TOXOPLASMA GONDII DR MONIKA RAJANI ASSOCIATE PROFESSOR DEPT

- Slides: 33
TOXOPLASMA GONDII DR MONIKA RAJANI ASSOCIATE PROFESSOR , DEPT OF MICROBIOLOGY CIMSH , LKO DR MONIKA RAJANI

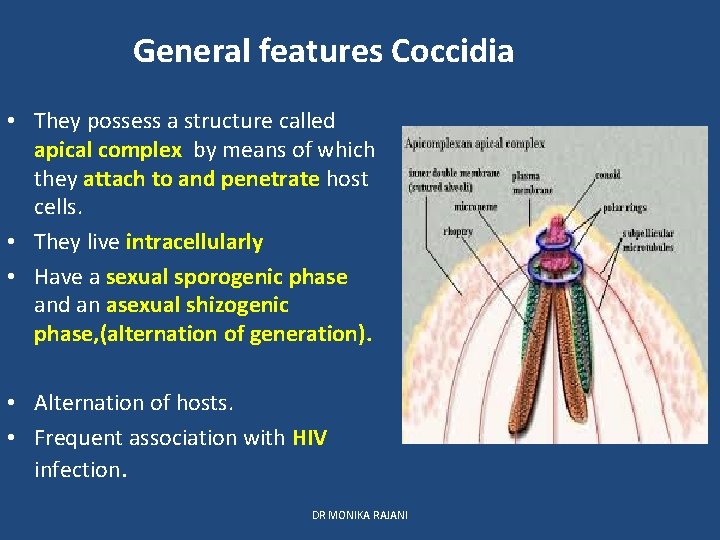
PHYLUM APICOMPLEXA CLASS SPOROZOA SUB CLASS COCCIDIA SUB ORDER EIMERIINA SUB ORDER HAEMOSPORINA GENUS Cryptosporidium Isospora, cyclospora Toxoplasma GENUS PLASMODIUM BABESIA DR MONIKA RAJANI
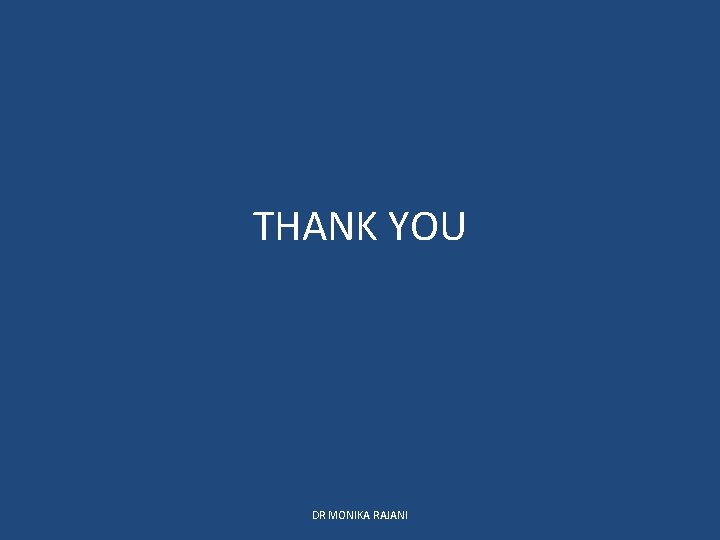
General features Coccidia • They possess a structure called apical complex by means of which they attach to and penetrate host cells. • They live intracellularly • Have a sexual sporogenic phase and an asexual shizogenic phase, (alternation of generation). • Alternation of hosts. • Frequent association with HIV infection. DR MONIKA RAJANI
Toxoplasma Gondii • Obligate intracellular coccidian parasite. • It was first described in a small North American rodent called gondii(Ctenodactylus gondii). • First recognised in a cyst in retina of child • Name “Toxo” is derived from Greek word “Toxon”meaning arc or brow referring to curved shape of trophozoite. • most common parasite globally with widest range of hosts DR MONIKA RAJANI
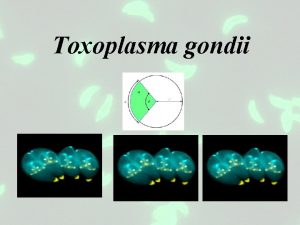
MORPHOLOGY T gondii occures in three forms: Trophozoite Tissue cyst shizogony Oocyst - sporogony Definitive host: cats and other felines : all three forms are seen • Intermediate host: humans, mammals (sheep, cattle, mice) and birds : only asexual forms are seen. • All three forms are infectious to man. • • • DR MONIKA RAJANI
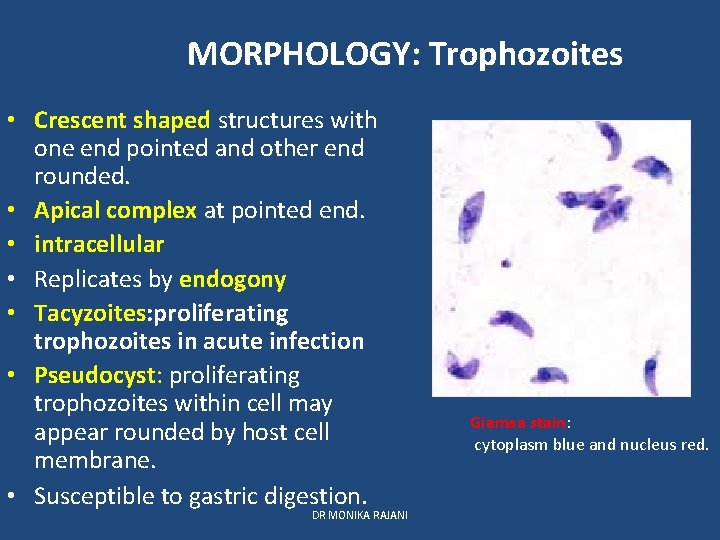
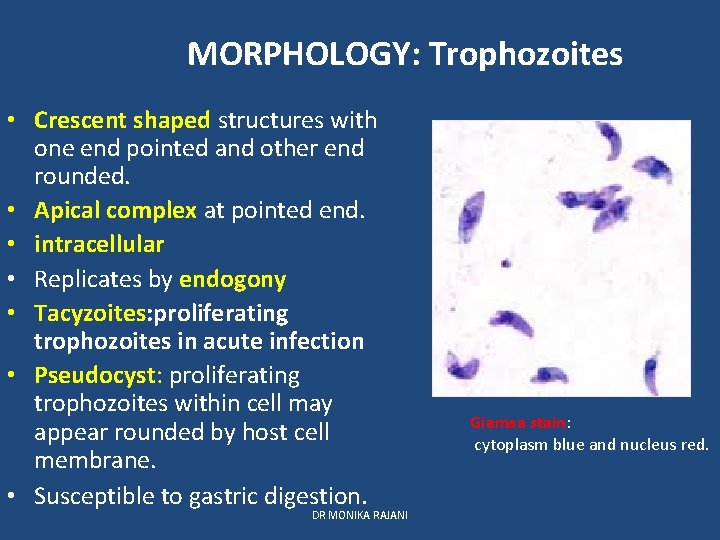
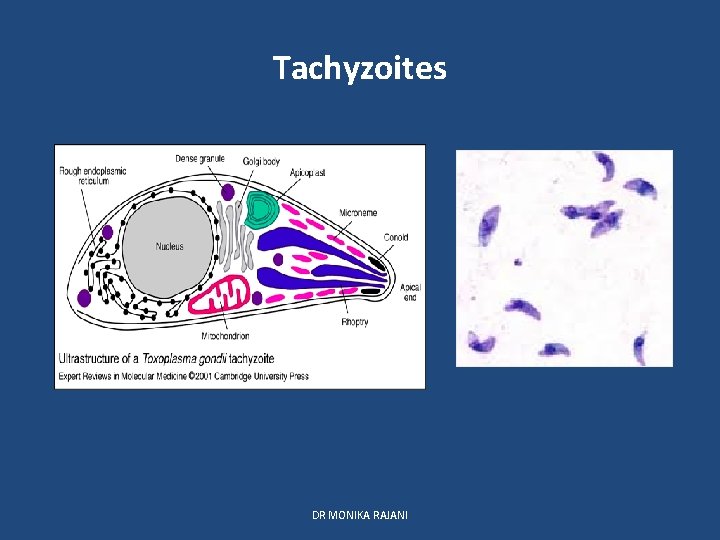
MORPHOLOGY: Trophozoites • Crescent shaped structures with one end pointed and other end rounded. • Apical complex at pointed end. • intracellular • Replicates by endogony • Tacyzoites: proliferating trophozoites in acute infection • Pseudocyst: proliferating trophozoites within cell may appear rounded by host cell membrane. • Susceptible to gastric digestion. DR MONIKA RAJANI Giemsa stain: cytoplasm blue and nucleus red.
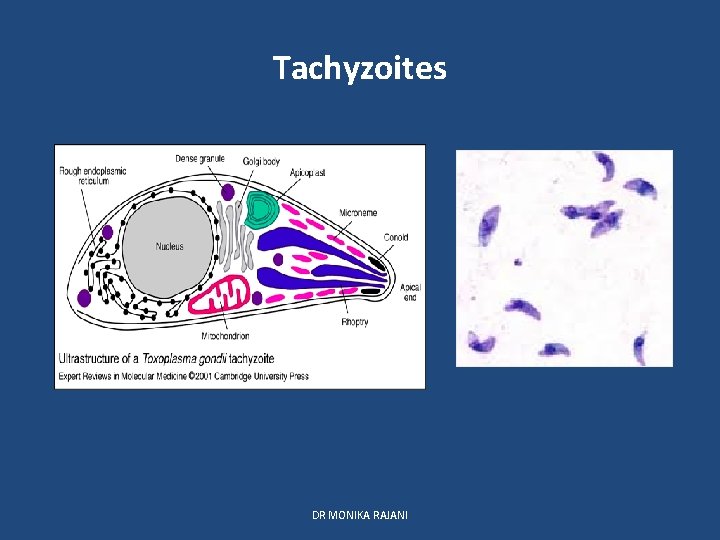
Tachyzoites DR MONIKA RAJANI
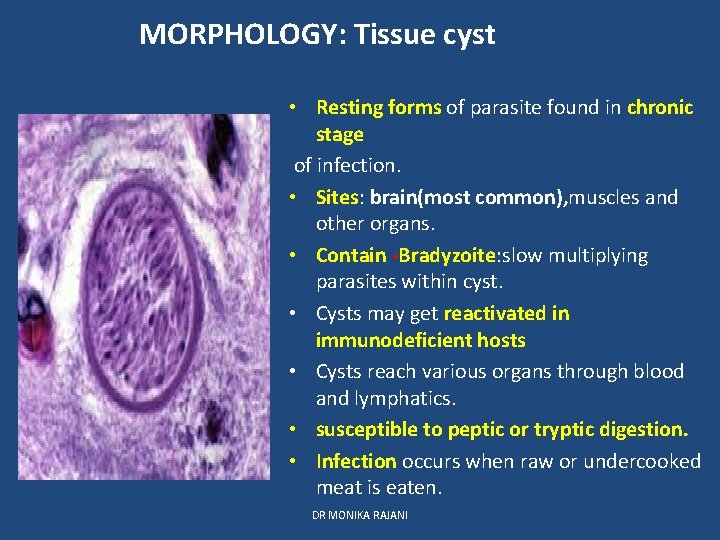
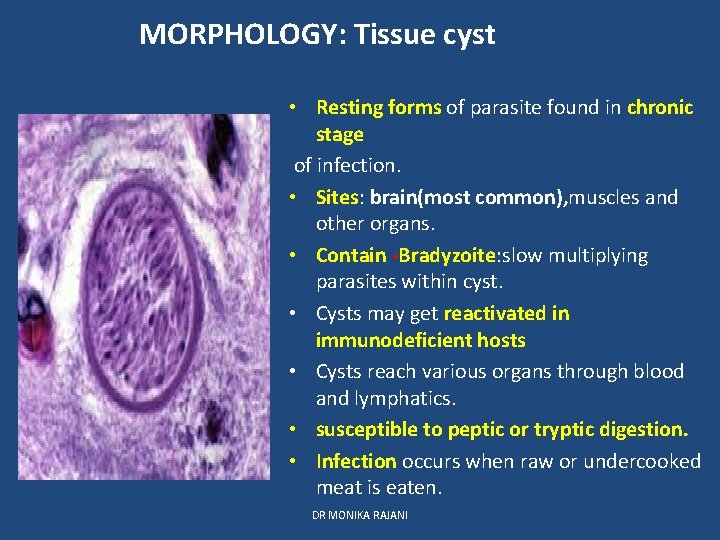
MORPHOLOGY: Tissue cyst • Resting forms of parasite found in chronic stage of infection. • Sites: brain(most common), muscles and other organs. • Contain -Bradyzoite: slow multiplying parasites within cyst. • Cysts may get reactivated in immunodeficient hosts • Cysts reach various organs through blood and lymphatics. • susceptible to peptic or tryptic digestion. • Infection occurs when raw or undercooked meat is eaten. DR MONIKA RAJANI
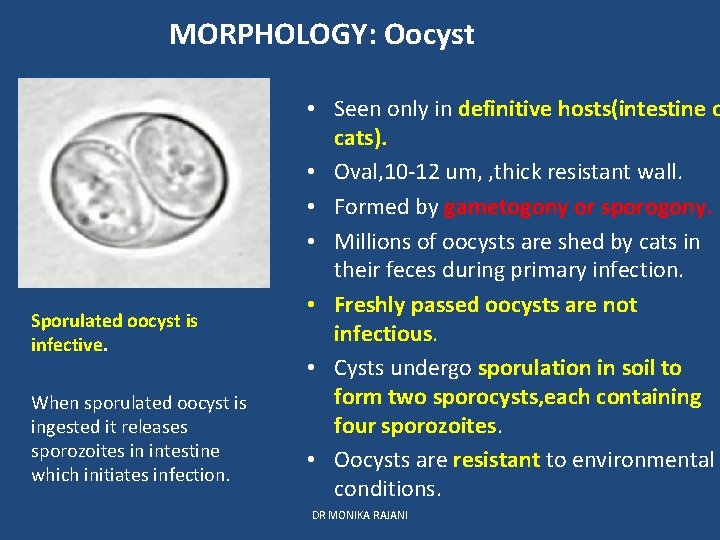
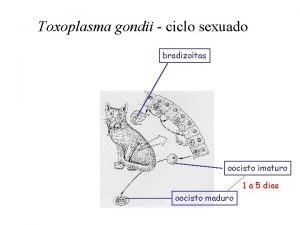
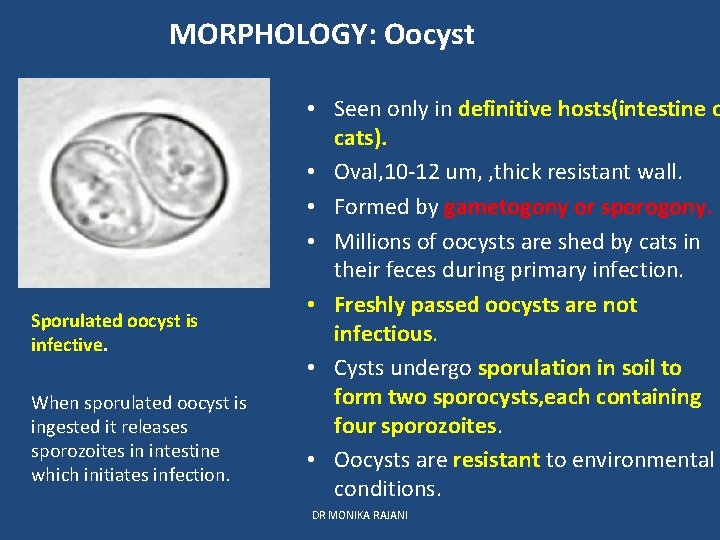
MORPHOLOGY: Oocyst Sporulated oocyst is infective. When sporulated oocyst is ingested it releases sporozoites in intestine which initiates infection. • Seen only in definitive hosts(intestine o cats). • Oval, 10 -12 um, , thick resistant wall. • Formed by gametogony or sporogony. • Millions of oocysts are shed by cats in their feces during primary infection. • Freshly passed oocysts are not infectious. • Cysts undergo sporulation in soil to form two sporocysts, each containing four sporozoites. • Oocysts are resistant to environmental conditions. DR MONIKA RAJANI
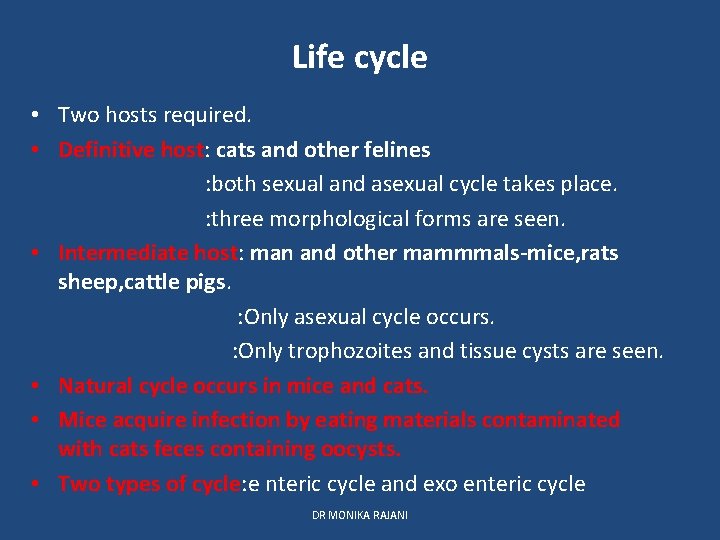
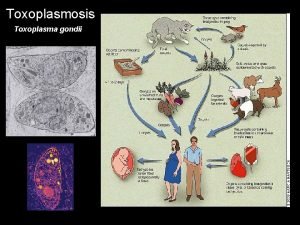
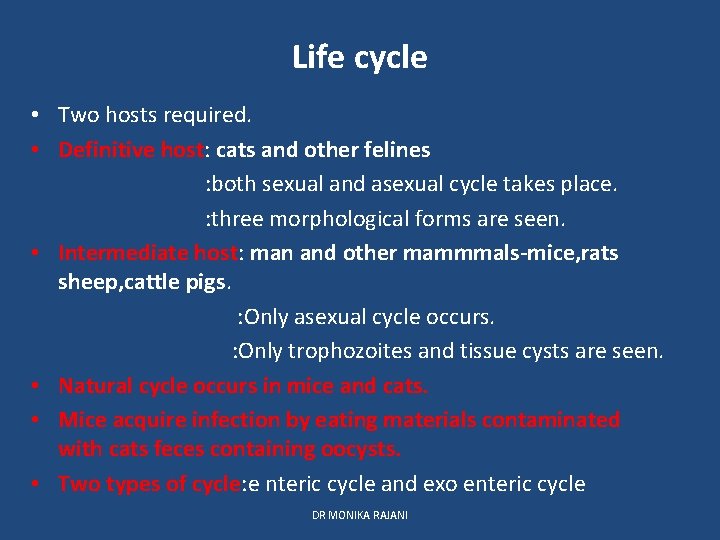
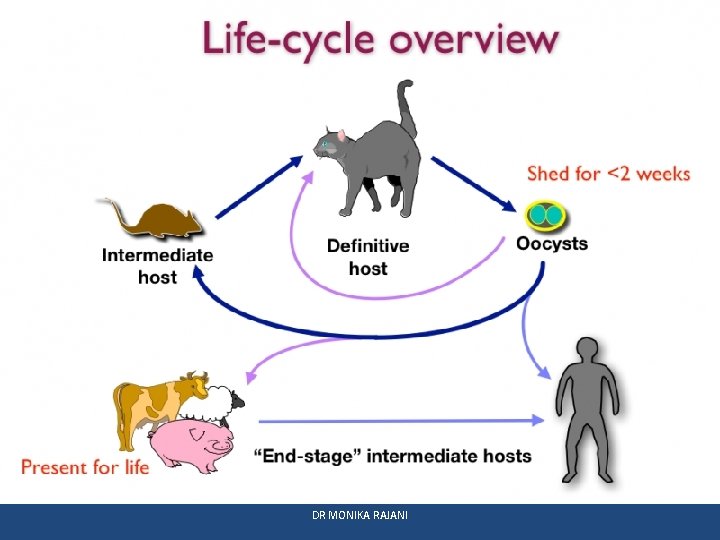
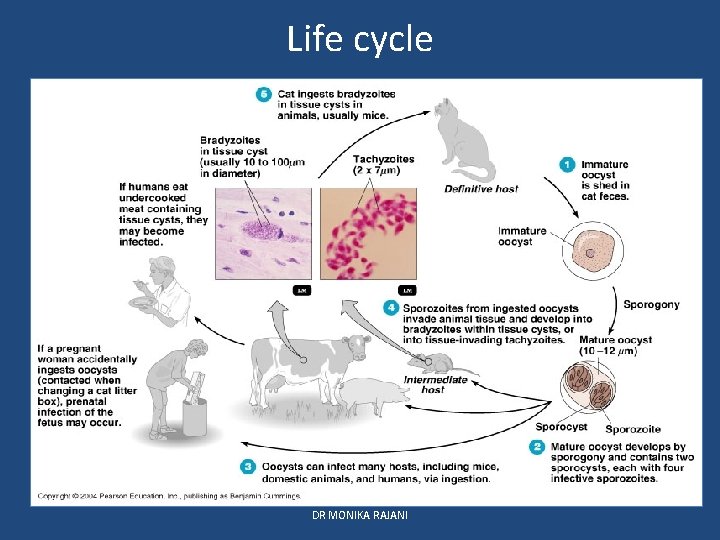
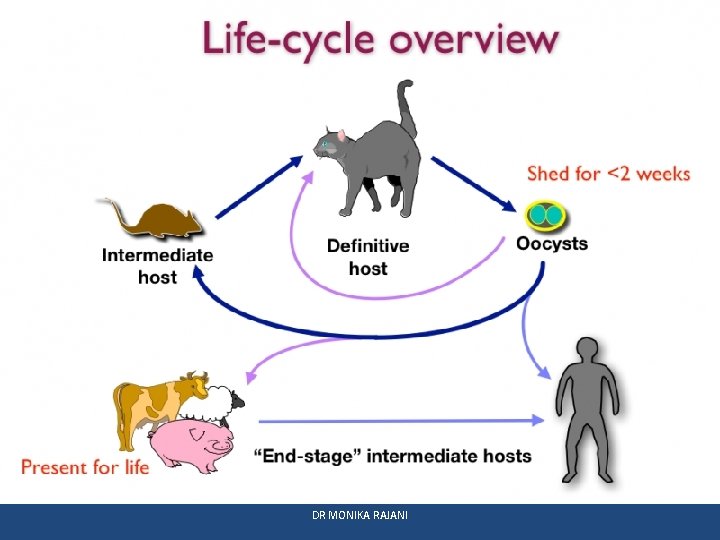
Life cycle • Two hosts required. • Definitive host: cats and other felines : both sexual and asexual cycle takes place. : three morphological forms are seen. • Intermediate host: man and other mammmals-mice, rats sheep, cattle pigs. : Only asexual cycle occurs. : Only trophozoites and tissue cysts are seen. • Natural cycle occurs in mice and cats. • Mice acquire infection by eating materials contaminated with cats feces containing oocysts. • Two types of cycle: e nteric cycle and exo enteric cycle DR MONIKA RAJANI
DR MONIKA RAJANI
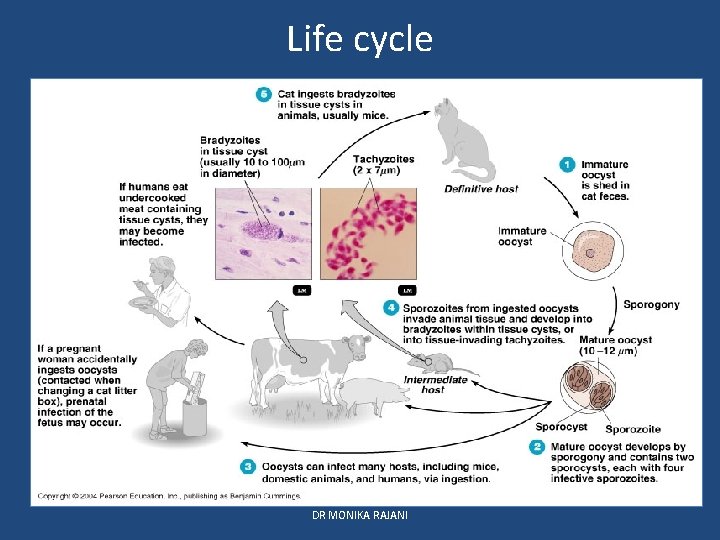
Life cycle DR MONIKA RAJANI
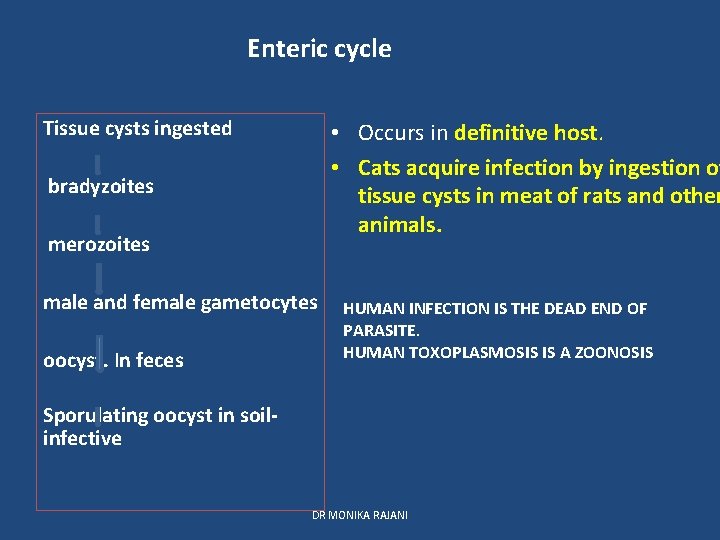
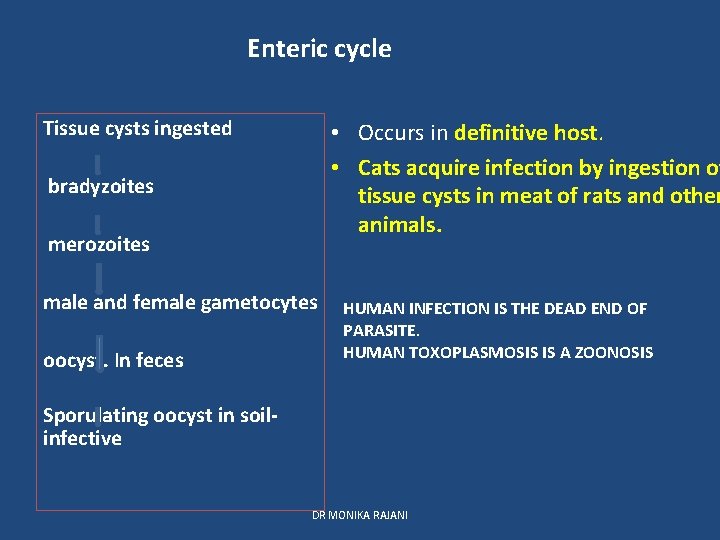
Enteric cycle Tissue cysts ingested • Occurs in definitive host. • Cats acquire infection by ingestion of tissue cysts in meat of rats and other animals. bradyzoites merozoites male and female gametocytes oocyst. In feces HUMAN INFECTION IS THE DEAD END OF PARASITE. HUMAN TOXOPLASMOSIS IS A ZOONOSIS Sporulating oocyst in soilinfective DR MONIKA RAJANI
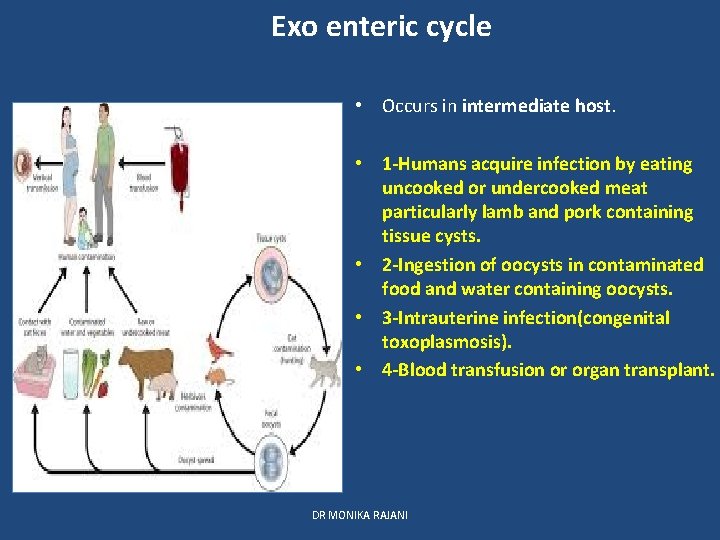
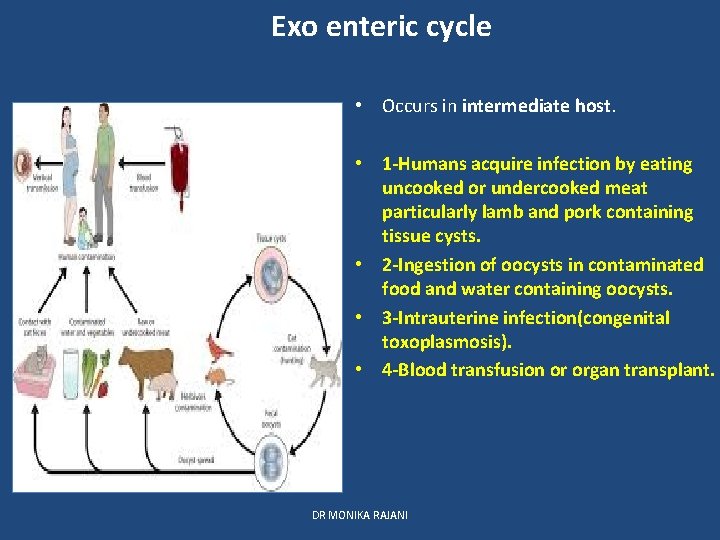
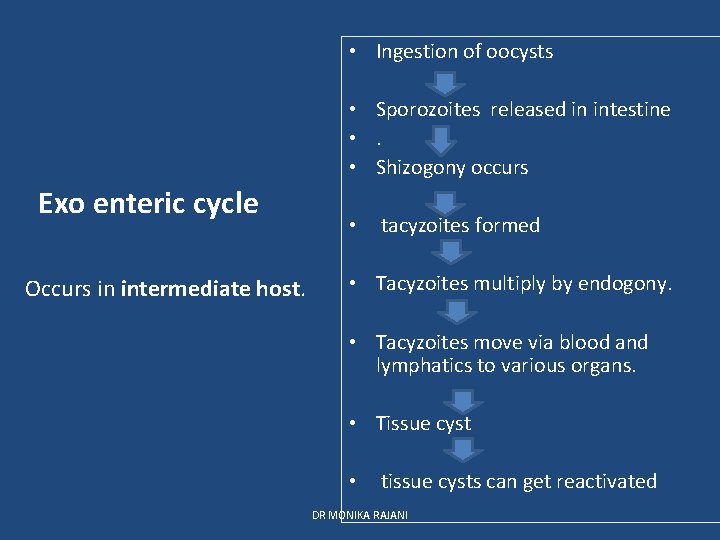
Exo enteric cycle • Occurs in intermediate host. • 1 -Humans acquire infection by eating uncooked or undercooked meat particularly lamb and pork containing tissue cysts. • 2 -Ingestion of oocysts in contaminated food and water containing oocysts. • 3 -Intrauterine infection(congenital toxoplasmosis). • 4 -Blood transfusion or organ transplant. DR MONIKA RAJANI
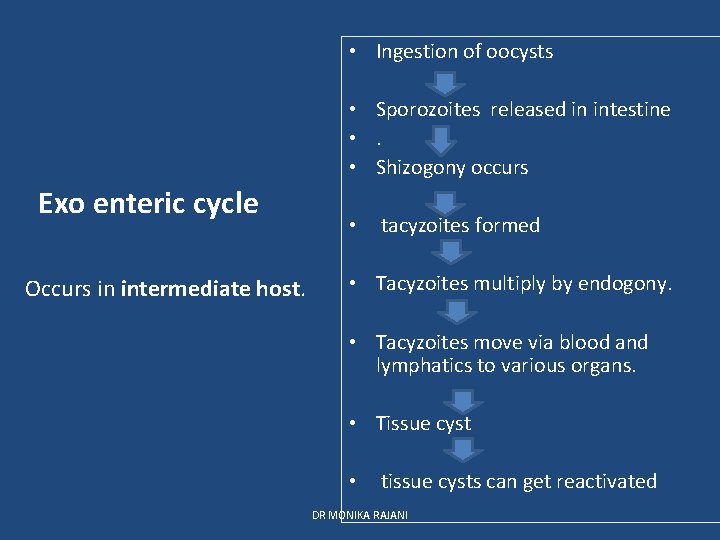
• Ingestion of oocysts • Sporozoites released in intestine • . • Shizogony occurs Exo enteric cycle Occurs in intermediate host. • tacyzoites formed • Tacyzoites multiply by endogony. • Tacyzoites move via blood and lymphatics to various organs. • Tissue cyst • tissue cysts can get reactivated DR MONIKA RAJANI
Pathogenicity and clinical features • Most human infections are asymptomatic. • Active progression of disease is seen in immunodeficient and HIV pts. • Clinical toxoplasmosis: congenital toxoplasmosis : Acquired toxoplasmosis. DR MONIKA RAJANI
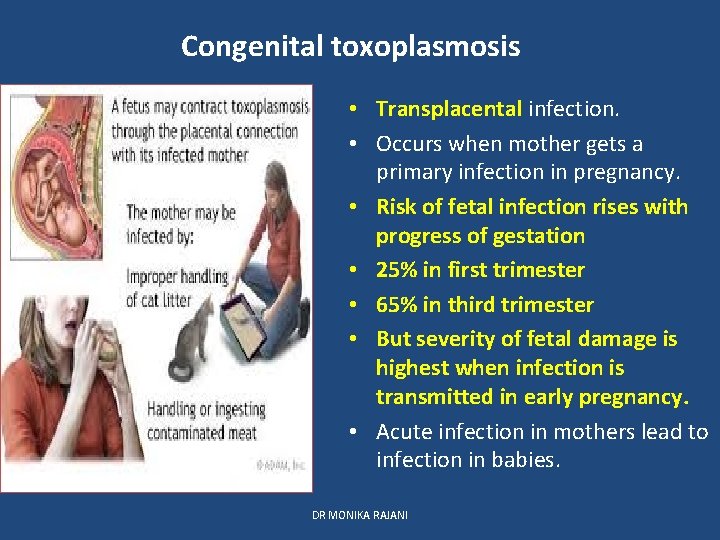
Congenital toxoplasmosis • Transplacental infection. • Occurs when mother gets a primary infection in pregnancy. • Risk of fetal infection rises with progress of gestation • 25% in first trimester • 65% in third trimester • But severity of fetal damage is highest when infection is transmitted in early pregnancy. • Acute infection in mothers lead to infection in babies. DR MONIKA RAJANI
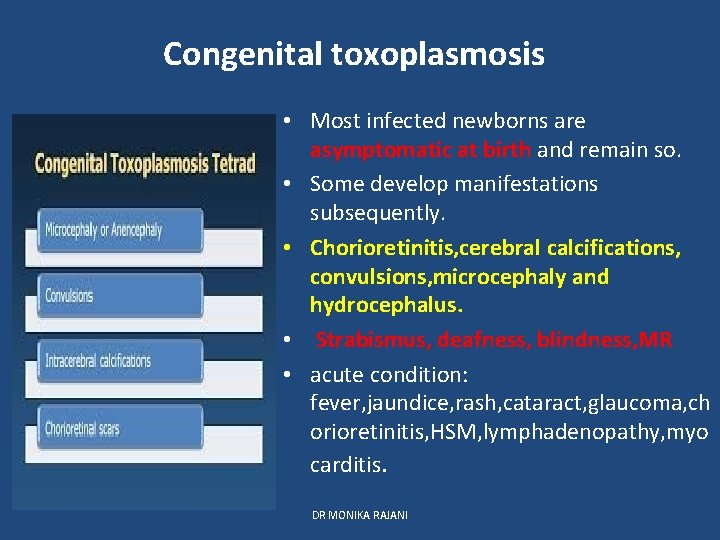
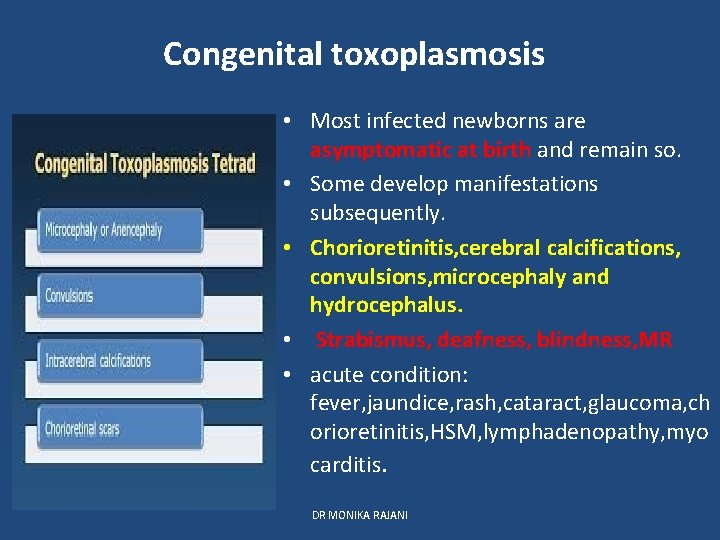
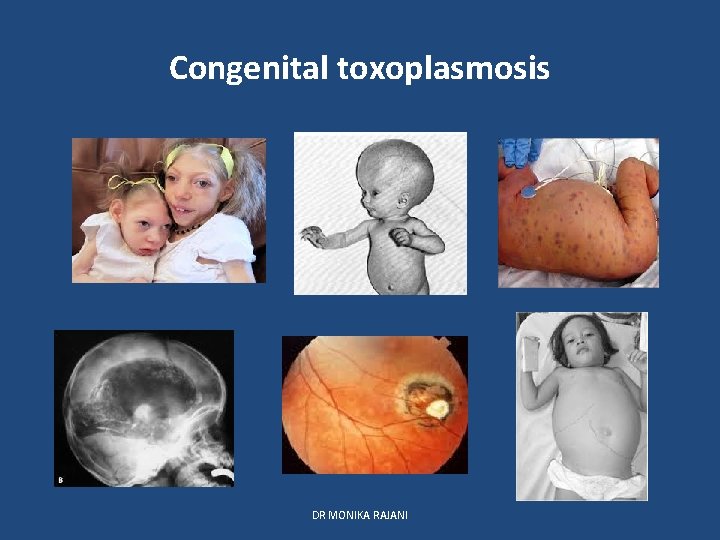
Congenital toxoplasmosis • Most infected newborns are asymptomatic at birth and remain so. • Some develop manifestations subsequently. • Chorioretinitis, cerebral calcifications, convulsions, microcephaly and hydrocephalus. • Strabismus, deafness, blindness, MR • acute condition: fever, jaundice, rash, cataract, glaucoma, ch orioretinitis, HSM, lymphadenopathy, myo carditis. DR MONIKA RAJANI
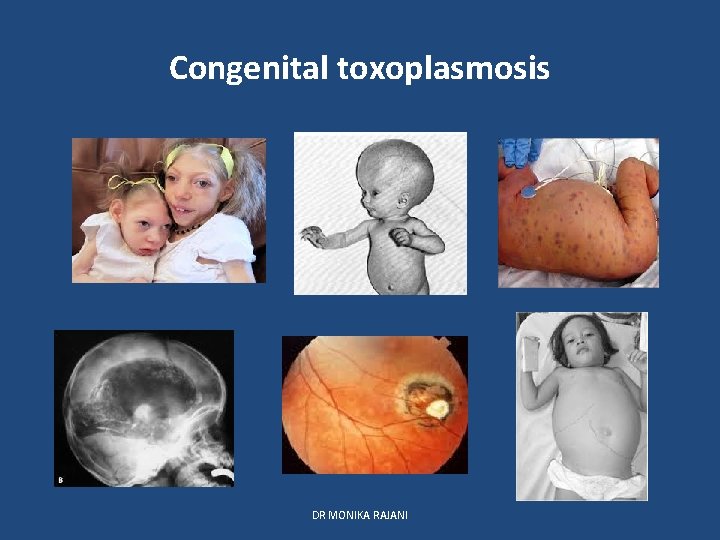
Congenital toxoplasmosis DR MONIKA RAJANI
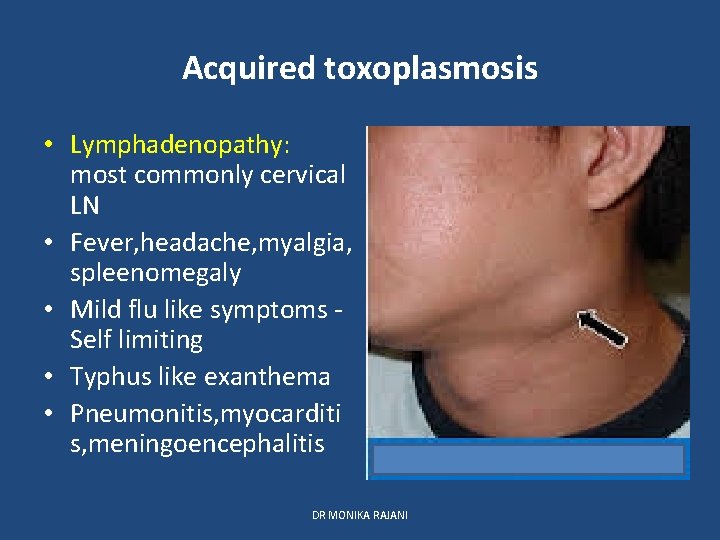
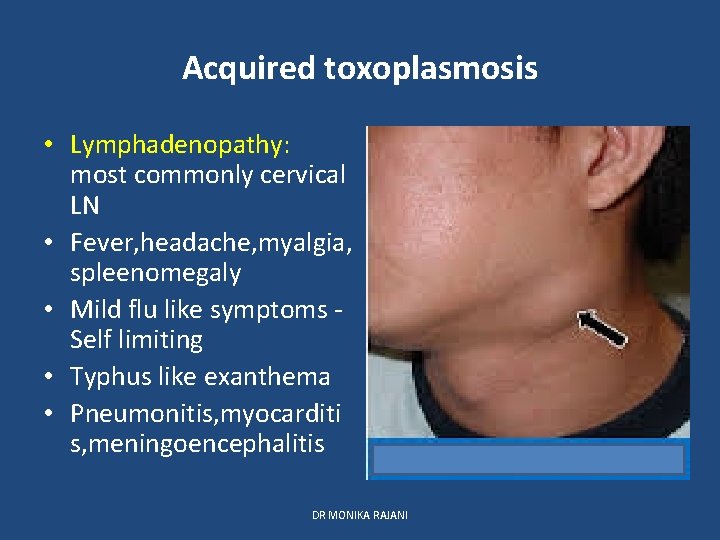
Acquired toxoplasmosis • Lymphadenopathy: most commonly cervical LN • Fever, headache, myalgia, spleenomegaly • Mild flu like symptoms Self limiting • Typhus like exanthema • Pneumonitis, myocarditi s, meningoencephalitis DR MONIKA RAJANI
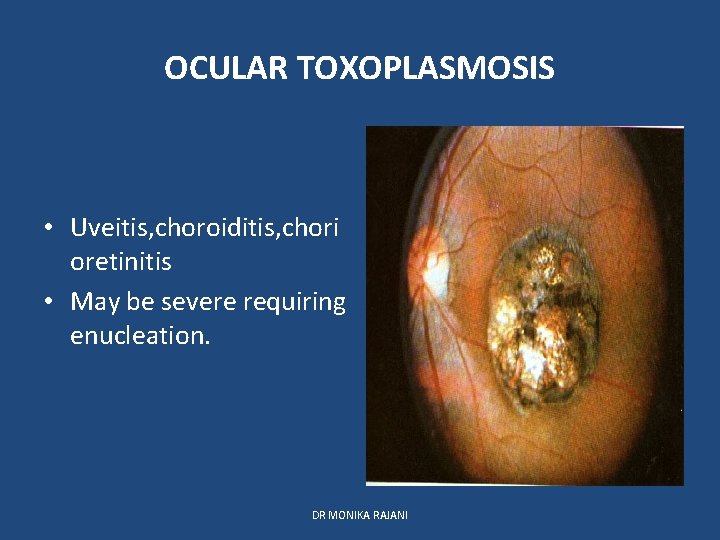
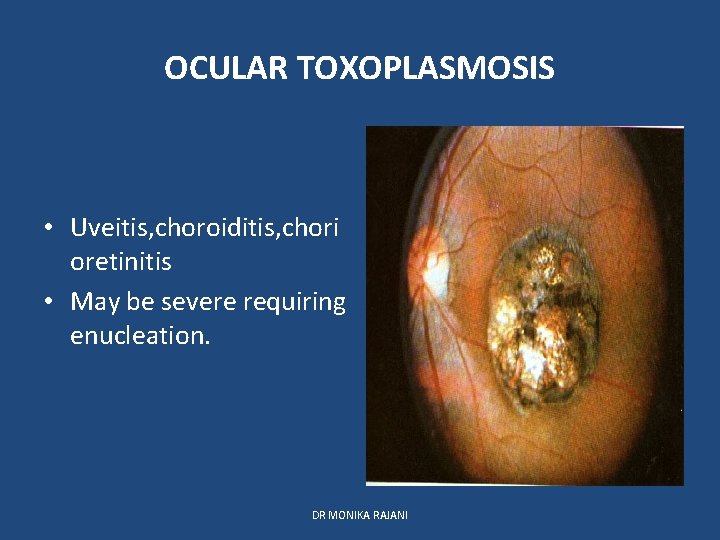
OCULAR TOXOPLASMOSIS • Uveitis, choroiditis, chori oretinitis • May be severe requiring enucleation. DR MONIKA RAJANI
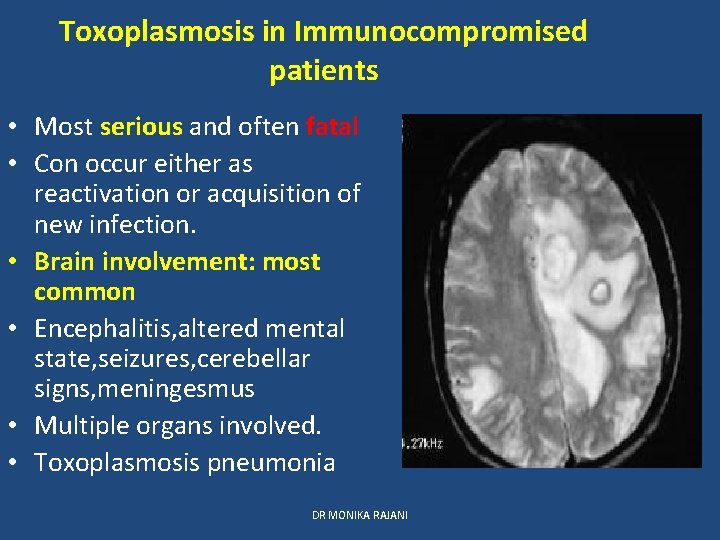
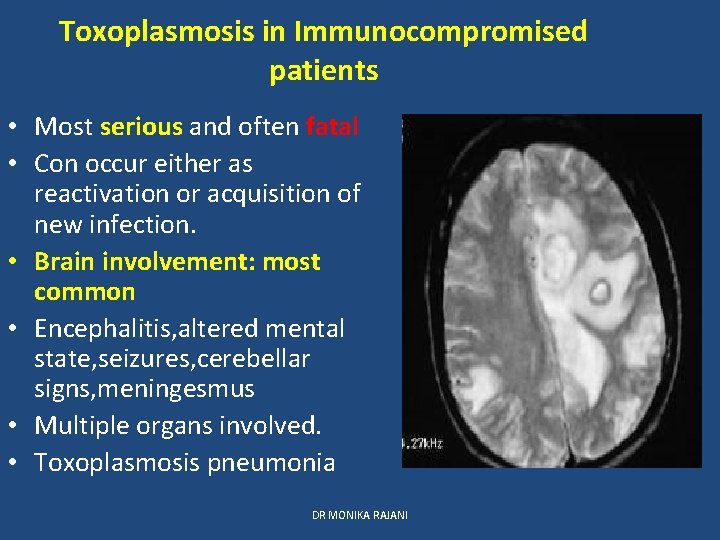
Toxoplasmosis in Immunocompromised patients • Most serious and often fatal • Con occur either as reactivation or acquisition of new infection. • Brain involvement: most common • Encephalitis, altered mental state, seizures, cerebellar signs, meningesmus • Multiple organs involved. • Toxoplasmosis pneumonia DR MONIKA RAJANI
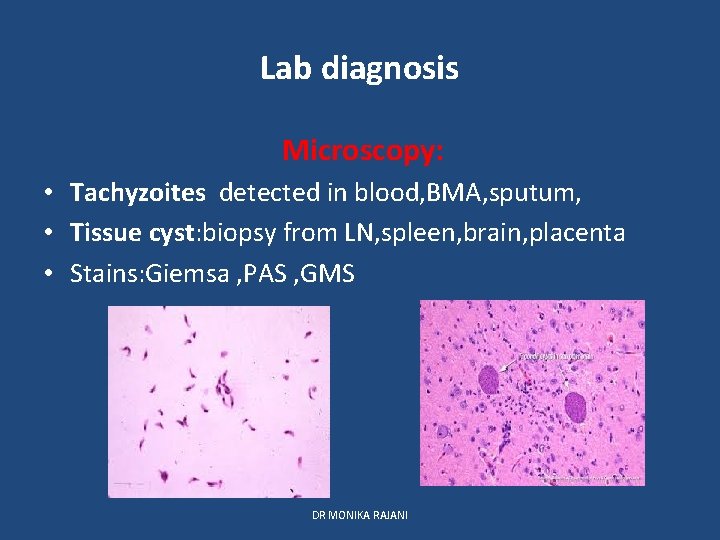
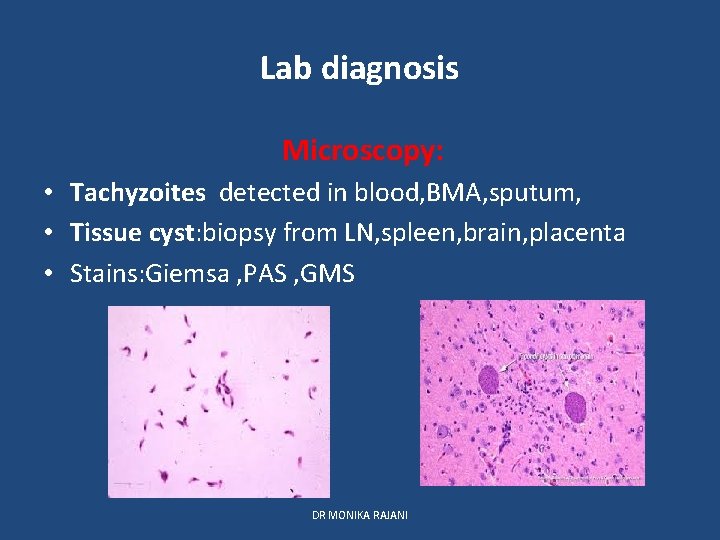
Lab diagnosis Microscopy: • Tachyzoites detected in blood, BMA, sputum, • Tissue cyst: biopsy from LN, spleen, brain, placenta • Stains: Giemsa , PAS , GMS DR MONIKA RAJANI
Lab diagnosis: Animal inoculation • By inoculating blood, BF or tissue specimens • Intraperitonial inoculation in mice or tissue culture. • Mice examined for Toxoplasma in peritonial exudate after 7 -10 days. DR MONIKA RAJANI
Serology • Main stay of diagnosis • Antibody detection • Ig. G : after 2 -3 weeks : By ELISA, IFAT , LA : indicates past infection : Sabin Feldman Dye Test • Ig. M : Indicates early primary infection : Congenital infection : By double sandwich Ig. M ELISA • Ig G avidity test: for recent infection DR MONIKA RAJANI
Serology • • • Antigen detection By ELISA Indicates recent toxoplasma infection Detected in blood and BF Detection of antigen in amniotic fluid is used to diagnose congenital toxoplasmosis DR MONIKA RAJANI
Skin test of Frenkel • Diluted toxoplasmin is injected intradermally • Delayed hypersenstivity reaction is seen. • Not very reliable for diagnosis DR MONIKA RAJANI
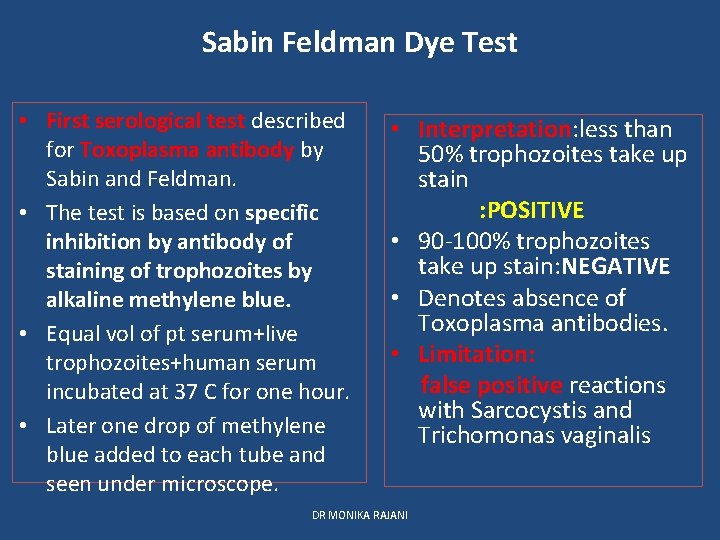
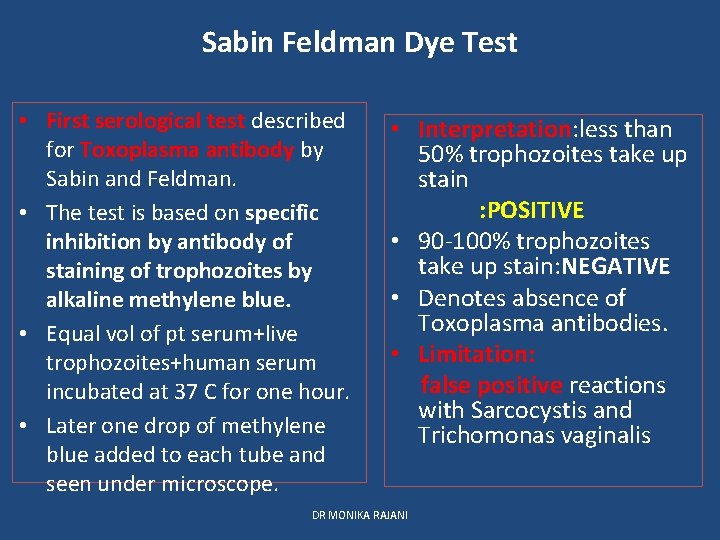
Sabin Feldman Dye Test • First serological test described for Toxoplasma antibody by Sabin and Feldman. • The test is based on specific inhibition by antibody of staining of trophozoites by alkaline methylene blue. • Equal vol of pt serum+live trophozoites+human serum incubated at 37 C for one hour. • Later one drop of methylene blue added to each tube and seen under microscope. • Interpretation: less than 50% trophozoites take up stain : POSITIVE • 90 -100% trophozoites take up stain: NEGATIVE • Denotes absence of Toxoplasma antibodies. • Limitation: false positive reactions with Sarcocystis and Trichomonas vaginalis DR MONIKA RAJANI
Molecular tests • PCR • DNA hybridisation technique DR MONIKA RAJANI
Imaging • In case of CNS involvement: CT scan : MRI • USG of fetus in utero at 20 -24 weeks of pregnancy is useful for diagnosis of congenital toxoplasmosis. DR MONIKA RAJANI
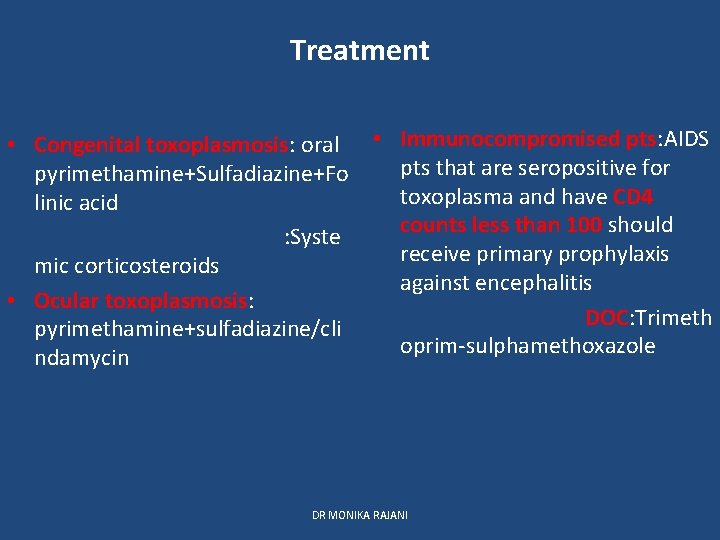
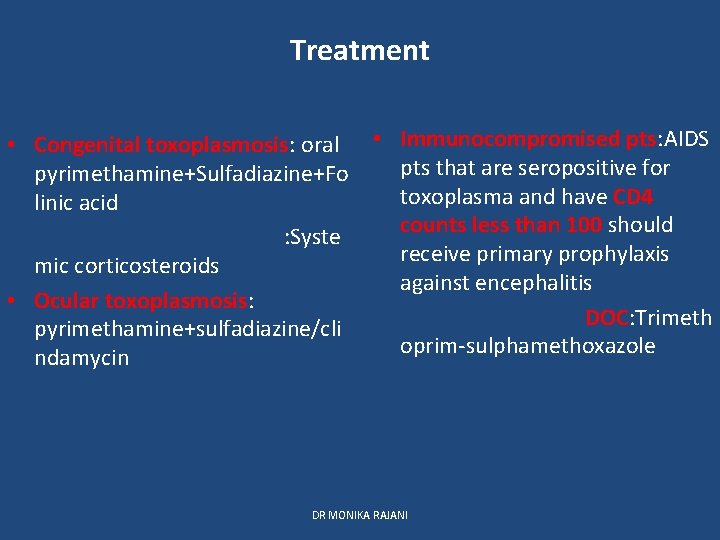
Treatment • Congenital toxoplasmosis: oral pyrimethamine+Sulfadiazine+Fo linic acid : Syste mic corticosteroids • Ocular toxoplasmosis: pyrimethamine+sulfadiazine/cli ndamycin • Immunocompromised pts: AIDS pts that are seropositive for toxoplasma and have CD 4 counts less than 100 should receive primary prophylaxis against encephalitis DOC: Trimeth oprim-sulphamethoxazole DR MONIKA RAJANI
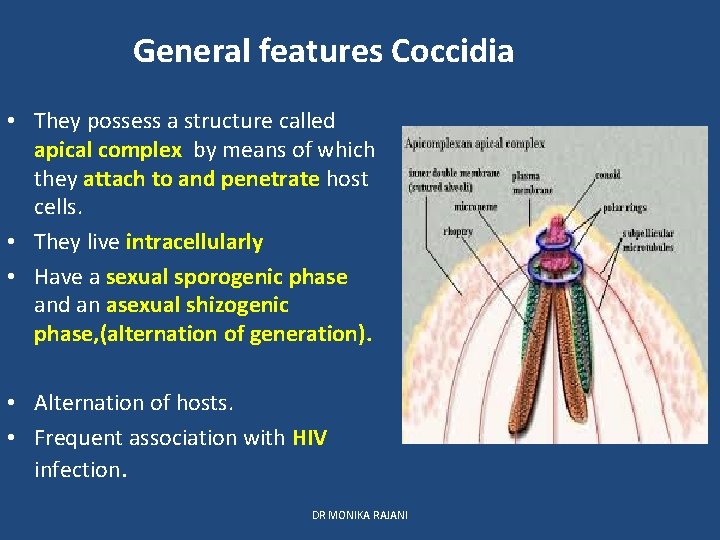
Prophylaxis • Individuals at risk should avoid contact with cat and its feces. • Proper cooking of meal • Proper washing of hands , fruits and vegetables before cooking and eating • Screening of blood before transfusion • Organ safety • No vaccine available for humans DR MONIKA RAJANI
THANK YOU DR MONIKA RAJANI
 Toxoplasma giemsa stain
Toxoplasma giemsa stain Taquizoitos de toxoplasma gondii
Taquizoitos de toxoplasma gondii Estructuras
Estructuras Toxoplasma gondii
Toxoplasma gondii Toxoplasma gondii bradyzoites
Toxoplasma gondii bradyzoites Sub reino protozoa
Sub reino protozoa Toxoplasma gondii familia
Toxoplasma gondii familia Promotion from associate professor to professor
Promotion from associate professor to professor Rajani shenoy
Rajani shenoy T gondii
T gondii Toxoplasma intermediate host
Toxoplasma intermediate host Albany county dss
Albany county dss Nebraska dept of agriculture
Nebraska dept of agriculture Dept of education
Dept of education Gome dept
Gome dept Dept. name of organization (of affiliation)
Dept. name of organization (of affiliation) La dept of revenue
La dept of revenue Dept a
Dept a Dept of education
Dept of education Gome dept
Gome dept Fl dept of agriculture
Fl dept of agriculture Dept. name of organization
Dept. name of organization Ee dept iitb
Ee dept iitb Dept c13 nmr
Dept c13 nmr Hoe dept
Hoe dept Ohio dept of developmental disabilities
Ohio dept of developmental disabilities Geaux biz login
Geaux biz login Central islip fire dept
Central islip fire dept Gome dept
Gome dept Mn dept of education
Mn dept of education Organizational structure of finance department
Organizational structure of finance department Dept ind onegov
Dept ind onegov Pt dept logistik
Pt dept logistik Florida dept of agriculture and consumer services
Florida dept of agriculture and consumer services