Progress Notes AODSPSYCSOC 255 Progress Notes There are



- Slides: 18
Progress Notes AODS/PSYC/SOC 255
Progress Notes There are several “styles” of progress notes: SOAP DAP BIRP
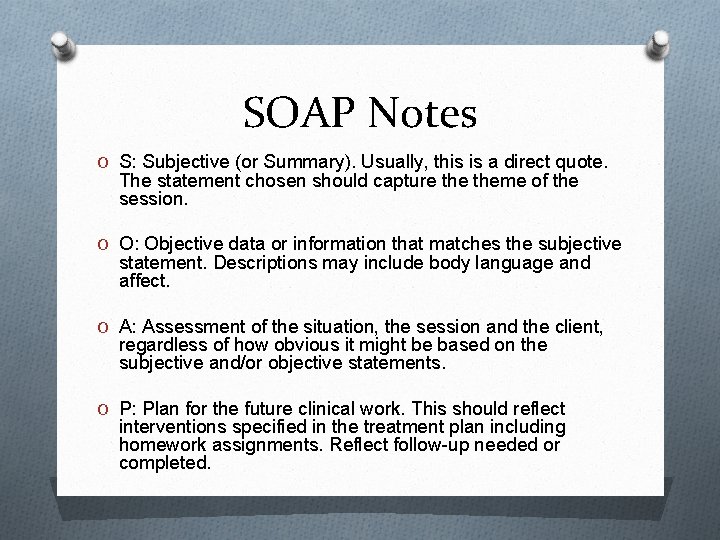
SOAP Notes O S: Subjective (or Summary). Usually, this is a direct quote. The statement chosen should capture theme of the session. O O: Objective data or information that matches the subjective statement. Descriptions may include body language and affect. O A: Assessment of the situation, the session and the client, regardless of how obvious it might be based on the subjective and/or objective statements. O P: Plan for the future clinical work. This should reflect interventions specified in the treatment plan including homework assignments. Reflect follow-up needed or completed.
Sample SOAP Note O Met with pt for initial session of 15 minutes O S: Pt reported that she is having trouble cutting down her drinking. She shared how her drinking increases as her stress increases. She stated that her three children are the main source of her stress. She reported eating drinking ‘between 3 -5 drinks per evening”. We discussed what it would look like to share this her drinking difficulties with her husband to seek support for her drinking behaviors.
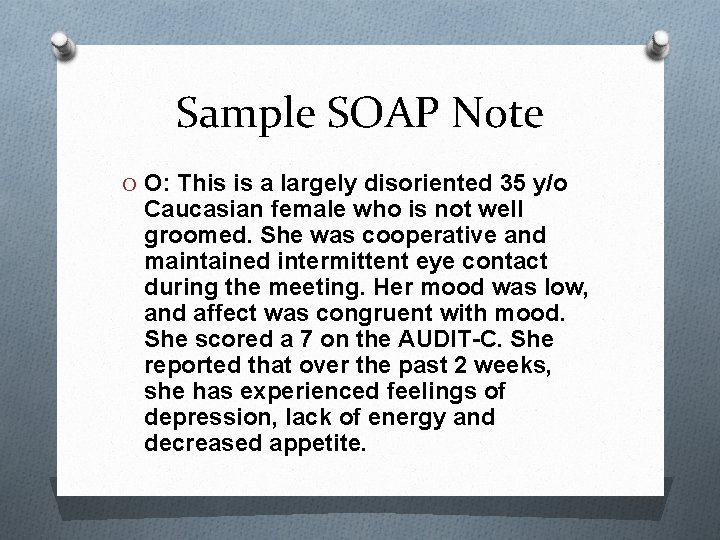
Sample SOAP Note O O: This is a largely disoriented 35 y/o Caucasian female who is not well groomed. She was cooperative and maintained intermittent eye contact during the meeting. Her mood was low, and affect was congruent with mood. She scored a 7 on the AUDIT-C. She reported that over the past 2 weeks, she has experienced feelings of depression, lack of energy and decreased appetite.
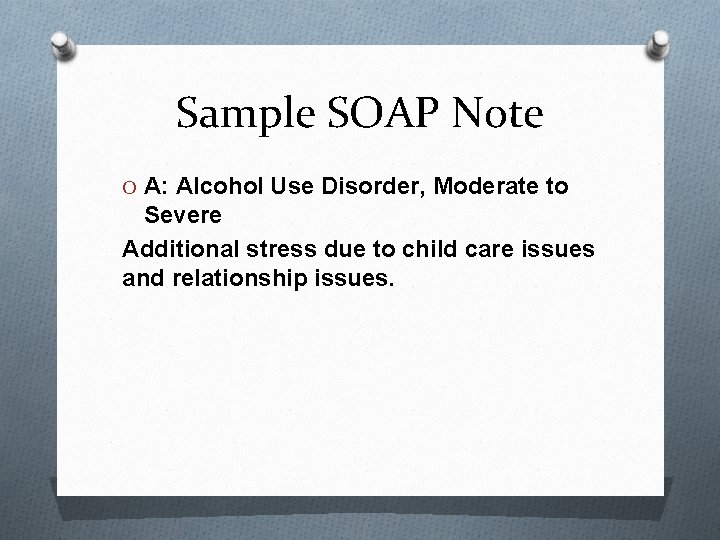
Sample SOAP Note O A: Alcohol Use Disorder, Moderate to Severe Additional stress due to child care issues and relationship issues.
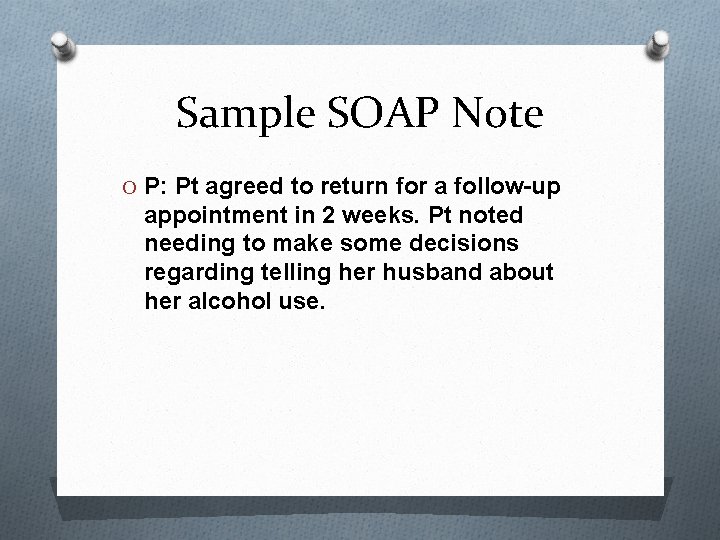
Sample SOAP Note O P: Pt agreed to return for a follow-up appointment in 2 weeks. Pt noted needing to make some decisions regarding telling her husband about her alcohol use.
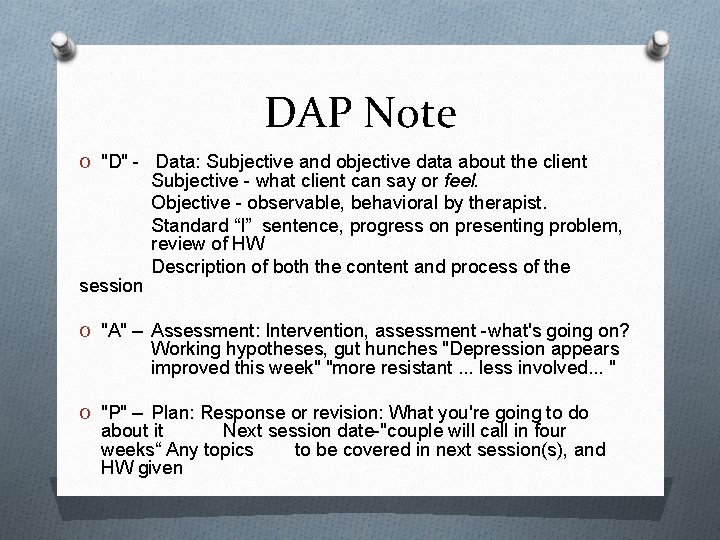
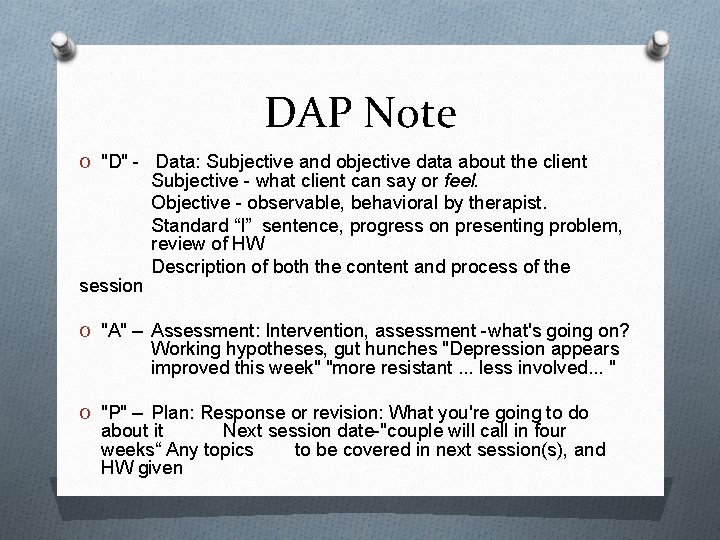
DAP Note O "D" - Data: Subjective and objective data about the client session Subjective - what client can say or feel. Objective - observable, behavioral by therapist. Standard “I” sentence, progress on presenting problem, review of HW Description of both the content and process of the O "A" – Assessment: Intervention, assessment -what's going on? Working hypotheses, gut hunches "Depression appears improved this week" "more resistant. . . less involved. . . " O "P" – Plan: Response or revision: What you're going to do about it Next session date-"couple will call in four weeks“ Any topics to be covered in next session(s), and HW given
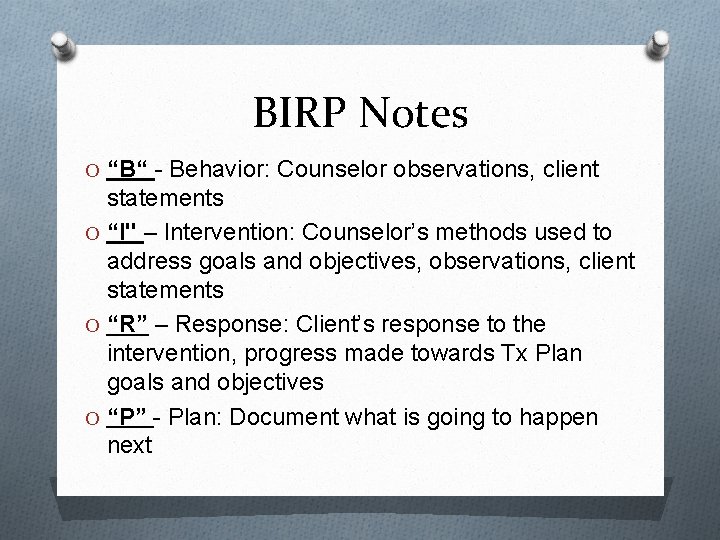
BIRP Notes O “B“ - Behavior: Counselor observations, client statements O “I" – Intervention: Counselor’s methods used to address goals and objectives, observations, client statements O “R” – Response: Client’s response to the intervention, progress made towards Tx Plan goals and objectives O “P” - Plan: Document what is going to happen next
Writing Treatment Plans

Treatment Planning O TREATMENT PLANNING: Process by which the counselor and the client identify and rank problems needing resolution; establish agreed upon immediate and long-term goals; and decide upon a treatment process and the resources to be utilized. O Explain assessment results to client in an understandable manner. O Identify and rank problems based on individual client needs in the written treatment plan. O Formulate agreed upon immediate and long-term goals using behavioral terms in the written treatment plan. O Identify the treatment methods and resources to be utilized as appropriate for the individual client.

Treatment Plan O The treatment plan serves as a guide for the client work, assisting both the client and the counselor in keeping a balanced focus on issues. It also helps the client and counselor prioritize issues that need to be addressed. O Addicted clients can present with both complicated and extensive problems, the treatment plan can prevent both the client and counselor from becoming overwhelmed in therapy process.
Treatment Plan O Guides the treatment process O It is dependent on screening O Who will be involved or informed? O Generally includes a “problem list” O Generally includes goals and time frame
Treatment Considerations O Are the client’s problems acute or chronic? O What limitations may impede services; such as; finances, transportation, employment, etc. O Does the seriousness of the client’s situation demonstrate the need for a structured inpatient environment? O Can the client’s concerns be handled on an outpatient basis?

Treatment Considerations O Are there requirements from the legal system? O Will the client need short or long term services? O Do you need to collaborate with other professionals? O Are there presenting problems outside of your scope of practice? O What are the client’s strengths? O Any special needs to be addressed?
Samples Abstinence: O Obtain and maintain sobriety O Live a chemical-free life O Cope with life without chemicals. Controlled drinking: O Follow patterns of use that reduce harm. O Stabilize one's health, finances, vocation/school, employment, living arrangements. O Complete a physical examination as prescribed and comply with medical advice. O Enhance health and fitness. O Resolve and avoid legal problems. O Develop sober leisure skills. Stabilize one's intimate relationships, marriage, family. O Include significant others such as spouse/partner, children, relatives, friends, etc. , in the recovery program as prescribed. O Improve social skills, assertiveness, emotional expression, communication.
Samples O Improve social support, friendships, social pursuits. Deal/cope with/resolve emotional problems/feelings such as rejection, depression, unresolved grief/mourning, shame, guilt, abandonment. O Improve coping skills, stress management skills, relaxation abilities, self-control. O Enhance self-esteem, confidence, and self-acceptance. Accept responsibility for the consequences of one's behavior. O Improve problem-solving ability, setting of priorities, persistence, frustration tolerance. O Be an active participant in the treatment program by attending/participating in: Scheduled education classes about chemical dependency and the process of recovery. O Scheduled counseling, psychotherapy, and educational groups (e. g. spirituality groups, men's and women's groups, etc. ). O Recreational activities to expand pleasures of physical activity, healthy competition, skill acquisition, socializing, interest areas, etc.
Samples O Prepare an aftercare plan, including a daily plan, home group meetings, and attendance at (#) of meetings per week for a total of (#) meetings/weeks/days. O Recognize and plan to prevent how becoming Hungry, Angry, Lonely, Tired (HALT) leads to drinking. O Identify high-risk situations, warning signs, and triggers; rehearse coping responses O Write a relapse prevention plan for oneself; teach relapse prevention to others. O Develop multiple alternatives to chemical use for high-risk situations