Transition to Registered Nursing Putting It All Together
- Slides: 32
Transition to Registered Nursing Putting It All Together West Coast University Week 6 6 -1
Review and Application of the Nursing Process 2
The Nursing Process Group at West Coast University: Working together in the quest of human response Hi, I’m Ns. Diagnosis ¡Hola!, I’m Ns. Planning Hey, I’m Ns. Implementation with Scientific Rationale I’m Ns. Assessment Yo, I’m Ns. FHP Dude, it’s me, Ns. Evaluation 3
Nursing Process • • • Cyclic Ongoing Client centered Promotes organization Promotes problem resolution 4
Step One: Assessment • • • Data collection Verification and validation Organization of data Data interpretation Database is formed 5
Types of Data • Subjective – feelings, perceptions, concerns • Objective – observable – measurable – felt by others 6
Recording Assessment Data • Tools with a purpose • Holistic data collection 7
Data Clustering • Relatedness • Patterns • Support facts 8
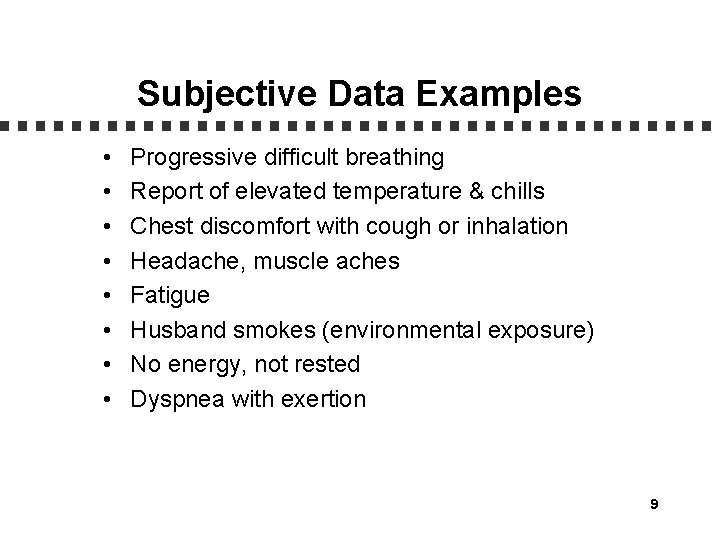
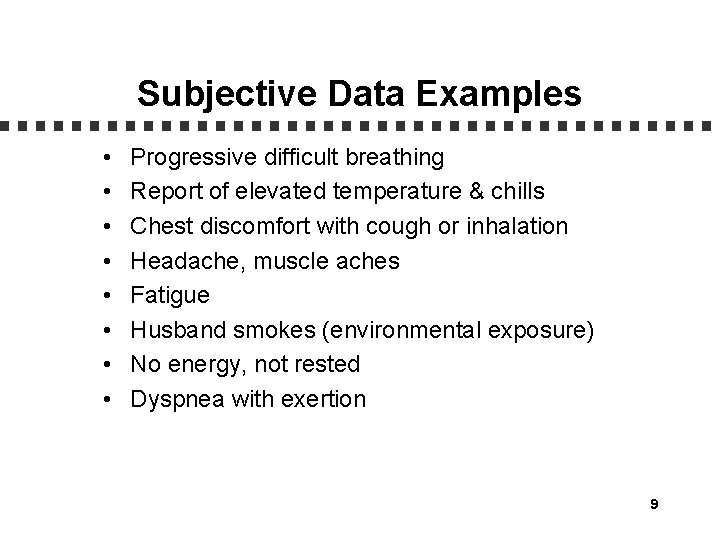
Subjective Data Examples • • Progressive difficult breathing Report of elevated temperature & chills Chest discomfort with cough or inhalation Headache, muscle aches Fatigue Husband smokes (environmental exposure) No energy, not rested Dyspnea with exertion 9
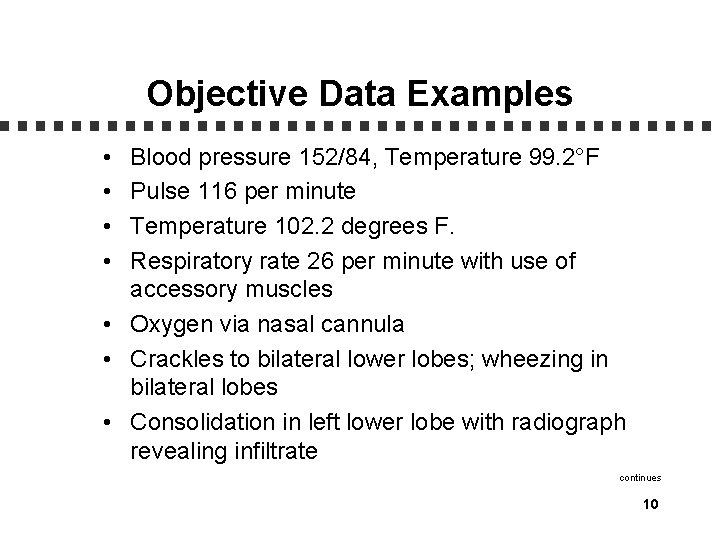
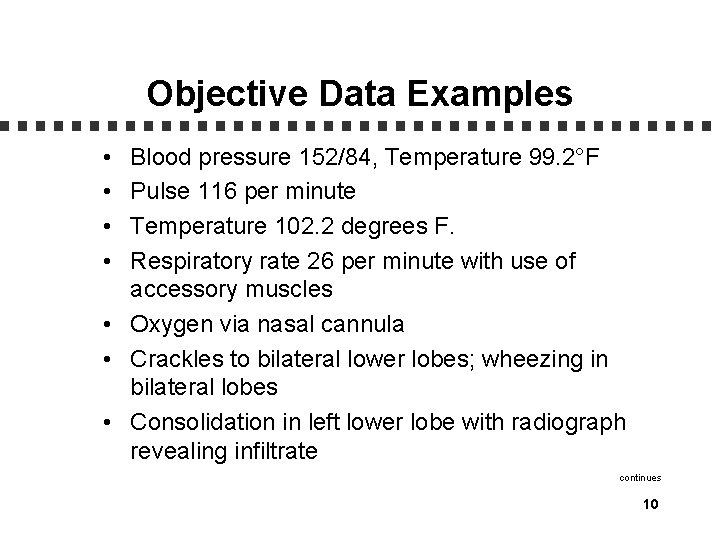
Objective Data Examples • • Blood pressure 152/84, Temperature 99. 2°F Pulse 116 per minute Temperature 102. 2 degrees F. Respiratory rate 26 per minute with use of accessory muscles • Oxygen via nasal cannula • Crackles to bilateral lower lobes; wheezing in bilateral lobes • Consolidation in left lower lobe with radiograph revealing infiltrate continues 10
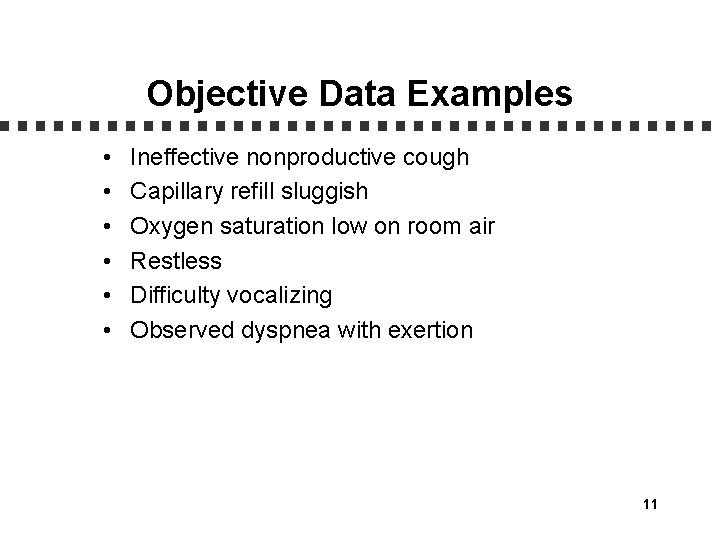
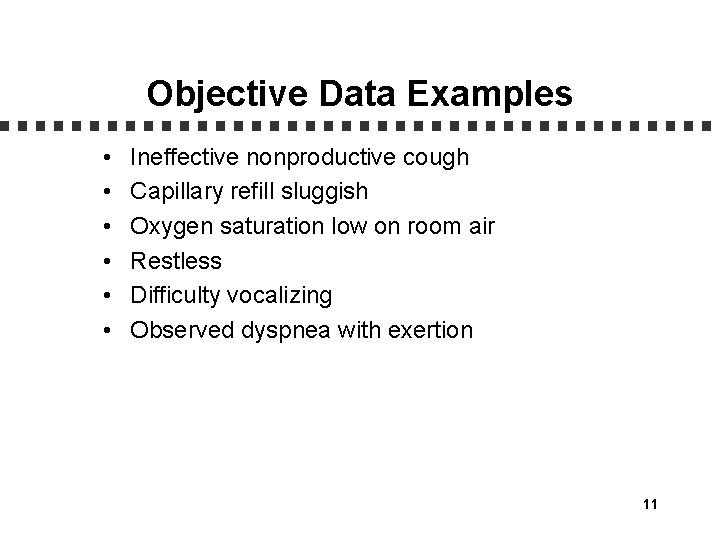
Objective Data Examples • • • Ineffective nonproductive cough Capillary refill sluggish Oxygen saturation low on room air Restless Difficulty vocalizing Observed dyspnea with exertion 11
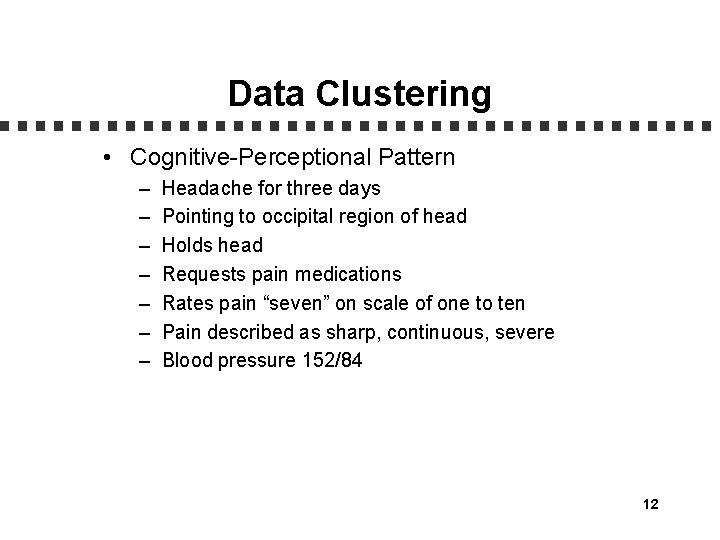
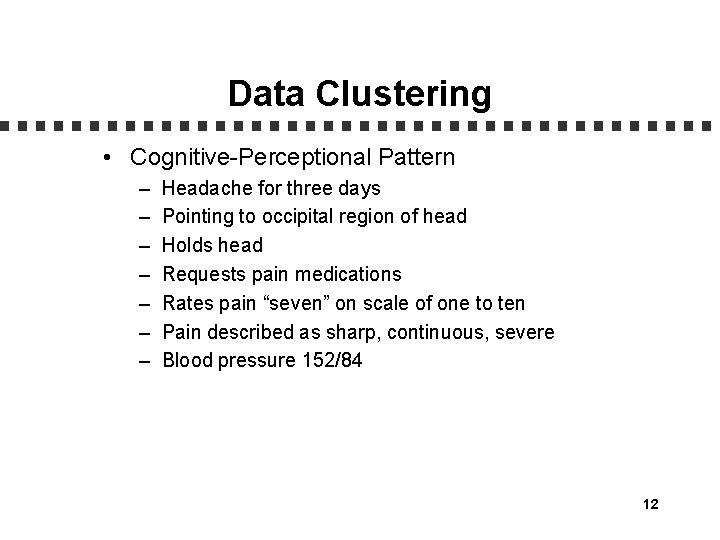
Data Clustering • Cognitive-Perceptional Pattern – – – – Headache for three days Pointing to occipital region of head Holds head Requests pain medications Rates pain “seven” on scale of one to ten Pain described as sharp, continuous, severe Blood pressure 152/84 12
Data Clustering • Activity-Exercise Pattern – Reports mild difficulty breathing – Oxygen two liters via nasal cannula – Skin color dull, pale pink-yellow undertones, capillary refill greater than two seconds – Decreased pulse in left foot – Cold extremities – Requires assistance with transfer – Left hand, left leg weakness – Reports, “Can’t move my leg and hand” 13
Data Clustering • Nutritional Metabolic Pattern – – Corner of mouth droops Difficulty pronouncing words Has not eaten since symptoms began Nausea 14
Step Two: Diagnosis • Problems identified • Potential problems identified • Diagnostic labels determined 15
Step Three: Planning • • Identify priorities Determine realistic goals and expected outcomes Determine interventions and rationale Communicate and document 16
Priorities • • Data may determine Discovered during interview, assessment Client’s preference Consider Maslow’s hierarchy 17
Goals and Expected Outcomes • • Unique to client Give direction to plan Focus on etiology Indicate intent or desired change 18
Planning Components • • • Subject Behavior Criteria of performance Time frame Condition 19
Step Four: Implementation • • Begins with assessment Assessment is ongoing Execute the care plan Has independent nursing function 20
Scientific Rationale • Scientific principles • Underlying reason • Utilizing resources 21
Acute Pain • Nursing Interventions + Scientific Rationales – Intervention • Encourage client to report pain/discomfort location, intensity, duration, etc. using the pain scale. Obtain an exact description. – Scientific Rationale • Changes in pain description may indicate a change in the client’s condition. 22
Acute Pain • Nursing Interventions + Scientific Rationales – Nursing Interventions • Administer smallest narcotic analgesic dose possible to aid in comfort, as per physician order. – Scientific Rationales • Narcotic analgesics affect the level of consciousness and may interfere with neurological assessment. 23
Mobility, Impaired Physical • Nursing Interventions + Scientific Rationales – Nursing Interventions • Monitor and screen client for mobility skills and activities. – Scientific Rationales • Screening and monitoring the client aids in identifying the level of impairment and provides a baseline of mobility abilities. Interventions may be planned appropriately. 24
Mobility, Impaired Physical • Nursing Interventions + Scientific Rationales – Nursing Interventions • Consult with physical therapy for further evaluation and development of a mobility plan. – Scientific Rationales • Allows staff to integrate collaborative plan, which will enhance and maximize client’s mobility. 25
Mobility, Impaired Physical • Nursing Interventions + Scientific Rationales – Nursing Interventions • Perform passive range of motion to weakened extremities at least twice daily. Encourage active range of motion and assist when needed. – Scientific Rationales • Strengthens muscles and prevents atrophy of muscle tissue. 26
Tissue Perfusion, Altered (cerebral/peripheral) • Nursing Interventions + Scientific Rationales – Nursing Interventions • Monitor dorsalis pedis and posterior tibial pulses bilaterally for equality and rate. – Scientific Rationales • Diminished or absent peripheral pulses insufficiency. indicate arterial 27
Tissue Perfusion, Altered (cerebral/peripheral) • Nursing Interventions + Scientific Rationales – Nursing Interventions • Monitor for change in neurological status. Use neurological flow sheets to record results of neurological assessments. – Scientific Rationales • Any change may indicate that the brain is deprived of adequate amount of oxygen due to further bleeding, increased intracranial pressure, or spasm of cerebral artery. 28
Tissue Perfusion, Altered (cerebral/peripheral) • Nursing Interventions + Scientific Rationales – Nursing Interventions • Maintain extremities in dependent position and maintain physical rest. – Scientific Rationales • To facilitate arterial blood flow through vessel narrowed by a thrombus. 29
Step Five: Evaluation • • • To measure effectiveness of plan To determine appropriateness of plan Focus on changes in client’s health status Progress toward goal attainment Document: – Goal met – Goal not met – Goal partially met • AEB (statement based on planning) 30
Revision, Modification, Discontinuation • Progress • Lack of progress 31
Assignment • Reading: – Duncan & De. Pew: Chapter 6, 7 • Topic: – Patient Education and Therapeutic Communication 32