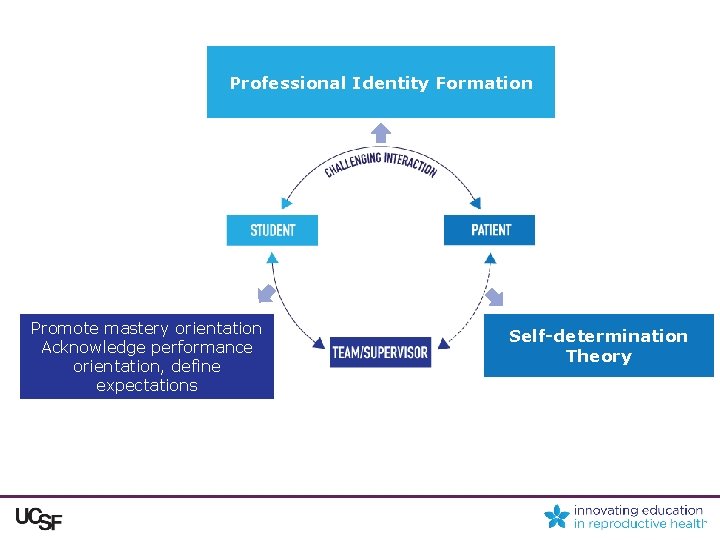
Professional Identity Formation Goal Orientation Theory Self-determination Theory

Support reflection about PIF Acknowledge and explore ideal notions about patients and interactions Goal Orientation Theory Self-determination Theory

Professional Identity Formation Goal Orientation Theory Self-determination Theory
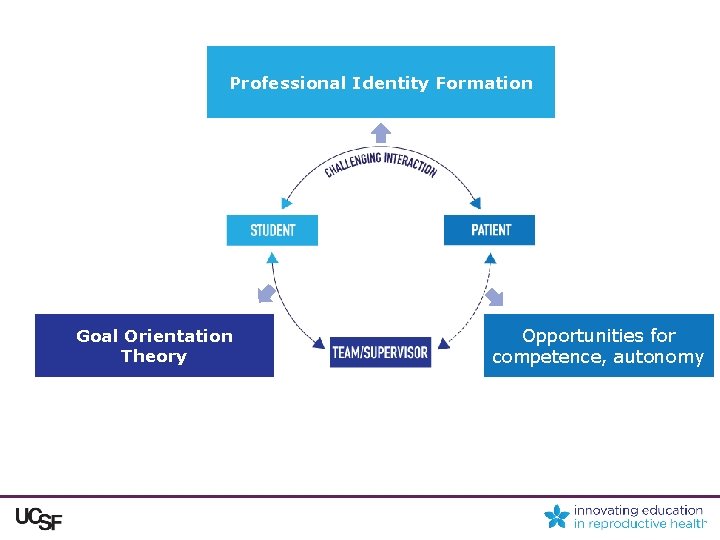
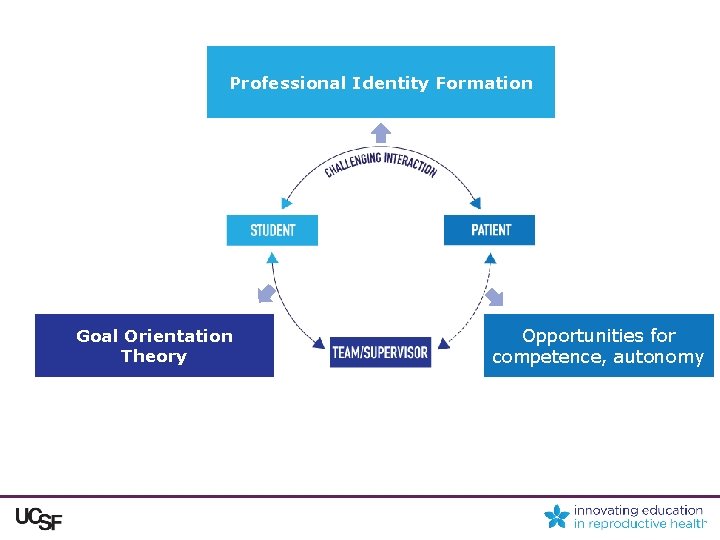
Professional Identity Formation Goal Orientation Theory Opportunities for competence, autonomy

Professional Identity Formation Goal Orientation Theory Self-determination Theory

Conclusion Students’ experiences of “difficult” patients interacted with their roles, identities and motivations as learners in complex ways. Clinical educators should consider these complexities as we teach medical students to provide high-quality care for patients whom might be considered “difficult. ”