Training Protocol For Emergency Glucagon Providers May 2017

- Slides: 42
Training Protocol For Emergency Glucagon Providers May, 2017 Revisions 1
Glucagon Training Protocol Ø Acknowledgements: Ø Multnomah ESD’s Department of Health and Social Services for the original development of this training tool. Ø Oregon Department of Education’s School Nurse Advisory Group for their professional expertise in updating these training tools. Ø The American Diabetes Association’s Safe At School Advisory Committee for their expertise in the development of these training tools.
Introduction Ø ORS 433. 800 -433. 830 Ø Allows for the administration of epinephrine for anyone experiencing a severe allergic reaction Ø Allows for the administration of Glucagon for an individual with a prescription for Glucagon suffering from severe hypoglycemia Ø Allows for the administration of an injectable medication to treat adrenal insufficiency when a student is experiencing an adrenal crisis Ø This training is for Glucagon only
Training Pre-Requisites Ø Must reasonably expect to have responsibility for or contact with a person at known risk for hypoglycemia Ø This is usually a person with diabetes Ø Person to be trained must be at least 18 years of age Ø School personnel – Medication Training
In the School Setting Ø Parents notify school or daycare of child’s medical needs Ø School initiates an individualized health plan (IHP) Ø School documents agreements among parents/school/daycare/medical provider Ø The school nurse or school counselor are usually the lead school staff for coordinating support for students with diabetes
Using The Protocol Ø Initial training or retraining Ø Covers: Ø An overview of diabetes Ø Recognition of symptoms Ø Factors that lead to hypoglycemia Ø Administration of glucagon Ø Necessary follow-up treatment
Key Elements of this Training Ø Ø Ø Reading through the protocol Observing procedure for administering glucagon A return demonstration (required) Asking questions Completing the open-book evaluation Statement of Completion of Training
Completion of Training Ø Trainee must satisfactorily complete the training Ø Statement of completion of training must be signed by the trainer Ø Statement of completion is provider-specific Ø Retraining is required every three years Ø Annual retraining is strongly recommended
Overview of Diabetes Ø A chronic/lifelong disease Ø Affects the way the body uses food Ø Pancreas produces insulin Ø Insulin allows glucose to go into the cells to be used for energy Ø In diabetes this system does not work Ø Glucose builds up in the blood stream Ø Insulin must be replaced with injections
Overview of Diabetes -- cont. Type 1 diabetes – Pancreas produces no insulin – Treated with insulin (by shots or pump) – Usual type for children and young adults – No prevention – Lifelong Type 2 diabetes – Not enough insulin produced or – Person does not respond to insulin – May be treated orally and/or with insulin – More common in adults
Hyperglycemia (high blood sugar) Ø Ø Ø Ø increased thirst frequent urination increased hunger weight loss irritability flushed, dry skin nausea and vomiting weakness and fatigue
Complications Ø High blood sugar levels may cause serious complications over time Ø blindness Ø kidney disease or nerve damage Ø heart disease Ø It is important to control blood sugar levels
Balance Ø Management of diabetes consists of an intricate balance of: Ø Insulin Ø Food intake Ø Physical activity Ø Physical/emotional stress, illness Ø Anything that tips this delicate balance can cause fluctuations in blood sugar
Hypoglycemia (Low Blood Sugar) Ø Most serious “emergency” problem that can occur with blood sugar control Ø Comes on very quickly Ø Requires early detection and immediate attention
Common Causes of Hypoglycemia Ø Ø Ø Too much diabetes medication Change in meal or snack times Not enough food Skipping or not finishing meals or snacks Getting more physical activity or exercise than usual Drinking alcohol without eating
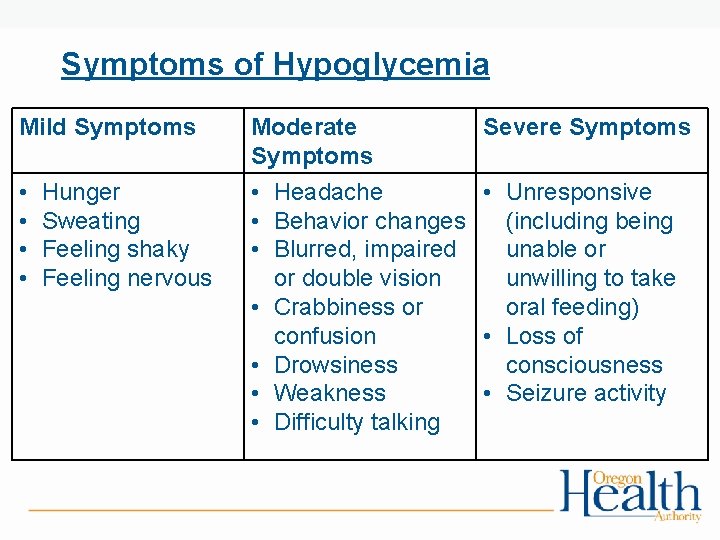
Mild Symptoms Ø Ø Hunger Sweating Feeling shaky Feeling nervous

Moderate Symptoms Ø Ø Ø Ø Headache Behavior changes Blurred, impaired or double vision Crabbiness or confusion Drowsiness Weakness Difficulty talking
Severe Symptoms Ø Unresponsiveness Ø Unwilling or unable to take oral feedings Ø Loss of consciousness Ø Seizure activity
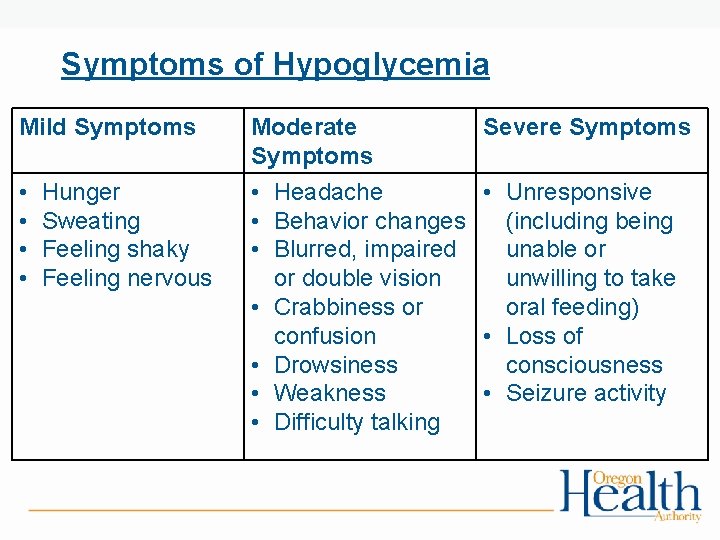
Symptoms of Hypoglycemia Mild Symptoms • • Hunger Sweating Feeling shaky Feeling nervous Moderate Symptoms • Headache • Behavior changes • Blurred, impaired or double vision • Crabbiness or confusion • Drowsiness • Weakness • Difficulty talking Severe Symptoms • Unresponsive (including being unable or unwilling to take oral feeding) • Loss of consciousness • Seizure activity
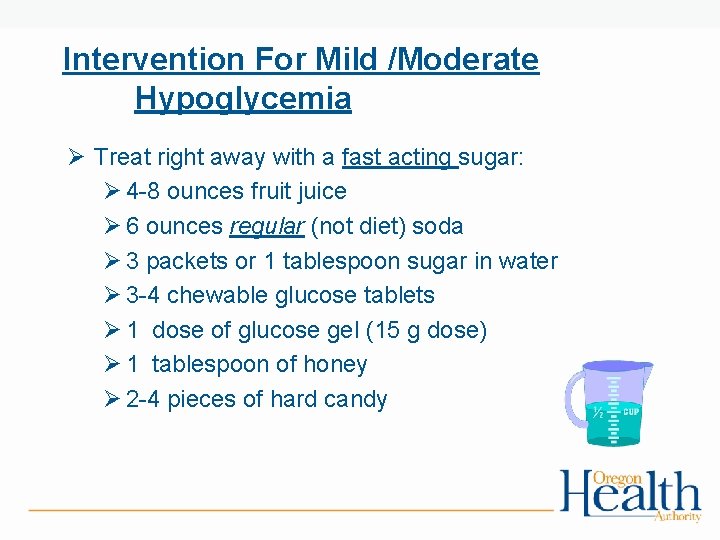
Intervention For Mild /Moderate Hypoglycemia Ø Treat right away with a fast acting sugar: Ø 4 -8 ounces fruit juice Ø 6 ounces regular (not diet) soda Ø 3 packets or 1 tablespoon sugar in water Ø 3 -4 chewable glucose tablets Ø 1 dose of glucose gel (15 g dose) Ø 1 tablespoon of honey Ø 2 -4 pieces of hard candy
15 Minute Rule After the initial treatment: Ø Observe and recheck in 15 minutes Ø Repeat fast-acting carbohydrate if blood sugar not in acceptable range Ø If the recheck is within an acceptable range, an extra snack should be given if meal is one hour away or more Ø After 2 nd treatment, if not above 80 or falling, call for help, parent, and 911
Treatment For Severe Symptoms of Hypoglycemia Ø Prepare to treat with glucagon if: Ø The person is unwilling or unable to take a treatment Ø The person does not feel better after the second treatment Ø The person is not improving after treatments outlined on physician orders Ø The symptoms worsen to the point the person is unable to swallow Ø Loss of consciousness or seizures occur
Glucagon Ø Ø Ø A hormone, like insulin, made in the pancreas Acts on the liver by converting glycogen to glucose Safe and relatively free from adverse reactions No human overdose has been reported May cause nausea and vomiting
Glucagon Emergency Kit Ø Available in package with supplies needed for administration Ø Contains: Ø a bottle of glucagon in powder form Ø a syringe filled with special diluting fluid Ø Obtained by prescription only for the individual with diabetes
Glucagon: Storage and Handling Ø Ø Store at room temperature {59° - 86°} Do not mix until needed Discard any unused portion Glucagon solution should be clear and of a water-like consistency Ø Check expiration dates periodically Ø Injection in fatty tissue or muscle of arm/thigh
Access to Glucagon Ø Assure a plan for emergencies Ø Kits need to be readily available and in close proximity to the student/person Ø On field trips, student may carry own kit if age/developmentally appropriate
Glucagon - Dosages Ø Manufactured in 1 mg vials Ø Person’s health care provider will determine individualized dose
Observation and Intervention Steps for Severe Hypoglycemia Ø IF PERSON IS UNRESPONSIVE, AND THEY ARE NOT BREATHING OR THEIR PULSE IS ABSENT: CALL 9 -1 -1 & Initiate CPR
Intervention/Severe Hypoglycemia—cont. Ø IF PERSON IS UNCONSCIOUS, BUT BREATHING AND PULSE ARE PRESENT, ASSUME SEVERE HYPOGLYCEMIA. Ø Delegate someone to call 9 -1 -1/EMS Ø Cut/clamp insulin tubing (if on insulin pump) Ø Obtain glucagon emergency kit Ø Prepare and administer glucagon
To Prepare Glucagon Ø Ø Ø Put on gloves Remove the flip-off seal from powdered glucagon Remove needle cover from syringe Do not remove plastic clip from syringe Insert the needle into the vial of powdered glucagon Push the plunger to inject the entire contents of the liquid into the vial of powdered glucagon
Prepare Glucagon -- cont. Ø Leave the needle on the syringe in the vial Ø Gently shake bottle until powder dissolves Ø Withdraw the right amount of medication
Administer Glucagon –cont. Ø Insert the needle into the loose skin/muscle of the upper arm or thigh Ø Administer all the medication Ø Carefully withdraw the needle at the same angle without releasing the person’s limb Ø Discard needle according to Oregon OSHA Bloodborne Pathogen Standards
Administer Glucagon—cont. Ø It may be difficult to give an injection to a person who is combative or having a seizure Ø Get assistance from another caregiver
Care Of The Person Ø Position person on side Ø Monitor for absent pulse/breath, or seizures Ø Improvement will usually be seen within 10 -15 minutes Ø Although rare, the person may be unresponsive for other reasons
Care Of The Person -- cont. Ø When responds and able to swallow, feed a fastacting source of sugar (page 7) Ø Start with clear, sugar-containing liquids Ø Feed longer-acting source of sugar if possible (carbohydrate and protein) Ø Seek consultation from medical provider for further direction
Follow-Up Ø Emergency responder will make decision about need for transport to medical facility Ø Students in school or daycare need to be taken from school by parent or 9 -1 -1 Ø The person or parent/guardian should seek consultation with their healthcare provider to prevent future episodes of hypoglycemia Ø Replace Glucagon Emergency Kit
REVIEW: Assessment and Treatment Ø Determine if person is experiencing symptoms of hypoglycemia Ø Test blood sugar if possible and if trained Ø Prepare to treat for low blood sugar
Mild/Moderate Hypoglycemia Ø Give oral treatment Ø 15 Minute Rule: (page 7) Ø Retest blood sugar in 15 minutes Ø If no improvement, give second fast acting treatment Ø If no improvement after two treatments. . .
Mild/Moderate-cont. Ø If blood glucose is below 80 or falling: Ø Call parent, designated contact, or 911 Ø If meal is more than 1 hr. away, follow with a carbohydrate/protein snack Ø If on insulin pump, treat and consult medical orders
REVIEW Severe Hypoglycemia Ø Ø Ø Tell someone to call 911 If on pump, clamp/cut tubing Prepare and administer glucagon Position person on side Monitor for absent pulse/breathing If person responds and can swallow-provide oral treatment Ø Follow-up with health care provider
Evaluation Tool Ø Open Book – pages 16 -18
QUESTIONS?