Transfer of The Critically Ill Patient Dr Ferenc


- Slides: 20
Transfer of The Critically Ill Patient Dr Ferenc Kovari M. D. Consultant in Anesthesia and Intensive Care 2016
Transfer of the critically ill patient • • Equipment Accompanying Personnel Preparation for Transport Monitoring During Transport Management During Transport Documentation Supplementary Equipment For Use During Transport Is The Patient Stable For Transport?
Equipment • As much of the equipment as possible should be mounted at or below the level of the patient. In particular, large arrays of vertical drip stands should be avoided. This allows unhindered access to the patient and improves stability of the patient’s bed. • Ideally all equipment within a transport should be standardized to enable the seamless transfer of patients without, for example, interruption of drug therapy or monitoring due to incompatibility of leads and transducers.
Equipment • All equipment should be robust, durable and lightweight. Electrical equipment must be designed to function on battery when not plugged into the mains. • Portable monitors should have a clear illuminated display and be capable of displaying ECG, arterial oxygen saturation, non-invasive and invasive blood pressure monitoring, capnography and temperature. • Alarms should be visible as well as audible.
Equipment-Trolley • • • Portable monitor-Fukuda DS 7100 (able to provide ECG, non invasive blood pressure, two invasive pressures, oxygen saturations, respiratory rate, temperature) Portable ventilator-Oxylog 3000 (capable of supplying positive end expiratory pressure (PEEP), variable oxygen concentrations, inspiratory / expiratory ratio, respiratory rate, and tidal volume). The ventilator will have disconnection and high pressure alarms End tidal carbon dioxide monitor Syringe drivers Infusion pumps

Equipment
Equipment- Transfer bag: • Essential drugs – Resuscitation drugs, sedatives (Drugs requiring fridge storage e. g. Atracurium and Suxamethonium must be collected from the fridge in A&E or ICU) • Airway and ventilation adjuncts • Suction equipment including Yankauer, catheters and nasogastric tubes • Equipment to gain and secure intravenous access and maintain circulation • High visibility jacket and a list of contact numbers.

Equipment- Transfer bag
Accompanying Personnel • The critically ill patient should be accompanied by a minimum of two attendants. • One attendant should be a medical practitioner with appropriate training in intensive care medicine, anesthesia, or other acute specialty. • He or she should be competent in resuscitation, airway care, ventilation and other organ support. • The responsible medical practitioner should be accompanied by another suitably experienced nurse, and or technician.
Preparation For Transport • Prior to departure, transport attendant must familiarize himself with treatment already undertaken and independently assess the patient’s condition. • In all cases, full clinical details must be obtained, for example, (vent settings, all current meds, latest ABG, CBC, Metabolic panel, CXR) before leaving the unit or OR. • Meticulous resuscitation and stabilization of the patient before transport is the key to avoiding complications during the journey.
Preparation For Transport • The airway should be assessed and if necessary secured and protected. • Intubated patients should normally be paralyzed and sedated. • If a PTX is present or likely, chest drains should be inserted prior to departure. • Secure venous access is mandatory and at least two wide bore IV cannulae are required. An arterial line is ideal for BP monitoring.
Preparation For Transport • Hypovolemic patients tolerate moving poorly and circulating volume should be near normal prior to transport. This may require loading with crystalloid, colloid or blood. If inotropes or other vasoactive agents are required to optimize hemodynamic status, patients should be stabilized on these before leaving the unit. • Patients who are persistently hypotensive despite resuscitation efforts should not be moved until stable. Continuing sources of blood loss or sepsis should be identified and controlled.
Monitoring During Transport • The standard of care and monitoring during transport should be at least as good as it is in the unit. • Minimum standards required for all patients are appropriate staff, ECG, BP monitoring and arterial oxygen saturation. • ICP monitoring may be required in certain patients. • A written record of pt status, monitored values, treatment given and any other clinically relevant information should be completed after transfer.
Management During Transport • All equipment must be securely stowed. Under no circumstances should equipment (e. g. infusion pump) be left on top of the patient. Gas cylinders must properly be placed at the foot of the bed or if necessary, under the bed. • Monitoring must be continuous throughout the transport. All monitors and pumps should be visible to accompanying staff. • Adequately resuscitated and stabilized patients should not normally require dramatic changes to treatment during transport.
Documentation • Clear records must be maintained of all stages. These should include details of the patients condition prior to and after transport, details of vital signs, clinical events and therapy given during transport. • FILLING OUT the TRANSFER AUDIT form is COMPULSORY and is the sole responsibility of the doctor on transfer. Please leave one photocopy at the receiving unit and bring back the original one and put it in to the transfer audit box situated at the nursing station in the ITU.
Is The Patient Stable For Transport • Airway – Airway safe or secured by intubation – Tracheal tube position confirmed on CXR • Ventilation – Paralyzed, sedated and ventilated – Adequate gas exchange confirmed by ABG
Is The Patient Stable For Transport • Circulation – HR, BP stable – Tissue and organ perfusion adequate – Any obvious blood loss controlled – Circulating blood volume restored – Hb adequate – Minimum of 2 routes of venous access • Neurology – Seizures controlled, metabolic causes excluded – Raised ICP appropriately managed
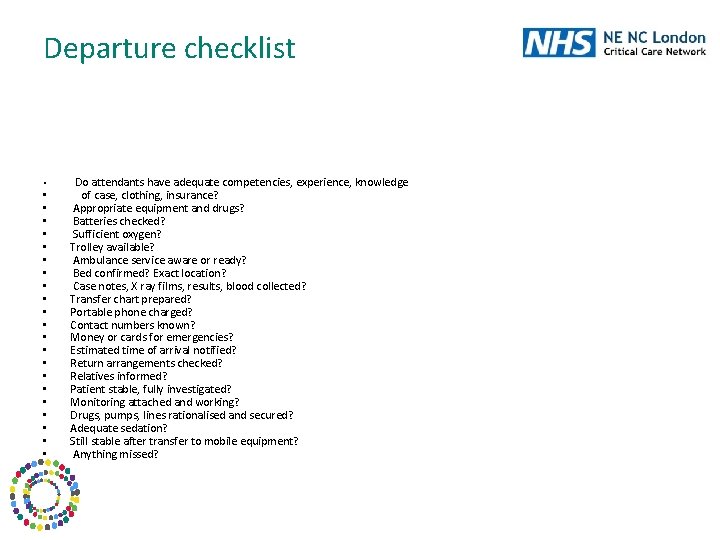
Departure checklist • • • • • • Do attendants have adequate competencies, experience, knowledge of case, clothing, insurance? Appropriate equipment and drugs? Batteries checked? Sufficient oxygen? Trolley available? Ambulance service aware or ready? Bed confirmed? Exact location? Case notes, X ray films, results, blood collected? Transfer chart prepared? Portable phone charged? Contact numbers known? Money or cards for emergencies? Estimated time of arrival notified? Return arrangements checked? Relatives informed? Patient stable, fully investigated? Monitoring attached and working? Drugs, pumps, lines rationalised and secured? Adequate sedation? Still stable after transfer to mobile equipment? Anything missed?
Trauma Patient – C-spine protected – PTX drained – Long bone/pelvic fractures stabilized – Intra-thoracic and intraabdominal bleeding controlled
References • Policy and Guidelines for the intra and inter hospital transfer of Patients • Guidelines for the transport of the critically ill adult. 2002. London, The Intensive Care Society
 Care of the critically ill surgical patient
Care of the critically ill surgical patient Surgical metabolism
Surgical metabolism Patient 2 patient
Patient 2 patient Thinking critically with psychological science answer key
Thinking critically with psychological science answer key Thinking critically with psychological science
Thinking critically with psychological science Critical thinking example in nursing
Critical thinking example in nursing Listening critically
Listening critically Aseptic field
Aseptic field Shakespeare sonnet 27 translation
Shakespeare sonnet 27 translation Thinking critically with psychological science
Thinking critically with psychological science Thinking critically
Thinking critically Negative issues
Negative issues Critically appraised topic voorbeeld
Critically appraised topic voorbeeld Thinking critically
Thinking critically Critically thoughful
Critically thoughful Www.antt
Www.antt Unit 16 the patient's mobility transfer skills
Unit 16 the patient's mobility transfer skills Vadkerti ferenc
Vadkerti ferenc Impulzus megmaradásának tétele
Impulzus megmaradásának tétele Janka ferenc
Janka ferenc Hőfokvezetési tényező
Hőfokvezetési tényező