Preoperative Pulmonary Function Evaluation in Lung Resection Ri
- Slides: 23
Preoperative Pulmonary Function Evaluation in Lung Resection Ri 李佩蓉/王奐之 CR 顏郁軒
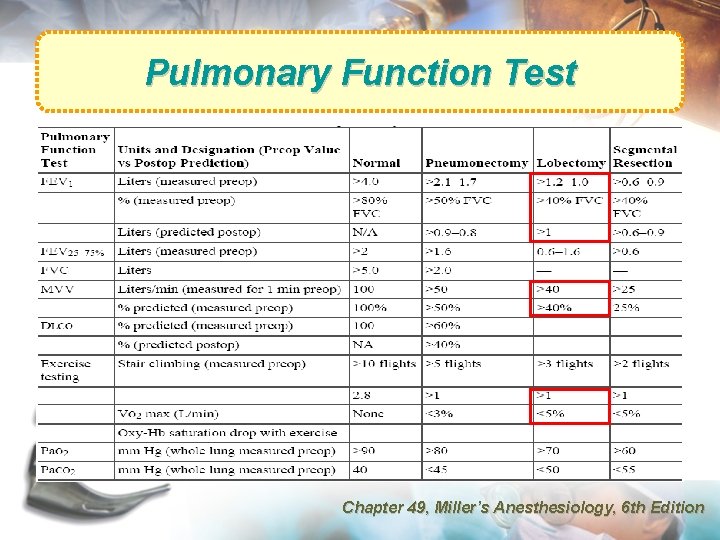
Pulmonary Function Test • Preoperative pulmonary evaluation of patients with lung cancer concerns both resectability and operability. – resectability: TNM staging – operability: how much tissue can be safely removed
Commonly Used Parameters • FEV 1 (Forced Expiratory Volume in 1 second) – FVC (Functional Vital Capacity) – FEV 1/FVC • MVV (Maximum Voluntary Ventilation) = MBC (Maximum Breathing Capacity) • DLCO (Diffusing Capacity of Carbon Monoxide) • VO 2 max (Maximum Oxygen Consumption)
FEV 1 • best parameter to predict risk of post-op complications (including death) • ppo. FEV 1 (predicted postoperative FEV 1) Am J of Med (2005) 118, 578– 583 Chest (2003) 123, 2096 -2103 Resp Med (2004) 98, 598 -605
MVV (MBC) • largest volume breathed voluntarily in 1 min • an estimate of the peak ventilation available to meet physiological demands • represents respiratory muscle strength and correlates with post-op morbidity Am J of Med (2005) 118, 578– 583 Chest (2003) 123, 2096 -2103 Resp Med (2004) 98, 598 -605
DLCO • independent predictor for risk of post-op complications (including death) • reflects alveolar membrane integrity and pulmonary capillary blood flow • low DLCO implies significant emphysema, and reduced pulmonary capillary vascular bed Am J of Med (2005) 118, 578– 583 Chest (2003) 123, 2096 -2103 Resp Med (2004) 98, 598 -605
VO 2 max (Exercise Test) • exercise capacity (measured as VO 2 max) • predictor of post-op complications (including death) – – exercise oximetry stair climbing shuttle walking 6 -minute walk test • helps to identify high-risk patients who can safely undergo lung resection Am J of Med (2005) 118, 578– 583
VO 2 max Eugene et al • VO 2 max > 1 L/min little complications Smith et al • VO 2 max > 20 ml/kg/min post-op complications 10% • VO 2 max = 15~20 ml/kg/min post-op complications 66% • VO 2 max < 15 ml/kg/min post-op complications 100% Markos et al • oxygen desaturation during a 12 -min walk, ppo. DLCO and ppo. FEV 1 were more reliable predictors of post-op mortality Chest (2003) 123, 2096 -2103
Other Parameters • FEF 25 -75%: highly variable • ABG: hypercapnia (>45 mm. Hg) • PPP (predicted postoperative product) – product of ppo. FEV 1 and ppo. DLCO Am J of Med (2005) 118, 578– 583
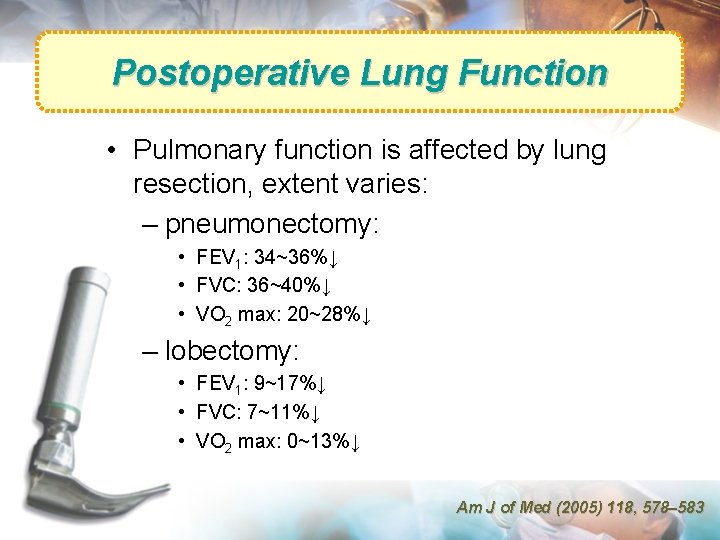
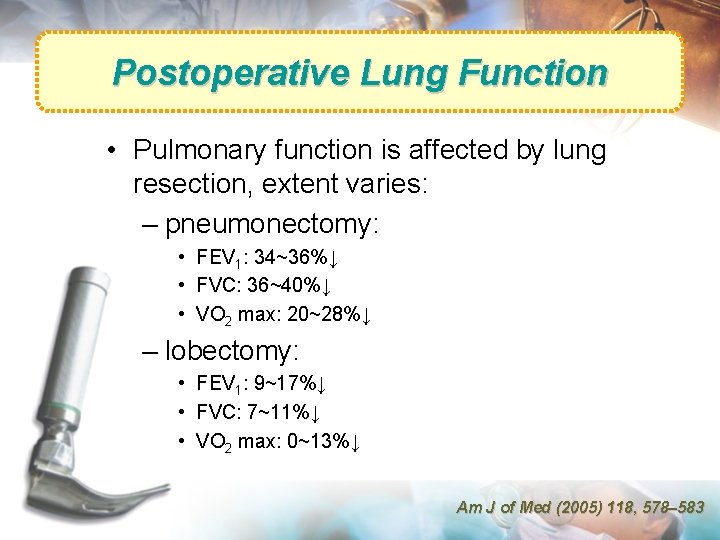
Postoperative Lung Function • Pulmonary function is affected by lung resection, extent varies: – pneumonectomy: • FEV 1: 34~36%↓ • FVC: 36~40%↓ • VO 2 max: 20~28%↓ – lobectomy: • FEV 1: 9~17%↓ • FVC: 7~11%↓ • VO 2 max: 0~13%↓ Am J of Med (2005) 118, 578– 583
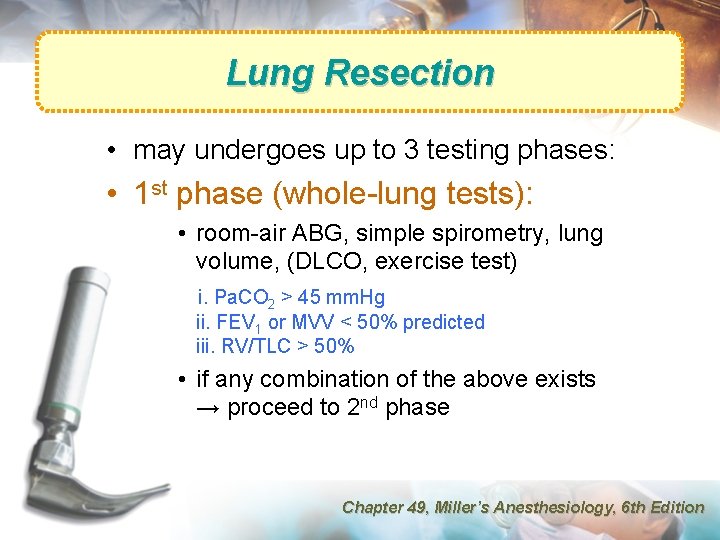
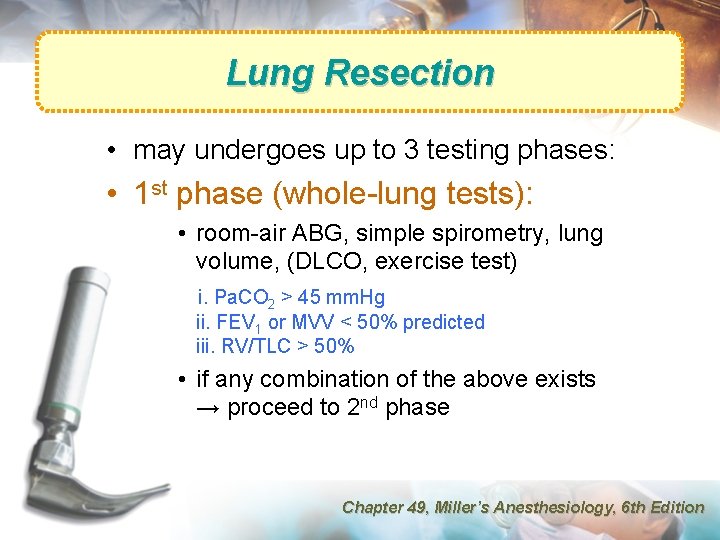
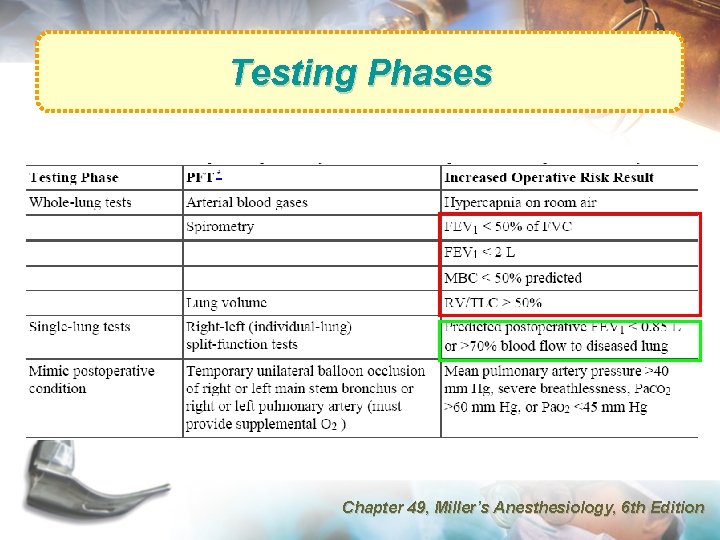
Lung Resection • may undergoes up to 3 testing phases: • 1 st phase (whole-lung tests): • room-air ABG, simple spirometry, lung volume, (DLCO, exercise test) i. Pa. CO 2 > 45 mm. Hg ii. FEV 1 or MVV < 50% predicted iii. RV/TLC > 50% • if any combination of the above exists → proceed to 2 nd phase Chapter 49, Miller’s Anesthesiology, 6 th Edition
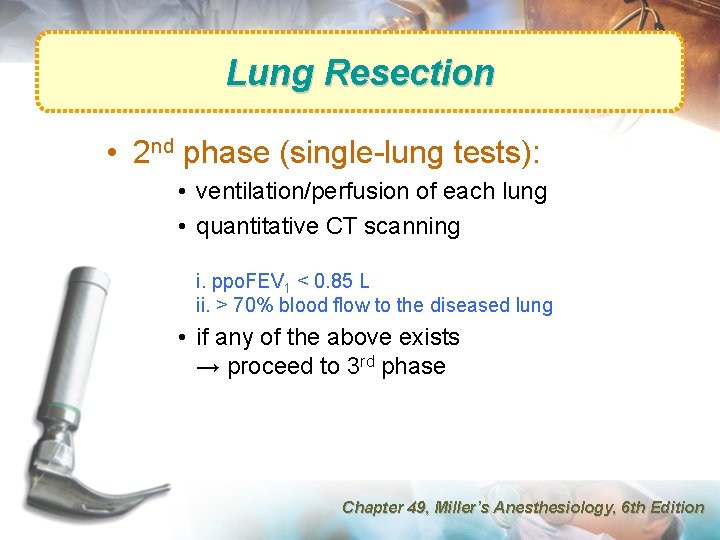
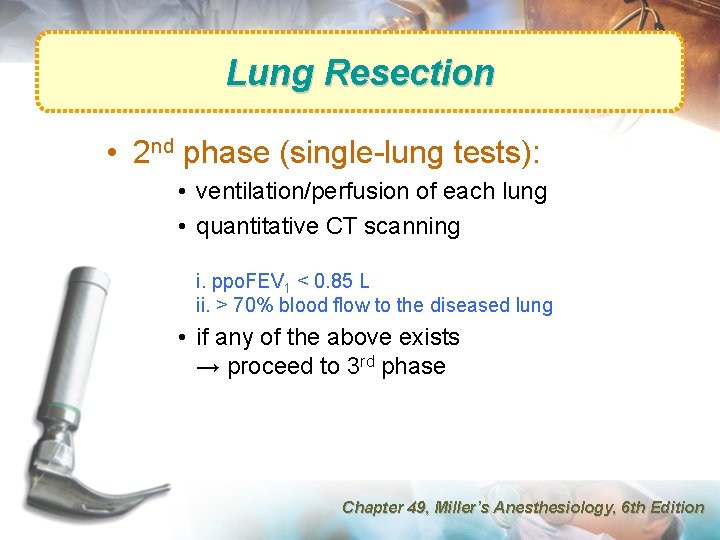
Lung Resection • 2 nd phase (single-lung tests): • ventilation/perfusion of each lung • quantitative CT scanning i. ppo. FEV 1 < 0. 85 L ii. > 70% blood flow to the diseased lung • if any of the above exists → proceed to 3 rd phase Chapter 49, Miller’s Anesthesiology, 6 th Edition
Prediction of Post-op Lung Function • Methods to predict postoperative pulmonary function: – segment method – radionuclide scanning techniques – quantitative computed tomography
Segment Method • 19 total segments (right 10, left 9) • estimated post-op pulmonary function = (pre-op pulmonary function) * (post-op remaining segments) / 19 • subsegments also being used (total of 42 subsegments) Am J of Med (2005) 118, 578– 583
Radionuclide Scanning Techniques • inhaled 133 Xe or intravenous 99 Tc-labeled macroaggregates • estimation by quantifying the perfusion to a specific area: ppo. FEV 1 = preoperative FEV 1 * % of radioactivity contributed by nonoperated lung Am J of Med (2005) 118, 578– 583
Quantitative Computed Tomography • -500~-910 Hounsfield unit is used to estimate functional lung volume • correlates better than radionuclide scanning method AJR (2002) 178, 667– 672
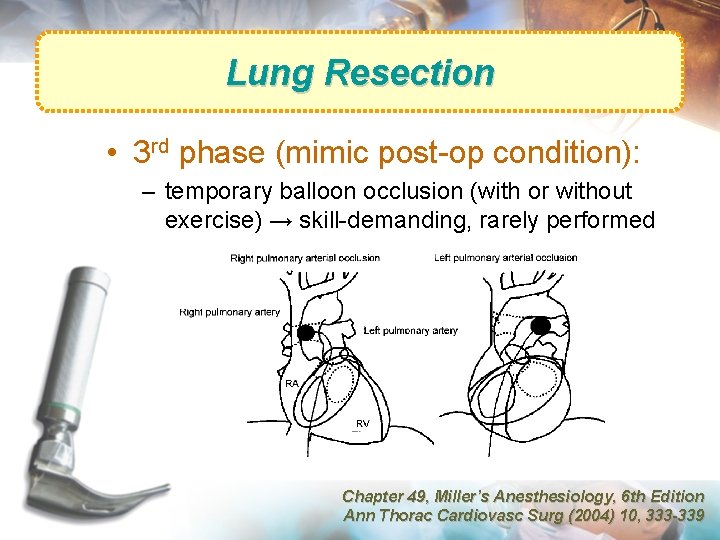
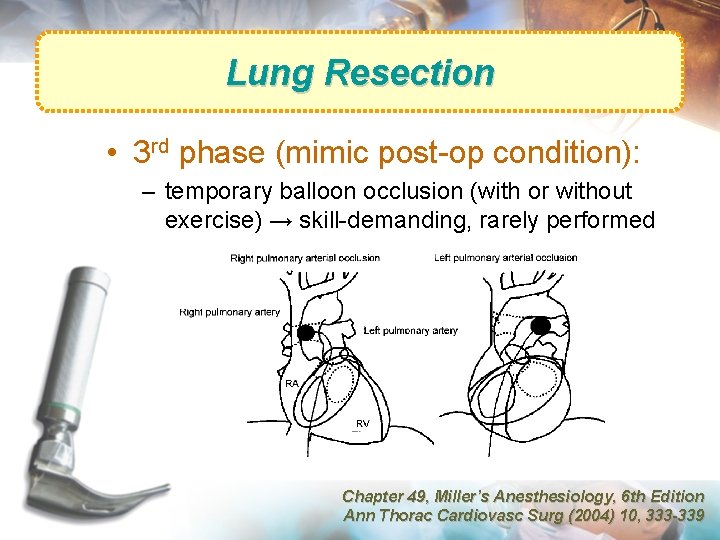
Lung Resection • 3 rd phase (mimic post-op condition): – temporary balloon occlusion (with or without exercise) → skill-demanding, rarely performed Chapter 49, Miller’s Anesthesiology, 6 th Edition Ann Thorac Cardiovasc Surg (2004) 10, 333 -339
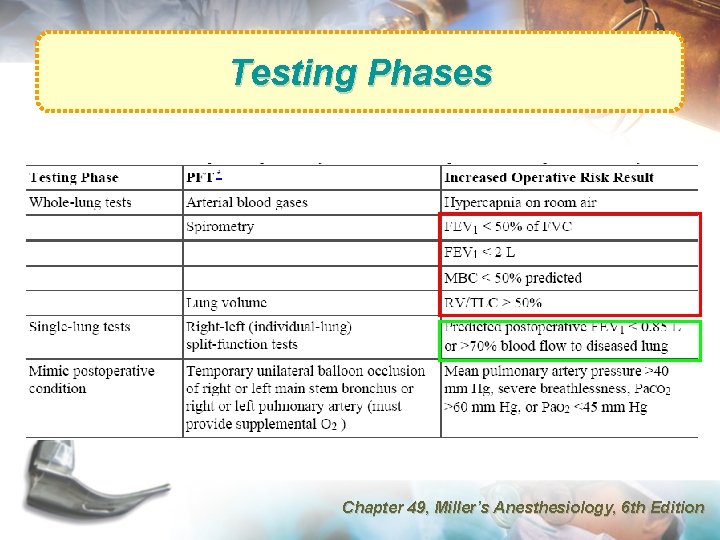
Testing Phases Chapter 49, Miller’s Anesthesiology, 6 th Edition
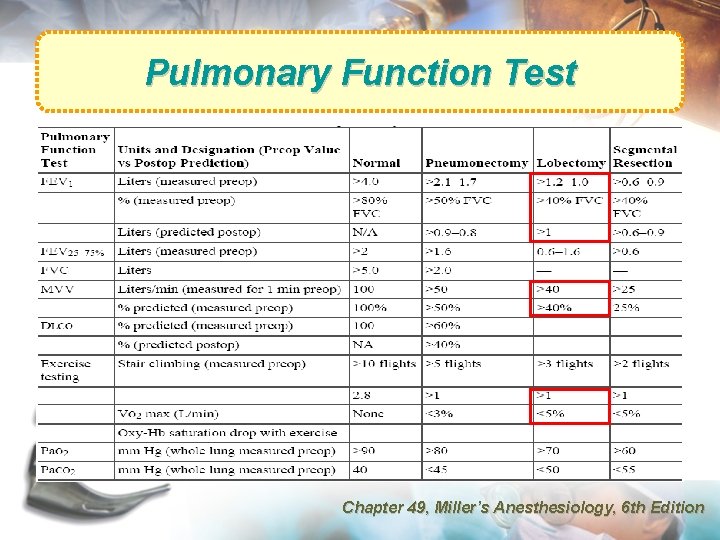
Pulmonary Function Test Chapter 49, Miller’s Anesthesiology, 6 th Edition
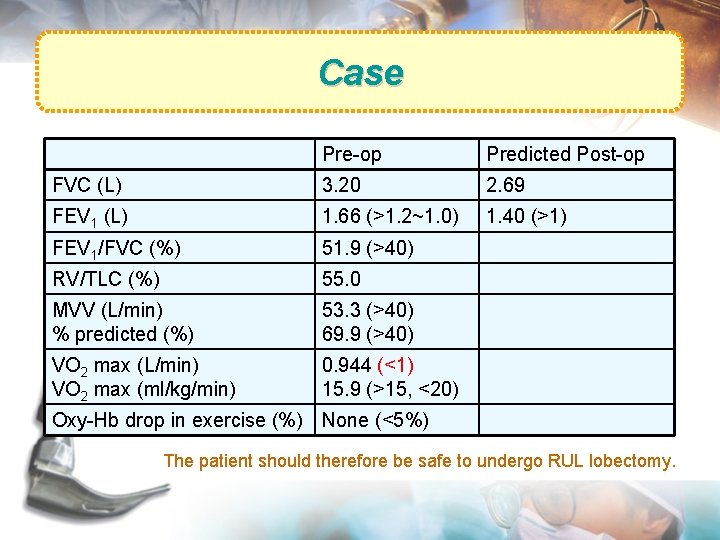
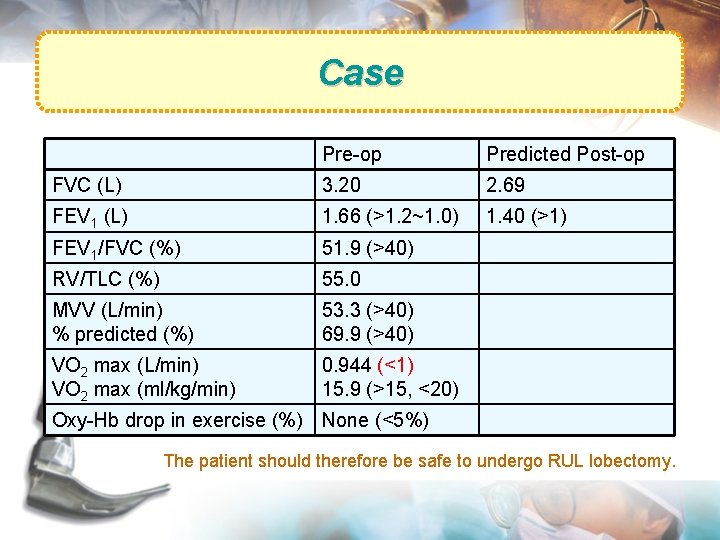
Case Pre-op Predicted Post-op FVC (L) 3. 20 2. 69 FEV 1 (L) 1. 66 (>1. 2~1. 0) 1. 40 (>1) FEV 1/FVC (%) 51. 9 (>40) RV/TLC (%) 55. 0 MVV (L/min) % predicted (%) 53. 3 (>40) 69. 9 (>40) VO 2 max (L/min) VO 2 max (ml/kg/min) 0. 944 (<1) 15. 9 (>15, <20) Oxy-Hb drop in exercise (%) None (<5%) The patient should therefore be safe to undergo RUL lobectomy.
Reference 1. Anesthesia for thoracic surgery, Miller: Miller’s Anesthesiology (2005) 6 th Edition, chapter 49 2. Pulmonary function testing, Miller: Miller’s Anesthesiology (2005) 6 th Edition, chapter 26 3. Mazzone et al. , Lung cancer: preoperative pulmonary evaluation of the lung resection candidate. Am J of Med (2005) 118, 578– 583 4. Datta et al. , Preoperative evaluation of patients undergoing lung resection surgery. Chest (2003) 123, 2096 -2103 5. Wang et al. , Pulmonary function tests in preoperative pulmonary evaluation. Resp Med (2004) 98, 598 -605 6. Tanita et al. , Review of preoperative functional evaluation for lung resection using the right ventricular hemodynamic functions. Ann Thorac Cardiovasc Surg (2004) 10, 333339 7. Wu et al. , Prediction of postoperative lung function in patients with lung cancer: comparison of quantitative CT with perfusion scintigraphy. AJR (2002) 178, 667 -672
Thank you for your attention!
predicted VO 2 = 5. 8 * weight in kg + 151 + 10. 1 (W of workload)