POST OPERATIVE CARE Crystal Pietrowski 7 NT Staff

- Slides: 22

POST OPERATIVE CARE Crystal Pietrowski 7 NT Staff RN/Nurse Educator Nicole Ladwig 8 NT Staff RN/Nurse Educator
Objectives Identify common things to monitor for in the post- operative patient Identify what can be done to prevent postoperative complications
Background Observation studies suggest that deterioration or patients on general medical/surgical wards is often preceded by changes in physiological observations that are recorded by clinical staff 624 hours prior to a serious adverse event (Thornlow, 2009). Most commonly changes are in respiratory rate, pulse, hypoxemia, dyspnea and alterations in mental status.
Pain Multimodal analgesia is utilized Various forms of pain medication: Epidural, PCA pump, IV Tylenol, IV ketamine, IV push medications Heat/Ice if ok per MD Distraction Repositioning Rest/Relaxation Techniques Monitor of over sedation Impaired renal and hepatic function may further affect the metabolism and excretion of may opioids, leading to prolonged exposure and increased side effects (Thornlow, 2009). Be cautious in older adult If pain is not adequately controlled: Patients may develop atelectasis, hypoxemia and respiratory distress (Thornlow, 2009). Patients may not engage in early ambulation and deep breather exercises (Thornlow, 2009). Patients can splint incision with pillow or blanket while doing activity/ coughing and deep breathing.
Bleeding Signs/Symptoms HR, BP, diaphoretic Watch labs- decreasing H&H Watch for blood in urine, blood in stool, increased bloody drainage from a drain or incision site
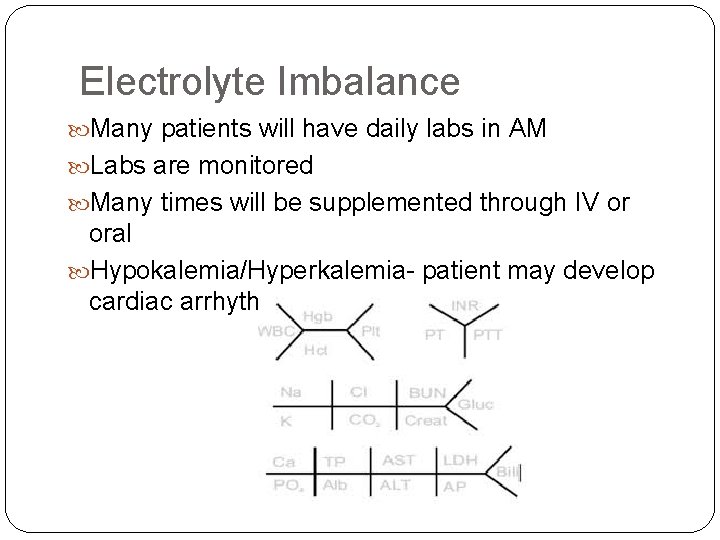
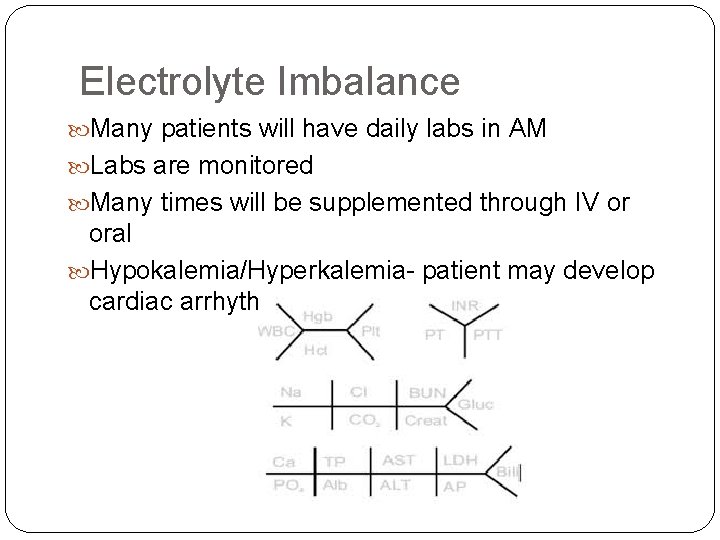
Electrolyte Imbalance Many patients will have daily labs in AM Labs are monitored Many times will be supplemented through IV or oral Hypokalemia/Hyperkalemia- patient may develop cardiac arrhythmias
Blood Clots Early ambulation SCDs – effective when worn for at least 20 hours in a day Anticoagulation: Heparin/Lovenox/aspirin Think if patient might need Lovenox at home- start teaching early Lovenox teaching kits available on most units Signs/Symptoms of a blood clot PE: SOB, Chest Pain, Cough DVT: Swelling in the affected leg. Rarely, there may be swelling in both legs. Pain and erythema in the leg. The pain often starts in the calf and can feel like cramping or a soreness.
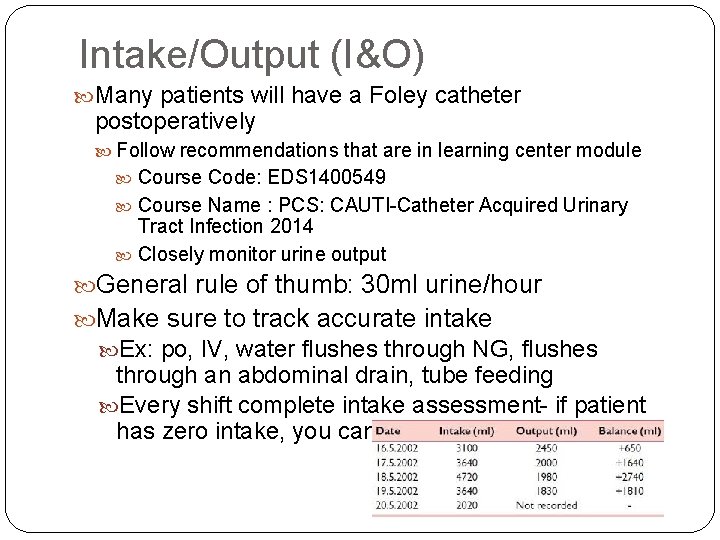
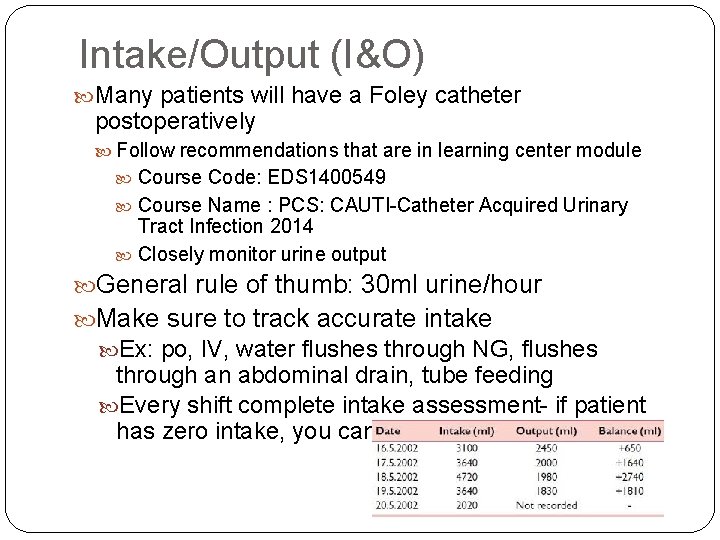
Intake/Output (I&O) Many patients will have a Foley catheter postoperatively Follow recommendations that are in learning center module Course Code: EDS 1400549 Course Name : PCS: CAUTI-Catheter Acquired Urinary Tract Infection 2014 Closely monitor urine output General rule of thumb: 30 ml urine/hour Make sure to track accurate intake Ex: po, IV, water flushes through NG, flushes through an abdominal drain, tube feeding Every shift complete intake assessment- if patient has zero intake, you can document “ 0” in EPIC
Respiratory Status Pay attention to fluid status Educate patient on Incentive Spirometry Use teachback method Recommend Incentive Spirometry/Coughing and Deep Breathing Activity will promote lung expansion
Nutrition Proper nutrition promotes wound healing Important to monitor nutritional status Poor nutrition can contribute to skin breakdown Need MD order for supplements Some patients sole nutrition will be TPN or TF Diet will progress slowly NPO Clears Fulls Goal (General, low fiber, etc. ) Diet goal varies- sometimes will be different from baseline/prior to admission Recommend soft/bland/non-greasy foods as they advance
Skin Full Skin Assessment upon admission and every shift At high risk for skin breakdown Long time on OR table/ in bed Decreased nutritional status Incontinence/Moisture Issues Pain that restricts independent movement Prolonged bed rest orders Make sure to take credit for the cares you provide Bathing, linen changes, turns etc. Be aware that high functioning patients are still at risk
Infection Signs/Symptoms of infection Changes in vital signs “chills” Changes in mental status Changes in lab values Wound/Incision/Line/Drain Redness, swelling, drainage, odor, increased pain
Anastomotic Leak Classic symptoms: abdominal pain, tachycardia, high fevers, rigid abdomen, often accompanied by hemodynamic instability May not always present with obvious symptoms- may have low grade fever, Failure to Thrive Imaging required to verify (ex: CT scan) May need urgent trip back to OR (Hyman, 2007)
Nausea/Vomiting was the most frequent complication in the first 24 hours post-operatively (Zietz, 2004) Common antiemetic's used: Zofran (IV or po) Compazine Benadryl Emesis bags in each nurse server on 7 NT/8 NT Take into consideration hydration status If not maintaining hydration- may want to recommend IVF Signs of dehydration?
Bowel Function Promote ambulation Promote fluid intake (IV, po, through feeding tube) Sometimes Reglan, Erythromycin or Entereg will be ordered to stimulate gut motility Watch for constipation- does patient need laxative/stool softener/enema? Can occur d/t narcotic use All patients taking narcotics should have a bowel regimen ordered (senna, miralax, etc. ) Ostomy – watch for increased output Keep accurate I/O Sometimes medications will be ordered to decrease output- ex: lomotil Dietary Modifications Patients will be instructed to measure output at home
Bowel Function (cont. ) Post-operative Ileus Definition: transient impairment of intestinal motility after abdominal surgery (Han. Geurts et al, 2007) Most frequent reason for a prolonged stay in the hospital after abdominal surgery (Leier, 2007) Factors influencing an ileus: Local intestinal inflammation Anesthetic agents Over hydration Post-operative analgesia (opioids) Reduced mobility Treatment could include: Insertion of an NG tube IV hydration SBO Symptoms: Cramping, abdominal pain, that comes and goes Nausea Vomiting Diarrhea Constipation Inability to have a bowel movement or pass gas Swelling of the abdomen (distention) Treatment: Bowel Rest, NG tube for decompression, OR trip if emergent http: //www. mayoclinic. org/diseases-conditions/intestinal-obstruction/basics/symptoms/con-20027567
Mobility Activity: per MD order Varies per Surgeon, but once cleared to ambulate, should be aggressive Patients can ambulate(same day as surgery) with MD order Activity helps increase strength, improve lung function, prevent blood clots and stimulates gut motility. Ensure that patients pain is well enough controlled that they can do activity PT/OT needed? Home PT/OT needed? Cane/Walker needed? Fall Risk? (anesthesia, opioids, obstacles, deconditioning)
Blood Sugar Control Poor control of blood glucose over time can lead to the development of longer term and debilitating and life threatening conditions (Holt, 2012). Cardiovascular Disease, peripheral vascular disease, retinopathy, neuropathy, and neuropathy Good blood sugar control can promote good wound healing Surgical intervention is a form of major trauma that triggers a metabolic stress response (Holt, 2012). Stress from surgery can cause a decrease in the ability for the pancreas to produce insulin. Patients who have a partial or total pancreatectomy will have decreased insulin production. Be Cautious: Insulin is a high alert medication! High risk of patient harm with medication administration errors. Regular Insulin If NPO or on TF as primary nutrition Humalog/Lantus Consult Diabetes Management Team/Diabetes Educators
Lines/Drains/Airway Make sure you assess all lines/drains/airway! Surgical Drains? Central Lines/PIVs? Epidural/PCA?
Patient Teaching Start teaching on day of admission Plan of Care Goals for the day (ex: IS 10 x/hr, ambulation- at least 4 walks per day, etc. ) Lines Drains Medications Diabetes Activity Diet Wound/Incision care Showering/Bathing When to seek medical attention Utilize Krames on demand or Lexicomp for patient education materials https: //www. kramesondemand. com/Bookmarks. aspx http: //online. lexi. com/lco/action/pcm
Preparing for Discharge What are the discharge barriers? Teaching needed? (lines/drains/medications/diabetes) Utilize Krames on demand or Lexicomp for patient education materials https: //www. kramesondemand. com/Bookmarks. aspx http: //online. lexi. com/lco/action/pcm Home care needed? What home supplies/equipment needed? Who should the patient contact for help when they go home?
References Holt, P. (2012) Pre and Post-operative needs of patients with diabetes. Nursing Standard. 26, 50 -56. Hyman, N et al. (2007) Anastomotic Leaks After Intestinal Anastomosis. Ann Surg. Feb 2007; 245(2): 254– 258. Leier, H. (2007) Does gum chewing help prevent impaired gastric motility in the post-operative period? Journal of the American Academy of Nurse Practioners; 19; 3, 133 -136. Thornlow, D. et al (2009) Cascade iatrogenesis: Factors leading to the development of adverse events in hospitalized older adults. International Journal of Nursing Studies. Wright, S. et al (2009) Enhanced recovery pathway in colorectal surgery 2: post-operative complications. Nursing Times; 105: 29, 24 -26 Zeitz, K. (2004) Post-operative complications in the first 24 hours: a general sugery audit. Journal of Advanced Nursing; 46; 6, 633 -640. http: //www. mayoclinic. org/diseases-conditions/pulmonaryembolism/basics/symptoms/con-20022849 http: //www. mayoclinic. org/diseases-conditions/deep-veinthrombosis/basics/symptoms/con-20031922
 Post operative nursing care
Post operative nursing care Fluothane
Fluothane Care plan for cataract
Care plan for cataract Post operative nursing care
Post operative nursing care Post operative nursing care
Post operative nursing care C section slideshare
C section slideshare Pre post peri
Pre post peri Epilepsy
Epilepsy Cleft lip and palate post operative care nursing diagnosis
Cleft lip and palate post operative care nursing diagnosis Dr ryan fernandes
Dr ryan fernandes Post operative nursing management
Post operative nursing management Preoperative patient education ppt
Preoperative patient education ppt Pre operative care
Pre operative care Levels of health care primary secondary tertiary
Levels of health care primary secondary tertiary Trauma-informed care activities for staff
Trauma-informed care activities for staff Operative clause words
Operative clause words Text types examples
Text types examples Smear layer definizione
Smear layer definizione Radial fissure bur
Radial fissure bur Naimun position paper
Naimun position paper Operative clauses
Operative clauses T shaped matrix band
T shaped matrix band Reiss text types
Reiss text types