The Pancreatic Islets Morphology of the Endocrine Pancreas
- Slides: 18
The Pancreatic Islets
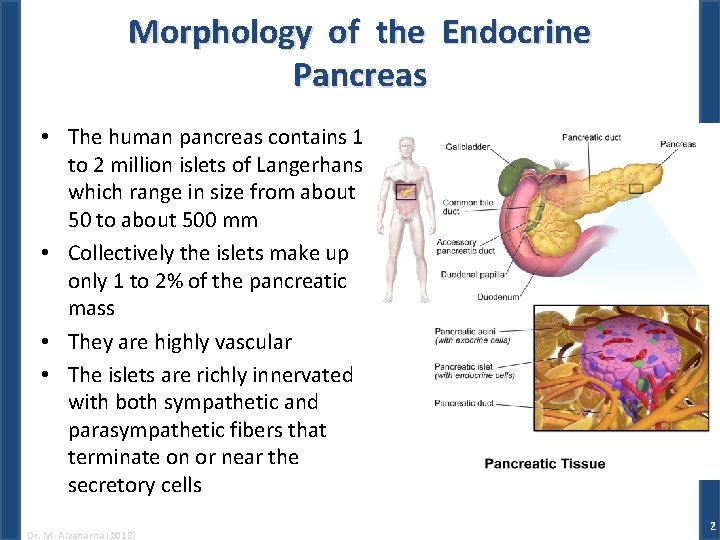
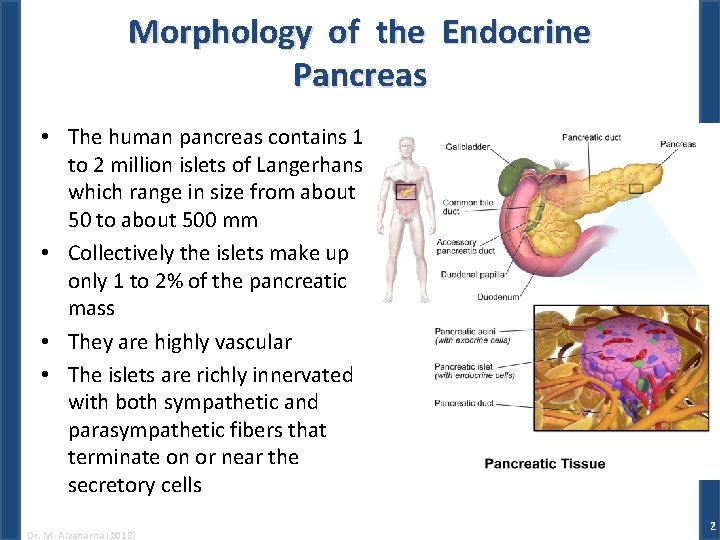
Morphology of the Endocrine Pancreas • The human pancreas contains 1 to 2 million islets of Langerhans which range in size from about 50 to about 500 mm • Collectively the islets make up only 1 to 2% of the pancreatic mass • They are highly vascular • The islets are richly innervated with both sympathetic and parasympathetic fibers that terminate on or near the secretory cells Dr. M. Alzaharna (2018) 2
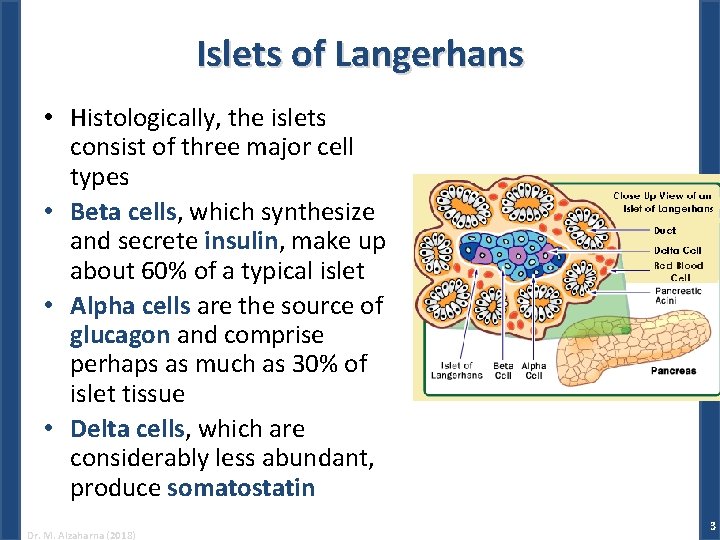
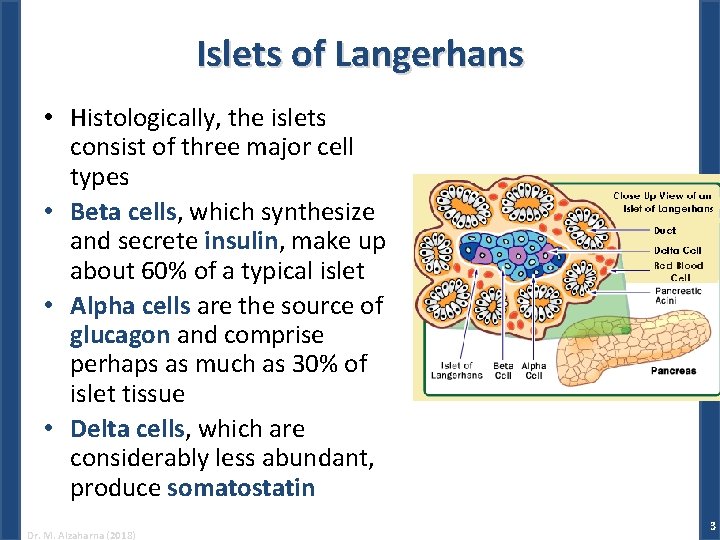
Islets of Langerhans • Histologically, the islets consist of three major cell types • Beta cells, which synthesize and secrete insulin, make up about 60% of a typical islet • Alpha cells are the source of glucagon and comprise perhaps as much as 30% of islet tissue • Delta cells, which are considerably less abundant, produce somatostatin Dr. M. Alzaharna (2018) 3
Glucagon • Glucagon is a simple unbranched peptide chain that consists of 29 amino acids • Glucagon is packaged, stored in membrane-bound granules, and secreted by exocytosis like other peptide hormones • It circulates without binding to carrier proteins and has a half-life in blood of about 5 minutes • Glucagon degradation: – 25% is destroyed during passage through the liver – The kidney is another important site of degradation – and a considerable fraction of circulating glucagon is destroyed by plasma peptidases Dr. M. Alzaharna (2018) 4
Physiological Actions of Glucagon • The physiological role of glucagon is to stimulate hepatic production and secretion of glucose and to a lesser extent, ketone bodies (which are derived from fatty acids) • Glucagon stimulates the liver to release glucose and produces a rapid increase in blood glucose concentration • Glucose that is released from the liver is obtained from: – breakdown of stored glycogen (glycogenolysis) – and new synthesis (gluconeogenesis) Dr. M. Alzaharna (2018) 5
Physiological Actions of Glucagon • All the effects of glucagon appear to be mediated by c. AMP • c. AMP results in: – phosphorylation of enzymes, • which increase or decrease their activity, – or phosphorylation of transcription factors • CREB (c. AMP response element-binding protein) which usually increases transcription of target genes Dr. M. Alzaharna (2018) 6
Glucose Production • Increase in hepatic glycogenolysis and gluconeogenesis leading to increase glucose production and release into the blood • Increase in lipolysis and mobilization of fatty acids (from triglycerides), resulting in increased levels of circulating ketoacids • Regulation is achieved both by: – modulating the activity of enzymes already present in cells • requires only seconds • By cofactors • phosphorylation and dephosphorylation – and by increasing or decreasing rates of enzyme synthesis and therefore the amounts of enzyme molecules • requires minutes or even hours Dr. M. Alzaharna (2018) 7
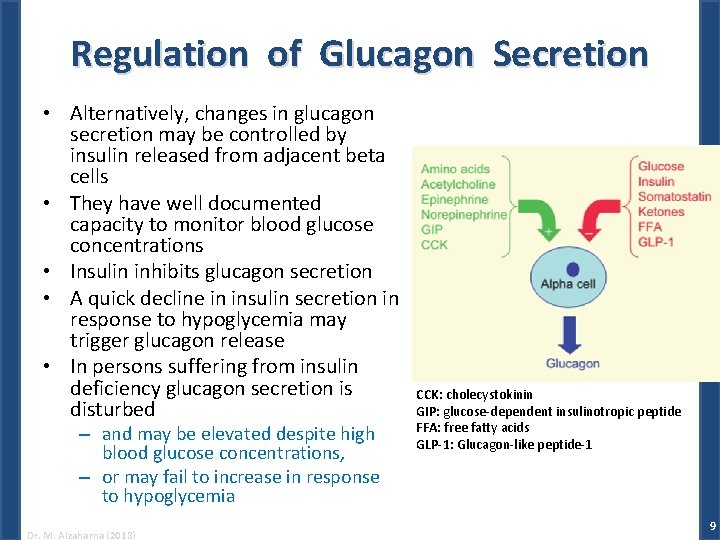
Regulation of Glucagon Secretion • The concentration of glucose in blood is the most important determinant of glucagon secretion in normal individuals – When the plasma glucose concentration exceeds 200 mg/d. L, glucagon secretion is maximally inhibited – Inhibitory effects of glucose are proportionately less at lower concentrations – and disappear when its concentration falls below 50 mg/d. L • Alpha cells can respond to fluctuations in blood glucose with either an increase or a decrease in glucagon output Dr. M. Alzaharna (2018) 8
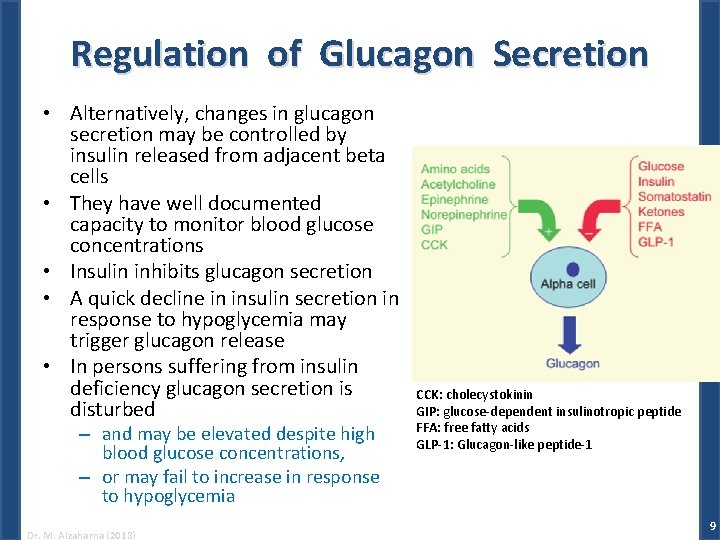
Regulation of Glucagon Secretion • Alternatively, changes in glucagon secretion may be controlled by insulin released from adjacent beta cells • They have well documented capacity to monitor blood glucose concentrations • Insulin inhibits glucagon secretion • A quick decline in insulin secretion in response to hypoglycemia may trigger glucagon release • In persons suffering from insulin deficiency glucagon secretion is disturbed – and may be elevated despite high blood glucose concentrations, – or may fail to increase in response to hypoglycemia Dr. M. Alzaharna (2018) CCK: cholecystokinin GIP: glucose-dependent insulinotropic peptide FFA: free fatty acids GLP-1: Glucagon-like peptide-1 9
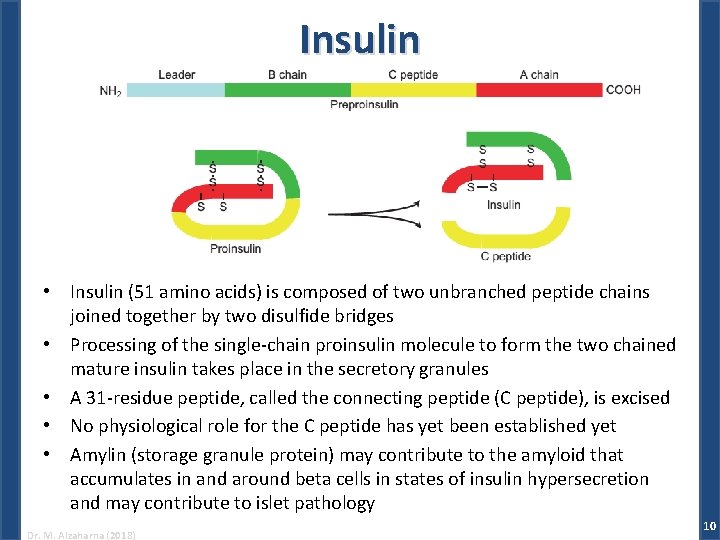
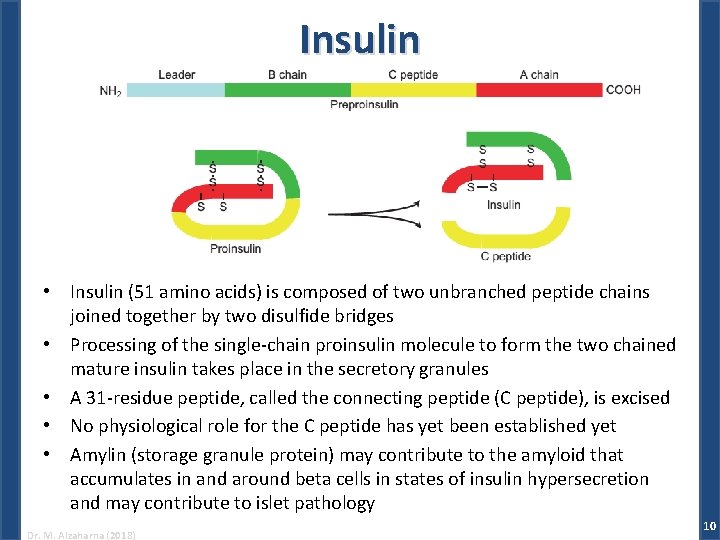
Insulin • Insulin (51 amino acids) is composed of two unbranched peptide chains joined together by two disulfide bridges • Processing of the single-chain proinsulin molecule to form the two chained mature insulin takes place in the secretory granules • A 31 -residue peptide, called the connecting peptide (C peptide), is excised • No physiological role for the C peptide has yet been established yet • Amylin (storage granule protein) may contribute to the amyloid that accumulates in and around beta cells in states of insulin hypersecretion and may contribute to islet pathology Dr. M. Alzaharna (2018) 10
Insulin • Insulin is cleared rapidly from the circulation with a half-life of four to six minutes • The first step in insulin degradation is receptor -mediated internalization by an endosomic mechanism • The liver is the principal site of insulin degradation Dr. M. Alzaharna (2018) 11
Physiological Actions of Insulin • Insulin is the only hormone with the ability to directly lower the blood glucose level • Promote the storage of chemical energy derived from food in the form of glycogen, proteins and lipids • While suppressing the mobilization of stored nutrients • The major target organs for insulin action are consequently: – the liver, muscles and adipose tissue, i. e. organs that are specialized for energy storage Dr. M. Alzaharna (2018) 12
The Principal Effects of Insulin 1. Stimulation of glycogen synthesis in skeletal muscle, liver and adipose tissue 2. Increase in hepatic glucose phosphorylation and a decrease in glucose dephosphorylation 3. Increase in glucose metabolism (glycolysis) with a simultaneous decrease in liver gluconeogenesis Dr. M. Alzaharna (2018) 13
Effects of insulin deficiency – Hyperglycemia • Blood glucose in diabetics may be 300 to 400 mg/d. L – Glycosuria (excretion of glucose in urine) • If blood glucose level exceeds about 180 mg/dl – Polyuria • excessive production of urine – Polydipsia • stimulates thirst – Polyphagia • appetite is increased – Weight loss Dr. M. Alzaharna (2018) 14
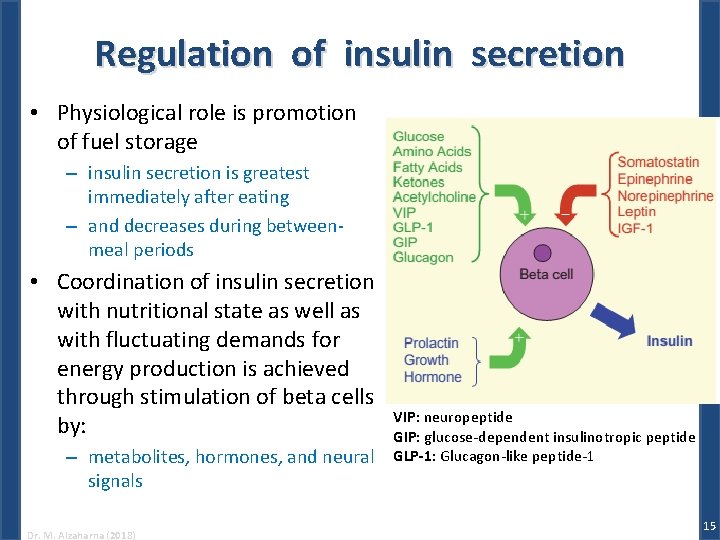
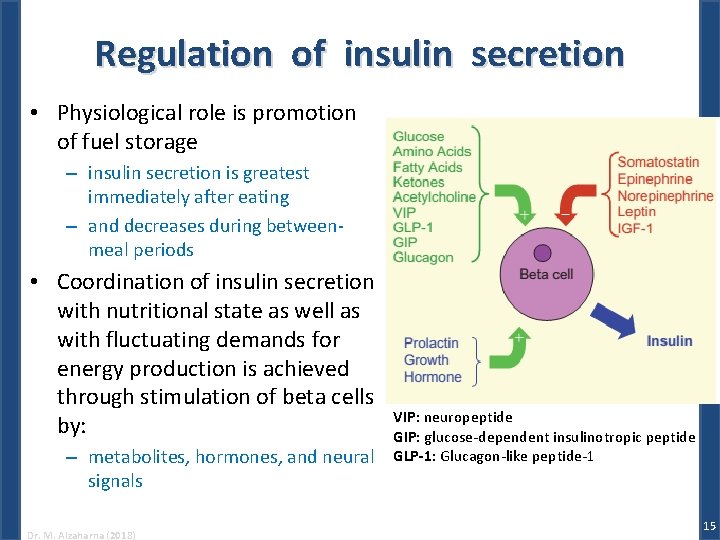
Regulation of insulin secretion • Physiological role is promotion of fuel storage – insulin secretion is greatest immediately after eating – and decreases during betweenmeal periods • Coordination of insulin secretion with nutritional state as well as with fluctuating demands for energy production is achieved through stimulation of beta cells by: – metabolites, hormones, and neural signals Dr. M. Alzaharna (2018) VIP: neuropeptide GIP: glucose-dependent insulinotropic peptide GLP-1: Glucagon-like peptide-1 15
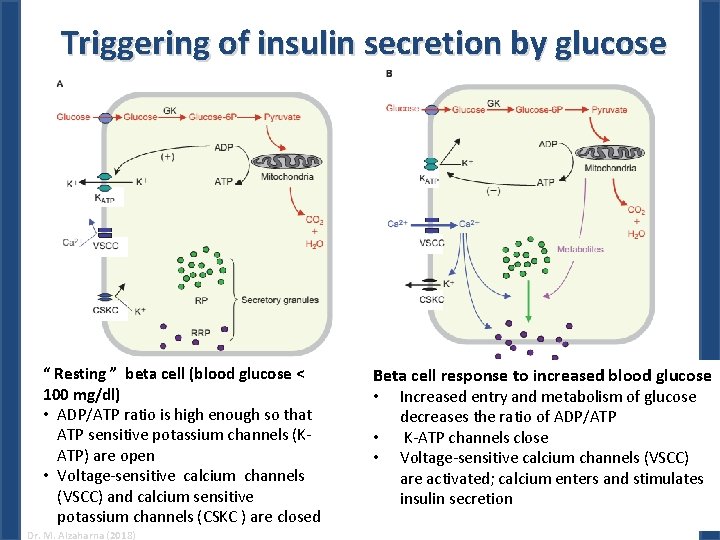
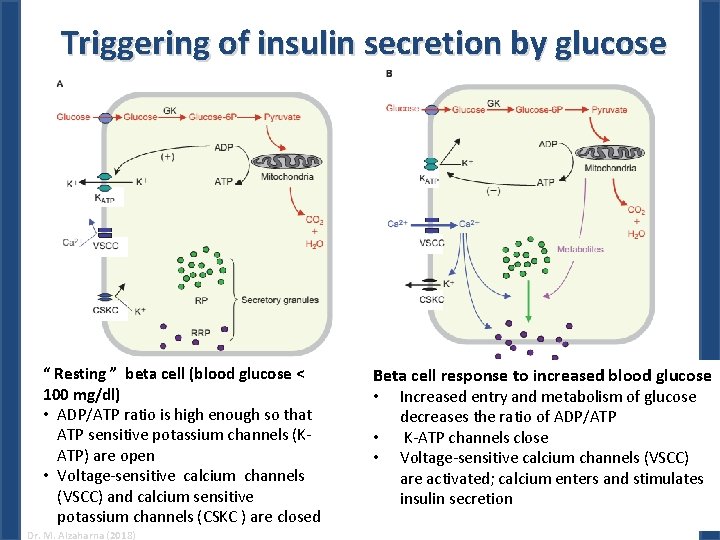
Triggering of insulin secretion by glucose “ Resting ” beta cell (blood glucose < 100 mg/dl) • ADP/ATP ratio is high enough so that ATP sensitive potassium channels (KATP) are open • Voltage-sensitive calcium channels (VSCC) and calcium sensitive potassium channels (CSKC ) are closed Dr. M. Alzaharna (2018) Beta cell response to increased blood glucose • Increased entry and metabolism of glucose • • decreases the ratio of ADP/ATP K-ATP channels close Voltage-sensitive calcium channels (VSCC) are activated; calcium enters and stimulates insulin secretion 16
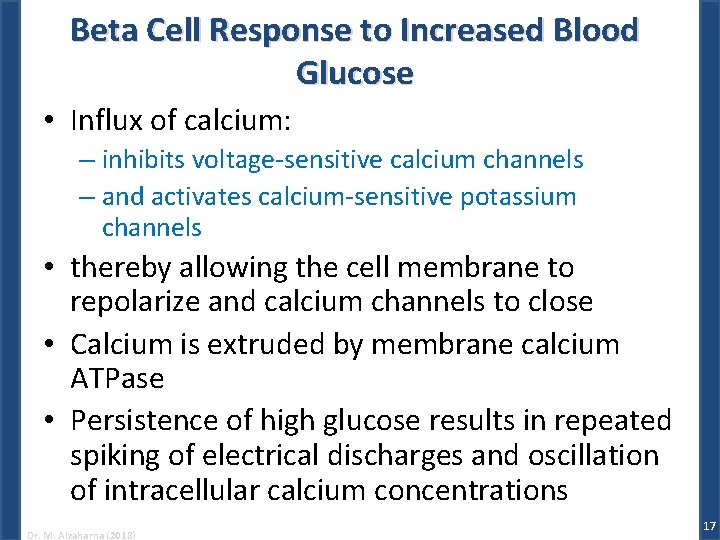
Beta Cell Response to Increased Blood Glucose • Influx of calcium: – inhibits voltage-sensitive calcium channels – and activates calcium-sensitive potassium channels • thereby allowing the cell membrane to repolarize and calcium channels to close • Calcium is extruded by membrane calcium ATPase • Persistence of high glucose results in repeated spiking of electrical discharges and oscillation of intracellular calcium concentrations Dr. M. Alzaharna (2018) 17
Somatostatin • Physiological importance of pancreatic somatostatin is not understood • Its major role may be as a paracrine regulator of insulin and glucagon secretion Dr. M. Alzaharna (2018) 18
 Funzione pancreas
Funzione pancreas Fungiform papillae histology
Fungiform papillae histology Pancreas head body tail
Pancreas head body tail Baylor
Baylor Inflectional morpheme
Inflectional morpheme Absorption
Absorption Pancreatitis pes statement
Pancreatitis pes statement Pancreatic juice
Pancreatic juice Pancreatic juice
Pancreatic juice Function of ruminant stomach
Function of ruminant stomach Daughter mother grandmother pancreatic lesions
Daughter mother grandmother pancreatic lesions Double duct sign
Double duct sign Structure of nucleolus
Structure of nucleolus Digestion of carbohydrates ppt
Digestion of carbohydrates ppt Hydrohepatosis
Hydrohepatosis Pancreatic calcification
Pancreatic calcification Content of pancreatic juice
Content of pancreatic juice Ranson
Ranson The main jobs of the large intestine are _____.
The main jobs of the large intestine are _____.