TRACHEA AND THORACIC DUCT DR GARIMA SEHGAL TRACHEA

- Slides: 27
TRACHEA AND THORACIC DUCT DR GARIMA SEHGAL

TRACHEA
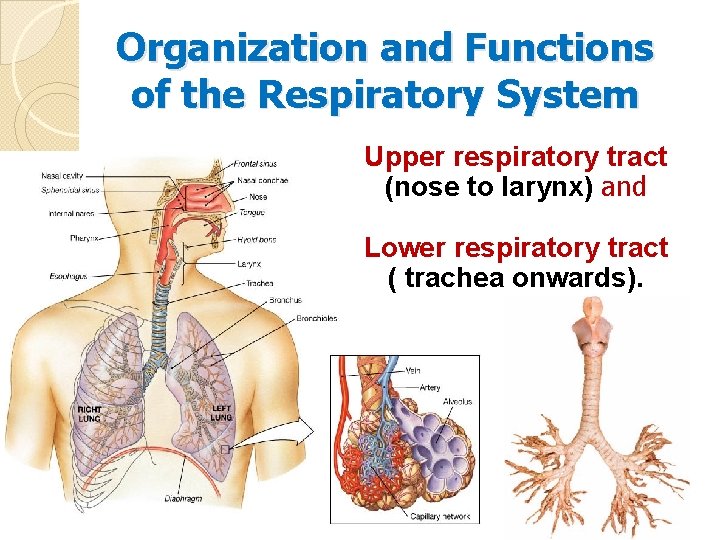
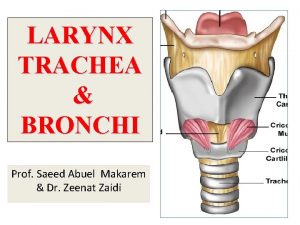
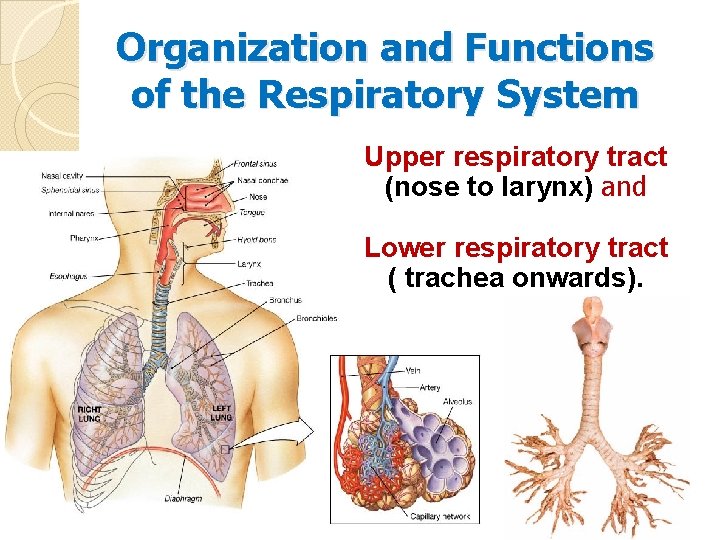
Organization and Functions of the Respiratory System Upper respiratory tract (nose to larynx) and Lower respiratory tract ( trachea onwards).
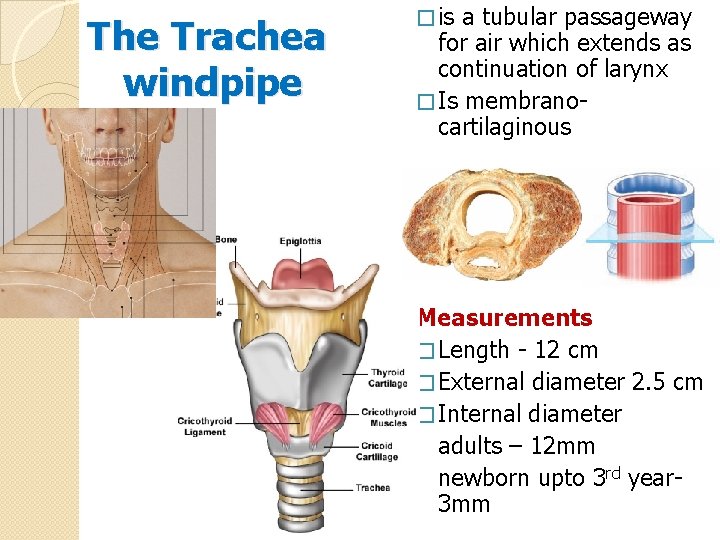
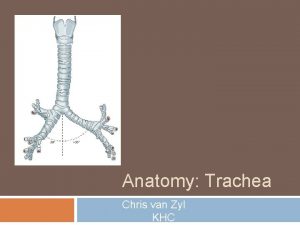
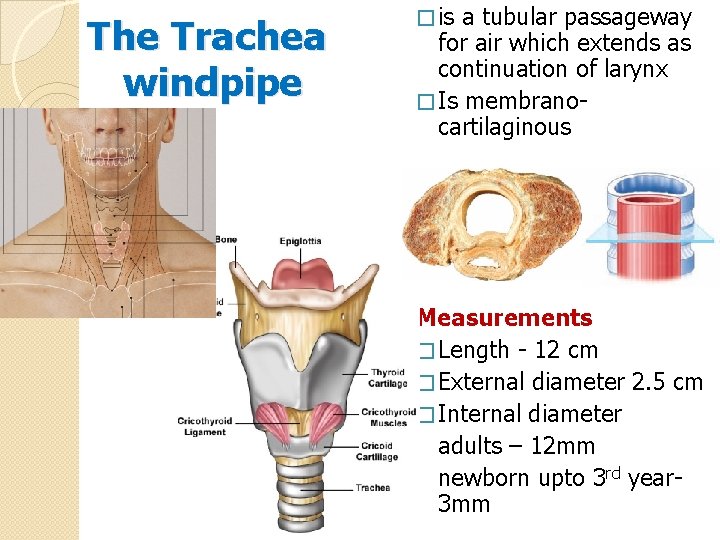
The Trachea windpipe � is a tubular passageway for air which extends as continuation of larynx � Is membranocartilaginous Measurements � Length - 12 cm � External diameter 2. 5 cm � Internal diameter adults – 12 mm newborn upto 3 rd year 3 mm
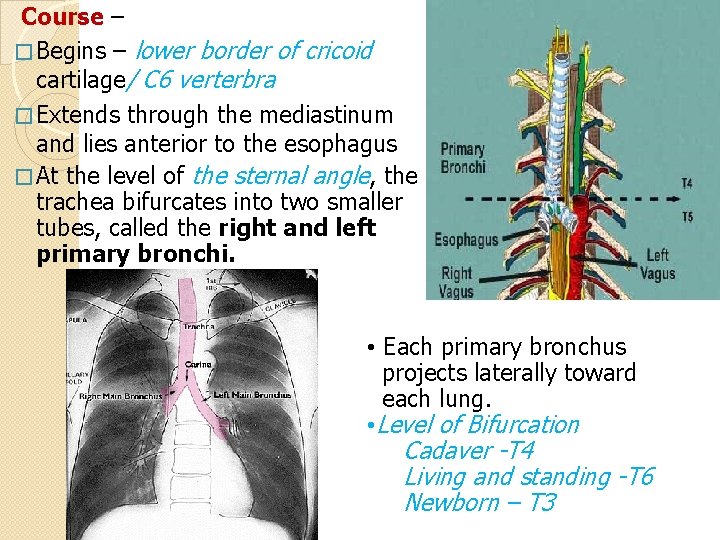
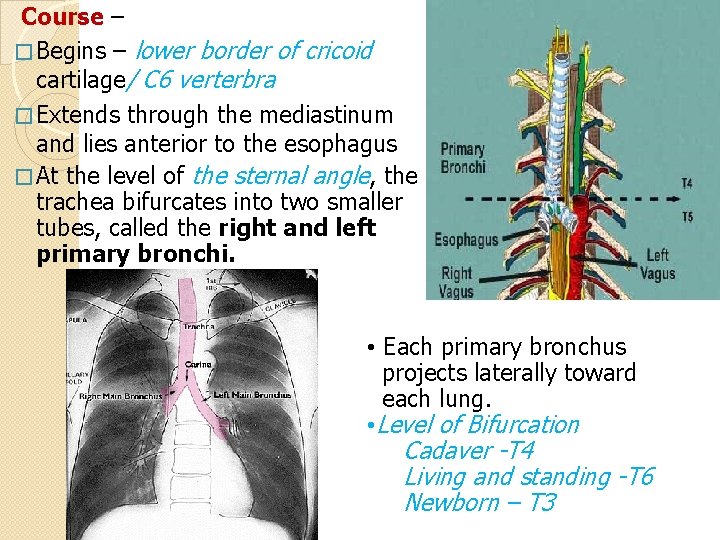
Course – � Begins – lower border of cricoid cartilage/ C 6 verterbra � Extends through the mediastinum and lies anterior to the esophagus � At the level of the sternal angle, the trachea bifurcates into two smaller tubes, called the right and left primary bronchi. • Each primary bronchus projects laterally toward each lung. • Level of Bifurcation Cadaver -T 4 Living and standing -T 6 Newborn – T 3
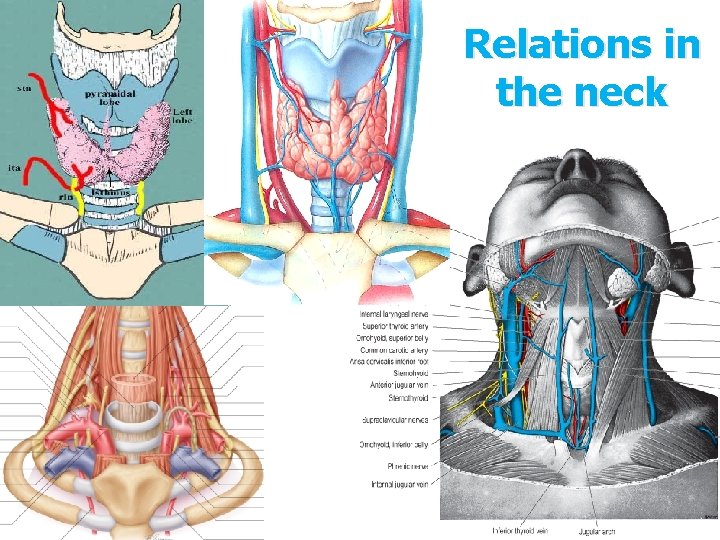
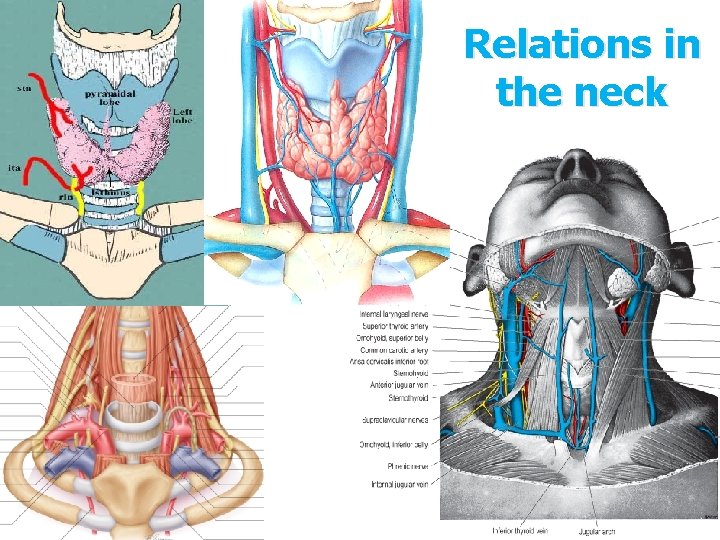
Relations in the neck
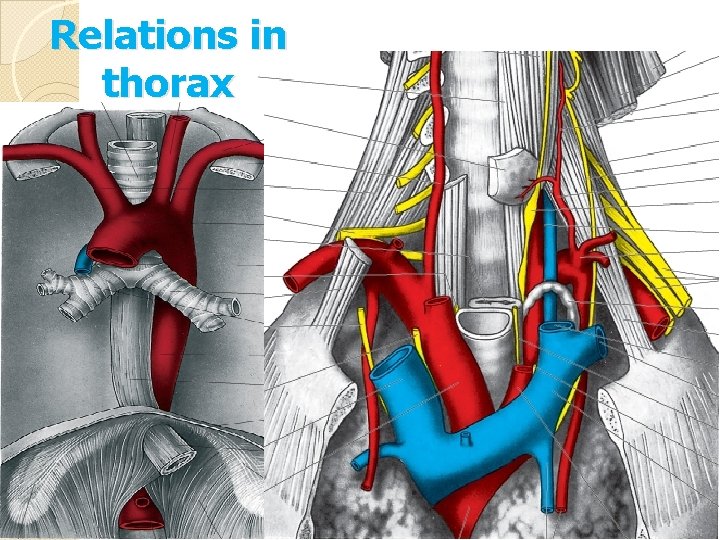
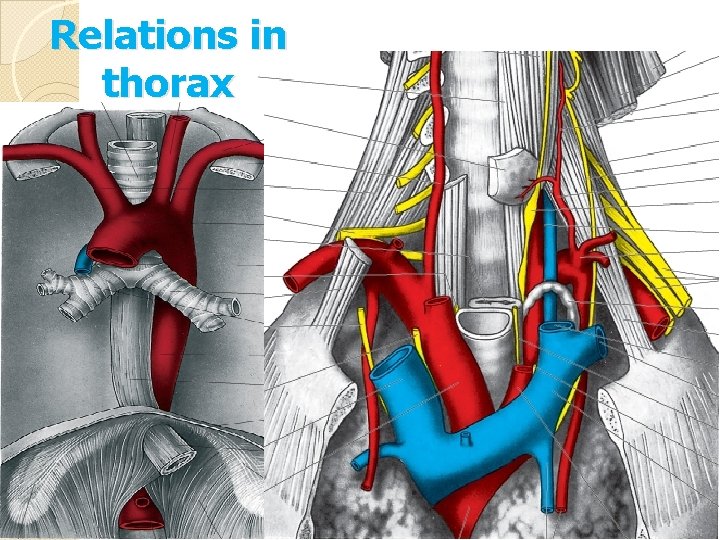
Relations in thorax
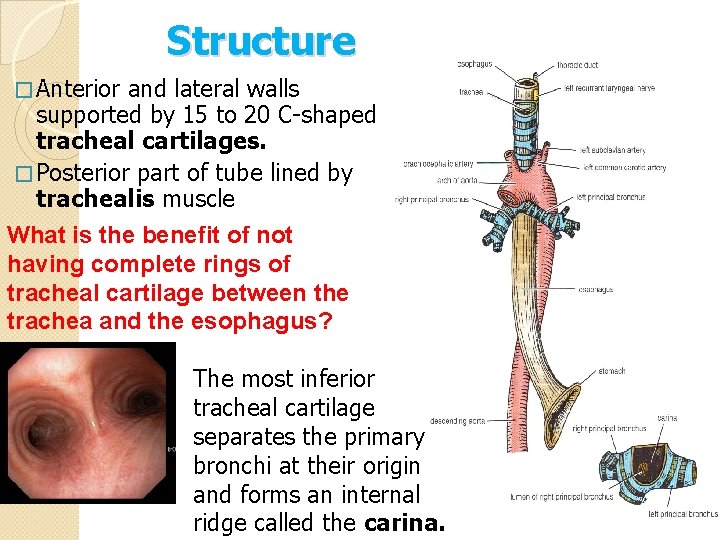
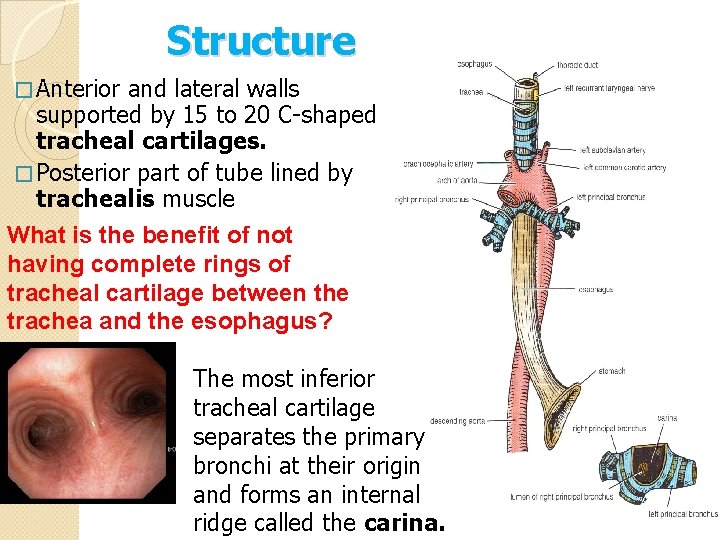
Structure � Anterior and lateral walls supported by 15 to 20 C-shaped tracheal cartilages. � Posterior part of tube lined by trachealis muscle What is the benefit of not having complete rings of tracheal cartilage between the trachea and the esophagus? The most inferior tracheal cartilage separates the primary bronchi at their origin and forms an internal ridge called the carina.
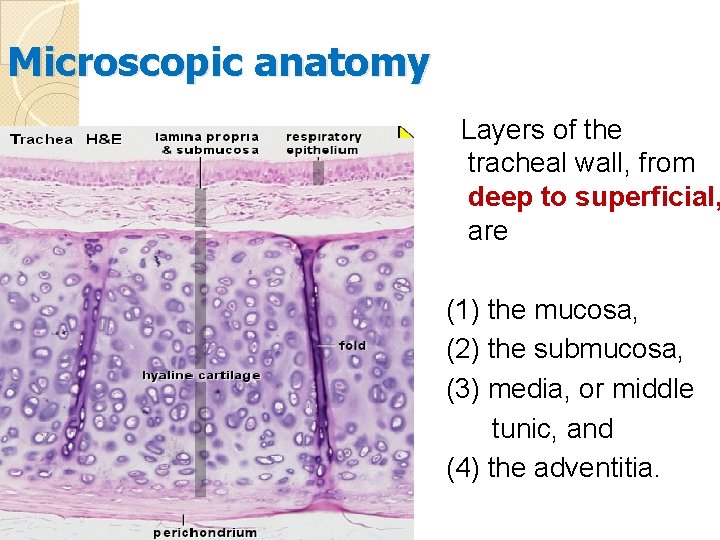
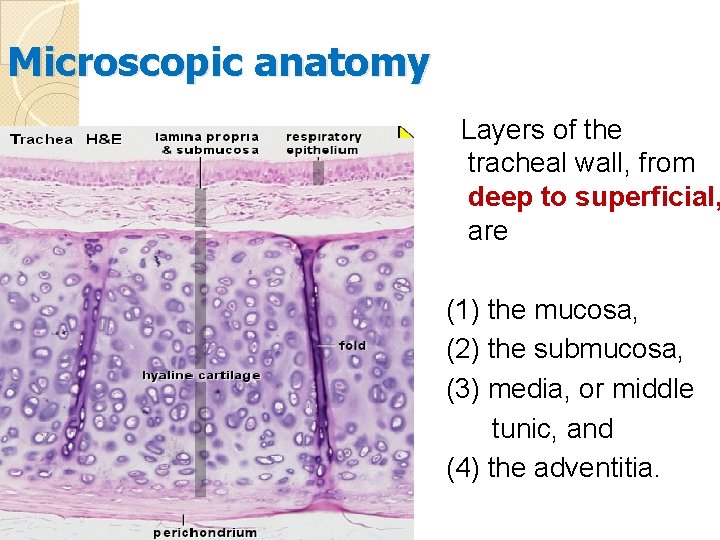
Microscopic anatomy Layers of the tracheal wall, from deep to superficial, are (1) the mucosa, (2) the submucosa, (3) media, or middle tunic, and (4) the adventitia.
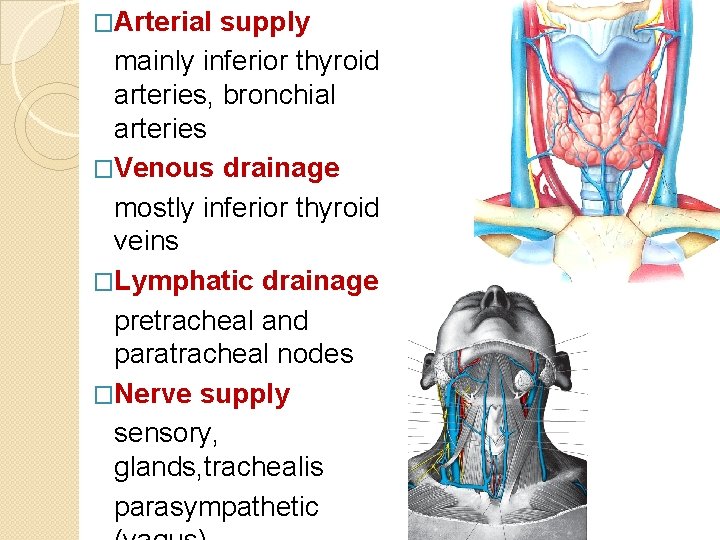
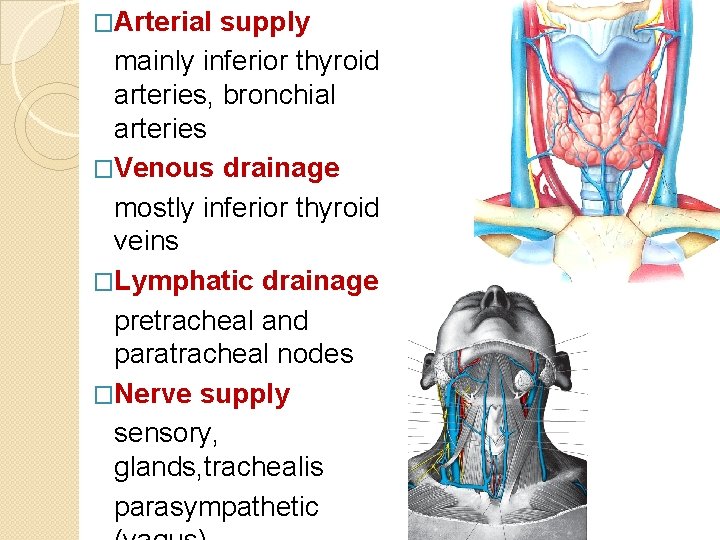
�Arterial supply mainly inferior thyroid arteries, bronchial arteries �Venous drainage mostly inferior thyroid veins �Lymphatic drainage pretracheal and paratracheal nodes �Nerve supply sensory, glands, trachealis parasympathetic
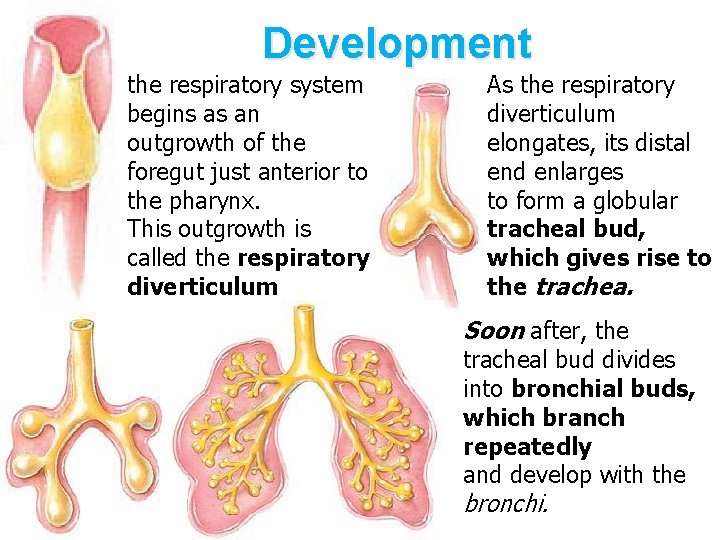
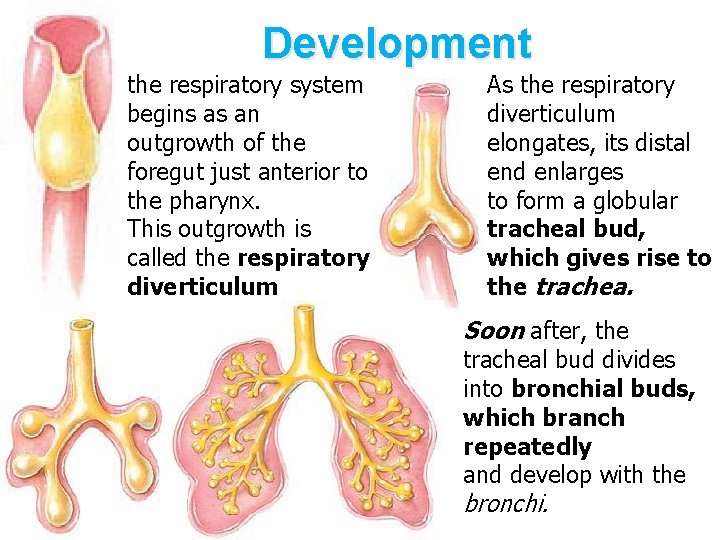
Development the respiratory system begins as an outgrowth of the foregut just anterior to the pharynx. This outgrowth is called the respiratory diverticulum As the respiratory diverticulum elongates, its distal end enlarges to form a globular tracheal bud, which gives rise to the trachea. Soon after, the tracheal bud divides into bronchial buds, which branch repeatedly and develop with the bronchi.
APPLIED ANATOMY
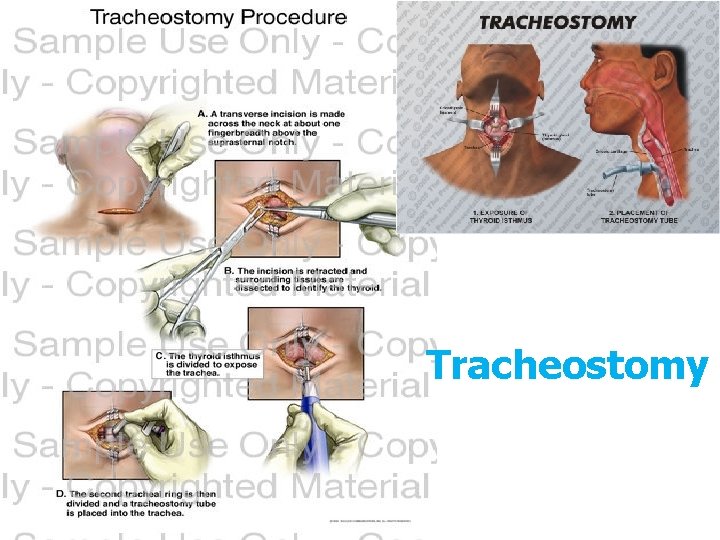
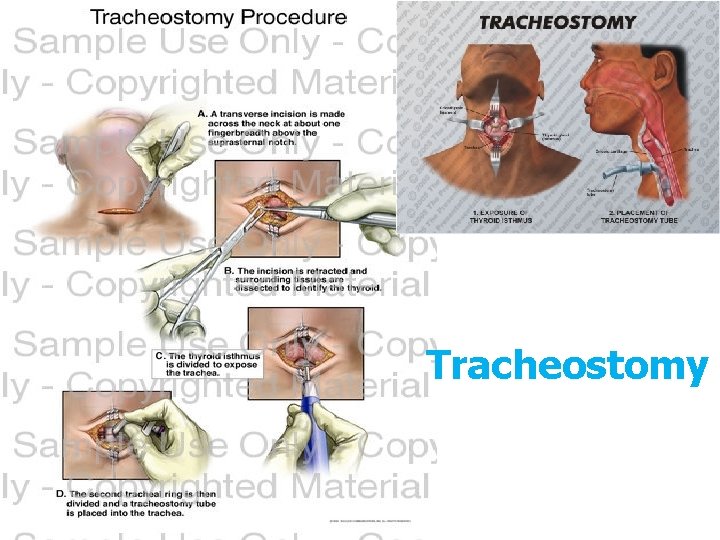
Tracheostomy
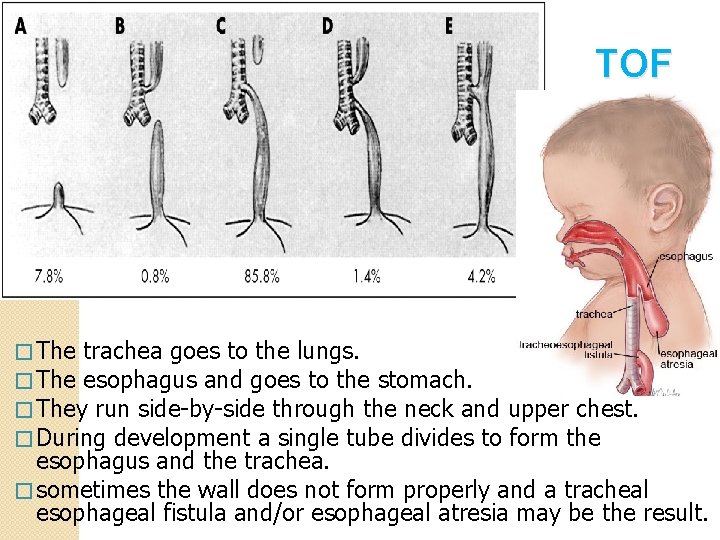
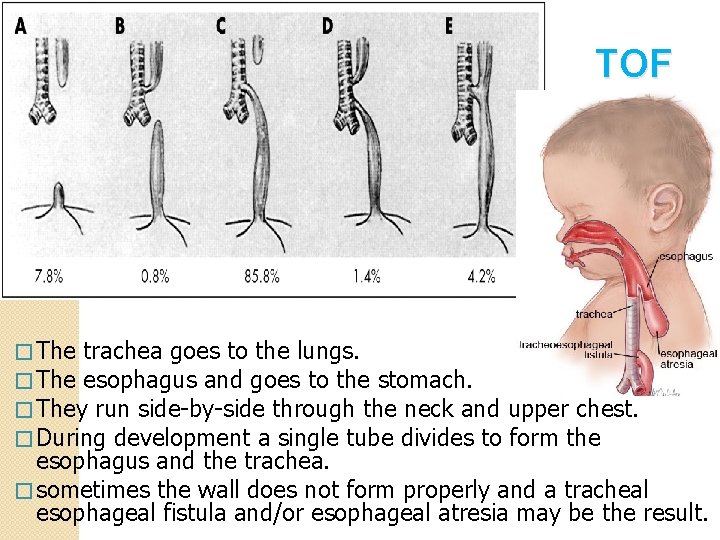
TOF � The trachea goes to the lungs. � The esophagus and goes to the stomach. � They run side-by-side through the neck and upper chest. � During development a single tube divides to form the esophagus and the trachea. � sometimes the wall does not form properly and a tracheal esophageal fistula and/or esophageal atresia may be the result.
THORACIC DUCT
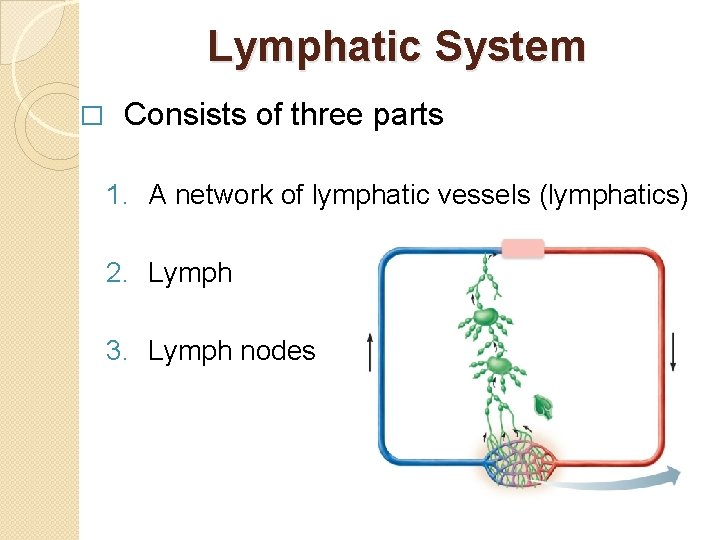
Lymphatic System � Consists of three parts 1. A network of lymphatic vessels (lymphatics) 2. Lymph 3. Lymph nodes
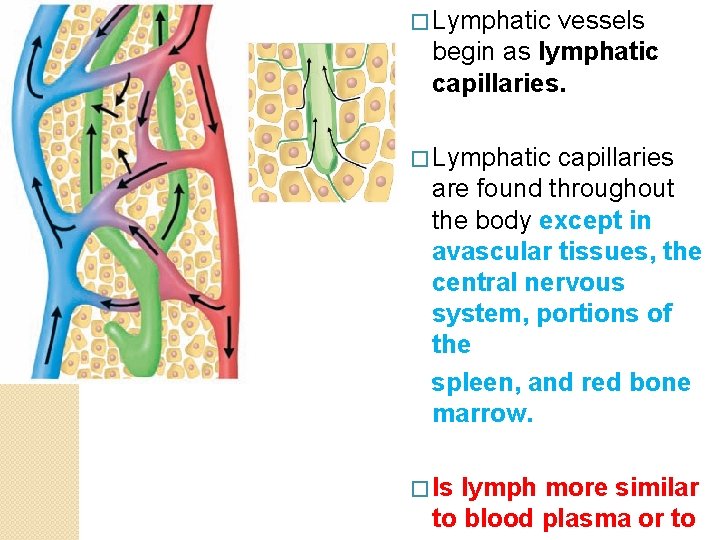
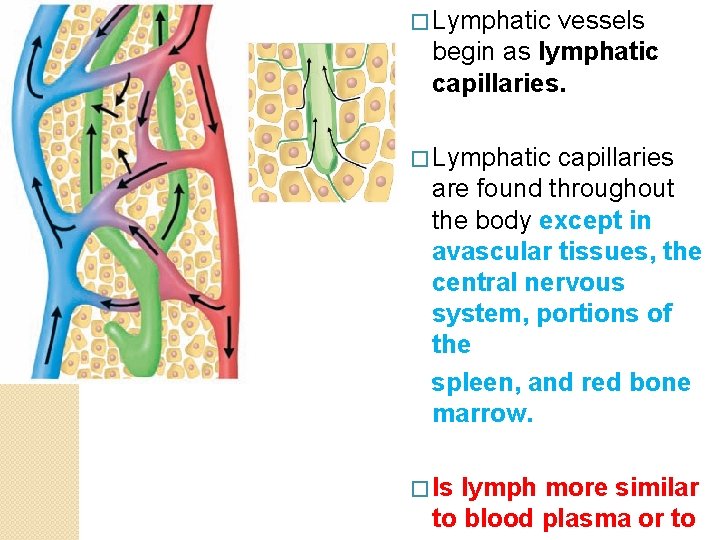
� Lymphatic vessels begin as lymphatic capillaries. � Lymphatic capillaries are found throughout the body except in avascular tissues, the central nervous system, portions of the spleen, and red bone marrow. � Is lymph more similar to blood plasma or to
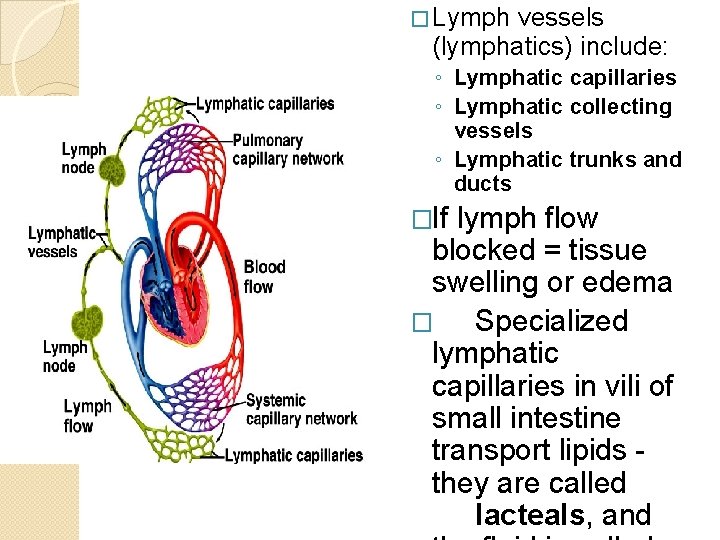
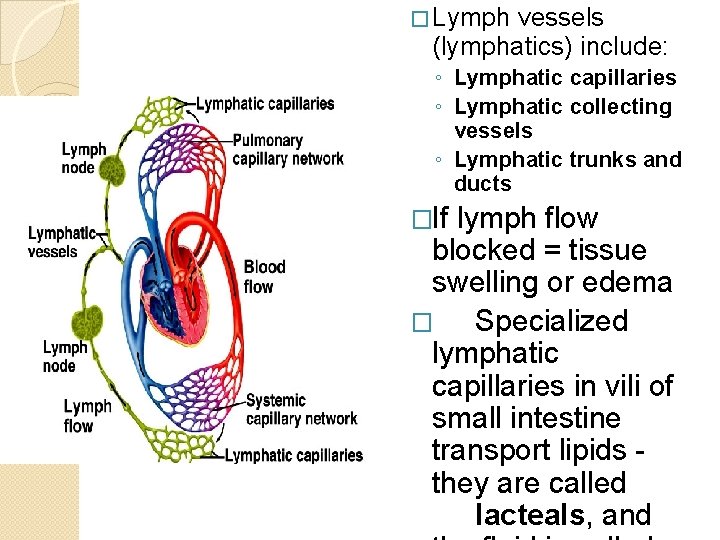
� Lymph vessels (lymphatics) include: ◦ Lymphatic capillaries ◦ Lymphatic collecting vessels ◦ Lymphatic trunks and ducts �If lymph flow blocked = tissue swelling or edema � Specialized lymphatic capillaries in vili of small intestine transport lipids they are called lacteals, and
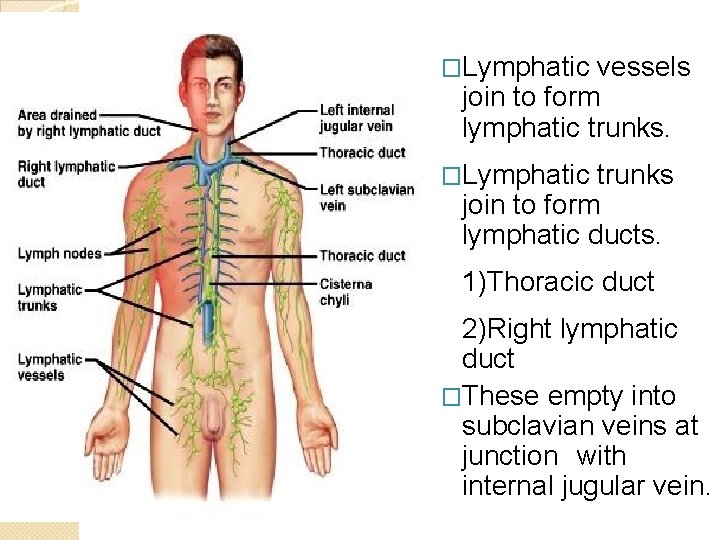
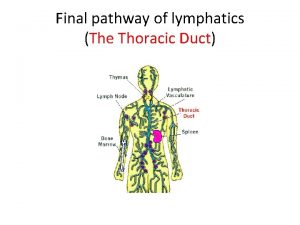
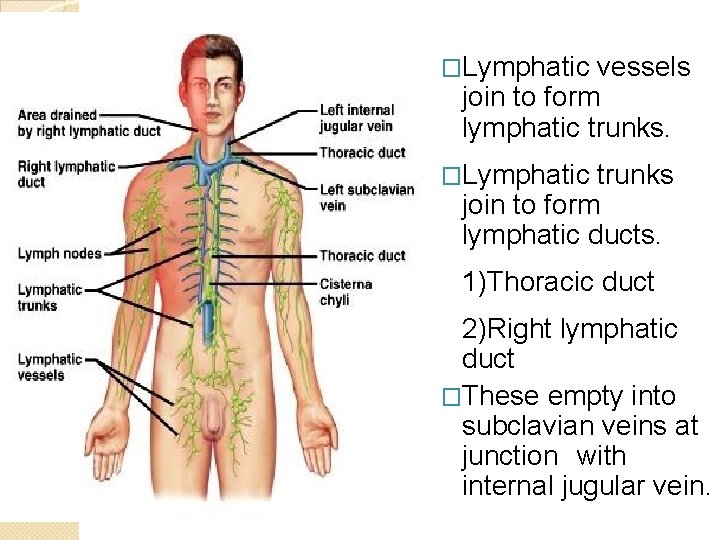
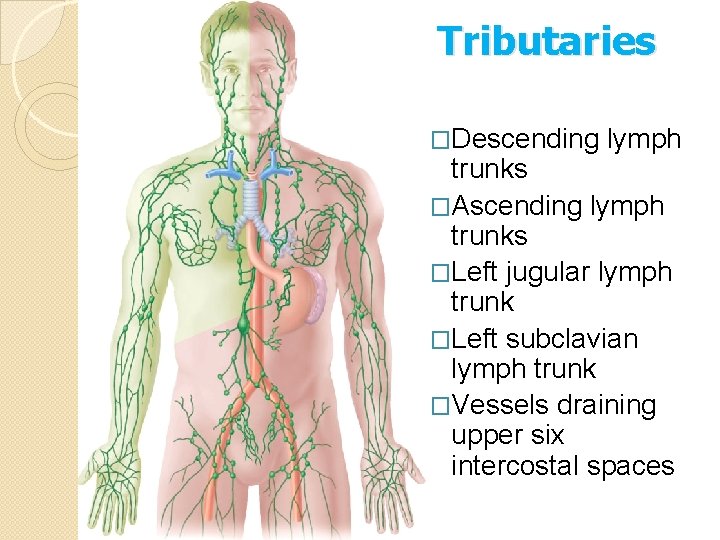
�Lymphatic vessels join to form lymphatic trunks. �Lymphatic trunks join to form lymphatic ducts. 1)Thoracic duct 2)Right lymphatic duct �These empty into subclavian veins at junction with internal jugular vein.
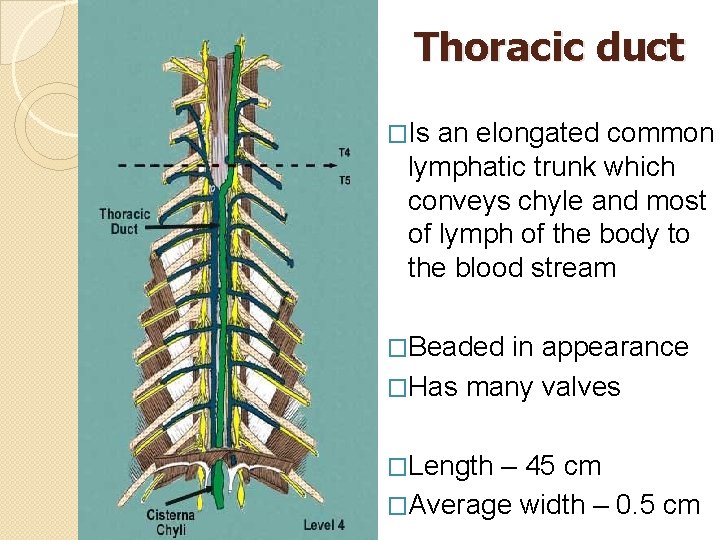
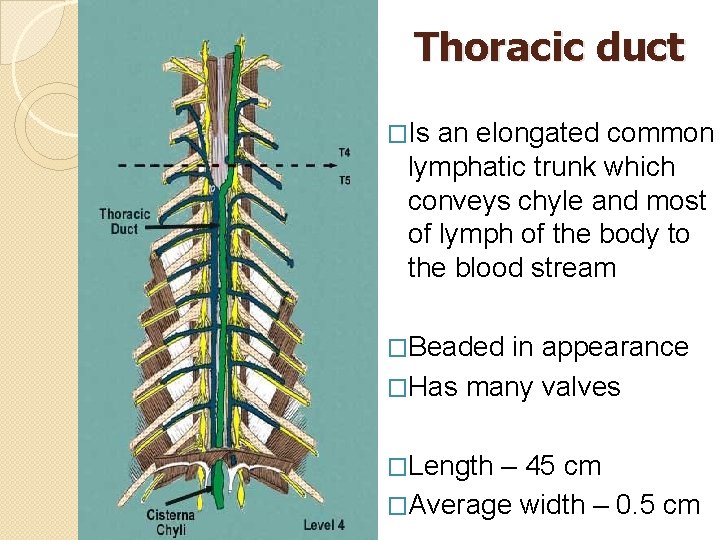
Thoracic duct �Is an elongated common lymphatic trunk which conveys chyle and most of lymph of the body to the blood stream �Beaded in appearance �Has many valves �Length – 45 cm �Average width – 0. 5 cm
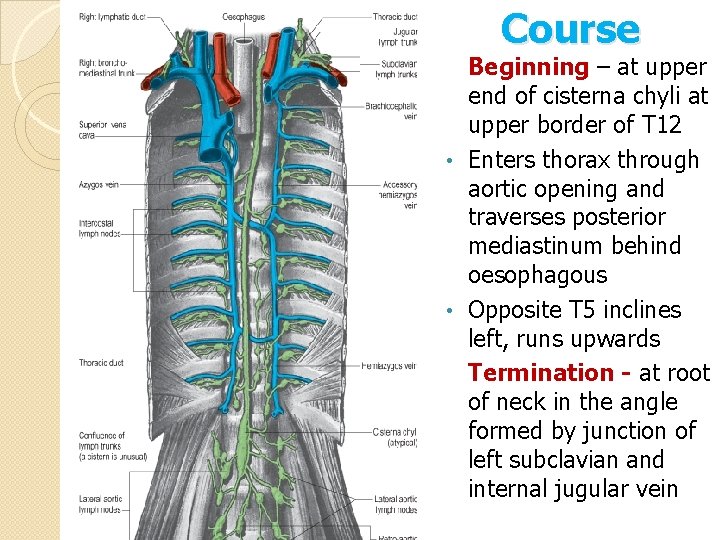
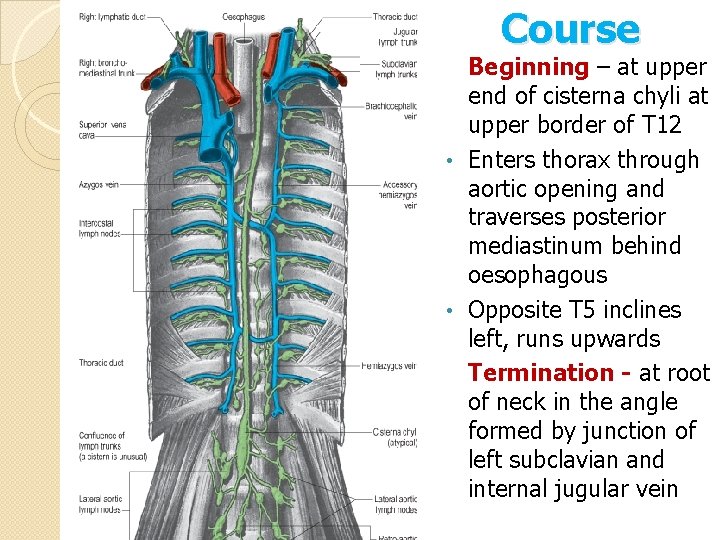
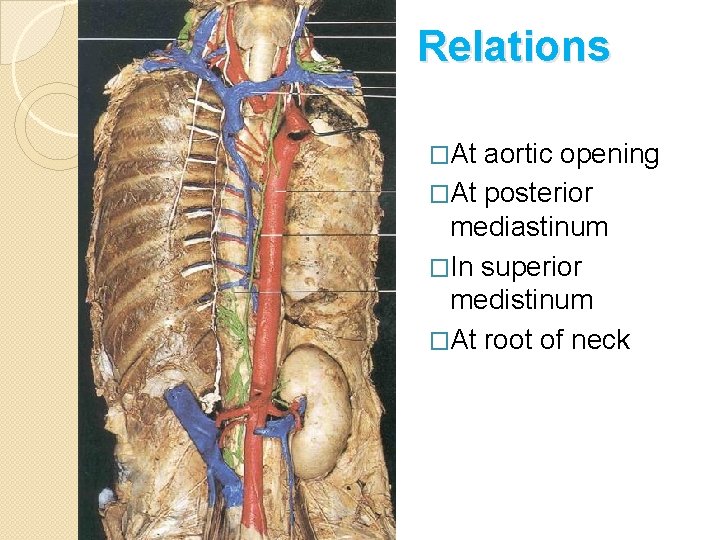
Course Beginning – at upper end of cisterna chyli at upper border of T 12 • Enters thorax through aortic opening and traverses posterior mediastinum behind oesophagous • Opposite T 5 inclines left, runs upwards Termination - at root of neck in the angle formed by junction of left subclavian and internal jugular vein
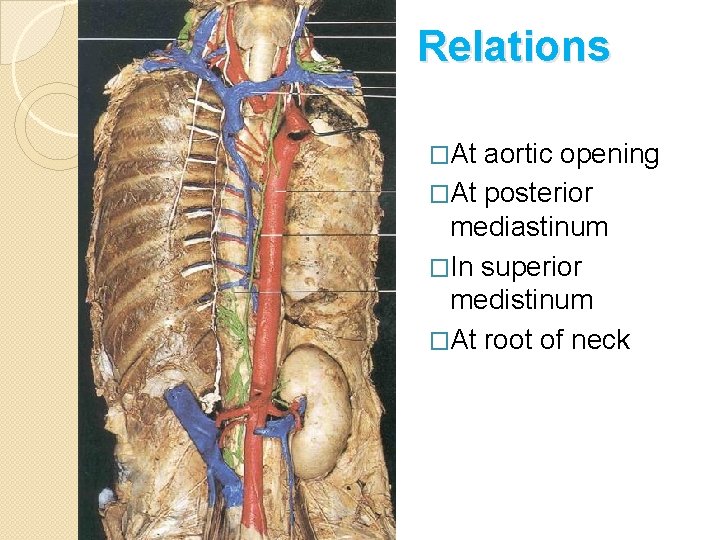
Relations �At aortic opening �At posterior mediastinum �In superior medistinum �At root of neck
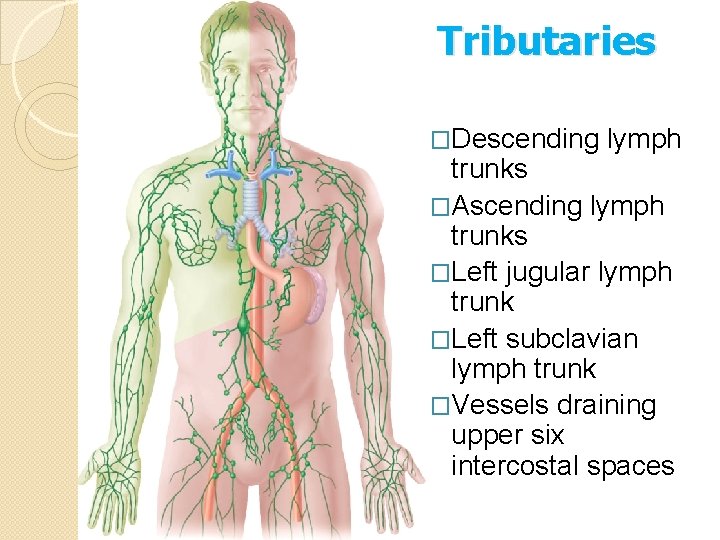
Tributaries �Descending lymph trunks �Ascending lymph trunks �Left jugular lymph trunk �Left subclavian lymph trunk �Vessels draining upper six intercostal spaces
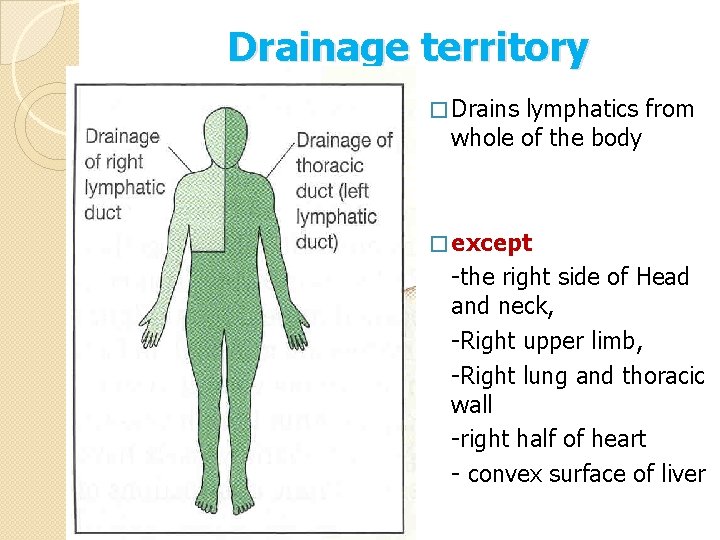
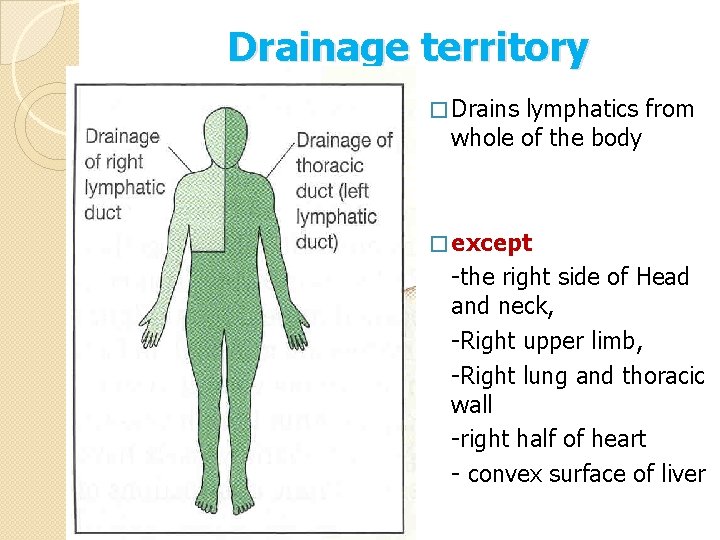
Drainage territory � Drains lymphatics from whole of the body � except -the right side of Head and neck, -Right upper limb, -Right lung and thoracic wall -right half of heart - convex surface of liver
APPLIED ANATOMY
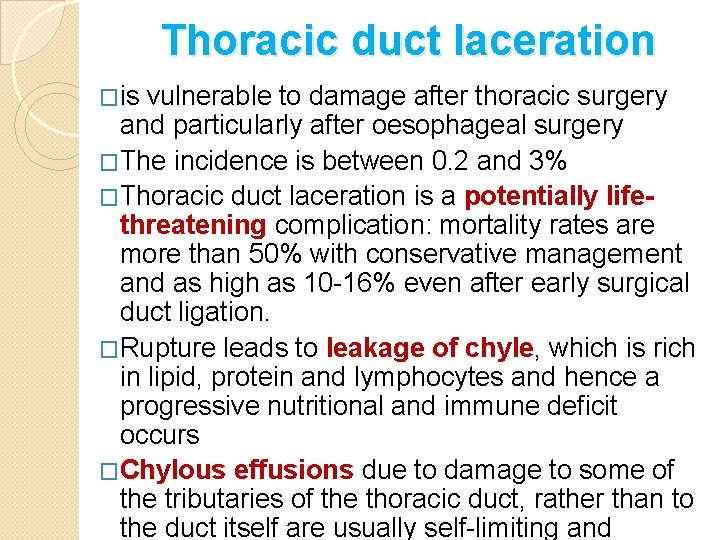
Thoracic duct laceration �is vulnerable to damage after thoracic surgery and particularly after oesophageal surgery �The incidence is between 0. 2 and 3% �Thoracic duct laceration is a potentially lifethreatening complication: mortality rates are more than 50% with conservative management and as high as 10 -16% even after early surgical duct ligation. �Rupture leads to leakage of chyle, which is rich in lipid, protein and lymphocytes and hence a progressive nutritional and immune deficit occurs �Chylous effusions due to damage to some of the tributaries of the thoracic duct, rather than to the duct itself are usually self-limiting and
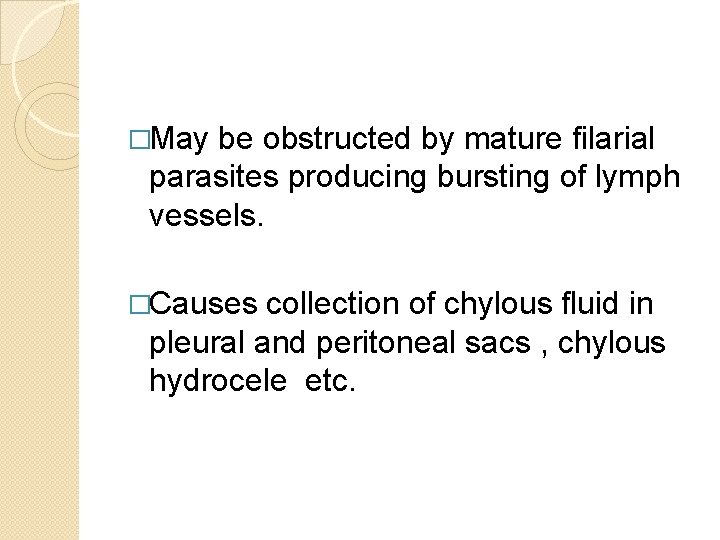
�May be obstructed by mature filarial parasites producing bursting of lymph vessels. �Causes collection of chylous fluid in pleural and peritoneal sacs , chylous hydrocele etc.
 Popularly called lymph glands
Popularly called lymph glands Thoracic duct
Thoracic duct Thoracic duct
Thoracic duct Aluyare
Aluyare Garima tiwari model
Garima tiwari model Sonia sehgal
Sonia sehgal Rahul sehgal md
Rahul sehgal md Cbs debating society
Cbs debating society Development of respiratory system
Development of respiratory system Pharynx and larynx and trachea
Pharynx and larynx and trachea Imaginary line through body
Imaginary line through body Antecubitis
Antecubitis Orbital cavity nasal cavity ventral cavity oral cavity
Orbital cavity nasal cavity ventral cavity oral cavity Lumbar vertebrae characteristics
Lumbar vertebrae characteristics Air passageway
Air passageway Larynx and trachea
Larynx and trachea Dermatome map
Dermatome map Trachea and thorax
Trachea and thorax Esophagus meaning
Esophagus meaning Respiratory tree
Respiratory tree Trunk and branch duct system
Trunk and branch duct system Mucus vs serous glands
Mucus vs serous glands Genu recurvatum
Genu recurvatum Arterial supply of thorax
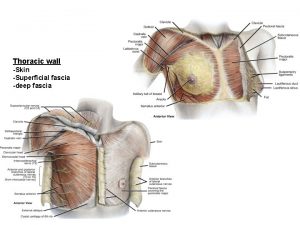
Arterial supply of thorax Superficial fascia of thorax
Superficial fascia of thorax Subcostales
Subcostales Sibson fascia
Sibson fascia Lymph nodes legs
Lymph nodes legs