POCT Glucose AccuChek Inform II Point of Care

- Slides: 19
POCT Glucose Accu-Chek Inform II Point of Care Testing Education Regional Laboratory Services Rev. 10/2017

Objectives: • • • Review the use of Accu-Chek Inform II Glucose meter Meter Components Principles of operation Specimen requirements Reagent/Supplies/Equipment Test Strip & Control Requirements Perform and document Quality Control Perform and document Patient Results Interpret Results/Documentation Troubleshooting Instrument Maintenance Competency requirements
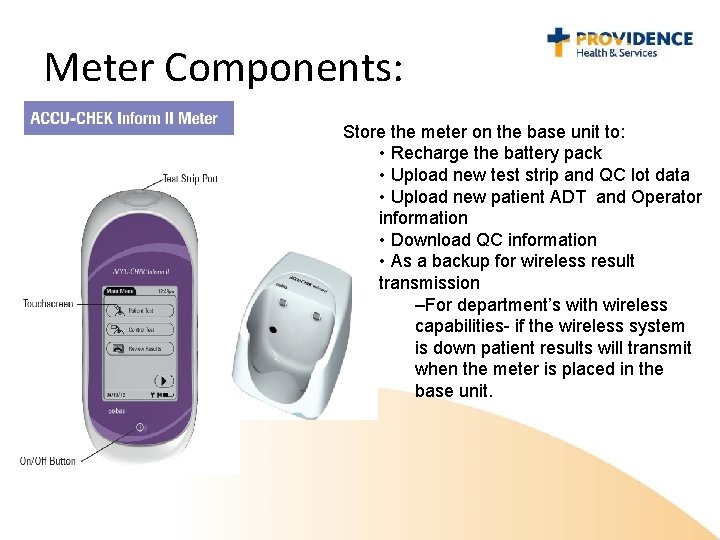
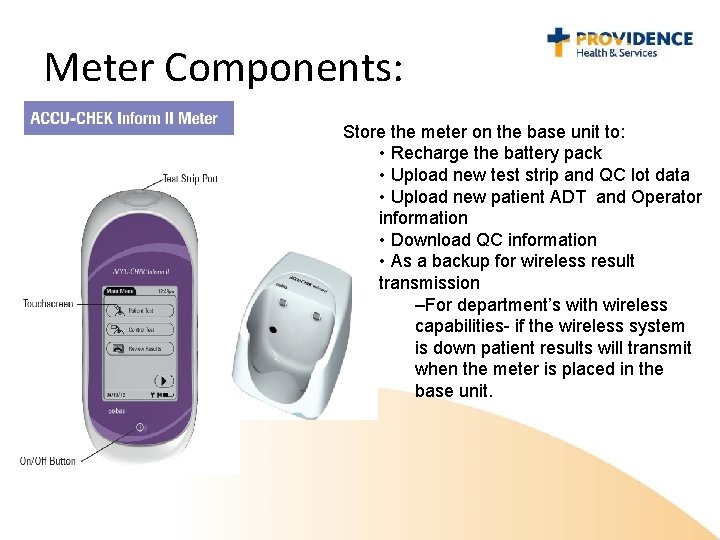
Meter Components: Store the meter on the base unit to: • Recharge the battery pack • Upload new test strip and QC lot data • Upload new patient ADT and Operator information • Download QC information • As a backup for wireless result transmission –For department’s with wireless capabilities- if the wireless system is down patient results will transmit when the meter is placed in the base unit.
Principles of Operation: • Test method – The meter combines whole blood with an enzyme in the test strip. – A small electrical current is produced and measured. This is proportional to the amount of glucose. • Regulatory class: This test is CLIA-waived • Confirmatory testing is required if unexpected results are obtained. Send a specimen to the laboratory if: – Result(s) are within critical ranges and they have not been previously verified (unless provider deems results are consistent with clinical picture) – No results are obtained (instrument displays a code instead of a value) – Repeated results on the meter are not within accepted limits – Confirmed results are inconsistent with the patient’s condition – Range limits for acceptable confirmation by repeat: § For values < 75 mg/d. L: If repeat value is within ± 15 mg/d. L of the original value, the original value is accepted. § Values > 75 mg/d. L: If repeat value is within ± 20% of the original value, the original value is accepted.
Specimen Requirements: • Acceptable specimens: – Capillary whole blood from a finger-stick or heel-stick; tested immediately – Fresh venous or arterial whole blood collected using a plain syringe (without anticoagulant); tested immediately – Venous or arterial whole blood collected in an EDTA or Heparin blood collection tube; tested within 30 minutes. – When testing is not performed at the patient bedside, the specimen must be labeled. Unlabeled specimens are unacceptable. • Unacceptable Specimens: – Self-testing with POCT equipment is not permitted within the Providence Health System for any reason. • In the event that a Providence Caregiver experiences a health complication: – testing should be performed using their own personal device, as prescribed by their physician and/or notify the department supervisor. – Clotted Specimens – Neonatal cord blood – Serum or plasma specimens
Important Information below! Specimen Limitations: • When is it NOT appropriate to obtain a capillary sample for glucose testing? – It is NOT acceptable to obtain a capillary sample for glucose testing when the following impaired peripheral circulation conditions apply: • • • Severe dehydration due to DKA or HHNK Hypotension Shock Peripheral Arterial Occlusive disease Decompensated Heart Failure NYHA Class IV • Venipuncture or line draws are the only acceptable samples when impaired peripheral circulation conditions are present.
Important Information Below! Specimen Limitations Cont. : • When is it NOT acceptable to use the Inform II glucose meter for any glucose testing? – It is NOT acceptable to use the Inform II meter for any glucose testing when the following conditions apply. Instead, a sample must be sent to the laboratory for glucose testing. • Specimens collected with anticoagulants other than EDTA or Heparin • Specimens from patients with Hematocrit of <10% or >65% • Specimens with marked lipemia (triglycerides >1800 mg/d. L) • Blood concentrations of galactose >15 mg/d. L • Intravenous administration of ascorbic acid that results in blood concentrations of Ascorbic acid >3 mg/d. L
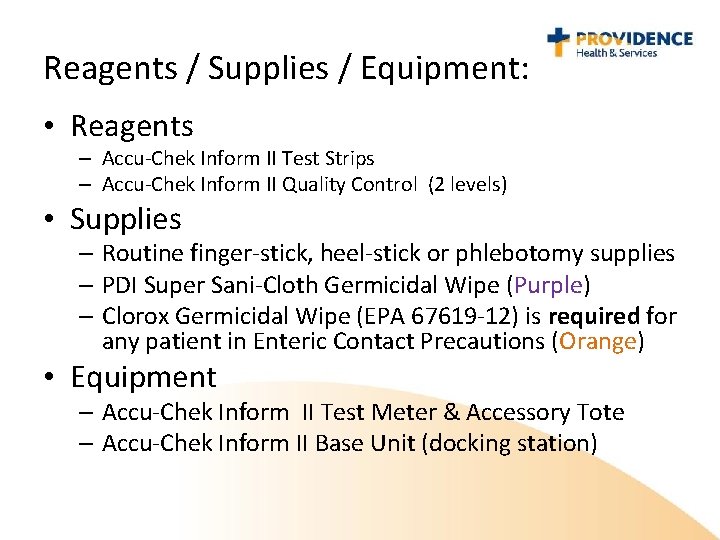
Reagents / Supplies / Equipment: • Reagents – Accu-Chek Inform II Test Strips – Accu-Chek Inform II Quality Control (2 levels) • Supplies – Routine finger-stick, heel-stick or phlebotomy supplies – PDI Super Sani-Cloth Germicidal Wipe (Purple) – Clorox Germicidal Wipe (EPA 67619 -12) is required for any patient in Enteric Contact Precautions (Orange) • Equipment – Accu-Chek Inform II Test Meter & Accessory Tote – Accu-Chek Inform II Base Unit (docking station)
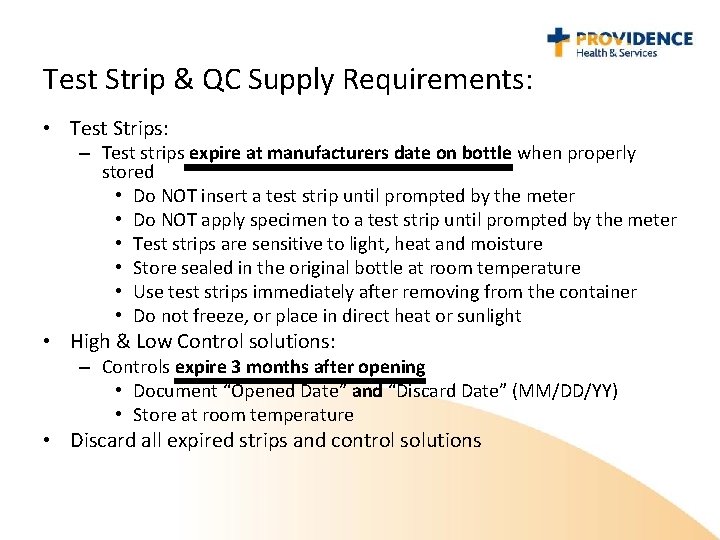
Test Strip & QC Supply Requirements: • Test Strips: – Test strips expire at manufacturers date on bottle when properly stored • Do NOT insert a test strip until prompted by the meter • Do NOT apply specimen to a test strip until prompted by the meter • Test strips are sensitive to light, heat and moisture • Store sealed in the original bottle at room temperature • Use test strips immediately after removing from the container • Do not freeze, or place in direct heat or sunlight • High & Low Control solutions: – Controls expire 3 months after opening • Document “Opened Date” and “Discard Date” (MM/DD/YY) • Store at room temperature • Discard all expired strips and control solutions
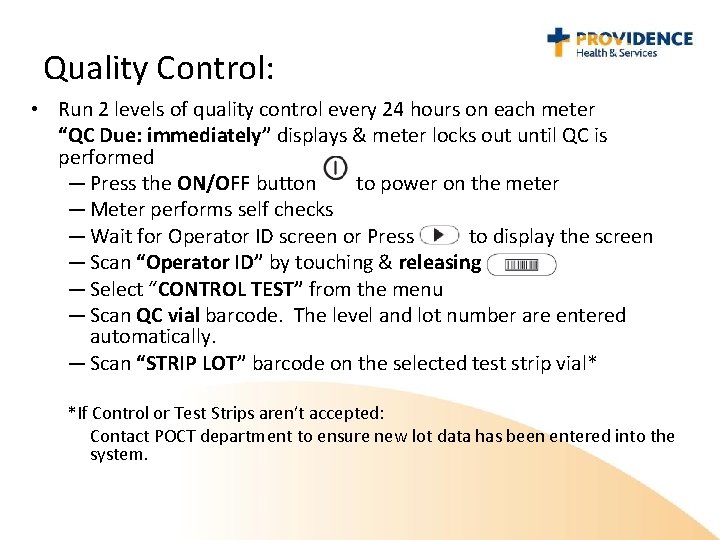
Quality Control: • Run 2 levels of quality control every 24 hours on each meter “QC Due: immediately” displays & meter locks out until QC is performed — Press the ON/OFF button to power on the meter — Meter performs self checks — Wait for Operator ID screen or Press to display the screen — Scan “Operator ID” by touching & releasing — Select “CONTROL TEST” from the menu — Scan QC vial barcode. The level and lot number are entered automatically. — Scan “STRIP LOT” barcode on the selected test strip vial* *If Control or Test Strips aren’t accepted: Contact POCT department to ensure new lot data has been entered into the system.
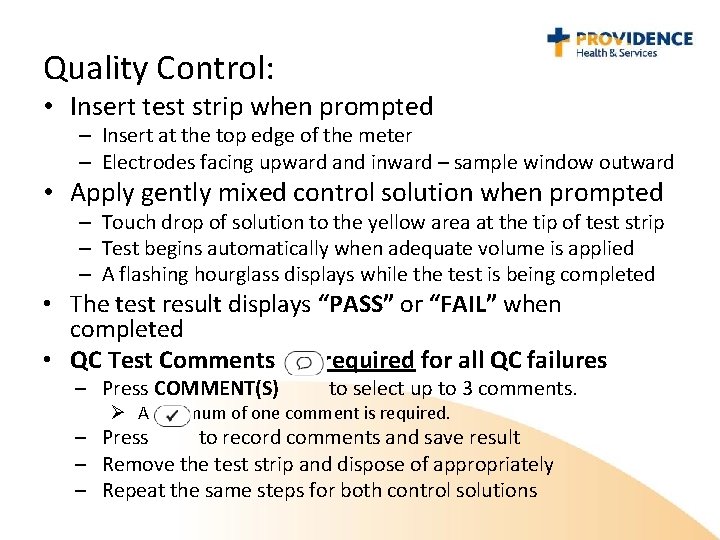
Quality Control: • Insert test strip when prompted – Insert at the top edge of the meter – Electrodes facing upward and inward – sample window outward • Apply gently mixed control solution when prompted – Touch drop of solution to the yellow area at the tip of test strip – Test begins automatically when adequate volume is applied – A flashing hourglass displays while the test is being completed • The test result displays “PASS” or “FAIL” when completed • QC Test Comments are required for all QC failures – Press COMMENT(S) to select up to 3 comments. Ø A minimum of one comment is required. – Press to record comments and save result – Remove the test strip and dispose of appropriately – Repeat the same steps for both control solutions
Patient Testing: Press the ON/OFF button to power on the meter Meter performs self checks* Wait for Operator ID screen or Press to display the screen Scan your “Operator ID” by touching and releasing Select “Patient Test” from the menu Scan the “Patient ID” and confirm the identification is correct Scan the “STRIP LOT” barcode from the test strip vial – If the barcode isn’t recognized – Contact the POCT department • Insert test strip when prompted • Obtain blood sample – Venous or arterial whole blood – Capillary sample • Clean puncture site (with either alcohol or soap and water) • Wipe away the first drop of blood • • *If the battery is flashing low, use a different meter for patient testing. low batteries may not produce accurate results. Meters with
Patient Testing Continued: • Apply sample when prompted (there will be an audible beep with a drop of blood displayed on the screen when the analyzer is ready for the sample to be applied) – Touch a drop of blood to the yellow area at the tip of the test strip – Test begins automatically when adequate sample volume is applied – A flashing hourglass displays while the test is being completed • The test result displays and the meter beeps when test is complete • Press to send the results wirelessly to the patient chart (for those departments with wireless transmission capabilities) and/or to return to the Main Menu. – NOTE: Failure to press will cause an extended delay in the wireless transmission of the result. • Remove and dispose of the test strip appropriately • Clean the meter and recharge the meter by placing it in the base unit
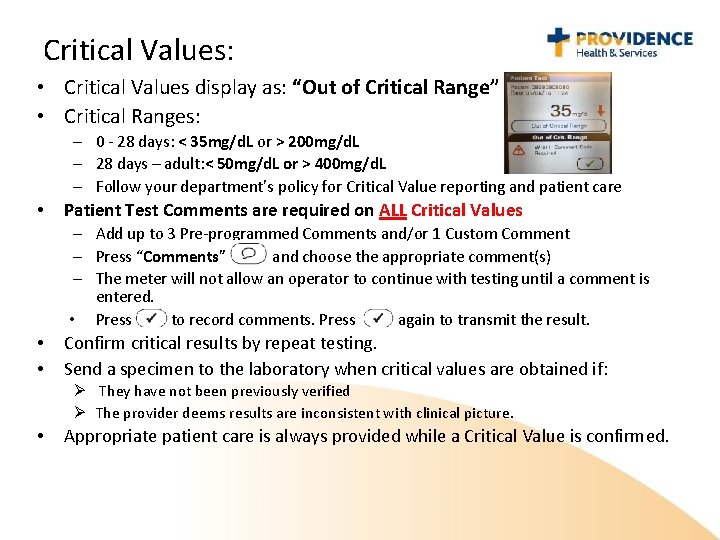
Critical Values: • Critical Values display as: “Out of Critical Range” • Critical Ranges: – 0 - 28 days: < 35 mg/d. L or > 200 mg/d. L – 28 days – adult: < 50 mg/d. L or > 400 mg/d. L – Follow your department’s policy for Critical Value reporting and patient care • Patient Test Comments are required on ALL Critical Values – Add up to 3 Pre-programmed Comments and/or 1 Custom Comment – Press “Comments” and choose the appropriate comment(s) – The meter will not allow an operator to continue with testing until a comment is entered. • Press to record comments. Press again to transmit the result. • • Confirm critical results by repeat testing. Send a specimen to the laboratory when critical values are obtained if: Ø They have not been previously verified Ø The provider deems results are inconsistent with clinical picture. • Appropriate patient care is always provided while a Critical Value is confirmed.
Interpret Result & Documentation: • Results outside the meter’s Reportable Range display as: “LO” (result < 10 mg/d. L) or “HI” (result > 600 mg/d. L) – Treat results outside the Reportable Range as Critical Values • Document results per your department work flow • For departments with wireless transmission capabilities: – Press to send the results wirelessly to the patient chart and/or to return to the Main Menu. – Note: Failure to press will cause an extended delay in the wireless transmission of the result. • Normal Reference Ranges: – 0 - 1 day – 1 - 28 days – 28 days - Adult 36 - 110 mg/d. L 47 - 110 mg/d. L 65 - 99 mg/d. L
Troubleshooting: • Always provide appropriate patient care as directed by a provider • If a result is unexpected or inconsistent with patient condition: – Check the meters battery life. • If the battery life is sufficient, perform QC using the same meter and same test strips • If the battery life is insufficient, perform QC using a charged meter and the same test strips – Perform Quality Control testing: § If QC is acceptable – the meter is performing as expected • REPEAT the patient test » If repeat results are within the range limits, report the original result. » If repeat does not confirm – Place an order for laboratory confirmation. » Note: Confirmation by repeat or comparison of values from different meters or methods may be misleading if specimens are not collected within 15 minutes of each other and tested immediately. § If QC fails – repeat the QC using new control solutions and/or a new vial of strips – If repeat QC is acceptable – the meter is performing as expected » REPEAT the patient test – If repeat QC fails: » Sequester the meter and the original test strip vial and QC solutions » Contact the POCT department » Start over with a different meter, a new test strip vial and new QC solutions » Place an order for laboratory confirmation.
Troubleshooting Continued: • Operator ID invalid message: – Contact your Point of Care Coordinator so they can investigate the possible reasons why your ID is invalid. Possible reasons: • Your certification has expired and the annual competency requirements were not met by your certification due date. • You received a new employee badge. Whenever an operator receives a new employee badge the barcode number changes on the badge and your Point of Care Coordinator must enter the new information into the glucose meter database. • You are a new employee and have either not been trained or have not been entered into the glucose meter database. • • – Never borrow or share your badge. It is against Providence Policy and could lead to corrective action. Performing patient testing using another employee’s badge is falsifying patient records. Patient Armband won’t scan: – Ensure that the barcode screen on the meter is clean – Obtain a new armband Meter won’t turn on: – Reset the meter by holding down the power button for 20 – 30 seconds.
Instrument Maintenance: • Transport the meter and all accessories in the tote (except into patient isolation rooms) • Store the meter on the base unit (docking station) • Sanitize the meter and tote between each patient • Approved sanitizing wipes are: – PDI Super Sani-Cloth (purple) is approved for routine usage – Clorox Germicidal Wipe (EPA 67619 -12) is required for any patient in Enteric Contact Precautions • Do not allow excess liquid to enter or remain on the meter • Clean the docking station as needed – Wipe the surfaces with a soft cloth dampened(not wet) with water – Do NOT get the connectors in the docking station wet – Dry thoroughly after cleaning
Annual Competency Requirements • On an annual basis the following must be completed by each testing operator: – Both low and high QC must be performed and pass – 1 patient test must be performed – All related/assigned Healthstream modules must be completed on time • Note: Failure to complete all of the above will result in the operator being locked out of the glucose meter.
 Accuchek inform
Accuchek inform Accuchek inform
Accuchek inform Abg poct
Abg poct Role of csf
Role of csf Maltose formation
Maltose formation Advantages of hexokinase method
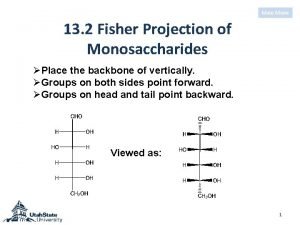
Advantages of hexokinase method Sorbose fischer projection
Sorbose fischer projection Fo2hb basso
Fo2hb basso Elektron poçt
Elektron poçt Linee guida poct
Linee guida poct Poct
Poct Poct přístroje
Poct přístroje Göyərçin poçt quşu rolunda
Göyərçin poçt quşu rolunda Primary secondary tertiary health care definition
Primary secondary tertiary health care definition Care certificate standard 3
Care certificate standard 3 Magnetul atrage cuprul
Magnetul atrage cuprul Palliative care vs hospice care
Palliative care vs hospice care Animale care nasc pui vii
Animale care nasc pui vii Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate Care certificate standard 7 answers
Care certificate standard 7 answers