Scott Maurer MD Associate Professor of Pediatrics University





- Slides: 34
Scott Maurer, MD Associate Professor of Pediatrics University of Pittsburgh School of Medicine Chief, Division of Palliative Medicine and Supportive Care Children’s Hospital of Pittsburgh of UPMC
§ Challenges in decision making § How hard can it really be? § What are the stakes? § When do we have these conversations § Who, what, when, where, and why? § Decision making in practice § Approaching difficult conversations § Using values and goals to guide decisions § Nuts and bolts § How does advance care planning work? § Judging success
§ The death of a child is out of the order of nature § It’s rare § It’s scary § Our culture hasn’t designed us to deal with children dying © 2015 Mitra Farmand
§ We are uncomfortable talking about it § Especially nurses and trainees § Medical trainees have cited lack of training and knowledge in this area § Those who are comfortable: § Misunderstand end of life care options § Including Do Not Resuscitate options § Hospice options § Nurses often feel decisions are made too late § Leads to uncertainty amongst medical team § Trickle down effect to parents/patients Kruse, et al. Plos One. 2017 Sanderson, et al. JAMA Peds. 2013 Kolarik, et al. Pediatrics. 2006 Mc. Callum, et al. J Pain Sympt Mgt. 2000 Michelson, et al. Ped Crit Care Med. 2013
§ Choices are complicated and numerous: § Continue disease directed therapy? § Experimental options? § Artificial life sustaining therapies? § G-tube? § Trach? § Vent? § Dialysis § ECMO § Do not resuscitate § End of life care at home? In hospital? § Hospice? Hinds, PS, et al. Cancer Nurs. 2001.
§ After the death of a child parents may have decisional regret about: § choosing the last course of chemotherapy § not talking with their child about death § not choosing the location of death § Significant numbers of parents have difficulty with unresolved grief and experience: § High rates of depression § Sleep disturbance § Increased physician visits § Greater likelihood to miss work Mack, J. , et al. J Clin Oncol. 2008 Wolfe, J. , et al. J Pain Symptom Manage. 2008 Kreicberges, U. , et al. NEJM. 2004 Lannen, PK. , et al. J Clin Oncol. 2008
§ Siblings suffer during the child’s illness and after their death § Psychosocial issues: § Sleep disturbance § Low self-esteem § Delayed maturity § Symptoms are worse in the first year § Increased anxiety/depression § Increased use of alcohol and illicit drugs § Almost all siblings claim to be affected by the loss many years later Rosenberg, et al. JPSM 2014. Eilegard, et al. Psychooncology. 2013
© 2015 Mitra Farmand
§ Are they ready for palliative care? § Who should we approach? § When should we approach them? § How to make a needs assessment: § Pain? § Decision making needs? § Rehab? § Social work/concrete needs? § Emotional needs? § Spiritual needs? § End of life care needs? § Bereavement needs?

The benefit of NOT having an agenda
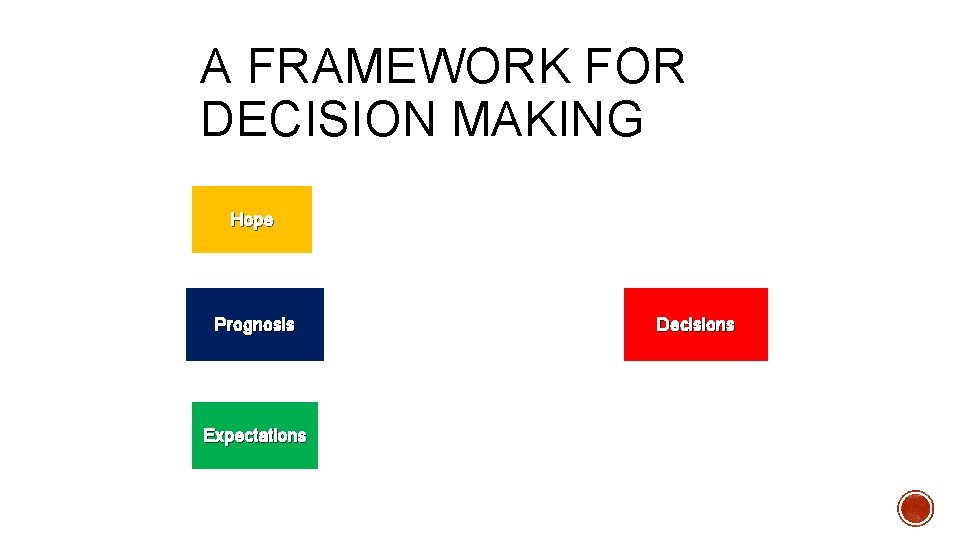
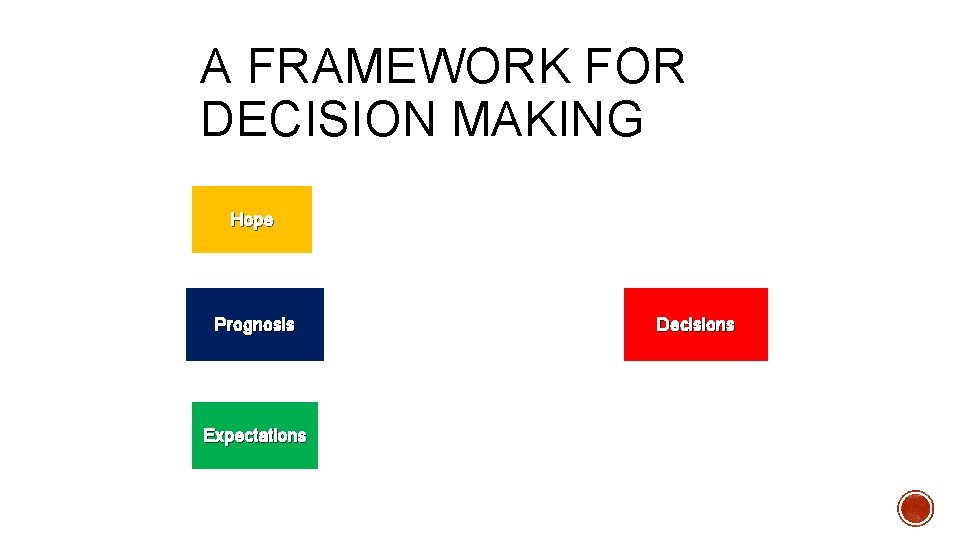
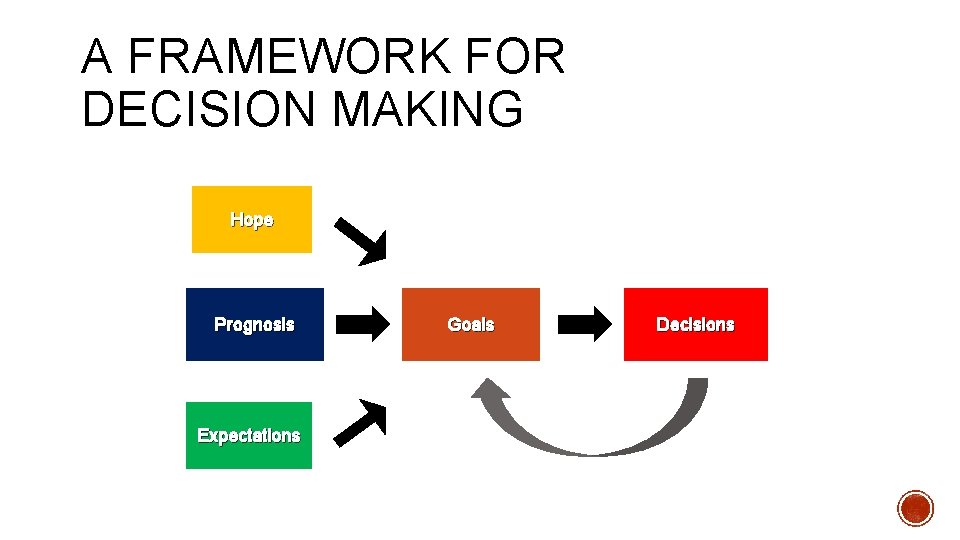
A FRAMEWORK FOR DECISION MAKING Hope Prognosis Expectations Decisions

A FRAMEWORK FOR DECISION MAKING Hope Prognosis Expectations Goals
GOALS § Cure § Life prolongation with an emphasis on quality of life § Comfort § Value of being realistic versus being neutral § Recognition of bias we bring to the table § Truly believing that there isn’t a right or wrong answer Macauley, JPM. 2011.

HOW GOALS CHANGE Cure Life Prolongation Comfort Treatment Intensity High Moderate Mild Minimal Attitude Win Fight Live with Embrace Disease Effect Eradicate Response Halt Progress None Advancing Illness
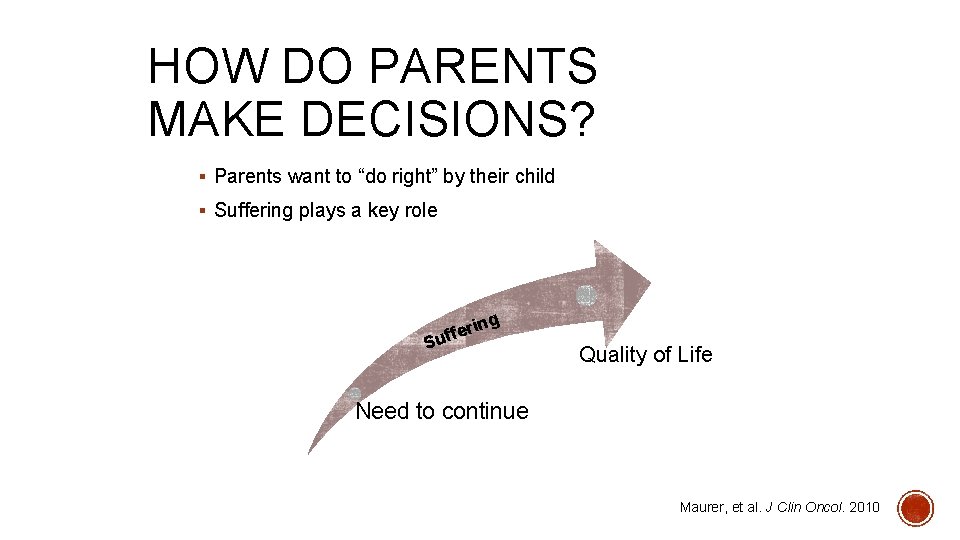
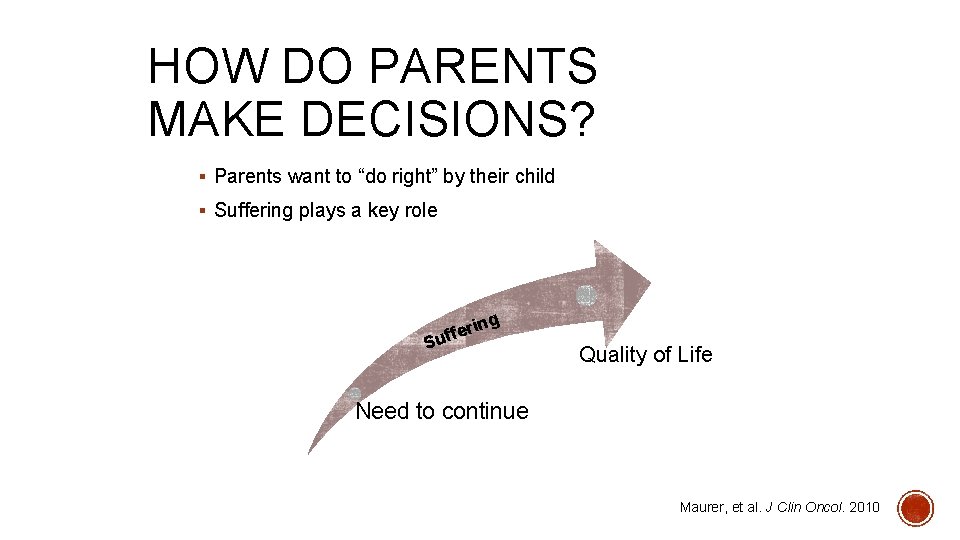
HOW DO PARENTS MAKE DECISIONS? § Parents want to “do right” by their child § Suffering plays a key role ng i r e uff S Quality of Life Need to continue Maurer, et al. J Clin Oncol. 2010
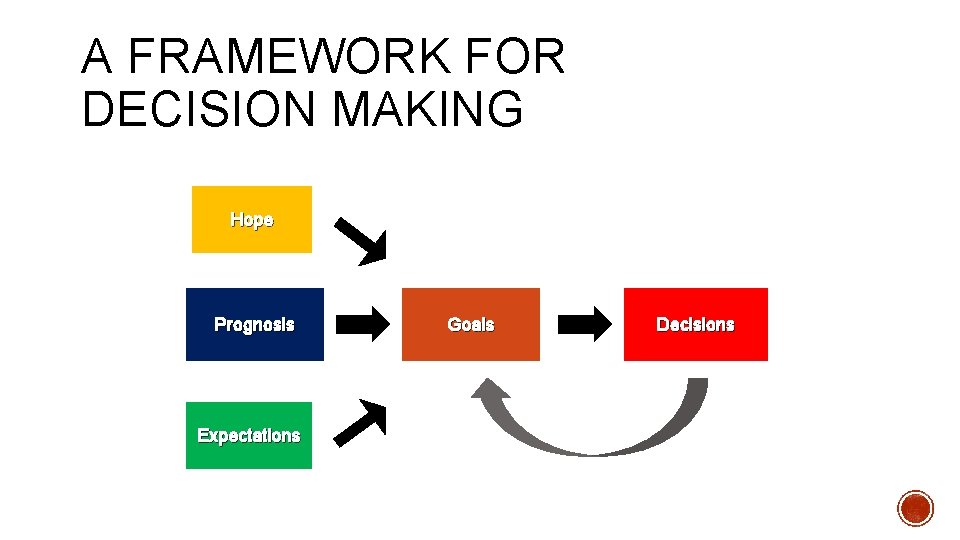
A FRAMEWORK FOR DECISION MAKING Hope Prognosis Expectations Goals Decisions

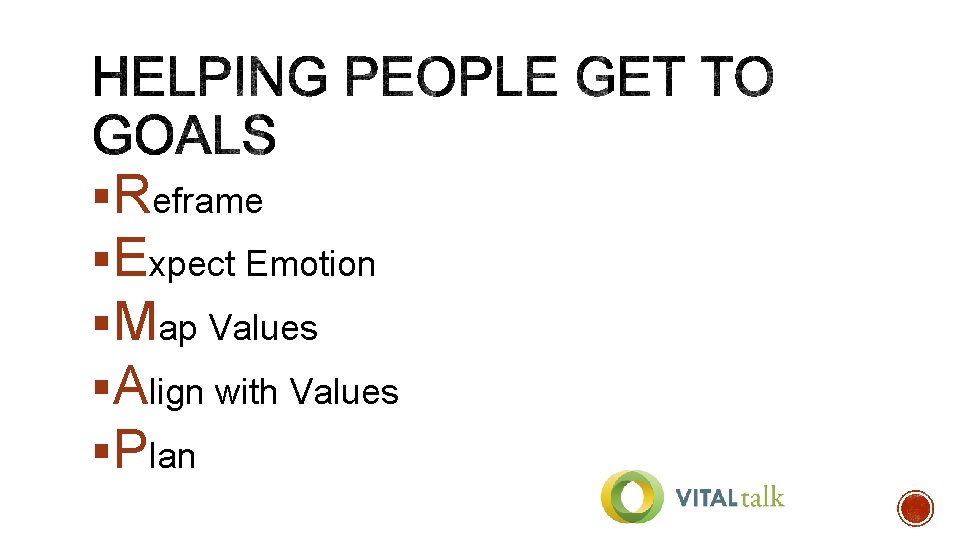
§Reframe §Expect Emotion §Map Values §Align with Values §Plan
§ An opportunity to talk about why the path we’re on isn’t working REFRAMIN G § Given what’s going on, it might be a good time to talk about what to do next. § We’re in a different place.
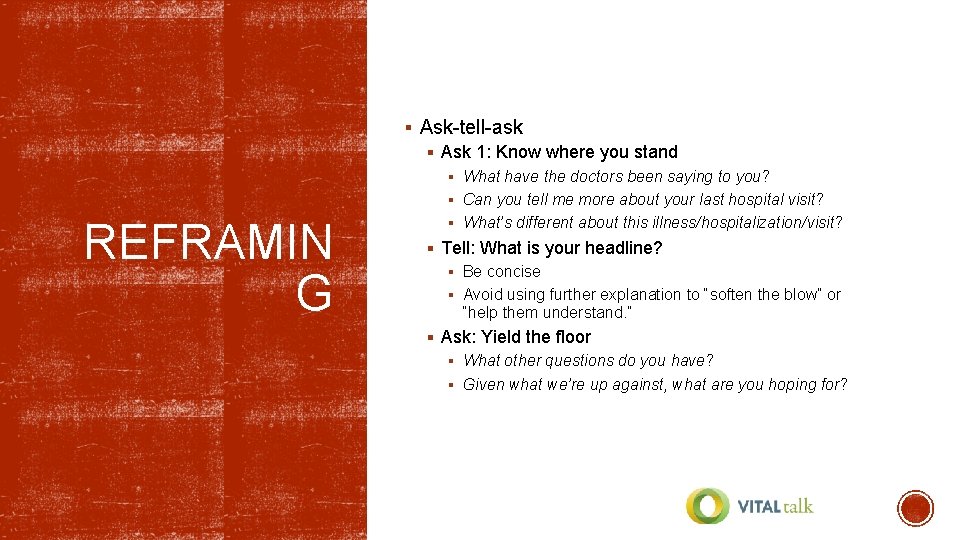
§ Ask-tell-ask § Ask 1: Know where you stand § What have the doctors been saying to you? § Can you tell me more about your last hospital visit? REFRAMIN G § What’s different about this illness/hospitalization/visit? § Tell: What is your headline? § Be concise § Avoid using further explanation to “soften the blow” or “help them understand. ” § Ask: Yield the floor § What other questions do you have? § Given what we’re up against, what are you hoping for?
§ Be cognizant of the type of response you are getting § Cognitive v/s emotional EXPECT EMOTION
© 2015 Mitra Farmand
§ Be cognizant of the type of response you are getting § Cognitive v/s emotional EXPECT EMOTION § NURSE § Name – This is really hard. § Understand – I can’t even imagine what you’re going through. § Respect – You are such a strong advocate for your child. § Support – I will support you no matter what. § Explore – Can you tell me more about what you’re thinking?
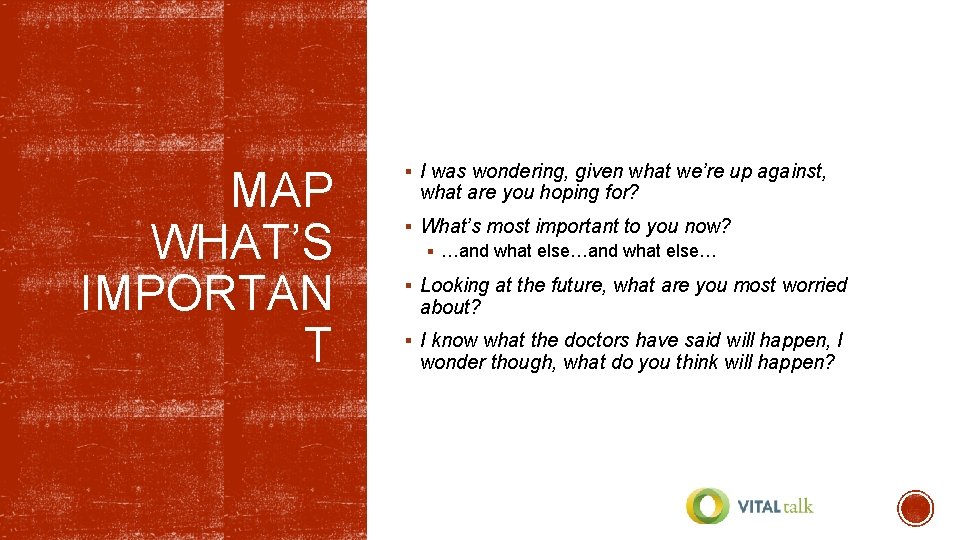
MAP WHAT’S IMPORTAN T § I was wondering, given what we’re up against, what are you hoping for? § What’s most important to you now? § …and what else… § Looking at the future, what are you most worried about? § I know what the doctors have said will happen, I wonder though, what do you think will happen?
§ What I’m hearing you say is… ALIGN WITH VALUES § It sounds like X, Y, and Z are really important to you. § Fighting the cancer is really important to you, and I also hear you say that you don’t want your son to suffer.
§ The balance between giving choices and making recommendations can be tough § Bear in mind the patient/parent’s goals and see how they align with their values PLAN § I am hearing that the most important thing after your baby is born is that he is comfortable and acknowledged as an important part of your family. Given that, can I make a suggestion as to what we might do moving forward?
§ Tell me more… § If a patient/parent says something you’re not sure about § If the patient/parent is having a difficult time talking § Use “I wish” statements § I wish the chemo had worked § I wish things were different § Give some space § You have every right to be angry § It’s ok to take a minute
§ A sense of being a “good parent” to the dying child can: § Provide emotional relief to the family § Possibly decrease morbidity in the bereavement period § Someone who: § Makes informed, unselfish decisions in the child’s best interest § Meets the child’s basic needs § Remains at the child’s side § Protects and advocates for the child § Shows love § Teaches moral values § Prevents suffering
§ There are several advance care planning tools for children and adolecents § My Wishes § 5 Wishes § Voicing My Choices § Studies have demonstrated that ACP discussions are: § Useful for patients/families of all ages § Emotionally intense § Anxiety provoking for providers § Best when done early in the disease course § Best when revisited Kazmerski, et al. Ped Pulmonology. 2016 Dallas, et al. Pediatrics. 2016 Needle & Smith. JPM. 2016 Lyon, et al. AIDS Care. 2017
§ Integrate the plan of care § Share plan across disciplines § Multidisciplinary Interdisciplinary § Share plan across settings § Clinic § Hospital § Home Health § Hospice
If you have resources • Use them! • Learn what they can offer! • Meet often! Child Life Music Therapy Art Therapy Behavioral Health Bereavement Care Social Work Spiritual Care Nutrition Rehab Services
§ Many families have no idea what resources are available to them § You don’t have to be an expert, you just need to know where to get help § Spirituality as an example: § Parents are often not asked about spiritual needs § Many desire spiritual support § Those that don’t, aren’t offended when asked § Simply asking about spiritual needs § Increased parental perception of support § Increased utilization of spiritual resources § Didn’t cost anything § YOU DON’T KNOW IF YOU DON’T ASK! Kelly, et al. J Pall Med. 2016.
§ Vital. Talk § Quick guides for communication SOME HELPFUL RESOURCE S § http: //vitaltalk. org/resources/quick-guides/ § It’s FREE in the app store § Advance Care Planning Documents § https: //agingwithdignity. org/five-wishes/pediatric

 Promotion from associate professor to professor
Promotion from associate professor to professor Dr scott maurer
Dr scott maurer Stephanie maurer
Stephanie maurer Schuffner dots malaria
Schuffner dots malaria Frank maurer
Frank maurer 戴敏育 台北大學
戴敏育 台北大學 Rainer maurer pforzheim
Rainer maurer pforzheim Rainer maurer pforzheim
Rainer maurer pforzheim Grafit eutektikum
Grafit eutektikum What is software implementation in software engineering
What is software implementation in software engineering Leslie bromberg
Leslie bromberg John maurer plumbing
John maurer plumbing Scott page university of michigan
Scott page university of michigan Normal range for vital signs
Normal range for vital signs Normal vital ranges
Normal vital ranges How many types of jaundice
How many types of jaundice Mummy restraint images
Mummy restraint images Volutrol
Volutrol Costochondritis
Costochondritis Normal vital signs for adults
Normal vital signs for adults Nips score
Nips score Differential diagnosis of jaundice in pediatrics
Differential diagnosis of jaundice in pediatrics Modern concept of paediatric nursing
Modern concept of paediatric nursing Modern concept of child health nursing
Modern concept of child health nursing Neurology shelf exam percentiles
Neurology shelf exam percentiles Chest pain in pediatrics
Chest pain in pediatrics New river valley pediatrics
New river valley pediatrics Im injection sites and volumes pediatrics
Im injection sites and volumes pediatrics Trends in pediatric nursing
Trends in pediatric nursing Necrotizing enterocolitis symptoms
Necrotizing enterocolitis symptoms Duke pediatrics durham nc
Duke pediatrics durham nc 11yo
11yo Vancouver clinic pediatrics
Vancouver clinic pediatrics Equipment used in pediatrics
Equipment used in pediatrics Lsuhsc pediatrics
Lsuhsc pediatrics