Six Sigma at Academic Medical Hospital The following
- Slides: 14
Six Sigma at Academic Medical Hospital The following presentation was developed by Jane Mc. Crea, Black Belt of the ED Wait Time Project at Academic Medical Hospital. The presentation follows the DMAIC methodology.
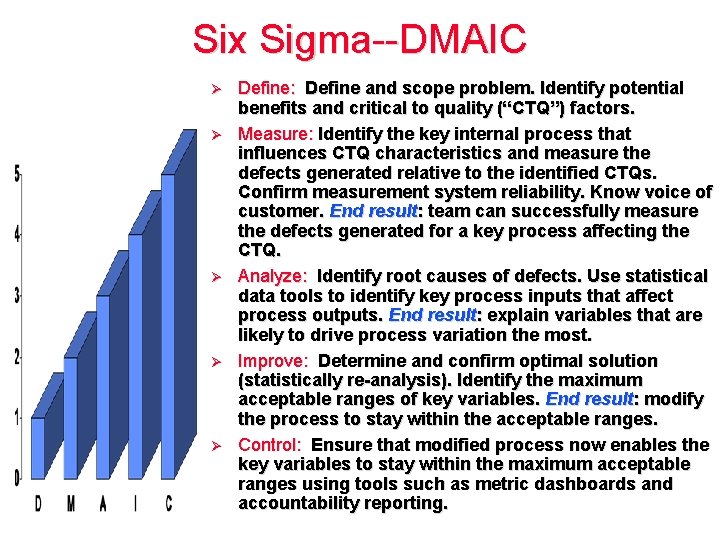
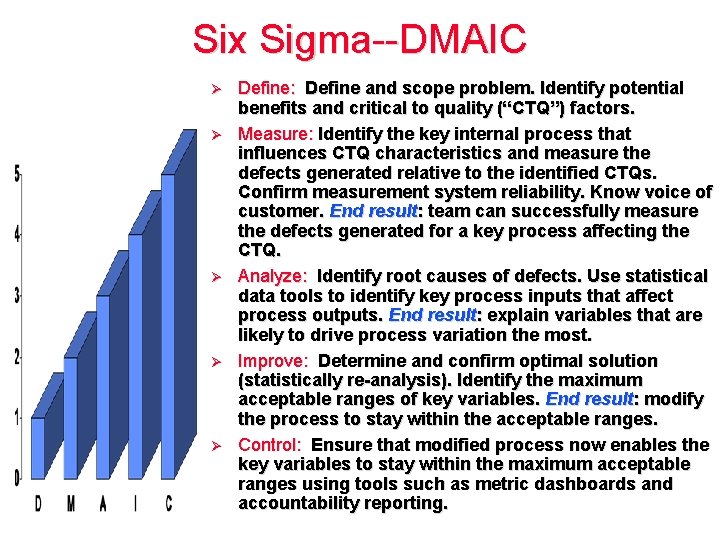
Six Sigma--DMAIC Ø Ø Ø Define: Define and scope problem. Identify potential benefits and critical to quality (“CTQ”) factors. Measure: Identify the key internal process that influences CTQ characteristics and measure the defects generated relative to the identified CTQs. Confirm measurement system reliability. Know voice of customer. End result: team can successfully measure the defects generated for a key process affecting the CTQ. Analyze: Identify root causes of defects. Use statistical data tools to identify key process inputs that affect process outputs. End result: explain variables that are likely to drive process variation the most. Improve: Determine and confirm optimal solution (statistically re-analysis). Identify the maximum acceptable ranges of key variables. End result: modify the process to stay within the acceptable ranges. Control: Ensure that modified process now enables the key variables to stay within the maximum acceptable ranges using tools such as metric dashboards and accountability reporting.
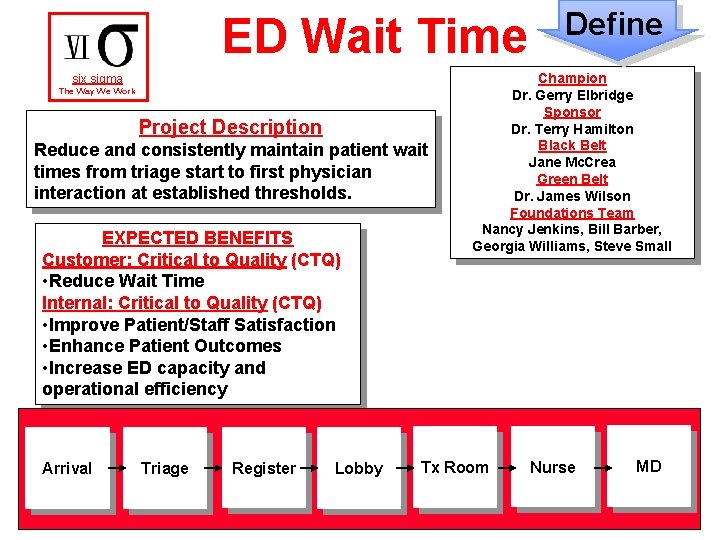
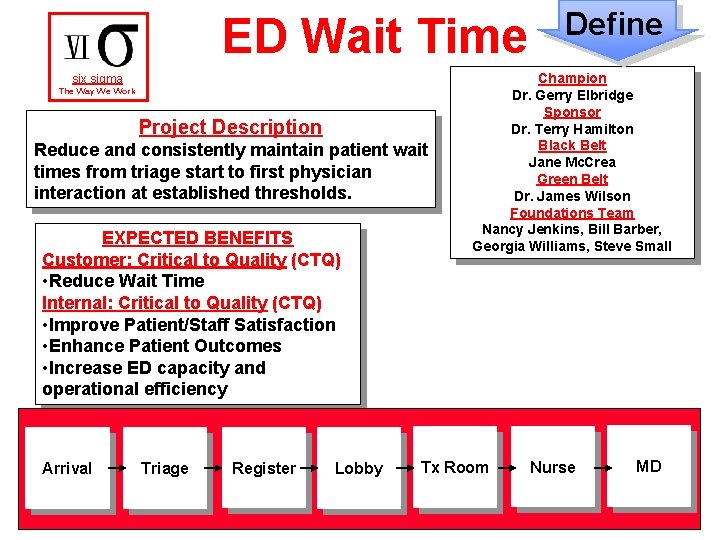
ED Wait Time six sigma The Way We Work Project Description Reduce and consistently maintain patient wait times from triage start to first physician interaction at established thresholds. EXPECTED BENEFITS Customer: Critical to Quality (CTQ) • Reduce Wait Time Internal: Critical to Quality (CTQ) • Improve Patient/Staff Satisfaction • Enhance Patient Outcomes • Increase ED capacity and operational efficiency Arrival Triage Register Lobby Define Champion Dr. Gerry Elbridge Sponsor Dr. Terry Hamilton Black Belt Jane Mc. Crea Green Belt Dr. James Wilson Foundations Team Nancy Jenkins, Bill Barber, Georgia Williams, Steve Small Tx Room Nurse MD
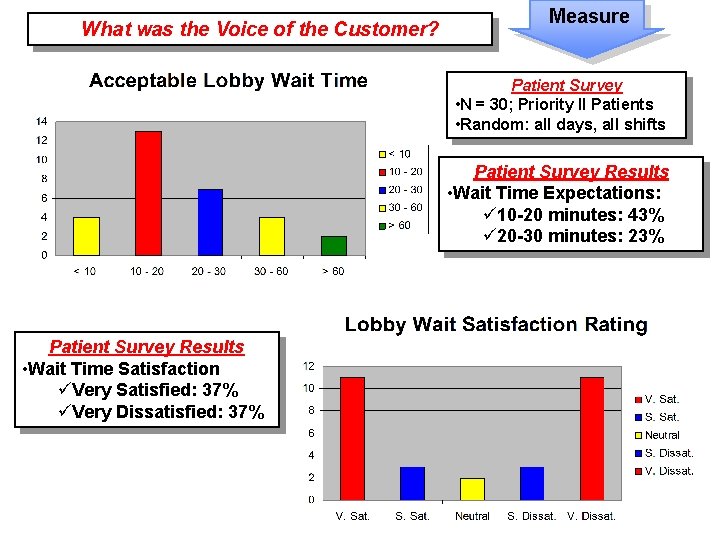
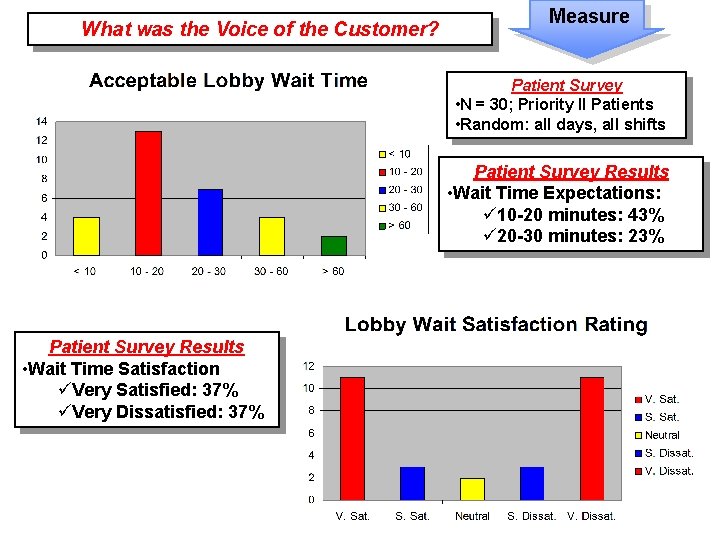
What was the Voice of the Customer? Measure Patient Survey • N = 30; Priority II Patients • Random: all days, all shifts Patient Survey Results • Wait Time Expectations: ü 10 -20 minutes: 43% ü 20 -30 minutes: 23% Patient Survey Results • Wait Time Satisfaction üVery Satisfied: 37% üVery Dissatisfied: 37%
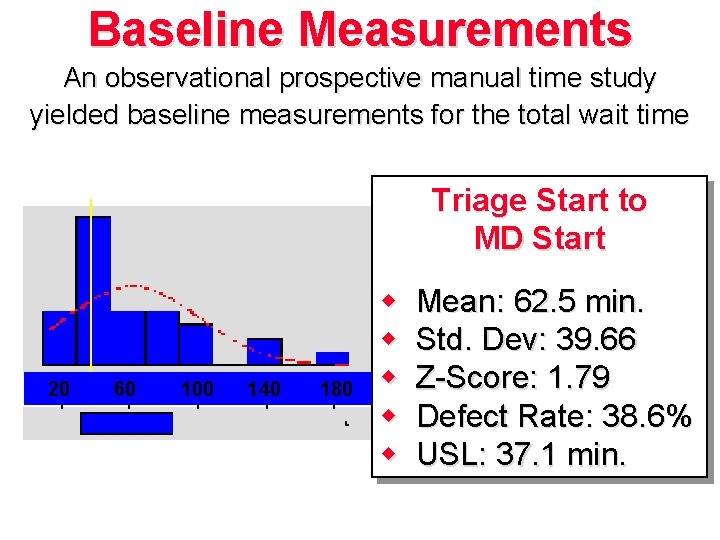
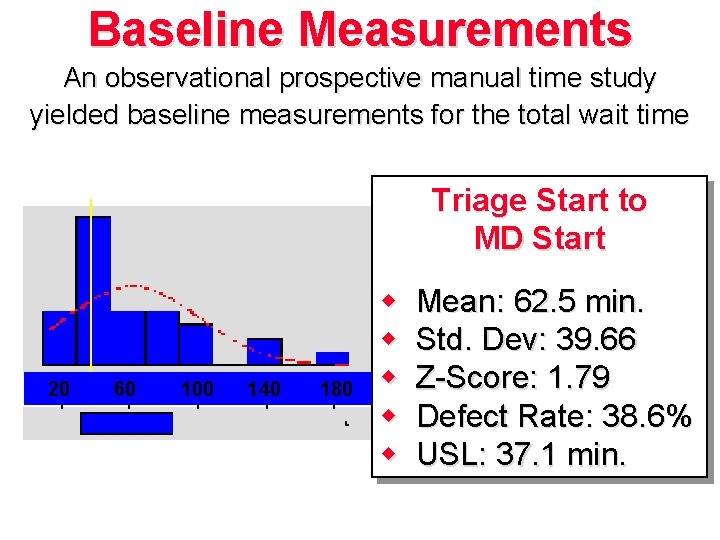
Baseline Measurements An observational prospective manual time study yielded baseline measurements for the total wait time Triage Start to MD Start 20 60 100 140 180 w Mean: 62. 5 min. w Std. Dev: 39. 66 w Z-Score: 1. 79 w Defect Rate: 38. 6% w USL: 37. 1 min.
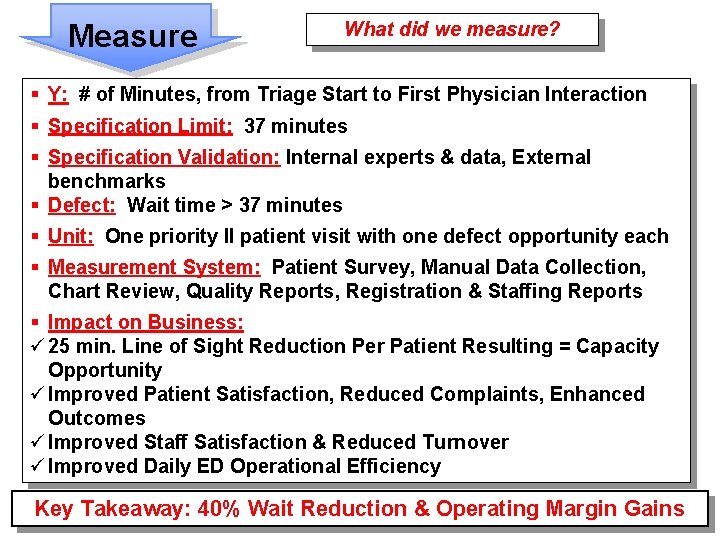
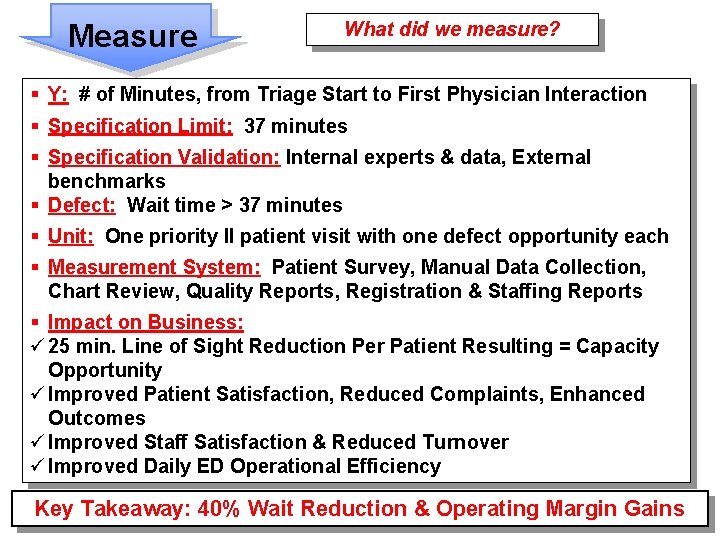
Measure What did we measure? § Y: # of Minutes, from Triage Start to First Physician Interaction § Specification Limit: 37 minutes § Specification Validation: Internal experts & data, External benchmarks § Defect: Wait time > 37 minutes § Unit: One priority II patient visit with one defect opportunity each § Measurement System: Patient Survey, Manual Data Collection, Chart Review, Quality Reports, Registration & Staffing Reports § Impact on Business: ü 25 min. Line of Sight Reduction Per Patient Resulting = Capacity Opportunity ü Improved Patient Satisfaction, Reduced Complaints, Enhanced Outcomes ü Improved Staff Satisfaction & Reduced Turnover ü Improved Daily ED Operational Efficiency Key Takeaway: 40% Wait Reduction & Operating Margin Gains
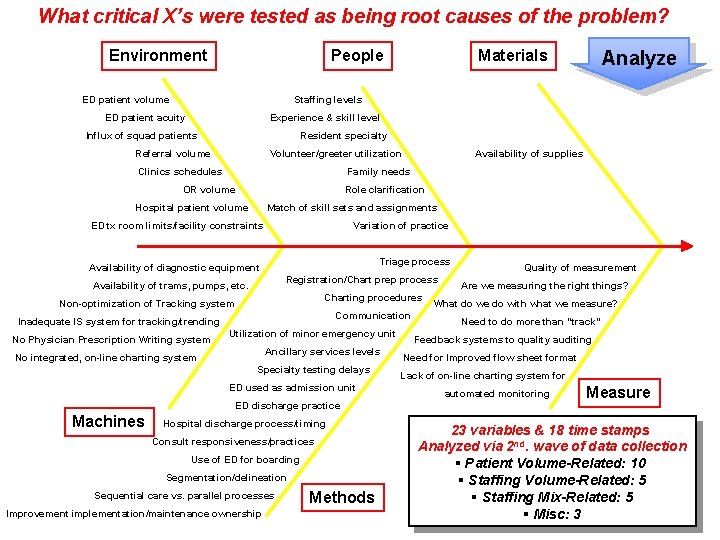
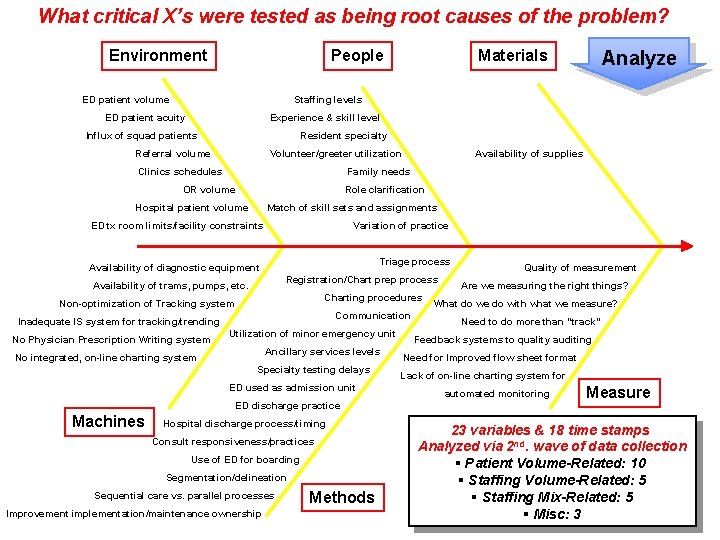
What critical X’s were tested as being root causes of the problem? Environment People ED patient volume Materials Analyze Staffing levels ED patient acuity Experience & skill level Influx of squad patients Resident specialty Referral volume Volunteer/greeter utilization Clinics schedules Family needs OR volume Role clarification Availability of supplies Hospital patient volume Match of skill sets and assignments ED tx room limits/facility constraints Variation of practice Triage process Availability of diagnostic equipment Quality of measurement Registration/Chart prep process Availability of trams, pumps, etc. Are we measuring the right things? Charting procedures Non-optimization of Tracking system What do we do with what we measure? Communication Inadequate IS system for tracking/trending Need to do more than “track” Utilization of minor emergency unit No Physician Prescription Writing system Feedback systems to quality auditing Ancillary services levels No integrated, on-line charting system Need for Improved flow sheet format Specialty testing delays Lack of on-line charting system for ED used as admission unit automated monitoring ED discharge practice Hospital discharge process/timing Measure Machines Consult responsiveness/practices Use of ED for boarding Segmentation/delineation Sequential care vs. parallel processes Improvement implementation/maintenance ownership Methods 23 variables & 18 time stamps Analyzed via 2 nd. wave of data collection § Patient Volume-Related: 10 § Staffing Volume-Related: 5 § Staffing Mix-Related: 5 § Misc: 3
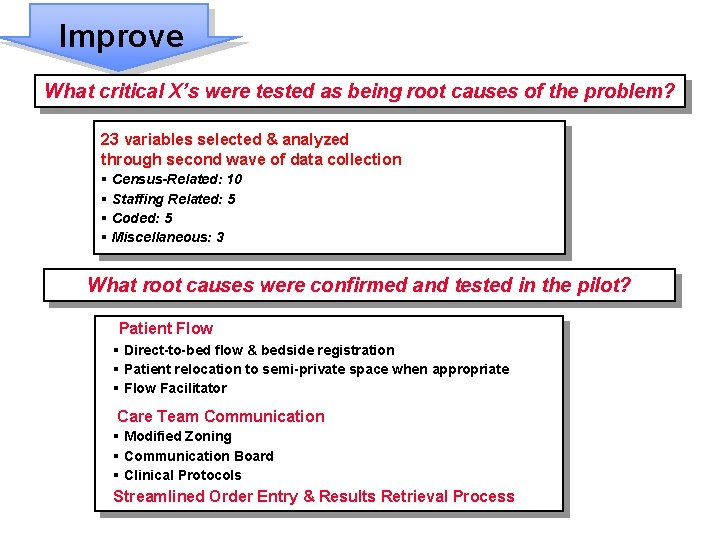
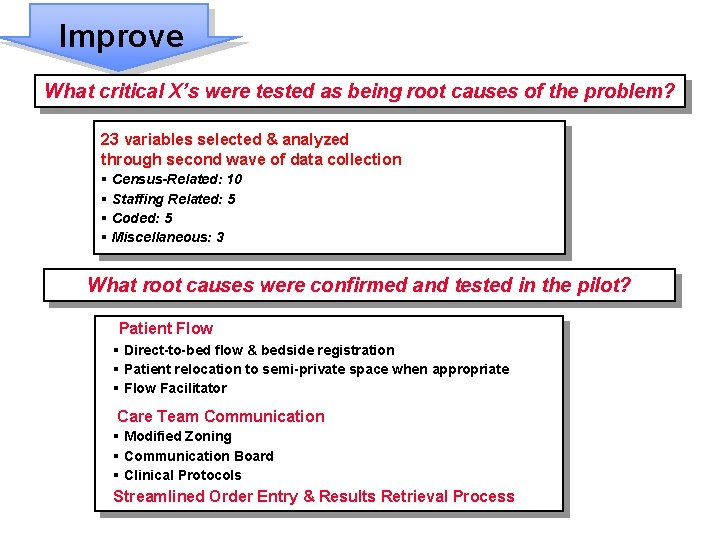
Improve What critical X’s were tested as being root causes of the problem? 23 variables selected & analyzed through second wave of data collection § Census-Related: 10 § Staffing Related: 5 § Coded: 5 § Miscellaneous: 3 What root causes were confirmed and tested in the pilot? Patient Flow § Direct-to-bed flow & bedside registration § Patient relocation to semi-private space when appropriate § Flow Facilitator Care Team Communication § Modified Zoning § Communication Board § Clinical Protocols Streamlined Order Entry & Results Retrieval Process
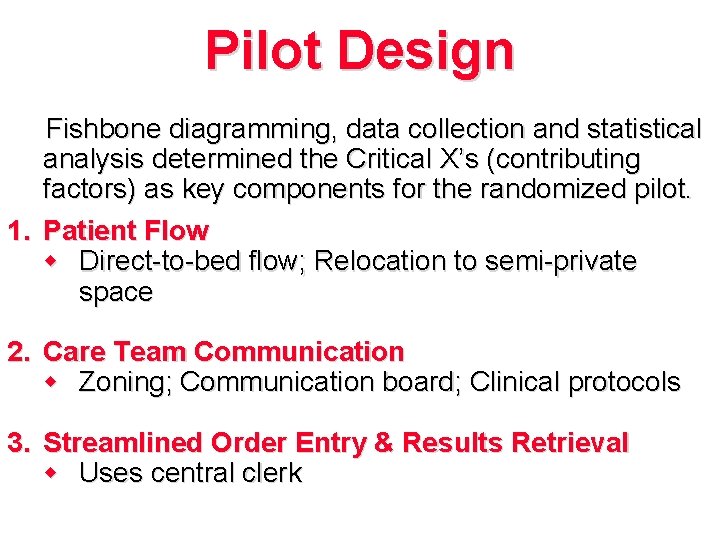
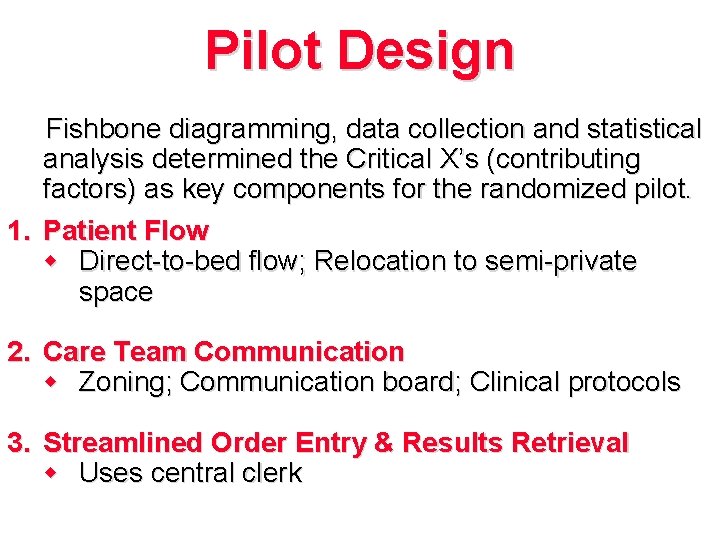
Pilot Design Fishbone diagramming, data collection and statistical analysis determined the Critical X’s (contributing factors) as key components for the randomized pilot. 1. Patient Flow w Direct-to-bed flow; Relocation to semi-private space 2. Care Team Communication w Zoning; Communication board; Clinical protocols 3. Streamlined Order Entry & Results Retrieval w Uses central clerk
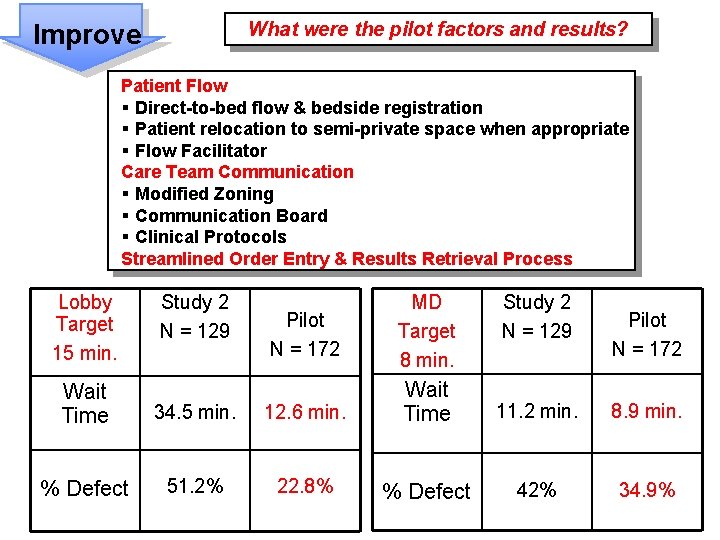
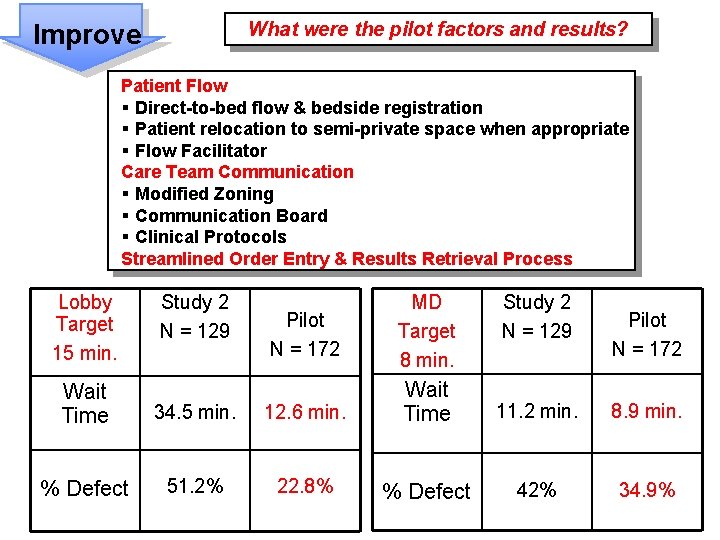
What were the pilot factors and results? Improve Patient Flow § Direct-to-bed flow & bedside registration § Patient relocation to semi-private space when appropriate § Flow Facilitator Care Team Communication § Modified Zoning § Communication Board § Clinical Protocols Streamlined Order Entry & Results Retrieval Process Lobby Target 15 min. Study 2 N = 129 Wait Time 34. 5 min. % Defect 51. 2% Pilot N = 172 MD Target 8 min. Study 2 N = 129 Pilot N = 172 12. 6 min. Wait Time 11. 2 min. 8. 9 min. 22. 8% % Defect 42% 34. 9%
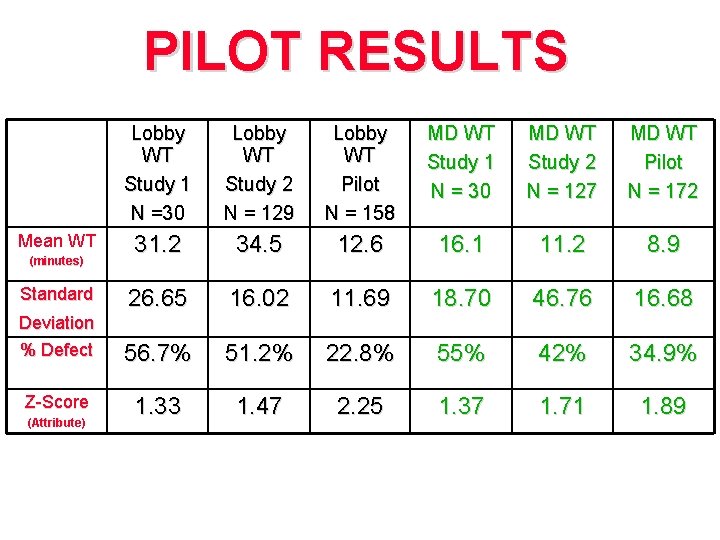
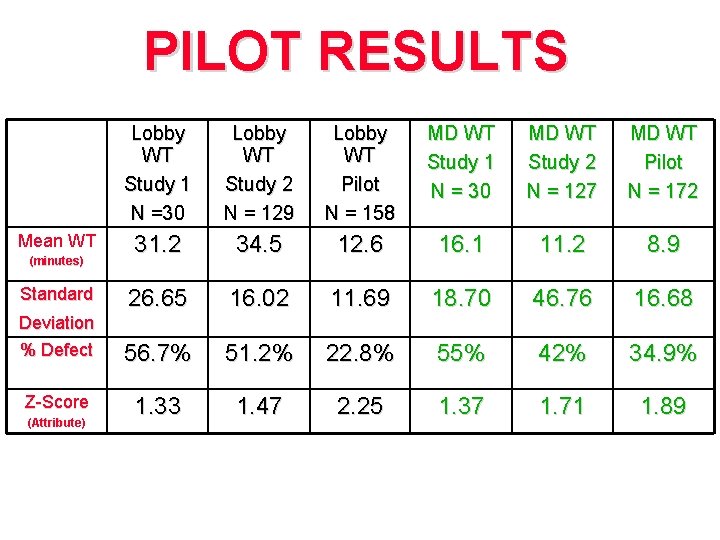
PILOT RESULTS Lobby WT Study 1 N =30 Lobby WT Study 2 N = 129 Lobby WT Pilot N = 158 MD WT Study 1 N = 30 MD WT Study 2 N = 127 MD WT Pilot N = 172 31. 2 34. 5 12. 6 16. 1 11. 2 8. 9 Standard 26. 65 16. 02 11. 69 18. 70 46. 76 16. 68 Deviation % Defect 56. 7% 51. 2% 22. 8% 55% 42% 34. 9% Z-Score 1. 33 1. 47 2. 25 1. 37 1. 71 1. 89 Mean WT (minutes) (Attribute)
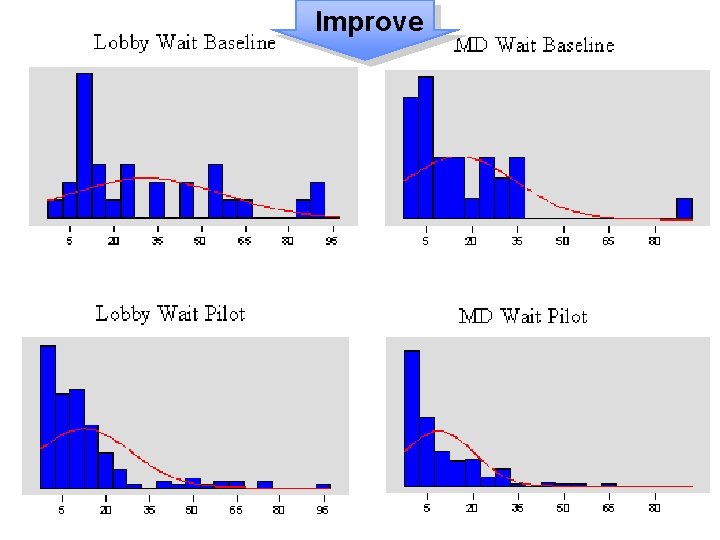
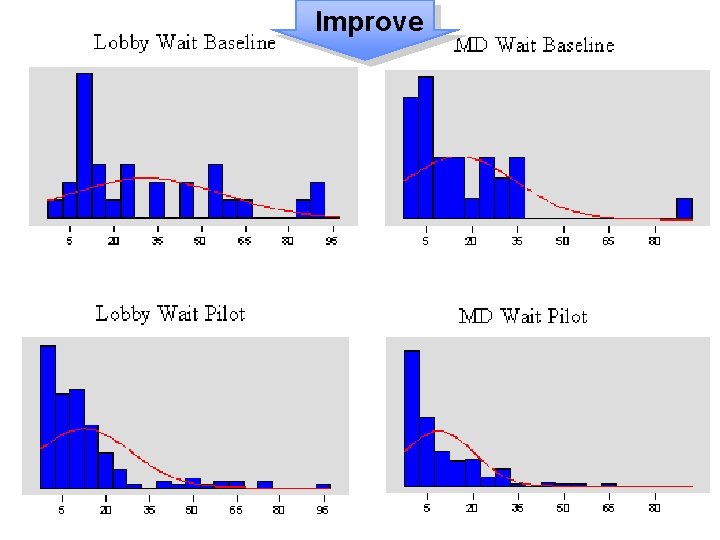
Improve
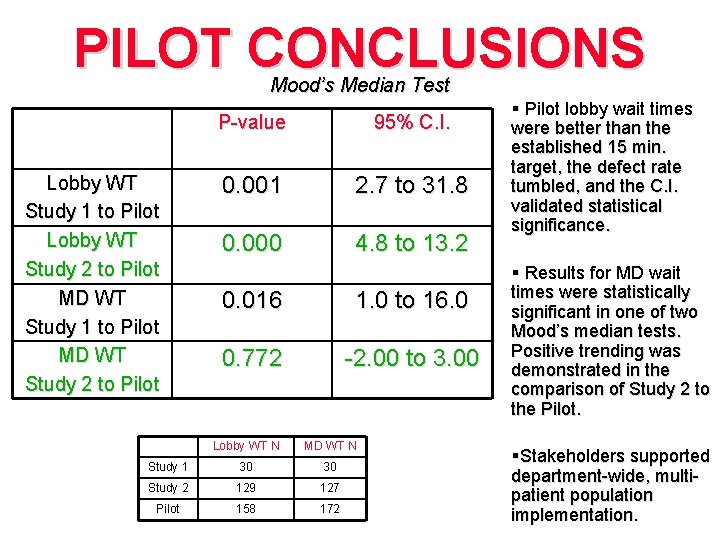
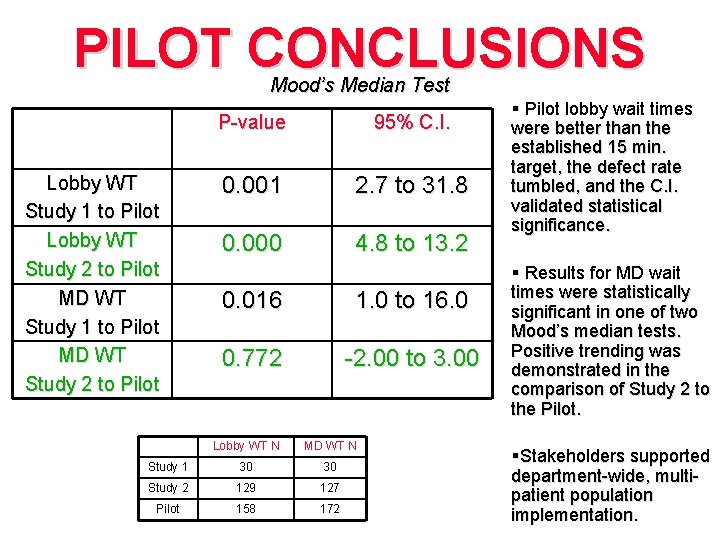
PILOT CONCLUSIONS Mood’s Median Test Lobby WT Study 1 to Pilot Lobby WT Study 2 to Pilot MD WT Study 1 to Pilot MD WT Study 2 to Pilot P-value 95% C. I. 0. 001 2. 7 to 31. 8 0. 000 4. 8 to 13. 2 0. 016 1. 0 to 16. 0 0. 772 -2. 00 to 3. 00 Lobby WT N MD WT N Study 1 30 30 Study 2 129 127 Pilot 158 172 § Pilot lobby wait times were better than the established 15 min. target, the defect rate tumbled, and the C. I. validated statistical significance. § Results for MD wait times were statistically significant in one of two Mood’s median tests. Positive trending was demonstrated in the comparison of Study 2 to the Pilot. §Stakeholders supported department-wide, multipatient population implementation.
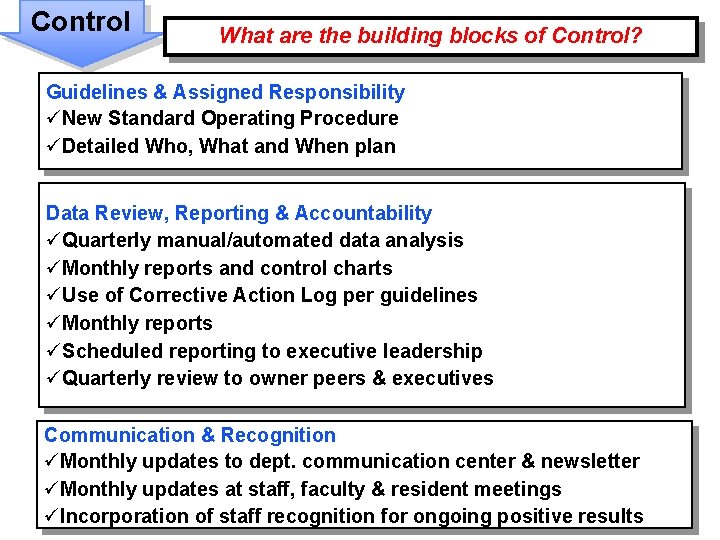
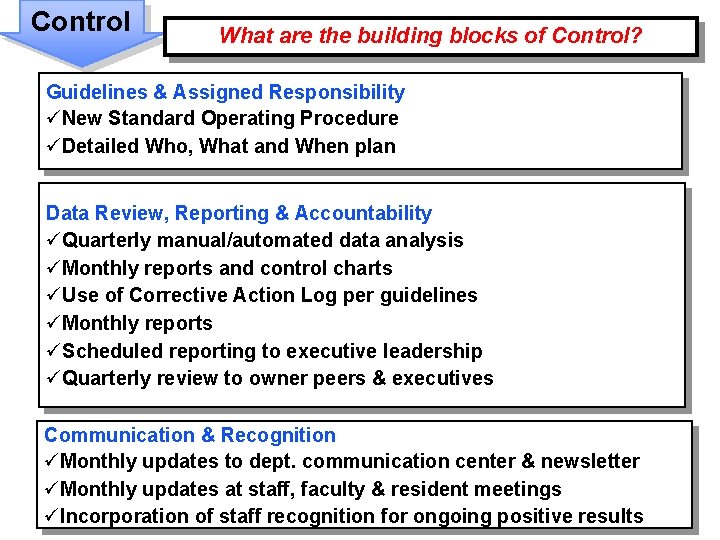
Control What are the building blocks of Control? Guidelines & Assigned Responsibility üNew Standard Operating Procedure üDetailed Who, What and When plan Data Review, Reporting & Accountability üQuarterly manual/automated data analysis üMonthly reports and control charts üUse of Corrective Action Log per guidelines üMonthly reports üScheduled reporting to executive leadership üQuarterly review to owner peers & executives Communication & Recognition üMonthly updates to dept. communication center & newsletter üMonthly updates at staff, faculty & resident meetings üIncorporation of staff recognition for ongoing positive results
 Six sigma at academic medical hospital case analysis
Six sigma at academic medical hospital case analysis Vcom white coat ceremony
Vcom white coat ceremony Vcom mission statement
Vcom mission statement Six fundamental values of academic integrity
Six fundamental values of academic integrity Cmmi six sigma
Cmmi six sigma Pilot plan template six sigma
Pilot plan template six sigma Define tollgate
Define tollgate Six sigma data types
Six sigma data types Who is this
Who is this Six sigma qualtec
Six sigma qualtec Six sigma forum
Six sigma forum Hidden factory concept
Hidden factory concept Mse six sigma
Mse six sigma Dmaic storyboard
Dmaic storyboard Six sigma belts hierarchy
Six sigma belts hierarchy