PULMONARY CIRCULATORY SYSTEM pulmonary circulatory system comprises of
- Slides: 26
PULMONARY CIRCULATORY SYSTEM
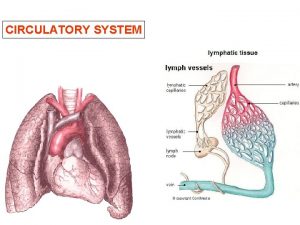
pulmonary circulatory system comprises of: • • 1. The Pulmonary vessels • 2. The Bronchial vessels • 3. The Lymphatics
1. Pulmonary Vessels • Pulmonary artery takes deoxygenated blood from the heart to the lungs whereas pulmonary veins bring oxygented blood from the lungs to heart.
2. The Bronchial Vessels • They supply the supporting tissues of the lungs, including the connective tissue, the septa and the large & small bronchi. • The bronchial arterial tree is oxygenated.
3. The Lymphatics • Lymphatics extends from all tissues of the lung upto the hilum where they form right and left lymphatic duct.
PRESSURES IN PULMONARY ARTERY
PRESSURE IN PULMONARY ARTERY • Systolic pulmonary arterial pressure 25 mm Hg • Diastolic arterial pulmonary pressure 08 mm Hg • Mean pulmonary arterial pressure 15 mm Hg
PULMONARY ARTERIAL PRESSURE • Approximately 17 mm. Hg.
PULMONARY CAPILLARY PRESSURE • Approximately 07 mm Hg
LEFT ATRIAL & PULMONARY VENOUS PRESSURES • Approximately 02 mm Hg in left atrium & Pulmonary veins.
PULMONARY WEDGE PRESSURE • This pressure is measured by inserting a catheter through right side of the heart & the pulmonary artery into one of the small branches of pulmonary arteries and then pushing the catheter until it wedges tightly in the artery. • The pressure then measured is called WEDGE PRESSURE. It is about 05 mm Hg.
ZONES OF PULMONARY BLOOD FLOW
1. ZONE 1 • In this zone of lungs NO blood flow at all during any part of the cardiac cycle.
2. ZONE 2 • It is the zone of intermittent blood flow. • During this pulmonary arterial pressure peaks BECAUSE the systolic pressure is greater than the alveolar pressure. • This zone is found in apices of lungs.
3. ZONE 3 • It is the zone of continuous blood flow BECAUSE the alveolar capillary pressure remains greater than the alveolar pressure during the entire cardiac cycle. • This zone is found in lower areas of lung.
NORMAL • Normally lungs have only zone 2 and 3 blood flow.
PULMONARY CIRCULATION WHEN LEFT ATRIAL PRESSURE RISES • An initial increase in left atrial pressure upto about 7 to 8 mm Hg has no effect on pulmonary pressure. • BUT any increase above this level in left atrial pressure increases pulmonary capillary pressure almost equally. • As a result due to raised pulmonary capillary pressure, pulmonary edema may result.
PULMONARY EDEMA • DEFINITION: The accumulation of free fluid in the pulmonary interstitial spaces.
MECHANISM • Any factor that causes the pulmonary interstitial fluid pressure to rise from negative range into the positive range, will cause sudden filling of the pulmonary interstitial spaces and even the alveoli.
CAUSES OF PULMONARY EDEMA • 1. Left heart failure • 2. Mitral valve disease • 3. Pneumonia
FACTORS THAT PREVENT THE DEVELOPMENT OF PULMONARY EDEMA • 1. Normal negativity of the interstitial fluid pressure of the lungs. • 2. The lymphatic pumping of the fluid out of the interstitial spaces. • 3. The increased osmosis of fluid into the pulmonary capillaries caused by decreased protein in the interstitial fluid.
FLUIDS IN PLEURAL CAVITY • The TOTAL AMOUNT of fluid in each pleural cavity is appox. 5 ml. • This amount usually remains small because all the excess is pumped away by lymphatic vessels opening directly from the pleural cavity into: • 1. The mediastinum. • 2. The superior surface of diaphragm. • 3. The lateral surfaces of parietal pleura.
CAUSE OF NEGATIVE PRESSURE IN PLEURAL SPACE • It is due to the pumping of fluid from the space by the lymphatics. • VALUE: -7 mm Hg
SIGNIFICANCE OF NEGATIVE PRESSURE IN PLEURAL SPACE • The NEGATIVITY of the pleural fluid pressure keeps the lungs pulled tightly against the parietal pleura of the chest cavity.
PLEURAL EFFUSION • It is the COLLECTION of large amounts of free fluid in the pleural space.
CAUSES OF PLEURAL EFUSION • 1. Blockage of lymphatic drainage from the pleural cavity. • 2. Cardiac failure. • 3. Reduced plasma colloid osmotic pressure. • 4. Infection or inflammation of pleural surfaces of the pleural cavity.
 Respiratory system circulatory system digestive system
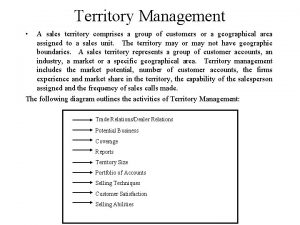
Respiratory system circulatory system digestive system Territory management definition
Territory management definition Happiness sadness anger fear disgust
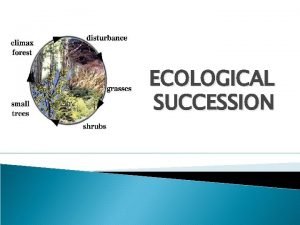
Happiness sadness anger fear disgust Secondary succesion
Secondary succesion Css comprises of style rules that are interpreted
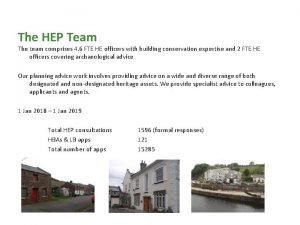
Css comprises of style rules that are interpreted Team comprises of
Team comprises of Comprises 70% of business entities in the united states
Comprises 70% of business entities in the united states Archaea
Archaea Typical gd comprises of a small group of candidates
Typical gd comprises of a small group of candidates Farm management meaning
Farm management meaning Tiny air sacs at the end of the bronchioles
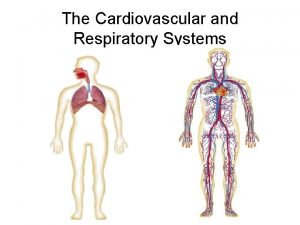
Tiny air sacs at the end of the bronchioles Circulatory system and respiratory system work together
Circulatory system and respiratory system work together Systemic circulation flow chart
Systemic circulation flow chart Circulatory system steps in order
Circulatory system steps in order Superchp
Superchp Circulatory system of lungfish
Circulatory system of lungfish Clams open circulatory system
Clams open circulatory system Horse heart
Horse heart Veinioles
Veinioles Closed circulatory system
Closed circulatory system Parts of circulatory system
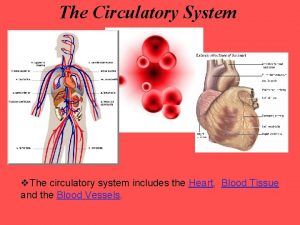
Parts of circulatory system 3 main parts of circulatory system
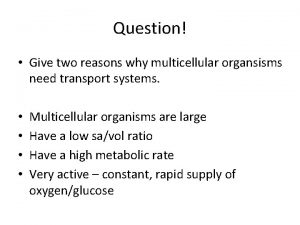
3 main parts of circulatory system Active animals
Active animals How circulatory system work
How circulatory system work What makes up the cardiovascular system
What makes up the cardiovascular system The actual exchange of gases occurs at the site of the *
The actual exchange of gases occurs at the site of the * Single vs double circulatory system
Single vs double circulatory system