Respiratory Insufficiency Sleep Apnoe Hypopnoe Syndrome SAHS Janos
- Slides: 32
Respiratory Insufficiency Sleep Apnoe Hypopnoe Syndrome (SAHS) Janos Varga MD, Ph. D National Koranyi Institue for TB and Pulmonology Courtesy of Prof Attila Somfay MD, Ph. D
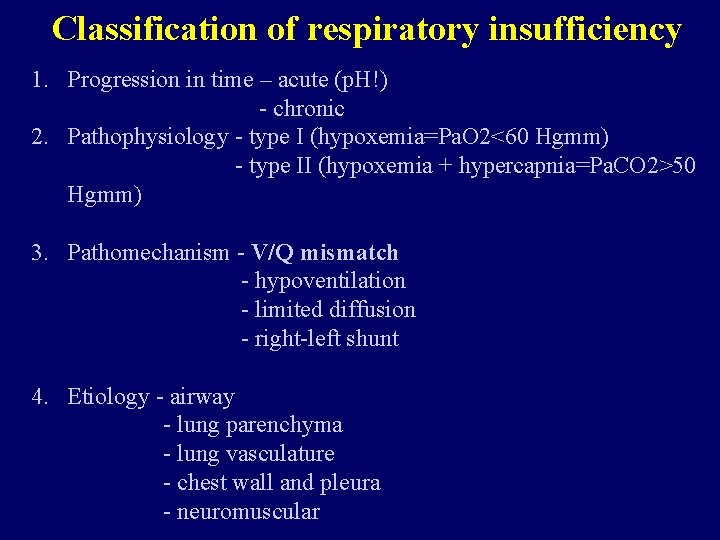
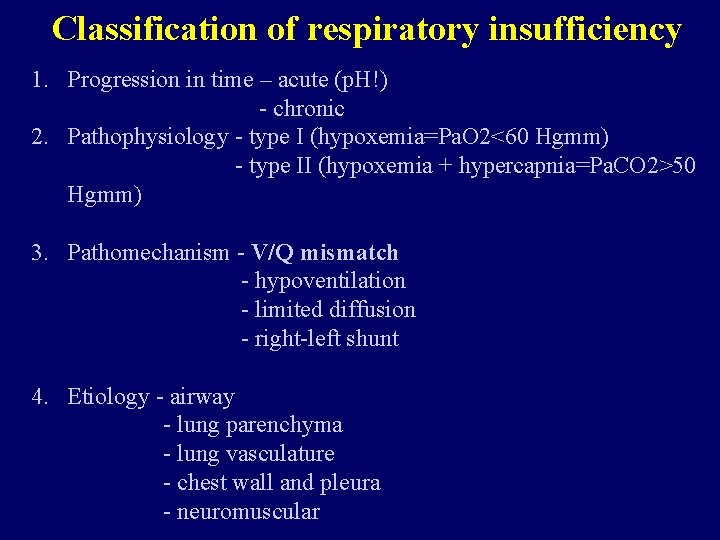
Classification of respiratory insufficiency 1. Progression in time – acute (p. H!) - chronic 2. Pathophysiology - type I (hypoxemia=Pa. O 2<60 Hgmm) - type II (hypoxemia + hypercapnia=Pa. CO 2>50 Hgmm) 3. Pathomechanism - V/Q mismatch - hypoventilation - limited diffusion - right-left shunt 4. Etiology - airway - lung parenchyma - lung vasculature - chest wall and pleura - neuromuscular
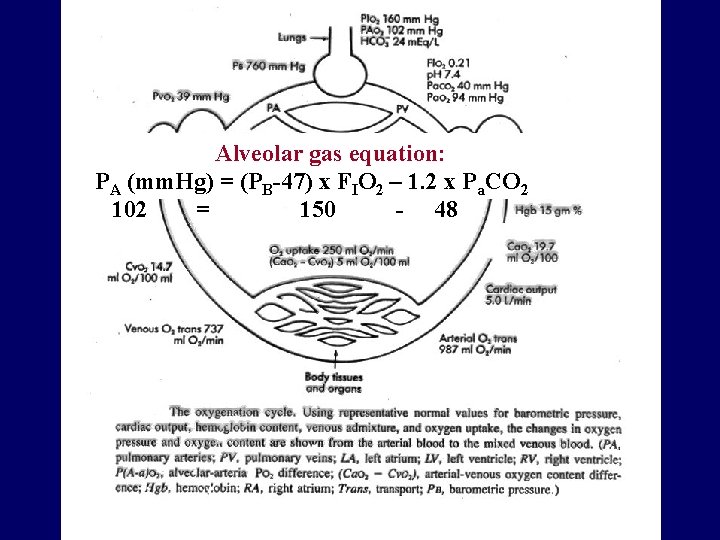
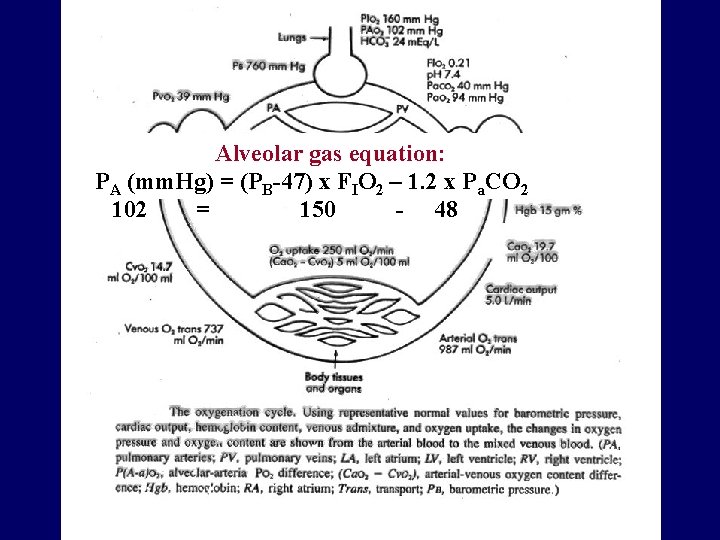
Alveolar gas equation: PA (mm. Hg) = (PB-47) x FIO 2 – 1. 2 x Pa. CO 2 102 = 150 - 48
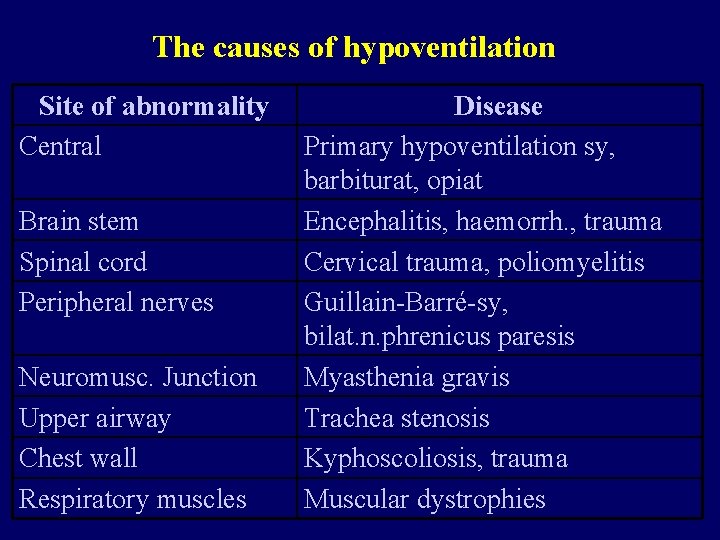
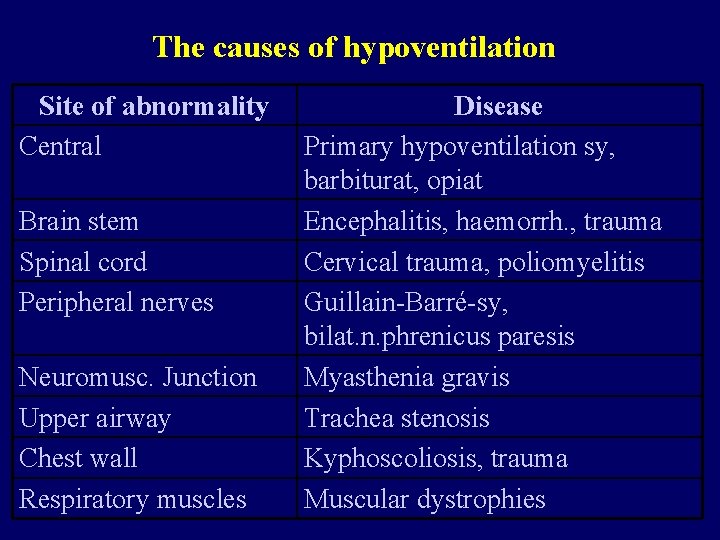
The causes of hypoventilation Site of abnormality Central Brain stem Spinal cord Peripheral nerves Neuromusc. Junction Upper airway Chest wall Respiratory muscles Disease Primary hypoventilation sy, barbiturat, opiat Encephalitis, haemorrh. , trauma Cervical trauma, poliomyelitis Guillain-Barré-sy, bilat. n. phrenicus paresis Myasthenia gravis Trachea stenosis Kyphoscoliosis, trauma Muscular dystrophies
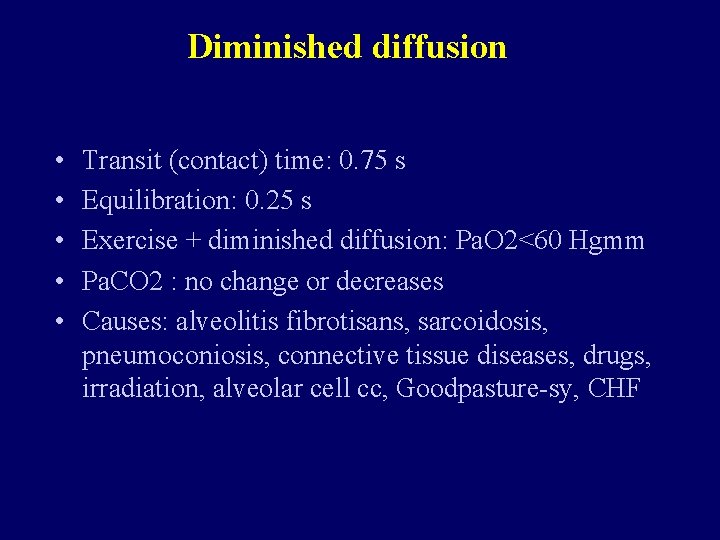
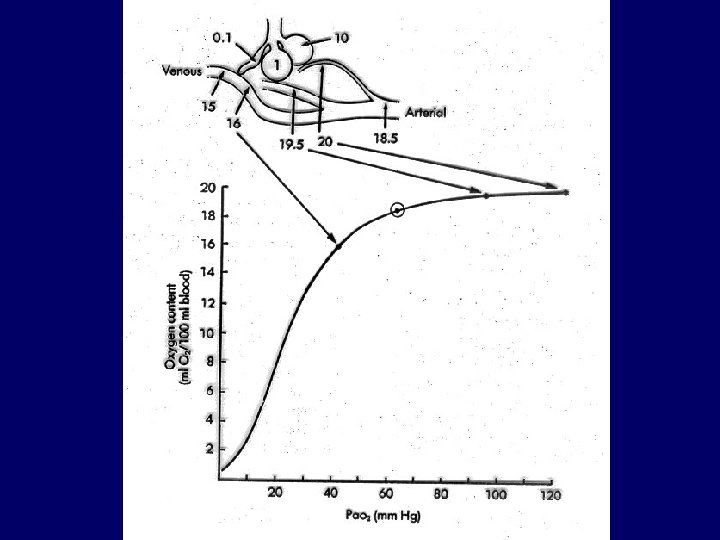
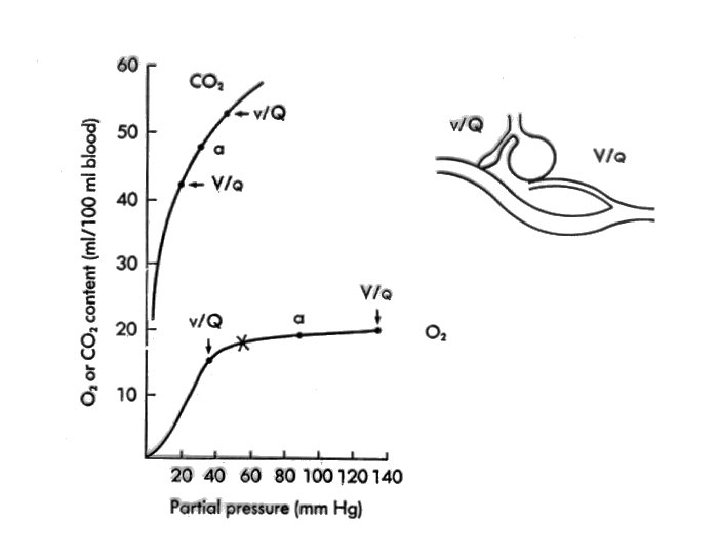
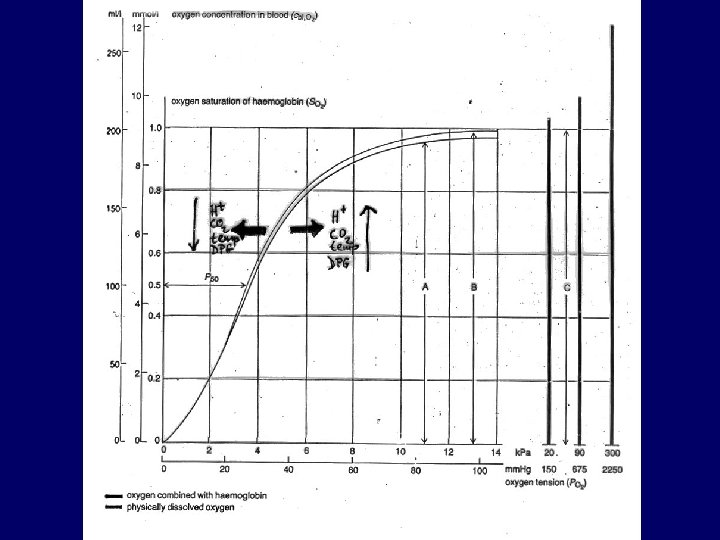
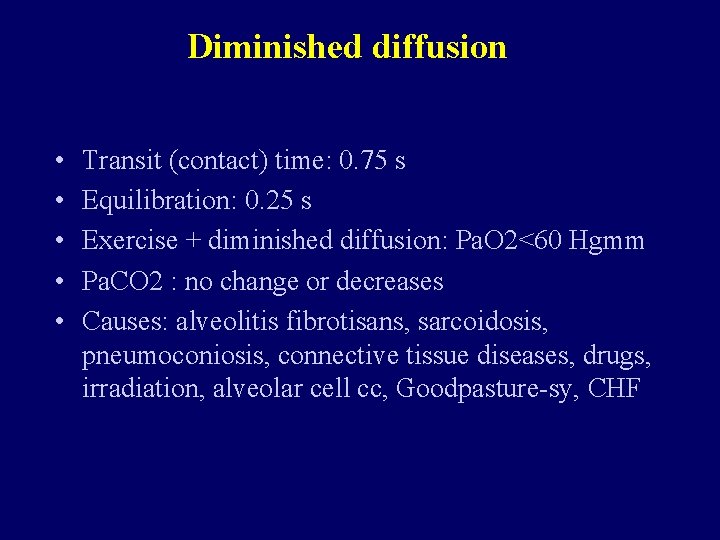
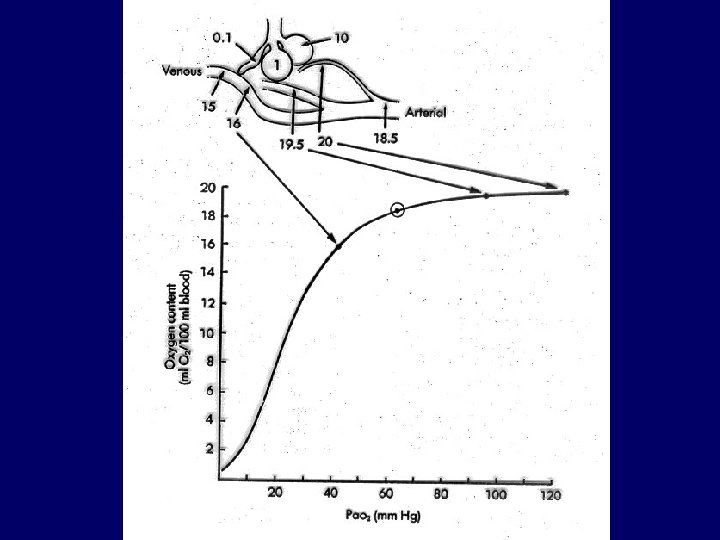
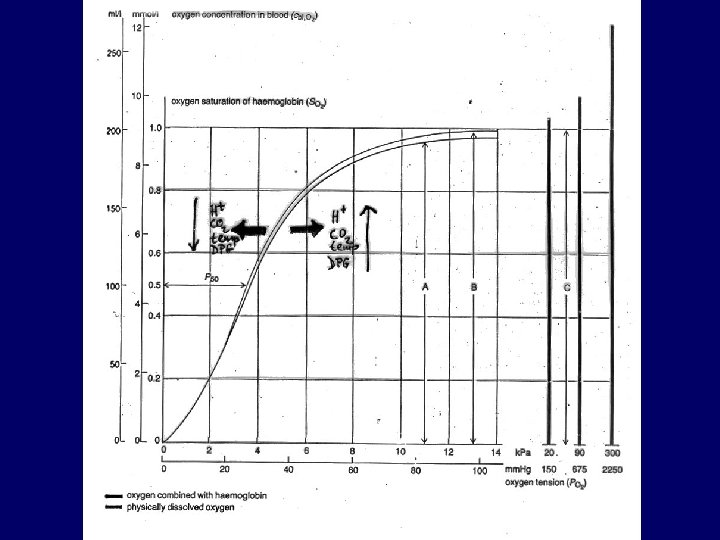
Diminished diffusion • • • Transit (contact) time: 0. 75 s Equilibration: 0. 25 s Exercise + diminished diffusion: Pa. O 2<60 Hgmm Pa. CO 2 : no change or decreases Causes: alveolitis fibrotisans, sarcoidosis, pneumoconiosis, connective tissue diseases, drugs, irradiation, alveolar cell cc, Goodpasture-sy, CHF
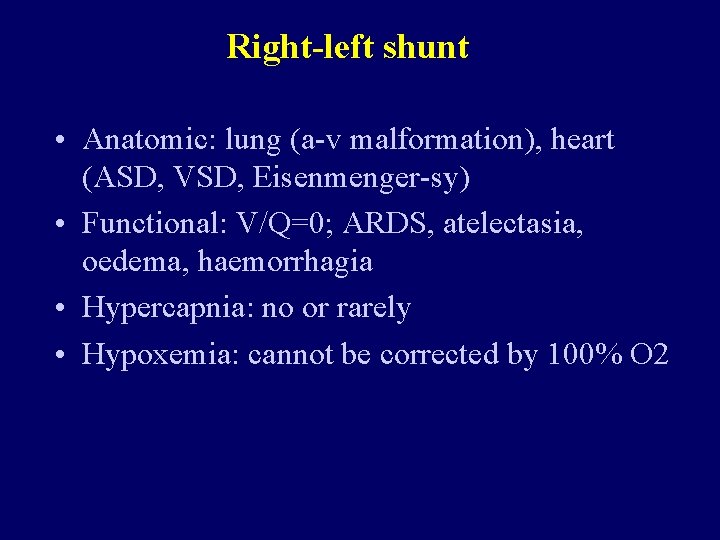
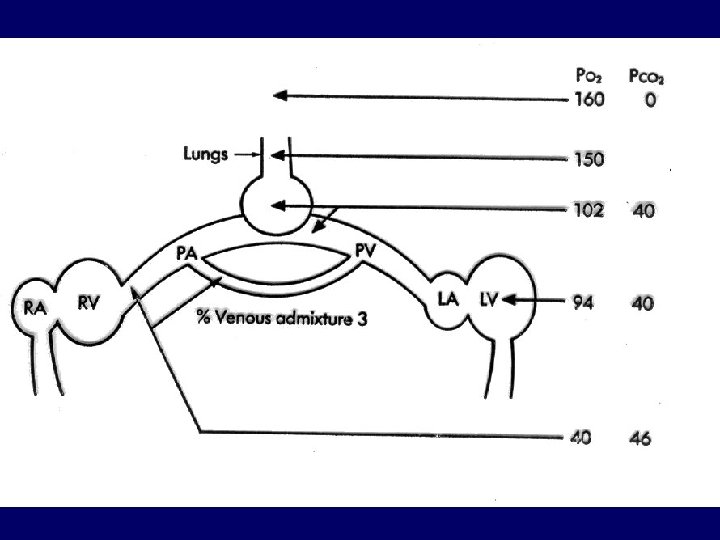
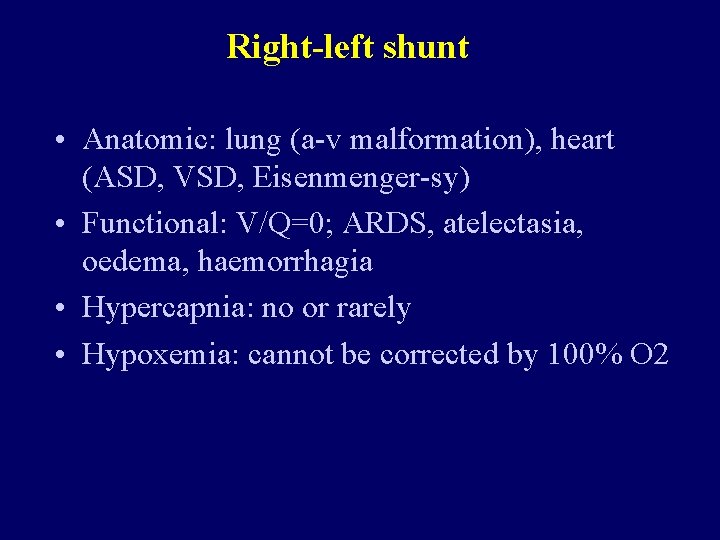
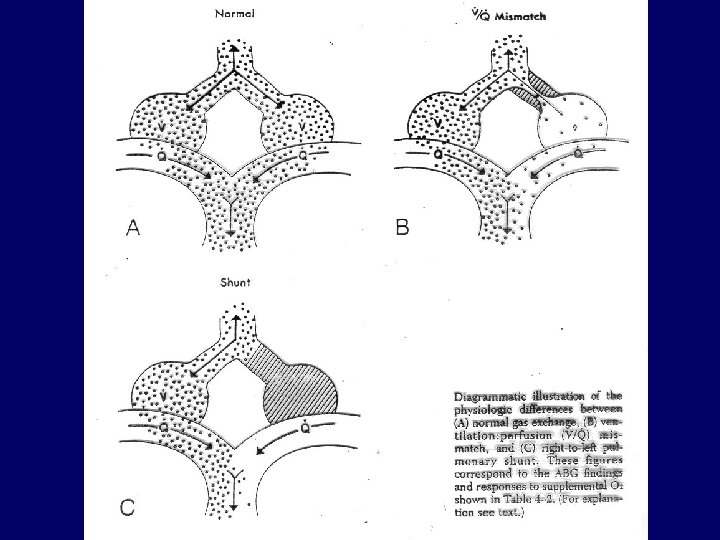
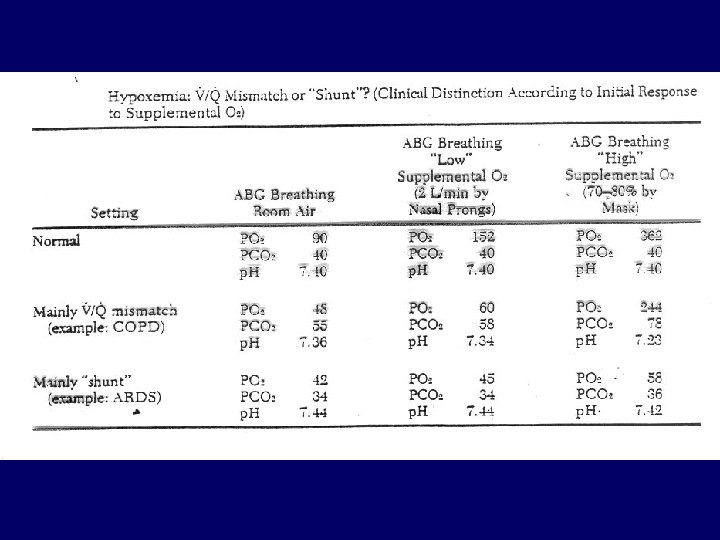
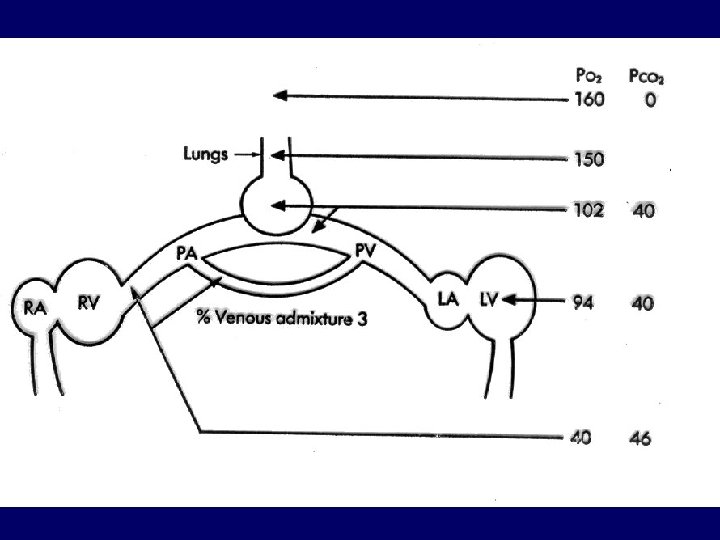
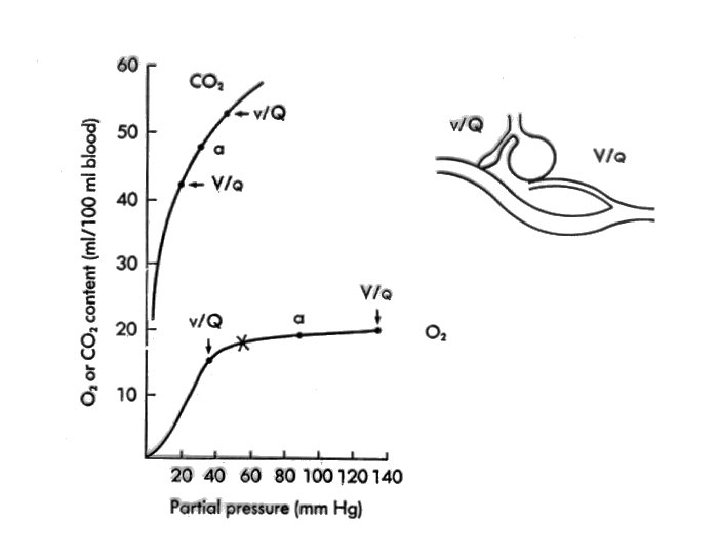
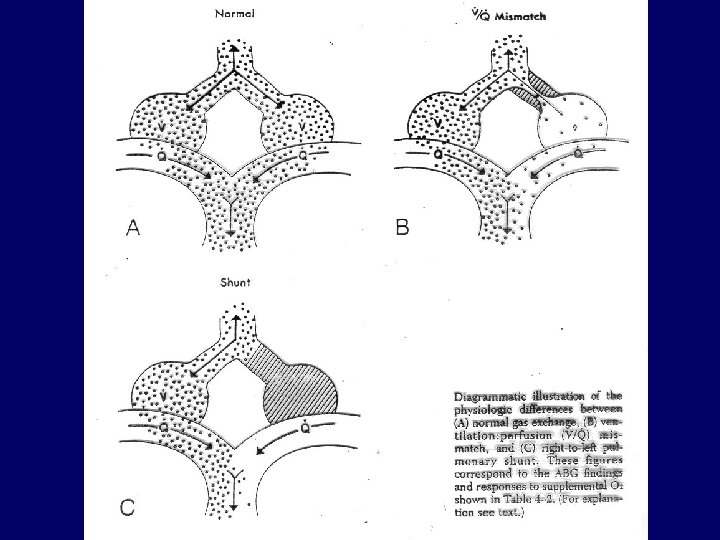
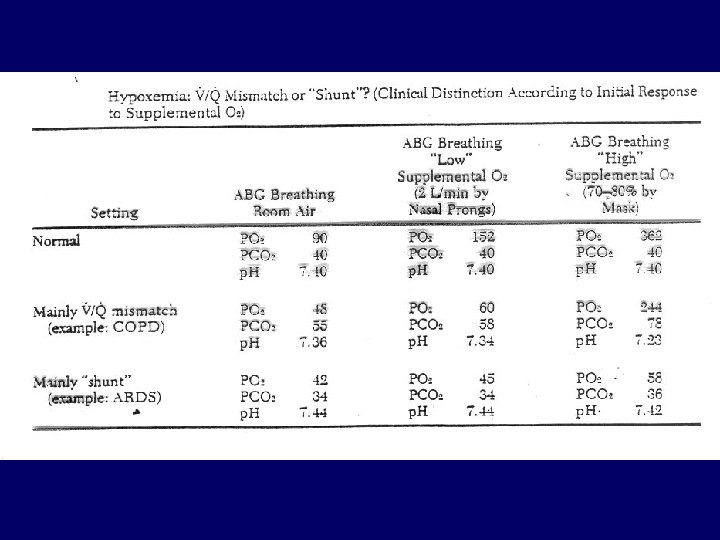
Right-left shunt • Anatomic: lung (a-v malformation), heart (ASD, VSD, Eisenmenger-sy) • Functional: V/Q=0; ARDS, atelectasia, oedema, haemorrhagia • Hypercapnia: no or rarely • Hypoxemia: cannot be corrected by 100% O 2
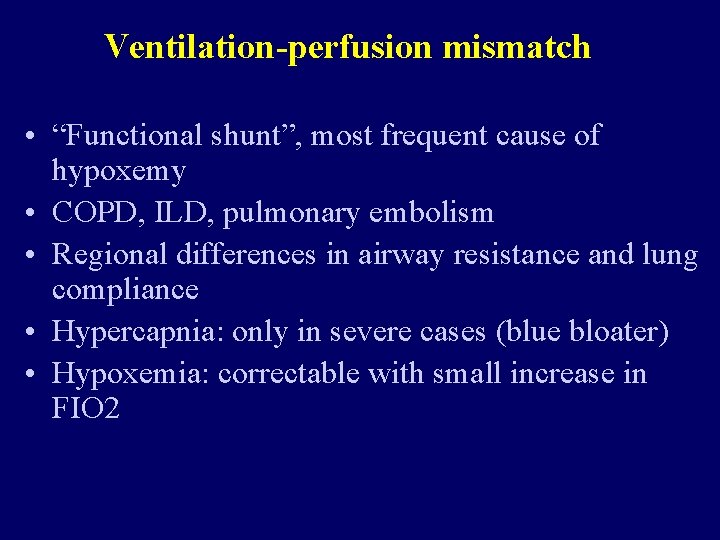
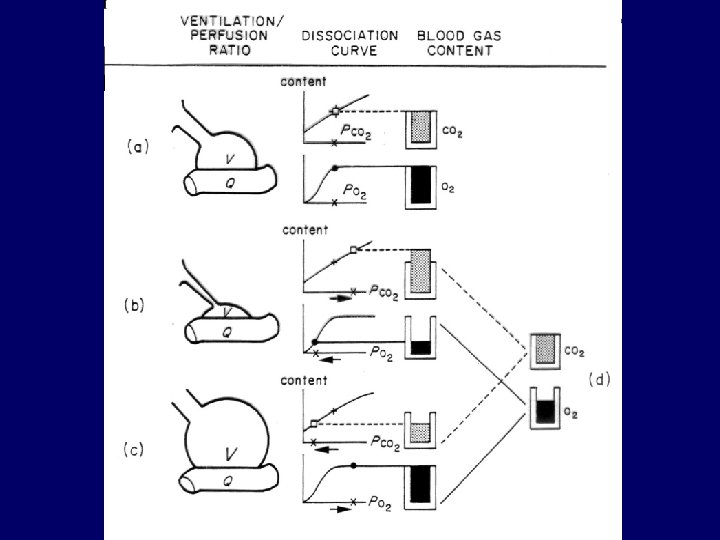
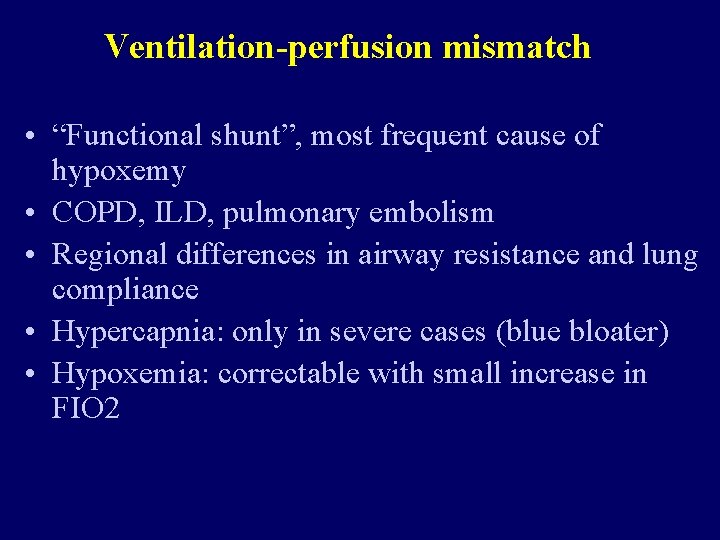
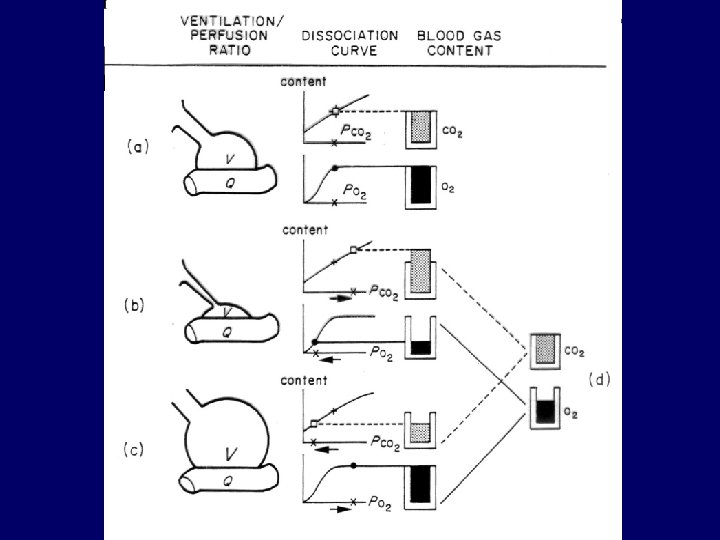
Ventilation-perfusion mismatch • “Functional shunt”, most frequent cause of hypoxemy • COPD, ILD, pulmonary embolism • Regional differences in airway resistance and lung compliance • Hypercapnia: only in severe cases (blue bloater) • Hypoxemia: correctable with small increase in FIO 2
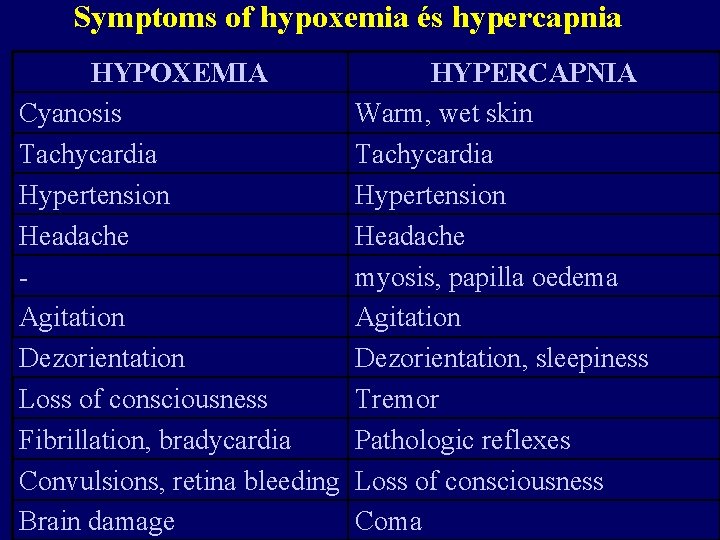
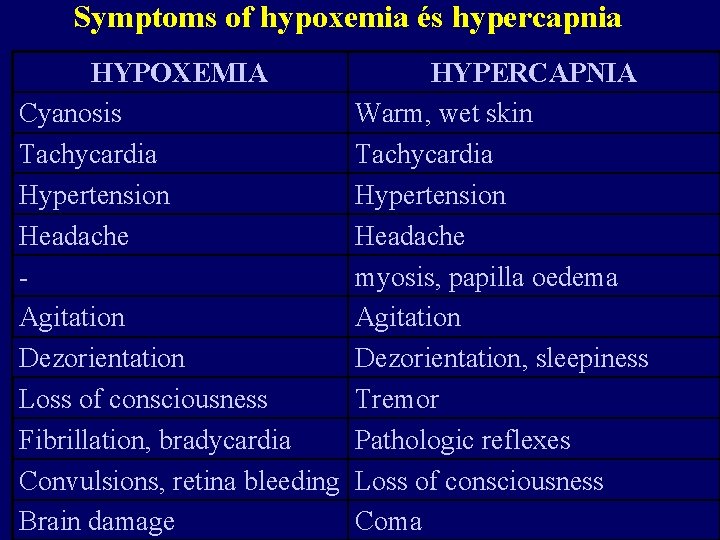
Symptoms of hypoxemia és hypercapnia HYPOXEMIA Cyanosis Tachycardia Hypertension Headache Agitation Dezorientation Loss of consciousness Fibrillation, bradycardia Convulsions, retina bleeding Brain damage HYPERCAPNIA Warm, wet skin Tachycardia Hypertension Headache myosis, papilla oedema Agitation Dezorientation, sleepiness Tremor Pathologic reflexes Loss of consciousness Coma
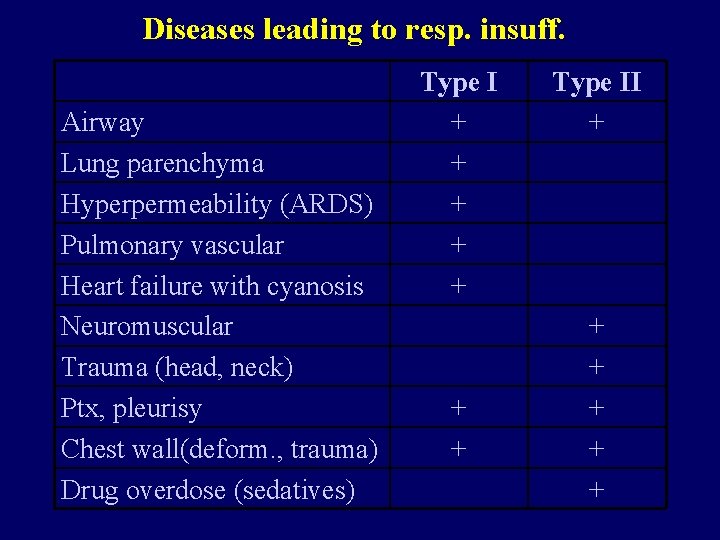
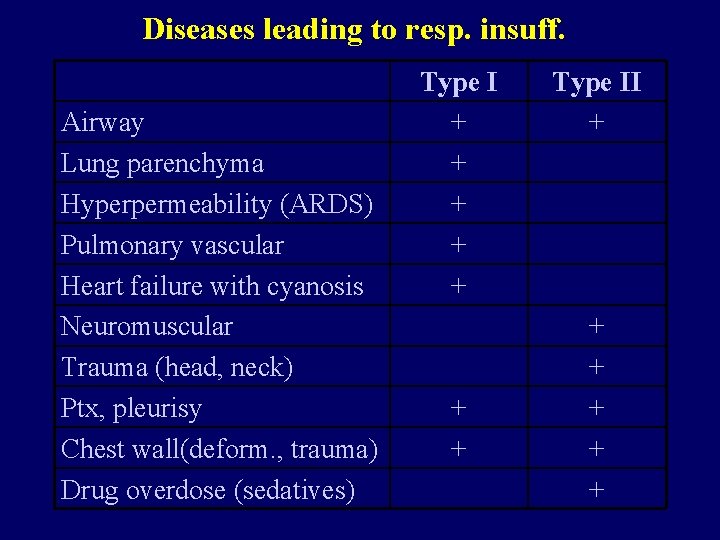
Diseases leading to resp. insuff. Airway Lung parenchyma Hyperpermeability (ARDS) Pulmonary vascular Heart failure with cyanosis Neuromuscular Trauma (head, neck) Ptx, pleurisy Chest wall(deform. , trauma) Drug overdose (sedatives) Type I + + + + Type II + + +
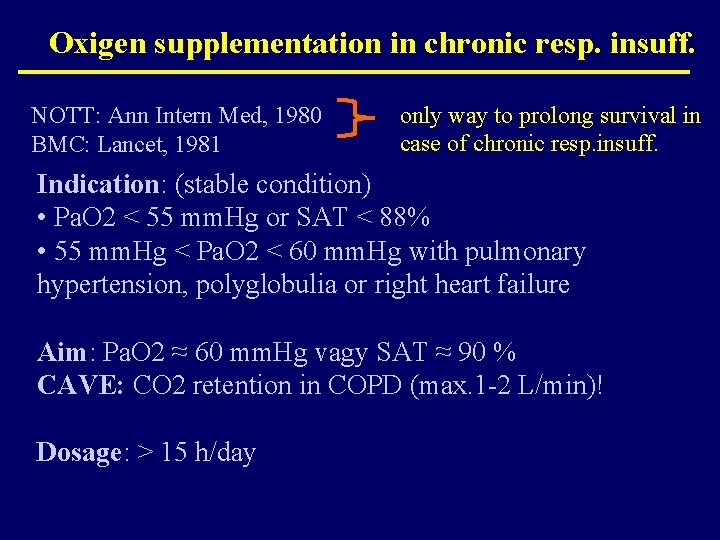
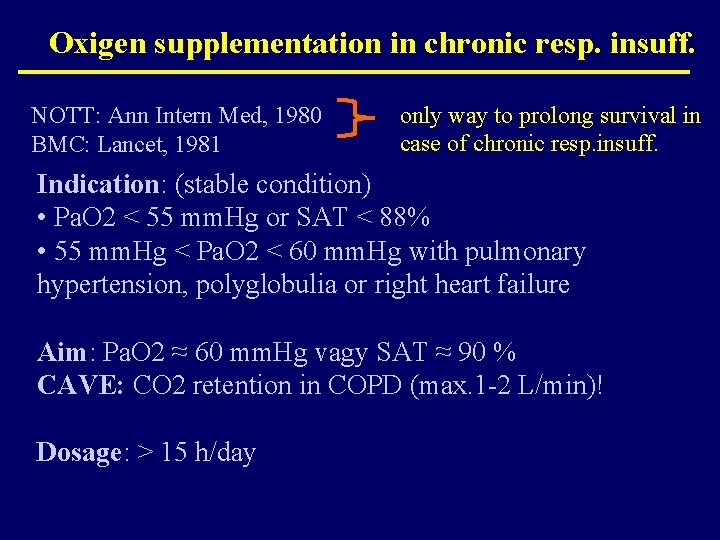
Oxigen supplementation in chronic resp. insuff. NOTT: Ann Intern Med, 1980 BMC: Lancet, 1981 only way to prolong survival in case of chronic resp. insuff. Indication: (stable condition) • Pa. O 2 < 55 mm. Hg or SAT < 88% • 55 mm. Hg < Pa. O 2 < 60 mm. Hg with pulmonary hypertension, polyglobulia or right heart failure Aim: Pa. O 2 ≈ 60 mm. Hg vagy SAT ≈ 90 % CAVE: CO 2 retention in COPD (max. 1 -2 L/min)! Dosage: > 15 h/day
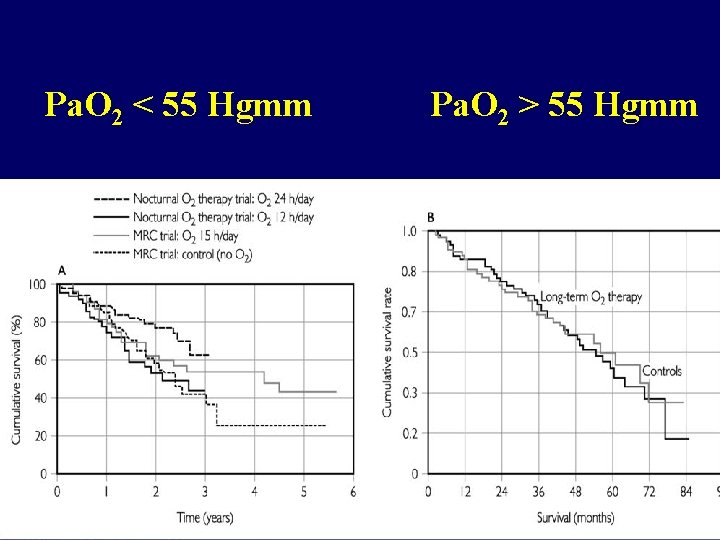
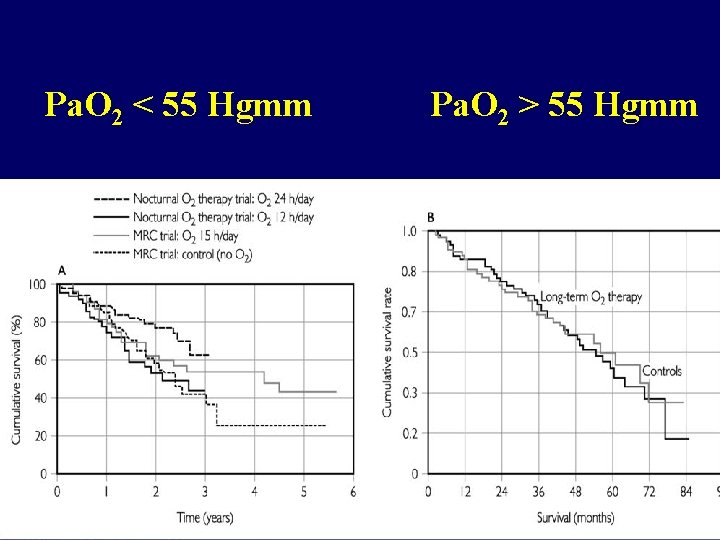
Pa. O 2 < 55 Hgmm Pa. O 2 > 55 Hgmm
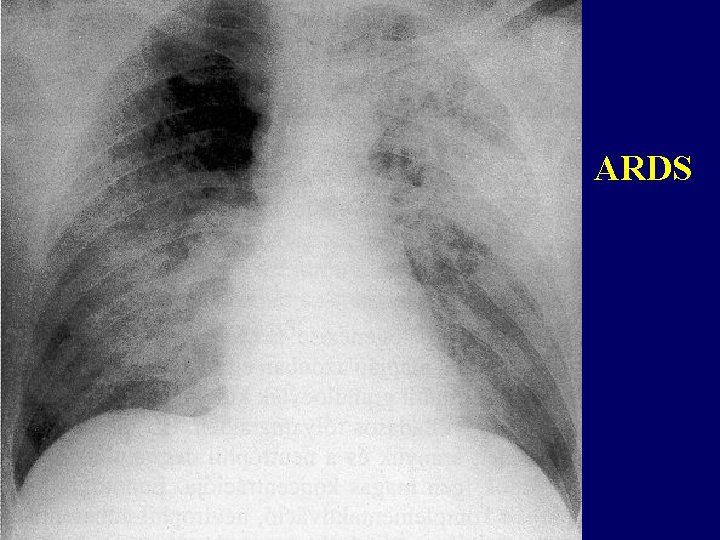
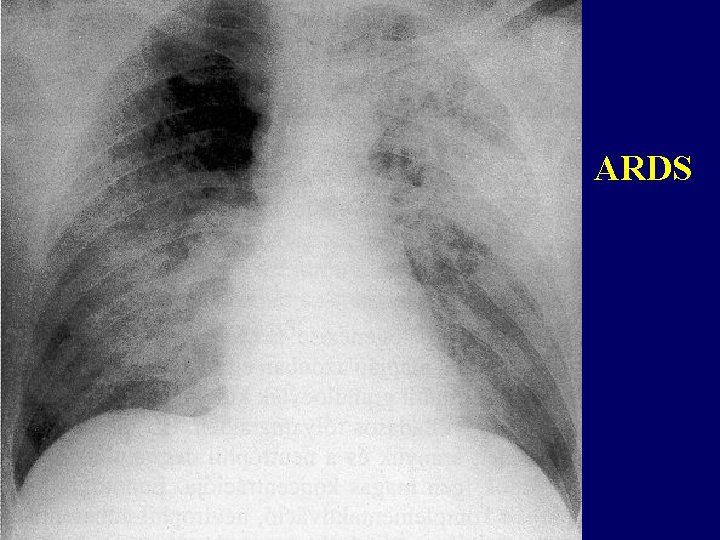
ARDS
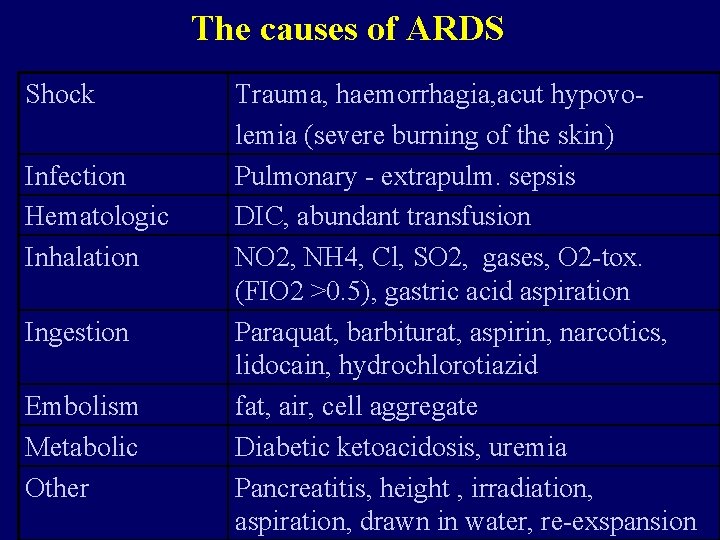
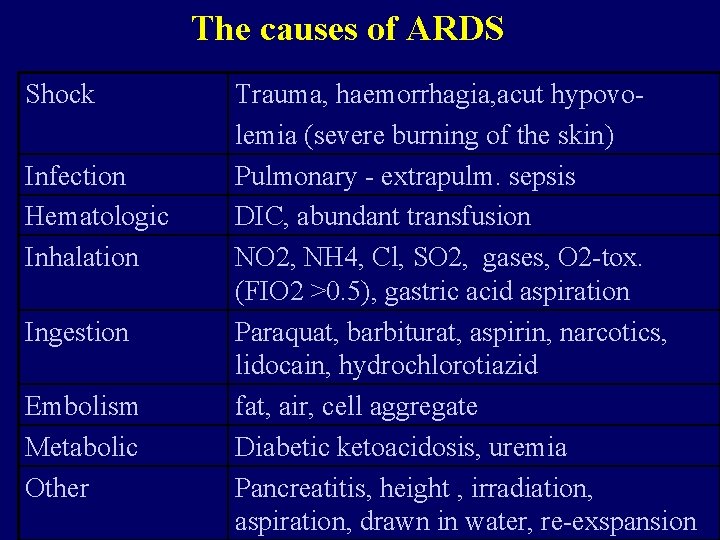
The causes of ARDS Shock Infection Hematologic Inhalation Ingestion Embolism Metabolic Other Trauma, haemorrhagia, acut hypovolemia (severe burning of the skin) Pulmonary - extrapulm. sepsis DIC, abundant transfusion NO 2, NH 4, Cl, SO 2, gases, O 2 -tox. (FIO 2 >0. 5), gastric acid aspiration Paraquat, barbiturat, aspirin, narcotics, lidocain, hydrochlorotiazid fat, air, cell aggregate Diabetic ketoacidosis, uremia Pancreatitis, height , irradiation, aspiration, drawn in water, re-exspansion
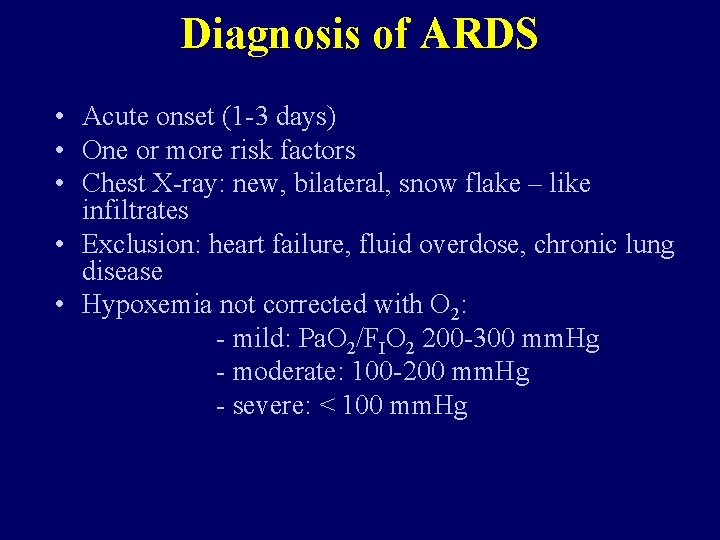
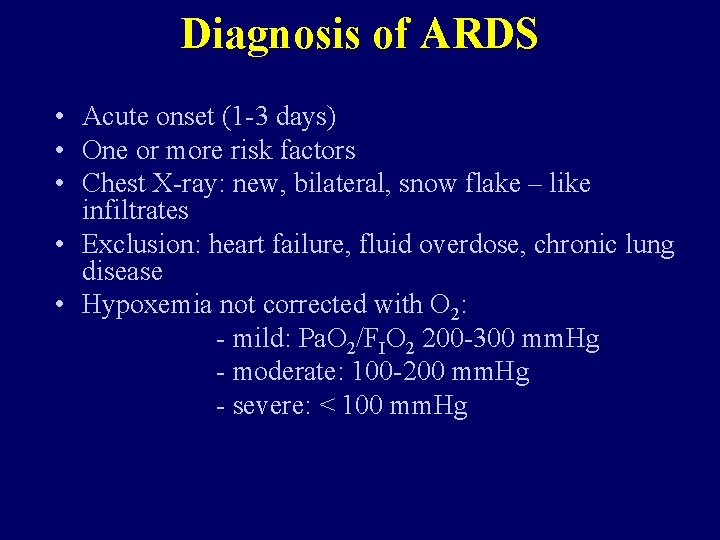
Diagnosis of ARDS • Acute onset (1 -3 days) • One or more risk factors • Chest X-ray: new, bilateral, snow flake – like infiltrates • Exclusion: heart failure, fluid overdose, chronic lung disease • Hypoxemia not corrected with O 2: - mild: Pa. O 2/FIO 2 200 -300 mm. Hg - moderate: 100 -200 mm. Hg - severe: < 100 mm. Hg
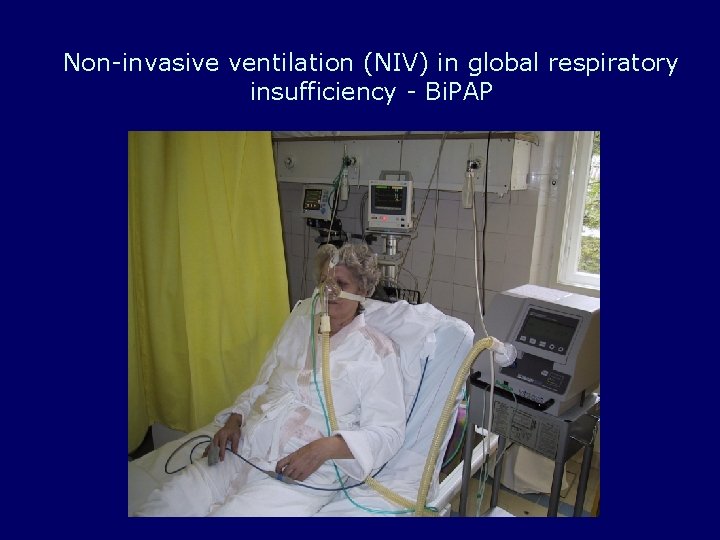
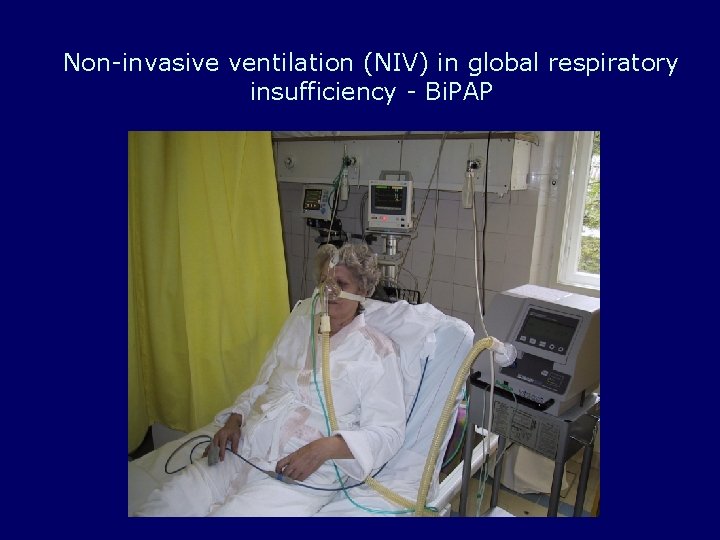
Non-invasive ventilation (NIV) in global respiratory insufficiency - Bi. PAP
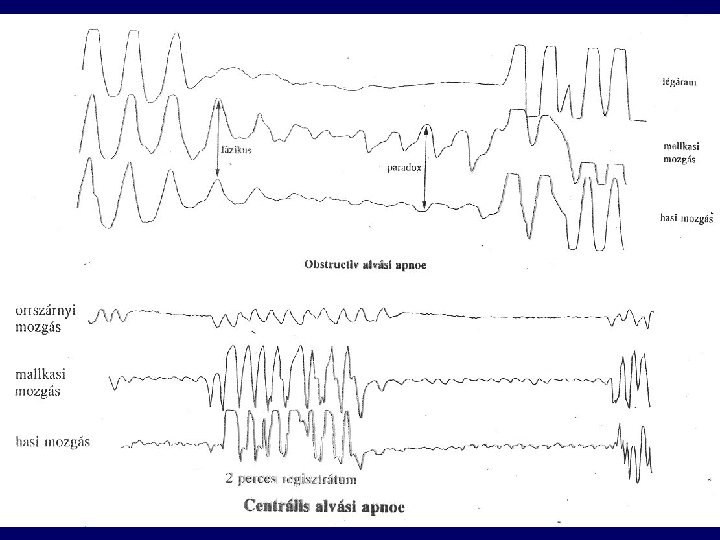
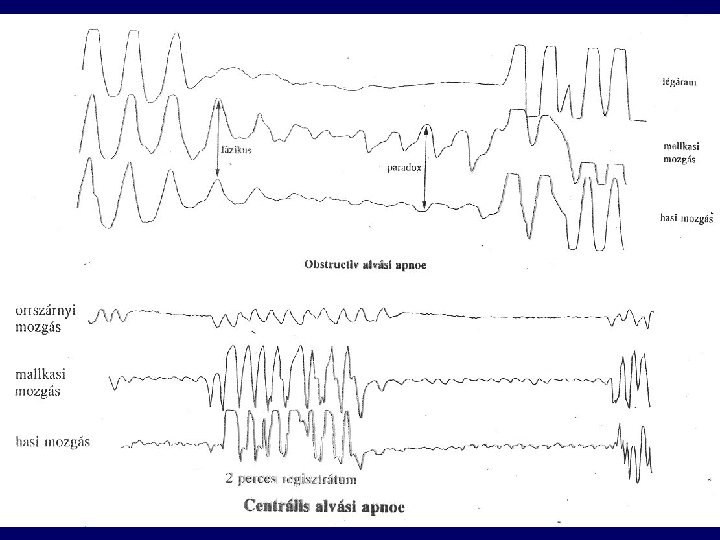
Sleep apnoe-hypopnoe syndrome (SAHS) • Dg: apnoe >5/h , >30/sleep period, SAT decrease: minimum 4% • Apnoe: > 10 s • Arousal (EEG) defraction of sleep • Apnoe index: Number of apnoe/h: <5 - mild: 5 -15 - moderate: 15 -30 - severe: >30
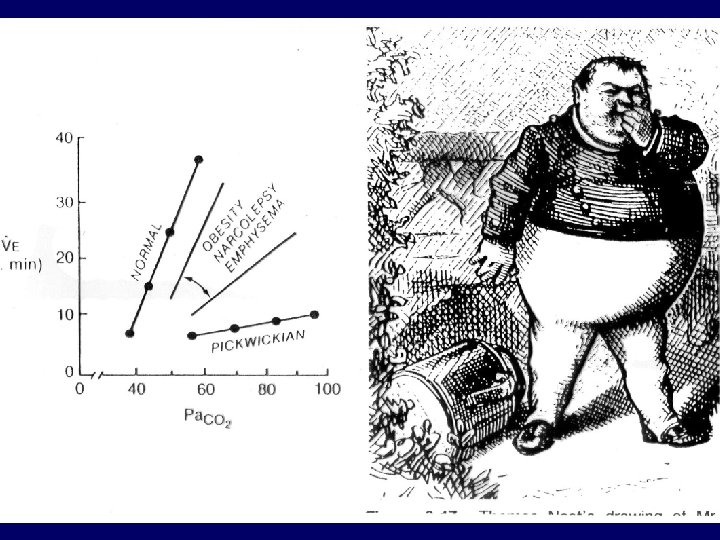
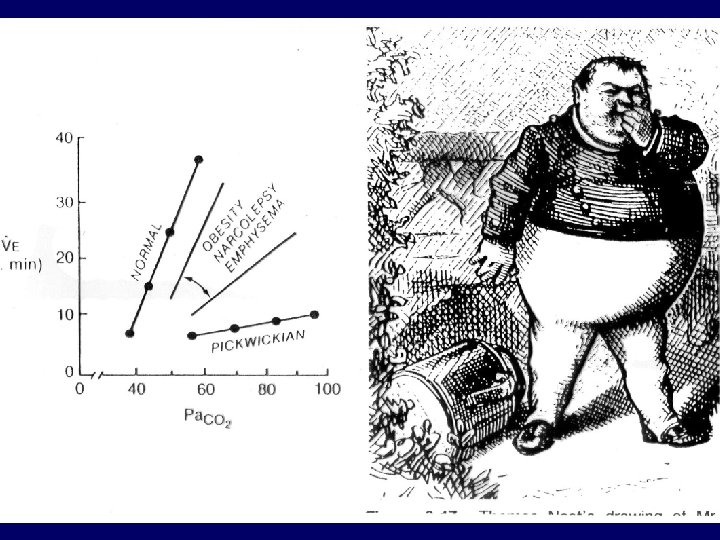
Types of SAHS • Central (kb. 5%) • Obstructive • Mixed Risk factors: - obesity - alcohol - sedatives
Symptoms of SAS • • • Daytime sleepiness Morning headache, tenebrosity Change in personality Strong hoarsness Movements during sleep Enuresis nocturna Impotency Hypertonia, arrhythmias Right heart failure
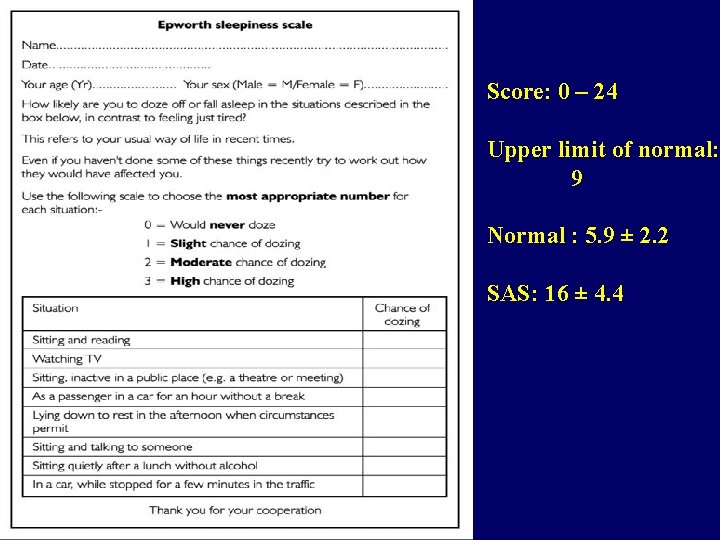
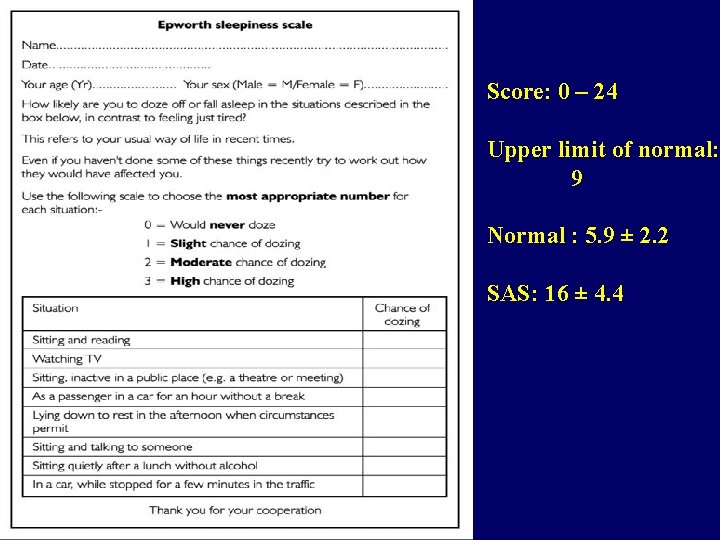
Score: 0 – 24 Upper limit of normal: 9 Normal : 5. 9 ± 2. 2 SAS: 16 ± 4. 4
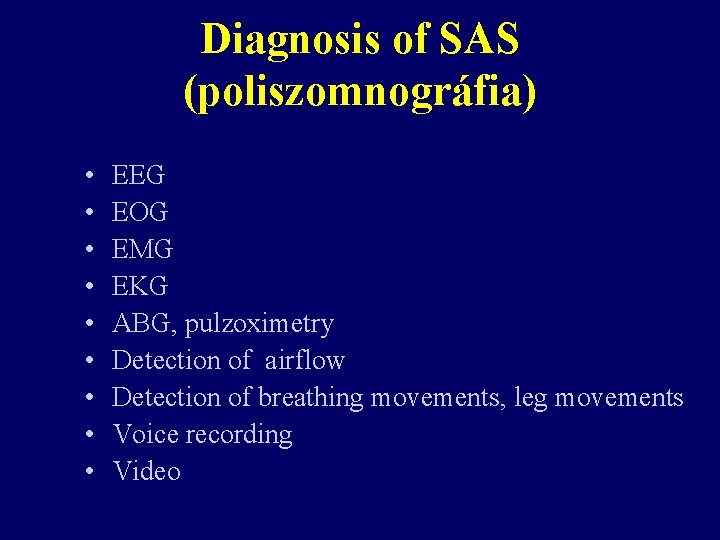
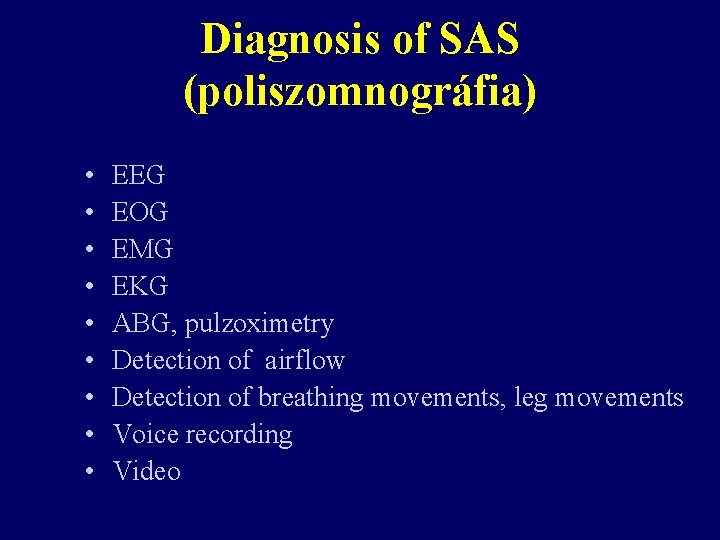
Diagnosis of SAS (poliszomnográfia) • • • EEG EOG EMG EKG ABG, pulzoximetry Detection of airflow Detection of breathing movements, leg movements Voice recording Video
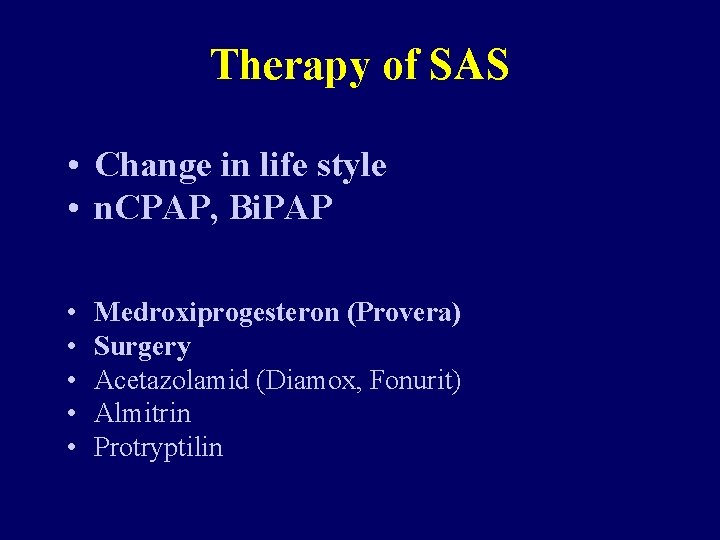
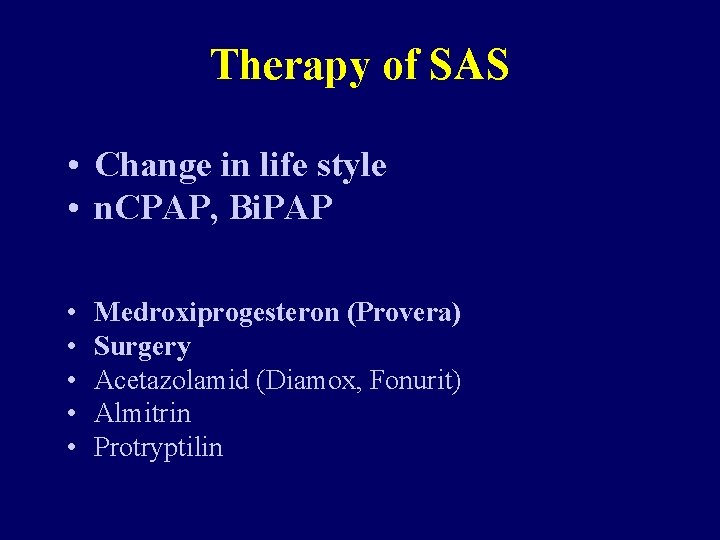
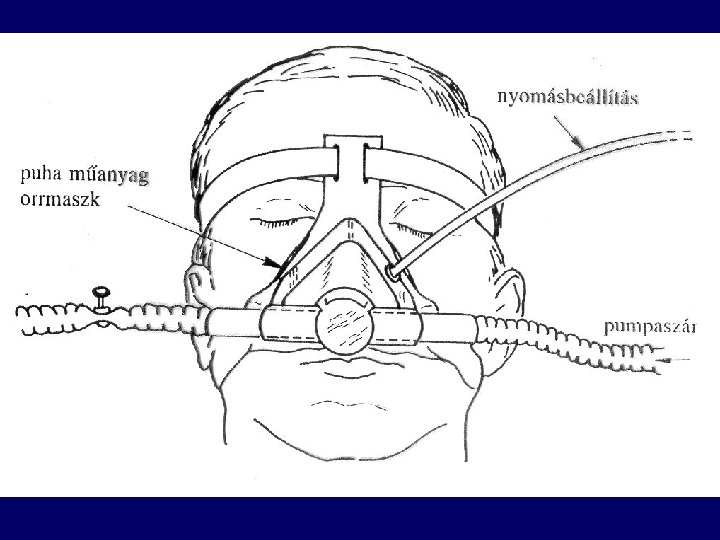
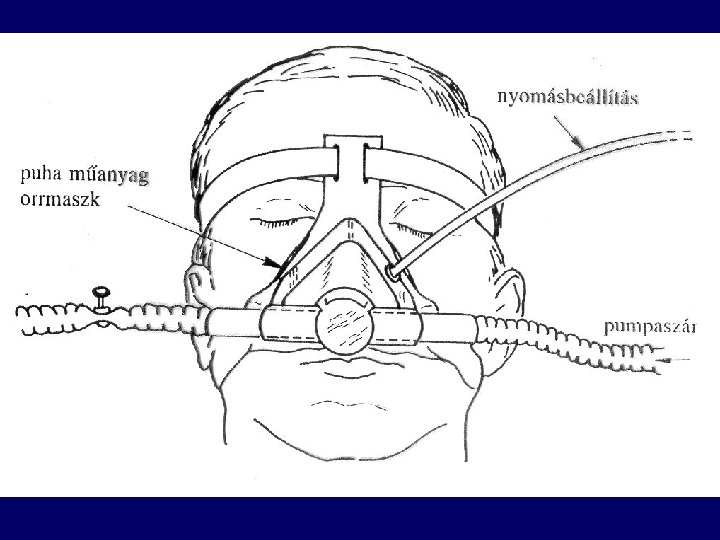
Therapy of SAS • Change in life style • n. CPAP, Bi. PAP • • • Medroxiprogesteron (Provera) Surgery Acetazolamid (Diamox, Fonurit) Almitrin Protryptilin
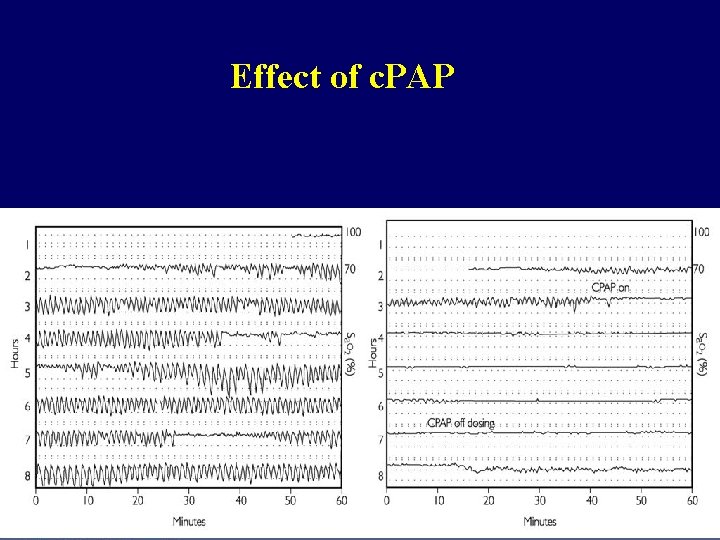
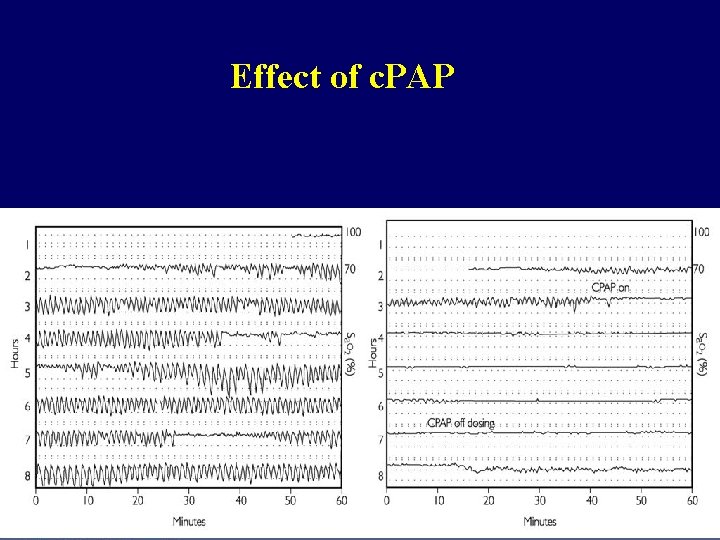
Effect of c. PAP
 Hypoxemy
Hypoxemy Conducting zone respiratory
Conducting zone respiratory Hac sahs
Hac sahs Sahs severo
Sahs severo Aspire sahs
Aspire sahs Eye lesions
Eye lesions Epi stool
Epi stool Convergence insufficiency latham
Convergence insufficiency latham Pseudo convergence insufficiency
Pseudo convergence insufficiency Passive insufficiency of hamstrings
Passive insufficiency of hamstrings Percussion test for venous insufficiency
Percussion test for venous insufficiency Active insufficiency
Active insufficiency Divergence insufficiency
Divergence insufficiency Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories شرح قصيدة come sleep بالعربي
شرح قصيدة come sleep بالعربي Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Module 23 sleep patterns and sleep theories
Module 23 sleep patterns and sleep theories Adults spend about ______% of their sleep in rem sleep.
Adults spend about ______% of their sleep in rem sleep. Reg és arany jános
Reg és arany jános Péter és jános az ékes kapuban
Péter és jános az ékes kapuban Nemcsók jános
Nemcsók jános Költői hitvallás
Költői hitvallás Burgess amputation
Burgess amputation Fültőmirigy elhelyezkedése
Fültőmirigy elhelyezkedése Rege a csodaszarvasról verselése
Rege a csodaszarvasról verselése Kis jános novella
Kis jános novella Harsányi jános főiskola
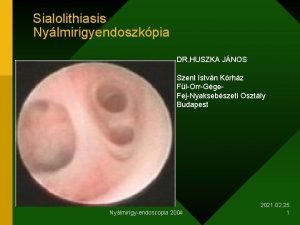
Harsányi jános főiskola Dr huszka jános
Dr huszka jános Tkrm
Tkrm Neumann jános informatikai kar
Neumann jános informatikai kar Dr huszka jános
Dr huszka jános Dr huszka jános vélemények
Dr huszka jános vélemények Efrir
Efrir