Pneumo Trieste 16 18 Aprile 2018 INCONTRO CON


![Sequential [Sepsis-Related] Organ Failure Assessment Score Abbreviations: FIO 2, fraction of inspired oxygen; MAP, Sequential [Sepsis-Related] Organ Failure Assessment Score Abbreviations: FIO 2, fraction of inspired oxygen; MAP,](https://slidetodoc.com/presentation_image_h2/b61b9b0afb9b4a8452d071be3f45d6a8/image-14.jpg)

- Slides: 36

Pneumo Trieste 16 -18 Aprile 2018 INCONTRO CON L’ESPERTO Capire e riconoscere le sepsi Gianni Biolo Dipartimento di Scienze Mediche Chirurgiche e della Salute Clinica Medica Generale e Terapia Medica Università di Trieste Azienda sanitaria Universitaria Integrata di Trieste - ASUITs
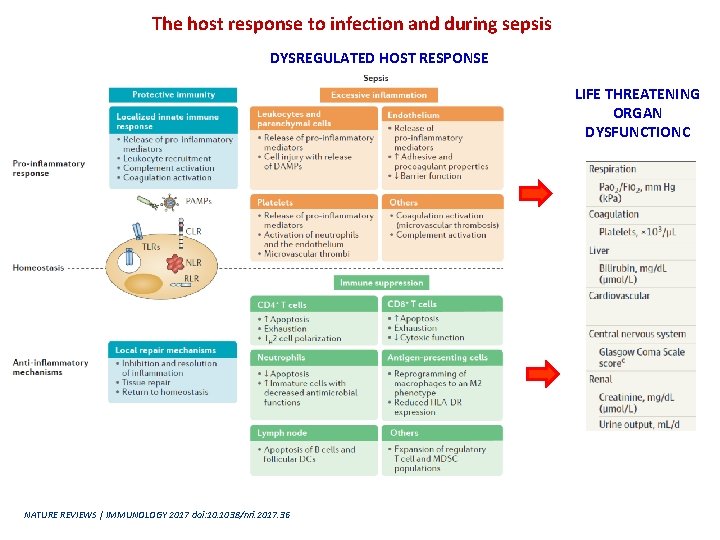
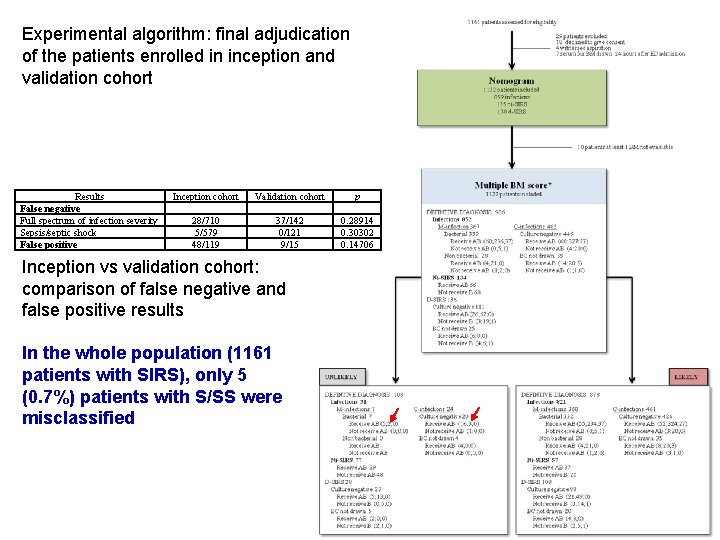
The host response to infection and during sepsis DYSREGULATED HOST RESPONSE LIFE THREATENING ORGAN DYSFUNCTIONC NATURE REVIEWS | IMMUNOLOGY 2017 doi: 10. 1038/nri. 2017. 36
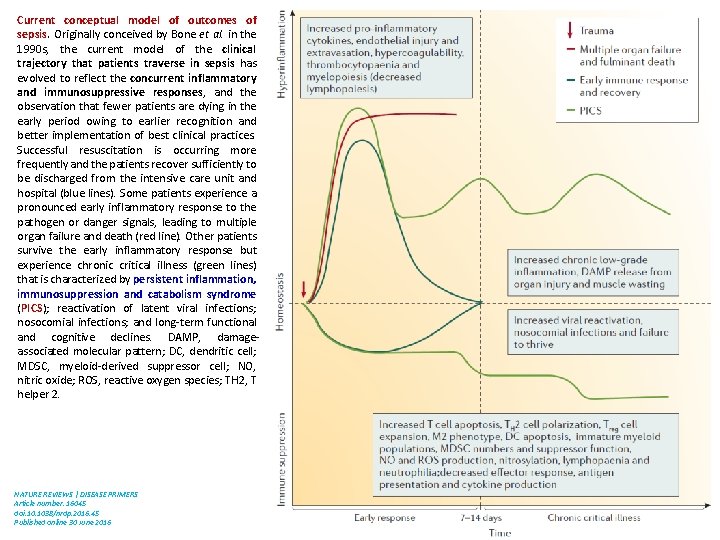
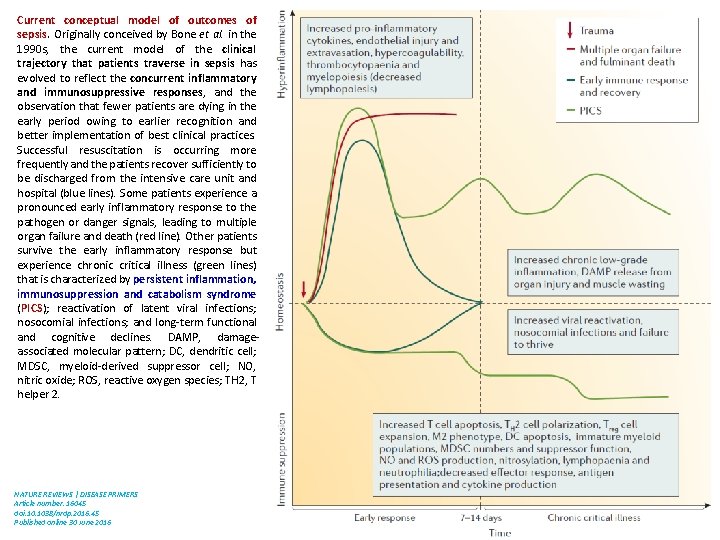
Current conceptual model of outcomes of sepsis. Originally conceived by Bone et al. in the 1990 s, the current model of the clinical trajectory that patients traverse in sepsis has evolved to reflect the concurrent inflammatory and immunosuppressive responses, and the observation that fewer patients are dying in the early period owing to earlier recognition and better implementation of best clinical practices. Successful resuscitation is occurring more frequently and the patients recover sufficiently to be discharged from the intensive care unit and hospital (blue lines). Some patients experience a pronounced early inflammatory response to the pathogen or danger signals, leading to multiple organ failure and death (red line). Other patients survive the early inflammatory response but experience chronic critical illness (green lines) that is characterized by persistent inflammation, immunosuppression and catabolism syndrome (PICS); reactivation of latent viral infections; nosocomial infections; and long-term functional and cognitive declines. DAMP, damageassociated molecular pattern; DC, dendritic cell; MDSC, myeloid-derived suppressor cell; NO, nitric oxide; ROS, reactive oxygen species; TH 2, T helper 2. NATURE REVIEWS | DISEASE PRIMERS Article number: 16045 doi: 10. 1038/nrdp. 2016. 45 Published online 30 June 2016
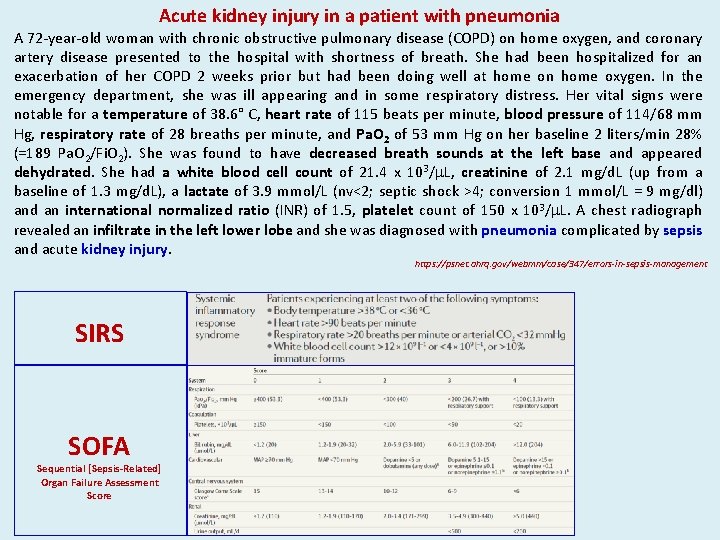
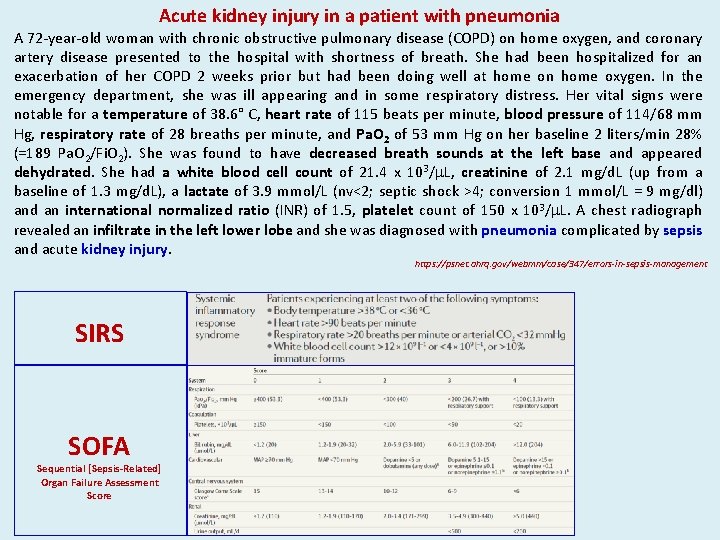
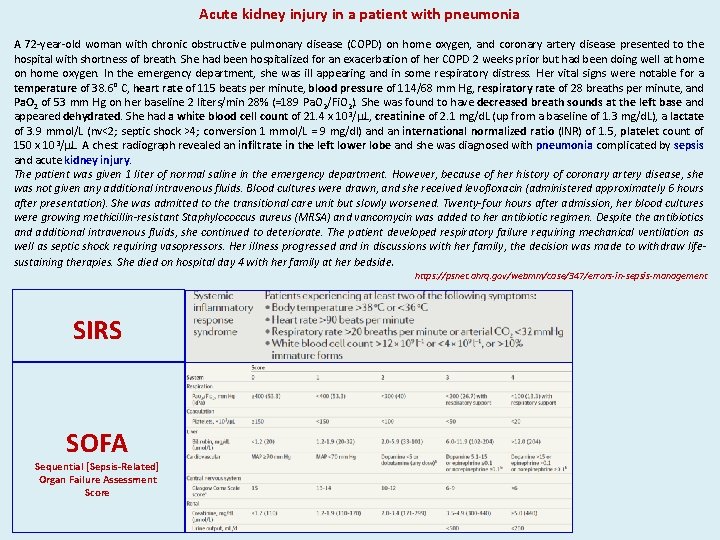
Acute kidney injury in a patient with pneumonia A 72 -year-old woman with chronic obstructive pulmonary disease (COPD) on home oxygen, and coronary artery disease presented to the hospital with shortness of breath. She had been hospitalized for an exacerbation of her COPD 2 weeks prior but had been doing well at home on home oxygen. In the emergency department, she was ill appearing and in some respiratory distress. Her vital signs were notable for a temperature of 38. 6° C, heart rate of 115 beats per minute, blood pressure of 114/68 mm Hg, respiratory rate of 28 breaths per minute, and Pa. O 2 of 53 mm Hg on her baseline 2 liters/min 28% (=189 Pa. O 2/Fi. O 2). She was found to have decreased breath sounds at the left base and appeared dehydrated. She had a white blood cell count of 21. 4 x 103/m. L, creatinine of 2. 1 mg/d. L (up from a baseline of 1. 3 mg/d. L), a lactate of 3. 9 mmol/L (nv<2; septic shock >4; conversion 1 mmol/L = 9 mg/dl) and an international normalized ratio (INR) of 1. 5, platelet count of 150 x 103/m. L. A chest radiograph revealed an infiltrate in the left lower lobe and she was diagnosed with pneumonia complicated by sepsis and acute kidney injury. https: //psnet. ahrq. gov/webmm/case/347/errors-in-sepsis-management SIRS SOFA Sequential [Sepsis-Related] Organ Failure Assessment Score
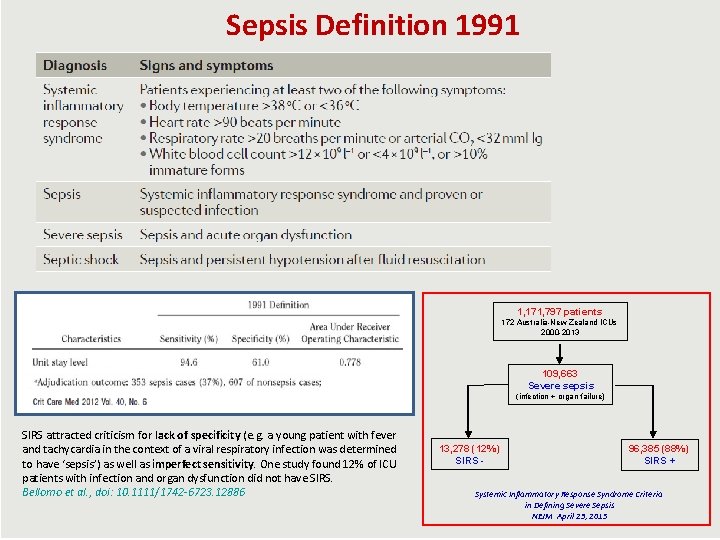
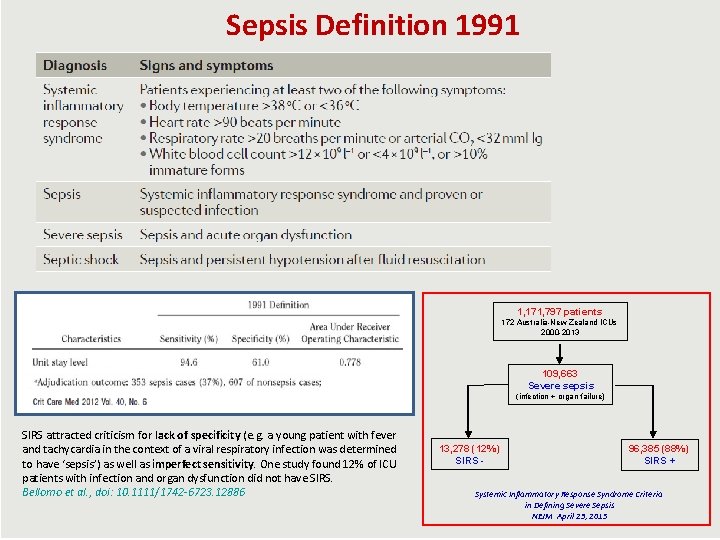
Sepsis Definition 1991 1, 171, 797 patients 172 Australia-New Zealand ICUs 2000 -2013 109, 663 Severe sepsis (infection + organ failure) SIRS attracted criticism for lack of specificity (e. g. a young patient with fever and tachycardia in the context of a viral respiratory infection was determined to have ‘sepsis’) as well as imperfect sensitivity. One study found 12% of ICU patients with infection and organ dysfunction did not have SIRS. Bellomo et al. , doi: 10. 1111/1742 -6723. 12886 13, 278 (12%) SIRS - 96, 385 (88%) SIRS + Systemic Inflammatory Response Syndrome Criteria in Defining Severe Sepsis NEJM April 23, 2015
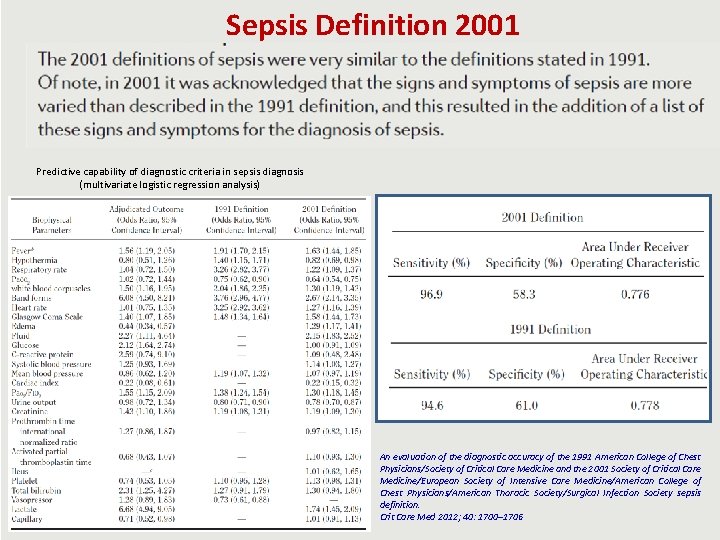
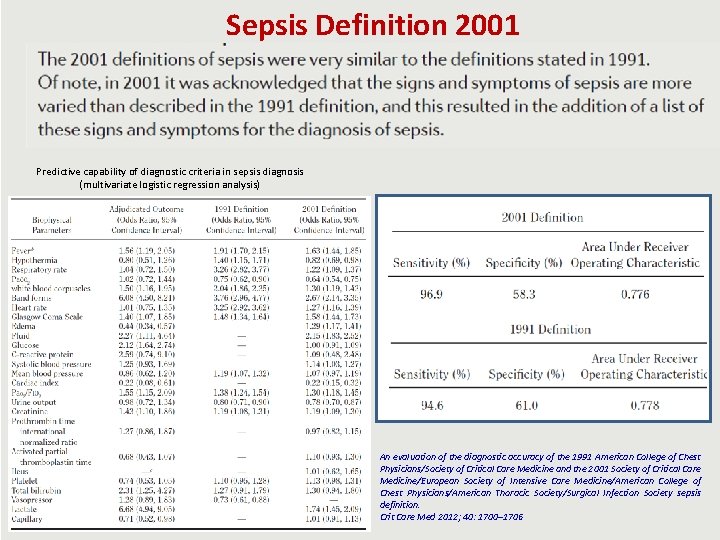
Sepsis Definition 2001 Predictive capability of diagnostic criteria in sepsis diagnosis (multivariate logistic regression analysis) An evaluation of the diagnostic accuracy of the 1991 American College of Chest Physicians/Society of Critical Care Medicine and the 2001 Society of Critical Care Medicine/European Society of Intensive Care Medicine/American College of Chest Physicians/American Thoracic Society/Surgical Infection Society sepsis definition. Crit Care Med 2012; 40: 1700– 1706
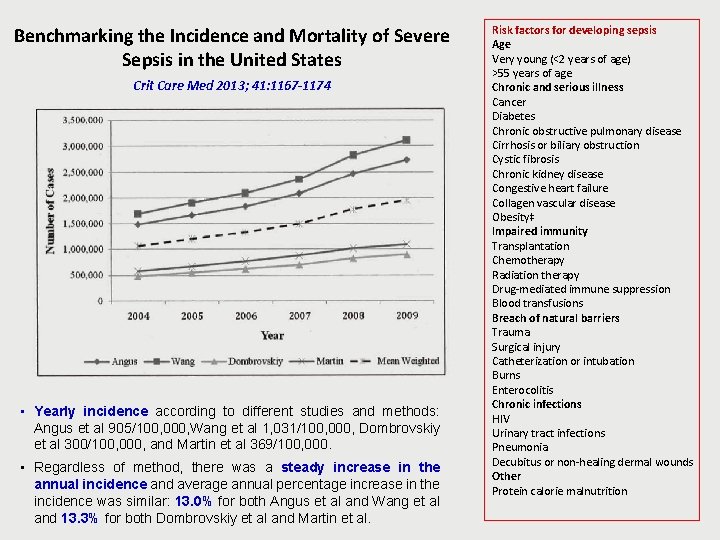
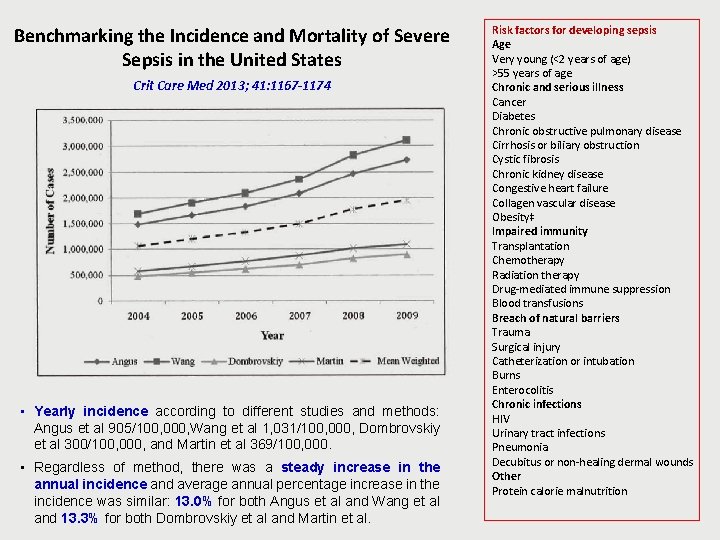
Benchmarking the Incidence and Mortality of Severe Sepsis in the United States Crit Care Med 2013; 41: 1167 -1174 • Yearly incidence according to different studies and methods: Angus et al 905/100, 000, Wang et al 1, 031/100, 000, Dombrovskiy et al 300/100, 000, and Martin et al 369/100, 000. • Regardless of method, there was a steady increase in the annual incidence and average annual percentage increase in the incidence was similar: 13. 0% for both Angus et al and Wang et al and 13. 3% for both Dombrovskiy et al and Martin et al. Risk factors for developing sepsis Age Very young (<2 years of age) >55 years of age Chronic and serious illness Cancer Diabetes Chronic obstructive pulmonary disease Cirrhosis or biliary obstruction Cystic fibrosis Chronic kidney disease Congestive heart failure Collagen vascular disease Obesity‡ Impaired immunity Transplantation Chemotherapy Radiation therapy Drug-mediated immune suppression Blood transfusions Breach of natural barriers Trauma Surgical injury Catheterization or intubation Burns Enterocolitis Chronic infections HIV Urinary tract infections Pneumonia Decubitus or non-healing dermal wounds Other Protein calorie malnutrition
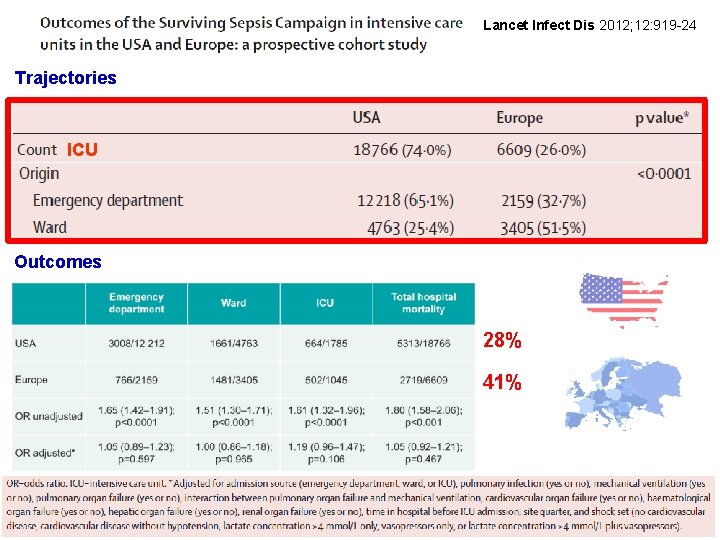
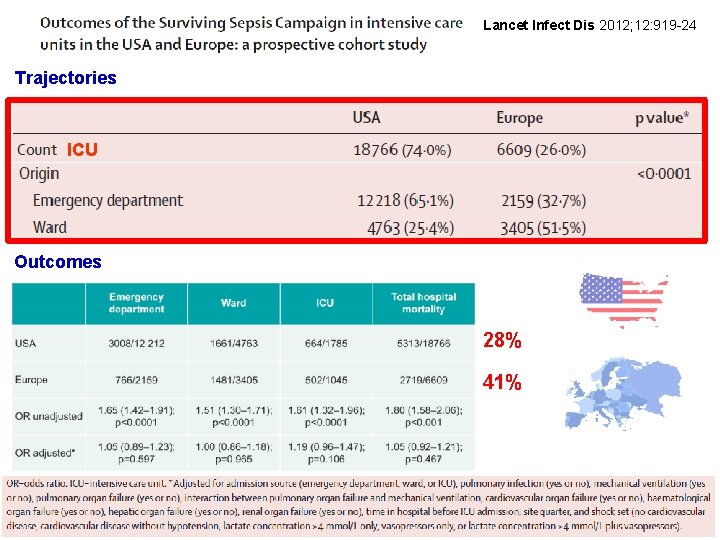
Lancet Infect Dis 2012; 12: 919 -24 Trajectories ICU Outcomes 28% 41%
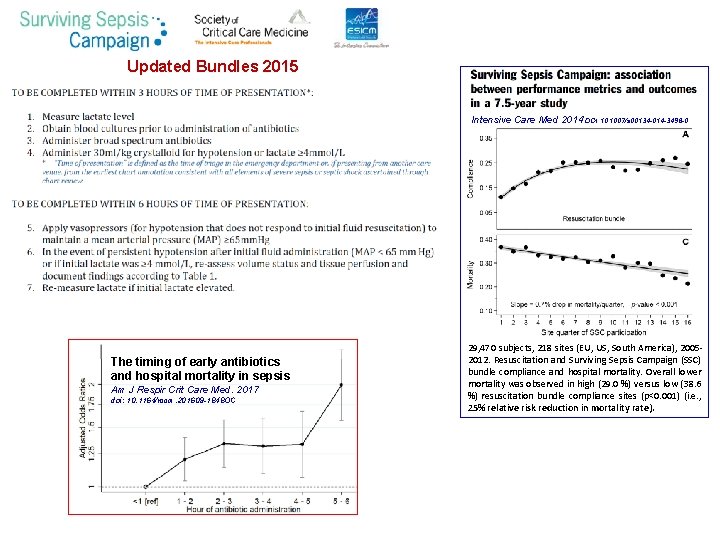
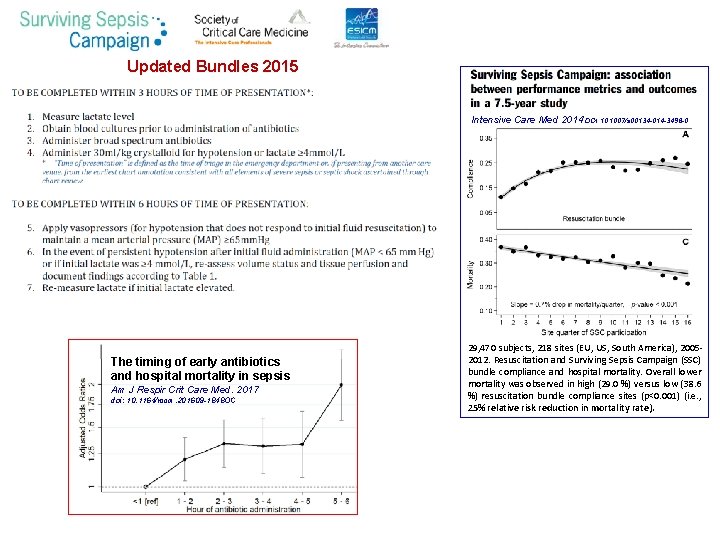
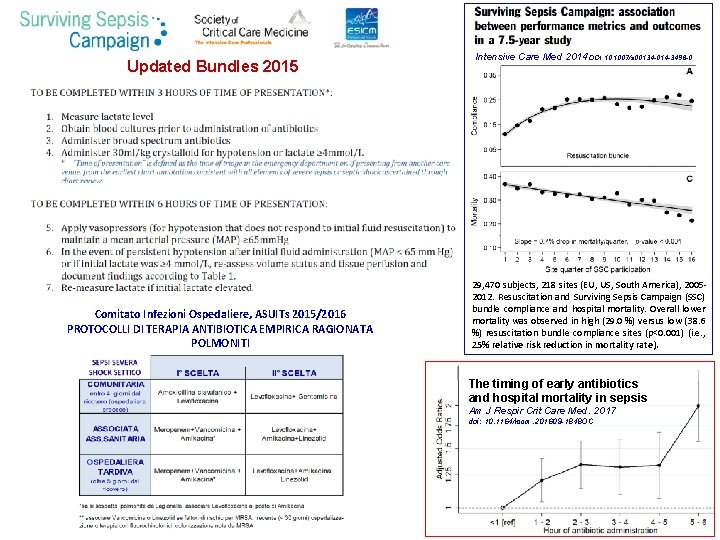
Updated Bundles 2015 Intensive Care Med 2014 DOI 10. 1007/s 00134 -014 -3496 -0 The timing of early antibiotics and hospital mortality in sepsis Am J Respir Crit Care Med. 2017 doi: 10. 1164/rccm. 201609 -1848 OC 29, 470 subjects, 218 sites (EU, US, South America), 20052012. Resuscitation and Surviving Sepsis Campaign (SSC) bundle compliance and hospital mortality. Overall lower mortality was observed in high (29. 0 %) versus low (38. 6 %) resuscitation bundle compliance sites (p<0. 001) (i. e. , 25% relative risk reduction in mortality rate).
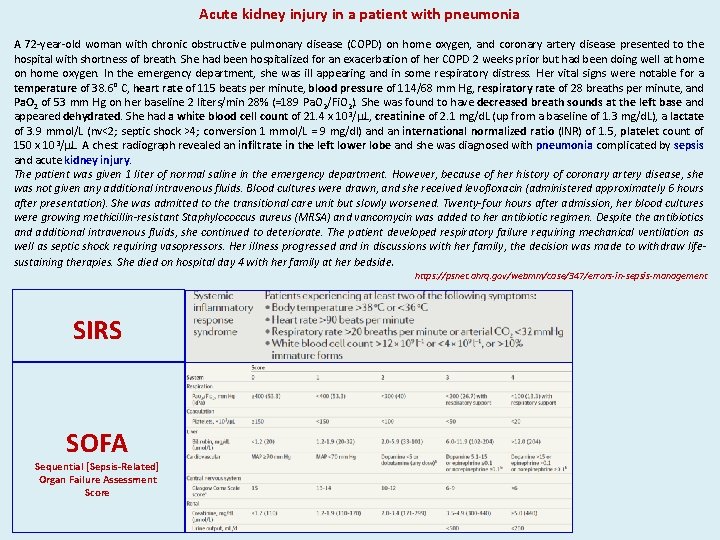
Acute kidney injury in a patient with pneumonia A 72 -year-old woman with chronic obstructive pulmonary disease (COPD) on home oxygen, and coronary artery disease presented to the hospital with shortness of breath. She had been hospitalized for an exacerbation of her COPD 2 weeks prior but had been doing well at home on home oxygen. In the emergency department, she was ill appearing and in some respiratory distress. Her vital signs were notable for a temperature of 38. 6° C, heart rate of 115 beats per minute, blood pressure of 114/68 mm Hg, respiratory rate of 28 breaths per minute, and Pa. O 2 of 53 mm Hg on her baseline 2 liters/min 28% (=189 Pa. O 2/Fi. O 2). She was found to have decreased breath sounds at the left base and appeared dehydrated. She had a white blood cell count of 21. 4 x 103/m. L, creatinine of 2. 1 mg/d. L (up from a baseline of 1. 3 mg/d. L), a lactate of 3. 9 mmol/L (nv<2; septic shock >4; conversion 1 mmol/L = 9 mg/dl) and an international normalized ratio (INR) of 1. 5, platelet count of 150 x 103/m. L. A chest radiograph revealed an infiltrate in the left lower lobe and she was diagnosed with pneumonia complicated by sepsis and acute kidney injury. The patient was given 1 liter of normal saline in the emergency department. However, because of her history of coronary artery disease, she was not given any additional intravenous fluids. Blood cultures were drawn, and she received levofloxacin (administered approximately 6 hours after presentation). She was admitted to the transitional care unit but slowly worsened. Twenty-four hours after admission, her blood cultures were growing methicillin-resistant Staphylococcus aureus (MRSA) and vancomycin was added to her antibiotic regimen. Despite the antibiotics and additional intravenous fluids, she continued to deteriorate. The patient developed respiratory failure requiring mechanical ventilation as well as septic shock requiring vasopressors. Her illness progressed and in discussions with her family, the decision was made to withdraw lifesustaining therapies. She died on hospital day 4 with her family at her bedside. https: //psnet. ahrq. gov/webmm/case/347/errors-in-sepsis-management SIRS SOFA Sequential [Sepsis-Related] Organ Failure Assessment Score
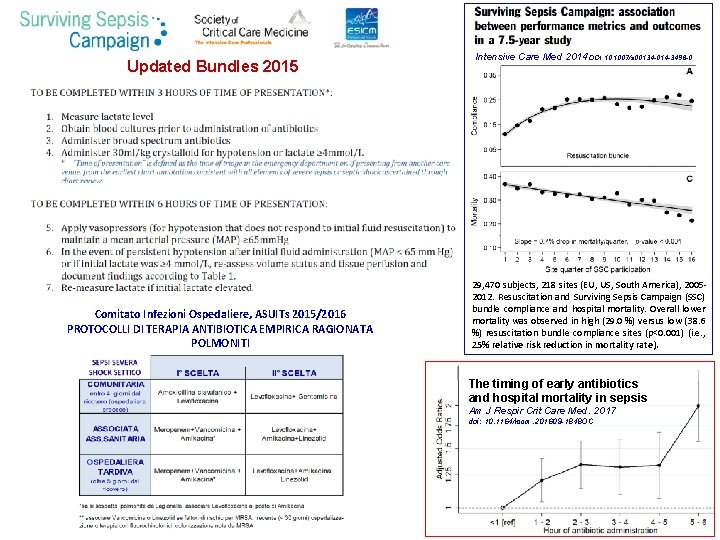
Updated Bundles 2015 Comitato Infezioni Ospedaliere, ASUITs 2015/2016 PROTOCOLLI DI TERAPIA ANTIBIOTICA EMPIRICA RAGIONATA POLMONITI Intensive Care Med 2014 DOI 10. 1007/s 00134 -014 -3496 -0 29, 470 subjects, 218 sites (EU, US, South America), 20052012. Resuscitation and Surviving Sepsis Campaign (SSC) bundle compliance and hospital mortality. Overall lower mortality was observed in high (29. 0 %) versus low (38. 6 %) resuscitation bundle compliance sites (p<0. 001) (i. e. , 25% relative risk reduction in mortality rate). The timing of early antibiotics and hospital mortality in sepsis Am J Respir Crit Care Med. 2017 doi: 10. 1164/rccm. 201609 -1848 OC

SIRS
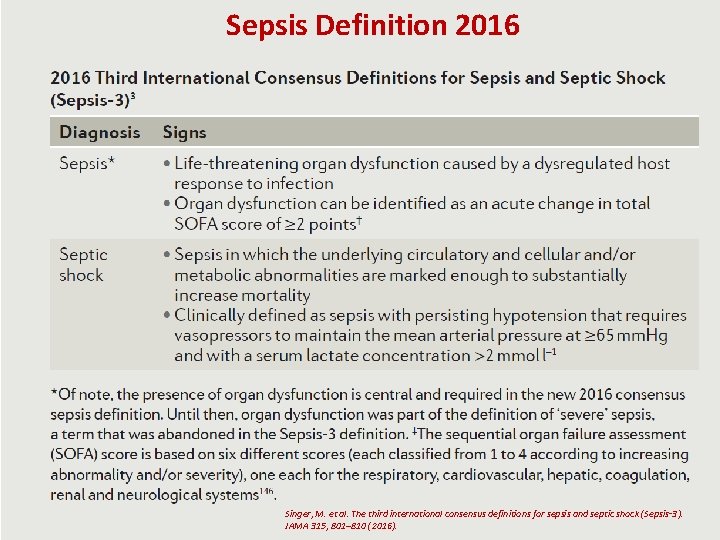
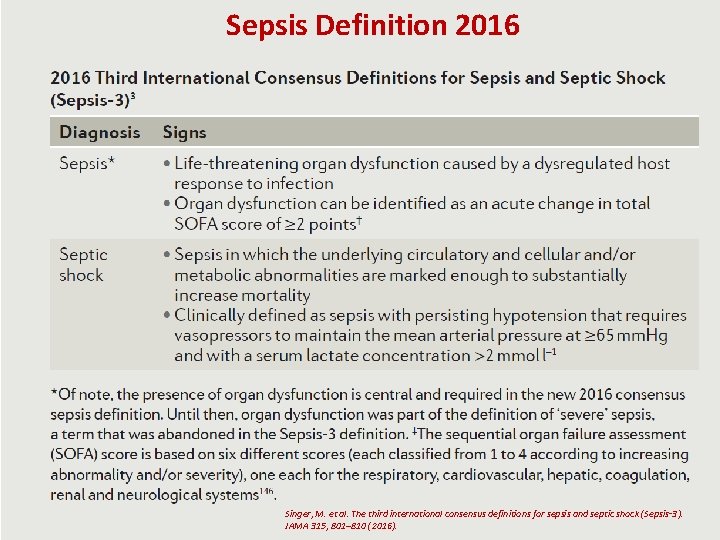
Sepsis Definition 2016 Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis‑ 3). JAMA 315, 801– 810 (2016).
![Sequential SepsisRelated Organ Failure Assessment Score Abbreviations FIO 2 fraction of inspired oxygen MAP Sequential [Sepsis-Related] Organ Failure Assessment Score Abbreviations: FIO 2, fraction of inspired oxygen; MAP,](https://slidetodoc.com/presentation_image_h2/b61b9b0afb9b4a8452d071be3f45d6a8/image-14.jpg)
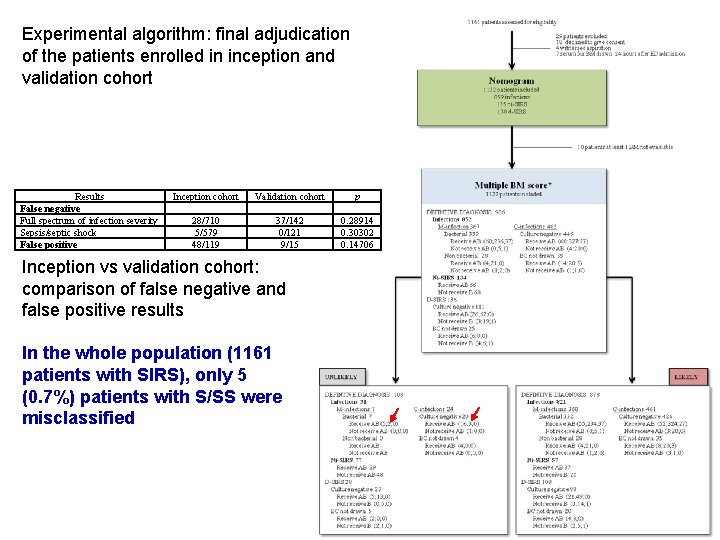
Sequential [Sepsis-Related] Organ Failure Assessment Score Abbreviations: FIO 2, fraction of inspired oxygen; MAP, mean arterial pressure; Pa. O 2, partial pressure of oxygen. b catecholamine doses are given as μg/kg/min for at least 1 hour. c Glasgow Coma Scale scores range from 3 -15; higher score indicates better neurological function. c Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis‑ 3). JAMA 315, 801– 810 (2016).
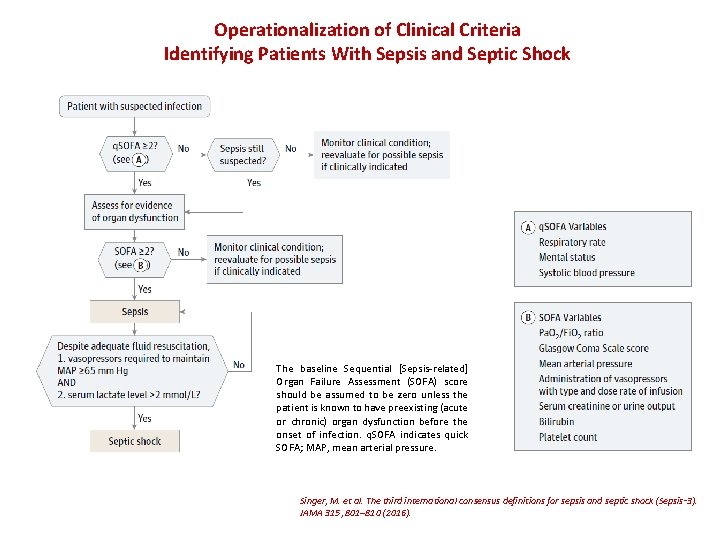
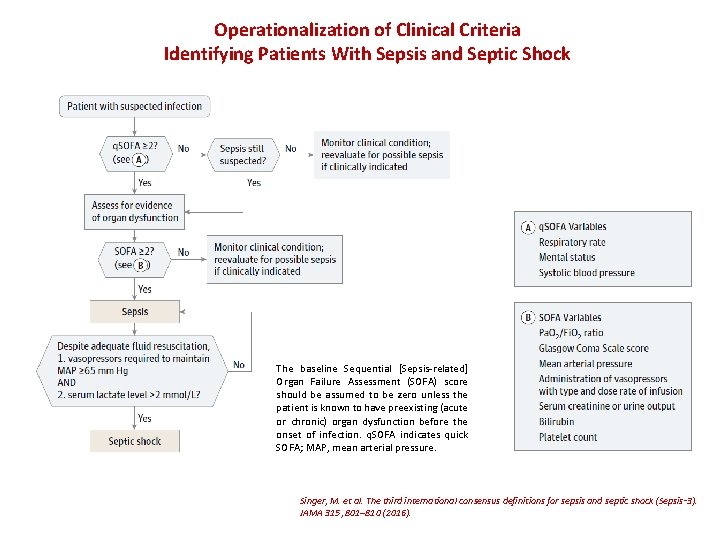
Operationalization of Clinical Criteria Identifying Patients With Sepsis and Septic Shock The baseline Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score should be assumed to be zero unless the patient is known to have preexisting (acute or chronic) organ dysfunction before the onset of infection. q. SOFA indicates quick SOFA; MAP, mean arterial pressure. Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis‑ 3). JAMA 315, 801– 810 (2016).
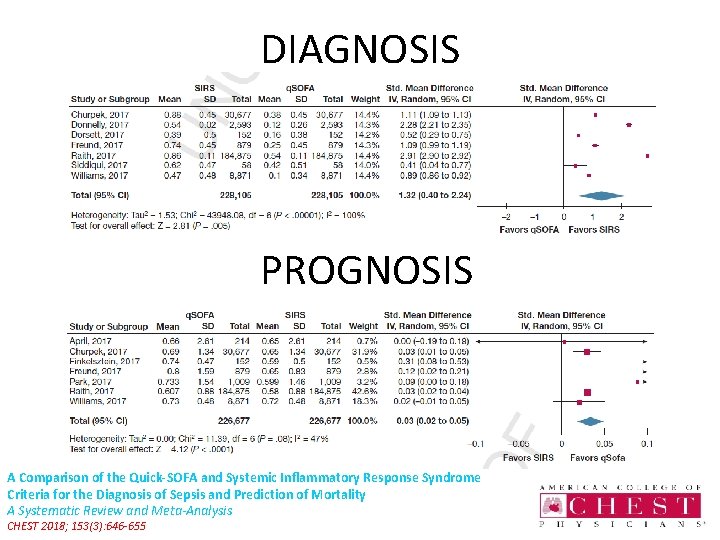
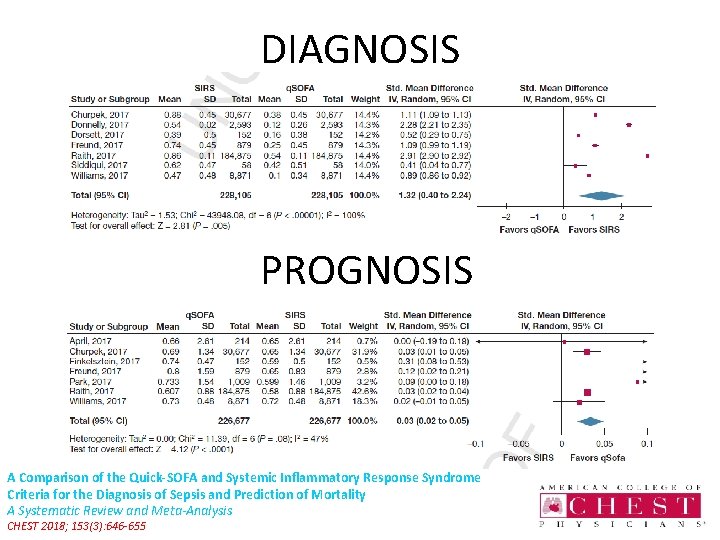
DIAGNOSIS PROGNOSIS A Comparison of the Quick-SOFA and Systemic Inflammatory Response Syndrome Criteria for the Diagnosis of Sepsis and Prediction of Mortality A Systematic Review and Meta-Analysis CHEST 2018; 153(3): 646 -655
… “the original intention of q. SOFA was to identify infection…but further studies focus on prognosis rather than diagnosis. . . ” … “ to identify infection… rely on clinical judgment”… January 17, 2017, Volume 137, 267 -28 Prognostic Accuracy of Sepsis-3 Criteria for In-Hospital Mortality Among Patients With Suspected Infection Presenting to the Emergency Department
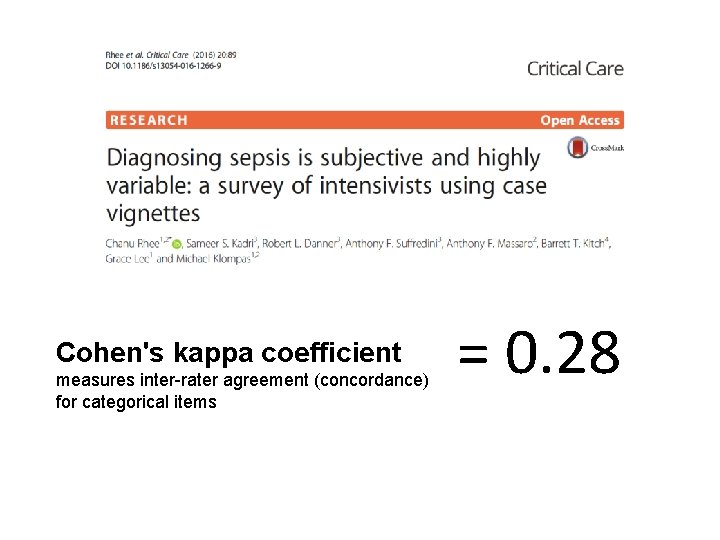
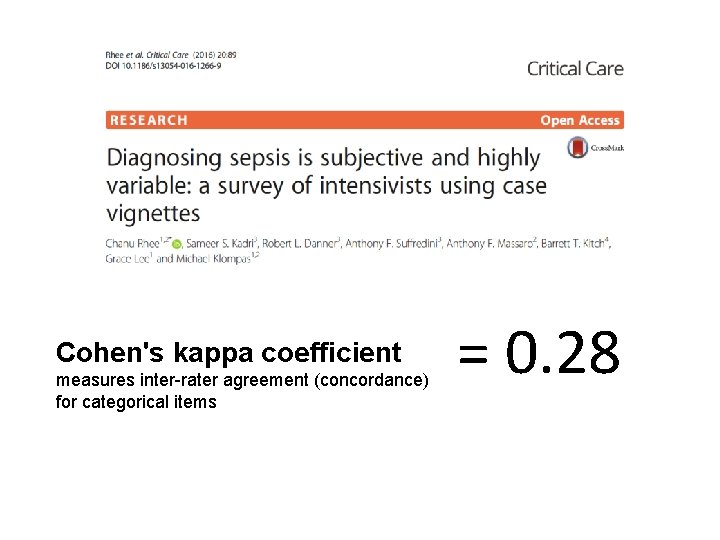
Cohen's kappa coefficient measures inter-rater agreement (concordance) for categorical items = 0. 28
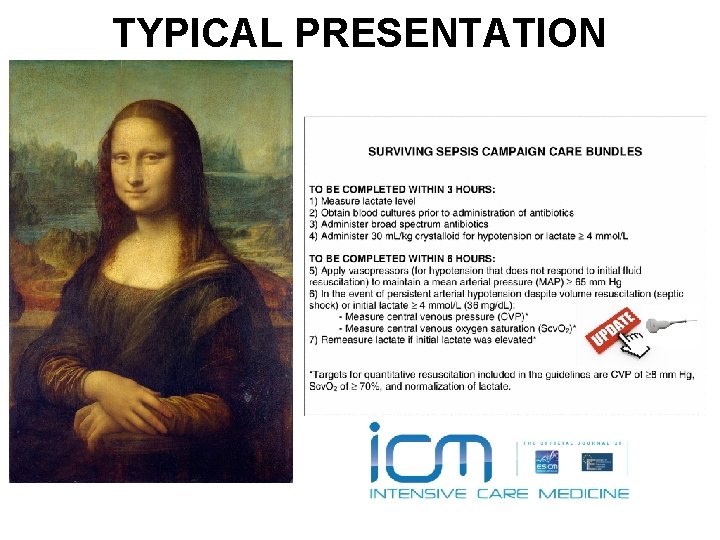
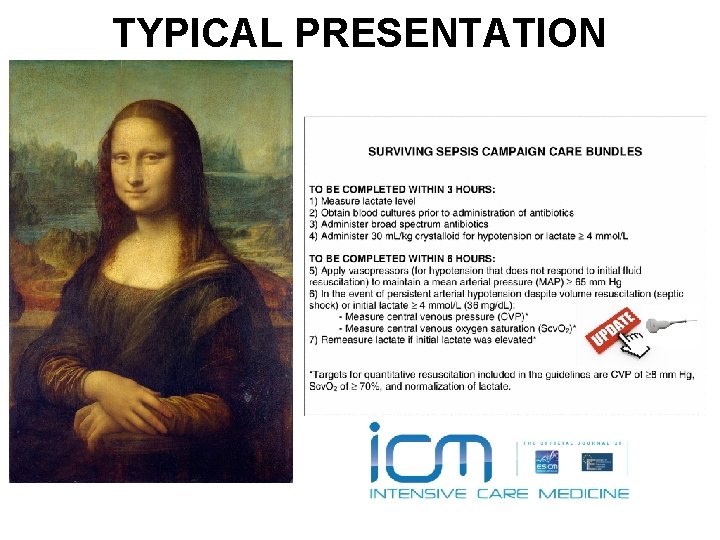
TYPICAL PRESENTATION
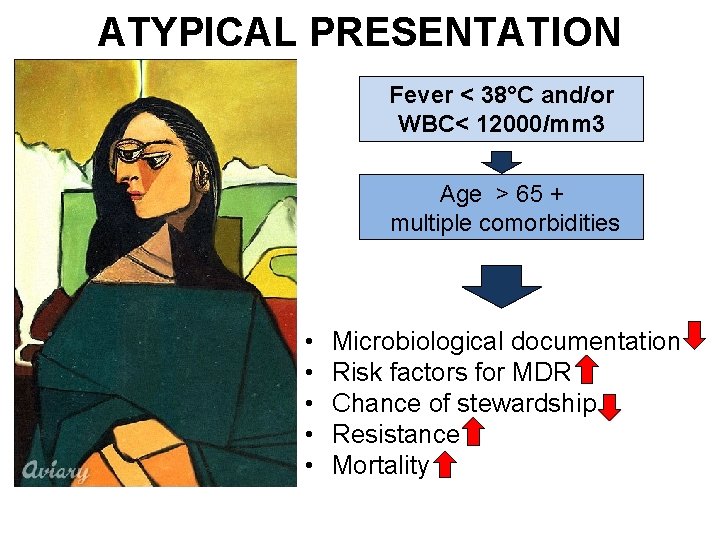
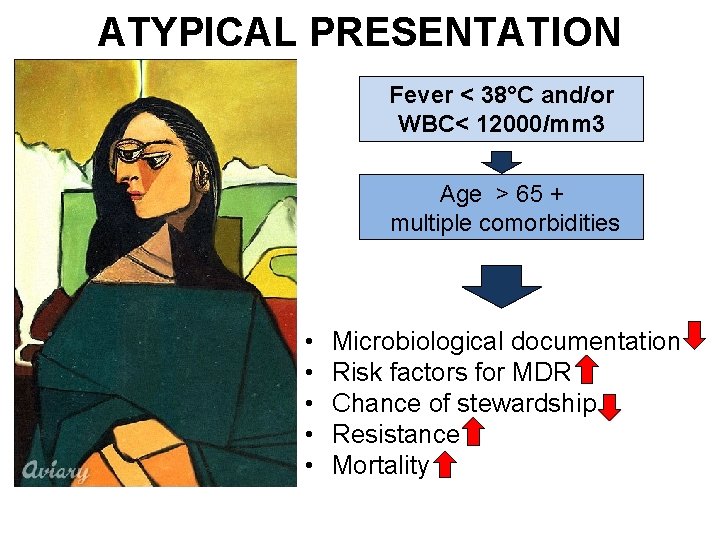
ATYPICAL PRESENTATION Fever < 38°C and/or WBC< 12000/mm 3 Age > 65 + multiple comorbidities • • • Microbiological documentation Risk factors for MDR Chance of stewardship Resistance Mortality
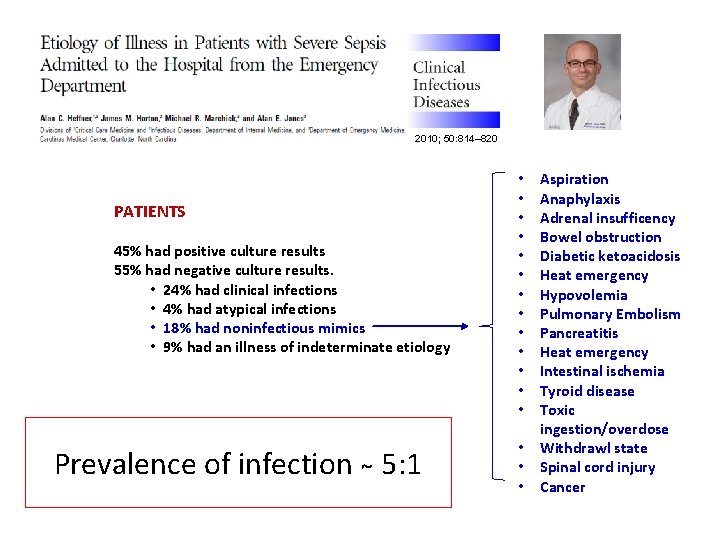
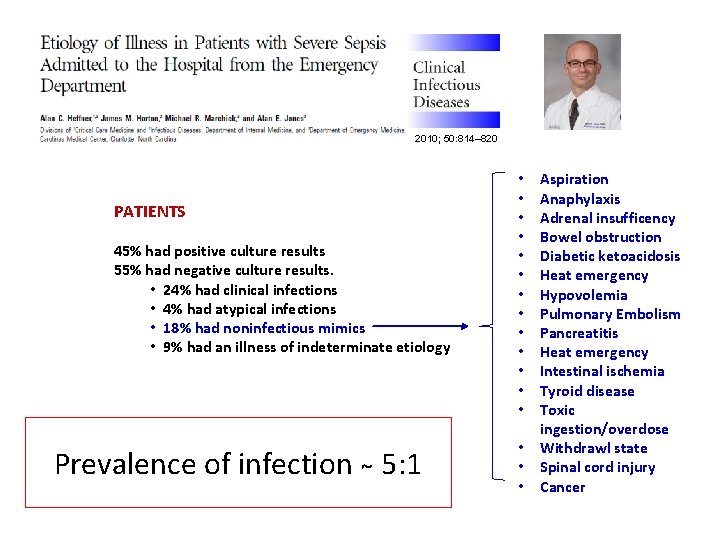
2010; 50: 814– 820 PATIENTS 45% had positive culture results 55% had negative culture results. • 24% had clinical infections • 4% had atypical infections • 18% had noninfectious mimics • 9% had an illness of indeterminate etiology Prevalence of infection 5: 1 • • • • Aspiration Anaphylaxis Adrenal insufficency Bowel obstruction Diabetic ketoacidosis Heat emergency Hypovolemia Pulmonary Embolism Pancreatitis Heat emergency Intestinal ischemia Tyroid disease Toxic ingestion/overdose Withdrawl state Spinal cord injury Cancer
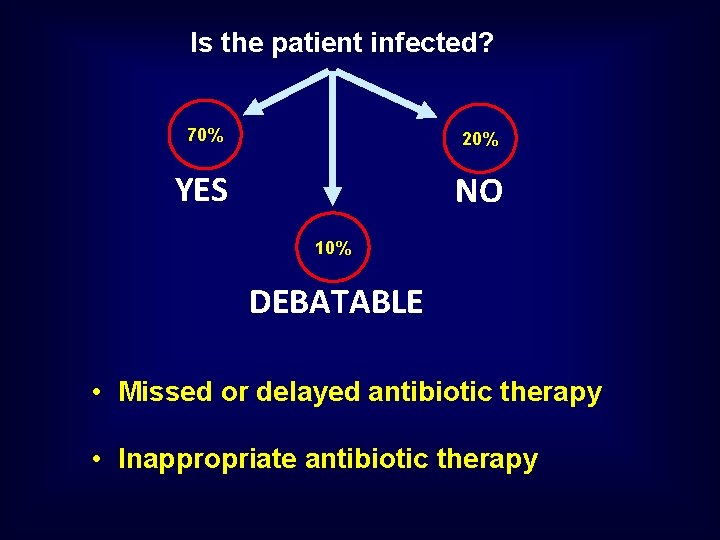
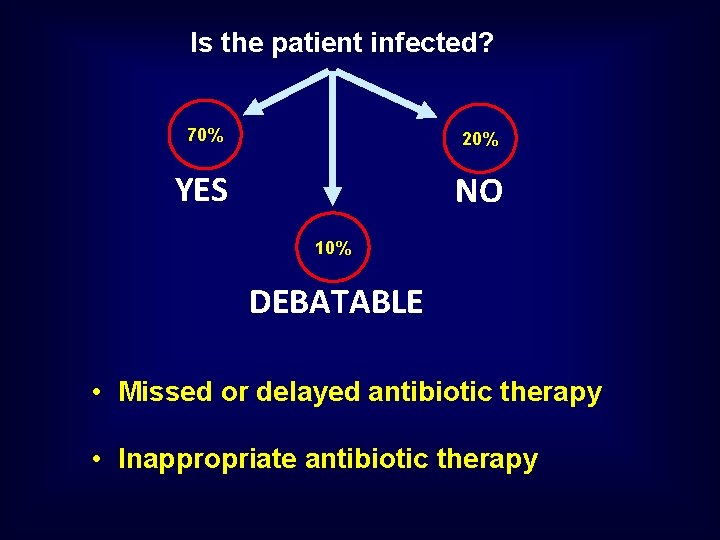
Is the patient infected? 70% 20% YES NO 10% DEBATABLE • Missed or delayed antibiotic therapy • Inappropriate antibiotic therapy
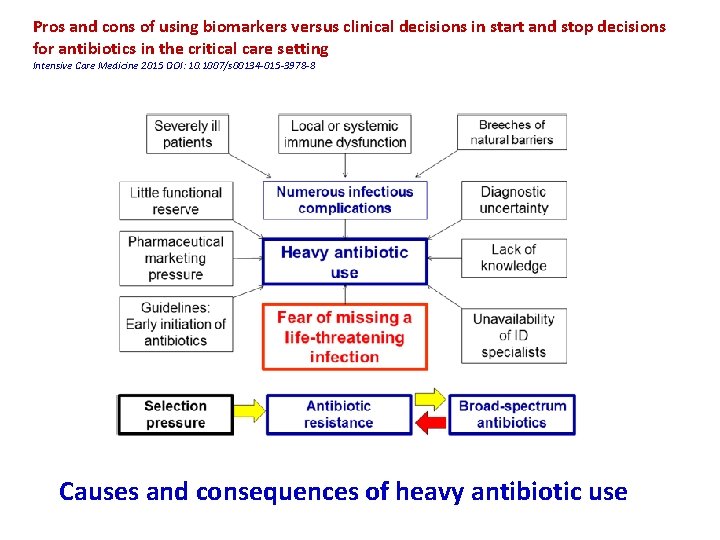
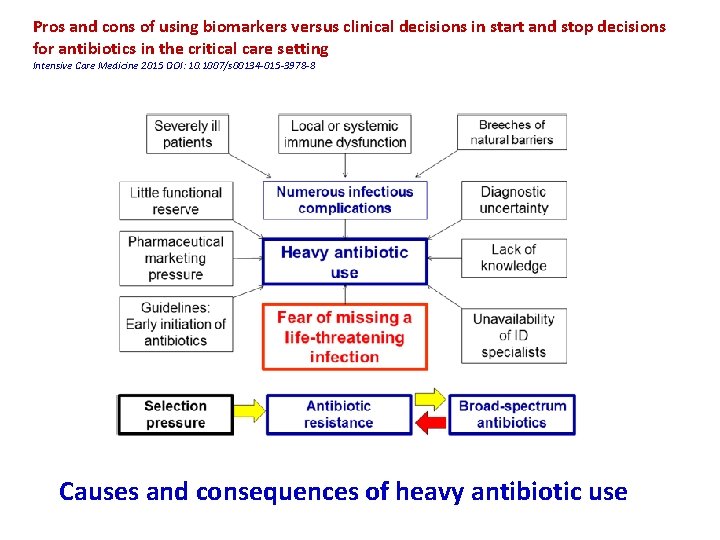
Pros and cons of using biomarkers versus clinical decisions in start and stop decisions for antibiotics in the critical care setting Intensive Care Medicine 2015 DOI: 10. 1007/s 00134 -015 -3978 -8 Causes and consequences of heavy antibiotic use
BIOMARKERS • • • Fast kinetics High sensitivity and specificty Fully automated technology Short turn around time Availability as point of care Low cost
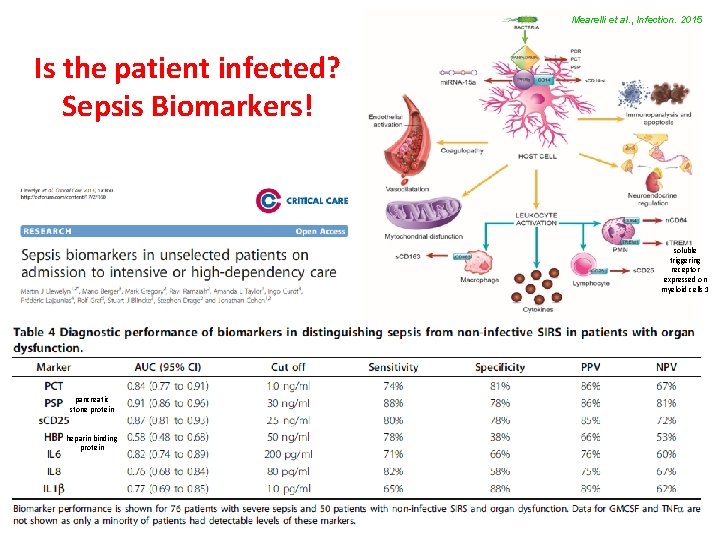
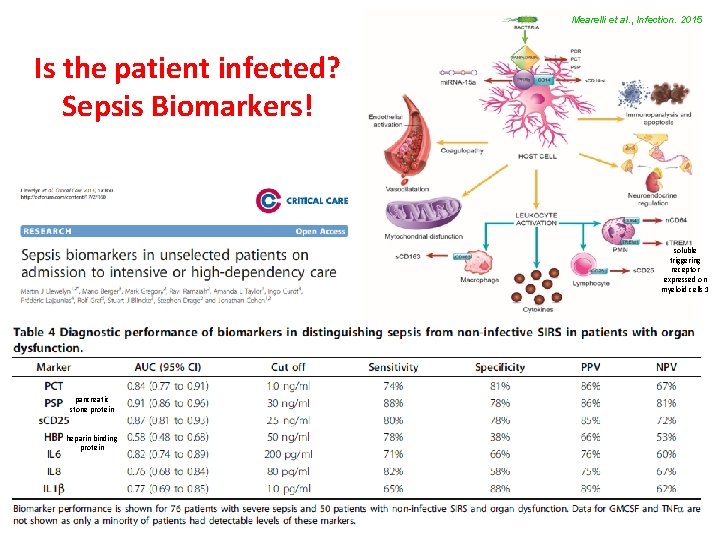
Mearelli et al. , Infection. 2015 Is the patient infected? Sepsis Biomarkers! soluble triggering receptor expressed on myeloid cells 1 pancreatic stone protein heparin binding protein
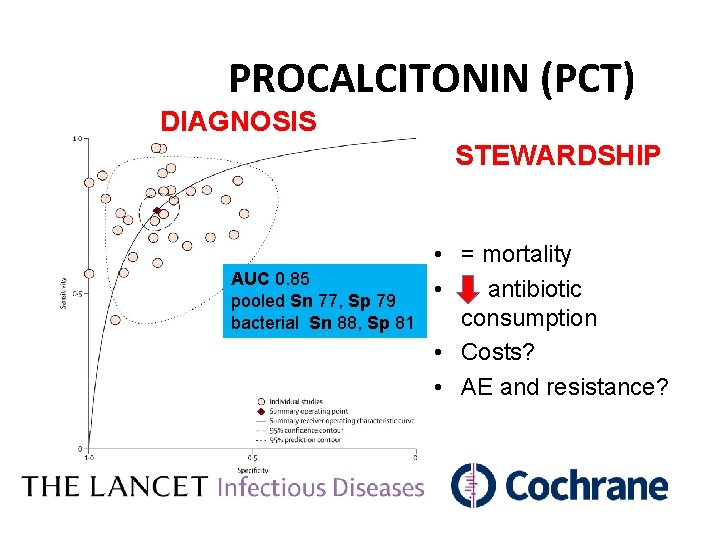
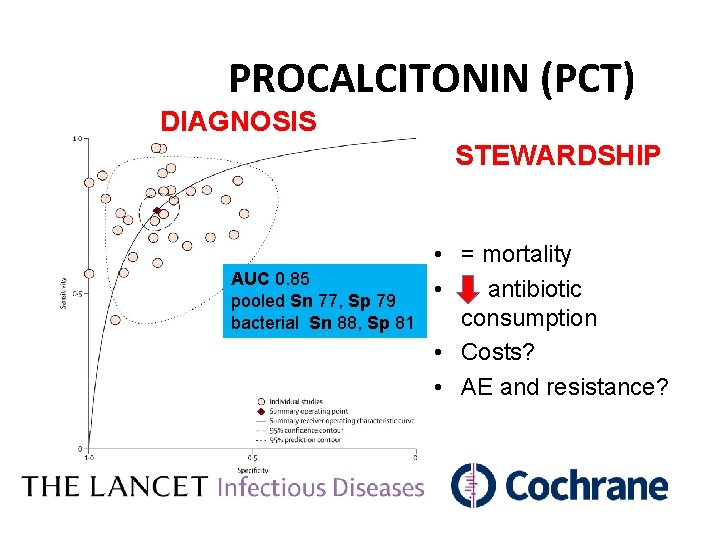
PROCALCITONIN (PCT) DIAGNOSIS STEWARDSHIP AUC 0. 85 pooled Sn 77, Sp 79 bacterial Sn 88, Sp 81 • = mortality • antibiotic consumption • Costs? • AE and resistance?
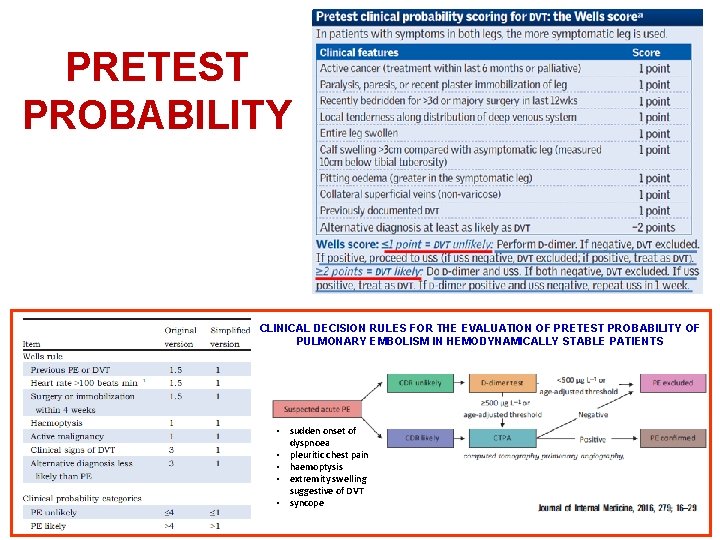
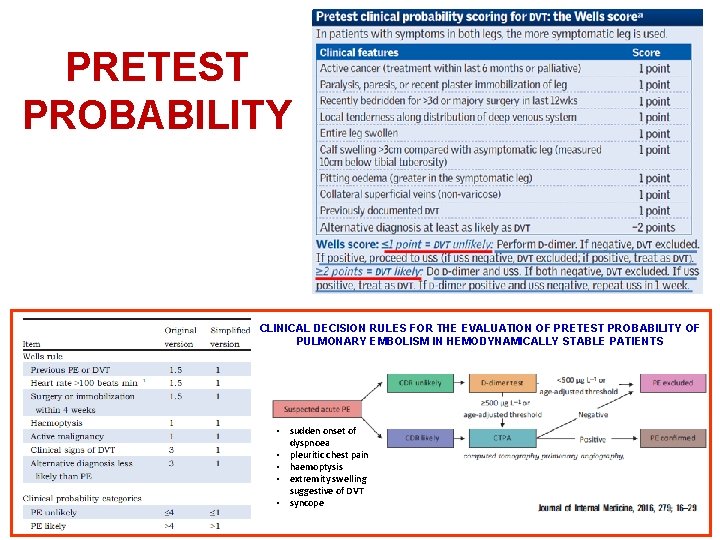
PRETEST PROBABILITY CLINICAL DECISION RULES FOR THE EVALUATION OF PRETEST PROBABILITY OF PULMONARY EMBOLISM IN HEMODYNAMICALLY STABLE PATIENTS • sudden onset of dyspnoea • pleuritic chest pain • haemoptysis • extremity swelling suggestive of DVT • syncope
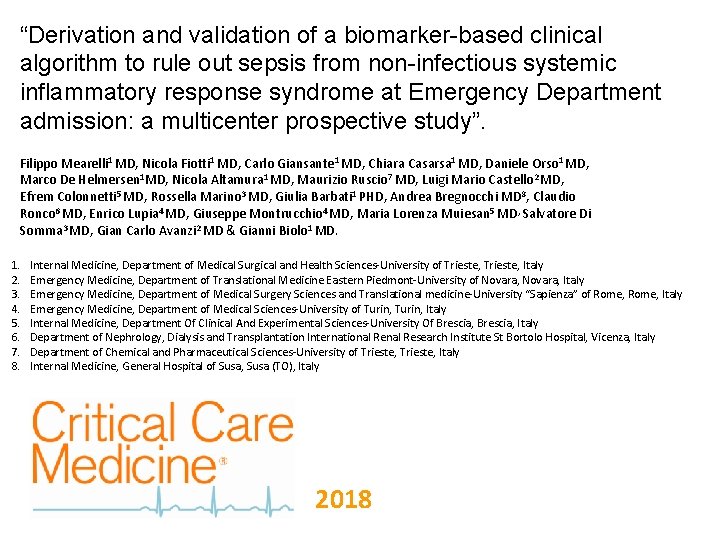
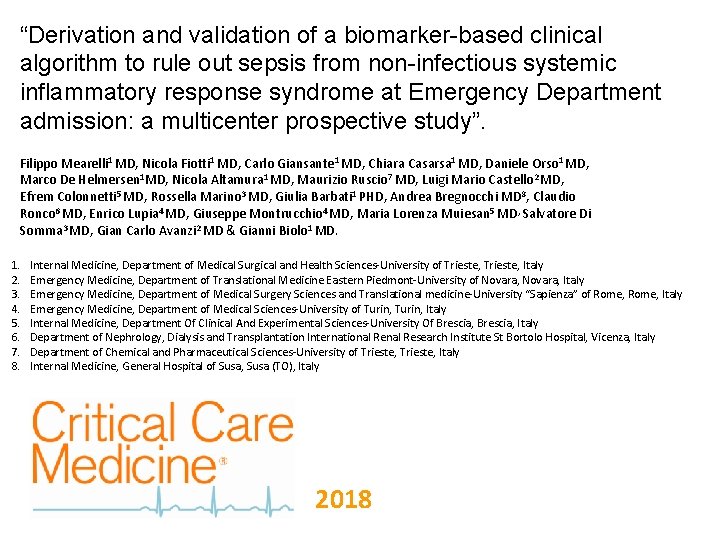
“Derivation and validation of a biomarker-based clinical algorithm to rule out sepsis from non-infectious systemic inflammatory response syndrome at Emergency Department admission: a multicenter prospective study”. Filippo Mearelli 1 MD, Nicola Fiotti 1 MD, Carlo Giansante 1 MD, Chiara Casarsa 1 MD, Daniele Orso 1 MD, Marco De Helmersen 1 MD, Nicola Altamura 1 MD, Maurizio Ruscio 7 MD, Luigi Mario Castello 2 MD, Efrem Colonnetti 5 MD, Rossella Marino 3 MD, Giulia Barbati 1 PHD, Andrea Bregnocchi MD 8, Claudio Ronco 6 MD, Enrico Lupia 4 MD, Giuseppe Montrucchio 4 MD, Maria Lorenza Muiesan 5 MD, Salvatore Di Somma 3 MD, Gian Carlo Avanzi 2 MD & Gianni Biolo 1 MD. 1. 2. 3. 4. 5. 6. 7. 8. Internal Medicine, Department of Medical Surgical and Health Sciences-University of Trieste, Italy Emergency Medicine, Department of Translational Medicine Eastern Piedmont-University of Novara, Italy Emergency Medicine, Department of Medical Surgery Sciences and Translational medicine-University “Sapienza” of Rome, Italy Emergency Medicine, Department of Medical Sciences-University of Turin, Italy Internal Medicine, Department Of Clinical And Experimental Sciences-University Of Brescia, Italy Department of Nephrology, Dialysis and Transplantation International Research Institute St Bortolo Hospital, Vicenza, Italy Department of Chemical and Pharmaceutical Sciences-University of Trieste, Italy Internal Medicine, General Hospital of Susa, Susa (TO), Italy 2018

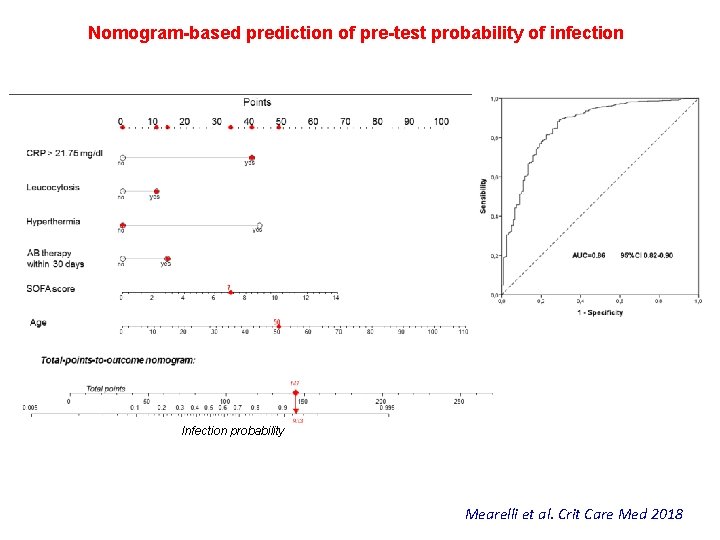
OBJECTIVE: to derive and validate an Experimental algorithm integrating a nomogram-based prediction of the pre-test probability of infection with a panel of serum biomarkers, which could robustly rule out sepsis/septic shock from noninfectious-SIRS. DESIGN: multicenter prospective study. SETTING: at Emergency Department admission in five University Hospitals. PATIENTS: 1132 consecutive patients with SIRS 947 adults in inception cohort 185 adults in validation cohort. Infections n=716 (%) 375 (52) 81 (73 -87) 3 (1 -4) 225 (31) Ni-SIRS n=120 (%) 61 (51) 72 (59 -83) 2 (1 -4) 2 (1 -3) 17 (14) 0. 768 0. 000 348 (49) 33 (5) 401 (56) 27 (4) 539 (75) 527 (74) 609 (85) 20 (17) 4 (3) 48 (40) 4 (3) 94 (78) 105 (87) 45 (37) 0. 000 0. 639 0. 001 1. 000 0. 565 0. 001 0. 000 0. 525 (0. 200 -3. 617) 14189 (8949 -23109) 399. 5 (270. 2 -649. 5) 31. 60 (25. 88 -35. 85) 500. 5 (313 -970. 5) 0. 127 (0. 077 -0. 2170) 9079 (5340 -16613) 283. 9 (215. 1 -499. 1) 11 (4. 15 -25. 62) 308 (194. 5 -529. 5) 0. 000 Severity of infection Uncomplicated infection Sepsis Septic shock 134 (19) 533 (74) 49 (7) - - Mortality§ 133 (19) 9 (7) 0. 002 Characteristics Male Median age (IQR) Median Charlson Index (IQR) Median SOFA score (IQR) Antibacterial therapy within 30 days Clinical variables Body temperature >38°C <36°C White blood cell count >12000/mm 3 <4000/mm 3 Respiratory rate >20/min or p. CO 2<32 mm. Hg Heart rate>90/min C Reactive Protein >21. 75 mg/dl Median BM at admission (IQR)^ PCT (ng/ml) s. CD 25 (pg/ml) s. TREM-1 (pg/ml) s. PLA 2 GIIA (ng/ml) Presepsin (pg/ml) Mearelli et al. Crit Care Med 2018 p
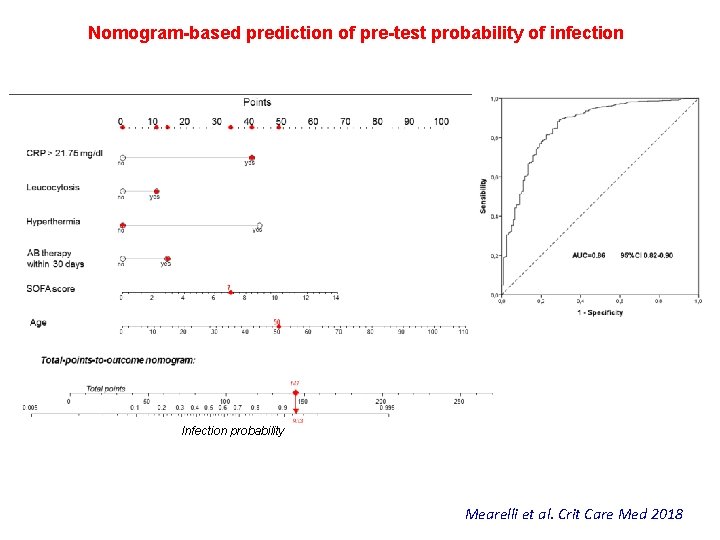
Nomogram-based prediction of pre-test probability of infection Infection probability Mearelli et al. Crit Care Med 2018
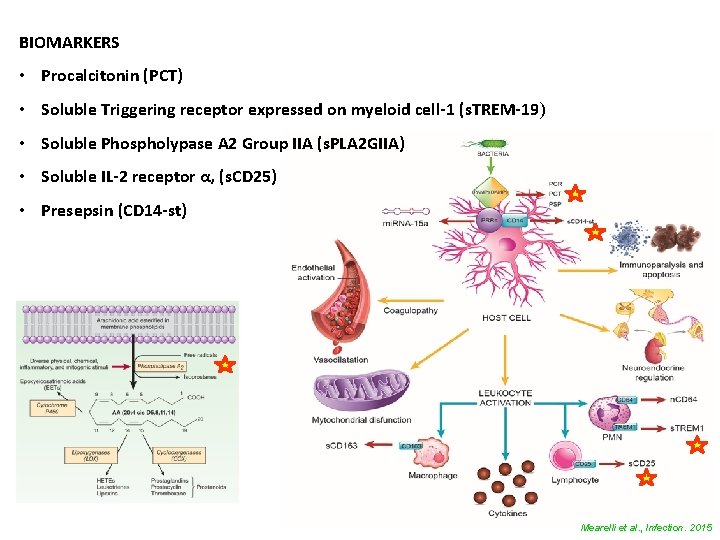
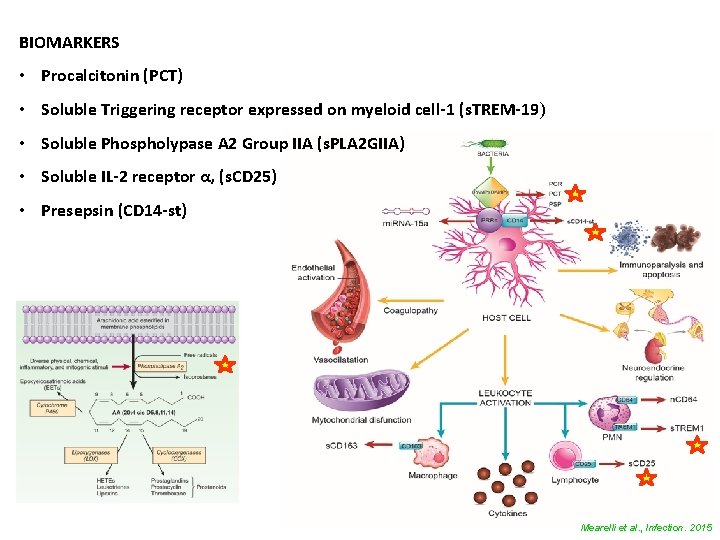
BIOMARKERS • Procalcitonin (PCT) • Soluble Triggering receptor expressed on myeloid cell-1 (s. TREM-19) • Soluble Phospholypase A 2 Group IIA (s. PLA 2 GIIA) • Soluble IL-2 receptor α, (s. CD 25) • Presepsin (CD 14 -st) Mearelli et al. , Infection. 2015
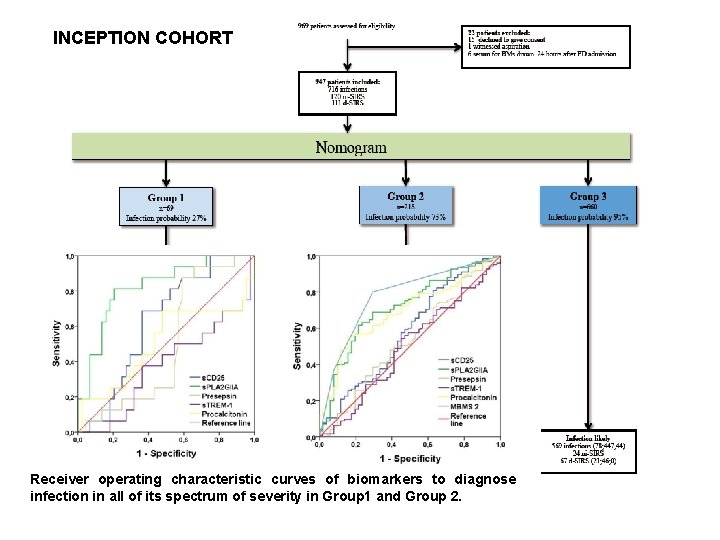
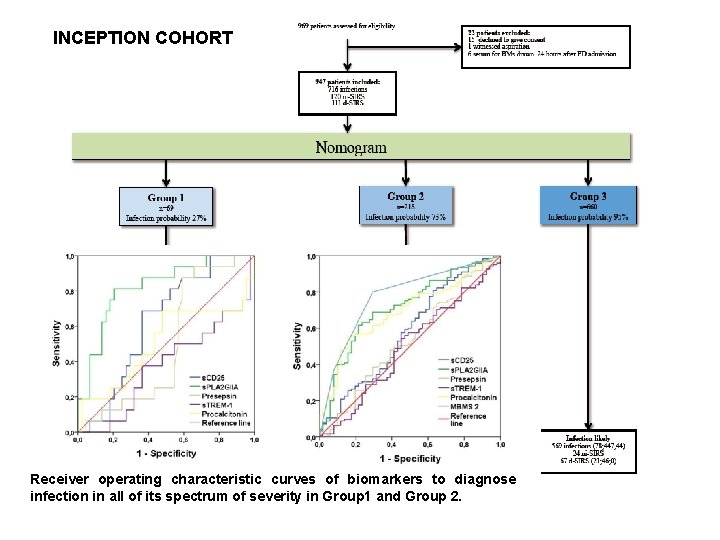
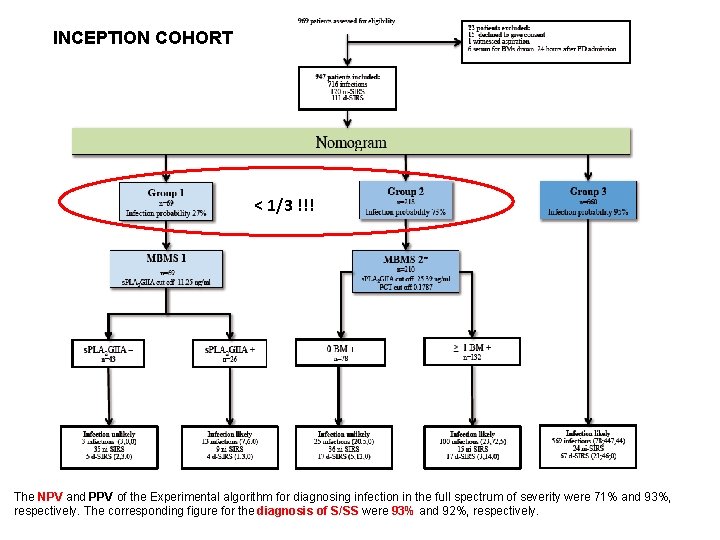
INCEPTION COHORT Receiver operating characteristic curves of biomarkers to diagnose infection in all of its spectrum of severity in Group 1 and Group 2.
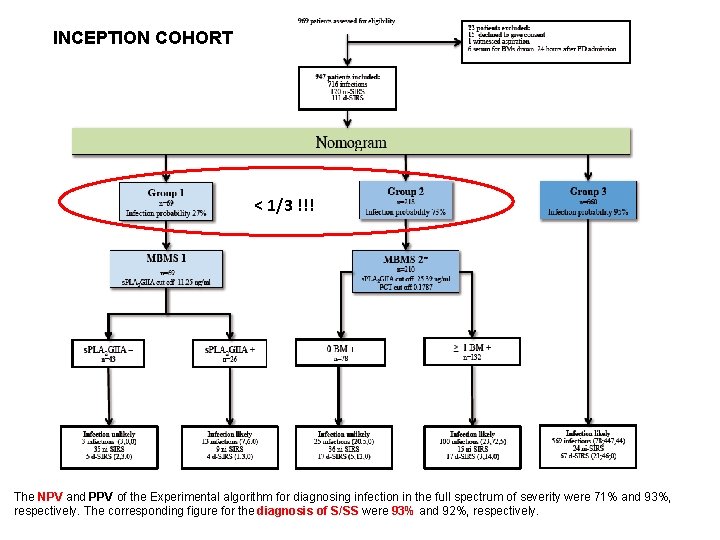
INCEPTION COHORT < 1/3 !!! The NPV and PPV of the Experimental algorithm for diagnosing infection in the full spectrum of severity were 71% and 93%, respectively. The corresponding figure for the diagnosis of S/SS were 93% and 92%, respectively.
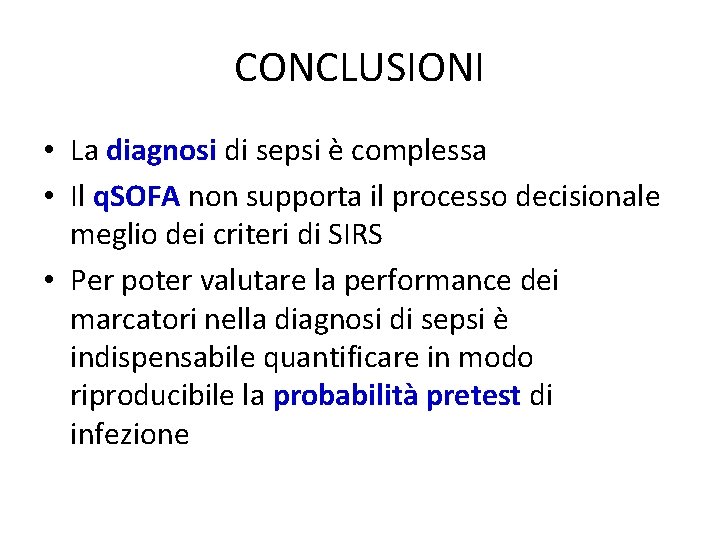
Experimental algorithm: final adjudication of the patients enrolled in inception and validation cohort Results False negative Full spectrum of infection severity Sepsis/septic shock False positive Inception cohort Validation cohort p 28/710 5/579 48/119 37/142 0/121 9/15 0. 28914 0. 30302 0. 14706 Inception vs validation cohort: comparison of false negative and false positive results In the whole population (1161 patients with SIRS), only 5 (0. 7%) patients with S/SS were misclassified
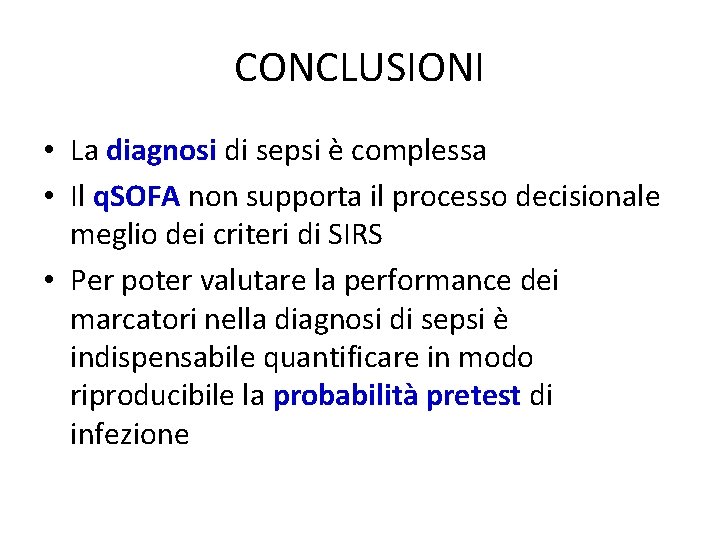
CONCLUSIONI • La diagnosi di sepsi è complessa • Il q. SOFA non supporta il processo decisionale meglio dei criteri di SIRS • Per poter valutare la performance dei marcatori nella diagnosi di sepsi è indispensabile quantificare in modo riproducibile la probabilità pretest di infezione
CONCLUSIONI • La combinazione di PCT e PLA 2 GII nei pazienti a non alta probabilità di infezione esclude la sepsi con un VPN del 93%. • La popolazione da testare per ottenere questo risultato è < 1/3.
 Incontro genitori prima comunione
Incontro genitori prima comunione Incontro tra oceano pacifico e atlantico
Incontro tra oceano pacifico e atlantico La relazione d'aiuto slide
La relazione d'aiuto slide Mcdonald criteria 2017
Mcdonald criteria 2017 Rossi aprile
Rossi aprile 20/4/1889
20/4/1889 Capacité pulmonaire totale
Capacité pulmonaire totale Il convertitore pneumo-idraulico
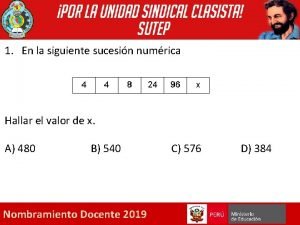
Il convertitore pneumo-idraulico Dada la siguiente secuencia rusia 2018 rusia 2018
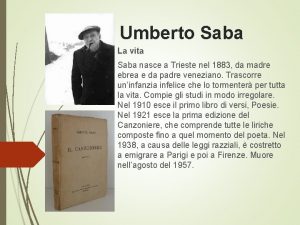
Dada la siguiente secuencia rusia 2018 rusia 2018 Saba goal zanichelli
Saba goal zanichelli Amai
Amai Istituto gestalt trieste
Istituto gestalt trieste Isc cupra ripatransone
Isc cupra ripatransone Z generation trieste
Z generation trieste Ssd trieste
Ssd trieste Villaggio del fanciullo trieste
Villaggio del fanciullo trieste Caritas trieste
Caritas trieste Lenormant
Lenormant Dico al mio cuore saba
Dico al mio cuore saba Stelle sulla terra trama
Stelle sulla terra trama Hotel savoia trieste
Hotel savoia trieste Renzo nicolini
Renzo nicolini Dipolarnost vode
Dipolarnost vode Tin yu
Tin yu Xin giữ con để con phụng sự chúa
Xin giữ con để con phụng sự chúa Mejor es pobre con honor que rico con
Mejor es pobre con honor que rico con Lluvia de palabras relacionadas con la paz
Lluvia de palabras relacionadas con la paz Problemi con percentuali e sconti con soluzioni
Problemi con percentuali e sconti con soluzioni Animales con rr
Animales con rr Talleres para padres con hijos discapacitados
Talleres para padres con hijos discapacitados Chúng con cầu xin nhờ đức kito con chúa
Chúng con cầu xin nhờ đức kito con chúa Imagenes de palabras con ba be bi bo bu
Imagenes de palabras con ba be bi bo bu Yo salgo con mis amigos
Yo salgo con mis amigos Con ca tụng chúa vì đã giải thoát con
Con ca tụng chúa vì đã giải thoát con Palabras con am em im om um
Palabras con am em im om um Dettato ortografico prima elementare
Dettato ortografico prima elementare Oracuones simples
Oracuones simples