What is this List salient features Case History


- Slides: 38

What is this ?
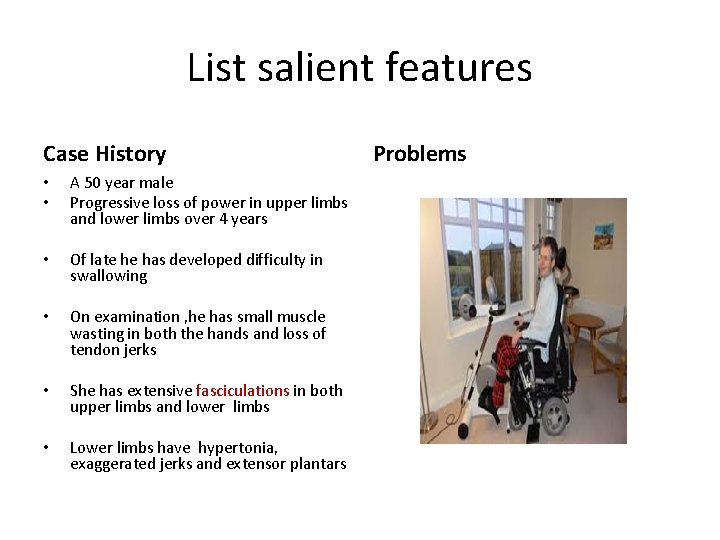
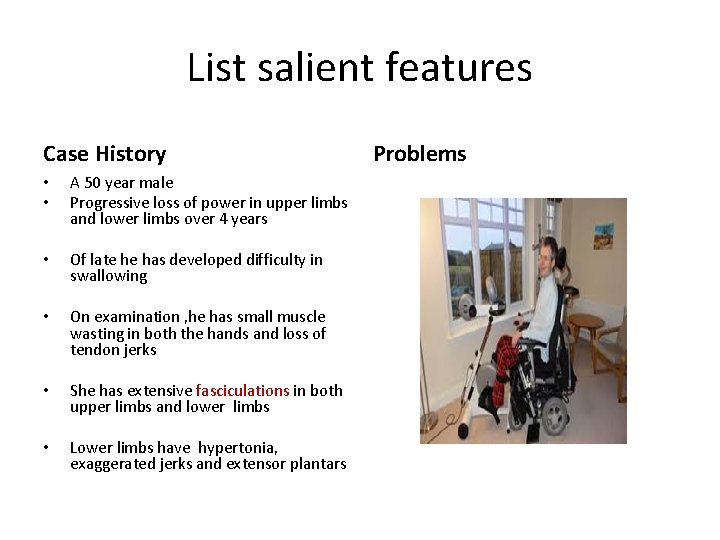
List salient features Case History • • A 50 year male Progressive loss of power in upper limbs and lower limbs over 4 years • Of late he has developed difficulty in swallowing • On examination , he has small muscle wasting in both the hands and loss of tendon jerks • She has extensive fasciculations in both upper limbs and lower limbs • Lower limbs have hypertonia, exaggerated jerks and extensor plantars Problems
Google image

List some causes of small muscle waiting
www. Google Images
Motor Neurone disease Dr Prabha Adhikari
15 minutes • • • What s motor Neurone disease Aetiology Clinical types Clinical features Prognosis Treatment
What is MND and Why • Disease of unknown cause -5/lakh • Degeneration of motor neurone , in the spinal cord, cranialnerve neuclei and pyramidal neurones cortex • 10%familaial • 20 % of them Gene superoxide desmutase 1 mutation • 95%-viral infections, trauma, electric shock , toxins
Clinical types • Progressive lateral sclerosis –Upper motor Neurone with wasting and fasciculation and exaggerated jerks • Progressive Muscular Atrophy-lower motor
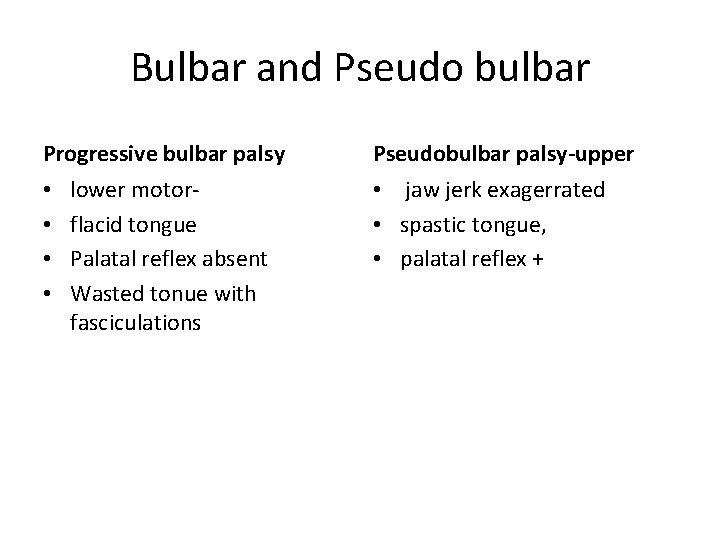
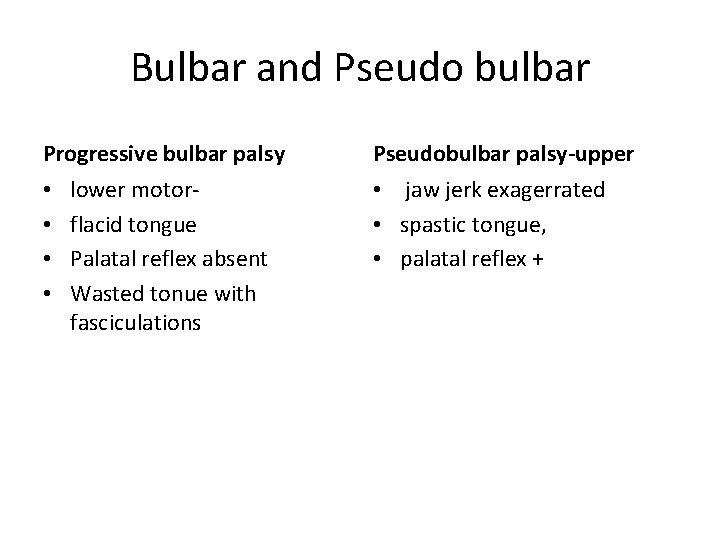
Bulbar and Pseudo bulbar Progressive bulbar palsy • • lower motorflacid tongue Palatal reflex absent Wasted tonue with fasciculations Pseudobulbar palsy-upper • jaw jerk exagerrated • spastic tongue, • palatal reflex +
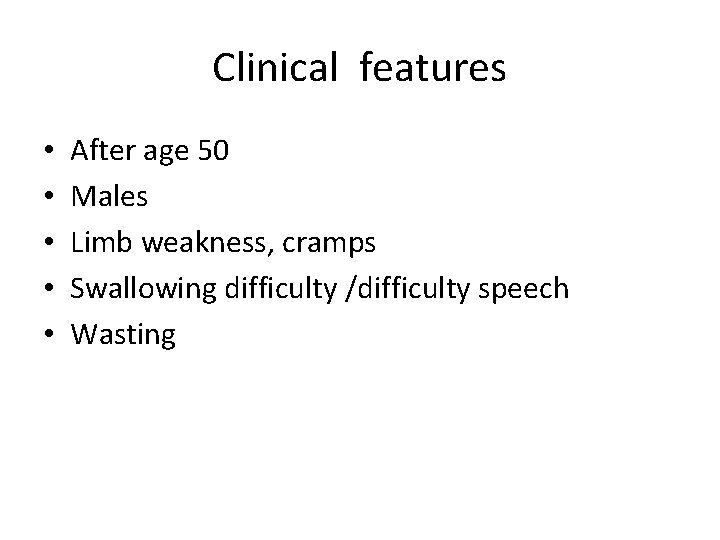
Clinical features • • • After age 50 Males Limb weakness, cramps Swallowing difficulty /difficulty speech Wasting
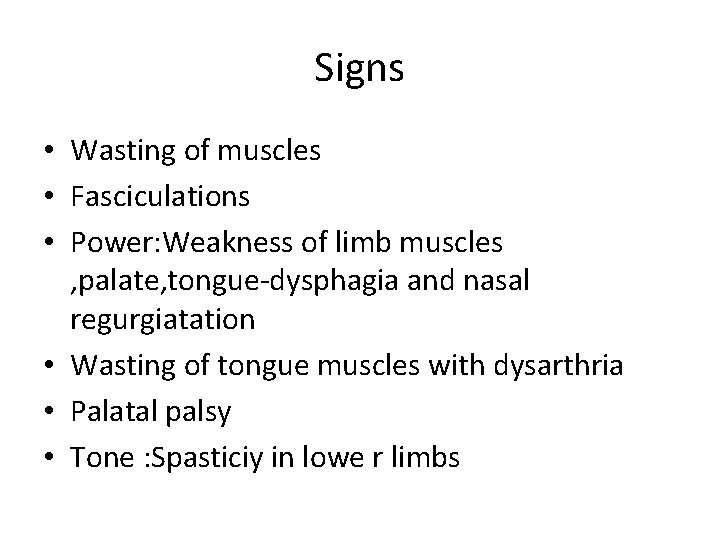
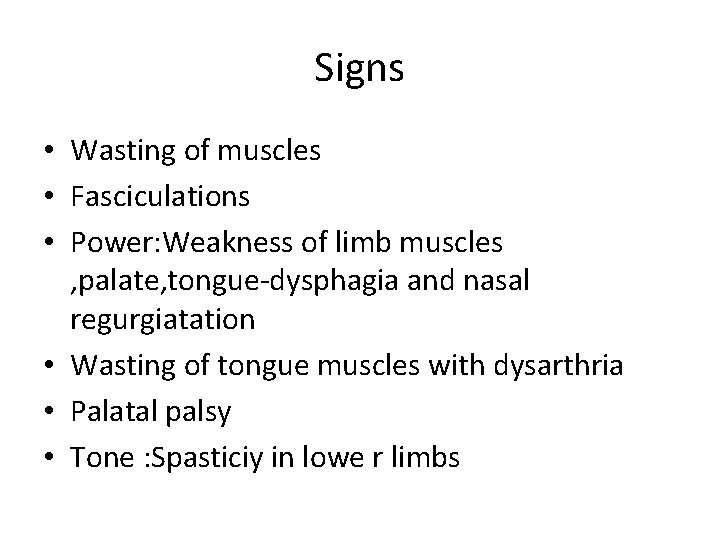
Signs • Wasting of muscles • Fasciculations • Power: Weakness of limb muscles , palate, tongue-dysphagia and nasal regurgiatation • Wasting of tongue muscles with dysarthria • Palatal palsy • Tone : Spasticiy in lowe r limbs
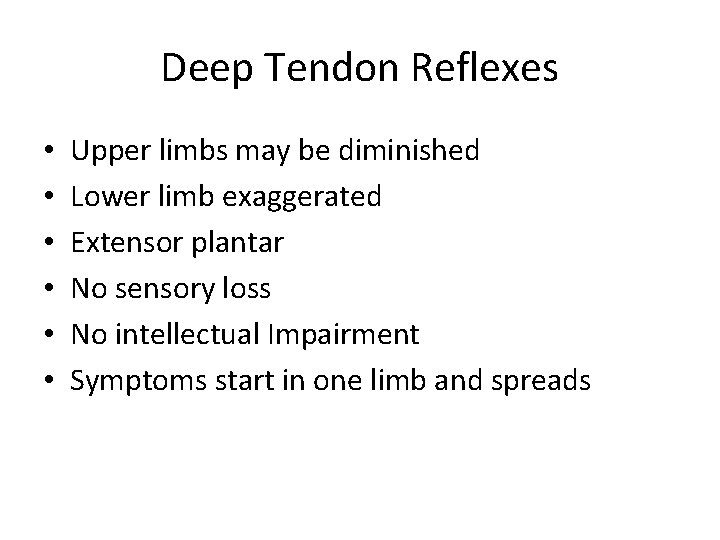
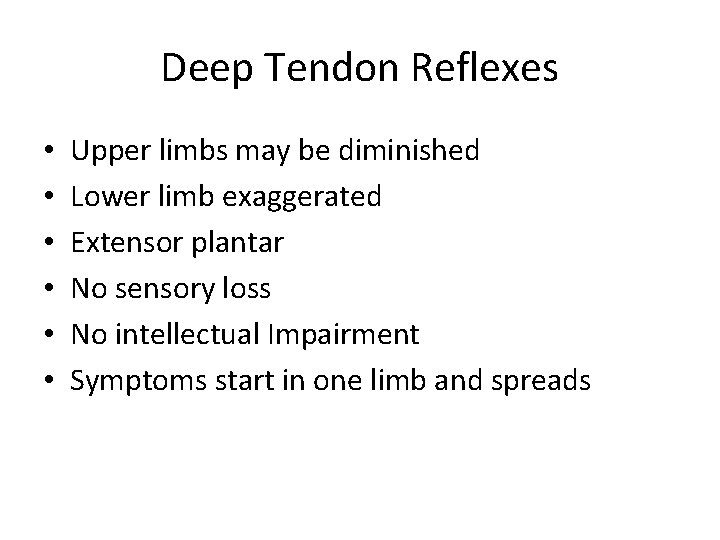
Deep Tendon Reflexes • • • Upper limbs may be diminished Lower limb exaggerated Extensor plantar No sensory loss No intellectual Impairment Symptoms start in one limb and spreads
DDInvestigations &Treatment • Differential • Diabetic amyotrophy • Spinal cord compression • Multifocal motor neuronopathy • Poliomyelitis NCV and EMG Fasciculations and fibrillation Deneravtion potential , reduced action potential
Glutamate antagonist • Riluzole 100 mg per day–prolongs life by 2 months • Nerve growth factors • Palliative care • Mechanical aids, communication aids • NIV • Feeding gastrostomy
MCQs 1. Motor Neurone disease has all the following features EXCEPT a. Lower motorneurone signs b. Sensory loss c. Upper motor neurone signs d. Dysphagiaand dysarthria
Question 2 • The most important diagnostic clinical feature of MND is • A. Exaggerated jerks • B. wasted muscles • C. dysphagia • D. Fasciculations extensive
Drug for MND • • A. Donepezil B. Riluzole C. Memantine D. Galatamine
Infections of the nervous system • A 28 year old male presents with high grade fever , head ache , projectile vomiting of 3 days after which he is comatose • Discuss with your neighbour for 5 minutes as to how you will examine such a patient
Lesson Plan • Solve the case • List organisms that can lead to bacterial meningitis and antibiotic choices • Describe clinical features and do three tests • Describe CSF findings • List CSF tests • List complications • List late complications
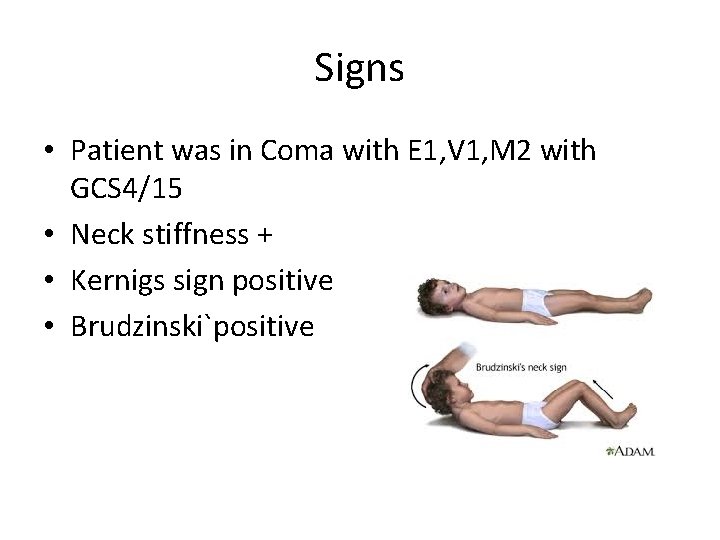
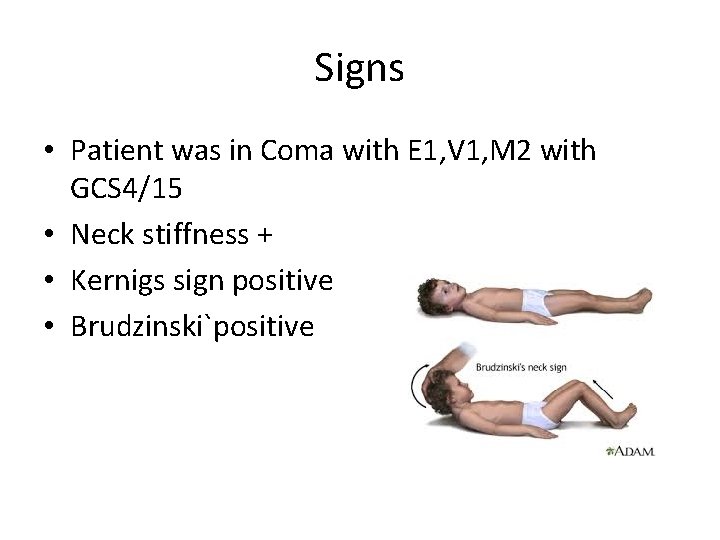
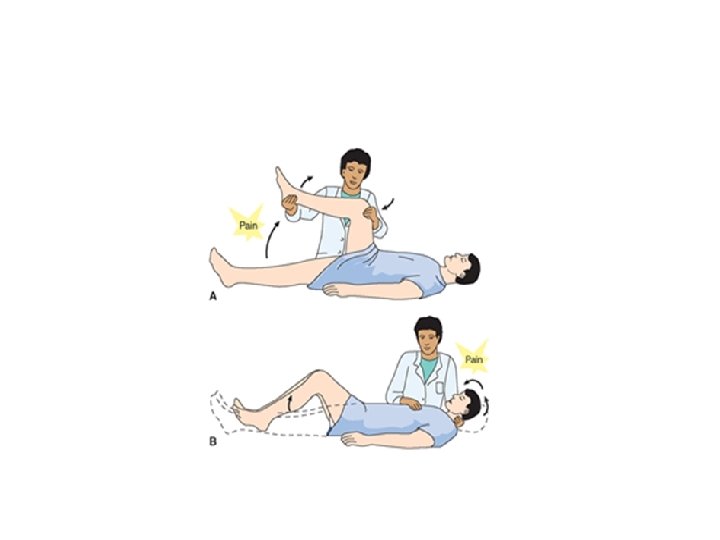
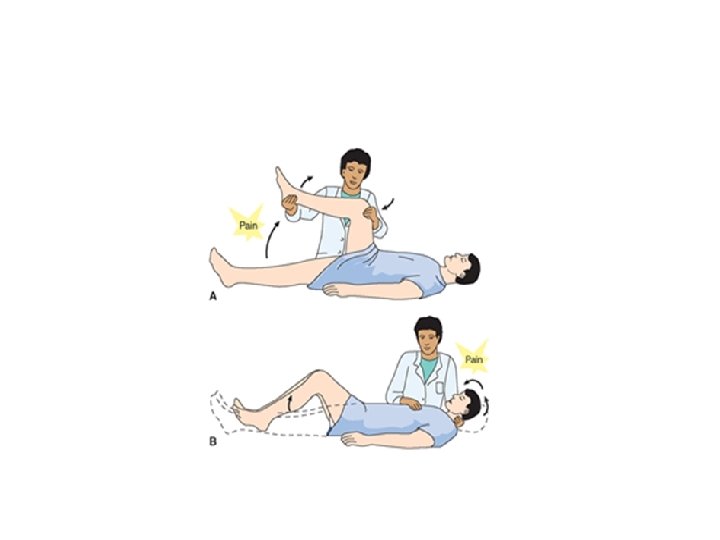
Signs • Patient was in Coma with E 1, V 1, M 2 with GCS 4/15 • Neck stiffness + • Kernigs sign positive • Brudzinski`positive
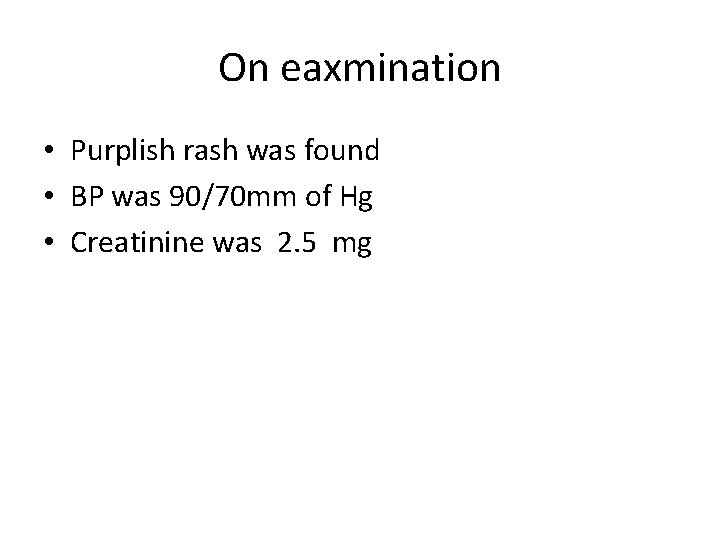
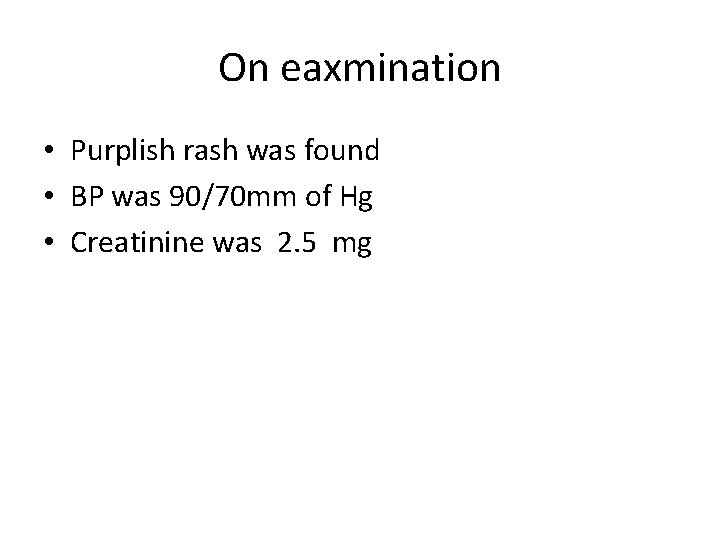
On eaxmination • Purplish rash was found • BP was 90/70 mm of Hg • Creatinine was 2. 5 mg
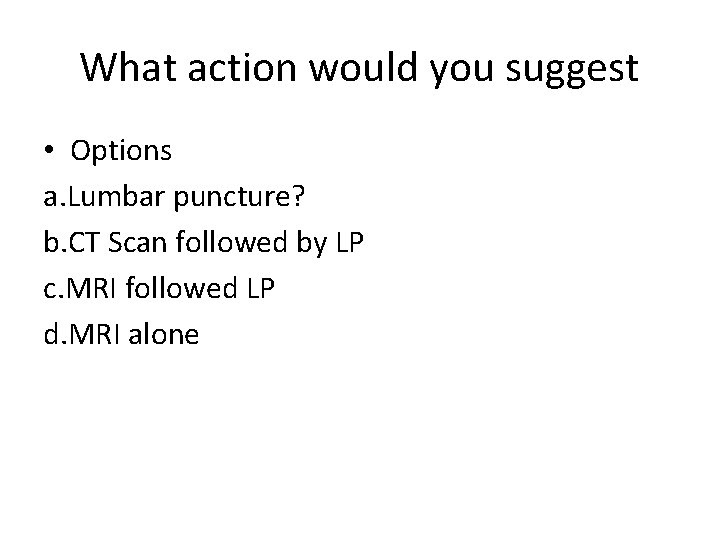
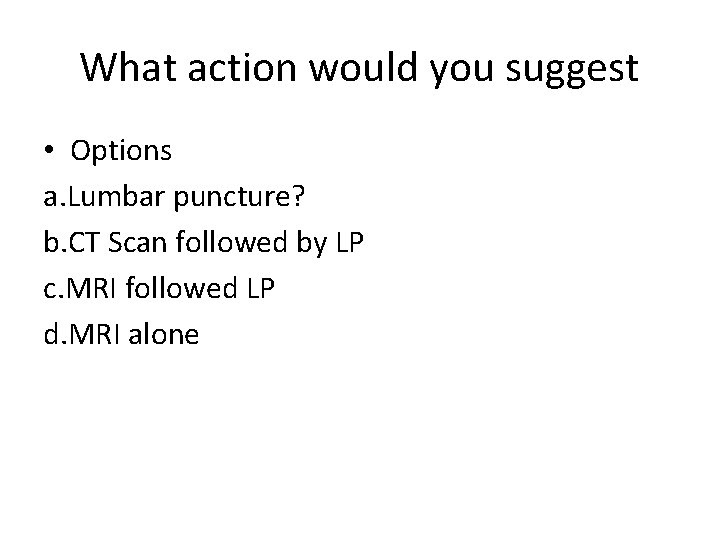
What action would you suggest • Options a. Lumbar puncture? b. CT Scan followed by LP c. MRI followed LP d. MRI alone
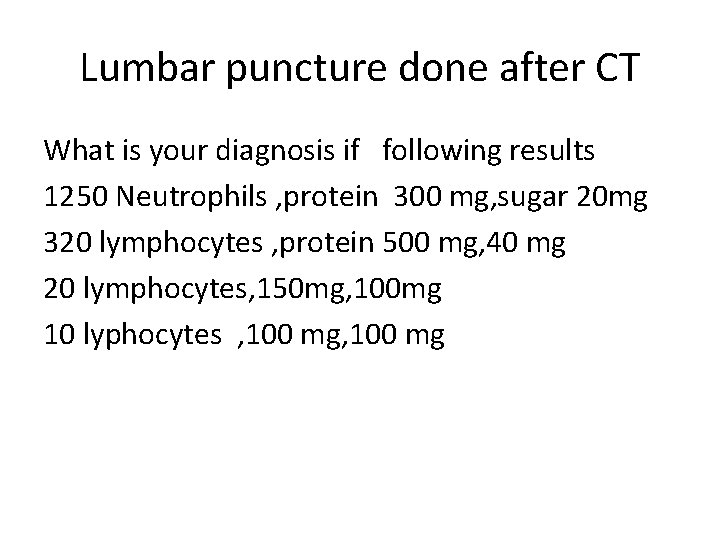
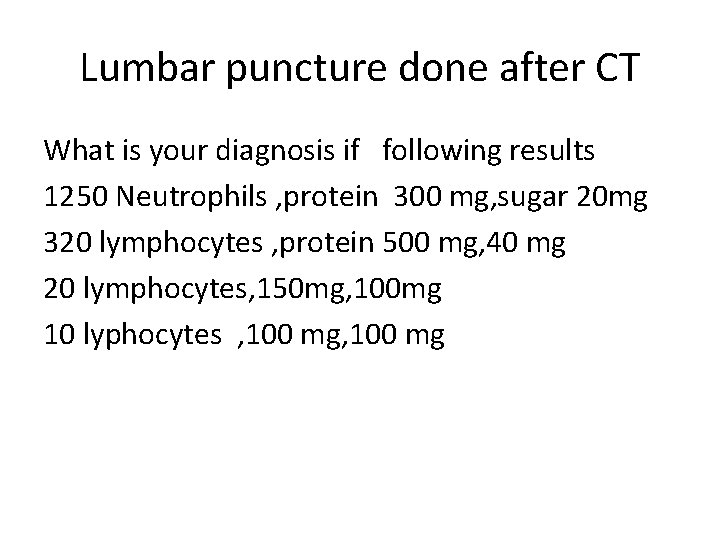
Lumbar puncture done after CT What is your diagnosis if following results 1250 Neutrophils , protein 300 mg, sugar 20 mg 320 lymphocytes , protein 500 mg, 40 mg 20 lymphocytes, 150 mg, 100 mg 10 lyphocytes , 100 mg
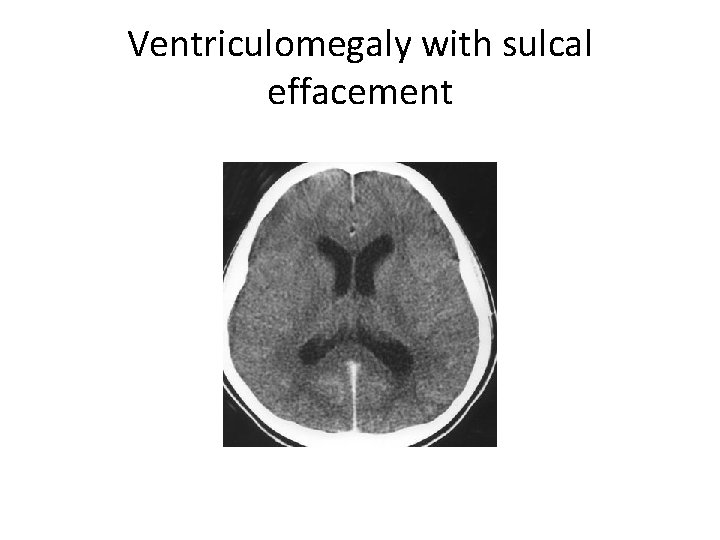
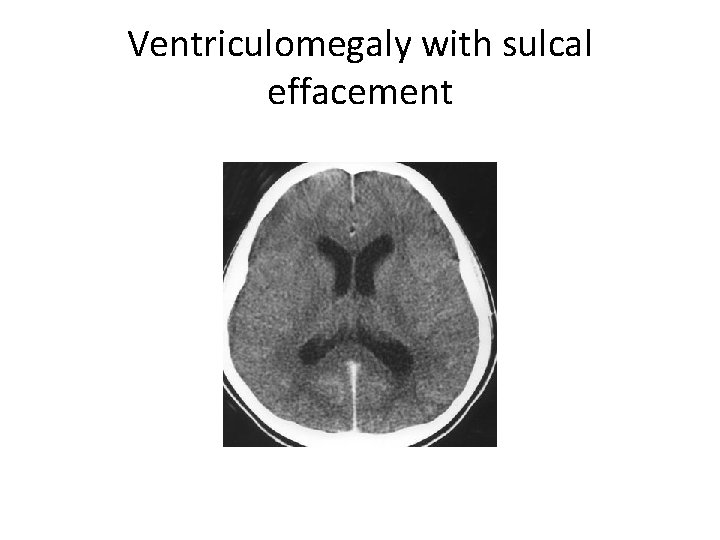
Ventriculomegaly with sulcal effacement
Treatment recommended • • Ceftrioxone 2 G IV BD Benzyl Penicillin 20 Lalks 6 th hourly IV Ampicillin 2 G IV 4 th hourly Chromaphenicol 1. G IV 6 th hourly with Vancomycin I GIV twice aday
Meninigitis with rash • Hypotension : Waterhouse Friedrickson syndrome • Benzyl Penicillin and corticosteroids
Meningitis without rash 18 -50 • Ceftrioxone 2 G IV BD • Sterp Penumoniae resistant to Penicillin • Vancomycin I G IV Bdor Rifamipicin 600 mg
>50 years • • Alocoholic, diabetic , immunosuppression and Brain stemsigns Listeria Monocytogenes Ampicillin 2 G IV 4 th hourly
Complications • • • Shock Waterhouse Friedricksons syndrome Sepsis DIC Renalfailure Peripheral. Gangrene Arthrits Pericarditis Coning ARDS
Sequale • Deafness
Anaphylaxis to betalactum • Chloramphenicol 1 G IV 6 th hourly • Vancomycin 1 G IV BD
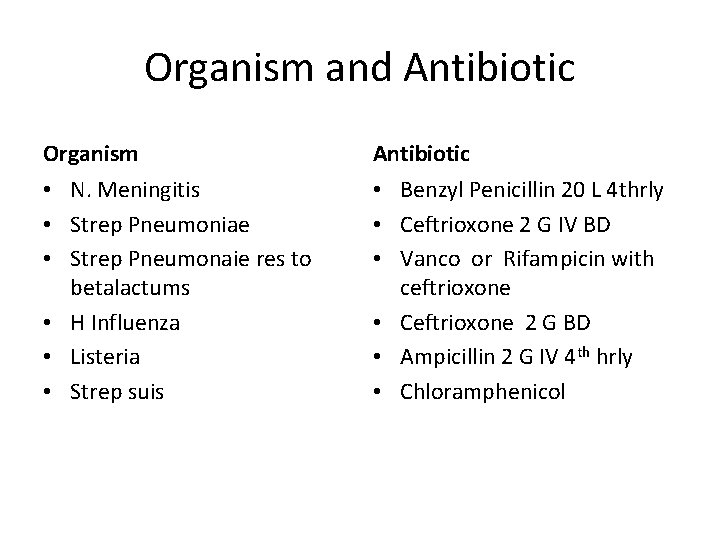
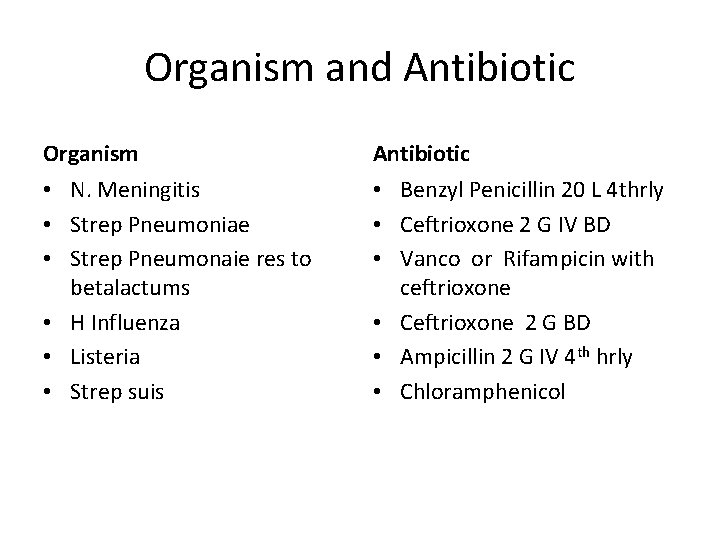
Organism and Antibiotic Organism Antibiotic • N. Meningitis • Strep Pneumoniae • Strep Pneumonaie res to betalactums • H Influenza • Listeria • Strep suis • Benzyl Penicillin 20 L 4 thrly • Ceftrioxone 2 G IV BD • Vanco or Rifampicin with ceftrioxone • Ceftrioxone 2 G BD • Ampicillin 2 G IV 4 th hrly • Chloramphenicol
Adjunctive steroids • • Dexa methsone prevents deafness 8 mg 6 th hourly or 8 th hourly Decreases raised ICT Improves head ache
Prevention • Oral Rifampicin 600 mg BD or Ciprofloxacin 500 mg for adult contacts and all children • Vaccines for Group and A and C
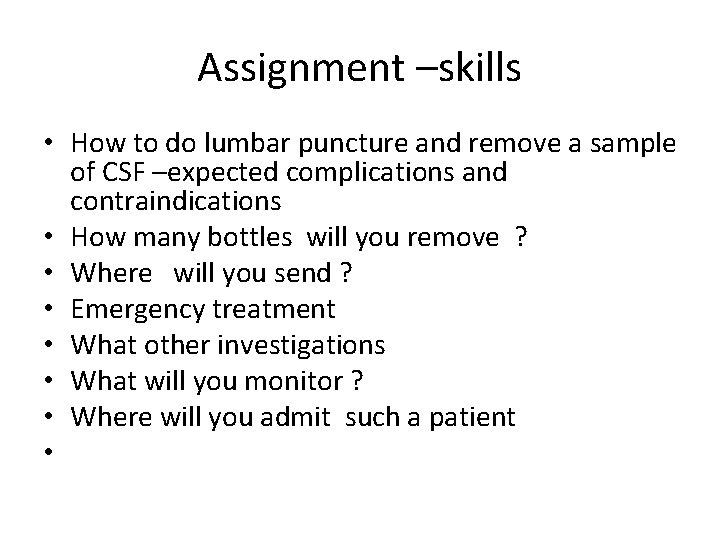
Assignment –skills • How to do lumbar puncture and remove a sample of CSF –expected complications and contraindications • How many bottles will you remove ? • Where will you send ? • Emergency treatment • What other investigations • What will you monitor ? • Where will you admit such a patient •